Abstract
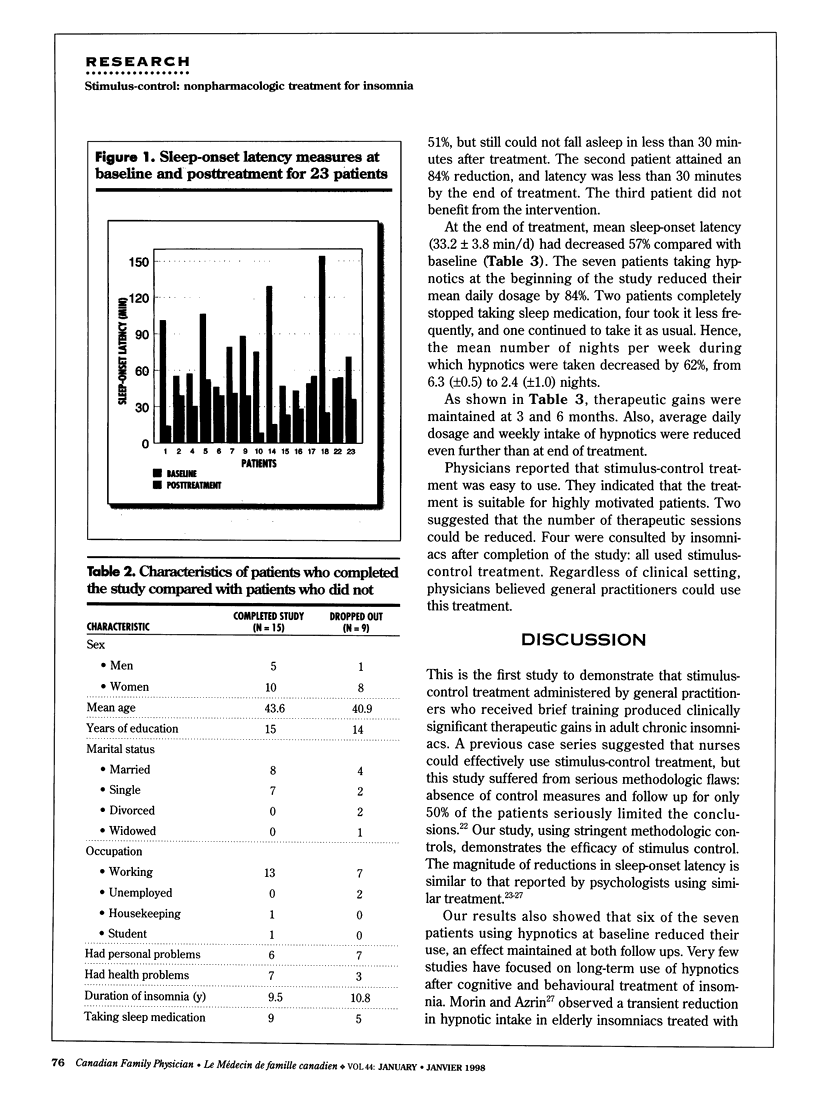
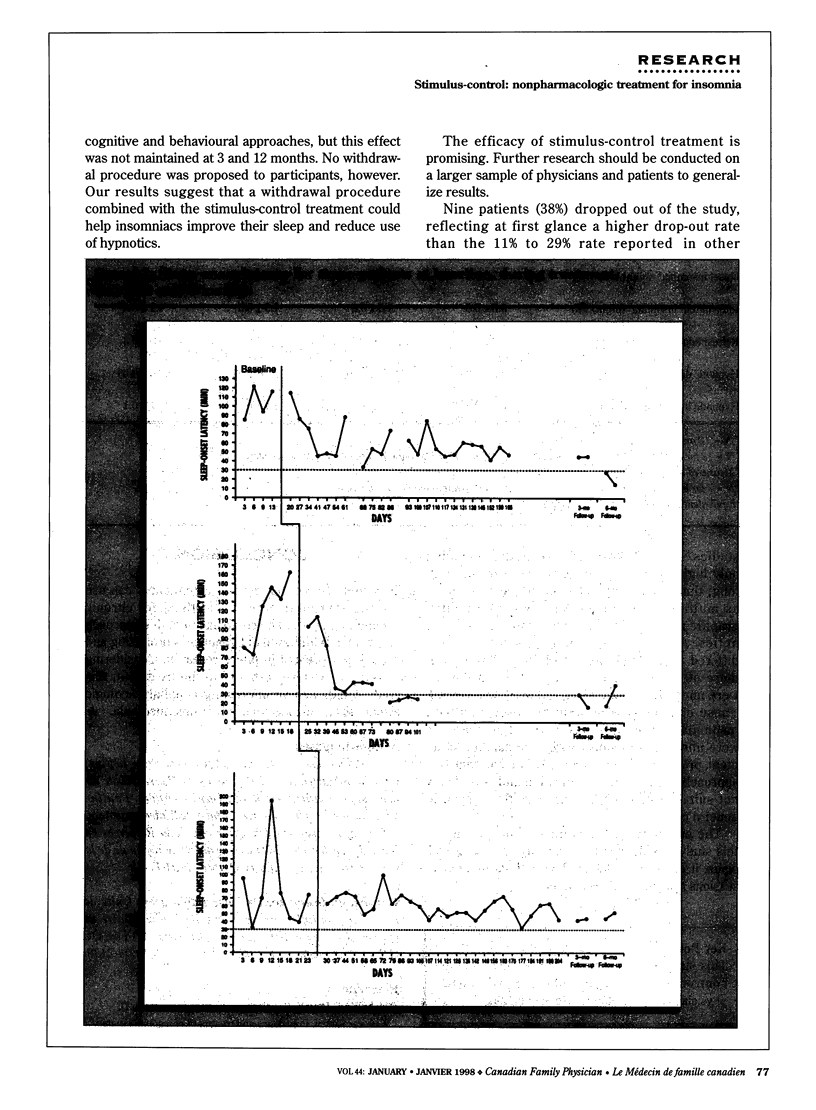
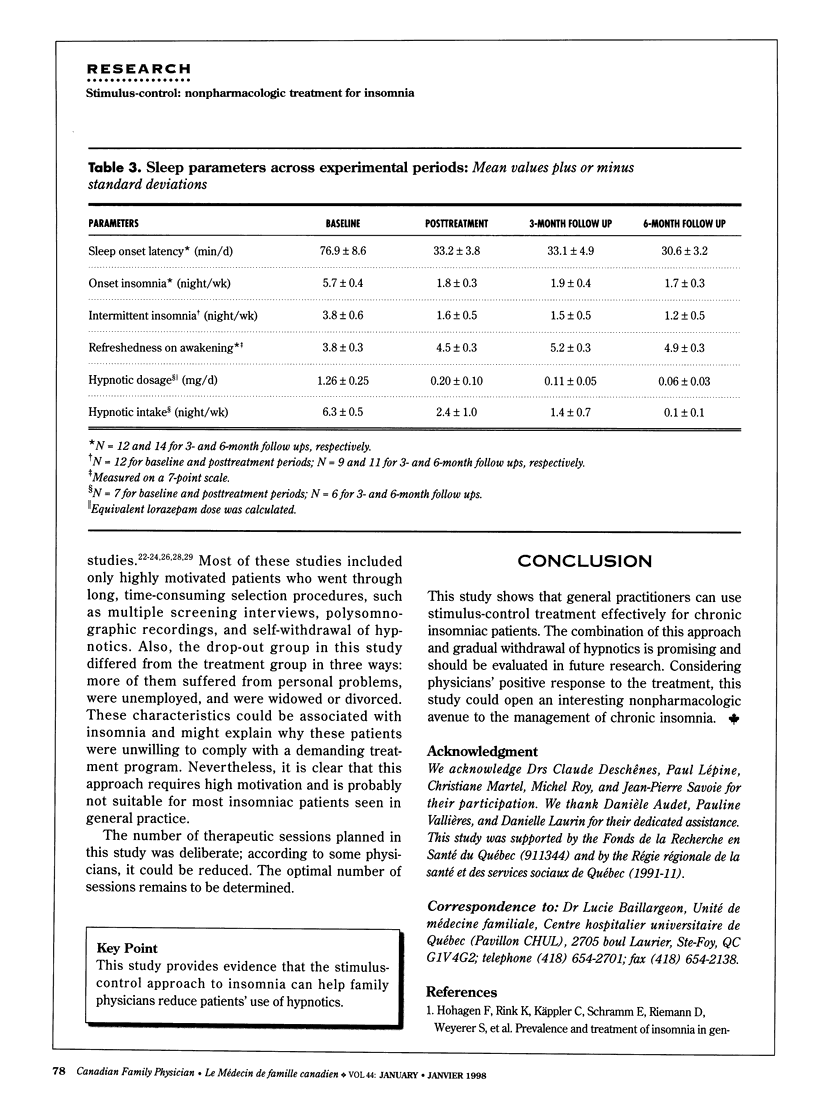
OBJECTIVES: To evaluate the efficacy and applicability of a behavioural treatment for insomnia that can be administered by family physicians in various clinical settings. DESIGN: Efficacy of the treatment was evaluated by single-case experimental designs (multiple baseline across subjects). Applicability was assessed through semistructured interviews with physicians. SETTING: Two private offices, two offices in community health centres, and one office in a family medicine unit. PARTICIPANTS: Six general practitioners and 24 chronic insomniac patients recruited through media advertisements and from physicians' practices. Of an initial 38 subjects screened, six were excluded for sleep-onset latency less than 30 minutes, five for psychological conditions, one for physical handicaps, and two for other reasons. INTERVENTIONS: Physicians used stimulus-control treatment during individual therapeutic sessions. Patients using hypnotics were encouraged to taper off their medications after treatment was initiated. MAIN OUTCOME MEASURES: Time it took patients to get to sleep (sleep-onset latency), amount of hypnotic use, and practitioners' evaluation of the treatment. RESULTS: Fifteen patients completed the treatment; 