Abstract
Purpose
Distance stereoacuity is used to monitor deterioration of intermittent exotropia (intermittent XT), but variability of stereoacuity has not been rigorously studied. The purpose of this study was to assess the variability of stereoacuity over one day, in children with intermittent XT.
Design
Prospective cohort study.
Methods
Setting: Clinical practice.
Patient population: Twelve children with intermittent XT.
Observation procedures: Stereoacuity was assessed using the Frisby Davis Distance and Distance Randot at distance and the Frisby and Preschool Randot at near. Tests were repeated 3 or 4 times over the day, with at least 2 hours between assessments.
Main outcome measure: ‘Variable’ stereoacuity defined as a change by 2 or more log levels between any 2 time points over the day.
Results
Variable stereoacuity at distance was found in 5 (42%) of 12 patients. Four (33%) of 12 patients were variable using Distance Randot test, 3 of whom also varied using Frisby Davis Distance. One patient was variable using Frisby Davis Distance only. Nine (75%) of 12 patients completed near stereoacuity testing; 2 (22%) of 9 showed variable near stereoacuity. Two (22%) of 9 were variable using Preschool Randot, 1 (11%) of whom also varied using Frisby. In some cases stereoacuity changed from measurable stereoacuity on one assessment to nil on another.
Conclusions
Nearly half of children with intermittent XT show marked changes in stereoacuity over the course of a single day. When based on isolated measures, an apparent change in distance stereoacuity between visits should be interpreted with caution.
Introduction
Intermittent exotropia (intermittent XT) is a relatively common form of childhood strabismus1, 2 characterized by intermittent divergent misalignment that is often greater at distance fixation. The natural history of intermittent XT and indications for surgery are not yet well defined3–6 but previous authors have suggested that progression of the disease is characterized by an increase in the angle of deviation,6, 7 decreasing control8, 9 and deteriorating distance stereoacuity.8, 10 Previous studies evaluating change in intermittent XT over time have compared isolated measures of angle, control and stereoacuity, implying that such isolated measures are sufficient to represent an individual patient at a given point in time. Nevertheless in a recent study by our group, 11 we reported that control can vary considerably over one day in some patients with intermittent XT. In the present study we evaluated the variability of stereoacuity over the course of one day in children with intermittent XT.
Methods
We previously reported11 variability of control in a cohort of 13 children with intermittent XT, prospectively enrolled from clinical practice. Twelve of these children (median age 8; range 3 to 13 years) also underwent measures of stereoacuity, at least 3 or 4 times over the course of the same day. As previously described,11 we excluded patients with convergence insufficiency type exotropia (near angle ≥10 prism diopters (pd) greater than distance) or co-existing ocular pathology. Assessments over the day were scheduled during the following time intervals: 08:00 – 10:30; 10:31 –13:00; 13:01 –15:30 and 15:31 – 18:00, allowing a minimum of 2 hours between assessments. Measures of control, stereoacuity and angle of deviation were performed at each assessment. At each testing point, the examiner did not have access to any results from prior exams on the same day or on previous clinic visits. The median of the 3 to 4 angle measurements for each patient (a summary of the angle of deviation for each patient) ranged from 12 to 42.5 pd (median 27.5 pd) at distance and 8 to 45 pd (median 20 pd) at near by alternating prism cover test (APCT). All tests were performed in habitual refractive correction. No patient had amblyopia which was defined as ≥ 0.2 LogMAR (Logarithm of the Minimum Angle of Resolution) inter-ocular difference and ≥0.3 LogMAR in one eye. Ability to comprehend all stereoacuity tasks was required for inclusion in this study. Testing was performed in the following order: Frisby Davis Distance, Distance Randot, Frisby, Preschool Randot.
Assessment of distance stereoacuity
We tested distance stereoacuity in all 12 patients, 3 or 4 times during the day, using 2 relatively new tests, the Frisby Davis Distance 12, 13 and Distance Randot.14 Both tests were administered according to previously described protocols13–15 but scores were converted to log seconds of arc to account for the non-linear progression in levels tested (Table 1).
Table 1.
