Abstract
Purines can modify ciliary epithelial secretion of aqueous humor into the eye. The source of the purinergic agonists acting in the ciliary epithelium, as in many epithelial tissues, is unknown. We found that the fluorescent ATP marker quinacrine stained rabbit and bovine ciliary epithelia but not the nerve fibers in the ciliary bodies. Cultured bovine pigmented and nonpigmented ciliary epithelial cells also stained intensely when incubated with quinacrine. Hypotonic stimulation of cultured epithelial cells increased the extracellular ATP concentration by 3-fold; this measurement underestimates actual release as the cells also displayed ecto-ATPase activity. The hypotonically triggered increase in ATP was inhibited by the Cl−-channel blocker 5-nitro-2-(3-phenylpropylamino)benzoic acid (NPPB) in both cell types. In contrast, the P-glycoprotein inhibitors tamoxifen and verapamil and the cystic fibrosis transmembrane conductance regulator (CFTR) blockers glybenclamide and diphenylamine-2-carboxylate did not affect ATP release from either cell type. This pharmacological profile suggests that ATP release is not restricted to P-glycoprotein or the cystic fibrosis transmembrane conductance regulator, but can proceed through a route sensitive to NPPB. ATP release also was triggered by ionomycin through a different NPPB-insensitive mechanism, inhibitable by the calcium/calmodulin-activated kinase II inhibitor KN-62. Thus, both layers of the ciliary epithelium store and release ATP, and purines likely modulate aqueous humor flow by paracrine and/or autocrine mechanisms within the two cell layers of this epithelium.
Keywords: aqueous humor secretion, hypotonic swelling, Cl− channel, ecto-ATPase, purinergic regulation
Glaucoma, a major cause of blindness, usually is associated with elevated intraocular pressure. Pharmacologic treatment of the ocular hypertension is now largely directed toward reducing aqueous humor formation by the ciliary epithelium, a bilayer consisting of a nonpigmented (NPE) and a pigmented (PE) epithelial cell layer (1). The precise mechanisms underlying aqueous humor secretion into the eye are uncertain, but the release of Cl− through basolateral channels of the NPE cells is thought to be rate limiting (2, 3). Thus, agents that can alter this Cl− conductance either directly or indirectly will alter aqueous humor production.
Several recent observations suggest important roles for extracellular ATP and adenosine in the regulation of ciliary epithelial chloride conductance and in the formation of aqueous humor. Purinergic receptors for adenosine and ATP are expressed by both the NPE and PE cells of the ciliary epithelial bilayer (4). Adenosine modifies the transport of Cl− in the NPE cells (5) and alters the flow of aqueous humor (6, 7), and ATP affects Cl− transport in the PE cells (8). Purines are detectable in the aqueous humor, and the combined concentrations of adenosine and its metabolite inosine can rise to micromolar levels (9). Although purines appear to be major regulators of aqueous humor formation, their physiological source is unknown. This study sought to identify the source and release mechanisms of the extracellular purines modulating ciliary epithelial function.
MATERIALS AND METHODS
Quinacrine Staining.
New Zealand White rabbits were injected i.p. with 85 mg/kg of quinacrine and sacrificed 48 hr later, or injected i.v. with 2 mg/kg of quinacrine and sacrificed 1 hr later. The animals were anesthetized with intramuscular injection of 35 mg/kg of ketamine and 5 mg/kg of xylazine before quinacrine injection, and sacrificed by injecting 60 mg/kg of pentobarbital i.v. Rabbit and bovine iris-ciliary body whole mounts were incubated for 30 min at 37°C in isotonic solution containing 5 μM quinacrine. All tissues were freeze-dried and paraffin-embedded before being sectioned at 10–12 μm. Transformed bovine PE and NPE cells were grown on glass coverslips for 3–4 days, washed three times, and incubated at 37°C and pH 7.4 in isotonic solution containing 1–2 μM quinacrine for intervals of 2–50 min. The tissue sections and cultured cells were visualized by fluorescence microscopy.
