Abstract
OBJECTIVE
To estimate how social support and social conflict relate to prenatal depressive symptoms and to generate a brief clinical tool to identify women at increased psychosocial risk.
METHODS
This is a prospective study following 1,047 pregnant women receiving care at two university-affiliated clinics from early pregnancy through 1 year postpartum. Structured interviews were conducted in the second trimester of pregnancy. Hierarchical and logistic regressions were used to examine potential direct and interactive effects of social support and conflict on prenatal depressive symptoms measured by the Center for Epidemiologic Studies-Depression Scale.
RESULTS
Thirty-three percent of the sample reported elevated levels of depressive symptoms predicted from sociodemographic factors, social support, and social conflict. Social support and conflict had independent effects on depressive symptoms although social conflict was a stronger predictor. There was a “dose–response,” with each increase in interpersonal risk factor resulting in consequent risk for probable depression based on symptom reports (Center for Epidemiologic Studies-Scale greater than or equal to 16). A composite of one social support and three conflict items were identified to be used by clinicians to identify interpersonal risk factors for depression in pregnancy. Seventy-six percent of women with a composite score of three or more high-risk responses reported depressive symptoms.
CONCLUSION
Increased assessment of social support and social conflict by clinicians during pregnancy can identify women who could benefit from group or individual interventions to enhance supportive and reduce negative social interactions.
Pregnancy is a time of profound physical and emotional change that inherently affects interpersonal relationships. Social interactions and conflict and the individual's response to them can be crucial triggers for depression.1,2 Social conflict can be defined as behaviors or interactions perceived as harmful, critical, and hostile and contribute to poor psychological outcome.3–5 Interpersonal risk factors such as insufficient social support and aggravated social conflict may have profound effects on women's mental and physical health during pregnancy,6–10 influencing pregnancy outcomes either directly or indirectly through unhealthy life style factors such as smoking or alcohol.11–14 Among women who gave birth to low birth weight infants, women who experienced any interpersonal conflict gave birth to infants with a mean weight of 261 g lower than women without conflict.15 There are also societal costs, including increased use of healthcare resources and lost productivity.16
Recently, attention regarding prenatal depression and screening during pregnancy has increased.17 Despite recommendations that healthcare providers offer routine and comprehensive screening for psychosocial risk factors during pregnancy,18 interpersonal violence and emotional distress often go unrecognized during routine encounters.19–21
Assessing the quality of women's social relationships (ie, social support and social conflict) can provide important information to identify pregnant women who may be at heightened psychosocial risk, beyond the information provided by screening for depression screening alone. Many women may be reluctant to report depressive symptoms because of stigma associated with mental health problems.22 Other women may attribute depressive symptoms to pregnancy, given the overlap in physiological symptoms (eg, sleeping and eating changes, somatic complaints).23 In both of these cases, women may under-report depressive symptoms, yet be more accurate in reporting related interpersonal risk factors.24 Moreover, assessing for psychosocial risk may provide direction for intervention efforts beyond traditional mental health treatment. Hogan Linden and Najarian3 provide a comprehensive evaluation of the efficacy of social support interventions. Cost- and time-effective group interventions to increase supportive networks can be built into prenatal care through models such as CenteringPregnancy (Centering Pregnancy and Parenting Association, Inc., Cheshire, CT) group prenatal care.25 Similarly, interventions aimed at reducing social conflict could take the form of conflict resolution, anger management, or stress reduction groups, as opposed to individual therapy. These programs may be more acceptable to pregnant women, and potentially more cost-effective to community agencies
This study was novel in that it simultaneously examined social support and social conflict as risk factors associated with self-reported depressive symptoms during early pregnancy. The primary aim of this study was to estimate how social support and social conflict relate to prenatal depressive symptoms in a sample of low-income, primarily minority women. Specifically, we examined potential independent and interactive effects of social support and social conflict on depressive symptoms. Although research on prenatal depression has demonstrated the importance of social support and social conflict, few studies have translated study results into strategies for clinical practice. Thus, the second aim was to generate a brief clinical assessment tool to help clinicians identify women at increased psychosocial risk because of limited social support or increased social conflict.
