Abstract
It has been proposed that activation of Toll-like receptors (TLRs) plays crucial roles in the polarization of adaptive immune responses. A synthetic Toll-like receptor 2 (TLR2) ligand, Pam3CSK4, has been reported to modulate the balance of Th1/Th2 responses. We evaluated the modulation effect of Pam3CSK4 on allergic immune response in a mouse rhinitis model sensitized to house dust mite allergen (HDM). Mice were sensitized and challenged with Dermatophagoides farinae allergen (Der f), and then the allergic mice were treated by Pam3CSK4. Nasal allergic symptoms and eosinophils were scored. Der f-specific cytokine responses were examined in the splenocytes and bronchoalveolar lavage fluid (BALF). Serum level of total IgE was also detected. After establishing a mouse allergic rhinitis model with HDM, we have showed that Pam3CSK4 treatment not only ameliorated the nasal allergic symptoms remarkably but also decreased the eosinophils and total inflammation cells in BALF significantly. Analysis of cytokine profile found that IFN-γ released from either BALF or stimulated splenocytes increased markedly in Pam3CSK4-treated mice, while IL-13 decreased significantly. Moreover, serum level of total IgE was significantly lower in Pam3CSK4-treated mice than in the untreated. Thus, in an allergic rhinitis mouse model developed with HDM, Pam3CSK4 was shown to exhibit an antiallergic effect, indicating its potential application in allergic diseases.
Keywords: Toll-like receptor 2 (TLR2), Ligand, Allergic immune response, Mite allergen
INTRODUCTION
The incidence of allergic diseases increases rapidly during last 20 years, especially in developed countries. It was explained by the hygiene hypothesis, that is, exposure to microbes or their products earlier in life results in decreased atopic sensitization (Liu, 2007; Tse and Horner, 2008). The mechanism underlying this relationship is still unkown.
Recently, the Toll-like receptor (TLR) family, a phylogenetically conserved structure in innate immunity, attracted considerable interest from immunologists. The components mainly derived from the microbes, named as pathogen-associated molecular patterns (PAMPs), are recognized by TLRs. At least ten members of TLRs have been identified in human, expressed in both innate and adaptive immune systems. Triggering of TLRs by different microbial components was able to modulate the adaptive immune response in host. Originally it was thought that the signaling via TLRs usually preferred to enhancement of Th1 response (Schnare et al., 2001), but accumulating evidence suggests that the effect of the TLR signaling on Th1/Th2 responses is more complicated (Agrawal et al., 2003; Phipps et al., 2007; Redecke et al., 2004). In terms of allergy, the signaling via TLR2, TLR4 and TLR9 is more important. It has been demonstrated that TLR9-triggering CpG-DNA has great therapeutic potentials for allergic diseases (Kline, 2007). Studies in TLR4 signaling showed that stimulation of TLR4 by relatively high dose of lipopolysaccharide reduced allergic inflammation in a murine model of asthma (Rodriguez et al., 2003). However, the role of TLR2 signaling in allergy remains controversial, since several studies reported that TLR2 ligands administered to murine models of allergy during the sensitization period led to an enhancement of Th2-mediated allergic inflammation (Chisholm et al., 2004; Redecke et al., 2004), while others showed TLR2 activation with its ligands suppressed Th2-type responses and IgE production in animal models either before or after airway allergen challenge (Patel et al., 2005; Revets et al., 2005).
