Abstract
Introduction
This article examines the literature on ADHD and unintentional driving injury. This literature has emerged over the last decade as part of the burgeoning epidemic of road traffic death and injury which is the number one cause of death in young adults in North America.
Methods
The available literature on observational outcome studies and experimental pharmacological interventions is critically reviewed. A meta-analysis of behavioral outcomes and a review of effect size of pharmacological studies are presented.
Results
Current data support the utility of stimulant medication in improving driving performance in younger ADHD drivers. A conceptual model of risk factors in young ADHD drivers is offered.
Conclusion
The current state of screening instruments for identifying high risk subjects within this clinical group is summarized along with a final section on emerging trends and future prospects for intervention.
Keywords: ADHD, motor vehicle collisions, non-accidental injury, meta-analysis
Résumé
Introduction
le présent article passe en revue la littérature sur le TDAH et les blessures non intentionnelles dues aux accidents de voiture. Cette littérature est apparue au cours des dix dernières années à la suite des nombreux accidents de la route qui sont la principale cause de mortalité chez les jeunes adultes en Amérique du nord.
Méthodologie
l’analyse des résultats et les interventions pharmacologiques expérimentales font l’objet d’une étude critique. L’article présente une méta-analyse des résultats du comportement des conducteurs, et évalue l’ampleur des études pharmacologiques et leur effet.
Résultats
les données actuelles attestent que les stimulants améliorent la conduite automobile des jeunes conducteurs qui souffrent de TDAH. L’article propose un modèle conceptuel des facteurs de risque chez ces mêmes jeunes conducteurs.
Conclusion
les auteurs récapitulent les instruments de dépistage qui permettent de détecter les sujets à risque élevé à l’intérieur de ce groupe ; ils concluent en présentant les tendances qui émergent et les possibilités futures en matière d’intervention.
Keywords: TDAH, accidents de voiture, blessures non intentionnelles, méta-analyse
Introduction
In the past decade, research has demonstrated an association between individuals with Attention Deficit Hyperactivity Disorder (ADHD) and driving (Barkley & Cox, in press). This common psychiatric disorder with its onset in childhood often persists throughout the life span and is characterized by symptoms of inattention, impulsiveness and hyperactivity (American Psychiatric Association, 1994). The disorder also encompasses many demographic, cognitive, and personality factors, described below, that are also related to driving risks and unintentional injury on the road, e.g., male gender, inattention and risk taking. This review will examine the available research regarding the relationship between ADHD and unintentional driving injury. In this review we propose that ADHD drivers are at increased risk because of an underlying problem with executive functioning. A better understanding of this relationship would help quantify risk factors related to driving that are unique to this condition as well as lead to the development, of screening instruments and countermeasures for this at-risk group of drivers. Such instruments have the potential for reducing morbidity and mortality for the patient and have important public health implications for the driving population at large.
Unintentional injury is a global public health concern. In the year 2000, an estimated five million people worldwide died from injuries (World Health Organization [WHO], 2002a). Unintentional injuries account for more than two-thirds of all injuries, the majority of which are related to road traffic (WHO, 2002a). The World Health Organization (WHO) reported that every year approximately 1.2 million people die and 50 million are injured from Motor Vehicle Collisions (MVC) and they estimated that by 2020 there would be a substantial increase in road traffic fatalities worldwide without appropriate action (WHO, 2004).
In high income countries, MVCs are the leading cause of death among children, adolescents and young adults (ages 4–29) (WHO, 2002b) and therefore, are considered a major cause of premature death and long-term disability. In the United States in 2004, there were close to 6.2 million MVCs that resulted in 42,636 deaths and close to three million injuries (National Highway Traffic Safety Administration [NHTSA], 2004). The economic burden of MVCs is extremely high and in the year 2004, traffic collisions alone cost the United States 230.6 billion dollars (NHTSA, 2004).
Public health policy is increasingly recognizing the burgeoning toll of death and morbidity to health services in North America. The WHO designated 2004 as the Road Safety year in recognition of this world wide epidemic; their logo was “Road safety is no accident”. In a joint statement in 2004, Health Canada and Transport Canada envisioned making Canadian roads the safest in the world by a reduction in serious injury and fatality by 30% by 2010 through a focus on preventative strategies as a major public health priority (Health Canada & Transport Canada, 2004).
Human Factor Research
There is an extensive literature on high risk driving populations. A recent report on contributing factors to MVCs stated that human factors, as opposed to vehicle and environmental factors are the predominant contributor to MVCs (United States General Accounting Office [GAO], 2003).
Risky driving behaviors are found to predict MVCs and driving citations (Blows, Ameratunga, Ivers, Lo, & Norton, 2005; McKnight & McKnight, 2000). Such behaviors include; speeding, following too close, driving under the influence of alcohol, cell phone use and not using seatbelts while driving. These behaviors cluster in young drivers and a propensity to risk taking contributes to increased rates of unintentional injury beyond the risk due to inexperience alone (Jonah, 1986). Numerous factors including demographic variables, personality and cognitive abilities have been explored to further understand their contribution to risky driving and MVCs. Young males (Turner & McClure, 2003; Williams & Shabanova, 2003) as well as older drivers (>65 years) (Preusser, Williams, Ferguson, Ulmer, & Weinstein, 1998; Williams & Shabanova, 2003; Zhang, Fraser, Lindsay, Clarke, & Mao, 1998) are consistently found to be related to increased negative driving outcomes. The evidence shows that both educational attainment and occupational status are inversely related to motor vehicle driver collision and injury (Hasselberg & Laflamme, 2003; Murray, 1998).
The concept of accident proneness as it relates to unintentional driving injury was first elucidated in the psychiatric literature by Tillman and Hobbes (1949), Professors of Psychiatry at the University of Western Ontario. They described a characterological style in a group of accident prone drivers referred by the Ministry of Transportation for recurrent accidents. The authors coined the phrase often repeated in this literature “a man drives as he lives”. Many further studies have presented evidence for associations between personality traits including risk taking, sensation seeking, impulsivity, difficulty in dealing with tension and controlling anger, substance abuse, antisocial tendencies as well as non-conformity and risky driving behaviors or MVC (Deffenbacher, Deffenbacher, Lynch, & Richards, 2003; Jonah, 2001; Tsuang, 1985). Psychosocial models of high risk driving including descriptions of temporary states involving high stress (Lagarde, Chastang, Gueguen, Coeuret-Pellicer, Chiron, & Lafont, 2004) and Problem Behavior Theory emphasizing lifestyle factors including low parental involvement and negative peer and parental influence (Shope, Waller, Raghunathan, & Patil, 2001; Shope, Raghunathan, & Patil, 2003) have been related to risky driving and negative driving outcomes.
Cognitive abilities likely play a significant role in driving risk. Inattention and distractibility, which are directly related to risky driving behavior, are cognitive factors that have been found to account for one fourth of MVCs (Treat et al., 1977). Poor risk perception, as well as impaired capacity to deploy appropriate judgment and reasoning while driving, have also been found to play a role in risky behaviors and negative driving outcomes (McKnight & McKnight, 2000; Ryb, Dischinger, Kufera, & Read, 2006). Deficits in these higher order cognitive factors of executive functioning are thought to underlie risky driving behaviors. Such deficits are more evident in young and older drivers and likely contribute to the higher collision rates found in these age categories (McKnight & McKnight, 1993; Treat et al, 1977). Normal maturational immaturities in areas of the brain underlying executive function, evident in younger ages (Blakemore & Choudhury, 2006), together with inexperience likely contribute to increased driving risk.
Methods: Search Strategy
Relevant articles regarding the relationship between categorical diagnoses or symptoms of ADHD and driving risks, were identified using both the PUBMED and PsychINFO databases. The search terms employed include: ADHD, Driving Risk, Driver Behavior, Driver performance, Motor Vehicle Collisions, Crashes and Accidents and Driving Offences. Additional articles were identified from the review of reference lists of pertinent articles, as well as through personal communication with relevant researchers.
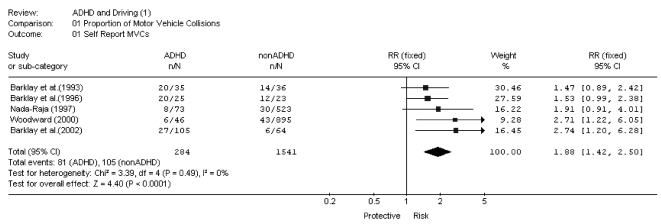
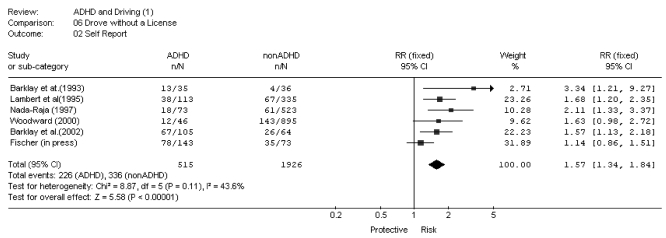
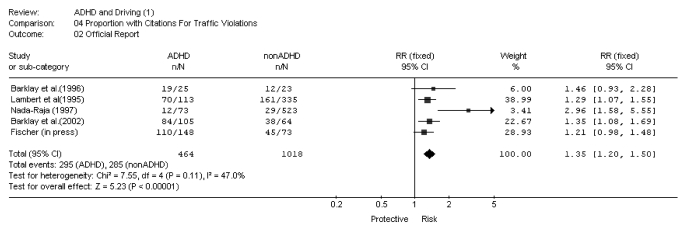
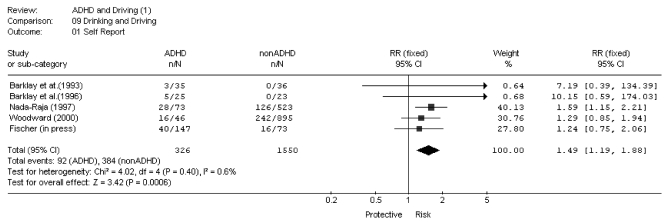
A meta-analysis (Figures 1–4) evaluating the relationship between ADHD status and various driving behaviors and outcomes was performed. Relevant categorical data was extracted and analyzed using RevMan 4.2, developed by the Cochrane Collaboration. Chi square tests were performed to assess heterogeneity between studies. P values <0.10 indicate substantial heterogeneity among the studies. The dichotomous data is expressed as relative risk (RR).