MATERIALS AND METHODS
Data for this study are from a larger study of young pregnant women (ages 14−25) enrolled in a randomized controlled trial aimed at promoting improved outcomes through group prenatal care.26,27 This was a prospective study following participants from early pregnancy through 1 year postpartum. Participants were recruited from large university affiliated obstetrics and gynecology clinics within the New Haven Hospital System, New Haven, Connecticut and Grady Memorial Hospital, Atlanta, Georgia. Inclusion criteria were 1) pregnant at less than 24 weeks gestation; 2) age at last birthday 25 years or younger; 3) no severe medical problem requiring individualized assessment and tracking as “a high-risk pregnancy”; 4) able to attend groups conducted in English or Spanish; and 5) willingness to be randomly assigned to group or individual prenatal care. Of 1,542 eligible adolescents and young women, 1,047 enrolled in the study (68% participation rate). Participants were predominantly African-American and Latina (mostly Puerto Rican), reflecting the population of prenatal patients using these clinics.
Between September 2001 and December 2004, young women attending their first or second prenatal care visit were referred by a health care provider or approached directly by research staff to be screened for eligibility. For eligible participants, research staff explained the study in detail, answered any questions, and obtained informed consent.
Baseline interviews occurred in the second trimester, at an average gestational age of 18 weeks (standard deviation±3.3). Structured interviews were conducted by audio computer-assisted self-interviewing.28 Audio computer-assisted self-interviewing allows respondents to listen over headphones to spoken questions that have been digitally recorded and stored on a computer, as well as displayed on the computer's screen. This technology helps participants who have lower reading skills complete psychological and behavioral measures with greater ease. All procedures were approved by the Yale University and Emory University Human Investigation Committees and by Institutional Review Boards at study centers. Participants were paid $25 for each interview.
Social support, a 7-item subscale of the Social Relationship Scale,29 assessed perceived availability of emotional and material support (eg, to talk about an interpersonal problem, to borrow money in a medical emergency, or for advice in making a decision). In the original study, Cronbach's α30 for this subscale was .8729 Cronbach's α30 provides a measure of inter-item correlation as an indicator of internal consistency, one form of measurement reliability. All responses were on a 5-point scale, ranging from 1=“definitely not” to 5=“definitely yes.” Items were summed to form a total score, ranging from 7 to 35.
Seven items of the social conflict subscale of the Social Relationship Scale assessed the perceived degree of social conflict in an individual's everyday social network. It assessed the potential costs of a large or close social network. The first six items asked the participant to rate perceived degree of conflict in interpersonal relationships in the past month. Possible responses on a 5-point scale ranged from 1=“definitely no” to 5=“definitely yes.” The seventh item asked the participant to indicate how often she had been involved in a social interaction or exchange that was unpleasant or distressing in the past month. Six possible responses ranged from 1=“every day” to 6=“not at all.” Cronbach's α30 for the measure was .84. Support and conflict items of the Social Relationship Scale were drawn from surveys conducted at The University of Michigan's Institute for Social Research at the time of scale development, including the work of Antonucci, Cobb, French, House, Kahn, Kessler, and Vinokur, and from Norbeck and colleagues31.
The Center for Epidemiological Studies-Depression Scale (CES-D)32 is a widely used, 20-item scale designed to measure major components of clinical depression. Respondents rate the frequency with which they experienced depression symptoms (e.g., crying, hopelessness) over the last 7 days on a 0−3 scale. Like prior studies among pregnant women, we used only the 15 cognitive- affective items of the scale, eliminating five somatic items that could reflect symptoms of pregnancy or depression (e.g., fatigue, appetite change).33 Cronbach's alpha30 for the Center for Epidemiological Studies-Depression Scale cognitive-affective subcomponent was .85.
Participants provided information about demographic characteristics using a measure designed for this study: age, race (African-American, Latina, or white or other), education (high school degree or currently in school or high school dropout), employment (full time or part-time or unemployed), number of previous children (0, 1, or 2), gestational age at baseline interview, relationship status with infant's father (currently in romantic relationship or not), and current cohabitation with infant's father (yes or no). In addition, level of community poverty (more than 25% of census tract below poverty level) was measured based on percent of people below poverty within the participant's census tract.