TLR2 recognizes components from a variety of microorganisms including lipoproteins, peptidoglycan and lipoteichoic acid mainly from Gram-negative bacteria. Analysis of TLR2-deficient mice showed that TLR2 is critical to the recognition of peptidoglycan and lipoproteins (Takeda et al., 2003). To date, it was suggested that TLR2 might play a key role in the development of allergy, because epidemic studies in children of farmers found that those children with a decreased risk of developing allergies have increased levels of TLR2 mRNA (Lauener et al., 2002), while TLR2 mRNA decreased in animal allergic model (Liu et al., 2006). In addition, gene polymorphism of TLR2 has been verified to be a major factor affecting the susceptibility to asthma and allergies in children of farmers (Eder et al., 2004). Previous studies on the role of TLR2 signaling usually used ovalbumin as allergen to develop the animal models. However, ovalbumin is not an aeroallergen, but a food allergen. Respiratory diseases naturally provoked by ovalbumin are not common in human. Recent studies suggest that the relationship between TLR stimulation and allergic responses is more complex, perhaps antigen-, timing-, dose- and type of TLR ligand-dependent (Berin et al., 2006; Wu et al., 2007). Thus, in the present study, we used the most common inhalant allergen in China (Wen, 2006), the house dust mite allergen (HDM), to develop a murine model of allergic rhinitis and to evaluate the effect of a synthetic TLR2 ligand, Pam3CSK4, on the established allergic immune response.
MATERIALS AND METHODS
Animals
Six- to eight-week-old female BALB/c mice were purchased from the Experimental Animal Center of Zhejiang University (Hangzhou, China). They are all kept under pathogen-free condition in the Laboratory of Animal Facility, Medical College of Zhejiang University.
Reagents
Dermatophagoides farinae (Der f) crude body extract (Medical Acarology Laboratory of Medical School, Fudan University, Shanghai, China) was used as the allergen, which was lyophilized and stored in 4 °C and dissolved in PBS before use. Synthetic bacterial lipopeptide Pam3CSK4 (InvivoGen, San Diego, California, USA) was prepared in sterile PBS.
Establishment of the allergic rhinitis model using Der f and treatment with Pam3CSK4
Mice were divided into three groups: control, allergic rhinitis, and Pam3CSK4 treatment. Each group contains 6 mice. Mice were sensitized via intraperitoneal injection (IP) with 100 µg of Der f and 1 mg of alum in 0.2 ml of PBS. A boosting injection was given on Day 7 with the same reagents. On Days 14~20, mice were challenged with Der f (1 µg/µl, 20 µl per mouse) via intranasal instillation for consecutively 7 d. For the control group, mice were sensitized and challenged with PBS in place of Der f. In the Pam3CSK4 treatment group, the mice were sensitized and challenged in the same way as in the allergic rhinitis group, but Pam3CSK4 (100 µg per mouse) was injected intraperitoneally once 1 d before the final allergen inhalant. Der f-allergic and negative control mice were given PBS via the same route.
Cytokine profile release by Der f-stimulated splenocytes in vitro
Splenocytes were isolated from mice after sacrificed on Day 21. They were cultured in RPMI-1640 medium containing 10% FCS at 2×106 cells/ml with Der f (50 µg/ml) stimulation at 37 °C and 5% CO2. After 72 h incubation, the supernatants of cells were collected and the concentrations of IL-13 and IFN-γ were assayed by commercial ELISA kits according to procedure protocols (R & D Systems, Minneapolis, MN, USA).
Bronchoalveolar lavage fluid (BALF)
Immediately after anesthesia, BALF was obtained as described in the following. Briefly, the right lung was lavaged in situ using two aliquots of 0.8 ml of PBS. The lavage of each mouse was kept on ice, then the BALF was centrifuged at 1500 r/min for 5 min, and the supernatant was aliquoted and stored at −70 °C for the detections of IFN-γ and IL-13. The BALF cell pellet was then resuspended in 1 ml of PBS and counted using a hemocytometer. The slides were made using a Cytospin (Shandon, UK) and were stained with Giemsa. Total cells and eosinophils in BALF were counted.
Total IgE detection
The levels of total IgE in mouse sera were detected by ELISA kit (BD Bioscience, San Jose, California, USA).
Evaluation of allergic symptoms
The numbers of sneezing and nose rubbing motions during 30 min after the final allergen challenge were recorded in each experimental group.
Statistical analysis
All the results were expressed as mean±SD. Comparison of means between different groups was performed using the Mann-Whitney U test or the two-tailed unpaired t test. Statistical significance was defined by P<0.05.