ATP Measurements.
Transformed bovine PE and NPE cells were grown in 60-mm Petri dishes for 6–10 days in DMEM (GIBCO/BRL) with 10% fetal bovine serum (HyClone) and 50 μg/ml of gentamycin (GIBCO/BRL). After washing three times with isotonic solution, dishes were incubated at 37°C with 800 μl of test solution. Dishes were agitated gently to minimize unstirred layer effects. Extracellular solution (200 μl) was removed at the indicated time and placed in a plastic cuvette on ice. ATP levels were determined by adding 200 μl of ATP assay mix to the 200-μl sample and then measuring luminescence with a Perkin–Elmer 650–10S fluorescence spectrophotometer. ATP measurements were performed at pH 7.65 to maximize the luciferin/luciferase reaction (10). Standard curves were produced daily. Data are presented as mean ± SE.
Cell Viability Assay.
The integrity of the cell membranes was tested by using the Live/Dead Reduced Biohazard Viability/Cytoxicity Kit (Molecular Probes). Briefly, cells grown on coverslips were incubated for 10 min at 37°C in control and test solutions containing 0.2% SYTO 10 and 0.2% Dead Red nucleic acid stains. After washing, cells were fixed for 1 hr with 4% glutaraldehyde. Cells were visualized with a fluorescein long-pass filter set exciting at 450–490 nm.
Solutions and Drugs.
Isotonic and hypotonic solutions contained: 105 mM NaCl, 5 mM KCl, 4.3 mM Hepes (acid), 5.7 mM Hepes (Na+), 5.0 mM NaHCO3, 0.5 mM MgCl2, and 1.3 mM CaCl2. Isotonic solution contained 85.0 mM mannitol (295–300 mOsm), but hypotonic solution did not (225–230 mOsm). The cAMP-stimulating mixture contained 500 μM 8-(4-chloro-phenylthio)-cAMP (cpt-cAMP), 100 μM 3 iso-butyl-1-methylxanthine, and 10 μM forskolin. 5-Nitro-2-(3-phenylpropylamino)benzoic acid (NPPB) and glybenclamide were stored as 100 mM stock solutions in dimethylformamide. Diphenylamine-2-carboxylate (DPC) was stored as a 500 mM stock in ethanol. Tamoxifen was a 10 mM stock in ethanol and stored for just 3 days. Verapamil was stored as a 22.5 mM stock in water, and diisothiocyanato-stilbene-2,2′-disulfonic acid (DIDS) was stored as a 20 mM stock in water. KN-62 was dissolved directly in aqueous solution as a preformed water-soluble complex with 2-hydroxypropyl-β-cyclodextrin obtained from Research Biochemicals (Natick, MA). DPC was purchased from Fluka, cpt-cAMP from Boehringer Mannheim, and NPPB from Biomol (Plymouth Meeting, PA). All other reagents were purchased from Sigma.
RESULTS
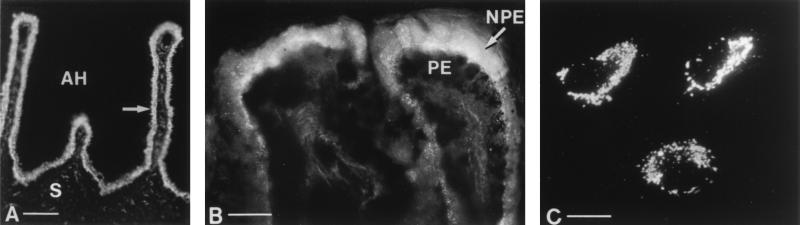
Potential sources of ATP in the anterior eye were identified with the purinergic marker quinacrine (11). The most fluorescent tissue in the ciliary body was the ciliary epithelium (Fig. 1A). Both the PE cell layer, which abuts the stroma, and the adjacent NPE layer, which faces the aqueous humor, displayed intense, diffuse cytoplasmic fluorescence in albino rabbit tissues after i.p. or i.v. injections or after in vitro incubations with quinacrine. In fresh bovine anterior-segment tissues, the staining was particulate and concentrated toward the apical membrane of the NPE cells (Fig. 1B). Fluorescence was not detected in bovine PE cells, but easily could have been obscured by the dense melanin granules. Cultured bovine NPE and pigment-free cultured PE cells both showed bright, particulate staining after incubation with quinacrine (Fig. 1C). Quinacrine did not stain any nerve fibers in the iris/ciliary body of either bovine or rabbit eyes, whereas vascular endothelial cells showed only faint staining.