Hierarchical regression was used to examine potential additive and interactive effects of social support and social conflict on prenatal depression. Hierarchical regression involves prediction of variance in a continuous dependent variable (ie, depressive symptoms) from blocks of related independent variables to examine additive and unique effects of different variables.34 Sociodemographic variables were entered as covariates in the first block, social support and social conflict were entered in the second block, and the interaction between social support and social conflict were entered in the third block, using the Baron and Kenny35 framework for testing for interactions. Next, logistic regression was used to examine how social support and social conflict items individually predict elevated depression, based on cutoff scores on the Center for Epidemiological Studies-Depression Scale used to denote “probable depression.” The sample size of 1,047 provides sufficient power (1–B>.80) to detect small effects (r<.15) in these analyses.
RESULTS
Demographic characteristics are presented in Table 1. By design, the sample was comprised of young women, with 49% of participants aged younger than 20 years at study entry. The majority (80%) were African American. Only 31% were currently employed; most had completed high school or were currently in school (75%). Two-thirds were nulliparous. Seventy percent of participants were in a relationship with the infant's father, with 38% cohabitating.
Table 1.
Baseline Demographic Characteristics of the Study Group, Including Parity and Poverty Level
| n (%) | Mean (±SD) | |
|---|---|---|
| Age (range 14−25 y) | 20.42 (±2.62) | |
| Gestational age (range 8−30 wk) | 18.10 (±3.33) | |
| Race or ethnicity | ||
| African-American | 833 (80) | |
| Latina | 133 (13) | |
| White or other | 81 (7) | |
| In HS or completed HS | 780 (75) | |
| Employed | 326 (31) | |
| In relationship with infant's father | 728 (70) | |
| Living with infant's father | 397 (38) | |
| Number of previous children | ||
| None | 667 (64) | |
| One | 258 (24) | |
| Two or more | 122 (12) | |
| Census tract below poverty level, range .01−.71 | .26 (±.14) | |
| In community with more than 25% below poverty level | 340 (33) |
SD, standard deviation; HS, high school.
Participants reported relatively high levels of social support and moderate levels of social conflict: mean scores, respectively, were 4.17 (standard deviation [SD]±.85; median 4.46, interquartile range 3.71−4.86) and 2.94 (SD ±1.03; median 3; interquartile range 2.14−3.71). The Pearson r correlation between social support and social conflict was −.41, P<.001. Based on cutoff scores for denoting “probable depression” in research using community samples, 33% of participants reported elevated levels of depressive symptoms (Center for Epidemiological Studies-Depression Scale more than 16; mean 12.74, median 11; SD ±8.45, interquartile range 6−18; range 1−43).
Table 2 presents results from hierarchical regression predicting depressive symptoms from sociodemographic factors, social support, and social conflict. Together, sociodemographic factors accounted for only 5% of the variance in depressive symptoms, with education and relationship status emerging as the only uniquely significant factors to predict depressive symptoms. Those with less education and not in a relationship with the infant's father were more likely to have depressive symptoms. Both social support (β=.21, P<.001) and social conflict (β=.47, P<.001) had independent effects on depressive symptoms and together accounted for an additional 34% of the variance in depressive symptoms. Social conflict emerged as a stronger predictor of depressive symptoms than social support. Finally, the interaction between social support and social conflict was non-significant; thus, these results do not provide support for an interactive or multiplicative effect of the two interpersonal factors on depressive symptoms.
Table 2.
Hierarchical Regression Analysis Predicting Depressive Symptoms From Sociodemographic Factors, Social Support, and Social Conflict
| r | Final β | ΔR2 | |
|---|---|---|---|
| Block 1: sociodemographic factors | .05* | ||
| Site | .02 | .02 | |
| Age | -.06 | -.04 | |
| Gestational age | -.02 | -.00 | |
| Parity | -.05 | -.05 | |
| African-American | -.01 | -.03 | |
| Latina | .01 | .02 | |
| Relationship with infant's father | -.15† | -.09† | |
| Living with infant's father | -.04 | .03 | |
| Education | .13† | .07† | |
| Unemployed | .11† | .02 | |
| Community poverty | -.03 | -.01 | |
| Block 2: interpersonal factors | .34† | ||
| Social support | -.45† | -.21† | |
| Social conflict | .58† | .47† | |
| Block 3: interaction | .00 | ||
| Social support × social conflict | .02 | -.05 |
r, Pearson bivariate correlation; Final β, standardized beta from final model; ΔR2, change in total variance accounted for in model by each block entered into hierarchical regression.