80% of them reduced their sleep-onset latency. Six of the seven patients using hypnotics at the beginning of the study reduced or stopped their medications. All therapeutic gains were maintained at 3 and 6 months. Physicians thought stimulus-control treatment could be used in medical practice, but specified that it was most useful for highly motivated patients. CONCLUSION: Family physicians can use stimulus-control treatment effectively for patients with chronic insomnia. This nonpharmacologic approach could help motivated patients reduce their use of hypnotics.
Full text
PDF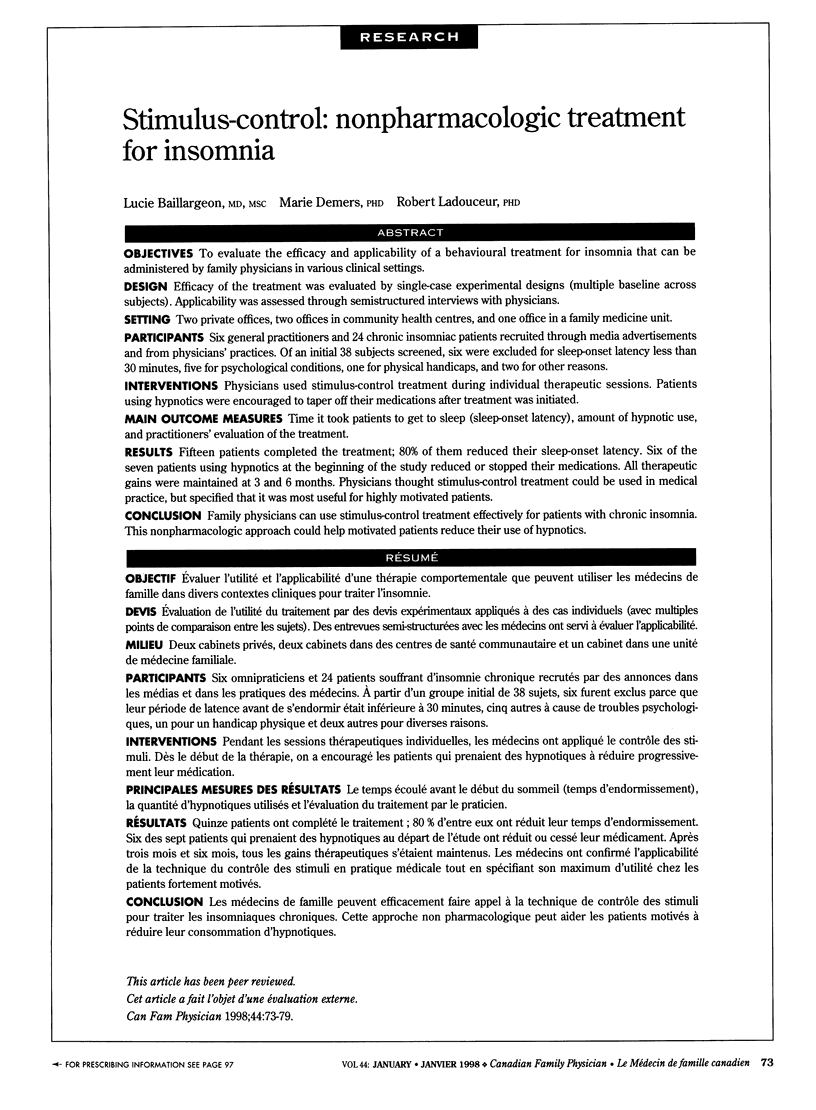


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baillargeon L., Demers M., Grégoire J. P., Pépin M. Enquête sur le traitement de l'insomnie par les omnipraticiens. Can Fam Physician. 1996 Mar;42:426–432. [PMC free article] [PubMed] [Google Scholar]
- Beck A. T., Epstein N., Brown G., Steer R. A. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988 Dec;56(6):893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Borkovec T. D. Insomnia. J Consult Clin Psychol. 1982 Dec;50(6):880–895. doi: 10.1037//0022-006x.50.6.880. [DOI] [PubMed] [Google Scholar]
- Childs-Clarke A. Stimulus control techniques for sleep onset insomnia. 1990 Aug 29-Sep 4Nurs Times. 86(35):52–53. [PubMed] [Google Scholar]
