Abstract
Introduction
The aim of this study is to address the complex psychopathologic factors involved in treatment refusal observed in adolescents suffering from a severe chronic illness.
Method
We report on five chronically ill adolescents (2 diabetes mellitus, 1 maple syrup urine disease, 1 bird fancier’s lung, 1 HIV infection) who were consecutively admitted to an inpatient psychiatric service as a result of a life-threatening refusal to comply with outpatient management of their medical illness. Case material is analyzed and discussed in the context of a review of the literature.
Results
Each subject was further characterized by: (1) the diagnosis of Borderline Personality Disorder; (2) severe family dysfunction (e.g. abuse, neglect and abandonment); and (3) frequent and prolonged pediatric hospitalizations. During their psychiatric hospitalization, the patients’ initial opposition to treatment shifted to mentalization and psychological questioning. From a psychodynamic perspective (attachment theory), we hypothesized that this behavior represented an attack on parental figures as embodied in the suicidal comportment.
Conclusion
Case material is presented to underline the possibility of co-occurring Borderline Personality Disorder when treating youths suffering from chronic illness and refusing treatment. Awareness of Borderline Personality Disorder may help pediatric staff when dealing with this refusal.
Keywords: treatment refusal, non-compliance, adolescents, chronic illness, borderline personality disorder
Résumé
Introduction
L’objectif de cette étude est de présenter les facteurs psychopathologiques complexes qui entrent dans le refus de traitement chez des adolescents souffrant de maladies chroniques graves.
Méthode
Nous présentons cinq adolescents atteints de maladies chroniques (deux souffrant de diabète sucré, un de la maladie du sirop d’érable, un de la maladie des éleveurs d’oiseaux et un du VIH) et hospitalisés en psychiatrie suite à leur refus de suivre les soins prescrits en clinique externe, refus qui peut entraîner la mort. Les données sont analysées et comparées à celles de la littérature.
Résultats
Chaque sujet est ensuite caractérisé par un diagnostic de personnalité limite, un sévère dysfonctionnement familial (abus, négligence et abandon) et de longues et fréquentes hospitalisations en pédiatrie. Pendant leur hospitalisation en service psychiatrique, l’opposition initiale des patients au traitement a changé en une mentalisation et un questionnement psychique. Adoptant une perspective psychodynamique (théorie de l’attachement), nous partons de l’hypothèse que ce comportement représente davantage une attaque de la figure parentale qu’un geste suicidaire.
Conclusion
Il convient d’envisager la possibilité d’un trouble de personnalité limite co-occurrent lorsque l’on soigne des adolescents qui souffrent de maladies chroniques et refusent le traitement. Traiter le trouble de personnalité limite peut aider le personnel pédiatrique à comprendre ce refus.
Keywords: refus de traitement, non-respect, adolescents, maladie chronique, trouble de personnalité limite
Introduction
Between 10 and 20 % of adolescents have a Chronic Illness (CI), achieving a severe intensity in ten percent of the cases (Wallander and Varni, 1998; Alvin et al, 1995). This frequency of CI is growing as medical research permits increasing longevity despite significant morbidity. Although intensive treatment may offer the chance of prolonged remission of a disorder, it also often implies prolonged hospitalization, temporary disfigurement, and a premature consideration of mortality. Consequently, such youths are, as a group, also vulnerable to anxiety disorders, avoidant strategies, ambivalence, poor self-esteem, depression as well as stresses associated with these secondary psychiatric disorders (Wallander and Varni, 1998; Alvin et al, 1995). Autonomy, cognitive and affective maturation, associated self-image changes, new relationships, coupling and the pursuit of career goals are core topics as youths approach adulthood. The stage of adolescence is usually undisrupted in chronically ill young people that must undergo treatment. However, CI may interfere with these developmental tasks (Wallander and Varni, 1998; Alvin et al, 1995).
Further, poor treatment compliance may be frequent (Alvin et al, 1995; Fitzgerald, 2001; Pucheu et al, 1999) and persistently non-compliant adolescents are generally impaired in a number of important social areas (Rianthavorn et al, 2004). Developmental tasks may be compromised if the youths, in pursuit of autonomy, rebel against the passive and dependent sick role by a compensatory need for control (Alvin et al, 1995; Pucheu et al, 1999; Traugott and Alpers, 1997), refusing to comply with treatment, and this refusal reciprocally sabotages normal psychosocial development and strains their relationships with caregivers.