Figure 1.
Quinacrine staining in ciliary epithelial cells. (A) PE and NPE cell layers fluoresced brightly (arrow) in tissue sections of the ciliary body of an albino rabbit injected i.p. with quinacrine. The PE layer lies closest to the stroma (S) whereas the adjacent NPE layer faces the aqueous humor (AH); both layers stain intensely. Both layers of the ciliary epithelium from rabbits injected i.v. with quinacrine, or incubated in quinacrine also stained intensely (not shown). (B) The NPE cells of bovine tissue incubated with quinacrine showed particulate staining that was brightest on the apical membrane of the cells, facing the PE cells. PE cells did not clearly display fluorescent granules, but the densely packed melanin granules could have obscured the dye. (C) Particulate staining was observed in melanin-free cultured PE cells incubated in quinacrine. Cultured NPE cells (not shown) showed a similar pattern and intensity of staining. (Magnification bars: A, 100 μm; B and C, 25 μm.)
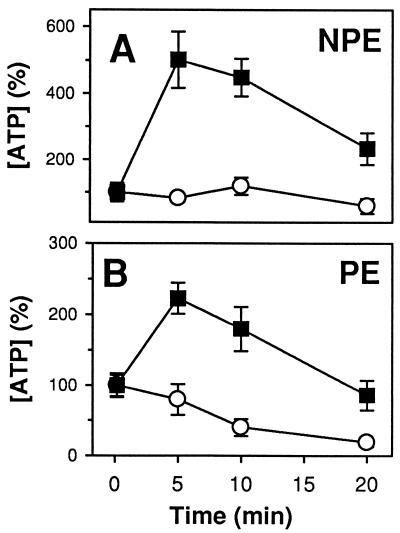
The relative intensity of the quinacrine staining in both PE and NPE cells suggested that the ciliary epithelium contained stores of ATP and that ciliary epithelial cells could act as a source of releasable ATP. Because hypotonic stimulation can trigger release of a range of cellular solutes (12), the effect of hypotonicity on ATP release was examined. Bathing cultured bovine ciliary epithelial cells in hypotonic solution increased the media concentration of ATP (Fig. 2). After 10 min, the mean levels of ATP for the entire series were elevated by 230 ± 27% (n = 29) and 272 ± 52% (n = 33) for the NPE and PE cells, respectively, normalized to the levels in isotonic solution. The absolute amounts of ATP released after swelling the NPE and PE cells were 1.6 ± 0.2 and 0.8 ± 0.1 pmol/cm2, respectively. The corresponding ATP concentrations reached at the apical membranes between the two cell layers in the intact epithelium can be estimated, assuming that approximately half the ATP is released in this direction and assuming an intermembrane separation of 1 μm. This is a highly conservative overestimate of separation because the NPE and PE cells are linked by gap junctions. The local ATP concentration thereby is estimated to exceed 4–8 μM, a range at which both ATP (8) and adenosine (5) exert transport effects on ciliary epithelial cells.
Figure 2.
Hypotonically triggered release of ATP from cultured bovine NPE (A) and PE (B) cells. Extracellular samples obtained from cells bathed in hypotonic solution (▪) showed an increase in ATP concentration whereas samples from cells bathed in isotonic solution (○) did not. ATP was normalized to the 10-sec isosmotic measurement for each set of experiments. Separate dishes were used for each time measurement (n = 5–10).