- Coates T. J., Killen J. D., George J., Marchini E., Silverman S., Thoresen C. Estimating sleep parameters: a multitrait--multimethod analysis. J Consult Clin Psychol. 1982 Jun;50(3):345–352. [PubMed] [Google Scholar]
- Espie C. A., Brooks D. N., Lindsay W. R. An evaluation of tailored psychological treatment of insomnia. J Behav Ther Exp Psychiatry. 1989 Jun;20(2):143–153. doi: 10.1016/0005-7916(89)90047-5. [DOI] [PubMed] [Google Scholar]
- Espie C. A., Lindsay W. R., Brooks D. N., Hood E. M., Turvey T. A controlled comparative investigation of psychological treatments for chronic sleep-onset insomnia. Behav Res Ther. 1989;27(1):79–88. doi: 10.1016/0005-7967(89)90123-x. [DOI] [PubMed] [Google Scholar]
- Espie C. A., Monk E., Hood E. M., Lindsay W. R. Establishing clinical criteria for the treatment of chronic insomnia: a comparison of insomniac and control populations. Health Bull (Edinb) 1988 Nov;46(6):318–326. [PubMed] [Google Scholar]
- File T. M., Jr, Tan J. S. Community-acquired pneumonia. The changing picture. Postgrad Med. 1992 Dec;92(8):197-8, 201-8, 211-4. doi: 10.1080/00325481.1992.11701560. [DOI] [PubMed] [Google Scholar]
- Hohagen F., Rink K., Käppler C., Schramm E., Riemann D., Weyerer S., Berger M. Prevalence and treatment of insomnia in general practice. A longitudinal study. Eur Arch Psychiatry Clin Neurosci. 1993;242(6):329–336. doi: 10.1007/BF02190245. [DOI] [PubMed] [Google Scholar]