Correlates of compliance in adolescents with severe CI
In what follows treatment compliance will be defined as a continuum from complete cooperation and compliance with treatment to treatment refusal. Treatment refusal will be defined as persistent and purposive non-compliance, which will include the refusal to behave in accordance with the rules and regulations established by an adult authority (Alvin et al, 1995; Fitzgerald, 2001). Non-compliance among adolescents with CI ranges from 10 to 40 %, while the rate of treatment refusal, although not specifically studied, is relatively rare (Alvin et al, 1995).
Non-compliance is associated with a number of factors among youths suffering with CI. Age is one such factor, such that youths younger than age eight may not yet have developed the cognitive maturity to understand the concept of death and thus feel no urgency to cooperate with treatment (Rianthavorn et al, 2004). Compliance of children is usually passive. By contrast, adolescents struggling to achieve separation and individuation may be particularly sensitive to the dependence implied by the sick role (Wallander and Varni, 1998), inadvertently sabotaging treatment as they strive for what they perceive to be autonomy. Non-compliance is further associated with a lack of social support, family dysfunction, poor parent-child communication and a strained relationship with the treating physician (Wallander and Varni, 1998; Bender et al, 1998; Bernstein et al, 2000; Hack and Chow, 2001). Additionally, just as CI is associated with a number of psychiatric disorders (e.g. depression and Post-Traumatic Stress Disorder), these same disorders can reciprocally drive non-compliance (Wallander and Varni, 1998; Alvin et al, 1995). In fact compliance improves upon resolution of such disorders (Rianthavorn et al, 2004).
Several of the factors that characterize non-compliance in CI also characterize Borderline Personality Disorder (BPD) (Wallander and Varni, 1998; Alvin et al, 1995; Pucheu et al, 1999), an association that has not yet been extensively explored. For example, patients suffering from BPD are characterized by poor social adjustment (e.g. greater emotionality, behavioral disorders, denial of illness and use of omnipotent defenses), a proneness to suicide attempts, a sensitivity to narcissistic injury and the use of primitive defenses (e.g. acting out and impulsivity). One could well imagine how such developmentally-compromised adolescents are also at high risk of sabotaging treatment compliance.
Authors have found in young adults a correlation between BPD and poor health-related lifestyle choices (Frankenburg and Zanarini, 2004), but BPD has not been specifically studied in non-compliant adolescents with CI and moreover in cases of treatment refusal. Parenthetically, the literature dealing with adults suffering from chronic medical conditions (e.g. pain, diabetes, organ transplantation) describes the problems of compliance with the nursing staff recommendations, the frequency of behavioral problems and the need to take precautions, when dealing with borderline personality disorder patients (Wasan et al, 2005; Pollock-Barziv and Davis, 2005; Huffman et al, 2003).
Wallander and Varni (1998) wrote that despite the biomedical uniqueness of each illness there is considerable commonality in the psychosocial ramifications of CI and that research would benefit from a “non-categorical approach”. These authors advocated that “more attention should be paid to intrapersonal correlates of adjustment, including the range of traditional personality traits”, and that “qualitative assessments should be enlightening”.
This article is a consideration of the BPD diagnosis as it presents among five patients consecutively admitted to an adolescent psychiatric inpatient service for having refused treatment of their severe medical CI.
Methods
The five patients reported on in this article were transferred from pediatric units at the request of pediatricians who failed to treat these adolescents. They were consecutively admitted to an inpatient closed unit within a Child and Adolescent General Psychiatry Department at a University Teaching General Hospital. The unit recruits adolescents presenting with severe or life-threatening psychiatric states (catatonic state, serious suicidal attempt…) and regionally-based. Hospital’s liaison physicians or previously treating specialized pediatricians - especially in case of rare and complex disease (case 3) - helped manage within the psychiatric unit the somatic illness of the five hospitalized patients.
All admissions were involuntary and at the parents’ request. According to the French Law none of the admissions required the adolescents’ consent. However, the adolescents gave their assent while being treated and all of them were individually followed after discharge in an OutPatient setting based on their place of residence and their desire to be seen.
