Abstract
Introduction
Defining somatization in pediatric populations presents a unique challenge, because DSM-IV somatization criteria may be inadequate for identifying a child with somatization. Two approaches exist. Child somatization has frequently been rooted in a questionnaire model, focusing on child or parent responses to assess how well a child conforms to a specific mental health profile. Others use a medical diagnosis model, designating a child with somatization as those for whom a limited number of medical measures have failed to reveal a pathological source of symptoms.
Method
We incorporate concepts based upon a literature review from January 1994 to June 2005 of PubMed, PsycINFO, and CINAHL on classification and diagnosis of somatization in children ages 6 to 12. Our goal is to understand in depth the topic and suggest a way to better understand and classify somatization in children.
Results
We incorporate an integrative approach toward defining child somatization and propose an algorithm to step-by-step classify children with somatic symptoms into three distinct groups: sick, somatizers, and well. This approach includes information from self-report questionnaire, physician questionnaire, and the child’s medical chart.
Conclusion
This new algorithm suggests an approach for differentiating primary care pediatric clinic visitors into three distinct groups. Although used in clinical practice, empirical validation is necessary to further validate this algorithm.
Keywords: somatoform disorders, classification, pediatrics, child psychiatry, child psychology, algorithms, diagnostic techniques and procedures
Résumé
Introduction
Il est particulièrement difficile de définir la somatisation chez les patients pédiatriques parce que les critères de somatisation définis dans le DSM-IV ne permettent pas toujours de reconnaître la somatisation chez les enfants. Deux approches coexistent. Dans la première approche, la somatisation fait l’objet d’un questionnaire, les réponses de l’enfant ou du parent servant à évaluer dans quelle mesure l’enfant entre dans un profil spécifique. La deuxième approche fait appel à un diagnostic médical, qui définit un enfant qui somatise comme un enfant chez lequel un certain nombre d’interventions médicales n’ont pas réussi à mettre à jour la source pathologique des symptômes.
Méthode
Nous utilisons des concepts basés sur une analyse des revues PubMed, PsycINFO et CINAHL publiées entre juin 1994 et juin 2005 qui traitent du classement et des diagnostics de somatisation chez les enfants âgés de 6 à 12 ans. Notre objectif est d’approfondir, de définir et de catégoriser la somatisation chez les enfants.
Résultats
Nous utilisons une approche intégrale pour définir la somatisation chez l’enfant et proposons un algorithme permettant de classer méthodiquement les enfants qui présentent des symptômes somatiques dans trois groupes distincts: enfants malades, enfants qui somatisent et enfants bien portants. Cette approche prend en compte les informations recueillies au moyen du questionnaire autoadministré, du questionnaire du médecin, ainsi que les données figurant au dossier médical de l’enfant.
Conclusion
Ce nouvel algorithme propose une approche qui classe dans trois groupes distincts les enfants qui fréquentent les cliniques pédiatriques. Bien que cet algorithme soit utilisé en pratique clinique, il doit être validé empiriquement.
Keywords: troubles somatoformes, classement, pédiatrie, psychiatrie de l’enfant, psychologie de l’enfant, algorithme, techniques et méthodes diagnostiques
Introduction
Somatization refers to a pattern of behavior in which individuals repeatedly seek medical help for disabling physical symptoms that they mistakenly attribute to physical disease (Campo & Fritsch, 1994). Among children, there is mounting evidence that somatization is both widespread and severe, warranting the attention and focus of both clinicians and researchers (Garralda, 1992). Pediatric physicians regularly encounter somatic symptoms which are not recognizably associated with any medical illness (Campo & Fritsch, 1994; Garralda, 1992). Somatization when broadly defined is found in as many as 20% of children aged 7–12 years attending primary care clinics, and as many as 47% of those referred to specialists at pediatric clinics (Garralda, 1992). In general population samples, 15.2% of school-aged children have multiple recurrent somatic symptoms (Garber, Walker, & Zeman, 1991), and as many as 4.5% of boys and 10.7% of girls aged 12–16 years meet criteria for a somatization syndrome (Offord, Boyle, Szatmari et al., 1987).
Despite evidence of somatization prevalence, identification of a child with somatization is complicated by methodological difficulties (Fritz, Fritsch, & Hagino, 1997; Campo, Jansen-McWilliams, & Comer et al., 1999; Walker, Garber, & Greene, 1991). Many acknowledge the need to synthesize information from multiple sources, both medical and psychosocial, in order to identify a child with somatization (Campo & Fritz, 2001; Shapiro & Rosenfeld, 1987; Silber & Pao, 2003). Also, pediatric somatization shares a number of limitations with the concept of adult somatization. Advances in knowledge of biological processes that underlie certain specific symptom patterns once thought to have strictly "non-organic" origins (e.g. chronic fatigue syndrome, fibromyalgia) often question the traditional somatization/physical illness dichotomy (Bell, Patarca, & Baldwin et al., 1998). Some even advocate a complete abolition of somatoform disorders, as the traditional concept of somatization assumes an exclusively psychogenetic etiology for symptoms, which is often an unacceptable etiology from a patient’s perspective (Sharpe & Mayou, 2004).
