Abstract
For individuals with temporomandibular joint (TMJ) disc displacement without reduction with limited mouth opening (closed lock), interventions vary from minimal treatment to surgery. In a single-blind trial, 106 individuals with TMJ closed lock were randomized among medical management, rehabilitation, arthroscopic surgery with post-operative rehabilitation, or arthroplasty with post-operative rehabilitation. Evaluations at baseline, 3, 6, 12, 18, 24, and 60 months used the Craniomandibular Index (CMI) and Symptom Severity Index (SSI) for jaw function and TMJ pain respectively. Using an intention-to-treat analysis, we observed no between-group difference at any follow-up for CMI (p ≥ 0.33) or SSI (p ≥ 0.08). Both outcomes showed within-group improvement (p < 0.0001) for all groups. The findings of this study suggest that primary treatment for individuals with TMJ closed lock should consist of medical management or rehabilitation. The use of this approach will avoid unnecessary surgical procedures.
Keywords: temporomandibular joint, closed lock, randomized clinical trial, effectiveness study
INTRODUCTION
Temporomandibular disorders (TMD) affect the temporomandibular joint (TMJ), masticatory muscles, and associated structures. Annually, from 1 to 3% of Americans seek professional care for TMD symptoms (Drangsholt et al., 1999). An estimated 2% of people with TMD have jaw locking from a permanently displaced intra-articular disc—that is, disc displacement without reduction with limited opening, or TMJ closed lock (LeResche, 1995). This advanced disorder can cause significant pain and interfere with jaw movement and function.
For most TMD, clinicians generally agree that non-surgical care should precede surgery. However, for TMJ closed lock, surgery has been described as preferable (Wilkes, 1991; Dimitroulis, 2005; Mercuri and Laskin, 1994). In practice, closed-lock treatment varies widely in invasiveness, based mainly on the provider's experiences.
Studies to date do not support a standard of care for primary or concomitant closed-lock therapy. A review of closed-lock treatment literature found “no distinguishing effects” among orthotics, physical therapy, arthrocentesis, and arthroscopic surgery (Kropmans et al., 1999). Since then, two randomized trials found no difference between selected non-surgical treatments (Minakuchi et al., 2001), or between arthroscopic surgery and discectomy (Holmlund et al., 2001).
This report describes the first adequately powered randomized study assessing the effectiveness of four treatment strategies for individuals with closed lock. The strategies, defined by their initial treatment modalities, were: Medical Management, Rehabilitation, Arthroscopy with Post-operative Rehabilitation, and Arthroplasty with Post-operative Rehabilitation. The null hypothesis was that initial treatment with medical management improves pain and jaw function as much and as quickly as initial treatment by rehabilitation with or without surgery.
MATERIALS & METHODS
Participants and Study Design
This randomized effectiveness study was conducted at the University of Minnesota from June, 1992, to June, 2004. Institutional Review Board approval was obtained and renewed annually during recruitment. Participants were recruited from the University's TMJ and Orofacial Pain Clinic, HealthPartners TMJ Clinics, and the authors' private practices. Inclusion criteria were: age 18 to 65 yrs; daily pain in affected joints aggravated by jaw movement and function; duplication of pain when the affected joint was examined; magnetic resonance imaging (MRI) diagnosis of stage III or IV closed lock (Wilkes, 1989); limited mouth opening; and at least two years' availability. Exclusion criteria, assessed by medical history, included: systemic rheumatic disease; generalized joint pain or swelling; pregnancy; concurrent use of steroids, anti-inflammatories, muscle relaxants, or narcotics; major psychiatric disease; any medical contraindication; drinking more than 3 alcoholic drinks daily; unwillingness to accept study treatments; and prior TMJ surgery. Eligibility was assessed, surgical risks discussed, consent obtained, and enrollment made by one of the authors. The randomized allocation had two strata defined by duration of decreased opening: “Non-chronic” (under 6 months' duration), and “Chronic”. Treatment assignment was concealed from participants and care provider(s) in sealed envelopes until the enrollment procedure was completed. The study coordinator then opened the envelope and informed the participant of the group assignment.