- Hyman R. B., Feldman H. R., Harris R. B., Levin R. F., Malloy G. B. The effects of relaxation training on clinical symptoms: a meta-analysis. Nurs Res. 1989 Jul-Aug;38(4):216–220. [PubMed] [Google Scholar]
- Kirmil-Gray K., Eagleston J. R., Thoresen C. E., Zarcone V. P., Jr Brief consultation and stress management treatments for drug-dependent insomnia: effects on sleep quality, self-efficacy, and daytime stress. J Behav Med. 1985 Mar;8(1):79–99. doi: 10.1007/BF00845513. [DOI] [PubMed] [Google Scholar]
- Legnani D., Lombardo V. M., Negretto G. G., Beghi G., Caratozzolo O. Comparative clinical and microbiological study of amoxycillin-clavulanic acid and ciprofloxacin in acute purulent exacerbations of chronic bronchitis. J Hosp Infect. 1992 Nov;22 (Suppl A):69–74. doi: 10.1016/s0195-6701(05)80009-x. [DOI] [PubMed] [Google Scholar]
- Marvel M. K., Amodei N. Single-subject experimental designs: a practical research alternative for practicing physicians. Fam Pract Res J. 1992 Jun;12(2):109–121. [PubMed] [Google Scholar]
- Mellinger G. D., Balter M. B., Uhlenhuth E. H. Insomnia and its treatment. Prevalence and correlates. Arch Gen Psychiatry. 1985 Mar;42(3):225–232. doi: 10.1001/archpsyc.1985.01790260019002. [DOI] [PubMed] [Google Scholar]