With or without a formal diagnostic category for somatization, both clinicians and researchers are likely to maintain an ongoing interest in the symptoms and behaviors of children who experience disruptive and recurrent physical distress with no identifiable physical basis. The availability of a comprehensive and accurate operational definition of this childhood experience is critical. In this manuscript, we review the relevant literature to determine the approaches used to classify somatization in children. Based upon our review, we outline the mental health and medical definitions of somatization in children. Guided by the framework for somatoform disorders as defined by the Diagnostic and Statistical Manual of Mental Disorders – 4th edition (DSM-IV; American Psychiatric Association (APA), 1994), we suggest an approach to classify children with somatic symptoms into three distinct groups of sick, somatizers, and well. Also, we provide an algorithm to step-by-step demonstrate this approach.
Review Conceptualization
We searched the databases of PubMed, PsycINFO, and CINAHL using the terms "somatization" and "classification." We also conducted an additional search using the terms of "somatization" and "diagnosis" with these three databases. In this additional search we restricted the search only to review articles on this topic. We read the relevant articles and included other relevant articles that were highlighted from reading the above retrieved articles. All the above searches were limited to children ages 6 to 12 years. These searches included articles published from January 1994 to June 2005. Articles were typically included if they focused on general somatization classification or diagnostic issues among children.
Somatization Overview
In general, there are a number of information sources used in assessing childhood somatization. Often child self-report or parent-report questionnaires assign children with somatic symptoms to a particular mental health profile (e.g., Campo et al., 1999; Lehmkuhl, Doepfner, & Plueck, 1998; Rocha, Prkachin, & Beaumont, 2003; Walker, Garber, & Greene, 1994). Besides questionnaires, physician medical diagnoses and/or patient medical chart reviews are used to identify children exhibiting a history of medically unexplained somatic complaints (e.g., Boey & Gohb, 2001; Pipe, 1999; Smith, Korban, & Kanj et al. 2004; Walker, Garber, & Greene, 1993; White, Alday, & Spirito, 2001). Both approaches have contributed to a growing understanding of the prevalence (Ruo, Rumsfeld, & Hlatky et al., 2003), predictors (Lehmkuhl et al., 1998; Rocha et al., 2003), treatment (Silber & Pao, 2003), and related risks (Campo et al., 1999) of child somatization, yet much remains to be learned. We review and then integrate both approaches and propose a theoretical alternative for clinicians and researchers to systematically identify a group of children who experience disabling somatic complaints, but whose physical health status differentiates them from children with symptoms more easily explained by medical illness.
Somatization Definitions Drawn From A Mental Health Profile
The DSM-IV (APA, 1994) provides detailed criteria for identifying adults with somatic disorders, rooted in profiles of the behaviors and symptoms that characterize somatization. These include the disorders of Somatization Disorder and Undifferentiated Somatoform Disorder. Somatization Disorder is defined as "a pattern of recurring, multiple, clinically significant somatic complaints" for which no medical explanation can be found to adequately account for the subject’s experience. A minimum number of complaints from several organ systems must be present. Undifferentiated Somatoform Disorder is defined as one or more physical complaints, persisting for a minimum of 6 months, that cannot be explained medically or better accounted for by another mental disorder. While the construct validity of these diagnostic classifications has long been considered speculative even for adult populations (Smith et al., 2004), there is little speculation over the inadequacy of DSM-IV criteria for defining somatization in childhood. Despite the relative abundance of children with somatization symptoms, it is rare for children to have symptom clusters that meet explicit DSM-IV diagnostic criteria (Walker et al., 1993). Fritz, Fritsch, and Hagino (1997) argue that the DSM-IV somatization criteria are tailored to an aggregate of symptoms experienced by adults, a shortcoming which probably accounts for the scarcity of child somatizers diagnosable under these criteria. For example, DSM-IV criteria for Somatization Disorder require the demonstration of at least one sexual disturbance (APA, 1994), a requisite clearly unsuitable for classifying pre-pubertal patients. This suggests that a clinical interview based solely on DSM-IV criteria may not diagnose somatization disorders in children.
Self-report scales are often used to understand somatization in children. Measures such as the Children’s Somatization Inventory (CSI; Walker & Garber, 1992) adapt DSM-IV criteria so that they are more appropriate for assessing children. A growing body of research supports the reliability and construct validity of the CSI (Garber et al., 1991; Litcher, Bromet, Carlson et al., 2001; Meesters, Muris, & Ghys et al., 2003; Walker et al., 1991; Walker et al., 1993). This includes high correlations between CSI scores and various independent measures of child somatization, such as the somatization scale of the Child Behavior Checklist (CBCL; Achenbach, 1991), as well as measures of psychological traits that have been linked with somatization in adult populations, such as anxiety (measured by the State-Trait Anxiety Inventory for Children; (Spielberger, 1973), and depression (measured by the Children’s Depression Inventory; (Kovacs, 1981).