For each case, we collected the main sociodemographic characteristics, the psychosocial background and the characteristics of the physical illness including number and length of hospitalizations in pediatric units. BPD was determined by retrospective chart review, using DSM-IV BPD symptoms, and in addition the Child version of the Retrospective Diagnostic Instrument for Borderlines (C-DIB-R) (Greenman et al, 1986). This specific and sensitive semi-structured instrument is widely used for reviewing charts with regards to borderline psychopathology, tapping cognitive and affective disturbances, impulsiveness and relationship impairments. A good interrater reliability was established for this instrument (_ = 0,72) (Guzder et al, 1996). GAF scales (Global Assessment Functioning) were scored upon admission and discharge.
The study of these patients was approved by an Ethics Committee and the identities of the patients have been significantly altered to protect the confidentiality.
Case series
Table 1 summarizes sociodemographic, clinical and psychosocial characteristics of the five patients. All patients were female aged 13 to 17 years. Physical illnesses included diabetes mellitus (n=2), bird Fancier’s lung, maple syrup urine disease and AIDS.
Table 1.
Demographic, clinical and psychosocial characteristics of 5 adolescents with life-threatening treatment refusal and borderline personality disorder
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | |
|---|---|---|---|---|---|
| Age | 17 | 13 | 17 | 16 | 17 |
| Gender | Female | Female | Female | Female | Female |
| Physical illness | |||||
| Name | Diabetes Mellitus | Bird Fancier’s lung | Maple Syrup Disease | Diabetes Mellitus | AIDS |
| Duration | 3 years | 3 years | 17 years | 4 years | 17 years |
| Current Treatment | Insulin, diet | Oxygen | Severe diet | Insulin, diet | Oral drugs |
| Hospitalizations (N) | 6 | 3 (last for 15 months) | >15 (total=3.5 years) | 12 | 7 |
| Psychosocial background | |||||
| Family history | Alcoholism | Fruit of rape | Alcoholism | ??? | HIV, addiction |
| Rupture in childhood | Parental divorce | Mother rejection | Provisional family | Provisional family | Mother death |
| Maltreatment | Sexual abuse | Violence | No | No | Neglect |
| DSM-IV BPD signs | |||||
| Unstable relationships | Severe | Moderate | Severe | Severe | Moderate |
| Impulsiveness | Severe | Severe | Severe | Severe | Severe |
| Affective instability | Severe | Moderate | Severe | Severe | Moderate |
| Inappropriate anger | Moderate | Severe | Severe | Severe | Severe |
| Suicidal threats | Severe | Moderate | Severe | Severe | Moderate |
| Identity disturbance | Severe | Severe | Moderate | Severe | Severe |
| Emptiness | No | Moderate | No | Severe | Moderate |
| Transient psychosis | Moderate | Severe | No | Severe | Severe |
| Abandonment | Severe | Severe | Severe | Severe | Moderate |
| Psychiatric variables | |||||
| GAF score at entry | 15 | 20 | 10 | 7 | 10 |
| GAF score at discharge | 55 | 70 | 75 | 45 | 68 |
| Child DIB-R score* | 7 | 8 | 8 | 8 | 7 |
AIDS: Auto-Immune Deficiency Syndrome; GAF: Global Assessment Functioning; BPD: Borderline Personality Disorder; DIB-R: Diagnostic Interview for Borderlines - Revised;
a score > 6 supports the diagnosis of Borderline Personality Disorder.
Case 1
From the time of diagnosis of type 1 diabetes at age 14 years till 17 years of age, Jade experienced three episodes of severe hypoglycemia and one of keto-acidosis (during a runaway from her home) due to insulin mismanagement. She signed herself out of the hospital against medical advice during her last medical hospitalization. The pediatric team, whom she experienced as extremely “rejecting”, requested a psychiatric hospitalization by court petition because of the mother’s failure to collaborate with outpatient psychiatric recommendations.
Family background
The parents divorced when Jade was 10-year-old. For several years subsequently the mother was described as unemployed, alcoholic, anxious, immature and passive. It was also noted that her stepfather was “violent” and involved in a sexual relationship with her and her younger sister. There were neither recorded psychiatric symptoms nor health-related disorders in Jade’s medical chart prior to adolescence.
Hospitalization
Jade was described as “manipulative” and “oppositional” upon admission. As she explored family stressors during successive interviews she gradually appeared less “dysphoric” and more authentic. We noted an improvement in her insulin management, a stronger alliance with the team and a return to school. However, during a two-day leave from the ward she and her mother decided she would not return. Her stepfather had left home during her stay in the hospital.