The final model was significant, F (14, 1,012)=46.60, P<.001, adjusted R2=.38.
P<.001.
P<.01.
Post hoc analyses were conducted to examine whether the effect of social support and social conflict on depression differed depending on site, age, race, parity, relationship status with infant's father, education, employment, or community poverty. No significant interactions were found, indicating that within this sample of low-income, young women, the effect of social support and social conflict on depressive symptoms is similar across various sociodemographic characteristics.
Having established that both social support and social conflict have independent effects on depressive symptoms, the next objective of these analyses aimed to identify a specific clinical assessment that could be used by clinicians to best identify pregnant women with interpersonal risk factors for depression. For these analyses, the 1−5 response scales for the social support and social conflict items were dichotomized to reflect high-risk or low-risk responses, with the two least favorable responses reflecting high risk. For example, on items such as, “Do you have someone to talk to when you are upset?” responses of “Definitely not” or “Probably not” were collapsed to reflect high risk, and responses of “Possibly, Probably yes, and Definitely yes” were collapsed to reflect low risk.
The associations between dichotomized items and elevated depression were first computed with unadjusted odds ratios. Then, multivariable logistic regression was used to estimate the unique effect of these items on elevated depressive symptoms, controlling for sociodemographic characteristics. Four items (SS4, PSC1, PSC4, PSC7) were associated with an odds ratio of 2 or higher in multivariate analysis (Table 3). None of the other items on the social conflict or social support scale had an odds ratio greater than 2.
Table 3.
Unadjusted and Adjusted Odds Ratio for Four Key Social Support and Social Conflict Items Predicting Elevated Depression in Logistic Regression Analysis (n=1,047)
| Item | Unadjusted OR | Adjusted OR |
|---|---|---|
| SS4: Are there people in your life you could turn to if you needed to borrow $10, get a ride to the doctor, or some other small immediate help? | 4.86* (3.03−7.80) | 2.29† (1.21−4.33) |
| PSC1: Do you feel that people in your life let you down by not showing you as much love and concern as you would have liked? | 4.04* (3.02−5.41) | 2.17* (1.51−3.11) |
| PSC4: Have you felt tense from arguing or disagreeing with people in your personal life? | 4.01* (2.99−5.40) | 2.06* (1.39−3.06) |
| PSC7: How often in the last month were you involved in a social interaction that was unpleasant or distressing? | 3.73* (2.74−5.06) | 2.22* (1.54−3.20) |
OR, odds ratio; SS, social support; PSC, social conflict.
Data in parentheses are 95% confidence intervals.
In multivariable analysis for adjusted odds ratios, sociodemographic variables were used as covariates and all social support and social conflict items were entered simultaneously. The entire scale is available upon request from Dr. Kerth O'Brien at obrienk@pdx.edu.
P<.001.
P<.01.
A variable reflecting a count of high-risk responses on these four key items was computed. This interpersonal risk composite was entered as a predictor of elevated depression in logistic regression, controlling for sociodemographic factors. Relative to women who gave no high-risk responses (ie, women with a 0 on the interpersonal risk composite; n=346), the odds of depression were significantly higher in women with one risk response (adjusted odds ratio [AOR] 3.37, 95% confidence interval [CI] 2.21−5.15; n=357), two risk responses (AOR 9.12, 95% CI 5.87−14.18; n=243), three risk responses (AOR 28.34, 95% CI 14.78−54.34; n=78), and four risk responses (AOR 28.20, 95% CI 9.60−82.75; n=23). Figure 1 illustrates the percentage of women with elevated depression for each grouping on the interpersonal risk composite. As shown, there was a “dose–response” effect, with each increase in interpersonal risk resulting in consequent risk for probable depression based on symptom reports (ie, Center for Epidemiologic Studies-Depression Scale 16 or more). A test of linear increase was significant, χ2 test of linear association was 199.2, df 1, n=1,047, P<.001). Specifically, although only 11% of women with a 0 on the interpersonal risk composite reported depressive symptoms, 29% of those with one risk factor reported depressive symptoms, 51% of those with two risk factors reported depressive symptoms, and more than 76% of those with three or more risk factors reported depressive symptoms.