Levels of stereoacuity showing equivalent log seconds of arc values, and where they follow a logarithmic progression. Actual levels tested on Frisby Davis Distance (FD2), Distance Randot (DR), Frisby and Preschool Randot (PSR) stereo tests are indicated by a checked box.
| Seconds of arc | Log of seconds of arc | FD2 test levels | DR test levels | Frisby test levels | PSR test levels |
|---|---|---|---|---|---|
| 20 | 1.30 | √* | |||
| 40 | 1.60 | √* | √ | √ | |
| 60 | 1.78 | √ | √ | √ | |
| 80 | 1.90 | √* | |||
| 100 | 2.00 | √* | √* | √* | |
| 160 | 2.20 | √* | |||
| 200 | 2.30 | √ | √* | √* | √* |
| 400 | 2.60 | † | √* | √* | √* |
| 800 | 2.90 | † | † | √* | |
| 1600 | 3.20 | † |
= Stereoacuity levels coinciding with logarithmic steps.
= Value assigned to represent ‘Nil’ since it follows the logarithmic progression. The next highest 0.3 log increment was chosen to represent nil for each test, because the highest measurable level differs between tests. Choosing the same log value to represent nil for all tests would introduce bias when comparing differences between tests, for example the difference between the highest measurable level and nil.
The Frisby Davis Distance, a real depth test, was tested at disparities of 200, 160, 80, 40 and 20 seconds of arc. At each disparity level, 2 out of 2 correct responses were required to pass. Threshold was recorded as the finest disparity at which 2 out of 2 shapes were correctly identified, as reported by Holmes and Fawcett.13 Due to the possibility of monocular cues providing false positive responses at thresholds of 200-80 seconds of arc,13 these levels were reassessed monocularly, as described previously.13 This monocular testing phase, carried out once threshold had been reached, was performed to ensure the threshold score reflected a binocular response. No patient in our study achieving a threshold of 200-80 seconds of arc was able to achieve this level monocularly confirming that responses reflected true binocular stereoacuity. Patients unable to respond at the 200 seconds of arc level were recorded as having ‘nil’ stereo. For analysis, ‘nil’ stereo was assigned the next highest log level i.e. 2.60 log seconds of arc (Table 1).
The Distance Randot, a Polaroid vectograph, was tested at disparities of 400, 200, 100 and 60 seconds of arc.14, 15 At each disparity level, 2 out of 2 correct responses were required to pass. Threshold was recorded as the finest disparity at which 2 out of 2 shapes were correctly identified. Patients unable to identify shapes at the 400 seconds of arc level were recorded as having ‘nil’ stereo. For analysis, ‘nil’ stereo was assigned the next highest log level i.e. 2.90 log seconds of arc (Table 1). A monocular testing phase was not performed for the Distance Randot test since it does not appear to have a problem with monocular cues.
Patients were classified as having ‘variable’ stereoacuity if there was a change of 2 or more log levels (≥ 0.6 log seconds of arc) between any time points over the day on either the Frisby Davis Distance or the Distance Randot test (Table 1). Patients who did not change by 2 or more log levels on either test were classified as ‘stable’.
Assessment of near stereoacuity
Nine of 12 patients completed at least 3 measures of stereoacuity with both Frisby and Preschool Randot tests over course of the day. Both tests were administered according to previously described protocols15–17 and scores were converted to log seconds of arc for the purposes of analysis.
The Frisby, a real depth test, was administered at a range of distances (as previously described)15, 17 to yield disparities of 400, 200, 100, 60 and 40 seconds of arc. At each disparity level, 2 out of 2 correct responses were required to pass. Threshold was recorded as the finest disparity at which 2 out of 2 presentations were correctly identified. Patients unable to respond at the 400 seconds of arc level were recorded as having ‘nil’ stereo. For analysis, ‘nil’ stereo was assigned the next highest log level i.e. 2.90 log seconds of arc (Table 1).
The Preschool Randot, a Polaroid vectograph, was performed at 40cms, testing disparities of 800, 400, 200, 100, 60 and 40 seconds of arc. At each disparity level, 2 out of 3 correct responses were required to pass. Threshold was recorded as the finest disparity at which 2 out of 3 shapes were correctly identified. Patients unable to identify shapes at the 800 seconds of arc level were recorded as having ‘nil’ stereo. For analysis, ‘nil’ stereo was assigned the next highest log level i.e. 3.20 log seconds of arc (Table 1). A monocular testing phase was not performed for either the Frisby or the Preschool Randot tests since previous studies have confirmed that these tests do not have a problem with monocular cues.17, 18
As described for distance tests, patients were classified as showing ‘variable’ stereoacuity if there was a change of 2 or more log levels (≥ 0.6 log seconds of arc) between any time points over the day on either the Frisby or the Preschool Randot. Patients who did not change by 2 or more log levels on either test were classified as ‘stable’.
