Abstract
Objective: The diagnoses of patients with duodenal protruding lesions are difficult when using conventional examinations such as computed tomography (CT) and conventional endoscope etc. Thus, we investigated the clinical value of endoscopic ultrasonography (EUS) with miniature ultrasonic probes on the diagnosis and treatment of duodenal protruding lesions. Methods: Patients with duodenal protruding lesions who were indicated for EUS were examined by EUS with 12~15 MHz miniature ultrasonic probes and double-cavity electronic endoscope. According to diagnosis of EUS, those patients were indicated for biopsy and treatment received biopsy, endoscopic resection or surgical excision. The postoperative histological results were compared with the preoperative diagnosis of EUS. Those patients without endoscopic resection or surgical excision were periodically followed up with EUS. Results: A total of 169 patients with duodenal protruding lesions were examined by EUS, of which 40 were diagnosed with cysts, 36 with inflammatory protruding or polyp, 25 with Brunner’s gland adenoma, 19 with ectopic pancreas, 17 with gastrointestinal stromal tumor, 12 with extrinsic compression, 12 with minor papilla, 6 with lipoma, 1 with adenocarcinoma and 1 with lymphoma. After EUS examinations, 75 patients received biopsy, endoscopic resection or surgical excision respectively. The postoperative histological results of 70 patients were completely consistent with the preoperative diagnosis of EUS, with 93.33% diagnostic accuracy. The results of follow-up with EUS indicated that duodenal cyst, Brunner’s gland adenoma, ectopic pancreas, gastrointestinal stromal tumor and lipoma remained unchanged within 1~3 years. No related complications occurred among all patients that received EUS examinations. Conclusion: EUS is an effective and reliable diagnostic method for duodenal protruding lesions.
Keywords: Endoscopic ultrasonography (EUS), Duodenal protruding lesions, Diagnosis, Follow-up
INTRODUCTION
Endoscopic ultrasonography (EUS) has the function of both endoscope and ultrasound, which cannot only show the surface of gastrointestinal mucosa, but also the structure of the gastrointestinal wall and the relationship with adjacent organs. The application of EUS has greatly improved the diagnosis of gastrointestinal diseases (Pfau and Chak, 2002; Menzel and Domschke, 2000; Xu et al., 2004; Rösch, 2003). It is difficult to diagnose and treat duodenal diseases because of Duodenum’s complex and specific surroundings. We performed EUS with miniature probes on patients who were diagnosed with duodenal protruding lesions by conventional endoscopy and other methods, and evaluated the values of EUS for the diagnosis and treatment of duodenal protruding lesions.
MATERIALS AND METHODS
Patients
A total of 169 patients, 108 males and 61 females with a median age of 54 years (range 21~78 years), who had been diagnosed with duodenal protruding lesions through Barium meal, conventional endoscope or computed tomography (CT) examinations and presented EUS indication, underwent EUS during the period from 2000 to 2006 in the First Affiliated Hospital, School of Medicine, Zhejiang University, China.
Instruments
Instruments of EUS include Olympus GIF-2T-240 double-cavity electronic gastroscope, Olympus MAJ drive systems of high-frequency echoprobe, UM-DP12-25R miniature ultrasonic probes with frequency spectrum of 12~15 MHz and Daker WP-800 water pump (Olympus Medical System Corp. Japan).
Methods
The preparations for EUS examination were the same as those of conventional gastroscope. Part of patients received intramuscular injection of Atropine or East Anisodamine to reduce the creeping and spasm of bowels if necessary. According to the information of the location and size of the lesion obtained by the conventional endoscopy examination, different frequencies ultrasonic microprobes and examination methods (water-soaking method or water-pour-in method) were used. Patients who presented with the indications underwent endoscopic biopsy, centesis, resection or surgical excision. Postoperative histopathologic results were compared with the preoperative diagnoses of EUS. Others were periodically followed up with conventional endoscope or EUS. The tolerance to EUS and complications related to the examination in all these patients were investigated as well.