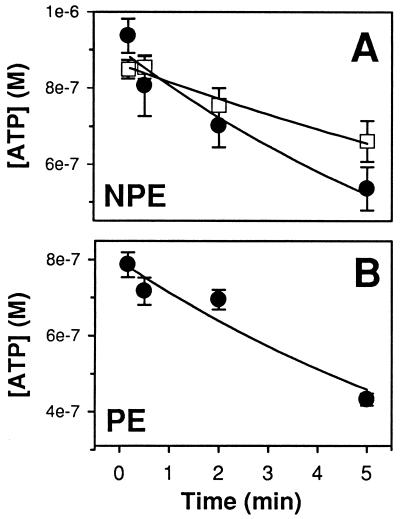
The ATP concentration in the external bath of both cell types fell substantially by 20 min even though the cells remained in hypotonic solution, suggesting the action of ecto-ATPases. When exogenous ATP was added to dishes containing PE and NPE cells, a time-dependent decrease in the concentration of ATP was found (Fig. 3). The rate of ATP degradation was decreased when the extracellular Ca2+ and Mg2+ levels were lowered from physiological levels to 1 μM (Fig. 3A), consistent with the requirement of ecto-ATPases for divalent cations (13).
Figure 3.
Degradation of externally added ATP by ciliary epithelial cells. ATP (1.2 μM) in isotonic solution was added to dishes of NPE (A) or PE (B) cells at t = 0, and a sample of extracellular solution was removed at the time indicated. Separate dishes were used for each time point. ATP was degraded at a lower rate (P < 0.05, n = 4–5) in isotonic containing only 1 μM Ca2+ and Mg2+ (A, □, τ = 19 ± 1 min) rather than 1.3 mM Ca2+ and 0.5 mM Mg2+ (A, •, τ = 8 ± 1 min; B, τ = 9 ± 2 min).
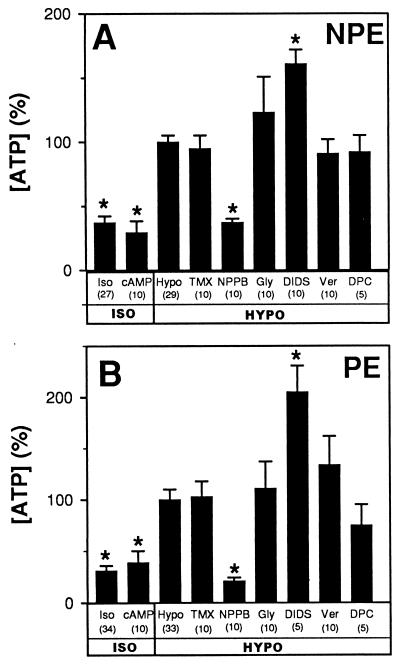
The hypotonically stimulated ATP release was abolished by a 100-μM concentration of the Cl−-channel blocker NPPB (Fig. 4), suggesting that the ATP was leaving both NPE and PE cells through an ion channel. In additional experiments, even 10 μM NPPB reduced the hypotonically stimulated ATP release from PE cells by 25 ± 11% (n = 11, P < 0.05 by paired t test). Some evidence suggests that ATP release from mammalian epithelial cells can proceed through members of the ATP-binding cassette family of proteins such as the cAMP-activated cystic fibrosis transmembrane conductance regulator (CFTR) (14, 15) or the swelling-activated P-glycoprotein (16, 30), but agreement is incomplete (10, 17). For this reason, agents known to affect activity of CFTR and P-glycoprotein were applied to the bovine NPE and PE cells. Isotonic release of ATP in the ciliary epithelial cells was unaltered by a cAMP-stimulating cocktail, and hypotonically triggered release was not blocked by glybenclamide, DPC, verapamil, or tamoxifen (Fig. 4). DIDS (18) increased the ATP concentration measured in the bath after hypotonic stimulation (Fig. 4).