One shortcoming of the CSI is that it relies solely on child self-report to assess symptom occurrence. When assessing adults, it is assumed that individuals are capable of reporting reliably on the history and severity of their symptoms. There is evidence that child self-reports cannot be relied upon to the same degree as by adults (Kovacs, 1986; Labbe, Williamson, & Southard, 1985; van den Brink, Bandell-Hoekstra, & Abu-Saad, 2001). This has led many to view a parental interview as an important source of information about child health and adjustment status (Canning, 1994). The Child Behavior Checklist (CBCL; Achenbach, 1991), a parent-report measure widely considered to be the gold standard of self-report child behavioral assessment, includes a somatization subscale that can be used to identify children with a pattern of somatization symptoms. However, using parental information introduces the potential interference of parental bias into the quantification of child symptoms. Although there are modest correlations between the child (CSI) and the separate parent version of the CSI (P-CSI; Litcher et al., 2001; Meesters et al., 2003; Garber, Van Slyke, & Walker, 1998), as well as the CSI and other parent-provided measures such as the CBCL (Litcher et al., 2001; Meesters et al., 2003), many argue that there is poor concordance between parent and child reports of children’s subjective symptoms (Taylor, Szatmari, & Boyle, 1996; Walker et al., 1993). Given these uncertainties, it is unclear whether either child or parent reports can stand alone as an untainted and reliable source of information on child illness behavior.
Even if one assumes a reasonably high degree of reliability in child- and/or parent-reported information, the CSI, CBCL, and other questionnaire-based measures are limited by their reliance on subjective sources of information to distinguish somatizing children from non-somatizing children. Objective information and not just self-report subjective information would be useful in distinguishing psychiatric somatization disorders from medical illness. An essential component of the concept of somatization is the absence of a known medical condition to account for the somatizers’ symptoms. Objective medical evidence such as lab tests and/or expert input from those with experience in diagnosing medical illness would further enhance an operational definition of somatization in children. The CSI and other self-report scales provide a useful measure of the level of impairment suffered as a result of somatic symptoms, but do not distinguish patients on the basis of medical evidence. Specifically, patients whose reported symptoms can be attributed to medical illness are not systematically differentiated from those whose symptoms are unexplained from a medical perspective.
An ideal operational definition of somatization would ensure that both medical and mental health characteristics are taken into account. This would help to ensure that children with identifiable medical illness, as well as non-somatizing, healthy children, are excluded from the group defined as somatizers. There is a demonstrated need for a new instrument, one that balances child- and/or parent-provided information with more objective, medical measures of child health status.
Somatization Definitions Drawn From a Medical Profile
Physicians with experience in diagnosing medical illnesses may be the best individuals to objectively assess a child’s physical health. A typical diagnosis-driven strategy has been to focus on individuals diagnosed with a particular illness such as recurrent abdominal pain (RAP; Walker et al., 1993; Fritz et al., 1997), chronic fatigue syndrome (Pipe, 1999), or pediatric headache (White et al., 2001). These illnesses apply to all cases where symptoms recur consistently and present a significant barrier to functioning. For example, RAP is defined as three or more episodes of abdominal pain over a period of at least three months, all severe enough to interfere with a child’s functioning (Fritz et al., 1997). Diagnosing in this way is traditionally a categorization by exclusion, based on the failure of an unfixed number of medical measures to explain a patient’s experience. This model is clearly limited in its applicability to the more general task of defining child somatization. To extend this paradigm to the broader task of defining children with somatic symptoms at large would be empirically imprecise. Rather than evaluating what characteristics are present in children with somatic symptoms, this type of definition would rely primarily on the absence of a known medical cause for symptoms, in order to distinguish somatizers from non-somatizers.
With the introduction of concrete diagnostic criteria for certain disorders frequently associated with somatization, notably the Rome and Rome-II criteria for functional gastrointestinal disorders (FGIDs; Thompson, Longstreth, & Drossman et al., 1999), medicine achieved an alternative to diagnosis by exclusion. However, these classifications for "functional" disorders (as distinguished from disorders with an identifiable structural basis) remain controversial, due to considerable overlap between the various FGIDs, as well as between these and other functional disorders including chronic fatigue syndrome, fibromyalgia, and chronic pelvic pain (Guthrie & Thompson, 2002). Furthermore, classifications based upon the Rome-II criteria and similar diagnostic systems differ from the DSM-IV classification of somatization in a number of important ways. Where the DSM-IV specifies that there should be no known physical cause that accounts for the severity of symptoms, these functional disorder criteria exclude etiology entirely, and encompass certain "stress-related" disorders such as Irritable Bowel Syndrome that are typically considered distinct from the somatoform disorders of the DSM. These classifications also do not distinguish patients with clinically relevant degrees of impairment from those whose behavioral functioning is relatively intact, nor do they detect somatizers whose symptom patterns may be subsyndromal or atypical, but nevertheless severely debilitating (Liebrand, Cuntz, & Hiller, 2002). Thus, for clinicians and researchers seeking to systematically identify children who closely resemble the DSM-IV’s characterization of somatization, classification by functional disorder may not be the best approach.