RESULTS
Allergic symptoms decreased significantly in Pam3CSK4-treated mice
The severity of allergic rhinitis was evaluated by two nasal symptoms, sneezing and nose rubbing. In our pilot experiments, the allergic symptoms exacerbated gradually since Day 14 after allergen challenge, and reached the peak during Days 20~30. Therefore, we administered Pam3CSK4 intraperitoneally once 1 d before final allergen challenge. As shown in Table 1, allergic symptoms in both Der f-allergic rhinitis and Pam3CSK4-treated mice are significantly higher than those of PBS mice (P<0.001), indicating that the animal model of allergic rhinitis is established. When compared with the Der f-allergic rhinitis mice, both the numbers of sneezing and nose rubbing decreased significantly in the Pam3CSK4-treated mice (Table 1), suggesting that activation of TLR2 signaling by Pam3CSK4 alleviated the allergic symptoms induced by HDM.
Table 1.
The numbers of sneezing and nose rubbing in different groups
| Numbers of sneezing | Numbers of nose rubbing | |
| Der f-allergic rhinitis group | 30.0±5.7** | 19.8±4.2** |
| Pam3CSK4 treatment group | 16.3±4.1**Δ | 12.2±2.8**Δ |
| PBS group | 4.6±1.6 | 2.3±1.2 |
P<0.001, as compared with PBS group
P<0.01, as compared with Der f-allegic group
Every group contained 6 mice
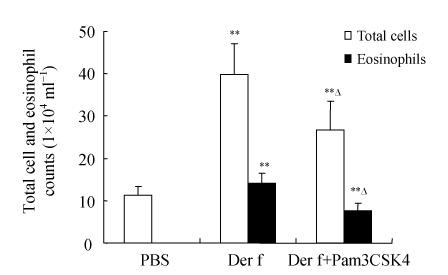
Pam3CSK4 treatment decreased the inflammatory cells in the BALF
Since the inflammatory cells, especially eosinophils, play a crucial role in allergic diseases, immediately after anesthesia, the BALF of each mouse was obtained. The BALF total cells and eosinophils were counted. The results show that either the number of total cells or eosinophils was significantly higher in the Der f-allergic rhinitis mice than in PBS mice (Fig.1, P<0.001). Moreover, after treatment with Pam3CSK4, both the total cells and eosinophils fell down markedly (P<0.01) as compared with the untreated Der f-allergic mice (Fig.1), indicating that Pam3CSK4 is able to attenuate allergic inflammation induced by HDM.
Fig. 1.
Total cell and eosinophil counts in BALF decreased significantly after Pam3CSK4 treatment
Pam3CSK4 was given to allergic mice once 1 d before the last intranasal challenge. ** P<0.001, as compared with PBS mice; ∆ P<0.01, as compared with untreated Der f-allergic mice
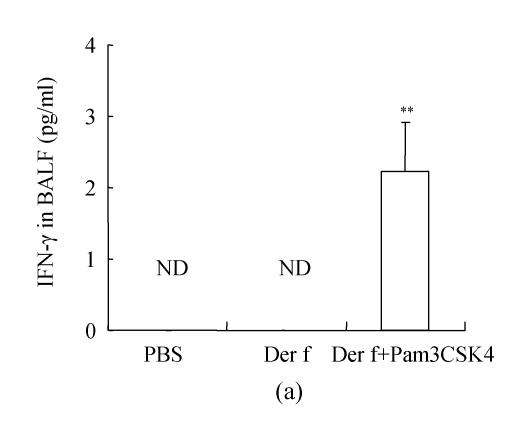
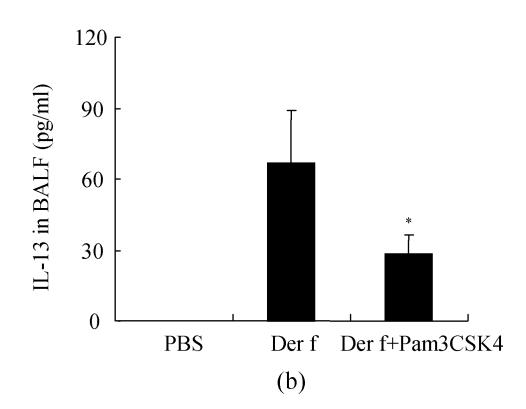
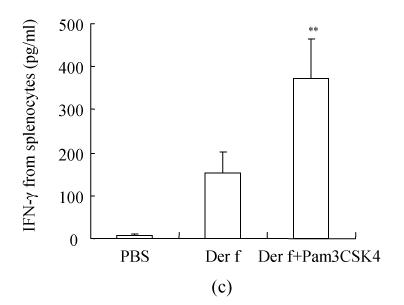
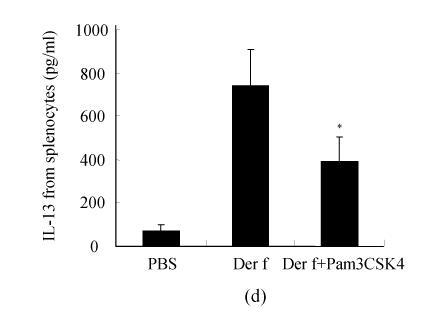