Clinical examinations and questionnaires were completed at baseline and three-, six-, 12-, 18-, 24-, and 60-month follow-ups. A single examiner, blinded to treatment assignment, performed all clinical measures. The examiner's reliability for the Craniomandibular Index (CMI) examination was assessed yearly relative to a gold-standard examiner, with inter-examiner intraclass correlation coefficients between 0.88 and 0.93. The examiner had no contact with participants except during planned clinical evaluations. When participants presented for evaluation, a research coordinator administered questionnaires, instructed them not to discuss treatment with the examiner, and placed a thin tape over both pre-auricular areas to conceal the surgical scar's absence or presence. Given these measures, further evaluation of the blind was deemed unnecessary. Masking participants to treatment would have required sham surgery, so the study was single-blind. The APPENDIX provides further details on participants, study design, and the flow of participants through the study.
Treatment Groups and Interventions
Participants were randomized among 4 treatment strategies labeled by their initial treatment modality: Medical Management, Rehabilitation, Arthroscopy, or Arthroplasty. All 4 treatment approaches represent current standard practice.
Medical Management included education on the participant's condition, with optimistic counseling, a self-help program (Wright and Schiffman, 1995), and a six-day regimen of oral methylprednisolone followed by non-steroidal anti-inflammatory drugs (NSAIDs) for 3-6 wks. Muscle relaxants and over-the-counter analgesics were used as needed. One dentist implemented all treatment.
Rehabilitation included treatment from a dentist, physical therapist, and health psychologist (Fricton et al., 1987a). Participants were randomly assigned to one of two treating dentists (ELS, JRF). Treatment was medical management (above) plus an intra-oral orthotic (splint), physical therapy, and cognitive-behavioral therapy. Physical therapy involved joint mobilization, physical therapy modalities, and a home exercise program. Cognitive-behavioral therapy included assessment of oral habits, maladaptive habits, and psychopathology, and two follow-up sessions focused on education, habit reversal, and improvement of compliance and self-efficacy.
Arthroscopy was performed by a randomly assigned oral surgeon (JQS or RBT), with the patient under general anesthesia (Moses and Poker, 1989). The superior joint space was lavaged, intracapsular adhesions underwent lysis, and intracapsular betamethasone was injected. Success was assessed when the mandible was manually moved through excursive movements.
Arthroplasty was an open-joint surgery performed by one oral surgeon (Clyde Wilkes) with patients under general anesthesia (Wilkes, 1991). A disc repositioning procedure (discoplasty) was attempted. If the tissues had degenerated too greatly, disc removal (discectomy) was performed.
The APPENDIX describes each treatment modality further.
All care providers followed their assigned participants for 6 mos, with additional follow-up as needed. Medical Management modalities were extended to the other groups; the surgical groups also received post-operative narcotics. Pre-operatively, surgical patients saw the physical therapist, psychologist, and surgeon. Post-operatively, surgical patients received the same treatments by physical therapists and psychologists as the Rehabilitation participants. If surgical patients needed an orthotic, one dentist inserted and monitored it. All but two Arthroscopy and five Arthroplasty patients received an orthotic. There were 15 bilateral and 8 unilateral arthroscopies, and 13 bilateral and 8 unilateral arthroplasties.
Study Measures
The primary outcome measures were the Craniomandibular Index (CMI) and the modified Symptom Severity Index (SSI). The CMI is a reliable, valid instrument for assessing jaw pain and dysfunction (Fricton and Schiffman, 1986, 1987). The SSI is a self-reported pain measure consisting of 5 reliable, valid subscales measuring sensory and affective intensity, frequency, duration, and tolerability of pain, and a non-specific symptom checklist (Fricton, 1990; Fricton and Schiffman, 1987; Fricton et al., 1987b). Clinical TMD studies, including the present study, have used a modified SSI excluding the symptom checklist (Wright et al., 1995, 2000; Shaefer et al., 2001; Fricton et al., 2002).
Adjustment variables included baseline CMI and SSI, baseline depression and somatization (Symptom Checklist-90-Revised; Derogatis, 1992), selected demographic variables (age, sex, and education; IMPATH, Fricton et al., 1987b), and family income (Health Status Questionnaire 2.0, Pearson National Computer Systems [NCS], Bloomington, MN, USA).
