After steady improvement until about 1980, the technology behind esophageal manometry saw little change until recent years. A variety of sensor technologies existed including solid-state strain gauge transducers, circumferentially sensitive transducers, multilumen perfused catheters with external pressure transducers, and the Dentsleeve device. However, irrespective of transducer design, the basic format of manometric studies was of multiple line-tracings representing pressure change versus time at several discrete esophageal loci. Furthermore, of the sensor designs available, only the Dentsleeve device provided a validated method for assessing sphincter relaxation. However, the Dentsleeve accomplished this at the expense of pressure response rate and spatial resolution leading some experts to focus instead on these limitations. In brief, little standardization existed in methodology among centers and there was no agreement regarding optimal assembly design or study interpretation.
High Resolution Manometry
Somewhat ironically, for all the attention historically given to the response characteristics of manometric transducers, the problem of providing adequate spatial resolution within the esophageal lumen was left largely ignored. The concept of high resolution manometry (HRM) is to vastly increase the number of pressure sensors on the manometric assembly so as to completely define the intraluminal pressure profile. Pressure sensors are placed in such close proximity to each other that by interpolating between adjacent sensors intraluminal pressure becomes a spatial continuum. The two key innovations facilitating the widespread application of high resolution manometry (HRM) were; 1) the introduction of a practical manometric device with 36 solid-state, circumferentially sensitive sensors spaced at 1 cm intervals (Sierra Scientific Instruments Inc., Los Angeles, CA), and 2) the development of sophisticated algorithms to display the expanded manometric dataset as pressure topography plots rather than 36 overlapping line tracings [1]. Together, these developments permit the visualization of esophageal motility as a continuum along the length of the esophagus with isobaric conditions among sensors indicated by color continuums (Figure 1). The relative timing of sphincter relaxation and segmental contraction as well as the position and length of the striated and smooth muscle segments are readily demonstrated [2]. Furthermore, reproducible measurements of sphincter relaxation can be made, no longer confounded by crural diaphragm contraction or movement of the sphincter [3]. Because intraluminal pressure gradients can be analyzed in detail, conditions conducive to successful or failed bolus transport can be defined [4]. These strengths are evident in Figure 2 illustrating one of the most common pressure topography signatures of achalasia, pan-esophageal pressurization [5].
Figure 1.
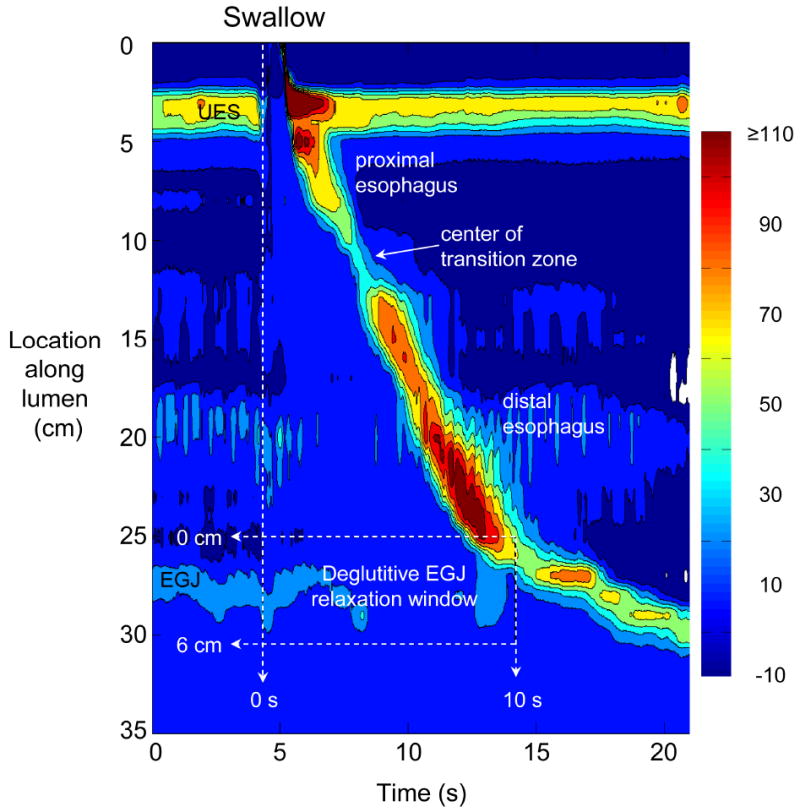
Typical pressure topography of a swallow spanning the entire esophagus from the pharynx (locations 0-2 cm) to stomach (locations 32-35 cm) of a normal subject with normal peristalsis and normal EGJ relaxation. Note that the transition zone demarcating the end of the proximal esophageal segment (striated muscle) and the beginning of the distal esophageal segment (smooth muscle) is readily identified as the pressure minimum between the sphincters. The onset of the deglutitive relaxation window is defined by the onset of upper sphincter relaxation while the offset is 10 s later. The spatial domain within which EGJ relaxation spans at least 6 cm, depending on the extent of esophageal shortening after the swallow.