Cytokine profile analysis after Pam3CSK4 treatment
The role of TLR2 signaling in allergic inflammation is a current debating topic. How TLR2 stimulation modulates the balance of Th1/Th2 immune responses is not well defined, maybe varying with the allergic model, strain, dose and timing. To characterize the polarization of the immune response after Pam3CSK4 treatment, IFN-γ and IL-13 were measured as indications of Th1 and Th2 responses, respectively. In BALF, IFN-γ could not be detected in both Der f-allergic rhinitis and PBS mice, whereas detected in 5 out of 6 mice of Pam3CSK4 treatment group (Fig.2a). Consistent with the result, the IFN-γ release from Der f-stimulated splenocytes was also significantly higher in Pam3CSK4-treated mice than in Der f-allergic rhinitis and PBS mice (Fig.2c). As for Th2 cytokine, IL-13 decreased significantly in the Pam3CSK4-treated mice as compared with the Der f-allergic rhinitis mice in both BALF and culture supernatant of splenocyte (Figs.2b and 2d). Therefore, TLR2 stimulation by Pam3CSK4 induced the release of IFN-γ and reduced the release of IL-13, indicating that the Pam3CSK4 treatment to the established allergic mice model could skew the allergic Th2 response to Th1 response. Thus, Pam3CSK4 might be used as Th1 adjuvant in a therapeutic vaccine in the prevention and treatment of allergy.
Fig. 2.
Pam3CSK4 enhanced IFN-γ and inhibited IL-13 productions. (a) IFN-γ in BALF; (b) IL-13 in BALF; (c) IFN-γ released from splenocytes stimulated with Der f; (d) IL-13 released from splenocytes stimulated with Der f
** P<0.001 and * P<0.01, as compared with untreated Der f-allergic rhinitis mice. ND: Not detected
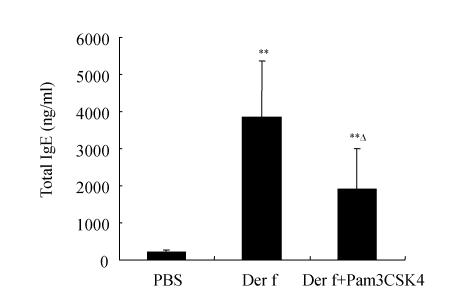
Pam3CSK4 treatment decreased the total level of IgE in allergic mice sera
IgE is the central antibody in the induction of allergy and a consequence of an extreme Th2 immune response. In order to know whether Th1 response induced by Pam3CSK4 could down-regulate the subsequent IgE synthesis, we detected the total IgE in mouse sera. The results show that serum total IgE levels were elevated in both the Der f-allergic group and the Pam3CSK4 treatment group as compared with the control group (P<0.001, Fig.3). Moreover, the level of total IgE decreased significantly in Pam3CSK4-treated mice compared with untreated Der f-allergic mice (Fig.3, P<0.05), indicating that the effect of Pam3CSK4 on the allergic immune response is rather rapid and efficient.