An Optimal Somatization Definition for Children
A distinct, operational definition is necessary if one is to build a more precise and generalizable understanding of the factors involved in child somatization. Such a definition would ideally involve the presence of certain medical and psychological characteristics, rather than the absence of a limited number of medical diagnoses. Additionally, an optimal definition would not be limited to any single, potentially limited source of information, but would balance valuable subjective information from reliable parent and child questionnaires and interviews with objective medical measures of physical health.
An Approach for Defining Somatization in Children
There is a need for an operational definition of somatization, one that is integrative and directly addresses the difficulties inherent in defining a child population of somatizers. A comprehensive approach is to synthesize information obtained directly from patients and their proxies (through child- or parent-report measures and interviews), along with objective medical information obtained from physicians and the child’s medical records. We propose an algorithm for categorizing children visiting a medical clinic into three distinct groups: Medically Ill, Somatizers, and Well. Defining somatization in this way can allow for reliable and consistent categorization into a well-defined somatizer group.
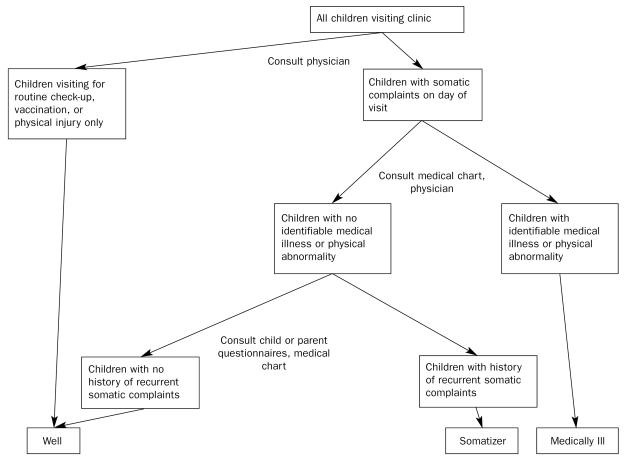
Although we recommend synthesizing information from several distinct sources, our underlying logic is consistent with the DSM-IV definition of somatization disorder, which states that "the essential feature of somatization disorder is a pattern of recurring, multiple, clinically significant somatic complaints…The multiple somatic complaints cannot be fully explained by any known general medical condition (APA, 1994)." In our approach, a child is classified as a somatizer if he/she demonstrates behaviors indicative of recurrent somatic symptoms, but where there is little evidence of serious physician concern for the child’s physical health. Figure 1 is a flowchart demonstrating the straightforward and simple logic by which this basic definition can be upheld while integrating information from each of the various sources.
Figure 1.
Flowchart outlining an integrative methodological approach to classifying children as medically ill, somatizers, or well.
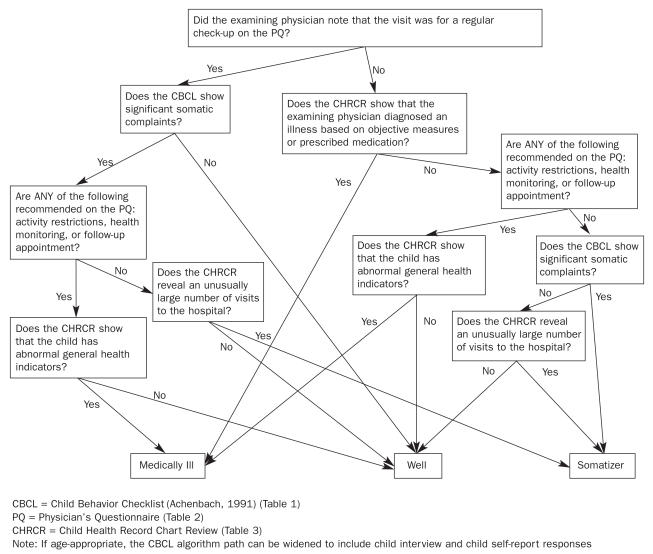
The algorithm we detail in Figure 2 illustrates this integrative approach in concrete terms, drawing on one previously existing measure for assessing child somatization based on parent report (the somatization sub-scale of the CBCL; Achenbach, 1991), as well as one original measure for assessing physicians’ medical opinions, and a compilation of information drawn from the child’s medical chart. The CBCL is suggested as the source of self-report information because its reliability and validity as a behavioral assessment tool are virtually undisputed; however, any child- or parent-report measure of somatization that is empirically well-validated (the CSI or P-CSI, for example) could easily be substituted or added alongside the CBCL without disturbing the algorithm’s structure. Many may prefer to include both child and parent information, especially when the child is old enough to understand the physician’s questions and/or complete a self-report questionnaire. As it stands, this algorithm has been successfully used to operationally categorize pediatric patients in a large urban public hospital. It is an example of the way in which our general integrative approach can be implemented in order to obtain a balanced and specific definition of child somatization.