Figure 1.
Meta Analysis on ADHD Status and Proportion of Self-Reported MVCs
Figure 4.
Meta Analysis on ADHD Status and Proportion of Self Reports of Having Driven Under the Influence of Alcohol
Effect sizes (Table 3) for important driving measures in the included experimental studies were calculated using Cohen’s d. An effect size greater than 0.8 is considered a large effect, 0.5 is a medium effect and 0.2 is a small effect (Cohen, 1988). Where means and/or standard deviations were not available to calculate effect sizes, significance tests were employed (Thalheimer & Cook, 2002).
Table 3.
Effect Sizes (Cohen’s d) of medications in Experimental Conditions
| Study | Sample size | Measure | Effect Size (Cohen’s d) |
|---|---|---|---|
| (Cox et al., 2000) | 7 | ISDS 10mg MPH vs. no med | 0.97 |
| (Cox et al., 2004b) | 6 | ISDS on OROS MPH vs. regular MPH | 2pm = 0.00385
5pm = 0.81 8pm = 1.86 11pm = 1.14 |
| (Cox et al., 2004a) | 12 | Driving errors due to inattention on OROS MPH vs. no med | 1.30 |
| (Barkley et al., 2005) | 53 |
|
|
| (Barkley et al., in press) | 18 |
|
|
| (BjØrkli et al., 2004) | 17 | Standard deviation in lateral position on 20mg MPH or Placebo | 0.69 |
| (Cox et al., in press) | 35 | Overall simulator driving performance in;
|
|
ISDS=Impaired Simulator Driving Score; all measures include only participants with ADHD
Observational studies
A summary of the thirteen reviewed observational studies can be found in Table 1. Results from these prospective and retrospective studies generally indicate there is an association between individuals with ADHD and increased driving risk. Significant heterogeneity of outcome estimates amongst studies are noted and reviewed.
Table 1.
Characteristics of Observational Studies Included in the Review
| Study | Sample | Study design | Definition of risk factor | Outcome Assessed | Methodological Shortcomings |
|---|---|---|---|---|---|
| (Weiss et al., 1997) | 75 ADHD – Referrals
91% male 44 non-ADHD Volunteers 89% male Mean age: 19 (17–24) |
Prospective cohort 10–12 year follow up | Assessed in hospital clinic primarily for restlessness and poor concentration at home and at school. | Driving Outcomes (S) | 1,2,3,4 |
| (Barkley et al., 1993) | 35 ADHD – Referrals
100% male 36 non-ADHD Volunteers 89% male Mean age: 19 (16–22) |
Prospective cohort 3–5 year follow up | ADHD diagnosis – DSMIII-R | Driving Outcomes
Driving Behaviour -Proxy respondent |
1,2,3,4 |
| (Murphy and Barkley, 1996) | 172 ADHD – Referrals
Mean age = 32, 68% male 30 non-ADHD, Psychiatric referrals w/out ADHD, Mean age: 36 34% male |
Cross sectional/retrospective cohort | ADHD diagnosis – DSMIII-R | Driving Outcomes (S) | 1,2,3
*Small control group |
| (Barkley et al., 1996) | 25 ADHD – Referrals
64% male 23 non-ADHD, 61% male -Volunteers and staff acquaintances Mean age: 22 (17–30) |
Cross sectional/retrospective cohort | ADHD diagnosis – DSMIV | Driving Outcomes (S&O)
Driving Performance - simulator Driving Knowledge – videotape test Driving Behaviour (S) |
1,3 |
| (Lambert et al., 1995) | 113 ADHD – Referrals
335 non-ADHD -Representative sample Mean age: 25 |
Prospective cohort – Childhood until age 25 | Proxy measure of DSMIV criteria to identify pervasive and severe childhood ADHD | Driving Outcomes (O) | 2,3 |
| (Nada-Raja et al., 1997) | 101 ADHD
46 CD/ODD 85 Anx/Dep disorders 684 No diagnosis -Birth cohort Age: 18 |
Prospective cohort 3 year follow up | Mental Health (at age 15): ADHD: 91st percentile of ADHD symptom scale | Driving Outcomes (S&O) | 2,4 |
| (Woodward et al., 2000) | 941 children grouped into 5 levels of attention difficulties
-Birth cohort age: 21 |
Prospective cohort 8 years follow up | Age 13
Extent of attentional difficulties reported by parents and teachers |
Driving Outcome (S)
Driving Behaviour (S) |
4 |
| (Barkley et al., 2002) | 105 ADHD – Referrals
75.2% male 64 non-ADHD 68.8% male -Volunteers Mean age: 21 (17–28) |
Cross sectional/retrospective cohort | ADHD DSMIV diagnosis | Driving Outcome (S&O)
Cognitive abilities – Conner’s CPT, CBDI Driving Performance - simulator Driving Knowledge – videotape test Driving Behaviour (S) Executive Functioning - Battery of tasks |
3 |
| (Richards et al., 2002) | 35 Males – 15 high ADHD; 20 low ADHD
24 female – 6 high ADHD; 18 low ADHD Mean age: 21 (18–24) Recruited University Students |
Cross sectional/retrospective cohort | Degree of current and childhood symptoms of ADHD | Driving Behaviour (S)
Driving Outcome (S) Driving Anger (S) |
1,2,3 |
| (Fischer et al., in press) | 158 ADHD – Referrals
81 non-ADHD -Volunteers Mean age 21 (19–25) Sample 91% male |
Prospective cohort >13 year follow up | ADHD DSMIV diagnosis | Driving Outcome (S&O)
Driving Performance and related cognitive abilities -simulator and on the road tests Driving Behaviour (S) |
2,3 |
| (Reimer et al., 2005) | 45 ADHD cases, 56% male
38 non-ADHD, 30, 53% male Age: 16–55 Sample from referrals to ADHD program and through advertisements |
Cross sectional/retrospective cohort | ADHD DSMIV diagnosis | Driving Behaviour (S) | 1,2,3 |
| (Malta et al., 2005) | 44 low aggression
44 high aggression Mean age: 19 45% male Recruited University Students |
Case Control | Full or sub clinical ADHD | Driving anger (S) | 1,3 |
| (Fried et al., 2006) | 26 ADHD
Mean age: 32.8 (18–51) 23 non-ADHD Mean age: 27.3 (18–51) Sample from referrals to ADHD program and through advertisements |
Cross sectional/retrospective Cohort | ADHD DSMIV diagnosis | Driving Outcomes (S)
Driving Behaviour (S) Neuropsychological testing |
1,2,3 |
Methodological Deficiencies: 1) small sample size, low power, 2) low to moderate control for confounders, 3) external validity – sample selection, 4) loss to follow up. (S) – Self Reports, (O) – Official Reports, CPT-Continuous Performance Test, CBDI – Cognitive Behavioral Driving Inventory
Driving Outcomes
Results from observational studies indicate that ADHD is likely associated with higher than normal rates of negative driving outcomes. A recent meta-analysis regarding diseases and accident involvement calculated a relative risk of 1.54 (1.12, 2.13) for ADHD (Truls, 2003). For the studies included in this review, the mean number of self-reported MVCs was significantly higher in 5 (Barkley, Guevremont, Anastopoulos, DuPaul, & Shelton, 1993; Barkley, Murphy, DuPaul, & Bush, 2002; Barkley, Murphy, & Kwasnik, 1996; Richards, Deffenbacher, & Rosen, 2002; Weiss, Hechtman, Perlman, Hopkins, & Wener, 1979) out of 7 (Barkley et al., 1993; Barkley et al., 2002; Barkley et al., 1996; Fischer, Barkley, Smallish, & Fletcher, in press; Murphy & Barkley, 1996; Richards et al., 2002; Weiss et al., 1979) studies. Official reports did indicate higher mean MVCs for the ADHD groups although results were not statistically significant (Barkley et al., 2002; Barkley et al., 1996).
Clinically, proportions are considered to be a more accurate measure than mean number of MVCs (Barkley et al., 2002). Higher mean differences between ADHD and non ADHD groups may reflect isolated individuals within the ADHD groups accounting for a disproportionate number of MVCs. Self and official reports of proportions of participants in the ADHD groups who had MVCs were not significantly higher than control groups in most of the studies which assessed this measure (Barkley et al., 1993; Barkley et al., 2002; Barkley et al., 1996; Fischer et al., in press; Lambert, 1995). However, Fried et al., (2006), found significantly more ADHD participants than controls self-reported as having being rear-ended and had more accidents on the highway. One birth cohort study found a higher proportion of MVCs for females with ADHD (Nada-Raja, Langley, McGee, Williams, Begg, & Reeder, 1997) while another found higher proportion of injury related MVCs in participants with high attentional difficulties (Woodward, Fergusson, & Horwood, 2000). These two birth cohorts used a combination of categorical DSM diagnosis criteria, as well as a measure of ADHD symptom severity which may account for the significant results compared to previous studies using only categorical diagnosis counts.
While taken together, the results provide some indication of a higher rate of MVCs for ADHD groups, the significance of these results may have been underrated as collisions are rare events and are confounded both by youth and inexperience. The more common negative driving outcomes are assessed in the following studies.