Fig. 3.
The total serum IgE decreased remarkably after Pam3CSK4 treatment
** P<0.001, as compared with PBS mice; ∆ P<0.05, as compared with untreated Der f-allergic rhinitis mice
DISCUSSION
The central goal in immunotherapy for allergic diseases is to develop more effective, safer and long-lasting therapeutical strategy. To reach this goal, scientists focus their interest on modulation of the skewed Th2 response toward a more balance Th1/Th2 response, since allergic diseases are strongly associated with Th2 immune response (Zhang et al., 2007). In order to stimulate the immune system towards a Th1 response, several approaches can be done such as strengthening the Th1 response by the addition of recombinant Th1 cytokines, CpG DNA, and blocking a Th2 type response with an antagonist against specific receptors. Recent studies have demonstrated that the activation of several TLR signaling was able to decrease allergic response and direct the balance of the immune system in favor of the Th1 response, representing a potential therapeutic strategy for the control of allergy. In the present study, based on the establishment of a mouse rhinitis model sensitized to the mite allergen, we have clearly showed that Pam3CSK4 as a TLR2 agonist is able to down-regulate the allergic parameters including the allergic symptoms, antigen-induced airway eosinophilia, IL-13 and IgE antibodies; however, it up-regulates IFN-γ production, indicating the therapeutic role of Pam3CSK4 in HDM-induced allergic rhinitis.
Although ovalbumin is the most commonly used allergen to develop animal models of allergy, we chose HDM to develop our animal model. We believe that the establishment of allergic animal model sensitized to HDM offers more clinical utility in studying the aetiology and treatment of inhalation allergies (Sarpong et al., 2003), and since HDM is more natural and common inhalant allergen than ovalbumin, this mouse allergic model should be more clinically relevant. More importantly, most of mite allergens are enzymes, and their enzymatic activities have been demonstrated to be required for the induction of Th2 and IgE responses (Akiba et al., 2006; Chapman et al., 2007). Recent study has showed that basophils are essential for TH2 responses induced by immunization with allergen as they were directly activated by protease allergens and produced Th2-inducing cytokines, including interleukin 4 (IL-4) and thymic stromal lymphopoietin (TSLP) (Sokol et al., 2008). Generally, basophils constitute 1%~2% of peripheral blood leukocytes and are not normal constituents of the lymph node. After immunization with protease allergen(s), basophils are activated and recruited to the draining lymph node where TSLP is produced, the important inducer of Th2 differentiation in vivo and in vitro (Sokol et al., 2008). Therefore, in our immunization protocol, sensitizing the mice via IP is easier and faster to initiate mouse sensitization due likely to much more lymph nodes distributed intraperitoneally. Although initiating mouse sensitization via nasal inhalation instead of IP route may be more relevant to human allergic to HDM, we have tried, but failed, in duration of a month. We speculate that it might need much longer time to establish a murine allergic model via nasal inhalant, perhaps since lymph tissues in nostril are not as plentiful as those in peritoneum. Our results show a significant increase in allergic symptoms, eosinophilia, total IgE and IL-13 in Der f-allergic rhinitis mice, suggesting that the mouse allergic rhinitis model in our experiments is successfully established.