RESULTS
Both the 5-layer structures of duodenal wall and parts of adjacent organs such as the cholecyst, common bile duct, pancreas and liver of all patients were observed through EUS with 12~15 MHz miniature ultrasonic probes. The EUS diagnoses and size of lesions of all 169 patients and histopathologic diagnoses of 75 patients from endoscopic biopsy, centesis, resection or surgical excision were listed in Table 1. The location and origin of lesions in the duodenal wall of 145 patients were listed in Table 2. According to results of the EUS, 7 of 12 cases of extrinsic compression were from the cholecyst and 5 from the pancreas, 12 cases with minor papilla lying in the descending portion. Tissue samples of 75 cases from endoscopic biopsy, centesis, resection or surgical excision were diagnosed by histopathology, with 70 cases proved to be identical to echo endoscopic diagnosis. Diagnosis accuracy of EUS was 93.33%. Five cases of misdiagnosis included 1 case of stromal tumor and 1 Brunner’s gland adenoma, which were misdiagnosed as inflammatory polyp, 1 inflammatory protruding as ectopic pancreas, 1 ectopic pancreas as stromal tumor, and 1 adenocarcinoma as malignant stromal tumor. There were still 77 cases with submucosa lesions that did not undergo endoscopic therapy or surgery, except cases with duodenal minor papilla and extrinsic compression, with most of the lesions less than 1 cm in diameter. Sixty cases were followed up by electronic endoscope or EUS for 5 to 36 months, and the results indicated that cyst, Brunner’s gland adenoma, ectopic pancreas, stromal tumor and lipoma were unchanged within the period of follow-up. All the patients tolerated EUS procedures, without showing serious complications such as bleeding, perforation or cardiopulmonary accident etc., and no complications occurred to those undergoing endoscopic therapy, either.
Table 1.
EUS diagnoses and sizes of duodenal protruding lesions (n=169) and histological results (n=75)
| EUS diagnosis | Number of patients | Sizes of lesions (cm) | Number of tissue samples (biopsy/surgeon) | Number with EUS diagnostic consistency |
| Cyst | 40 | 0.25~1.56 | 8 (8/0) | 8 |
| Inflammatory protruding or polyp | 36 | 0.30~2.00 | 36 (34/2) | 34 |
| Brunner’s adenoma | 25 | 0.35~2.15 | 12 (10/2) | 12 |
| Ectopic pancreas | 19 | 0.70~2.57 | 6 (3/3) | 5 |
| Stromal tumor | 17 | 0.60~3.30 | 6 (2/4) | 5 |
| Extrinsic compression | 12 | 3 (0/3) | 3 | |
| Minor papilla | 12 | |||
| Lipoma | 6 | 0.74~1.60 | 2 (2/0) | 2 |
| Adenocarcinoma | 1 | 3.50 | 1 (0/1) | |
| Lymphoma | 1 | 1 (1/0) | 1 | |
| Total | 169 | 75 (60/15) | 70 (93.33%) |
Table 2.
Locations and origins of duodenal lesions (n=145)
| Diseases | Bulb | Junction of bulb and descending | Descending portion | Mucosa | Submucosa | Muscularis mucosa |
| Cyst (n=40) | 21 | 7 | 12 | 40 | ||
| Inflammatory protruding or polyp (n=36) | 27 | 6 | 3 | 36 | ||
| Brunner’s adenoma (n=25) | 14 | 5 | 6 | 2 | 23 | |