Assessment of angle
At each assessment, the angle of deviation was measured by alternating prism cover test (ACT) at distance (3 meters) and near (1/3 meter) fixation. A change in angle was defined as a difference of ≥ 10 prism diopters (pd) between any measurements over the day. Patients showing a change of ≥10 pd at distance or near fixation, were classified as showing a ‘variable’ angle of deviation.
Assessment of control
Control was assessed at each time point as described in our recent report.11 Control was scored using a previously described scale for both distance (3 meters) and near (1/3 meter) fixation.19 Control assessment followed the standard testing procedure reported previously, 11, 19 commencing with observation for spontaneous tropia over a 30 second time period (score 5 = constant tropia, score 3 = tropia for <50% of observed time). If no spontaneous tropia was observed, recovery of phoria was rated as the poorest of 3, 10-second periods of occlusion (score 2 = >5 second recovery, score 0 = <1 second recovery). Patients were categorized as showing ‘variable’ control if a change of ≥ 2 levels on the scale occurred over the course of the day.11 Individual patients were analyzed to determine whether those showing variable distance control over the day also showed variable distance stereoacuity and whether those showing variable near control also showed variable near stereoacuity. In addition, for all patients, we assessed agreement between distance stereoacuity values and the distance control score, and between near stereoacuity values and the near control score, at each time point over the day.
Results
Distance stereoacuity
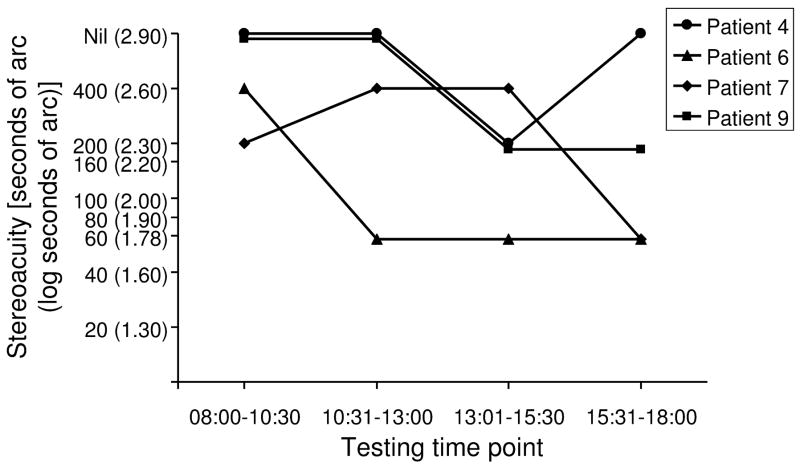
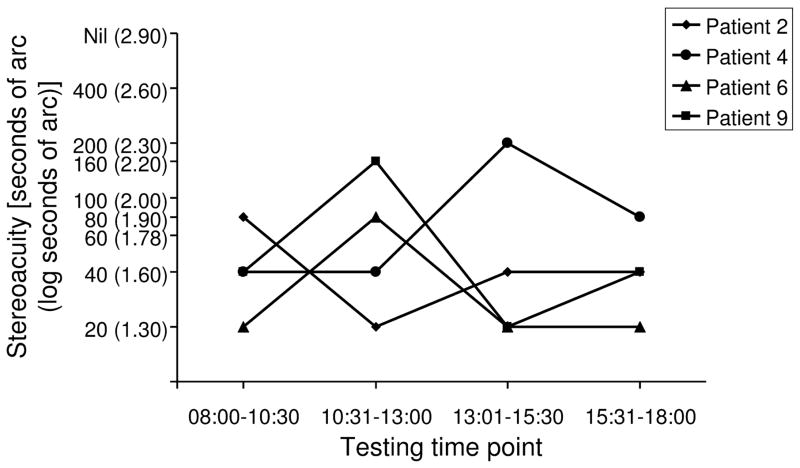
Five (42%) of 12 patients showed variable stereoacuity on either Frisby Davis Distance or Distance Randot over the course of the day (supplemental material available at www.ajo.com): 4 (33%) of 12 were variable using the Distance Randot test, 3 of whom also varied using the Frisby Davis Distance. Of the 4 who varied using the Distance Randot, 2 changed between no measurable (‘nil’) and subnormal stereoacuity (Figure 1). Similar, marked variability was seen using the Frisby Davis Distance test (Figure 2) but not to the level of ‘nil’. For both tests, change was not consistently in the direction of either progressive improvement or progressive deterioration. The age of those with variable stereoacuity was not significantly younger than those with stable distance stereoacuity (median 10 vs 8 years; p=0.6, Wilcoxon)
Figure 1.