Follow-up
Jade was poorly cooperative with treatment at two years follow up. As a byproduct of the hospitalization our pediatric team better understood her behavior, facilitating their alliance with her.
Case 2
Ophelia, 11-year-old, was suffering from Bird Fancier’s Lung, and was admitted to the Intensive Care Unit for a two-month treatment of respiratory deficiency. Then needing oxygen nightly, she was transferred to a long-stay pediatric setting where she manifested multiple behavioral difficulties (e.g. thefts, running away and verbal and physical confrontations with the nurses who described her as “manipulative” with her peers). Anticipating transfer to a foster family, she refused her nightly oxygen treatment and was instead transferred to a psychiatric service for one month. The pediatric service expressed its wish not to have Ophelia back.
Family background
Several events in her history reflect the psychosocial stresses she endured. First, Ophelia was the product of a rape during her mother’s tenure as a prostitute. Second, Ophelia was the victim of her stepfather’s violence, for which reason she reported him to the authorities. Lastly, her mother preferred not to dispose of the birds rather than have her daughter back home.
Hospitalization
Upon admission Ophelia presented as a reticent but mature-appearing 13-year-old girl. In short order, she responsibly managed her illness and interacted with her peers, even if she sometimes hurled defiance at others. She appropriately expressed fear of residing with a foster family and developed mentalization of her difficulty leaving the medical ward. She was more collaborative with the treatment team upon return to the pediatric unit after the one month predicted period and an explanation on her worries of desertion.
Follow-up
At two years follow up Ophelia had a better alliance with the pediatric staff while awaiting placement with the foster family, although she still had mild anxious and behavioral symptoms.
Case 3
Sandy was a 17-year-old female suffering from Maple Syrup Urine Disease (MSUD), and was psychiatrically hospitalized for the treatment of severe behavioral disorders. Her presenting symptoms included an oscillation between over-eating and refusal to eat, both of which dangerously increased her Leucine and Isoleucine levels. The previous year, she had several comas. She had insomnia and was noted to steal, lie and skip school and to feel dysphoric and suicidal.
Family background
Sandy’s parents were Portuguese. Her oldest sister died 15 days postpartum from MSUD, and Sandy was placed in a foster family three months postpartum as her biological parents were unable to cope with her medical condition. She remained however in contact with them during placement. She had been hospitalized several times in a pediatric unit since her twelfth year for the treatment of intentional over-eating and behavioral problems (ie oppositionality and aggression) towards her foster parents.
Hospitalization
Sandy was not psychiatrically symptomatic during her hospitalization. She neither ate too dangerously little nor to excess. During hospitalization, she and her biological parents strove to advance her to Mahler’s developmental phase of separation individuation. After only one month of hospitalization and as a result of her emotional growth on the psychiatric ward Sandy was discharged home to her biological parents for the first time since she was three-month-old.
Follow-up
At nineteen year old Sandy was a professional student living with her parents. She had some minor behavioral symptoms but otherwise competently managed her complicated diet and treatment.
Case 4
Sally was diagnosed with type 1 diabetes at 12-year-old. She put her life at risk six times by either discontinuing her insulin or mismanaging her doses. She was oppositional in her relationships at home and school and in relation to the medical team, and was placed with a foster family after a suicide attempt and then admitted to a psychiatric unit.
Family background
For unspecified reasons she was intermittently placed in first foster care from two months of age to twelve years of age. Overall, Sally’s biography was uncertain. She did appear without landmarks in her personal history.
Hospitalization
Sally, 16-year-old upon admission, was uncooperative during her intake interviews. Although seeming to understand and appreciate the gravity of a diagnosis of type 1 diabetes, she refused to collaborate with the medical and dietary management. As she was often angry, oppositional and impulsive during psychiatric hospitalization, she was discharged. At her request during outpatient management, she was re-hospitalized and although more cooperative was again discharged because of poor frustration tolerance and further aggressive episodes.
Follow-up
Her physical and emotional status remained unchanged at three months follow up. Her pediatrician requested another psychiatric admission for treatment non-compliance, but this was delayed as the psychiatric staff felt that she was still not ready for psychological work.