The findings in our study strongly suggest that allergic rhinitis sensitized to HDM is inhibited by Pam3CSK4, since the allergic symptoms, airway eosinophils, serum total IgE and IL-13 reduced significantly in Pam3CSK4 treatment group compared with the allergic rhinitis group, while IFN-γ increased. Previous studies have evaluated the effect of TLR2 signaling on allergic diseases, but the results are conflicting. In our model, triggering of TLR2 with Pam3CSK4 showed a beneficial antiallergic effect on allergic rhinitis, which is consistent with several previous studies (Akdis et al., 2003; Patel et al., 2005; Revets et al., 2005). The mechanism of its antiallergic effect is still elusive. TLR2 has been reported as an important pattern recognition receptor (PRR) on regulatory T cells (Tregs) and the CD4+ CD25+ Treg subset in TLR2-deficient mice is significantly reduced compared to wild type mice, suggesting a relationship between Tregs and TLR2 (Sutmuller et al., 2006). However, Patel et al.(2005) reported that, by using blocking antibodies, the antiallergic effect of Pam3CSK4 was independent of IL-10 or TGF-β, but critically dependent on IL-12, and hence, Tregs are unlikely to play an important role in the therapeutic effect of Pam3CSK4. Therefore, it was suggested that TLR2 activation by Pam3CSK4 stimulates the antigen-presenting cells to secrete cytokines such as IL-12 and IFN-γ, which causes the enhancement of IFN-γ synthesis by T cells, resulting in decreased Th2 cell differentiation and attenuated eosinophilic airways inflammation, which might be the same as activation of TLR9 with CpG DNA (Kline, 2007). Besides, a more recent study has showed that Pam3CSK4-mediated suppression of Ag-induced degranulation of bone marrow-derived mast cells required no TLR2 signal, most probably by electrostatic forces to reduce the level of active allergen and in turn, Pam3CSK4 was responsible for the suppression of Ag-induced degranulation (Fehrenbach et al., 2007).
It was proposed that the increase of allergic diseases in the industrialized world has often been related to a decline in infections during childhood, since a reduction in the overall microbial burden and low stimulation of TLRs will result in weak Th1 imprinting and unrestrained Th2 responses that presumably allow an increase in allergy (Liu, 2007; Tse and Horner, 2008). Our results show that triggering of TLR2 by its agonist Pam3CSK4 decreased allergic inflammation and skewed Th2 response toward Th1 response, supporting this hygiene hypothesis. In accordance with a recent study demonstrating that TLR2 ligands inhibited allergen-specific Th2 responses in vitro in sensitized individuals allergic to HDM allergen (Taylor et al., 2006), our study further confirms the inhibitory effect of TLR2 ligand on allergic immune responses in vivo in mouse HDM-induced allergic rhinitis model.
In summary, based on a mouse allergic rhinitis model with the house dust mite allergen that developed in the current studies, we have clearly showed that the stimulation of TLR2 with Pam3CSK4 was able to decrease not only allergic symptoms but also the Th2 response in allergic mice, suggesting its therapeutic effect on allergic diseases. Further studies need to be done to evaluate the persistence of its antiallergic effect, potential side effects, and effects related with various timing and route of administration in animal models.