Figure 4.
Manipulation of ATP release from cultured NPE (A) and PE (B) cells. ATP release in isotonic solution (Iso) was not triggered by a cAMP-stimulating cocktail. Hypotonic solution (Hypo) led to an increase in ATP that was blocked by 100 μM NPPB, but unaffected by 10 μM tamoxifen (TMX), 100 μM glybenclamide (Gly), 100 μM verapamil (Ver), or 500 μM DPC. DIDS (100 μM) increased ATP levels. (∗ = different from hypotonic levels, P < 0.001). The vehicles had no significant effect. ATP concentration was normalized to the mean hypotonic level for each day’s experiments.
Because exocytosis is likely involved in ATP release from some nonneural cells (19, 20), we also tested the effects of elevating intracellular Ca2+ by applying 3.0–5.0 μM concentrations of the ionophore ionomycin. Ionomycin increased the ATP release of bovine NPE cells by 284 ± 93% (n = 9, P < 0.02). This stimulation was reduced by ≈60% to 118 ± 51% (P < 0.02 by paired analysis) by including 500 nM KN-62, a blocker of both calcium/calmodulin-activated kinase II (21) and P2X7 pores (22). In separate experiments, 100 μM NPPB had no detectable effect on the ionomycin-stimulated ATP release (n = 9). Neither 100 μM NPPB nor 500 nm KN-62 affected the standard curve constructed with known concentrations of ATP. There was no microscopically evident increase in permeability to Dead Red after exposure to hypotonicity or ionomycin.
DISCUSSION
This study establishes that both NPE and PE cells of the ciliary epithelium act as a source of purines. The cells store, release, and catabolize ATP. Further, the swelling-activated release of ATP from ciliary epithelial cells occurs through a route different from CFTR (14, 15) and P-glycoprotein (16, 30).
Because of its binding affinity for adenine nucleotides in general and especially ATP, the fluorescent acridine derivative quinacrine is the preferred available light-microscopic marker for intracellular ATP stores (23). Quinacrine labels putative purinergic central and peripheral neurons (24), which presumably bind the dye because of high vesicular content of ATP. In the peripheral nervous system, quinacrine labels subsets of sympathetic and parasympathetic neurons and their terminal fibers. In the eye, quinacrine does not stain nerve fibers (25, 26), and there are no reports of physiologically active ATP release from the ocular autonomic innervation. The present study confirms the absence of quinacrine staining of peripheral nerve fibers in the eye but now demonstrates intense staining of the ciliary epithelium. Previous histochemical attempts to localize purinergic sources in the ciliary body with quinacrine (25, 26) used whole-mount preparations and reported only background fluorescence. Because the ciliary epithelium covers the entire ciliary body when viewed as a whole mount, specific localization to the epithelium requires tissue sections perpendicular to the epithelial surface, as performed here. The particulate staining in bovine cells as compared with the diffuse cytoplasmic staining of rabbit cells may reflect a species difference in the storage mechanism. The apical localization of the quinacrine staining in fresh bovine NPE cells may indicate a polarized release of ATP.
The cation dependence of the rate of ATP degradation (Fig. 3) is consistent with the requirements for the known ecto-ATPase enzymes (13) and strongly suggests their presence in both ciliary epithelial cell types. Ecto-ATPase activity on NPE and PE cells would limit the duration of any ATP stimulation of P2 receptors and could lead to the extracellular production of adenosine capable of stimulating P1 receptors. The decrease in the concentration of ATP after 20 min in hypotonic solution reflects both the actions of ecto-ATPases and a decline in the rate of ATP release, for ecto-ATPases acting on a steady release would lead to a constant level of extracellular ATP (10). The functional importance of the ecto-ATPases is further indicated by the action of DIDS to increase the concentration of ATP measured in the bath after hypotonic stimulation. This stimulation cannot be explained by the action of DIDS to block some types of Cl− channels but could reflect its effect to inhibit ecto-ATPases (27). The hypotonic stimulations of baseline release by ciliary epithelial cells were almost an order of magnitude higher than the 36% increase reported in hepatocytes (28) (Fig. 4). Furthermore, our measurements underestimate the actual magnitude of ATP release because of the ecto-enzymatic activity noted with both NPE and PE cells (Fig. 3).