Figure 2.
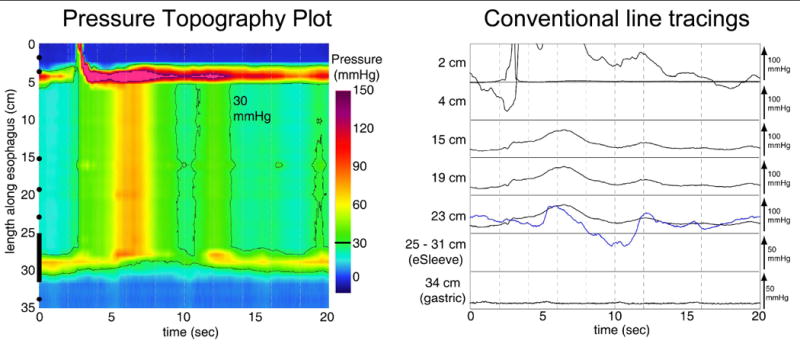
Achalasia associated with pan-esophageal pressurization depicted in terms of pressure topography and contrasted with conventional line tracings. In the pressure topography plot pressure magnitude is indicated by color intensity and the black line indicates the 30 mmHg isobaric pressure contour; note that the EGJ never relaxes to a pressure of less than 30 mmHg. Also note that although the intraesophageal pressure approaches 90 mmHg after the swallow, this is not indicative of spasm or vigorous achalasia as it occurs within a closed chamber sealed by the sphincter at either end. The conventional line tracings to the right are extracted from the same data as in the topography plot using only the sensors at 3, 4, 15, 19, 23, 25-31 (eSleeve™) and 34 cm. The blue line represents the eSleeve™ recording, which is the highest instantaneous pressure among sensors 26-32 and a sensitive indicator of EGJ relaxation.
Once the clinician becomes familiar with the HRM pressure topography format, recordings can be quickly appraised as technically adequate or not based on positioning of the assembly so as to encompass both upper and lower esophageal sphincters and normal performance of the pressure sensors. However, with the adoption of the pressure topography display methodology, the classification of esophageal motility developed for conventional manometric systems requires some revision. Toward that goal, we performed a comprehensive characterization of esophageal HRM data in 75 normal subjects and 400 patients using analysis paradigms unique to pressure topography interpretation [5, 6]. In the process, we developed a systematic, pressure topography oriented classification of motor disorders of the distal esophagus. The two major strengths of pressure topography plots compared to conventional manometric recordings are: 1) the ability to easily delineate the spatial limits and contractile characteristics of individual contractile segments along the esophagus (Figure 1) and, 2) the ability to easily distinguish between loci of compartmentalized esophageal pressurization (Figure 2) and rapidly propagated esophageal contractions. Making these distinctions was of great utility in distinguishing distal esophageal spasm, vigorous achalasia, functional obstruction, and subtypes of nutcracker esophagus.
The Next Horizon: High Definition Manometry
High resolution manometry provides a sufficient degree of spatial detail to characterize motor function and dysfunction along the length of the esophagus. Intraesophageal pressure gradients can be demonstrated and understood in the context of peristaltic activity and outflow obstruction. Sphincter relaxation can be precisely quantified. However, the potential exists to even further enhance spatial pressure resolution with a technology recently dubbed high definition manometry. With high definition manometry, not only are pressure sensors spaced even more closely together than the 1 cm standard of high resolution manometry, but the radial characteristics at each axial position are preserved. Figure 3 illustrates a prototype high definition manometric assembly (Sierra Scientific Instruments Inc) alongside what has become a standard HRM assembly. On the high definition assembly, there are 4 banks of 4 rings each (16 rings in all) with the rings spaced 3 mm apart and the banks spaced 4 mm apart. Each ring has 8 radial sensor, resulting in 128 independent pressure recordings spanning 4.8 cm.