Figure 2.
Flowchart detailing an algorithm for classifying children as medically ill, somatizers, or well.
An Algorithm Measures for Categorizing Medically Ill, Somatizing, and Well Children
Besides any relevant clinical interviews, these three forms are used to categorize children:
The somatization subscale of the Child Behavior Checklist (CBCL; Achenbach, 1991) (Table 1) (and if developmentally appropriate, a child interview and self-report questionnaire such as the CSI; Walker & Garber, 1992)
The Physician’s Questionnaire (PQ) (Table 2)
Chart review of the child’s health record (Table 3)
Table 1.
Somatization Subscale of the Child Behavior Checklist (CBCL)
| 0 = Not True (as far as you know) | |||
|---|---|---|---|
| 1 = Somewhat or Sometimes True | |||
| 2 = Very True or Often True | |||
| 0 | 1 | 2 | 1. Feels dizzy |
| 0 | 1 | 2 | 2. Overtired |
| 3. Physical problems without known medical cause: | |||
| 0 | 1 | 2 | a. Aches or pains (not stomach or headaches) |
| 0 | 1 | 2 | b. Headaches |
| 0 | 1 | 2 | c. Nausea, feels sick |
| 0 | 1 | 2 | d. Problems with eyes (not if corrected by glasses)
(describe): ____________________ |
| 0 | 1 | 2 | e. Rashes or other skin problems |
| 0 | 1 | 2 | f. Stomach aches or cramps |
| 0 | 1 | 2 | g. Vomiting, throwing up |
Reproduced by permission from Achenbach, T. M. (1991). Manual for the Child Behavior Checklist /4–18 and 1991 Profile. Burlington, Vt: University of Vermont Department of Psychiatry.
Table 2.
The Physician’s Questionnaire (PQ)
| Child Somatization: Primary Care Physician’s Form | |
| Child’s Name | |
| Chart # | |
| 1. Was this visit solely for a regular checkup? | |
| Yes □ | |
| No □ | |
| 2. Do you think this child should be kept away from school or other daily activities? | |
| Major restrictions | No restrictions |
| 1- - - - - - - - -2- - - - - - - - -3- - - - - - - - -4- - - - - - - - -5- - - - - - - - -6- - - - - - - - -7 | |
| 3. Do you think this child’s health should be monitored closely in the immediate future? | |
| Extremely closely | Not exceptionally closely |
| 1- - - - - - - - -2- - - - - - - - -3- - - - - - - - -4- - - - - - - - -5- - - - - - - - -6- - - - - - - - -7 | |
| 4. Do you recommend a follow-up visit? | |
| Highly recommended | Not needed |
| 1- - - - - - - - -2- - - - - - - - -3- - - - - - - - -4- - - - - - - - -5- - - - - - - - -6- - - - - - - - -7 | |
Table 3.
Child Health Record Chart Review
| 1. Diagnosis: Does the chart describe the identification of an illness based on objective medical measures (e.g. positive lab test results)? | |
| Yes □ | No □ |
| 2. Medication: Does the physician prescribe medication? | |
| Yes □ | No □ |
| 3. General health indicators: Do the child’s height, weight, and blood pressure measurements place them below the 5th or above the 95th percentile for their age group? | |
| Yes □ | No □ |
| 4. Frequency of service utilization: How many clinic visits has the child made over the course of the past year? __________ | |
| 5. Number of school absences:a How many days has the child been absent from school over the past year? __________ | |
Not all medical records may contain this information, and the algorithm can work without it.
The Child Behavior Checklist
The Child Behavior Checklist (CBCL; Achenbach, 1991) is used to examine parental perceptions of the child’s behavior. The part of the scale used in this algorithm assesses the child’s behavior along a single dimension: somatic problems (see Table 1). For each of the 9 items, mothers are asked to rate the degree to which a particular behavior resembles their child’s current behavior (0= not true; 1= somewhat or sometimes true; 2= very true or often true). This instrument is the self-report gold standard for child behavioral assessment, has adequate reliability and validity, and correlates well with other measures of child maladjustment (Achenbach, 1991). The CBCL manual provides a normative scale for conversion of raw score on these 9 items to percentile rank. We consider a score in the borderline clinical or clinical range (95th percentile or above on the normative scale) to be indicative of significant somatic complaints that pose a substantial disruption in the child’s functioning.