Our characterization of ATP release in the ciliary epithelial cells has identified an additional release mechanism. The concentration-dependent blockage by NPPB suggests that an ion channel is involved. Significant inhibition was noted at even 10 μM, at which concentration NPPB appears free of nonspecific effects (29). It has been proposed that ATP transport proceeds through CFTR (14, 15) or P-glycoprotein (16, 30) in other epithelial cells. However, the inability of two blockers of CFTR channels, DPC and glybenclamide, to inhibit the hypotonically triggered ATP efflux argues against a role of CFTR in ciliary epithelial cells. This result is consistent with the undetectability of CFTR transcripts in NPE cells (31) and the unaltered aqueous humor flow in patients with cystic fibrosis (32). The inability of cAMP to stimulate ATP efflux in ciliary epithelial cells further supports this conclusion. The P-glycoprotein blockers tamoxifen and verapamil did not inhibit ATP efflux from either PE or NPE cells, indicating that P-glycoprotein also is not involved in ATP transport in these cells. The ineffectiveness of tamoxifen also argues against ATP release through the conduit for large organic osmolytes, VSOAC (33). We conclude that ATP leaves through a NPPB-sensitive mechanism that is likely to be, but is not necessarily, a channel. Although we have excluded CFTR and P-glycoprotein, other members of the ATP-binding cassette family of proteins (34) may mediate the hypotonically stimulated ATP release.
We also have observed that ATP release can be triggered by ionomycin. This second release is inhibited by 500 nM KN-62 but, in contrast to swelling-activated release, is unaffected by 100 μM NPPB. This observation suggests that ciliary epithelial cells can use two pathways, which differ at some point in their signaling or mechanisms of ATP release.
Like other cytochemical stains, quinacrine is not molecularly specific. However, in conjunction with the functional release of ATP by both PE and NPE cells and the action of ecto-ATPases on these cells, the results identify the ciliary epithelium itself as a source of purines previously shown to modulate aqueous humor production (6, 7). The absence of quinacrine staining of the terminal nerve fibers suggests that the neural contribution for ATP delivery to the ciliary epithelium must be very small, consistent with the known variability in neuronal ATP content (24). In view of the known purinergic receptors (4) and purinergic modulation of transport of both NPE (5) and PE cells (8) of the ciliary epithelium, we propose an interlayer autocrine/paracrine model of the purinergic regulation of aqueous humor formation, in which: (i) ATP (and possibly other nucleotides and adenosine) are released by NPE and PE cells; (ii) membrane ecto-enzymes hydrolyze ATP to extracellular adenosine (35); (iii) the resulting adenosine acts on NPE cells to stimulate aqueous humor formation by activating Cl− channels (5); (iv) extracellular ATP stimulates aqueous humor reabsorption by activating PE anion channels (8); and (v) net aqueous humor formation is regulated at least in part by coordinating these opposing purinergic effects on unidirectional secretion and reabsorption. Exploitation of this local purinergic mechanism may provide a new pathway for antiglaucoma drug development.
Acknowledgments
We are grateful to Dr. Patricia Grimes (University of Pennsylvania) for helpful advice in the morphologic analysis. This work was funded in part by training grants (EY-07035 and HL-07027) for C.H.M., by research grants to R.A.S. (EY05454) and M.M.C. (EY-10691), and by a core facilities grant (EY-01583), all from the National Institutes of Health. R.A.S. is a Research to Prevent Blindness Senior Scientific Investigator.