The observational studies consistently indicated that the ADHD group received more driving citations than control groups. Eight studies assessed differences in means and proportions of citations for various violations including speeding and other traffic violations, license suspensions and driving without a license (Barkley et al., 1993; Barkley et al., 2002; Barkley et al., 1996; Fischer et al., in press; Fried et al., 2006; Lambert, 1995; Murphy & Barkley, 1996; Nada-Raja et al., 1997). All but one study (Fried et al., 2006), which did not control for driving experience, showed that the ADHD groups committed significantly more violations. These results were, for the most part, corroborated with official driving records when assessed (Barkley et al., 2002; Barkley et al., 1996; Fischer et al., in press; Lambert, 1995; Nada-Raja et al., 1997). While Nada-Raja et al. (1997) found higher citation rates for females with ADHD, higher proportions of citations were associated with a diagnosis of Oppositional Defiant Disorder/Conduct Disorder (ODD/CD) in males. Barkley et al. (1993) also found many driving measures to be significantly associated with ODD/CD; however, the relative contribution of each condition could not be assessed given the high correlation between ADHD and ODD/CD ratings. Taken together, evidence from observational studies indicates that groups with ADHD are at higher risk for negative driving outcomes. The meta-analyses independently conducted on the studies reviewed here are in support of this finding. An overall relative risk of 1.88 (1.42, 2.50) was found for ADHD status and MVCs (Figure 1). This is only slightly higher than the overall Relative Risk found in the IMMORTAL study (1.54) (Truls, 2003). The other meta analyses can be found in Figures 2–4. The results indicate that ADHD status is a risk factor for various driving behaviors and outcomes.
Figure 2.
Meta Analysis on ADHD Status and Proportion of Official Reports of Citations
Driving Behaviors and Performance: Self-Report Scales and Simulators
Self-reported driving behaviors were investigated in various observational studies (Barkley et al., 1993; Barkley et al., 2002; Barkley et al., 1996; Fischer et al., in press; Fried et al., 2006; Nada-Raja et al., 1997; Reimer et al., 2005; Richards et al., 2002; Woodward et al., 2000) employing either the Driving Behaviour Rating Scale (DBRS) (Barkley et al., 1993; Barkley et al., 2002; Barkley et al., 1996; Fischer et al., in press) the Driving Behavior Questionnaire (DBQ) (Fried et al., 2006; Reimer et al., 2005; Woodward et al., 2000) or the Survey of Driving (Richards et al., 2002), which all measure risky driving behaviors. More risky driving behaviors were consistently found in ADHD groups compared to non-ADHD groups. Less safe driving habits reported by ADHD groups may contribute to increased negative driving outcomes. Self-reports, however can be unreliable sources of data (Schwartz & Oyserman,
Reimer et al. (2005) assessed the interaction between age (16–55) and ADHD status and its effect on driving behavior using the DBQ. Significant interactions between age and ADHD status were identified, after controlling for gender, for self-reported errors and violations while driving. ADHD participants more than 40 years of age had “normalized” error scores; those older than 30 years reported “normalized” violation scores. Males reported more violations than females. Current findings did not allow the authors to distinguish between learning new safer driving behaviors with age from improved avoidance of detection of violations.
Fried et al. (2006) evaluated driving behavior using the DBQ and found that the ADHD group had significantly more lapses, errors and violations than controls. Furthermore, the ADHD group was separated into low and high driving risk according to DBQ score. While no statistically significant differences between these groups were identified, there were trends for the high risk ADHD group to have more co morbidities and neuropsychological deficits characterized as slow processing speeds. While this study has a small sample size, it provides insight to the potential for a high driving risk subgroup within ADHD populations.
Three studies employed a simulator to assess driving performance. A simulator measures short term driving skills rather than established habits and practices (Barkley et al., 2002; Barkley et al., 1996; Fischer et al., in press). In two of the three studies, the ADHD group experienced significantly more scrapes, collisions (Barkley et al., 1996; Fischer et al., in press), steering variability (Fischer et al., in press) and poorer steering control (Barkley et al., 1996) that may reflect poor motor control and coordination (Barkley et al., 1996; Fischer et al., in press). A recent large-scale study using similar aged subjects was unable to replicate these results (Barkley et al., 2002), but did find significant differences in a simulator measure correlated with IQ.
Both “subjective” self-report and “objective” simulator measures show evidence of moderate problem driving in ADHD samples; the difference in reporting rates will reflect the reporting source. Subjective reports are prone to minimizing driving risks whereas simulator observations may not reveal real driving behaviors. Both of these methodologies are likely to yield conservative estimates of risk.
Cognitive Abilities Related to Driving
A number of studies examined cognitive abilities associated with safe driving performance. Measures of both inattention and impulsivity were found to be higher in the ADHD groups as compared to controls. Fisher et al.(in press) employed an on the road driving test as well as a simulated driving test to identify basic cognitive abilities that may be related to problems in driving performance. A blind observer on the actual road test found more errors in driving performance attributable to impulsivity in the ADHD group. There were no differences between groups in errors attributed to inattention and distraction. Results from the driving simulator, which assessed various reaction times, indicated impulsive response style, as well as more inattentiveness and a reduced capacity for flexible response to changing road conditions in the ADHD group.
Barkley et al. (2002) evaluated inattention and impulsive responding utilizing the Conners CPT that yielded scores of reaction time, visual discrimination and response inhibition to visual stimuli and the self-report Cognitive Behavioral Driving Inventory (CBDI). While there was no difference between groups in impulsive responding, the ADHD group was significantly less attentive on the CPT. The CBDI found no differences between the ADHD and control groups on regular visual reaction time and discrimination tasks. However, the ADHD group made more errors on reversed visual reaction differential response tasks suggesting lower rates of rule-governed behavior and on a visual scanning task, particularly in the right visual field. The significant differences in these measures in ADHD populations suggest that abnormalities in cognitive processing involving inattention and impulsivity play a role in negative driving outcomes. These two studies assessed cognitive abilities in young adults; hence the results may not generalize to older adults with ADHD.
Fried et al. (2006) explored various areas of neuropsychological functioning in ADHD participants that were separated into high and low driving risk groups. Higher-order cognitive processing was measured using the WAIS-III and Stroop tasks. Significant differences were not found between high and low risk groups although the small sample size of 26 subjects may have precluded finding a significant difference. However, there was a trend for greater deficits in processing speed on the WAIS-III subtests in the high risk ADHD group. This finding, if replicated, may provide insight into further mechanism underlying increased driving risks in high risk ADHD groups.
Two recent studies have assessed specific cognitive abilities, in ADHD participants, that are associated with driving. Cox’s group examined the time course of neuropsychological effects on 35 male adolescents diagnosed with ADHD. These participants completed three separate assessments (5, 8, 11 PM) over three days and on different medications OROS MPH, mixed amphetemine salts-extended release (MAS XR) and placebo (Wilson, Cox, Merkel, Moore, & Coghill, in press). The assessments consisted of two neuropsychological tests, the Delayed Matching-to-Sample and the Go/No-Go that measures visual memory, attention span, and response inhibition. Both OROS MPH and MAS-XR contributed to better performance over placebo. Whilst both stimulants were shown to exert an observable neuropsychological effect 15 hours after ingestion, only OROS MPH demonstrated statistically significant gains in visual memory and response inhibition as measured by the Delayed-Matching-to-Sample and Go-No-Go tests, respectively. A composite neuropsychological score and the Impaired Driving Score, a composite measure of impairment on the driving simulator calculated from a previous study (Cox, Merkel, Moore, Thorndike, Muller, & Kovatchev, in press-a), were significantly positively correlated. While this correlation is small, it suggests a connection between the neuropsychological deficits of distractibility, visual memory and impulsiveness and driving performance. This preliminary finding in a small sample lends support to OROS MPH having a more robust effect on cognitive functioning underlying driving performance particularly later in the evening.
In a second study, Cox, Punja, Powers, Merkel, Burket, & Moore, (in press-b) compared the driving performance of young adults with ADHD on manual versus automatic transmissions. Manual transmission has been found to be related to greater arousal (Zeier, 1979) and Cox et al (in press-b) both hypothesized and found it to be associated with subjective reports of higher attention while driving as well as safer driving on an objective overall simulator driving performance measure. While this was only a small pilot study, it suggests the potential for one behavioral intervention that could impact cognitive abilities and lead to safer driving in ADHD populations.
Driving Knowledge
Barkley et al. (2002; 1996) conducted videotape tests of driving knowledge which required rapid decision-making and found difference between ADHD and non-ADHD groups in some of the measures. The instrument used had not been previously validated. ADHD groups were shown to have lower scores in knowledge of driving rules and regulations than control subjects. The differences in driving knowledge between the groups was thought to reflect difficulties in rapid decision making possibly related to slow processing speed rather than a deficit in actual knowledge (Barley et al., 1996). These findings are in keeping with the findings from Fried et al. (2006) who found slower processing speed on neuropsychological testing in the high risk ADHD drivers.
Driving Anger
Trait driving anger and aggression are consistently associated with risky driving and negative driving outcomes (Arnett, Offer, & Fine, 1997; Deffenbacher, Huff, Lynch, Oetting, & Salvatore, 2000; Malta, Blanchard, & Freidenberg, 2005). Personality factors such as sensation seeking and impulsivity as well as alcohol use have all been associated with higher frequency of aggressive driving (Dahlen, Martin, Ragan, & Kuhlman, 2005; Jonah, 2001;Yu, Evans, & Perfetti, 2004), Individuals with ADHD are more likely to exhibit correlates of aggressive traits such as antisocial behavior and alcohol use (Barkley, Fischer, Edelbrock, & Smallish, 1990; Whalen, Jamner, & Henker, 2002) and additional studies have reported that anger and problems with anger control are over-represented in adults and adolescents with ADHD (Ramirez et al., 1997). These studies suggest that individuals with ADHD may be more prone to aggressive driving, which may be a contributing factor to their increased driving risk.