Treating clinicians assessed treatment compliance through the six-month follow-up, rating it as none or poor (0), adequate (1), or good to excellent (2). Medication use was assessed from data collected at follow-up visits.
Statistical Procedures
The primary analyses were by intention-to-treat; individuals receiving a second treatment modality during follow-up were analyzed according to their original treatment assignments. Ten participants withdrew after randomization, but before receiving therapy (Appendix Fig.). Eight were examined 5 yrs later; the five-year analyses include them. To assess their influence, we included, in a secondary five-year analysis, only participants receiving treatment.
The planned primary analysis was a separate one-way ANOVA at each follow-up time, unadjusted for multiple comparisons. As will become clear, adjustment was unnecessary. We checked whether combining times would produce a group difference using a repeated-measures analysis (linear mixed model, PROC MIXED, SAS Institute, Cary, NC, USA). Another analysis compared treatment groups at each follow-up time, adjusting for variables specified above (SAS GLM procedure). Other planned analyses compared groups by treatment compliance and medication use. Improvement from baseline was tested in each group at each follow-up time by paired t tests.
Assuming that a less invasive strategy would be preferred unless a more invasive treatment strategy would be superior, we planned 3 contrasting treatments—Medical Management vs. each of the other groups—for both the CMI and SSI, giving 6 total comparisons. The key to sample size specification was a meaningful improvement in jaw function and TMJ pain. Chronic pain studies have estimated a clinically important pain reduction as up to 50% (Turk et al., 1993). Population norms for the CMI and SSI are 0.10 and 0.03, respectively (Schiffman et al., 1990). The study population's baseline CMI and SSI means were 0.45 and 0.62, respectively. Based on a 40% decrease in TMD-related pain, a clinically meaningful difference at follow-up would be 0.4 × (0.45 − 0.10) = 0.14 for the CMI, and 0.4 × (0.62 − 0.03) = 0.24 for the SSI. The power calculation assumed a one-way ANOVA with per-comparison alpha of 0.05/6 = 0.0083. With one-sided hypothesis tests, 20 individuals per group gave 80% power per-comparison to detect differences of 0.12 and 0.18 in the CMI and SSI, respectively.
RESULTS
Counts of participants randomized to each treatment group, acceptance of their assigned treatment, and attendance at each follow-up visit are presented (Table 1). Comparison of treatment groups at baseline showed no differences (p ≥ 0.09, Table 2). According to the same baseline characteristics, the ten participants declining their assigned treatment did not differ from those accepting it (p > 0.2).
Table 1.
Total Participants Randomized, Total Participants Accepting Randomized Treatment at Baseline, and Total Participants Seen at Six Follow-up Intervals (Distributions by Treatment Group)
| Treatment Groups | Randomized | Treatment Received |
3 Mos | 6 Mos | 12 Mos | 18 Mos | 24 Mos | 60 Mos, Randomized |
60 Mos, Treatment Received |
|---|---|---|---|---|---|---|---|---|---|
| Medical Management | 29 | 29 | 28 | 28 | 29 | 25 | 26 | 27 | 27 |
| Rehabilitation | 25 | 23 | 22 | 20 | 22 | 22 | 21 | 23 | 21 |
| Arthroscopic Surgery | 26 | 23 | 23 | 21 | 23 | 20 | 22 | 24 | 22 |
| Arthroplasty Surgery | 26 | 21 | 20 | 19 | 20 | 21 | 20 | 24 | 20 |
| Totals | 106 | 96 | 93 | 88 | 94 | 88 | 89 | 98 | 90 |
Table 2.