ABBREVIATIONS
- NPE
nonpigmented
- PE
pigmented
- NPPB
5-nitro-2-(3-phenylpropylamino)benzoic acid
- CFTR
cystic fibrosis transmembrane conductance regulator
- DPC
diphenylamine-2-carboxylate
- DIDS
diisothiocyanato-stilbene-2,2′-disulfonic acid
References
- 1.Krupin T, Civan M M. In: The Glaucomas. 2nd Ed. Ritch R, Shields M B, Krupin T, editors. St. Louis: Mosby; 1995. pp. 251–280. [Google Scholar]
- 2.Bowler J M, Peart D, Purves R D, Carré D A, Macknight A D C, Civan M M. Exp Eye Res. 1996;62:131–139. doi: 10.1006/exer.1996.0017. [DOI] [PubMed] [Google Scholar]
- 3.Civan M M. News Physiol Sci. 1997;12:158–162. [Google Scholar]
- 4.Wax M, Sanghavi D M, Lee C H, Kapadia M. Exp Eye Res. 1993;57:89–95. doi: 10.1006/exer.1993.1102. [DOI] [PubMed] [Google Scholar]
- 5.Carré D A, Mitchell C H, Peterson-Yantorno K, Coca-Prados M, Civan M M. Am J Physiol. 1997;273:C1354–C1361. doi: 10.1152/ajpcell.1997.273.4.C1354. [DOI] [PubMed] [Google Scholar]
- 6.Crosson C E. J Pharmacol Exp Ther. 1995;273:320–326. [PubMed] [Google Scholar]
- 7.Crosson C E, Gray T. Invest Ophthalmol Visual Sci. 1996;37:1833–1839. [PubMed] [Google Scholar]
- 8.Mitchell, C. H., Peterson-Yantorno, K., Coca-Prados, M. & Civan, M. M. (1997) Invest. Ophthalmol. Visual Sci. 38, Suppl., S1042, (abstr.).
- 9.Petrovich, M., Gray, T. & Crosson, C. E. (1997) Invest. Ophthalmol. Visual Sci. 38, Suppl., S820, (abstr.).
- 10.Grygorczyk R, Hanrahan J W. Am J Physiol. 1997;272:C1058–C1066. doi: 10.1152/ajpcell.1997.272.3.C1058. [DOI] [PubMed] [Google Scholar]
- 11.Belai A, Burnstock G. Cell Tissue Res. 1994;278:197–200. doi: 10.1007/BF00305792. [DOI] [PubMed] [Google Scholar]
- 12.Hoffmann E K. Curr Top Membr Transp. 1987;30:125–180. [Google Scholar]
- 13.Meghji P, Burnstock G. Life Sci. 1995;57:763–771. doi: 10.1016/0024-3205(95)02004-3. [DOI] [PubMed] [Google Scholar]
- 14.Schwiebert E M, Egan M E, Hwang T H, Fulmer S B, Allen S S, Cutting G R, Guggino W B. Cell. 1995;81:1063–1073. doi: 10.1016/s0092-8674(05)80011-x. [DOI] [PubMed] [Google Scholar]
- 15.Prat A G, Reisin I L, Ausiello D A, Cantiello H F. Am J Physiol. 1996;270:C538–C545. doi: 10.1152/ajpcell.1996.270.2.C538. [DOI] [PubMed] [Google Scholar]
- 16.Roman R M, Wang Y, Lidofsky S D, Feranchak A P, Lomri N, Scharschmidt B F, Fitz J G. J Biol Chem. 1997;272:21970–21976. doi: 10.1074/jbc.272.35.21970. [DOI] [PubMed] [Google Scholar]
- 17.Reddy M M, Quinton P M, Haws C, Wine J J, Grygorczyk R, Tabcharani J A, Hanrahan J W, Gunderson K L, Kopito R R. Science. 1996;271:1876–1879. doi: 10.1126/science.271.5257.1876. [DOI] [PubMed] [Google Scholar]