Figure 3.
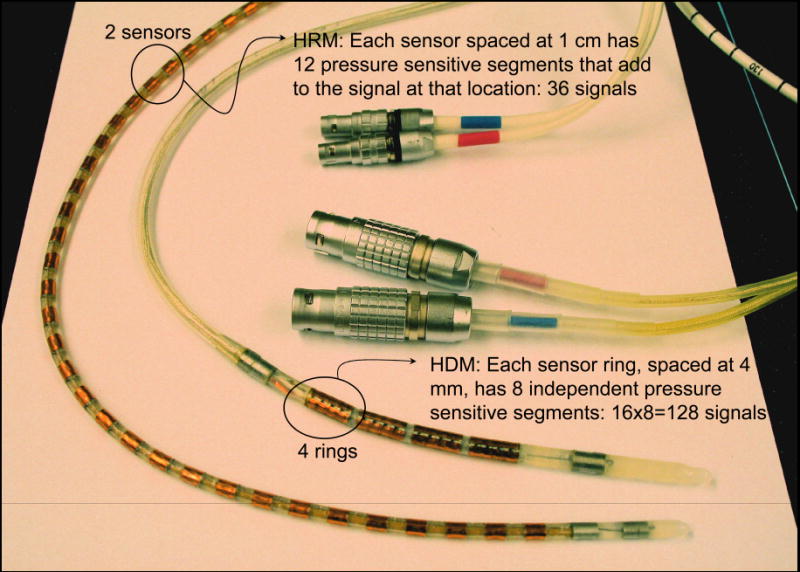
Standard clinical HRM assembly alongside a prototype high definition manometry catheter. Although each of the sensors on the HRM assembly is circumferentially sensitive, the radial signals are averaged within the assembly so that a mean pressure is generated at each recording site. The prototype high definition assembly houses 16 rings of 8 pressure sensors, oriented 45° apart. The active recording surface is only 4.8 cm in length but incorporates 128 discrete pressure signals thereby preserving both axial and radial pressure detail.
High definition manometry has the potential to define the pressure morphology of complex anatomical zones such as the EGJ in ways previously not possible. Figure 4 was constructed from recordings made with the prototype high definition assembly in Figure 3 in a normal volunteer (A) and a patient with a small hiatal hernia (B). Note how clearly the technology isolates the crural diaphragm (CD) contribution to the EGJ in terms of its axial position, degree of radial asymmetry, and magnitude. Similarly, baseline and respiratory variation in intragastric pressure are readily compared to pressure loci within the EGJ and distal esophagus. With the current focus on innovative reflux treatments predicated on anatomic and intraluminal manipulation of the EGJ, the potential of this measurement technology is very promising.
Figure 4.
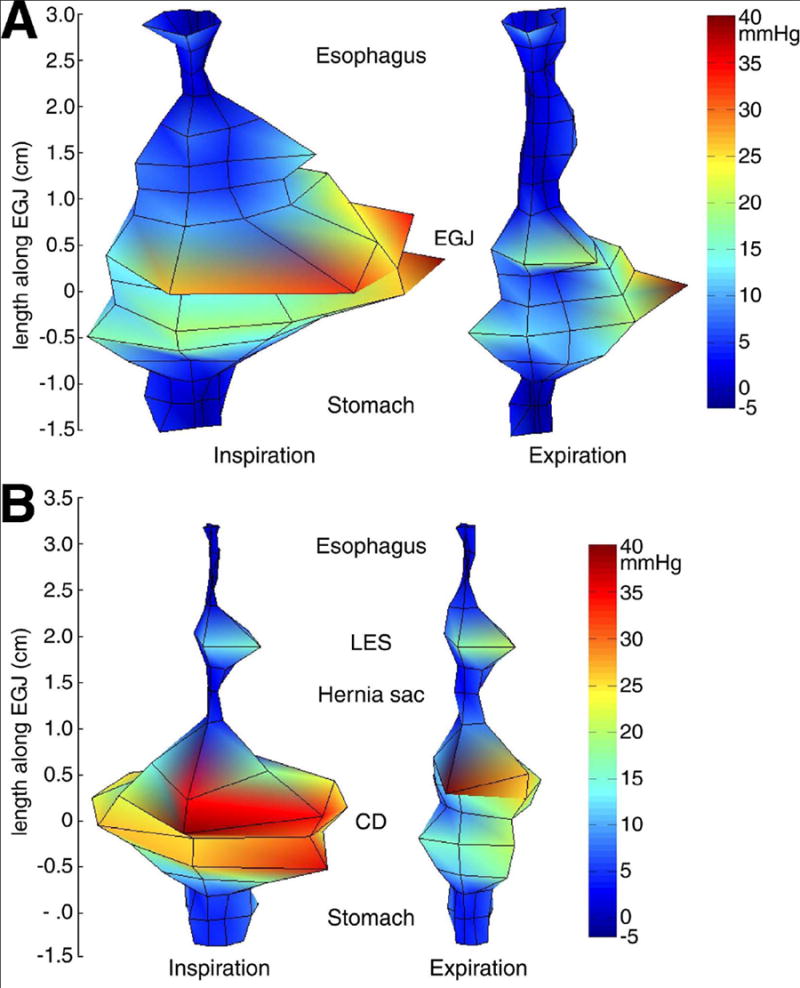
High definition recordings of the EGJ in a normal individual (A) and a patient with a 2 cm separation between the lower esophageal sphincter (LES) and the crural diaphragm (CD). Pressure is scaled both by color and deflection from the central axis with the deepest blue being -5 mmHg relative to atmospheric pressure and red being 40 mmHg. For reasons of illustration, the quadrilateral sector of pressure contributed by each sensor is delineated by black lines on the surface of the solid. Although only the instants of peak inspiration and expiration are illustrated, pressures are acquired in real time and can also be displayed as movies.