Fig. 1.
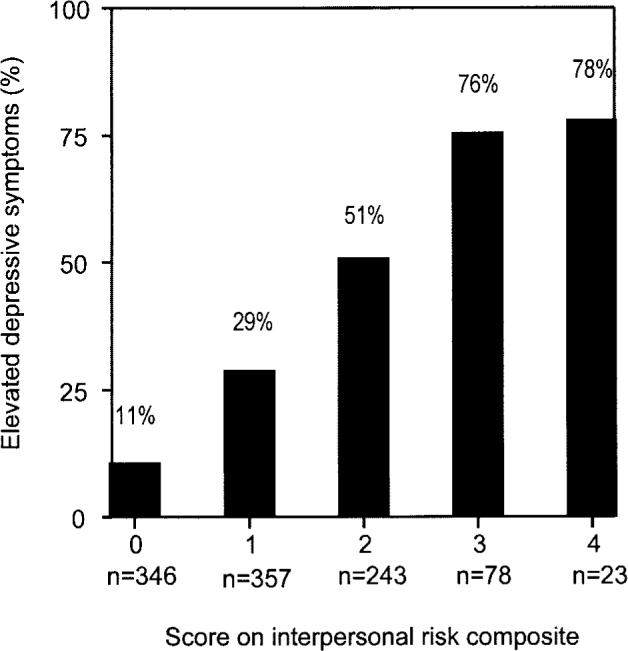
Percent of women with elevated depressive symptoms among women with different scores on the interpersonal risk composite. Scores on the interpersonal risk composite reflect how many of the four key interpersonal risk factors were endorsed (SS4, PSC1, PSC4, PSC7). Bars show the percent of women with elevated depressive symptoms on the Center for Epidemiologic Studies-Depression Scale (16 or more) in groups with varying interpersonal risk factor composite scores. SS, social support; PSC, social conflict. Both scales are from the Social Relationship Scale.28
DISCUSSION
Rates of depression especially during the second and third trimester are substantial; 33% of the women in this sample score 16 or more on the Center for Epidemiologic Studies-Depression Scale. Milan and Ickovics9 found a 30% prevalence using the Center for Epidemiologic Studies-Depression Scale in a similar population. For women of low socioeconomic status, the rates of depressive symptoms by self-report for the second trimester were 39% and 47%.36
Interpersonal factors of social support and social conflict play a substantial role in the experience of depressive symptoms in pregnancy. Within this sample of low-income, young pregnant women, most women reported relatively high levels of social support and moderate levels of social conflict. The interpersonal risk factors of low social support and high social conflict independently predict depressive symptoms in pregnancy, suggesting that social support does not buffer these women from the effects of social conflict. In our study population, social conflict was more strongly related to depression than social support. The relationship among social support, social conflict, and depression may be universal among low-income, young pregnant women because the effect of social support and social conflict on depressive symptoms in pregnancy was similar across age, race, parity, education, relationship with infant's father, community poverty, and employment.
It is common practice for obstetricians and midwives to assess levels of social support in pregnant clients and make recommendations to enhance and strengthen interpersonal support networks. It is less common for clinicians to assess for areas of interpersonal conflict. The Postpartum Depression Predictors Inventory, a widely used instrument to assess pregnant women for risk for postpartum depression, includes four questions assessing social support and none specifically addressing social conflict.37 Four items emerged from our research that capture the interpersonal risk factors most strongly associated with depression. One item assesses the presence of social support to provide for small immediate help. Three items assess social conflict including feeling let down and unloved, feeling tense from arguing, and the frequency of unpleasant and distressing social interactions. (Table 3) These items could be used as screening questions within a busy clinical situation to identify and target women in the second trimester of pregnancy who could benefit from early prevention efforts and clinical interventions to resolve interpersonal conflict effectively.