Variable stereoacuity using the Distance Randot test. Stereoacuity values are shown at 4 testing time points over one day in the 4 (33%) of 12 patients who showed variability using the Distance Randot test. Variable stereoacuity was defined as a change of 2 or more log levels (≥ 0.6 log seconds of arc) between any testing time points over the day.
Figure 2.
Variable stereoacuity using the Frisby Davis Distance test. Stereoacuity values are shown at 4 testing time points over one day in the 4 (33%) of 12 patients who showed variability using the Frisby Davis test. Variable stereoacuity was defined as a change of 2 or more log levels (≥0.6 log seconds of arc) between any testing time points over the day.
Near stereoacuity
Two (22%) of 9 patients showed variable near stereoacuity over the day. Both children varied using the Preschool Randot; 1 also varied using the Frisby (supplemental material available at www.ajo.com). Of the 2 who varied on the Preschool Randot, 1 changed from ‘nil’ to measurable stereoacuity.
Angle of deviation
Three (25%) of the 12 patients showed a change in angle (≥ 10 prism diopters) either for distance or near fixation over the day. Of the 3 showing variability, all 3 varied at near and 1 also varied at distance. No correlation was found between distance angle of deviation and either Frisby Davis Distance stereoacuity (r= −0.04, P=0.8, Spearman) or Distance Randot stereoacuity (r=0.2, P=0.2). No correlation was found between near angle of deviation and either Frisby stereoacuity (r=0.2, P=0.2) or Preschool Randot stereoacuity (r=0.3, P=0.08).
Control
Of the 5 patients showing variable stereoacuity using distance tests, none showed variable distance control over the day. Of the 2 patients showing variable stereoacuity using near tests, 1 (50%) of 2 showed variable control at near over the day. Across all patients, there was no correlation between the stereoacuity scores on the Frisby Davis Distance and the distance control score at the same assessment time point (r=−0.09, P=0.5, Spearman) or between stereoacuity on the Distance Randot and distance control scores at the same assessment time point (r=−0.2, P=0.1). Likewise there was no correlation between the near control score and stereoacuity scores on the Frisby (r=0.08, P=0.7). There was marginal correlation between near control score and stereoacuity measured using the Preschool Randot (r=0.35, P=0.05).
Discussion
Distance stereoacuity varies considerably over the course of one day in some patients with intermittent XT, including change from absent (nil measurable) on one assessment to measurable on another. The pattern of change was not consistently towards improvement over the day, suggesting this was not a practice effect, or towards deterioration, suggesting it was not due to fatigue. Variability occurred on the ‘real-life’ Frisby Davis Distance and Frisby tests as well as on the random dot Distance Randot and Preschool Randot tests.
Worsening distance stereoacuity has been suggested as an objective measure of change in the underlying severity of intermittent XT and as a means of evaluating the need for surgery.8–10, 20 Nevertheless we found marked variability in stereoacuity measures within a single day. Changes from 20 to 80 seconds of arc, 40 to 200 seconds of arc and 200 seconds of arc to nil occurred in our subjects, changes that might have previously been considered clinically significant. Our findings suggest that isolated measures of stereoacuity may not be a reliable means of representing severity or detecting change over time in an individual patient with intermittent XT.
Previous studies examining distance stereoacuity in intermittent XT used a different method of measuring stereoacuity10, 20, 21 (Mentor B-VAT which is no longer commercially available) and showed improvements in distance stereoacuity post operatively. A recent study by our group also found that, using the Frisby Davis Distance and Distance Randot tests in a cohort of patients with intermittent XT, overall distance stereoacuity thresholds improved post operatively22. Nevertheless, the findings of this present study suggest that isolated measures of stereoacuity should be interpreted with caution and that multiple measures may be needed to better capture true stereoacuity status and guide surgical decision making.
Near stereoacuity is generally expected to be normal in patients with intermittent XT 10, 15, 20, 23 although it may be reduced in cases with co-existing monofixation syndrome.24 While mostly within normal limits and stable in our study, it is of note that some patients showed variability even of near stereoacuity over the day.