Footnotes
Project (No. 39800135) supported by the National Natural Science Foundation of China
References
- 1.Agrawal S, Agrawal A, Doughty B, Gerwitz A, Blenis J, van Dyke T, Pulendran B. Cutting edge: different Toll-like receptor agonists instruct dendritic cells to induce distinct Th responses via differential modulation of extracellular signal-regulated kinase-mitogen-activated protein kinase and c-Fos. J Immunol. 2003;171(10):4984–4989. doi: 10.4049/jimmunol.171.10.4984. [DOI] [PubMed] [Google Scholar]
- 2.Akdis CA, Kussebi F, Pulendran B, Akdis M, Lauener RP, Schmidt-Weber CB, Klunker S, Isitmangil G, Hansjee N, Wynn TA, et al. Inhibition of T helper 2-type responses, IgE production and eosinophilia by synthetic lipopeptides. Eur J Immunol. 2003;33(10):2717–2726. doi: 10.1002/eji.200323329. [DOI] [PubMed] [Google Scholar]
- 3.Akiba H, Mitsuishi K, Ikeda S, Okumura K, Ogawa H. Crucial commitment of proteolytic activity of a purified recombinant major house dust mite allergen Der p1 to sensitization toward IgE and IgG responses. J Immunol. 2006;177(3):1609–1617. doi: 10.4049/jimmunol.177.3.1609. [DOI] [PubMed] [Google Scholar]
- 4.Berin MC, Zheng Y, Domaradzki M, Li XM, Sampson HA. Role of TLR4 in allergic sensitization to food proteins in mice. Allergy. 2006;61(1):64–71. doi: 10.1111/j.1398-9995.2006.01012.x. [DOI] [PubMed] [Google Scholar]
- 5.Chapman MD, Wünschmann S, Pomés A. Proteases as Th2 adjuvants. Curr Allergy Asthma Rep. 2007;7(5):363–367. doi: 10.1007/s11882-007-0055-6. [DOI] [PubMed] [Google Scholar]
- 6.Chisholm D, Libet L, Hayashi T, Horner AA. Airway peptidoglycan and immunostimulatory DNA exposures have divergent effects on the development of airway allergen hypersensitivities. J Allergy Clin Immunol. 2004;113(3):448–454. doi: 10.1016/j.jaci.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 7.Eder W, Klimecki W, Yu L, von Mutius E, Riedler J, Braun-Fahrlander C, Nowak D, Martinez FD. Toll-like receptor 2 as a major gene for asthma in children of European farmers. J Allergy Clin Immunol. 2004;113(3):482–488. doi: 10.1016/j.jaci.2003.12.374. [DOI] [PubMed] [Google Scholar]
- 8.Fehrenbach K, Port F, Grochowy G, Kalis C, Bessler WB, Galanos C, Krystal G, Freudenberg M, Michael Huber M. Stimulation of mast cells via FcvarepsilonR1 and TLR2: the type of ligand determines the outcome. Mol Immunol. 2007;44(8):2087–2094. doi: 10.1016/j.molimm.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 9.Kline JN. Immunotherapy of asthma using CpG oligodeoxynucleotides. Immunol Res. 2007;39(1-3):279–286. doi: 10.1007/s12026-007-0083-2. [DOI] [PubMed] [Google Scholar]
- 10.Lauener RP, Birchler T, Adamski J, Braun-Fahrlander C, Bufe A, Herz U, von Mutius E, Nowak D, Riedler J, Waser M, Senhauser FH ALEX study group. Expression of CD14 and Toll-like receptor 2 in farmers’ and non-farmers’ children. Lancet. 2002;360(9331):465–466. doi: 10.1016/S0140-6736(02)09641-1. [DOI] [PubMed] [Google Scholar]
- 11.Liu AH. Hygiene theory and allergy and asthma prevention. Paediatr Perinat Epidemiol. 2007;21(Suppl. 3):2–7. doi: 10.1111/j.1365-3016.2007.00878.x. [DOI] [PubMed] [Google Scholar]
- 12.Liu RM, Zhang CJ, Cui TP, Wu JM. The study of correlation between the mRNA expression of Toll-like receptors and cytokines of intracellular CD4+ T cell in splenic macrophages of allergic asthma mice model. Chin J Lab Med. 2006;29(8):698–701. (in Chinese) [Google Scholar]
- 13.Patel M, Xu D, Kewin P, Choo-Kang B, McSharry C, Thomson NC, Liew FY. TLR2 agonist ameliorates established allergic airway inflammation by promoting Th1 response and not via regulatory T cells. J Immunol. 2005;174(12):7558–7563. doi: 10.4049/jimmunol.174.12.7558. [DOI] [PubMed] [Google Scholar]