In summary, new tools have availed themselves in the recent years with the potential to redefine the science of esophageal manometry. Whereas the technology was historically encumbered by a variety of well-cataloged technological constraints, advances in transducer technology and computer processing coupled with paradigm shifts in the way that pressure recordings are conceptualized have matured the science. For the first time, esophageal manometry has the potential to be not only a robust research tool, but also a well-standardized, objective clinical test. Furthermore, innovation begets discovery, and the pace of innovation continues to be rapid. Hence, the future of esophageal manometry is bright; much remains to be done to define the full potential of this technology.
Acknowledgments
This work was supported by R01 DC00646 (PJK) from the Public Health Service
Abbreviations
- HRM
High-resolution manometry
- LES
lower esophageal sphincter
- CD
crural diaphragm
- EGJ
esophagogastric junction
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Clouse RE, Staiano A, Alrakawi A, Haroian L. Application of topographical methods to clinical esophageal manometry. Am J Gastroenterol. 2000;95:2720–30. doi: 10.1111/j.1572-0241.2000.03178.x. [DOI] [PubMed] [Google Scholar]
- 2.Ghosh SK, Pandolfino JE, Zhang Q, Jarosz A, Shah N, Kahrilas PJ. Quantifying esophageal peristalsis with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol. 2006;290:G988–97. doi: 10.1152/ajpgi.00510.2005. [DOI] [PubMed] [Google Scholar]
- 3.Ghosh SK, Pandolfino JE, Rice J, Clarke JO, Kwiatek M, Kahrilas PJ. Impaired deglutitive EGJ relaxation in clinical esophageal manometry: a quantitiative analysis of 400 patients and 75 controls. Am J Physiol. 2007;293:G878–G885. doi: 10.1152/ajpgi.00252.2007. [DOI] [PubMed] [Google Scholar]
- 4.Ghosh SK, Kahrilas PJ, Lodhia N, Pandolfino JE. Utilizing intraluminal pressure differences to predict esophageal bolus flow dynamics. Am J Physiol. 2007;293:G1023–G1028. doi: 10.1152/ajpgi.00384.2007. [DOI] [PubMed] [Google Scholar]
- 5.Pandolfino JE, Ghosh SK, Rice J, Clarke JO, Kwiatek MA, Kahrilas PJ. Classifying esophageal motility by pressure topography characteristics: a study of 400 patients and 75 controls. Am J Gastroenterol. doi: 10.1111/j.1572-0241.2007.01532.x. In Press. [DOI] [PubMed] [Google Scholar]
- 6.Kahrilas PJ, Ghosh SK, Pandolfino JE. Esophageal motility in terms of pressure topography: the Chicago classification. J Clin Gastroenterol. doi: 10.1097/MCG.0b013e31815ea291. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]