A recent cross-sectional study compared self-reported driving anger in college students with high versus low ADHD symptoms (Richards et al., 2002). The high ADHD symptom group experienced significantly greater driving anger, reporting increased hostile verbal and physical aggression although, there were some discrepancies in findings between the measures employed. Higher mean scores for risky and aggressive behaviors while driving were found across the measures, although not all reached statistical significance. Another recent study found significantly higher prevalence of lifetime diagnosis of ADHD and a trend for increased prevalence of current diagnosis of ADHD in aggressive versus non-aggressive drivers (Malta et al., 2005). These two studies provide correlational evidence of a potential relationship between ADHD symptoms and driving anger and aggression. Sub clinical ADHD cases were included and the results may not be able to be generalized beyond the college students that were used as participants (Malta et al., 2005; Richards et al., 2002).
Methodological Issues in Observational Studies
1) Follow-up of Cohort
Selection bias can occur in prospective studies with subject attrition due to loss to follow-up. Response rates in the studies ranged from 41% to 93%, and results from studies with high loss to follow-up should be interpreted with caution. As well, effect sizes may be skewed based on the length of follow-up in each study. The periods of outcome assessment range from 1 to 3 years. Shorter follow-ups may limit observations during the period of risk and miss later cases thus, decreasing the magnitude of the effect of ADHD on outcome. None of the follow up studies determined ADHD status at follow-up & thus diluted the association of ADHD with negative driving outcome.
2) Survey Methods
Most observational studies employed surveys to assess driving risks and negative outcomes. Such results may be less accurate than objective outcomes. However, individuals with ADHD, as compared to controls, tend to overestimate their driving performance and therefore these results may, in fact, be underestimating the magnitude of difference between the groups (Knouse, Bagwell, Barkley, & Murphy, 2005).
3) Control for Potential Confounders, Covariates and Intervening Variables
Confounders are variables that may be responsible, in part, for the observed relationship between ADHD and driving risk or outcome. Numerous factors are known to be associated with driving risks and few are controlled in most of the reviewed studies. Almost all studies controlled for age and gender (Barkley et al. 1993; Barkley et al., 2002; Barkley et al., 1996; Fischer et al., in press; Lambert, 1995; Nada-Raja et al., 1997; Weiss et al., 1979; Woodward et al., 2000) except for a few studies that did not control for at least one of the variables (Fried et al., 2006; Richards et al., 2002). Various studies also controlled for socioeconomic status (Barkley et al., 1996; Barkley et al., 2002; Fried et al., 2006; Malta et al., 2005; Weiss et al., 1979; Woodward et al., 2000).
Driving experience, including both length of time driving and amount driven are speculated to confound the relationship between ADHD and driving. The study that best assessed these confounding factors found both these factors to be significant covariates (Woodward et al., 2000). While most studies controlled for at least one of the factors (Barkley et al. 1993; Barkley et al., 2002; Barkley et al., 1996; Fischer et al., in press; Lambert, 1995; Malta et al., 2005; Reimer et al., 2005; Richards et al., 2002), many did not (Fried et al., 2006; Murphy & Barkley, 1996; Nada-Raja et al., 1997; Weiss et al., 1979).
Medication used to treat ADHD is considered to be an intervening variable as it precedes driving outcome and may mitigate risk factors of inattention and impulsivity in the ADHD population. This variable was controlled in two (Barkley et al., 2002; Barkley et al., 1996) of the three (Barkley et al., 2002; Barkley et al., 1996; Fischer et al., in press) studies that included driving performance assessment where subjects were asked to stop taking medications before evaluation on a simulator. Failure to control for medication use is likely to skew results producing more conservative estimates of negative driving outcomes as medication use in ADHD groups likely decreases driving risk.
Finally, co morbidities including Oppositional Defiant Disorder (ODD) and Conduct Disorder (CD) may be important confounders to the ADHD-driving relationship. Males with conduct and antisocial symptoms are known to have increased negative driving outcome (Noyes, 1985; Tillman & Hobbes, 1949) and ADHD (Barkley et al., 1996; Murphy & Barkley, 1996). While various studies controlled for comorbid OCC/CD diagnosis or symptomology (Barkley et al. 1993; Barkley et al., 2002; Fried et al., 2006; Richards et al., 2002; Woodward et al., 2000) a few assessed extent of comorbidities in groups ( Murphy & Barkley, 1996; Nada-Raja et al., 1997) while others did neither (Barkley et al., 1996; Fischer et al., in press; Lambert, 1995; Malta et al., 2005; Reimer et al., 2005; Weiss et al., 1979) and this may have lead to skewed estimates of the true nature of the ADHD-driving relationship.
4) Sample Selection
The majority of observational studies employed consecutively referred patients for the ADHD group, and the non-ADHD groups included consecutive referrals without ADHD (Murphy & Barkley, 1996; Fried et al., 2006) or were recruited though advertisements or acquaintances of staff (Barkley et al. 1993; Barkley et al., 2002; Barkley et al., 1996; Fischer et al., in press; Weiss et al., 1979). Future studies would benefit from recruiting a less biased comparison group since volunteers tend to be healthier than non-volunteers (Sackett et al, 1979). Similarly clinic samples are less representative than random community samples of individuals with ADHD subjects and therefore it may not be appropriate to generalize the results from such studies to the population at large.
Experimental studies
This review includes studies that have explored psychopharmacological (Barkley, Anderson, & Kruesi, in press; Barkley, Murphy, O’Connell, & Connor, 2005; BjØrkli, FlØ, Jenssen, Ryum, & Zeiner, 2004; Cox, Humphrey, Merkel, Penberthy, & Kovatchev, 2004a; Cox, Merkel, Kovatchev, & Seward, 2000; Cox et al., in press-a; Cox, Merkel, Penberthy, Kovatchev, & Hankin, 2004) and alcohol effects (Barkley, Murphy, O’Connell, & Anderson, 2006) on driving in ADHD populations and summaries of these studies can be found in Table 2. A randomized double blind study is the gold standard as it minimizes both confounding and assessment biases. To date, four experimental studies have used this design to assess the effect of medications used to treat ADHD on driving risk (Barkley et al, in press; Barkley et al, 2005; BjØrkli et al., 2004; Cox et al, in press-a). The studies generally indicate positive medication effects on driving risks in ADHD populations.
Table 2.
Characteristics of Experimental Studies Included in the Review
| Study | Sample | Study design | Definition of risk factor | Outcome Assessed | Comments |
|---|---|---|---|---|---|
| (Cox et al., 2000) | 7 ADHD males referrals
6 non-ADHD males Recruited through ads Mean age = 22 (19–26) |
Cross over, counter-balanced design, double blind placebo controlled study | ADHD DSMIV diagnosis
Drug administration:
|
Driving Performance-driving simulator (O,S) |
|
| (Cox et al., 2004b) | 6 ADHD males
Recruited by high school nurse and newspaper ads Mean age = 17.2 (16–19) |
Randomized, crossover, single blind study | ADHD DSMIV diagnosis
Randomized drug administration:
|
Driving Behaviour
Daily diary - self reported risky driving practices Driving Performance -driving simulator (O,E) |
|
| (Cox et al., 2004a) | 12 ADHD males
Recruited by high school nurse and newspaper ads Mean age = 17.8 |
Randomized, cross over, single blind study | ADHD DSMIV diagnosis
Randomized drug administration:
|
Driving Performance -standard road course |
|
| (Barkley et al., 2005) | 53 ADHD 74% male consecutive referrals
Mean age = 37 (18–65) |
Randomized double blind, placebo controlled, within subject crossover design | ADHD DSMIV diagnosis
Randomized drug administration:
|
Driving Performance -driving simulator (O,E,S)
Cognitive abilities -Conner’s CPT |
|
| (Barkley et al., in press) | 18 adults with ADHD, 44% male
Recruited via newspaper ads and internal email solicitations Mean age = 37 (22–60) |
Randomized double blind placebo controlled within subject crossover design | ADHD DSMIV diagnosis
Randomized drug administration:
|
Driving Behaviour -self & other reports
Driving Performance -driving simulator (O,S,E) |
|
| (Barkley et al., 2006) | 50 ADHD
Mean age = 33 years Consecutive referrals 40 Non-ADHD Mean age = 29 years Recruited through advertisements |
Randomized, placebo controlled, single blind, factorial design | ADHD DSMIV diagnosis
|
Driving Performance -driving simulator performance (O,S,E)
Cognitive Abilities -CPT |
|
| (BjØrkli et al., 2004) | 17 ADHD, all males
Mean age = 28 (18–50) Recruited from ADHD society of Norway 29 Non-ADHD, all male Mean age = 31 (18–50) Employees and University students |
Randomized double blind placebo controlled crossover study | ADHD DSMIV diagnosis
Randomized Drug administration: ADHD
|
Driving performance -driving simulator (O) |
|
| (Cox et al., in press) | 35 ADHD 54% male
Mean age 1 = 7.8 (16–19) Referrals from physicians, nurses, teachers and volunteers from ads in newspaper/radio |
Randomized double blind placebo controlled crossover study | ADHD DSMIV diagnosis
Randomized drug administration:
|
Driving Performance -driving simulator (O,S,E) |
|
O – Objective measure of driving performance, S = Self rating of driving performance, E = Examiner rating of driving performance
Stimulant Medications (Methylphenidate and Dexamphetamine)
The established efficacy of stimulants in alleviating ADHD core symptoms of inattention, distractibility and impulsiveness has clear implication for improved driving skills. The first experimental study to evaluate the effects of Methylphenidate (MPH) on driving risk, Cox et al. (2000), was a double blind, placebo controlled study that found significant improvements in both self-report and simulator driving performance for the ADHD group receiving 10mg MPH compared to a placebo, but not for the non-ADHD group. However, sample size for this study was only 13 and the authors did not mention randomization.