One possible explanation for variable stereoacuity is variability of angle but none of the 5 patients with variable distance stereoacuity had a variable angle of deviation at distance fixation. At near, 1 (50%) of 2 patients with variable near stereoacuity had a variable angle at near fixation and so overall there appeared to be no relationship between variable angle and variable stereoacuity.
Another possible explanation for the variable stereoacuity found in this study, is that changes reflect test retest reliability. There are limited data on the test retest reliability of stereo tests in children, but Fawcett et al,25 studying the Pre school Randot test, reported the 95% limits of agreement for inter-observer reliability to be approximately 0.3 log seconds of arc. This value falls well within the ≥ 0.6 log seconds of arc range chosen to define variability in our study, suggesting we did indeed detect ‘real’ change in stereoacuity values. Establishing limits of agreement based on test retest data in pediatric populations for the Frisby, Frisby Davis Distance and Distance Randot stereotests, would enable more accurate identification of real changes in stereoacuity. An alternative explanation for our findings is that subtle, but real sensory changes occur throughout day and that this fluctuation is a normal, but previously unreported feature of intermittent XT. If this were true, one might expect to find associated changes in other parameters such as the angle of deviation or ability to control.
Although we have recently reported variability of control in some of these cases11 we did not find it to be associated with changes in stereoacuity. It remains uncertain whether control and stereoacuity are inter-related: some authors10, 23, 26, 27 suggest that the level of stereoacuity is indeed correlated to the degree of control and others10, 15 that it is not. In this present study we generally did not find a relationship between the degree of control and the level of stereoacuity with the exception of a marginal correlation between near stereoacuity measured by Preschool Randot and near control. In addition, for a given patient, the presence of variable control did not necessarily coexist with variable stereoacuity i.e. most patients with variable control had stable stereoacuity or vice versa. We have observed that some patients with constant exotropia at distance (score 5) during the control assessment, appear ‘straight’ when testing stereoacuity seconds later. Therefore simultaneous assessment of control and stereoacuity may be needed to properly evaluate a potential relationship between stereoacuity and control.
The possibility of a relationship between stereoacuity and angle of deviation has not been extensively studied in intermittent XT, but our findings appear consistent with other reports26, 28 that there is no obvious correlation between the two.
The findings of this study highlight one of the primary, on-going challenges for studies of intermittent XT - the lack of well-defined measures of severity. If stereoacuity and control can vary considerably over one day, it would seem impossible for clinicians to be sure they are capturing real change in a patient’s underlying condition, when based on an isolated measure from visit to visit. Further work establishing reliable outcome measures is necessary before embarking on much needed natural history and interventional studies.
There are a number of weaknesses to our study. A small number of patients were studied which, while unlikely to alter our main finding that stereoacuity varies over one day in a proportion of patients, may have limited our ability to detect relationships between stereoacuity and angle or control. In light of what we now know about variability of control11 the possibility of a relationship between control and stereoacuity may be better addressed by measuring control and stereoacuity simultaneously. The young age of the patients in our study may have contributed to variability in attention which may have led to variable stereoacuity. As suggested in our previous report on variable control,11 the lack of progressive deterioration towards the end of the day argues against a marked effect of attention or fatigue. Nevertheless, we did not monitor whether or not children rested between assessments which, had they done so, may have negated any effect of fatigue. Whether stereoacuity and control vary due to attention, fatigue, test retest reliability or some other reason some patients show marked changes in stereoacuity and control over short periods of time. It may be that such fluctuations are an integral part of childhood intermittent XT.
Our finding of variable stereoacuity over one day in some patients with intermittent XT suggests that isolated measures of stereoacuity cannot be relied upon to represent severity or change in severity over time. For individual patients with intermittent XT, isolated measures of stereoacuity should be interpreted with caution.
Table 2.