Case 5
Nancy was an adolescent who was born with HIV during her mother’s pregnancy with her. Her mother died of AIDS when Nancy was 9-year-old, although Nancy was unaware of the cause of her mother’s death until ten years of age when she required anti-retroviral treatment. She was often ill with opportunistic diseases. During her last pediatric hospitalization she related poorly with physicians and nurses, demanding anti-retroviral treatment by gastric catheter rather than orally. Further, she attempted suicide while on the ward and required police involvement to resolve a physical altercation with another adolescent. She was referred to the inpatient psychiatric unit, as she was non-compliant with the anti-retroviral treatment upon discharge from the pediatric ward.
Family background
Nancy’s mother was a drug-addict who died from AIDS. Her father, who had a history of drug addiction, was alcoholic and being treated for HIV. Nancy, who was a talented student in High School, resided with her father and maternal aunt who was her legal guardian.
Hospitalization
Upon admission, Nancy, 17-year-old, was suffering from a brief mixed state with both irritability and dysphoric mood, that resolved within 3 days without psychotropic drugs. She expressed anger at both her family and the medical team. Nancy could soothe her in response to family counseling (during which time family aggression was addressed), residential treatment and an infectious disease consultation. She accordingly became more compliant with the anti-retroviral treatment, taking it first by gastric catheter in a sort of drug-addict way, then orally. By the time of discharge, Nancy was able to acknowledge her ambivalence about treatment.
Follow-up
Nancy reverted to poor compliance at follow up several months after discharge. However, she remained free of major behavioral difficulties, was compliant with psychotherapy and became aware of the risks of contracting a resistant viral strain due to her non-compliance.
Discussion
These cases of treatment refusal in chronically ill adolescents were characterized by a co-morbid psychiatric diagnosis of borderline personality disorder. They were all further characterized by abandonment or separation and early developmental stresses, poor psychosocial background, and in three of the cases (# cases 1, 2 and 5) by severe family dysfunction (including abuse, violence and/or neglect). Their medical evolutions were thus compatible with the early predictors of poor outcome among adolescents with CI, especially developmental struggles, family dysfunction and lack of psychosocial support which are also associated with borderline personality disorder. As well, the underlying biologic condition led to multiple and prolonged pediatric hospitalizations (Refer to Table 1: number and length of pediatric hospitalizations). Therefore, the length and number of hospitalizations observed in these five cases prior to the admission in a psychiatric unit support the idea that a more effective treatment was provided within a psychiatric versus a non-psychiatric inpatient setting. This idea is also supported from an ethical perspective, since they all had a life-threatening condition.
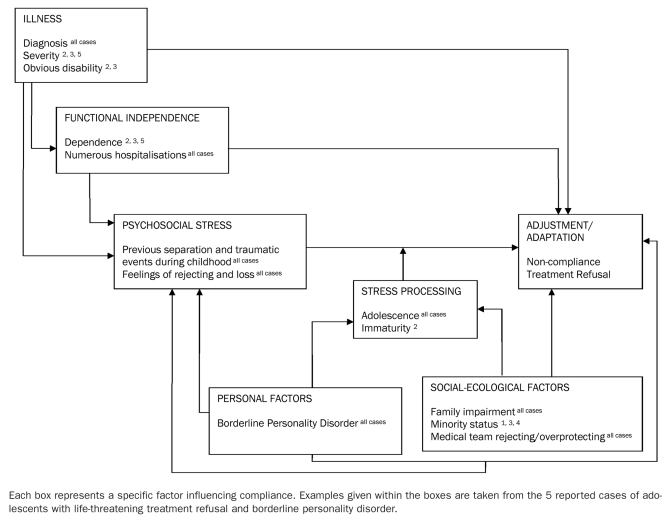
Wallander and Varni (1998) proposed a multifactorial model for individual and family maladjustment in cases of pediatric chronic illness. In Figure 1 we have integrated into that model the case examples of adolescents suffering from CI, life-threatening treatment refusal and BPD. All of the potentially involved factors interact with each other.
Figure 1.
Conceptual model of adolescent adjustment to pediatric chronic physical illness (adapted from Wallander and Varni, 1998)
Above all, the adolescent chronic illness in the context of family dysfunction exacerbates the underlying problematic of borderline personality disorder, culminating in treatment refusal (Figure 1).