| Ectopic pancreas (n=19) | 12 | 4 | 3 | 1 | 14 | 4 |
| Stromal tumor (n=17) | 10 | 2 | 5 | 1 | 3 | 13 |
| Lipoma (n=6) | 2 | 2 | 2 | 6 | ||
| Adenocarcinoma (n=1) | 1 | Infiltrate to muscularis propria | ||||
| Lymphoma (n=1) | 1 | Infiltrate to adventitia | ||||
DISCUSSION AND CONCLUSION
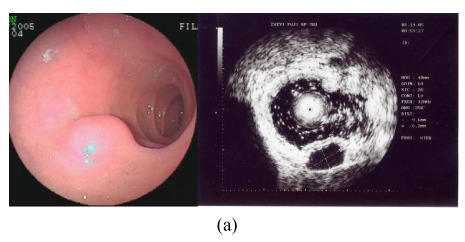
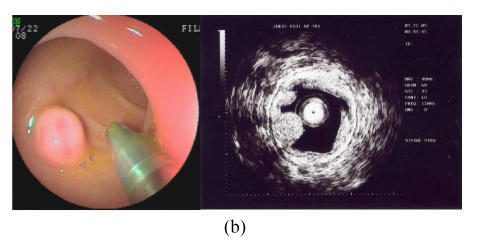
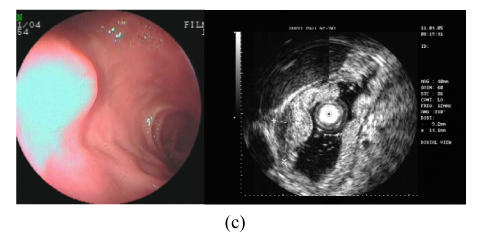
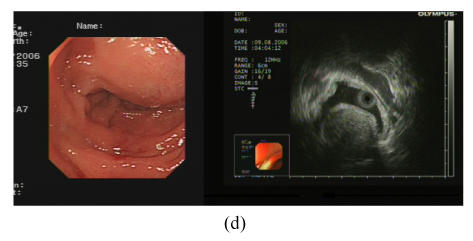
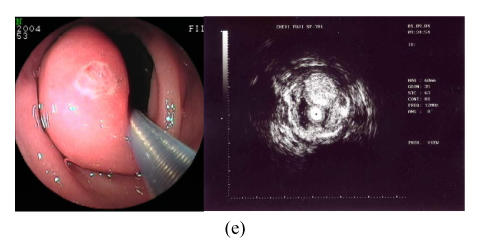
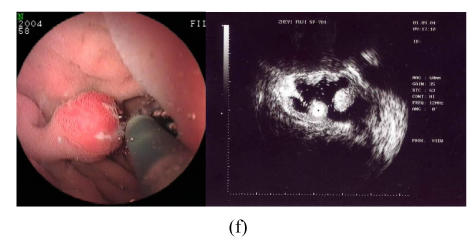
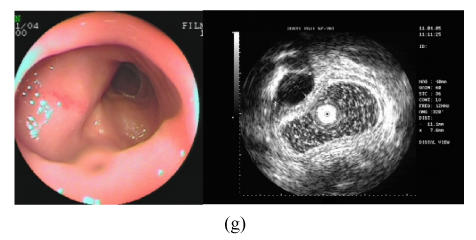
EUS has been reported to be the best examination method for gastrointestinal submucosal lesions, and it cannot only confirm if the lesion is a true submucosal one, but also ascertain accurately its size, location, origin and nature (Rösch et al., 2002; Buscarini et al., 1999; Saftoiu et al., 2003). In the present study, the 169 patients can be classified into two groups: submucosal and pseudo-submucosal lesions. The former group consisted of cyst, Brunner’s gland adenoma, ectopic pancreas, stromal tumor and lipoma, while the latter consisted of inflammatory swelling, polyp and extrinsic compression. Submucosal lesions were mostly single, and likely to lie in the duodenal bulb. Most of them appeared to be protrusions with smooth surface and normal color under electronic endoscope, which were difficult to be distinguished from each other, but the protrusions were seen quite differently under EUS (Wiech et al., 2005; Brand et al., 2002; Ponsaing et al., 2007). The cysts showed round and anechoic masses with a clear margin and enhancement behind. The lesions often originated from submucosa, and could be deformed by compression (Fig.1a). Brunner’s gland adenomas displayed round or orbicular-ovate, homogeneous and middle-hyperechoic masses with a clear margin. Some might have tubular structure inside, and most of them originated from submucosa (Fig.1b). Ectopic pancreases were observed as non-homogeneous middle-hypoechoic and pathy masses with an unclear margin and tubular structure inside. Most of them originated from submucosa and muscular layer, and might have an opening on surface (Fig.1c). Most of stromal tumors presented hypoechoic and homogeneous masses with a clear margin. There would be non-homogeneous echoes, liquefied and destroyed surroundings if the lesions were large or inclined to be malignant (Fig.1d). Lipomas presented homogeneous and hyperechoic masses with a clear margin and echo decline phenomenon behind, and most of them originated from submucosa (Fig.1e). On basis of ultrasound imaging features above, it is suggested that EUS is of value in identifying the size, location, number, origin and nature of most submucosal lesions, and more capable than Barium meal, CT or conventional endoscope for the diagnosis of submucosal lesions of the duodenum (Ponsaing et al., 2007; Gourtsoyiannis et al., 2001; Lau et al., 2004).