The Physician’s Questionnaire
The Physician’s Questionnaire (PQ) (Table 2) is completed by the child’s primary care physician (e.g., pediatrician) at the time of the clinic visit. This measure is designed to help differentiate between illnesses and the possibility of somatization. It elicits the physician’s recommendations for activity restrictions, health monitoring, and a follow-up visit as a means of quantifying the level of concern for the child’s physical health. The PQ consists of four items; one yes/no question that assesses the reason for the clinic visit and three Likert-style scale questions about health recommendations. For scoring the algorithm, a score of 1 or 2 on any of the three Likert-style scale questions is considered a positive response. In our clinical experience, we have found pediatricians to be very cooperative in completing these 4 brief items.
The Child Health Record Chart Review
The Child Health Record Chart Review (CHRCR) (Table 3) is a protocol used to obtain objective data on the child’s health history. The following four aspects of the medical chart are referred to in the process of categorizing the child:
Diagnosis: Except for children coming for a check-up and/or immunization, almost every child visiting a primary care physician is given a medical illness diagnosis. The presence of such a diagnosis does not necessarily indicate that a child is very sick. It is often standard medical procedure to diagnose for administrative and billing purposes. Thus, diagnoses in themselves are inadequate for categorizing child patients. The results of a lab test, imaging scan, or other objective measure of physical health can place a child definitively in the medically ill category, if the pathological source of the malady is found. If the medical chart shows clearly that an illness has been diagnosed on the basis of objective medical findings, this is considered a definitive indication that the child is physically ill. Diagnoses recorded with no reference made to any objective measurements of physical health are considered less definitive. For the purposes of this algorithm, injuries are not considered to be illnesses and allergies are considered to be illnesses only if they have an asthmatic element to them. Any visit made for a follow-up on an initial diagnosis is considered to be a visit for an illness.
Medication: The nature of a prescription can be a valuable indicator of how sick a primary care physician thinks a child might be. Some treatments recommended by the physician, however, such as saline drops, are considered non-medications, and are generally prescribed primarily for the mother’s comfort.
General Health Indicators: A child’s blood pressure, height, and weight percentiles in comparison to his/her appropriate age group can be indicative of illness. Children that are below the 5th and above the 95th percentile on these general health indicators are more likely to have medical problems and are considered to have abnormal health indicators for the somatization algorithm.
Frequency of Service Utilization: Children with an abnormally high number of clinic visits in the year preceding the interview date are more likely to belong in either the medically ill or somatizer categories. Frequent medical services utilization is often an indicator of a somatization disorder (Spielberger, 1973) and indicates that the child’s somatic complaints have significantly impeded his or her functioning, to the point that repeated clinic visits are warranted. For the purposes of the algorithm, an abnormally high number of visits could be determined by a frequency distribution of the particular primary care clinic.
Number of School Absences: Some medical records may contain information regarding school absences. If this information is present, this can help support the approach that the child is more likely to belong in either the medically ill or somatizer categories. As not all medical records contain this information, we have not directly included it in the formal algorithm.
The Somatization Algorithm: A Step-by-step Approach
The somatization status of the child is determined by a combination of the three sources of information detailed above. Figure 2 presents a step-by-step algorithm by which children are categorized into a particular health status group—Medically Ill, Somatizers, or Well.
A child is classified as a somatizer if he/she demonstrates behaviors indicative of recurrent somatic symptoms, but where there is little evidence of serious concern for the child’s physical health. The use of the PQ and the child’s health record allow for a deeper understanding of the child’s physical health, while the CBCL provides a subjective account of the child’s somatic complaints. The algorithm presented provides a systematic means of differentiating child somatizers from children who are likely to be physically ill ("Medically Ill" children), and from healthy children visiting the clinic for a check-up, immunization, or physical injury ("Well" children).
More data is needed to determine the reliability and validity of this algorithm. Our approach is only a step towards addressing the complex issues necessary to assess and diagnose a child with somatization.
Conclusions
The algorithm shown in Figure 2 and described above suggests an operational definition of childhood somatization. This algorithm suggests a new construct of child somatization that is easily quantifiable, and based upon information drawn from a wide variety of independent sources (parent’s interview and self-report, child interview and self-report (if applicable), physician’s notes in the medical chart, independent physician’s questionnaire, and several child medical measures). The process of determining the presence of somatization is also "user-friendly," involving uncomplicated judgment and scoring. This algorithm can be useful to both those early on in their clinical training, as well as those with many years of clinical practice. Implementing this algorithm can 1) aid in the identification of children whose suffering may not be adequately acknowledged by their primary care physicians whom may now refer these children for appropriate mental health treatment, 2) allow pediatricians to save on costs and patient burden by reducing unnecessary testing, and 3) enable researchers to classify children into appropriate categories.