We found a strong dose–response effect, whereby as the number of interpersonal risk factors increased, so too did the proportion of women reporting depressive symptoms. This ranged from 11% of women reporting high depressive symptoms among those with no interpersonal risk factors, to 78% of women reporting high depressive symptoms among those with four interpersonal risk factors. Although the goal of this article is not to determine a specific cutoff score, these four questions could be used to target discussion in the clinical setting. It would be reasonable to use a cutoff of three or more high-risk responses to the four screening questions as the threshold to refer or offer intervention to strengthen interpersonal relationships. Addressing the interpersonal risk factor of social conflict could make a positive contribution toward improving pregnancy outcomes and postpartum function of young pregnant women.
Interpretation of these findings must recognize the limitations of this study. Self-reported depressive symptoms were measured, rather than the syndrome “depression” as defined in the Diagnostic and Statistical Manual of Mental Disorders. However, the cognitive-affective component of the Center for Epidemiologic Studies-Depression Scale has been demonstrated to be predictive of depression in pregnancy.32 The study population also represents a predominantly young group of nulliparous women with limited socioeconomic resources. Depressive symptoms in a more demographically and economically diverse group may identify other factors that are more useful. Our results were also limited to second trimester screening and may not be generalized to screening later in pregnancy or postpartum. Further longitudinal research could elucidate the cause and effect relationship between interpersonal risk factors and pregnancy depression and gestational age, because the impending birth will have distinct effects on social interactions. Strengths of this study include its prospective design and inclusion of a large sample of low-income, minority women from two distinct communities, a demographic underrepresented in research studies.
In conclusion, this study adds to our understanding of the contribution of low social support and high social conflict to depressive symptoms in pregnancy among low-income, minority young women. The findings identify four questions to assist clinicians to assess interpersonal conflict and social support to identify pregnant women most vulnerable to depression These women can be recognized and targeted for prevention efforts to assist them with strategies to build supportive relationships, and reduce interpersonal conflict during pregnancy to reduce their risk for depression and improve the health and function of both mothers and infants.
Acknowledgments
Funded by grant number NIMH R01 MH/HD61175, to Jeannette R. Ickovics, PhD.
Footnotes
Financial Disclosure The authors have no potential conflicts of interest to disclose.
REFERENCES
- 1.Paarlberg KM, Vingerhoets AJ, Passchier J, Heinen AG, Dekker GA, van Geijn HP. Psychosocial factors as predictors of maternal well-being and pregnancy-related complaints. J Psychosom Obstet Gynaecol. 1996;17:93–102. doi: 10.3109/01674829609025669. [DOI] [PubMed] [Google Scholar]
- 2.Seguin L, Potvin L, St-Denis M, Loiselle J. Chronic stressors, social support, and depression during pregnancy. Obstet Gynecol. 1995;85:583–9. doi: 10.1016/0029-7844(94)00449-N. [DOI] [PubMed] [Google Scholar]
- 3.Hogan BE, Linden W, Najarian B. Social support interventions–do they work? Clin Psychol Rev. 2002;22:383–442. doi: 10.1016/s0272-7358(01)00102-7. [DOI] [PubMed] [Google Scholar]