- Morin C. M., Azrin N. H. Behavioral and cognitive treatments of geriatric insomnia. J Consult Clin Psychol. 1988 Oct;56(5):748–753. doi: 10.1037//0022-006x.56.5.748. [DOI] [PubMed] [Google Scholar]
- Morin C. M., Azrin N. H. Stimulus control and imagery training in treating sleep-maintenance insomnia. J Consult Clin Psychol. 1987 Apr;55(2):260–262. doi: 10.1037//0022-006x.55.2.260. [DOI] [PubMed] [Google Scholar]
- Morin C. M., Culbert J. P., Schwartz S. M. Nonpharmacological interventions for insomnia: a meta-analysis of treatment efficacy. Am J Psychiatry. 1994 Aug;151(8):1172–1180. doi: 10.1176/ajp.151.8.1172. [DOI] [PubMed] [Google Scholar]
- Nicassio P. M., Pate J. K., Mendlowitz D. R., Woodward N. Insomnia: nonpharmacologic management by private practice physicians. South Med J. 1985 May;78(5):556–560. doi: 10.1097/00007611-198505000-00015. [DOI] [PubMed] [Google Scholar]
- Rademaker C. M., Sips A. P., Beumer H. M., Hoepelman I. M., Overbeek B. P., Möllers M. J., Rozenberg-Arska M., Verhoef J. A double-blind comparison of low-dose ofloxacin and amoxycillin/clavulanic acid in acute exacerbations of chronic bronchitis. J Antimicrob Chemother. 1990 Nov;26 (Suppl 500):75–81. doi: 10.1093/jac/26.suppl_d.75. [DOI] [PubMed] [Google Scholar]
- Spielman A. J., Saskin P., Thorpy M. J. Treatment of chronic insomnia by restriction of time in bed. Sleep. 1987 Feb;10(1):45–56. [PubMed] [Google Scholar]