Immediate release (IR) and sustained release methylphenidate (OROS MPH) have also been compared. Cox et al. (2004b) assessed simulator driving performance in 6 participants with ADHD after randomized administration of either four times daily IR-MPH or one OROS MPH once daily, both of which were maintained for seven days. There was a significant positive medication effect on the composite Impaired Driving Score (IDS). Drivers were assessed on the simulator at four points during the day. The IDS for the IR-MPH group worsened throughout the day, while the IDS for OROS MPH improved. The IDS was significantly worse for immediate release methylphenidate while driving at night (8 pm). Simulator measures of inappropriate braking missed stop signals, collisions and erratic speed control indicated significantly better performance on OROS MPH than on IR-MPH. This data provides evidence of sustained improvement for ADHD participants, on sustained as compared to IR–MPH. However, medication compliance was not assessed.
Results from a study comparing controlled released MPH and no drug on a standardized driving course found a significantly lower number of inattentive errors, as recorded by a blinded rater, for the ADHD subjects on OROS MPH condition. This argues for medication improving cognitive abilities associated with driving (Cox et al., 2004a). The three MPH studies indicate better driving performance on MPH, particularly sustained released MPH. However, the small, all male sample in all three studies may limit generalization of results. Furthermore the, results may be difficult to interpret, given the absence of placebo and non-ADHD control groups, in the latter two studies (Cox et al., 2004a; Cox et al. 2004b).
Two recent studies tested medication effects of MPH in older and larger samples and found fewer positive effects than the previous studies (Barkley et al., 2005; BjØrkli et al., 2004). A Norwegian study including 17 ADHD and 29 non-ADHD participants found very few medication effects on simulator driving performance and of the five driving scenarios assessed, only one showed that medication improved driving performance in that there was a trend for the ADHD group on MPH to have decreased lane swerving compared to placebo (BjØrkli et al., 2004). In this same driving scenario, the study’s most complex driving task, navigational abilities of the ADHD group on MPH as compared to placebo improved, though results did not reach statistical criteria. This suggests that the ADHD group may have more driving difficulties with complex tasks and a greater benefit to medication may be derived when engaged in demanding driving tasks. Of interest is the finding that younger individuals in the ADHD placebo group had poorer driving performance. They used the brakes more frequently and engaged in variable speeds more so than older participants.
Barkley et al., (2005) examined the impact of 10 and 20 mg of MPH and placebo on simulator driving performance of 53 participants with ADHD. Few significant differences were identified in this larger scale MPH study. However, compared to placebo, participants on high dose MPH had lower steering variability, and those on low dose MPH had higher numbers of turn signal indicators. Higher dose of MPH also resulted in a lower average speed than low dose MPH. ADHD behaviors related to driving were assessed using the Conners’ Scales. Levels of hyperactivity, but not inattention were found to be significantly lower among those on high dose MPH relative to the placebo condition.
A possible reason for the few significant results found in these two studies may be the older age of participants. In the two studies the mean age of the adults was 37 (Barkley et al., 2005) and 30 (BjØrkli et al., 2004) as compared with previous experimental studies where the mean ages were 22, 17.2, 17.8 (Cox et al., 2000; Cox et al. 2004a; Cox et al. 2004b), respectively. Reimer et al. (2005) observed that adults with ADHD may learn mechanisms to compensate for poor driving abilities and hence medication may not be seen as effective for improving driving performance in comparison to younger populations because of the relatively improved driving behavior seen with age. The sensitivity and specificity of different simulators may also have affected the results.
Only one study by Cox et al (in press-a) included a “head to head” placebo controlled comparison of two long-acting stimulant medications, methylphenidate (OROS MPH) and dexamphetamine (MAS XR), in their effect on driving performance in ADHD participants. A group of 35 adolescent drivers were compared on a driving simulator at 5,8 and 11pm, after taking 72 mg of long-acting OROS MPH, 30 mg of MAS XR, or placebo in a randomized, double-blind, placebo-controlled, crossover study design. Driving performance was also rated by subjects and investigators. The overall Impaired Driving Score demonstrated that OROS MPH led to better driving performance compared with both placebo and MAS XR, whereas MAS XR demonstrated no overall statistical improvement over placebo. Specifically, relative to placebo, OROS MPH resulted in less time driving off the road, fewer instances of speeding, less variable speed control and more time at a stop sign, whereas MAS XR resulted in only less inappropriate use of brakes. OROS MPH and MAS XR worked equally well for male and female participants, and equally well with teenagers who have combined and inattentive subtypes of ADHD. This study showed a robust effect of OROS MPH on simulator performance up to 15 hours after ingestion: an observation not previously reported. No equivalent long-term effects were seen for MAS XR. The authors note that the study may have been underpowered to detect an effect of dexamphetamine. This study used a fixed dose schedule based on previous research indicating optimum dose equivalents for symptom control of ADHD symptoms in classroom and home environments and that may limit the titration’s generalization to simulator or real driving environments. Individual titration of optimal dose for each medication might have found different optimal doses for the dexamphetamine. Importantly subjects rated both stimulants as equally efficacious. This argues for the primacy of objective measures of driving performance over subjective reporting in experimental design. These important findings merit replication in further independent studies. We did not find any other published study on the effects of Dexamphetamine on driving.
The only reported long-term study of the effects of stimulants is a twelve month observational study of a convenience sample of 100 ADHD adults (60 males and 40 females) (Jerome & Segal, 2001).These patients were consecutive attendees at a general psychiatric out patient clinic. The patients were treated with either methylphenidate or dexamphetamine. ADHD symptoms resolved in response to treatment along with a parallel improvement in driving profile obtained from self and collateral spousal report on the Jerome Driving Questionnaire, described later in this paper. Patients and their spouses noted that driving became less prone to speeding, with reduced distractibility to road conditions and less irritability with other road users. Standard medication doses used to manage target symptoms of ADHD appeared to “normalize” the patients driving profiles. Collateral ratings at baseline showed more impairment and greater improvement with treatment than did patients own self-report.
Non Stimulant Medication (Atomoxetine)
Atomoxetine, a non-stimulant treatment for adult ADHD holds theoretical promise for improving driving in ADHD populations particularly because of its relatively long duration of action compared to the stimulants, giving coverage during the later evening. One pilot study has assessed non-stimulant medication effects on driving in ADHD populations and some significant results were identified. Barkley et al. (in press) compared driving performance in 18 adult participants diagnosed with ADHD at baseline, on placebo and on atomoxetine (1.2 mg/kg daily for 2 weeks). Assessment measures include self and collateral reports of ADHD symptoms, functional impairment and safe driving behaviors. In addition, measures of performance on a virtual reality driving simulator, and self and examiner ratings of simulator performance were obtained. A double-blind, placebo controlled, within-subjects crossover design was used. Significant beneficial effects for atomoxetine relative to placebo were noted on self-ratings of ADHD symptoms, functional impairments of activities of daily living, self-ratings of safe driving behavior, and self-evaluations of overall simulator driving performance. The effects of atomoxetine on examiner ratings and simulator scores were not significant. A practice effect was noted on some of the simulator measures that may have “obscured” drug effects. The authors concluded that atomoxetine may have beneficial effects on ADHD symptoms and driving behavior that, if replicated, may offer one means of reducing the driving risks evident in teens and adults with ADHD. These results indicate subjective, but no objective benefit of atomoxetine on driving performance in ADHD participants. The mean age of the sample was high compared to younger ADHD populations that might show more objective impairments. Both the fixed dose schedule and the relatively short period of exposure may have limited optimum effects of the medication. In addition the relatively short exposure time to the simulator, which was done to avoid simulator sickness, may have limited findings.
Table 3 summarizes effect sizes of medications on simulator measures. A robust effect of methylphenidate on a range of measures of driving performance with long acting methylphenidate preparations working up to 15 hours after ingestion is demonstrated. Current data do not support similar positive objective findings for dexamphetamine or atomoxetine.
Alcohol Effects
A recently published study employed a factorial design to investigate potential differential effects of alcohol impairment on ADHD and non-ADHD groups in relation to driving (Barkley et al., 2006). Barkley et al. (1996; 2002) in previous studies reported significantly higher frequency of alcohol use and alcohol dependency in ADHD as compared to non-ADHD groups. Several observational studies found more self or proxy reports of drinking and driving in ADHD participants as compared to controls (Figure 4) (Barkley et al., 1993; Barkley et al., 1996; Fischer et al., in press; Nada-Raja et al., 1997; Woodward et al., 2000) though differences failed to reach statistical significance in some studies (Barkley et al., 1996; Fischer et al., in press; Woodward et al., 2000). As alcohol use is known to be a causal factor in negative driving outcomes, it is likely to contribute to the increased driving risks found in ADHD populations. Alcohol induced impairments are known to have similar deleterious effects to ADHD on executive function leading to reduced inhibition or impulsivity (Fillmore, 2003). Therefore, alcohol may magnify areas of alcohol-induced impairments in individuals with ADHD. Barkley et al. (2006) reported the effects of two levels of Blood Alcohol Concentration (BAC) (40 mg/dl and 80 mg/dl) on various cognitive and behavioral measures. Measures of inattention on the Conners CPT as well as self-reports of driving behavior and examiner ratings of simulator driving performance indicate a significantly greater detrimental effect of alcohol, irrespective of dose, for individuals with ADHD as compared to the non-ADHD group. No such results were found for the impulsivity measures on the CPT or any of the computer simulator scores. Alcohol appeared to mediate its effects in ADHD as compared to control samples through its negative impact on attention. It is possible that the BAC levels employed in this study may have been too low to impact the performance on the simulator. Collision risk increases drastically with increasing BAC (Zador, 1991) and at higher BAC levels, group differences in driving performance might have been detected on the simulator.