Frisby Davis Distance (FD2) and Distance Randot (DR) stereoacuity measured over one day in children with intermittent exotropia.
| Time 1 FD2 | Time 2 FD2 | Time 3 FD2 | Time 4 FD2 | Time 1 DR | Time 2 DR | Time 3 DR | Time 4 DR | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient number | 08:00–10:30 | 10:31–13:00 | 13:01–15:30 | 15:31–18:00 | 08:00–10:30 | 10:31–13:00 | 13:01–15:30 | 15:31–18:00 | ||||||||
| Secarc | Log | Secarc | Log | Secarc | Log | Secarc | Log | Secarc | Log | Secarc | Log | Secarc | Log | Secarc | Log | |
| 1 | 20 | 1.30 | - | - | 40 | 1.60 | 20 | 1.30 | 60 | 1.78 | - | - | 60 | 1.78 | 200 | 2.30 |
| †2 | 80 | 1.90 | 20 | 1.30 | 40 | 1.60 | 40 | 1.60 | 100 | 2.00 | 100 | 2.00 | 100 | 2.00 | 100 | 2.00 |
| 3 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 80 | 1.90 | 60 | 1.78 | 60 | 1.78 | 60 | 1.78 | 60 | 1.78 |
| †*4 | 40 | 1.60 | 40 | 1.60 | 200 | 2.30 | 80 | 1.90 | nil | 2.90 | nil | 2.90 | 200 | 2.30 | nil | 2.90 |
| 5 | 20 | 1.30 | 20 | 1.30 | 40 | 1.60 | 20 | 1.30 | 200 | 2.30 | 200 | 2.30 | 60 | 1.78 | 100 | 2.00 |
| †*6 | 20 | 1.30 | 80 | 1.90 | 20 | 1.30 | 20 | 1.30 | 400 | 2.60 | 60 | 1.78 | 60 | 1.78 | 60 | 1.78 |
| *7 | 40 | 1.60 | 40 | 1.60 | 20 | 1.30 | 20 | 1.30 | 200 | 2.30 | 400 | 2.60 | 400 | 2.60 | 60 | 1.78 |
| 8 | 20 | 1.30 | 20 | 1.30 | 20 | 1.30 | 20 | 1.30 | 60 | 1.78 | - | - | 60 | 1.78 | 60 | 1.78 |
| †*9 | 40 | 1.60 | 160 | 2.20 | 20 | 1.30 | 40 | 1.60 | nil | 2.90 | nil | 2.90 | 200 | 2.30 | 200 | 2.30 |
| 10 | 20 | 1.30 | 20 | 1.30 | 20 | 1.30 | 40 | 1.60 | 60 | 1.78 | 60 | 1.78 | 60 | 1.78 | 60 | 1.78 |
| 11 | 40 | 1.60 | 20 | 1.30 | 40 | 1.60 | 20 | 1.30 | nil | 2.90 | nil | 2.90 | nil | 2.90 | nil | 2.90 |
| 13 | 20 | 1.30 | 20 | 1.30 | 20 | 1.30 | 40 | 1.60 | 60 | 1.78 | 60 | 1.78 | 60 | 1.78 | 60 | 1.78 |
= patients with variable distance stereoacuity (defined as a change of 2 or more log levels (≥ 0.6 log seconds of arc) over the day) using the Distance Randot test.
= patients with variable distance stereoacuity (defined as a change of 2 or more log levels (≥ 0.6 log seconds of arc) over the day) using the Frisby Davis Distance test.
= not tested
Table 3.
Near Frisby and Preschool Randot stereoacuity measured over one day in children with intermittent exotropia.
| Time 1 Frisby | Time 2 Frisby | Time 3 Frisby | Time 4 Frisby | Time 1 PSR | Time 2 PSR | Time 3 PSR | Time 4 PSR | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient number | 08:00–10:30 | 10:31–13:00 | 13:01–15:30 | 15:31–18:00 | 08:00–10:30 | 10:31–13:00 | 13:01–15:30 | 15:31–18:00 | ||||||||
| Secarc | Log | Secarc | Log | Secarc | Log | Secarc | Log | Secarc | Log | Secarc | Log | Secarc | Log | Secarc | Log | |
| 2 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 60 | 1.78 | 40 | 1.60 | 60 | 1.78 |
| †*4 | 60 | 1.78 | 200 | 2.30 | 400 | 2.60 | 200 | 2.30 | nil | 3.20 | 100 | 2.00 | 100 | 2.00 | 100 | 2.00 |
| 5 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 100 | 2.00 | 40 | 1.60 | 40 | 1.60 | - | - |
| 6 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 |
| 7 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 |
| 9 | 60 | 1.78 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 |
| 10 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 60 | 1.78 | 60 | 1.78 | 60 | 1.78 | 60 | 1.78 |
| *11 | 60 | 1.78 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 200 | 2.30 | 100 | 2.00 | 100 | 2.00 | 400 | 2.60 |
| 13 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 | 40 | 1.60 |
= patients with variable near stereoacuity (defined as a change of 2 or more log levels (≥ 0.6 log seconds of arc) over the day) using the Preschool Randot test.