- 4.Pagel MD, Erdly WW, Becker J. Social networks: we get by with (and in spite of) a little help from our friends. J Pers Soc Psychol. 1987;53:793–804. doi: 10.1037//0022-3514.53.4.793. [DOI] [PubMed] [Google Scholar]
- 5.Rook KS. The negative side of social interaction: impact on psychological well-being. J Pers Soc Psychol. 1984;46:1097–108. doi: 10.1037//0022-3514.46.5.1097. [DOI] [PubMed] [Google Scholar]
- 6.Paarlberg KM, Vingerhoets AJ, Passchier J, Dekker GA. Psychosocial factors and pregnancy outcome: a review with emphasis on methodological issues. J Psychosom Res. 1995;39:563–95. doi: 10.1016/0022-3999(95)00018-6. [DOI] [PubMed] [Google Scholar]
- 7.Jesse DE, Walcott-McQuigg J, Mariella A, Swanson MS. Risks and protective factors associated with symptoms of depression in low-income African American and Caucasian women during pregnancy. J Midwifery Womens Health. 2005;50:405–10. doi: 10.1016/j.jmwh.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 8.McKee MD, Cunningham M, Jankowski KR, Zayas L. Health-related functional status in pregnancy: relationship to depression and social support in a multi-ethnic population. Obstet Gynecol. 2001;97:988–93. doi: 10.1016/s0029-7844(01)01377-1. [DOI] [PubMed] [Google Scholar]
- 9.Milan S, Ickovics JR, Kershaw T, Lewis J, Meade C, Ethier K. Prevalence, course, and predictors of emotional distress in pregnant and parenting adolescents. J Consult Clin Psychol. 2004;72:328–40. doi: 10.1037/0022-006X.72.2.328. [DOI] [PubMed] [Google Scholar]
- 10.Copper RL, Goldenberg RL, Das A, Elder N, Swain M, Norman G, et al. The preterm prediction study: maternal stress is associated with spontaneous preterm birth at less than thirty-five weeks' gestation. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Am J Obstet Gynecol. 1996;175:1286–92. doi: 10.1016/s0002-9378(96)70042-x. [DOI] [PubMed] [Google Scholar]
- 11.Ahluwalia IB, Mack KA, Mokdad A. Mental and physical distress and high-risk behaviors among reproductive-age women. Obstet Gynecol. 2004;104:477–83. doi: 10.1097/01.AOG.0000137920.58741.26. [DOI] [PubMed] [Google Scholar]
- 12.Orr ST, James SA, Blackmore Prince C. Maternal prenatal depressive symptoms and spontaneous preterm births among African-American women in Baltimore, Maryland. Am J Epidemiol. 2002;156:797–802. doi: 10.1093/aje/kwf131. [DOI] [PubMed] [Google Scholar]
- 13.Dole N, Savitz DA, Hertz-Picciotto I, Siega-Riz AM, McMahon MJ, Buekens P. Maternal stress and preterm birth. Am J Epidemiol. 2003;157:14–24. doi: 10.1093/aje/kwf176. [DOI] [PubMed] [Google Scholar]
- 14.Hedegaard M, Henriksen TB, Sabroe S, Secher NJ. Psychological distress in pregnancy and preterm delivery. BMJ. 1993;307:234–9. doi: 10.1136/bmj.307.6898.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grimstad H, Schei B, Backe B, Jacobsen G. Interpersonal conflict and physical abuse in relation to pregnancy and infant birth weight. J Womens Health Gend Based Med. 1999;8:847–53. doi: 10.1089/152460999319165. [DOI] [PubMed] [Google Scholar]
- 16.Andersson L, Sundstrom-Poromaa I, Wulff M, Astrom M, Bixo M. Implications of antenatal depression and anxiety for obstetric outcome. Obstet Gynecol. 2004;104:467–76. doi: 10.1097/01.AOG.0000135277.04565.e9. [DOI] [PubMed] [Google Scholar]
- 17.Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, et al. Perinatal depression: prevalence, screening accuracy, and screening outcomes. Evid Rep Technol Assess (Summ) 2005:1–8. doi: 10.1037/e439372005-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American College Obstetricians and Gynecologists. ACOG Educational Bulletin. Vol. 255. ACOG; Washington, DC: 1999. Psychosocial risk factors: perinatal screening and intervention. [PubMed] [Google Scholar]