Methodological Issues in Experimental Studies
The sample sizes of the experimental studies range from six to 90 participants and therefore, power may limit the validity of results, particularly in the smallest studies. A limitation in comparing results in these experimental studies is that different simulators may have different levels of sensitivity and specificity. Ecological validity remains a problem; simulator study results cannot be generalized to real driving situations. Also, simulator sickness is a common problem sometimes limiting testing time to unrealistically short periods of observation. Sensitivity to practice effects may obscure real differences between groups. These criticisms apply to all studies that employed lab measures to assess driving risks (Barkley et al., in press; Barkley et al., 2002; Barkley et al., 1996; Barkley et al., 2006; Barkley et al., 2005; BjØrkli et al., 2004; Cox et al., 2000; Cox et al., in press-a; Cox et al., 2004b; Fischer et al., in press). The question of adherence to medication regimens was not routinely assessed or independently validated in some studies. A final issue is that all currently available studies are industry sponsored.
Conceptual Synthesis
Emerging data on adolescent brain development argue for the primacy of executive functional deficits in explaining proneness for risk taking behaviors and a range of physical accidents in young adults. Abundant empirical evidence shows that age-related brain changes are regional in nature (Sowell, Thompson, & Leonard, Welcome, & Tan, 2004). The frontal lobe, including the prefrontal cortex (PFC) is the seat of “Executive Functional Control”. The underlying processes of myelination, pruning of grey matter and synaptogenesis limit the rate of maturation of the PFC, both at the anatomical and molecular level, well into the second decade in normal adolescents (Blakemore & Choudhury, 2006).
Recent conceptual models of ADHD have characterized the condition as being mediated by deficits in executive function control (Barkley, 1997). Core functional impairments in executive function related to response inhibition, working memory and flexible strategic response help explain both general ADHD pathology and its specific manifestations in problem driving in this group.
Immature executive skill development including underdeveloped inhibitory control and decision making abilities can be thought of as lying along a continuum and may help to explain the increased risk taking and inaccurate risk perception apparent in high risk taking groups of adolescence and young adults. Whilst lack of driving experience may be a general factor leading to increased accident risk in young adults, the neurobiological basis for immature executive functioning present in young adults, in general and, in ADHD populations, in particular, who manifest ongoing immaturities in adaptive function is thought to be paramount. This maturational deficit of social and cognitive delay, typically observable from early childhood and continuing through the early adult years, would help explain the particularly acute driving vulnerability in young adults with ADHD (Stein, Szumowski, Blondis, & Roizen, 1995). As Barkley has noted (Barkley et al., 1996; 2002) it was not the knowledge base of driving skills that differentiated the driving problems in ADHD youth so much as their inability to apply these rules at the appropriate time and under the appropriate circumstances. In other words the problem is an output problem; they can “talk the talk but they can’t walk the walk.”
Screening for negative Driving Outcome
An effective screening tool would be one that could reliably predict negative driving outcomes in an ADHD population. Barkley et al. (1996) expressed a need for a more rigorous screening tool that would identify adaptive impairments and assess the true nature of driving risk. While survey instruments are limited by self-report and hence potential bias, they are the quickest and most efficient method of assessment. Questionnaires evaluating participants driving style and specific driving behaviors are the most practical approach for clinical settings. An awareness of overestimating of driving abilities in ADHD populations and use of collateral data in conjunction with self- reports could allow for better assessment of driving risk in ADHD populations using survey instruments. To date, few easy to use screening instruments have been employed to identify high risk drivers in ADHD populations. As discussed above, the DBRS (Barkley et al., 1993; Barkley et al., 2002; Barkley et al., 1996; Fischer et al, in press), the DBQ (Fried et al., 2006; Reimer, 2005; Woodward et al., 2000), and the Survey of Driving (Richards et al, 2002)] have been used in research studies and all measure driving behavior. The Jerome Driving Questionnaire (Jerome & Segal, 2005) is a screening tool in development showing preliminary promise. This 9 item, visual analog scale provides self-report and collateral data related to driving style. Preliminary results indicate that it has a four factor structure including attention, impulsivity, alertness and emotional lability. The JDQ appears to have predictive validity in assessing risk of future driving problems in young drivers in a 3 year prospective follow up of young drivers utilizing official driving records as an objective outcome measure. Self-reported measures of “Risk Taking” and “Day Dreaming” at baseline correlated with accidents and moving violations at 3 year follow-up in a normal novice driver sample. Interestingly, these JDQ dimensions load on the attention and impulsiveness factors of this novel instrument’s factor structure as well as correlate with independent measures of inattention and impulsivity on the Conners CPT. There is a need for such standardized screening tools for reliably evaluating current and future risk as this would likely encourage clinicians to routinely evaluate driving risk in their patients.
Conclusions
Research on the connection between ADHD and driving has made substantial progress over the past few decades. The thirteen observational studies reviewed in this paper provide evidence of a relationship between ADHD and negative driving outcomes, with an average Relative Risk of 1.54. This relationship is evident to a greater extent in driving violations and citations than in MVCs, but this is likely due to the rarity of reported collisions, which should be especially apparent in younger age groups with less driving experience (Kweo & Kockelman, 2003). The question of differential vulnerability in relation to subtypes of ADHD as well as relative impact of different symptom clusters remains to be addressed although the available data implicates attention difficulties being paramount.
Observational evidence for the mechanisms through which ADHD affects driving risks has been less extensive and conclusive. Our review of deficits in cognitive abilities found evidence for inattentiveness, particularly visual inattentiveness and impulsiveness correlating with problem driving outcome. Slow processing and distractibility and problems with visual memory are also associated with negative driving outcomes. Theoretically, impulsivity leads to excessive speed and problems disengaging from risky strategic maneuvers which when combined with attention problems lead to late counter measures that would likely transact to magnify risk. These factors would likely vary depending on driving experience and the cognitive demands of the prevailing road conditions and the in-car situation, e.g. cell phone use, the number of passengers, etc. Particularly risky environments may be ones of monotonous highways although convincing data about possible mechanisms and the relationship to changing road conditions is not yet available. Thus, evidence has been found that implicated cognitive deficits in operational control, or basic cognitive functioning as well as tactical control or the ability to maneuver the vehicle. Higher levels of strategic planning, which theoretically may be deficient in ADHD drivers have not yet been explored.
Experimental studies indicate that stimulants and to a lesser extent non-stimulant drugs used to treat ADHD improve areas of driving performance. Since young drivers are at increased risk driving later in the night when immediate release stimulants appear ineffective, the long acting medications have evident advantages. Methylphenidate may show some superiority in areas of response inhibition and visual memory in comparison to dexamphetamine (Wilson et al., in press). However, the relative superiority of long-acting methylphenidate over dexamphetamine is not in keeping with the clinical effects on ADHD symptom control of these two medications and needs to be demonstrated by further independent studies. The medications likely mediate their effect via improvement in executive functioning particularly on tasks of complex attention as well as response inhibition (Jerome & Segal, 2000). At the current time, the benefit of atomoxetine on subjective driver report lacks support from more objective simulator findings.
The field would be advanced by a longitudinal prospective study from academic centers comparing a representative sample of adult ADHD drivers, both male and female, with a broad age range and utilizing all available treatments both pharmacological as well as the psychological strategies which so far are not represented in the intervention literature. The role of motivational interviewing strategies that promote compliance and facilitate behavioral change is also worthy of exploration. In particular the question of adherence to medication regimens over time to improve driving skills is likely to be a critical question based on our knowledge of poor long-term medication adherence for young adults with ADHD. Such a naturalistic study would examine the effects of the common co morbidities and in particular the impact of Substance Use Disorder and Conduct Disorder in this vulnerable population
The individual attending physician has an opportunity to reduce morbidity and mortality for the individual ADHD patient as well as contribute to improved public health for the driving population at large by making the roads safer one driver at a time. Safety on the public highway is a public health issue. However, this public health issue may require a public health solution as suggested by the WHO with specific targets for vulnerable populations. Legislated interventions within the internal environment of the vehicle that regulate the use of cell phones and govern speed as well as provide appropriate cues to the distracted driver may prove to be a more effective intervention for improving road safety than individual treatment regimens given the emerging evidence of the lack of voluntary use of optional in-car speed governors in drivers prone to speeding (Jamson, 2006).
A number of jurisdictions including Canada and UK now require physicians to report ADHD drivers thought to be at risk of problem driving to the Ministry of Transportation. However, no standardized well validated tool currently exists to help guide clinicians in evaluating patient driving risk as well as response to treatment. The development of such a reliable metric would encourage clinicians to identify and manage their patients with problem driving more reliably. The question of medico-legal liability is in its infancy with no established case law for physicians found negligent of failing to adequately treat ADHD patients with the appropriate medications to reduce driving risk. Whilst the available literature does not yet provide clear evidence that stimulant medication should be the standard of care for problem drivers long term, it is probably only a matter of time before this question will be debated in a legal arena. Meanwhile it behooves the prudent physician to keep abreast of the emerging literature in this area and to provide clinical management targeted at improving the driving safety for patients.
Figure 3.