As there is a dearth of literature concerning an exacerbation of borderline personality traits as a result of severe, life threatening illness, the question remains unclear as to whether these traits indeed represent co-morbid or pre-existing features. In other words, it is either the somatic illness that precipitate expression of BPD features or the pre-existing (although undocumented) symptomatic BPD features that are expressed through the patient’s reaction towards the illness and particularly its treatment. Either way, it seems to us that treatment refusal in an adolescent with CI could represent a BPD symptom equivalent. Therefore BPD is worth ruling out in presence of a treatment refusal in adolescents suffering from CI.
From a psychodynamic perspective (attachment theory), treatment refusal is probably multifactorial. Notwithstanding, in all but one case (case 4), this behavior could represent an attack on an internal parental representation (e.g. represented by pediatrician) in the form of suicidal ideation or an attempt without a wish to die. In terms of transference, a patient with BPD may actively enact in a repetition with a health professional (e.g. pediatrician or nurse) the abandonment from a caretaker that he or she experienced passively and early as a youth resulting in an insecure attachment (Bateman and Fonagy, 2003). Indeed, loss and rejection were common in the discourse of both the patients and the health care workers, and from this perspective the treatment refusal can be regarded as an acting out.
Fitzgerald (2001) recommends that health professionals be coached to depersonalize the patients’ negative feelings and destructive behaviors including the treatment refusal. Counter-transference manifestations of both the individual health care professionals (nurses, physicians, etc.) and the environments where these difficult patients are treated (e.g., wards, inpatient units, etc.) must be considered in the care of these challenging patients, for whom the system appears to fail. Such counter-transference manifestations, most commonly the feelings of frustration, are worth resolving during staff meetings with the help of an organizational theory, in order to defuse the staffs’ rejections of the patients, maximize the staffs’ self-reflections and minimize the potential for acting-out (Butterill et al, 1992). Physicians can, in turn, guide the adolescent to gain mastery over his/her dependency on the treatment team via strategies other than treatment refusal (Traugott and Alpers, 1997). Psychiatric hospitalization helped the adolescents gain capacity for mentalization of their conflicts and develop a nascent ability to introspect, culminating in a better alliance with the treating team and better compliance with the treatment recommendations. This is particularly manifest by cases 2 and 3.
However, the prognosis of these cases remains guarded, and depends in part on family’s collaboration with medical and psychiatric treatment and on the adolescent’s ability to reconcile with strongly negative affects. We consider that family no-cooperation with psychiatric care (cases 1, 5) or patient’s immaturity (case 4) may explain the cases 1, 4 and 5 poor outcomes. By contrast the collaboration of the patient’s parents described in case 3 was manifest by their accepting her home on discharge and encouraging her psychological growth. As well, in case 2, Ophelia’s evolving maturity and capacity for mentalization permitted recognition and resolution of her conflictual feelings towards the pediatric nurses and thus a good outcome.
Limitations
First, the methodology of this present consecutive case series is based on a retrospective chart review. Second, the target sample was restricted to psychiatric inpatients diagnosed with co-morbid BPD and may thus not be representative of all adolescents refusing treatment for chronic illness. Third, a new C-DIB-R was not conducted during patient’s follow-up to verify the stability of the BPD features over time.
Conclusion
Case material was presented underlining the possibility of co-occurring BPD in youths suffering from chronic illness and refusing their somatic treatment. Furthermore, we tend to consider that in certain occurrences treatment refusal of adolescents with CI might be better addressed in a closed adolescent psychiatry unit within a General Hospital, provided that pediatricians could liaise with the psychiatric staff and that it might facilitate the understanding and treatment of the complex underlying individual and family psychopathology. In all cases, co-morbid or pre-existing BPD should be rule out and addressed when necessary to help the patients and staff appreciate the patient’s feelings of loss and rejection.