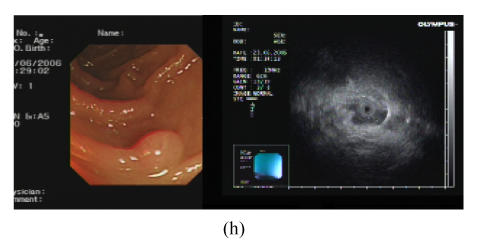
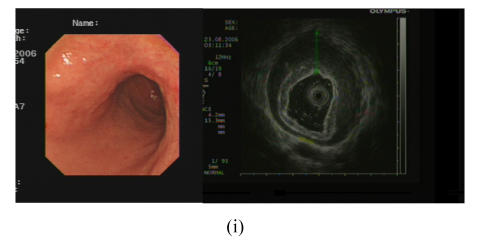
Fig. 1.
(a) Duodenal cyst; (b) Duodenal Brunner’s gland adenoma; (c) Duodenal ectopic pancreas; (d) Duodenal stromal tumor; (e) Duodenal lipoma; (f) Duodenal polyp; (g) Duodenal extrinsic compression (cholecyst); (h) Duodenal minor papilla; (i) Duodenal B-cell lymphoma
In the present study, the duodenal bulb was the predominate site for pseudo-submucosal lesions as for the real submucosal lesions. Most of polyps and inflammatory lesions could be identified by conventional endoscope, while some with color and structure similar to surrounding mucosa and an unclear margin were hardly detected. The latter could be distinguished by EUS, which presented non-homogeneous and middle-hypoechoic masses without an envelope, and a majority of them originated from epithelium or mucosa with a normal series of submucosa, muscularis propria and adventitia (Fig.1f). On basis of the echoic characteristics, we could easily distinguish pseudo-submucosal lesions from real ones by EUS. According to previous studies (Pfau and Chak, 2002; Arguello, 2007), the diagnostic accuracy of EUS for the gastrointestinal tract extrinsic compression was almost 100%, which was also confirmed in our study. Extrinsic compressions were diagnosed by echoic characteristics of complete layer and structure, the curved compression adventitia and the cross section image of surrounding tissues and organs. Of the 169 patients, there were 12 cases of duodenal extrinsic compressions, and most of the organs that caused compression were the cholecyst (Fig.1g) and pancreas. Three of these patients underwent surgery, and the postoperative diagnoses were confirmed to be the same as preoperative EUS diagnosis. It is suggested that EUS has the incomparable superiority in diagnosing polyps, inflammatory protrusions and extrinsic compressions in the duodenum (Xu et al., 2004) that may be difficult for conventional endoscope to examine.
Duodenal minor papilla could be easily misdiagnosed as polyps or others; nevertheless, EUS can give right diagnosis due to its echo characteristics (Fig.1h). In the present study, 12 cases were diagnosed as minor papilla by EUS, which seemed indefinite under conventional endoscope. In addition, diagnosed by EUS, we had 1 duodenal B-cell lymphoma that presented a hypoechoic mass, diffuse and obviously thickened wall with normal structure disappeared (Fig.1i), which was clinically important to the diagnosis of gastrointestinal lymphoma in future (Okanobu et al., 2005).