= patients with variable near stereoacuity (defined as a change of 2 or more log levels (≥ 0.6 log seconds of arc) over the day) using the Frisby test.
= not tested.
Acknowledgments
Funding/Support: Supported by National Institutes of Health Grants EY015799, EY011751 (JMH), Research to Prevent Blindness, Inc., New York, NY (JMH as Olga Keith Weiss Scholar and an unrestricted grant to the Department of Ophthalmology, Mayo Clinic), and Mayo Foundation, Rochester, MN.
Supported by: National Institutes of Health Grants EY015799 and EY011751 (JMH), Research to Prevent Blindness, Inc., New York, NY (JMH as Olga Keith Weiss Scholar and an unrestricted grant to the Department of Ophthalmology, Mayo Clinic), and Mayo Foundation, Rochester, MN.
Footnotes
Institutional Review Board/Ethics Committee approval was obtained for this study through the Mayo Clinic College of Medicine. All experiments and data collection were conducted in a manner compliant with the Health Insurance Portability and Accountability Act.
Financial disclosures: No conflicting financial relationships exist
Supplemental material available at: www.ajo.com
Contributions of authors: Design of study (JMH, BGM); Conduct of study (JMH, BGM, SRH, DAL); Collection (JMH, BGM, SRH); Management (JMH, BGM, SRH, DAL); Analysis (JMH, SRH, DAL); Interpretation of data (JMH, SRH, BGM, DAL); Preparation/review of manuscript (JMH, SRH, BGM, DAL)
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Govindan M, Mohney BG, Diehl NN, Burke JP. Incidence and types of childhood exotropia. A population-based study. Ophthalmology. 2005;112:104–108. doi: 10.1016/j.ophtha.2004.07.033. [DOI] [PubMed] [Google Scholar]
- 2.Mohney BG, Huffaker RK. Common forms of childhood exotropia. Ophthalmology. 2003;110:2093–2096. doi: 10.1016/j.ophtha.2003.04.001. [DOI] [PubMed] [Google Scholar]
- 3.Hatt S, Gnanaraj L. Interventions for intermittent exotropia. Cochrane Database Syst Rev. 2006;19:CD003737. doi: 10.1002/14651858.CD003737.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Abroms AD, Mohney BG, Rush DP, Parks MM, Tong PY. Timely surgery in intermittent and constant exotropia for superior sensory outcome. Am J Ophthalmol. 2001;131:111–116. doi: 10.1016/s0002-9394(00)00623-1. [DOI] [PubMed] [Google Scholar]
- 5.Romanchuk KG, Dotchin SA, Zurevinsky J. The natural history of surgically untreated intermittent exotropia–looking into the distant future. J AAPOS. 2006;10:225–231. doi: 10.1016/j.jaapos.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 6.Nusz KJ, Mohney BG, Diehl NN. The course of intermittent exotropia in a population-based cohort. Ophthalmology. 2006;113:1154–1158. doi: 10.1016/j.ophtha.2006.01.033. [DOI] [PubMed] [Google Scholar]
- 7.Kii T, Nakagawa T. Natural history of intermittent exotropia–statistical study of preoperative strabismic angle in different age groups. Nippon Ganka Gakkai Zasshi. 1992;96:904–909. [PubMed] [Google Scholar]
- 8.Santiago AP, Ing MR, Kushner BJ, Rosenbaum AL. Intermittent exotropia. In: Rosenbaum AL, Santiago AP, editors. Clinical Strabismus Management Principles and Surgical Techniques. Philadelphia: W.B. Saunders Company; 1999. pp. 163–175. [Google Scholar]
- 9.von Noorden GK, Campos EC. Exodeviations. In: von Noorden GK, Campos EC, editors. Binocular Vision and Ocular Motility. Theory and Management of Strabismus. 6. St. Louis: Mosby; 2002. pp. 356–376. [Google Scholar]
- 10.Stathacopoulos RA, Rosenbaum AL, Zanoni D, et al. Distance stereoacuity. Assessing control in intermittent exotropia. Ophthalmology. 1993;100:495–500. doi: 10.1016/s0161-6420(93)31616-7. [DOI] [PubMed] [Google Scholar]