References
- Achenbach TM. Manual for the Child Behavior Checklist /4–18 and 1991 Profile. Burlington, VT: University of Vermont; 1991. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Bell RI, Patarca R, Baldwin CM, Klimas NG, Schwartz GE, Hardin EE. Serum neopterin and somatization in women with chemical intolerance, depressives, and normals. Neuropsychobiology. 1998;38:13–18. doi: 10.1159/000026511. [DOI] [PubMed] [Google Scholar]
- Boey CC, Goh KL. The significance of life-events as contributing factors in childhood recurrent abdominal pain in an urban community in Malaysia. Journal of Psychosomatic Research. 2001;51:559–562. doi: 10.1016/s0022-3999(01)00232-x. [DOI] [PubMed] [Google Scholar]
- Campo JV, Fritsch SL. Somatization in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:1223–1235. doi: 10.1097/00004583-199411000-00003. [DOI] [PubMed] [Google Scholar]
- Campo JV, Fritz G. A management model for pediatric somatization. Psychosomatics. 2001;42:467–476. doi: 10.1176/appi.psy.42.6.467. [DOI] [PubMed] [Google Scholar]
- Campo JV, Jansen-McWilliams L, Comer DM, Kelleher KJ. Somatization in pediatric primary care: Association with psychopathology, functional impairment, and use of services. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:1093–1101. doi: 10.1097/00004583-199909000-00012. [DOI] [PubMed] [Google Scholar]
- Canning EH. Mental disorders in chronically ill children: Case identification and parent-child discrepancy. Psychosomatic Medicine. 1994;56:104–108. doi: 10.1097/00006842-199403000-00005. [DOI] [PubMed] [Google Scholar]
- Fritz GK, Fritsch S, Hagino O. Somatoform disorders in children and adolescents: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1329–1338. doi: 10.1097/00004583-199710000-00014. [DOI] [PubMed] [Google Scholar]
- Garralda ME. A selective review of child psychiatric syndromes with a somatic presentation. British Journal of Psychiatry. 1992;161:759–773. doi: 10.1192/bjp.161.6.759. [DOI] [PubMed] [Google Scholar]
- Garber J, Van Slyke DA, Walker LS. Concordance between mothers’ and children’s reports of somatic and emotional symptoms in patients with recurrent abdominal pain or emotional disorders. Journal of Abnormal Child Psychology. 1998;26:381–391. doi: 10.1023/a:1021955907190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J, Walker LS, Zeman J. Somatization symptoms in a community sample of children and adolescents: Further validation of the Children’s Somatization Inventory. Psychological Assessment. 1991;3:588–595. [Google Scholar]
- Guthrie E, Thompson D. ABC of psychological medicine: Abdominal pain and functional gastrointestinal disorders. BMJ. 2002;325:702–703. [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. Rating scales to assess depression in school-aged children. Acta Paedopsychiatrica. 1981;46:305–315. [PubMed] [Google Scholar]
- Kovacs M. A developmental perspective on methods and measures in the assessment of depressive disorders: The clinical interview. In: Rutter M, Izard CE, Read PB, editors. Depression in young people: Developmental and clinical perspectives. Vol. 1. New York, NY: Guilford; 1986. pp. 435–465. Chapter 15. [Google Scholar]
- Labbé EE, Williamson DA, Southard DR. Reliability and validity of children’s reports of migraine headache symptoms. Journal of Psychopathology and Behavioral Assessment. 1985;7:375–383. [Google Scholar]
- Lehmkuhl G, Doepfner M, Plueck J, Berner W, Fegert JM, Huss M, Lenz K, Schmeck K, Lehmkuhl U, Poustka F. Prevalence of behavioral problems and somatic complaints of children aged four to ten as rated by their parents. Zeitschrift für Kinder-und Jugendpsychiatrie und Psychotherapie. 1998;26:83–96. [PubMed] [Google Scholar]
- Liebrand R, Cuntz U, Hiller W. Assessment of functional gastrointestinal disorders using the Gastro-Questionnaire. International Journal of Behavioral Medicine. 2002;9:155–173. doi: 10.1207/s15327558ijbm0902_06. [DOI] [PubMed] [Google Scholar]
- Litcher L, Bromet E, Carlson G, Gilbert T, Panina N, Golovakha E, Goldgaber D, Gluzman S, Garber J. Ukrainian application of the Children’s Somatization Inventory: Psychometric properties and associations with internalizing symptoms. Journal of Abnormal Child Psychology. 2001;29:165–175. doi: 10.1023/a:1005240214564. [DOI] [PubMed] [Google Scholar]
- Mayou R, Levenson J, Sharpe M. Somatoform disorders in DSM-V. Psychosomatics. 2003;44:449–451. doi: 10.1176/appi.psy.44.6.449. [DOI] [PubMed] [Google Scholar]