Seventy-five patients who had the indications were referred to endoscopic biopsy, puncture, resection or surgical excision. The postoperative histopathological results showed that the size, origin and number of lesions of all patients were completely consistent with the diagnoses of EUS; the nature of lesions of 70 patients agreed with preoperative EUS diagnosis. Diagnosis accuracy of EUS was 93.33%, which disclosed that EUS was almost as valuable as pathology for duodenal protruding lesions, especially for inflammatory swelling, polyps, extrinsic compressions, cysts, Brunner’s gland adenoma and lipoma (Xu et al., 2004; 2006; Rösch et al., 2002). However, lesions with an untypical echoic image tend to be misdiagnosed, for instance, polyps, ectopic pancreas or stromal tumors became unspecific under EUS when they were small. Patients who did not receive therapy were followed up by EUS or conventional endoscope, which showed that cysts, Brunner’s gland adenoma, ectopic pancreas, stromal tumors and lipoma had no change in size of lesions and clinical symptoms during 2~3 years. It suggests that a follow-up is needed if lesions are small, deep or without symptoms due to slow growth.
It is of importance for both physicians and surgeons to grasp the indication of therapy for lesions lying in the duodenum, because of the high frequency of formidable complications of therapy like perforation etc., due to the thin wall, narrow cavity and connection to cholangiopancreatic ducts. EUS helps us get better understanding of the indications of endoscopic and surgical therapies. For Brunner’s gland adenoma, stromal adenoma, lipoma and ectopic pancreas originated from submucosa or more superficial, endoscopic resection can be administered without perforation; for cyst from submucosa, endoscopic puncture is effective, economical, convenient, minimally invasive and safe; and for lesions originated from muscularis propria or adventitia, surgical or laparoscopic excision is better than endoscopic therapy. Patients, who refuse to receive surgery or do not have indications, will be followed up in order to avoid complications caused by surgery and excessive treatment. In addition, treatment modality can be well represented for inflammatory swellings and extrinsic compressions because of the precise diagnosis by EUS. Our study shows that EUS is an effective and safe method for both the diagnosis and treatment of duodenal protruding lesions, confirming the findings of others (Izumi et al., 1999; Waxman et al., 2002; Shim and Jung, 2005; Ichikawa et al., 2007).
Finally, EUS has greatly improved the accuracy rate of diagnosis and treatment of duodenal protruding lesions. However, it cannot replace histopathology. It has poor capability in distinguishing benign and malignant masses, and likely leads to misdiagnosis for lesions with similar echoic images. Miniature ultrasonic probes are vulnerable and cannot show far field of big lesions very clearly. Furthermore, it is impossible to carry out real-time EUS-guided needle puncture. In clinical practice, therefore, EUS needs to be performed together with other methods.
Footnotes
Project (No. 491010-W10495) supported by the Scientific Research Foundation of Medicine and Health of Zhejiang Province, China
References
- 1.Arguello L. Endoscopic ultrasonography in submucosal lesions and extrinsic compressions of the gastrointestinal tract. Minerva Med. 2007;98(4):389–393. [PubMed] [Google Scholar]
- 2.Brand B, Oesterhelweg L, Binmoeller KF, Srirann PV, Bohnacker S, Seewald S, Weerth AD, Soehendra N. Impact of endoscopic ultrasound for evaluation of submucosal lesions in gastrointestinal tract. Dig Liver Dis. 2002;34(4):290–297. doi: 10.1016/S1590-8658(02)80150-5. [DOI] [PubMed] [Google Scholar]