- 14.Phipps S, Lam CE, Foster PS, Matthaei KI. The contribution of Toll-like receptors to the pathogenesis of asthma. Immunol Cell Biol. 2007;85(6):463–470. doi: 10.1038/sj.icb.7100104. [DOI] [PubMed] [Google Scholar]
- 15.Redecke V, Hacker H, Datta SK, Fermin A, Pitha PM, Broide DH, Raz E. Cutting edge: activation of Toll-like receptor 2 induces a Th2 immune response and promotes experimental asthma. J Immunol. 2004;172(5):2739–2743. doi: 10.4049/jimmunol.172.5.2739. [DOI] [PubMed] [Google Scholar]
- 16.Revets H, Pynaert G, Grooten J, Baetselier P. Lipoprotein I, a TLR2/4 ligand modulates Th2-driven allergic immune responses. J Immunol. 2005;174(2):1097–1103. doi: 10.4049/jimmunol.174.2.1097. [DOI] [PubMed] [Google Scholar]
- 17.Rodriguez D, Keller AC, Faquim-Mauro EL, de Macedo MS, Cunha FQ, Lefort J, Vargaftig BB, Russo M. Bacterial lipopolysaccharide signaling through Toll-like receptor 4 suppresses asthma-like responses via nitric oxide synthase 2 activity. J Immunol. 2003;171(2):1001–1008. doi: 10.4049/jimmunol.171.2.1001. [DOI] [PubMed] [Google Scholar]
- 18.Sarpong SB, Zhang LY, Kleeberger SR. A novel mouse model of experimental asthma. Int Arch Allergy Immunol. 2003;132(4):346–354. doi: 10.1159/000074902. [DOI] [PubMed] [Google Scholar]
- 19.Schnare M, Barton GM, Holt AC, Takeda K, Akira S, Medzhitov R. Toll-like receptors control activation of adaptive immune responses. Nat Immunol. 2001;2(10):947–950. doi: 10.1038/ni712. [DOI] [PubMed] [Google Scholar]
- 20.Sokol CL, Gregory M, Barton GM, Farr AG, Medzhitov R. A mechanism for the initiation of allergen-induced T helper type 2 responses. Nat Immunol. 2008;9(3):310–318. doi: 10.1038/ni1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sutmuller RP, den Brok MH, Kramer M, Bennink EJ, Toonen LM, Joosten LA, Akira S, Netea MG, Adema GJ. Toll-like receptor 2 controls expansion and function of the thyroid axis. J Clin Invest. 2006;116(2):485–494. doi: 10.1172/JCI25439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Takeda K, Kaisho T, Akira S. Toll-like receptors. Annu Rev Immunol. 2003;21(1):335–376. doi: 10.1146/annurev.immunol.21.120601.141126. [DOI] [PubMed] [Google Scholar]
- 23.Taylor RC, Richmond P, Upham JW. Toll-like receptor 2 ligands inhibit TH2 responses to mite allergen. J Allergy Clin Immunol. 2006;117(5):1148–1154. doi: 10.1016/j.jaci.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 24.Tse K, Horner AA. Defining a role for ambient TLR ligand exposures in the genesis and prevention of allergic diseases. Semin Immunopathol. 2008;30(1):53–62. doi: 10.1007/s00281-007-0098-8. [DOI] [PubMed] [Google Scholar]
- 25.Wen TH. Vaccines for Child Allergic Asthma and Immunotherapy. In: Chinese Medical Association-Sub-association of Allergology, editor. National Symposium on Diagnosis and Management of Child Allergic Diseases in Advance. Chengdu, China: 2006. pp. 38–40. Symposium and Abstract,(in Chinese) [Google Scholar]
- 26.Wu Q, Martin RJ, Rino JG, Jeyaseelan S, Breed R, Chu HW. A deficient TLR2 signaling promotes airway mucin production in Mycoplasma pneumoniae-infected allergic mice. Am J Physiol Lung Cell Mol Physiol. 2007;292(5):L1064–L1072. doi: 10.1152/ajplung.00301.2006. [DOI] [PubMed] [Google Scholar]
- 27.Zhang K, Zhu D, Kepley C, Terada T, Saxon A. Chimeric human fcgamma-allergen fusion proteins in the prevention of allergy. Immunol Allergy Clin North Am. 2007;27(1):93–103. doi: 10.1016/j.iac.2006.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]