- 11.Hatt SR, Mohney BG, Leske DA, Holmes JM. Variability of Control in Intermittent Exotropia. Ophthalmology. 2007 doi: 10.1016/j.ophtha.2007.03.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adams WE, Hrisos S, Richardson S, Davis H, Frisby JP, Clarke MP. Frisby Davis distance stereoacuity values in visually normal children. Br J Ophthalmol. 2005;89:1438–1441. doi: 10.1136/bjo.2005.071761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holmes JM, Fawcett SL. Testing distance stereoacuity with the Frisby-Davis 2 (FD2) test. Am J Ophthalmol. 2005;139:193–195. doi: 10.1016/j.ajo.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 14.Fu VL, Birch EE, Holmes JM. Assessment of a new distance Randot stereoacuity test. J AAPOS. 2006;10:419–423. doi: 10.1016/j.jaapos.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 15.Holmes JM, Birch EE, Leske DA, Fu VL, Mohney BG. New tests of distance stereoacuity and their role in evaluating intermittent exotropia. Ophthalmology. 2007;114:1215–1220. doi: 10.1016/j.ophtha.2006.06.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Birch E, Williams C, Hunter J, Lapa MC ALSPAC “Children in Focus” Study Team. Random dot stereoacuity of preschool children. J Pediatr Ophthalmol Strabismus. 1997;34:217–222. doi: 10.3928/0191-3913-19970701-08. [DOI] [PubMed] [Google Scholar]
- 17.Leske DA, Holmes JM. Maximum angle of horizontal strabismus consistent with true stereopsis. J AAPOS. 2004;8:28–34. doi: 10.1016/j.jaapos.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 18.Holmes JM, Leske DA. Monocular clues in tests of stereoacuity. V. Nurnberg, Germany: Berufsverband der Orthoptistinnen Deutchlands; 1999. pp. 103–106. [Google Scholar]
- 19.Mohney BG, Holmes JM. An office-based scale for assessing control in intermittent exotropia. Strabismus. 2006;14:147–150. doi: 10.1080/09273970600894716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O’Neal TD, Rosenbaum AL, Stathacopoulos RA. Distance stereo acuity improvement in intermittent exotropic patients following strabismus surgery. J Pediatr Ophthalmol Strabismus. 1995;32:353–357. doi: 10.3928/0191-3913-19951101-06. [DOI] [PubMed] [Google Scholar]
- 21.Yildirim C, Mutlu FM, Chen Y, Altinsoy HI. Assessment of central and peripheral fusion and near and distance stereoacuity in intermittent exotropic patients before and after strabismus surgery. Am J Ophthalmol. 1999;128:222–230. doi: 10.1016/s0002-9394(99)00079-3. [DOI] [PubMed] [Google Scholar]
- 22.Adams WE, Leske DA, Hatt SR, et al. Improvement in distance stereoacuity following surgery for intermittent exotropia. J AAPOS. 2007 doi: 10.1016/j.jaapos.2007.09.015. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yildirim C, Altinsoy HI. Distance alternate-letter suppression test for objective assessment of sensorial status in intermittent exotropia. Eur J Ophthalmol. 2000;10:4–10. doi: 10.1177/112067210001000102. [DOI] [PubMed] [Google Scholar]
- 24.Baker JD, Davies GT. Monofixational intermittent exotropia. Arch Ophthalmol. 1979;97:93–95. doi: 10.1001/archopht.1979.01020010033007. [DOI] [PubMed] [Google Scholar]
- 25.Fawcett SL, Birch EE. Interobserver test-retest reliability of the Randot preschool stereoacuity test. J AAPOS. 2000;4:354–358. doi: 10.1067/mpa.2000.110340. [DOI] [PubMed] [Google Scholar]
- 26.Hatt SR, Haggerty H, Buck D, Adams WE, Strong NP, Clarke MP. Distance Stereoacuity in Intermittent Exotropia. Br J Ophthalmol. 2006 doi: 10.1136/bjo.2006.099465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buck D, Hatt SR, Haggerty HHS, Strong NP, Steen NICMP. The use of the Newcastle control score in the management of intermittent exotropia. Br J Ophthalmol. 2006;91:215–218. doi: 10.1136/bjo.2006.097790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Walsh LA, LaRoche GR, Tremblay F. The use of binocular visual acuity in the assessment of intermittent exotropia. J AAPOS. 2000;4:154–157. [PubMed] [Google Scholar]