- 18.Gögelein H. Biochim Biophys Acta. 1988;947:521–547. doi: 10.1016/0304-4157(88)90006-8. [DOI] [PubMed] [Google Scholar]
- 19.Rojas E, Pollard H B, Heldman E. FEBS Lett. 1985;185:323–327. doi: 10.1016/0014-5793(85)80931-5. [DOI] [PubMed] [Google Scholar]
- 20.Osipchuk Y, Cahalan M. Nature (London) 1992;359:241–244. doi: 10.1038/359241a0. [DOI] [PubMed] [Google Scholar]
- 21.Tokumitsu H, Chijiwa T, Hagiwara M, Mizutani A, Terasawa M, Hidaka H. J Biol Chem. 1990;265:4315–4320. [PubMed] [Google Scholar]
- 22.Gargett C E, Wiley J S. Br J Pharmacol. 1997;120:1483–1490. doi: 10.1038/sj.bjp.0701081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.White P N, Thorne P R, Housley G D, Mockett B, Billett T E, Burnstock G. Hearing Res. 1995;90:97–105. doi: 10.1016/0378-5955(95)00151-1. [DOI] [PubMed] [Google Scholar]
- 24.Knight G E, Hoyle C H, Burnstock G. Comp Biochem Physiol. 1992;102:305–314. doi: 10.1016/0742-8413(92)90116-o. [DOI] [PubMed] [Google Scholar]
- 25.Olson L, Ålund M, Norberg K-A. Cell Tissue Res. 1976;171:407–423. doi: 10.1007/BF00220234. [DOI] [PubMed] [Google Scholar]
- 26.Burnstock G, Cocks T, Crowe R, Kasakov L. Br J Pharmacol. 1978;63:125–138. doi: 10.1111/j.1476-5381.1978.tb07782.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ziganshin A U, Ziganshina L E, King B F, Pintor J, Burnstock G. Biochem Pharmacol. 1996;51:897–901. doi: 10.1016/0006-2952(95)02252-x. [DOI] [PubMed] [Google Scholar]
- 28.Wang Y, Roman R, Lidofsky S D, Fitz J G. Proc Natl Acad Sci USA. 1996;93:12020–12025. doi: 10.1073/pnas.93.21.12020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wangemann, P., Wittner, M., Di Stefano, A., Englert, H. C., Lang, H. J., Schlatter, E. & Greger, R. (1986) Pflügers Arch. 407, Suppl. 2, S128–S141. [DOI] [PubMed]
- 30.Abraham E H, Prat A G, Gerweck L, Seneveratne T, Arceci R J, Krammer R, Guidotti G, Cantiello H F. Proc Natl Acad Sci USA. 1993;90:312–316. doi: 10.1073/pnas.90.1.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coca-Prados M, Anguíta J, Chalfant M L, Civan M M. Am J Physiol. 1995;268:C572–C579. doi: 10.1152/ajpcell.1995.268.3.C572. [DOI] [PubMed] [Google Scholar]
- 32.McCannel C A, Scanlon P D, Thibodeau S, Brubaker R F. Invest Ophthalmol Visual Sci. 1992;33:160–164. [PubMed] [Google Scholar]
- 33.Strange K, Emma F, Jackson P S. Am J Physiol. 1996;270:C711–C730. doi: 10.1152/ajpcell.1996.270.3.C711. [DOI] [PubMed] [Google Scholar]
- 34.Allikmets R, Gerrard B, Hutchinson A, Dean M. Hum Mol Genet. 1996;5:1649–1655. doi: 10.1093/hmg/5.10.1649. [DOI] [PubMed] [Google Scholar]
- 35.Dubyak G R, El-Moatassim C. Am J Physiol. 1993;265:C577–C606. doi: 10.1152/ajpcell.1993.265.3.C577. [DOI] [PubMed] [Google Scholar]