- 19.Roter DL, Hall JA, Kern DE, Barker LR, Cole KA, Roca RP. Improving physicians' interviewing skills and reducing patients' emotional distress. A randomized clinical trial. Arch Intern Med. 1995;155:1877–84. [PubMed] [Google Scholar]
- 20.Parker B, McFarlane J, Soeken K. Abuse during pregnancy: effects on maternal complications and birth weight in adult and teenage women. Obstet Gynecol. 1994;84:323–8. [PubMed] [Google Scholar]
- 21.Durant T, Colley Gilbert B, Saltzman LE, Johnson CH. Opportunities for intervention: discussing physical abuse during prenatal care visits. Am J Prev Med. 2000;19:238–44. doi: 10.1016/s0749-3797(00)00232-4. [DOI] [PubMed] [Google Scholar]
- 22.Shakespeare J, Blake F, Garcia J. A qualitative study of the acceptability of routine screening of postnatal women using the Edinburgh Postnatal Depression Scale. Br J Gen Pract. 2003;53:614–9. [PMC free article] [PubMed] [Google Scholar]
- 23.Righetti-Veltema M, Conne-Perreard E, Bousquet A, Manzano J. Risk factors and predictive signs of postpartum depression. J Affect Disord. 1998;49:167–80. doi: 10.1016/s0165-0327(97)00110-9. [DOI] [PubMed] [Google Scholar]
- 24.Kennedy HP, Beck CT, Driscoll JW. A light in the fog: caring for women with postpartum depression. J Midwifery Womens Health. 2002;47:318–30. doi: 10.1016/s1526-9523(02)00272-6. [DOI] [PubMed] [Google Scholar]
- 25.Massey Z, Rising SS, Ickovics J. CenteringPregnancy group prenatal care: promoting relationship-centered care. J Obstet Gynecol Neonatal Nurs. 2006;35:286–94. doi: 10.1111/j.1552-6909.2006.00040.x. [DOI] [PubMed] [Google Scholar]
- 26.Ickovics J, Kershaw T, Westdahl C, Rising SS, Klima C, Reynolds H, et al. Group prenatal care improves preterm birth weight: results from a matched cohort study at public clinics. Obstet Gynecol. 2003;102:1051–7. doi: 10.1016/s0029-7844(03)00765-8. [DOI] [PubMed] [Google Scholar]
- 27.Kershaw TS, Milan S, Westdahl C, Lewis J, Rising SS, Fletcher R, et al. Avoidance, anxiety, and sex: the influence of romantic attachment on HIV-risk among pregnant women. AIDS Behav. 2007;11:299–311. doi: 10.1007/s10461-006-9153-z. [DOI] [PubMed] [Google Scholar]
- 28.C'de Baca J, Lapham SC, Skipper BJ, Watkins ML. Use of computer interview data to test associations between risk factors and pregnancy outcomes. Comput Biomed Res. 1997;30:232–43. doi: 10.1006/cbmr.1997.1449. [DOI] [PubMed] [Google Scholar]
- 29.O'brien K, Wortman CB, Kessler RC, Joseph JG. Social relationships of men at risk for AIDS. Soc Sci Med. 1993;36:1161–7. doi: 10.1016/0277-9536(93)90236-w. [DOI] [PubMed] [Google Scholar]
- 30.Norbeck JS, Lindsey AM, Carrieri VL. The development of an instrument to measure social support. Nurs Res. 1981;30:264–9. [PubMed] [Google Scholar]
- 31.Radloff L. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 32.Kalichman SC, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV-AIDS. J Nerv Ment Dis. 2000;188:662–70. doi: 10.1097/00005053-200010000-00004. [DOI] [PubMed] [Google Scholar]
- 33.Allen MJ, Yen WM. Introduction to measurement theory. Waveland Press; Prospect Heights (IL): 2002. [Google Scholar]
- 34.Cohen J, Cohen P. Applied multiple regression-correlation analysis for the behavioral sciences. L. Erlbaum Associates, Inc; Hillsdale (NJ): 1983. [Google Scholar]
- 35.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 36.Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of depression during pregnancy: systematic review. Obstet Gynecol. 2004;103:698–709. doi: 10.1097/01.AOG.0000116689.75396.5f. [DOI] [PubMed] [Google Scholar]
- 37.Beck CT. Revision of the postpartum depression predictors inventory. J Obstet Gynecol Neonatal Nurs. 2002;31:394–402. doi: 10.1111/j.1552-6909.2002.tb00061.x. [DOI] [PubMed] [Google Scholar]