- Meesters C, Muris P, Ghys A, Reumerman T, Rooijmans M. The Children’s Somatization Inventory: Further evidence for its reliability and validity in a pediatric and a community sample of Dutch children and adolescents. Journal of Pediatric Psychology. 2003;28:413–422. doi: 10.1093/jpepsy/jsg031. [DOI] [PubMed] [Google Scholar]
- Offord DR, Boyle MH, Szatmari P, Rae-Grant NI, Links PS, Cadman DT, Byles JA, Crawford JW, Blum HM, Byrne C. Ontario Child Health Study: II. Six-month prevalence of disorder and rates of service utilization Archives of General Psychiatry. 1987;44:832–836. doi: 10.1001/archpsyc.1987.01800210084013. [DOI] [PubMed] [Google Scholar]
- Pipe R. A review of family factors in chronic fatigue syndrome. In: Garralda E, editor. Occasional Paper OP16. Vol. 16. New York, NY: Association for Child Psychology and Psychiatry; 1999. pp. 9–12. Chapter 2. [Google Scholar]
- Rocha EM, Prkachin KM, Beaumont SL, Hardy CL, Zumbo BD. Pain reactivity and somatization in kindergarten-age children. Journal of Pediatric Psychology. 2003;28:47–57. doi: 10.1093/jpepsy/28.1.47. [DOI] [PubMed] [Google Scholar]
- Ruo B, Rumsfeld JS, Hlatky MA, Liu H, Browner WS, Whooley MA. Depressive symptoms and health-related quality of life: The Heart and Soul Study. JAMA. 2003;290:215–224. doi: 10.1001/jama.290.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro EG, Rosenfeld AA. The somatizing child: Diagnosis and treatment of conversion and somatization disorders. New York, NY: Springer; 1987. [Google Scholar]
- Sharpe M, Mayou R. Somatoform disorders: A help or hindrance to good patient care? British Journal of Psychiatry. 2004;184:465–467. doi: 10.1192/bjp.184.6.465. [DOI] [PubMed] [Google Scholar]
- Silber TJ, Pao M. Somatization disorders in children and adolescents. Pediatrics in Review. 2003;24:255–264. doi: 10.1542/pir.24-8-255. [DOI] [PubMed] [Google Scholar]
- Smith RC, Korban E, Kanj M, Haddad R, Lyles JS, Lein C, Gardiner JC, Hodges A, Dwamena FC, Coffey J, Collins C. A method for rating charts to identify and classify patients with medically unexplained symptoms. Psychotherapy and Psychosomatics. 2004;73:36–42. doi: 10.1159/000074438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD. Manual for the State-Trait Anxiety Inventory for Children. Palo Alto, CA: Consulting Psychologists Press; 1973. [Google Scholar]
- Taylor DC, Szatmari P, Boyle MH, Offord DR. Somatization and the vocabulary of everyday bodily experiences and concerns: A community study of adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:491–499. doi: 10.1097/00004583-199604000-00015. [DOI] [PubMed] [Google Scholar]
- Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Muller-Lissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999;45(Supplement II):1143–1147. doi: 10.1136/gut.45.2008.ii43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Brink M, Bandell-Hoekstra EN, Abu-Saad HH. The occurrence of recall bias in pediatric headache: A comparison of questionnaire and diary data. Headache. 2001;41:11–20. doi: 10.1046/j.1526-4610.2001.111006011.x. [DOI] [PubMed] [Google Scholar]
- Walker LS, Garber J. Children’s Somatization Inventory: Preliminary manual. Nashville, TN: Vanderbilt University; 1992. [Google Scholar]
- Walker LS, Garber J, Greene JW. Somatization symptoms in pediatric abdominal pain patients: Relation to chronicity of abdominal pain and parent somatization. Journal of Abnormal Child Psychology. 1991;19:379–392. doi: 10.1007/BF00919084. [DOI] [PubMed] [Google Scholar]
- Walker LS, Garber J, Greene JW. Psychosocial correlates of recurrent childhood pain: A comparison of pediatric patients with recurrent abdominal pain, organic illness, and psychiatric disorders. Journal of Abnormal Psychology. 1993;102:248–258. doi: 10.1037//0021-843x.102.2.248. [DOI] [PubMed] [Google Scholar]
- Walker LS, Garber J, Greene JW. Somatic complaints in pediatric patients: A prospective study of the role of negative life events, child social and academic competence, and parental somatic symptoms. Journal of Consulting and Clinical Psychology. 1994;62:1213–1221. doi: 10.1037//0022-006x.62.6.1213. [DOI] [PubMed] [Google Scholar]
- White KS, Alday CS, Spirito A. Characteristics of children presenting to a behavioral treatment program for pediatric headache. Journal of Clinical Psychology in Medical Settings. 2001;8:109–117. [Google Scholar]