- 3.Buscarini E, Stasi MD, Rassi S, Silva M, Giangregorio F. Endosonographic diagnosis of submucosal upper gastrointestinal tract lesions and large fold gastropathies by catheter probe. Gastrointest Endosc. 1999;49(2):184–191. doi: 10.1016/S0016-5107(99)70484-0. [DOI] [PubMed] [Google Scholar]
- 4.Gourtsoyiannis N, Grammatikakis J, Prassopoulos P. Role of conventional radiology in the diagnosis and staging of gastrointestinal tract neoplasms. Semin Surg Oncol. 2001;20(2):91–108. doi: 10.1002/ssu.1023. [DOI] [PubMed] [Google Scholar]
- 5.Ichikawa T, Kudo M, Matsui S, Okada M, Kitano M. Endoscopic ultrasonogrsphy with three miniature probes of different frequency is an accurate diagnostic tool for endoscopic submucosal of dissection. Hepatogastroenterology. 2007;54(73):325–328. [PubMed] [Google Scholar]
- 6.Izumi Y, Inoue H, Kawano T, Tani M, Tada M, Okabe S, Takeshita K, Endo M. Endosonography during endoscopic mucosal resection to enhance its safety: a new technique. Surg Endosc. 1999;13(4):358–360. doi: 10.1007/s004649900989. [DOI] [PubMed] [Google Scholar]
- 7.Lau S, Tam KF, Kam CK, Lui CY, Siu CW, Lam HS, Mak KL. Imaging of gastrointestinal stromal tumors. Clin Radiol. 2004;59(6):487–498. doi: 10.1016/j.crad.2003.10.018. [DOI] [PubMed] [Google Scholar]
- 8.Menzel J, Domschke W. Gastrointestinal miniprobe sonography: the current status. Am J Gastroenterol. 2000;95(3):605–616. doi: 10.1111/j.1572-0241.2000.01832.x. [DOI] [PubMed] [Google Scholar]
- 9.Okanobu H, Hata J, Haruma K, Mitsuoka Y, Kunihiro K, Manabe N, Tanaka S, Chayama K. A classification system of echogenicity for gastrointestinal neoplasm. Digestion. 2005;72(1):8–12. doi: 10.1159/000087216. [DOI] [PubMed] [Google Scholar]
- 10.Pfau PR, Chak A. Endoscopic ultrasonography. Endoscopy. 2002;34(1):21–28. doi: 10.1055/s-2002-19394. [DOI] [PubMed] [Google Scholar]
- 11.Ponsaing LG, Kiss K, Loft A, Jensen LI, Hansen MB. Diagnostic procedures for submucosal tumors in the gastrointestinal tract. World J Gastroenterol. 2007;13(24):3301–3310. doi: 10.3748/wjg.v13.i24.3301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rösch T. Endoscopic ultrasonography: imaging and beyond. Gut. 2003;52(8):1220–1226. doi: 10.1136/gut.52.8.1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rösch T, Kaper B, Will U, Baronius W, Strobel M, Lorenz R, Ulm K. Accuracy of endoscopic ultrasonography in upper gastrointestinal submucosal lesions: a prospective multicenter study. Scand J Gastroenterol. 2002;37(7):856–862. doi: 10.1080/713786521. [DOI] [PubMed] [Google Scholar]
- 14.Saftoiu A, Vilmann P, Ciurea T. Utility of endoscopic ultrasound for the diagnosis and treatment of submucosal tumors of the upper gastrointestinal tract. Rom J Gastroenterol. 2003;12(3):215–219. [PubMed] [Google Scholar]
- 15.Shim CS, Jung IS. Endoscopic removal of submucosal tumors: preprocedure diagnosis, technical options and results. Endoscopy. 2005;37(7):646–654. doi: 10.1055/s-2005-861477. [DOI] [PubMed] [Google Scholar]
- 16.Waxman I, Saitoh Y, Raju GS, Watari J, Yokota K, Reeves AL, Kohgo Y. High-frequency probe EUS-assisted endoscopic mucosal resection: a therapeutic strategy for submucosal tumor of the GI tract. Gastrointest Endosc. 2002;55(1):44–49. doi: 10.1067/mge.2002.119871. [DOI] [PubMed] [Google Scholar]
- 17.Wiech T, Walch A, Werner M. Histopathological classification of nonneoplastic and neoplastic gastrointestinal submucosal lesions. Endoscopy. 2005;37(7):630–634. doi: 10.1055/s-2005-870127. [DOI] [PubMed] [Google Scholar]
- 18.Xu GQ, Li YW, Han YM, Li YM, Chen WX, Ji F, Li HJ, Gu Q. Miniature ultrasonic probes for diagnosis and treatment of digestive tract diseases. World J Gastroenterol. 2004;10:1948–1953. doi: 10.3748/wjg.v10.i13.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xu GQ, Zhang H, Li YM, Chen HT, Ji F, Chen CX, Ren GP, Ni XY. Diagnosis and treatment of duodenal Brunner’s adenoma of 15 cases. Chin J Digest. 2006;28(8):511–514. (in Chinese) [Google Scholar]