Meta Analysis on ADHD Status and Proportion of Self Reports of Having Driven Without a License
Footnotes
Reprinted with permission: Jerome, L., Segal, A. & Habinski, L., in press, Current Psychiatry Reports, Philadelphia, 2006
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, D.C.: Author; 1994. [Google Scholar]
- Arnett JJ, Offer D, Fine MA. Reckless driving in adolescence: ‘state’ and ‘trait’ factors. Accident Analysis and Prevention. 1997;29(1):57–63. doi: 10.1016/s0001-4575(97)87007-8. [DOI] [PubMed] [Google Scholar]
- Barkley RA. ADHD and the Nature of Self-Control. New York: Guilford Press; 1997. [Google Scholar]
- Barkley RA, Anderson DL, Kruesi M. A pilot study of Atomoxetine on driving performance in adults with Attention Deficit Hyperactivity Disorder (ADHD) Journal of Attention Disorders. doi: 10.1177/1087054706292122. in press. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Cox D. A Review of Driving Performance and Adverse Outcomes in Adolescents and Adults with Attention-Deficit/Hyperactivity Disorder. Journal of Safety Research in press. [Google Scholar]
- Barkley RA, Fischer M, Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria: I. An 8-year prospective follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29(4):546–57. doi: 10.1097/00004583-199007000-00007. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Guevremont DC, Anastopoulos AD, DuPaul GJ, Shelton TL. Driving-related risks and outcomes of attention deficit hyperactivity disorder in adolescents and young adults: a 3- to 5-year follow-up survey. Pediatrics. 1993;92(2):212–218. [PubMed] [Google Scholar]
- Barkley RA, Murphy KR, DuPaul GJ, Bush T. Driving in young adults with attention-deficit/hyperactivity disorder: knowledge, performance, adverse outcomes, and the role of executive functioning. Journal of the International Neuropsychological Society. 2002;8:655–672. doi: 10.1017/s1355617702801345. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Murphy KR, Kwasnik D. Motor vehicle driving competencies and risks in teens and young adults with attention deficit hyperactivity disorder. Pediatrics. 1996;98(6):1089–1095. [PubMed] [Google Scholar]
- Barkley RA, Murphy KR, O’Connell T, Anderson D. Effects of two doses of alcohol on simulator driving performance in adults with attention-deficit/hyperactivity disorder. Neuropsychology. 2006;20(1):77–87. doi: 10.1037/0894-4105.20.1.77. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Murphy KR, O’Connell T, Connor DF. Effects of two doses of methylphenidate on simulator driving performance in adults with attention deficit hyperactivity disorder. Journal of Safety Research. 2005;36:121–131. doi: 10.1016/j.jsr.2005.01.001. [DOI] [PubMed] [Google Scholar]
- BjØrkli C, FlØ M, Jenssen GD, Ryum T, Zeiner P. Assessment of fitness to drive among patients with learning difficulties. IMMORTAL. 2004 Deliverable R1.8. Retrieved on November 1, 2005 from http://www.immortal.or.at/index.php.
- Blakemore SJ, Choudhury S. Development of the adolescent brain: implications for executive function and social cognition. The Journal of Child Psychology and Psychiatry. 2006;47(3–4):296–312. doi: 10.1111/j.1469-7610.2006.01611.x. [DOI] [PubMed] [Google Scholar]
- Blows S, Ameratunga S, Ivers RQ, Lo SK, Norton R. Risky driving habits and motor vehicle driver injury. Accident Analysis and Prevention. 2005;37(4):619–624. doi: 10.1016/j.aap.2005.03.003. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioural Sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cox DJ, Humphrey JW, Merkel RL, Penberthy JK, Kovatchev B. Controlled-release methylphenidate improves attention during on-road driving by adolescents with attention-deficit/hyperactivity disorder. Journal of the American Board of Family Practice. 2004a;17(4):235–239. doi: 10.3122/jabfm.17.4.235. [DOI] [PubMed] [Google Scholar]
- Cox DJ, Merkel RL, Kovatchev B, Seward R. Effect of stimulant medication on driving performance of young adults with attention-deficit hyperactivity disorder: a preliminary double-blind placebo controlled trial. Journal of Nervous and Mental Disease. 2000;188(4):230–234. doi: 10.1097/00005053-200004000-00006. [DOI] [PubMed] [Google Scholar]
- Cox DJ, Merkel RL, Moore M, Thorndike F, Muller C, Kovatchev B. Relative benefits of stimulant therapy with OROS Methylphenidate versus mixed amphetamine salts extended-release in improving the driving performance of adolescent drivers with ADHD. Pediatrics. doi: 10.1542/peds.2005-2947. in press-a. [DOI] [PubMed] [Google Scholar]
- Cox DJ, Merkel RL, Penberthy JK, Kovatchev B, Hankin CS. Impact of methylphenidate delivery profiles on driving performance of adolescents with attention-deficit/hyperactivity disorder: a pilot study. Journal of the American Academy of Child and Adolescent Psychiatry. 2004b;43(3):269–275. doi: 10.1097/00004583-200403000-00007. [DOI] [PubMed] [Google Scholar]
- Cox DJ, Punja M, Powers K, Merkel RL, Burket R, Moore M. Manual transmission enhances attention and driving performance of ADHD adolescent males: Pilot study. Journal of Attention Disorders. doi: 10.1177/1087054706288103. in press-b. [DOI] [PubMed] [Google Scholar]
- Dahlen ER, Martin RC, Ragan K, Kuhlman MM. Driving anger, sensation-seeking, impulsiveness and boredom proneness in the prediction of unsafe driving. Accident Analysis and Prevention. 2005;37(2):341–348. doi: 10.1016/j.aap.2004.10.006. [DOI] [PubMed] [Google Scholar]
- Deffenbacher JL, Deffenbacher DM, Lynch RS, Richards TL. Anger, aggression and risky behaviour: a comparison of high and low anger drivers. Behaviour Research and Therapy. 2003;41(6):701–718. doi: 10.1016/s0005-7967(02)00046-3. [DOI] [PubMed] [Google Scholar]
- Deffenbacher JL, Huff ME, Lynch RS, Oetting ER, Salvatore NF. Characteristics and treatment of high anger drivers. Journal of Counseling Psychology. 2000;47(1):5–17. [Google Scholar]
- Fillmore MT. Drug abuse as a problem of impaired control: current approaches and findings. Behavioural and Cognitive Neuroscience Reviews. 2003;2(3):179–197. doi: 10.1177/1534582303257007. [DOI] [PubMed] [Google Scholar]
- Fischer M, Barkley RA, Smallish L, Fletcher K. Hyperactive children as young adults: driving abilities, safe driving behaviours and adverse driving outcomes. Accident Analysis and Prevention. doi: 10.1016/j.aap.2006.06.008. in press. [DOI] [PubMed] [Google Scholar]
- Fried R, Petty CR, Surman CB, Reimer B, Aleardi M, Martin JM, et al. Characterizing impaired driving in adults with attention-deficit/hyperactivity disorder: a controlled study. Journal of Clinical Psychiatry. 2006;67:567–574. doi: 10.4088/jcp.v67n0407. [DOI] [PubMed] [Google Scholar]
- Hasselberg M, Laflamme L. Socioeconomic background and road traffic injuries: a study of young car drivers in Sweden. Traffic Injury Prevention. 2003;4:249–254. doi: 10.1080/15389580309882. [DOI] [PubMed] [Google Scholar]
- Health Canada & Transport Canada. Road safety in Canada, an Overview. 2004 Mar; Retrieved April 1, 2006, from http://www.tc.gc.ca/roadsafety/stats/overview/2004/menu.htm.