References
- Alvin P, Rey C, Frappier JY. Therapeutic compliance in adolescents with chronic illness. Arch Pediatr. 1995;2(9):874–882. doi: 10.1016/0929-693x(96)81267-x. [Article in French] [DOI] [PubMed] [Google Scholar]
- Bateman AW, Fonagy P. The development of an attachment-based treatment program for borderline personality disorder. Bull Meninger Clin Summer. 2003;67(3):187–211. doi: 10.1521/bumc.67.3.187.23439. [DOI] [PubMed] [Google Scholar]
- Bender B, Milgrom H, Rand C, Ackerson L. Psychological factors associated with medication nonadherence in asthmatic children. J Asthma. 1998;35:347–353. doi: 10.3109/02770909809075667. [DOI] [PubMed] [Google Scholar]
- Bernstein GA, Anderson LK, Hektner JM, Realmuto G. Imipramine compliance in adolescents. J Am Acad Child Adolesc Psychiatry. 2000;39:284–291. doi: 10.1097/00004583-200003000-00009. [DOI] [PubMed] [Google Scholar]
- Butterill D, O’Hanlon J, Book H. When the System is the Problem, Don’t Blame the Patient: Problems Inherent in the Interdisciplinary Inpatient Team. Can J Psychiatry. 1992;37(3):168–172. doi: 10.1177/070674379203700304. [DOI] [PubMed] [Google Scholar]
- Fitzgerald D. Non-compliance in adolescents with chronic lung disease: causative factors and practical approach. Paediatr Respir Rev. 2001;2(3):260–267. doi: 10.1053/prrv.2001.0149. [DOI] [PubMed] [Google Scholar]
- Frankenburg FR, Zanarini MC. The association between borderline personality disorder and chronic medical illnesses, poor health-related lifestyle choices, and costly forms of health care utilization. J Clin Psychiatry. 2004;65(12):1660–1665. doi: 10.4088/jcp.v65n1211. [DOI] [PubMed] [Google Scholar]
- Greenman DA, Gunderson JG, Cane M, Saltzman PR. An examination of the borderline diagnosis in children. Am J Psychiatry. 1986;149:1723–1726. doi: 10.1176/ajp.143.8.998. [DOI] [PubMed] [Google Scholar]
- Guzder J, Paris J, Zelkowitz P, Marchessault K. Risk factors for borderline pathology in children. J Am Acad Child Adolesc Psychiatry. 1996;35(1):26–33. doi: 10.1097/00004583-199601000-00009. [DOI] [PubMed] [Google Scholar]
- Hack S, Chow B. Pediatric psychotropic medication compliance: a literature review and research-based suggestions for improving treatment compliance. J Child Adolesc Psychopharmacol. 2001;11:59–67. doi: 10.1089/104454601750143465. [DOI] [PubMed] [Google Scholar]
- Huffman JC, Popkin MK, Stern TA. Psychiatric considerations in the patient receiving organ transplantation: a clinical case conference. General Hospital Psychiatry. 2003;25(6):484–491. doi: 10.1016/s0163-8343(03)00090-2. [DOI] [PubMed] [Google Scholar]
- Pollock-BarZiv SM, Davis C. Personality factors and disordered eating in young women with type 1 diabetes mellitus. Psychosomatics. 2005;46(1):11–18. doi: 10.1176/appi.psy.46.1.11. [DOI] [PubMed] [Google Scholar]
- Pucheu S, Antonelli P, Consoli SM. Psychodynamic aspects of adolescents’ therapeutic compliance following a kidney transplant. In: Sugar M, editor. Trauma and Adolescence. Monograph Series of the International Society for Adolescent Psychiatry. 1. Madison, Connecticut: International Universities Press; 1999. pp. 125–141. [Google Scholar]
- Rianthavorn P, Ettenger RB, Malekzadeh M, Marik JL, Struber M. Noncompliance with immunosuppressive medications in pediatric and adolescent patients receiving solid-organ transplants. Transplantation. 2004;77(5):778–782. doi: 10.1097/01.tp.0000110410.11524.7b. [DOI] [PubMed] [Google Scholar]
- Traugott I, Alpers A. In their own hands: adolescents’ refusals of medical treatment. Arch Pediatr Adolesc Med. 1997;151(9):922–927. doi: 10.1001/archpedi.1997.02170460060010. [DOI] [PubMed] [Google Scholar]
- Wallander JL, Varni JW. Effects of pediatric chronic physical disorders on child and family adjustment. J Child Psychol Psychiat. 1998;39(1):29–46. [PubMed] [Google Scholar]
- Wasan AD, Wooton J, Jamison RN. Dealing with difficult patients in your pain practice [Review] Regional Anesthesia & Pain Medicine. 2005;30(2):184–192. doi: 10.1016/j.rapm.2004.11.005. [DOI] [PubMed] [Google Scholar]