- Jamson S. Would those who need it use it? Investigating the relationship between drivers speed choice and their use of a voluntary ISA system. Transportation Research Part F. 2006;9:195–206. [Google Scholar]
- Jerome L, Segal AU. ADHD, Executive Function and Problem Driving. The ADHD Report. 2000;8(2):7–11. [Google Scholar]
- Jerome L, Segal AU. Benefit of long term stimulants on driving in adults with ADHD. Journal of Nervous and Mental Disease. 2001;189(1):63–64. doi: 10.1097/00005053-200101000-00013. [DOI] [PubMed] [Google Scholar]
- Jerome L, Segal AU. Prediction of driving accident risk in novice drivers in Ontario: The development of a screening instrument. International Conference on Driver Behaviour and Training (2nd 2005 Edinburgh, Scotland); 2005. Driver behavior and training, Vol 2.-(Human factors in road and rail transport). Editor Lisa Dorn. 207–222. [Google Scholar]
- Jonah BA. Accident risk and risk taking behavior among young drivers. Accident Analysis and Prevention. 1986;18(4):255–271. doi: 10.1016/0001-4575(86)90041-2. [DOI] [PubMed] [Google Scholar]
- Jonah BA. Sensation seeking, risky driving and behavioural adaptation. Accident Analysis and Prevention. 2001;33:679–684. doi: 10.1016/s0001-4575(00)00085-3. [DOI] [PubMed] [Google Scholar]
- Knouse LE, Bagwell CL, Barkley BA, Murphy KR. Accuracy of self evaluation in adults with ADHD: evidence from a driving study. Journal of Attention Disorders. 2005;8(4):221–234. doi: 10.1177/1087054705280159. [DOI] [PubMed] [Google Scholar]
- Kweon YJ, Kockelman KM. Overall injury risk to different drivers: combining exposure, frequency and severity models. Accident Analysis and Prevention. 2003;35:441–450. doi: 10.1016/s0001-4575(02)00021-0. [DOI] [PubMed] [Google Scholar]
- Lagarde E, Chastang JF, Gueguen A, Coeuret-Pellicer M, Chiron M, Lafont S. Emotional stress and traffic accidents: the impact of separation and divorce. Epidemiology. 2004;15(6):762–766. doi: 10.1097/01.ede.0000142140.77194.ad. [DOI] [PubMed] [Google Scholar]
- Lambert NM. Analysis of Driving Histories of ADHD Subjects. Washington, DC: U.S. Department of Transportation; 1995. (Publication Number DOT HS 808 417) [Google Scholar]
- Malta LS, Blanchard EB, Freidenberg BM. Psychiatric and behavioral problems in aggressive drivers. Behavior Research and Therapy. 2005;43:1467–1484. doi: 10.1016/j.brat.2004.11.004. [DOI] [PubMed] [Google Scholar]
- McKnight AJ, McKnight AS. The effect of cellular phone use upon driver attention. Accident and Analysis Prevention. 1993;25:259–265. doi: 10.1016/0001-4575(93)90020-w. [DOI] [PubMed] [Google Scholar]
- McKnight AJ, McKnight AS. The behavioural contributors to highway crashes of youthful drivers. Annual Proceedings - Association for the Advancement of Automotive Medicine. 2000;44:321–33. [PMC free article] [PubMed] [Google Scholar]
- Murphy K, Barkley RA. Attention deficit hyper-activity disorder adults: comorbidities and adaptive impairments. Comprehensive Psychiatry. 1996;37(6):393–401. doi: 10.1016/s0010-440x(96)90022-x. [DOI] [PubMed] [Google Scholar]
- Murray A. The home and school background of young drivers involved in traffic accidents. Accident Analysis and Prevention. 1998;30(2):169–182. doi: 10.1016/s0001-4575(97)00088-2. [DOI] [PubMed] [Google Scholar]
- Nada-Raja S, Langley JD, McGee R, Williams SM, Begg DJ, Reeder AI. Inattentive and hyperactive behaviors and driving offenses in adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(4):515–522. doi: 10.1097/00004583-199704000-00014. [DOI] [PubMed] [Google Scholar]
- National Highway Traffic Safety Administration. Traffic Safety Facts. Washington, DC: U.S. Department of Transportation; 2004. (Publication number DOT HS 809 911) [Google Scholar]
- Noyes R. Motor vehicle accidents related to psychiatric impairment. Psychosomatics. 1985;26:569–580. doi: 10.1016/S0033-3182(85)72820-4. [DOI] [PubMed] [Google Scholar]
- Preusser DF, Williams AF, Ferguson SA, Ulmer RG, Weinstein HB. Fatal crash risk for older drivers at intersections. Accident Analysis and Prevention. 1998;30(2):151–159. doi: 10.1016/s0001-4575(97)00090-0. [DOI] [PubMed] [Google Scholar]
- Ramirez CA, Rosen LA, Deffenbacher JL, Hurst H, Nicoletta C, Rosencranz T, et al. Anger and anger expression in adults with high ADHD symptoms. Journal of Attentional Disorders. 1997;2:115–128. [Google Scholar]
- Reimer B, D’Ambrosio LA, Gilbert J, Coughlin JF, Biederman J, Surman C, et al. Behavior differences in drivers with attention deficit hyper-activity disorder: the driving behavior questionnaire. Accident Analysis and Prevention. 2005;37:996–1004. doi: 10.1016/j.aap.2005.05.002. [DOI] [PubMed] [Google Scholar]
- Richards TL, Deffenbacher JL, Rosen LA. Driving anger and other driving-related behaviors in high and low ADHD symptom college students. Journal of Attention Disorders. 2002;6(1):25–38. doi: 10.1177/108705470200600104. [DOI] [PubMed] [Google Scholar]
- Ryb GE, Dischinger PC, Kufera JA, Read KM. Risk perception and impulsivity: association with risky behaviours and substance abuse disorders. Accident Analysis and Prevention. 2006;38:567–573. doi: 10.1016/j.aap.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Sackett DL. Bias in analytic research. Journal of Chronic Diseases. 1979;32:51–63. doi: 10.1016/0021-9681(79)90012-2. [DOI] [PubMed] [Google Scholar]
- Schwartz N, Oyserman D. Asking questions about behaviour, cognition, communication and questionnaire construction. American Journal of Evaluation. 2001;22(2):127–160. [Google Scholar]
- Shope JT, Raghunathan TE, Patil SM. Examining trajectories of adolescent risk factors as predictors of subsequent high-risk driving behaviour. Journal of Adolescent Health. 2003;32:214–224. doi: 10.1016/s1054-139x(02)00424-x. [DOI] [PubMed] [Google Scholar]
- Shope JT, Waller PF, Raghunathan TE, Patil SM. Adolescent antecedents of high-risk driving behaviour into young adulthood: substance use and parental influences. Accident Analysis and Prevention. 2001;33:649–658. doi: 10.1016/s0001-4575(00)00079-8. [DOI] [PubMed] [Google Scholar]
- Sowell ER, Thompson PM, Leonard CM, Welcome SE, Tan E. Longitudinal mapping of cortical thickness and brain growth in normal children. Journal of Neuroscience. 2004;24(38):8223–8231. doi: 10.1523/JNEUROSCI.1798-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MA, Szumowski E, Blondis TA, Roizen NJ. Adaptive skills dysfunction in ADD and ADHD children. Journal of Child Psychology and Psychiatry. 1995;36:663–670. doi: 10.1111/j.1469-7610.1995.tb02320.x. [DOI] [PubMed] [Google Scholar]
- Thalheimer W, Cook S. How to Calculate Effect Sizes from Published Research Articles: A simplified methodology. 2002 Retrieved April 1, 2006, from http://work-learning.com/effect_sizes.htm.
- Tillman WA, Hobbs GE. The accident-prone automobile driver. The American Journal of Psychiatry. 1949;106:321–331. doi: 10.1176/ajp.106.5.321. [DOI] [PubMed] [Google Scholar]
- Treat JR, McDonald NS, Shinar D, Hume RD, Mayer RE, Stansifer RL, et al. Tri-Level Study of the Causes of Traffic Accidents, Vol. I: Causal Factor Tabulations and Assessment. Washington D.C.: U.S. Department of Transportation; 1977. (Publication Number DOT-HS-805-085) [Google Scholar]
- Truls V. Impairment, diseases, and their relative risks of accident involvement: results from meta-analysis. Impaired Motorists, Methods of Roadside Testing and Assessment for Licensing (IMMORTAL) 2003 Deliverable R1.1. Retrieved on November 1, 2005 from http://www.immortal.or.at/index.php.
- Tsuang MT. Psychiatric aspects of traffic accidents. The American Journal of Psychiatry. 1985;142(5):538–546. doi: 10.1176/ajp.142.5.538. [DOI] [PubMed] [Google Scholar]
- Turner D, McClure R. Age and gender differences in risk taking behaviours as an explanation for high incidence of motor vehicle crashes in young males. Injury Control and Safety Promotion. 2003;10(3):123–130. doi: 10.1076/icsp.10.3.123.14560. [DOI] [PubMed] [Google Scholar]
- United States General Accounting Office. Research Continues on a Variety of Factors That Contribute to Motor Vehicle Crashes. Washington D.C: United States General Accounting Office; 2003. [Google Scholar]
- Weiss G, Hechtman L, Perlman T, Hopkins J, Wener A. Hyperactives as young Adults: A controlled prospective ten-year follow-up of 75 children. Archives of General Psychiatry. 1979;36(6):675–681. doi: 10.1001/archpsyc.1979.01780060065007. [DOI] [PubMed] [Google Scholar]
- Whalen CK, Jamner LD, Henker B. The ADHD spectrum and everyday life: experience sampling of adolescent moods, activities, smoking and drinking. Child Development. 2002;73(1):209–227. doi: 10.1111/1467-8624.00401. [DOI] [PubMed] [Google Scholar]
- Williams AF, Shabanova VI. Responsibility of drivers, by age and gender, for motor-vehicle crash deaths. J Safety Res. 2003;34950:527–31. doi: 10.1016/j.jsr.2003.03.001. [DOI] [PubMed] [Google Scholar]
- Wilson KH, Cox DJ, Merkel RL, Moore M, Coghill D. Effect of extended release stimulant-based medications on neuropsychological functioning among adolescents with Attention Deficit Hyperactivity Disorder. Archives of Clinical Neuropsychology. doi: 10.1016/j.acn.2006.06.016. in press. [DOI] [PubMed] [Google Scholar]
- Woodward LJ, Fergusson DM, Horwood LJ. Driving outcomes of young people with attentional difficulties in adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39(5):627–634. doi: 10.1097/00004583-200005000-00017. [DOI] [PubMed] [Google Scholar]
- World Health Organization. The Injury Chartbook: A Graphical Overview of the Global Burden of Injuries. Geneva: WHO; 2002a. [Google Scholar]
- World Health Organization. Injury: A Leading Cause of the Global Burden of Disease, 2000. Geneva: WHO; 2002b. [Google Scholar]
- World Health Organization. World Report on Road Traffic Injury Prevention. Geneva: WHO; 2004. [Google Scholar]
- Yu J, Evans PC, Perfetti L. Road aggression among drinking drivers: Alcohol and non-alcohol effects on aggressive driving and road rage. Journal of Criminal Justice. 2004;32(5):421–430. [Google Scholar]
- Zador PL. Alcohol-related relative risk of fatal driver injuries in relation to driver age and sex. Journal of Studies on Alcohol. 1991;52(4):302–310. doi: 10.15288/jsa.1991.52.302. [DOI] [PubMed] [Google Scholar]
- Zeier H. Concurrent physiological activity of driver and passenger when driving with and without automatic transmission in heavy city traffic. Ergonomics. 1979;22(7):799–810. doi: 10.1080/00140137908924658. [DOI] [PubMed] [Google Scholar]
- Zhang J, Fraser S, Lindsay J, Clarke K, Mao Y. Age-specific patterns of factors related to fatal motor vehicle traffic crashes: focus on young and elderly drivers. Public Health. 1998;112:289–295. doi: 10.1038/sj.ph.1900485. [DOI] [PubMed] [Google Scholar]