Baseline Measures and Adjustment Variables [Means and (Standard Error of the Mean) by Treatment Group]
| Treatment Groups (Total Study Sample = 106) |
Birth Date (a) | Age (b) | % Females | Education (c) | Family Income (d) | Marital Status (e) | Depression | Somatization |
|---|---|---|---|---|---|---|---|---|
| Medical Management (n = 29) | 20,473 (645) | 33.7 (1.8) | 90 | H - 4/29 | 6.39 (0.45) | S - 4/29 | 49.6 (2.0) | 50.8 (1.7) |
| C - 22/29 | M - 22/29 | |||||||
| G - 3/29 | D - 3/29 | |||||||
| Rehabilitation (n = 25) | 21,916 (611) | 30.0 (1.7) | 100 | H - 4/25 | 5.72 (0.54) | S - 8/25 | 49.1 (2.4) | 50.3 (2.0) |
| C - 19/25 | M - 11/25 | |||||||
| G - 2/25 | D - 6/25 | |||||||
| Arthroscopic Surgery (n = 26) | 21,277 (628) | 31.8 (1.7) | 85 | H - 6/26 | 5.38 (0.39) | S - 6/26 | 51.0 (1.8) | 52.2 (2.0) |
| C - 16/26 | M - 18/26 | |||||||
| G - 4/26 | D - 2/26 | |||||||
| Arthroplasty Surgery (n = 26) | 21,264 (646) | 31.4 (1.9) | 96 | H - 10/26 | 5.38 (0.43) | S - 7/26 | 52.0 (2.0) | 53.5 (1.5) |
| C - 14/26 | M - 16/26 | |||||||
| G - 2/26 | D - 3/26 | |||||||
| P-value for difference | p = 0.4 | p = 0.5 | p = 0.2 | p = 0.3 | p = 0.09 | p = 0.3 | p = 0.7 | p = 0.5 |
Number of days since 1960 to day of birth.
Age in yrs at start of the study.
Overall, 23% were high school graduates (H), 67% had a Vocational Tech or college education (C), and 10% had a Graduate College education (G).
The response categories were 1 (0 to $10,000) to 9 ($90,000 or more). The highest value, 6.39, represents an average annual family income between $60,000 and $70,000.
Overall, 24% were single (S), 63% were married (M), and 13% were divorced (D).
CMI results (Table 3) and SSI results (Table 4) show 2 rows of p-values. The upper row indicates differences between groups at each follow-up time, unadjusted for multiple comparisons. Group means did not differ at any follow-up for either CMI (p > 0.3) or SSI (p ≥ 0.08); neither was there a between-group difference after the exclusion of participants who declined assigned treatment (p ≥ 0.5; “60-month Treatment Received” in Tables 3 and 4). Repeated-measures analysis of CMI showed no difference between groups in average or time-course. Repeated-measures analysis of SSI showed group differences only if follow-up time was treated as a continuous predictor, i.e., based on the assumption that SSI declined linearly. Then, the groups differed in time trend (p = 0.03): Arthroplasty achieved full effect by 3 mos, while the other groups improved throughout the 60-month follow-up. Adjusted analyses of CMI showed no group differences at any follow-up (p ≥ 0.09). In adjusted analyses of SSI, Arthroplasty was superior to Medical Management at the six-month follow-up (p = 0.02, with multiple comparisons disregarded); otherwise, groups did not differ. All groups improved over baseline (p < 0.0001) at all follow-up times for both CMI and SSI (lower row of p-values in Tables 3 and 4).
Table 3.
Craniomandibular Index (CMI) (Observed Means and Standard Deviations by Treatment Group and Follow-up Interval)
| Treatment Groups | Baseline before Treatment, Mean Scores |
3 Mos Post-trt. |
6 Mos Post-trt. |
12 Mos Post-trt. |
18 Mos Post-trt. |
24 Mos Post-trt. |
60 Mos Intention- to-Treat |
60 Mos Treatment Received |
|---|---|---|---|---|---|---|---|---|
| Medical Management (MM) | ||||||||
| Number with data | n = 29 | n = 29 | n = 26 | n = 28 | n = 24 | n = 26 | n = 27 | n = 27 |
| Mean score and (SD) | 0.44 (0.16) | 0.31 (0.17) | 0.24 (0.16) | 0.19 (0.13) | 0.16 (0.11) | 0.19 (0.14) | 0.20 (0.17) | 0.20 (0.17) |
| Rehabilitation (NS) | ||||||||
| Number with data | n = 24 | n = 22 | n = 21 | n = 22 | n = 22 | n = 20 | n = 23 | n = 21 |
| Mean Score and (SD) | 0.45 (0.13) | 0.26 (0.12) | 0.23 (0.13) | 0.19 (0.14) | 0.19 (0.16) | 0.16 (0.15) | 0.20 (0.14) | 0.19 (0.14) |
| Arthroscopic Surgery (AS) | ||||||||
| Number with data | n = 25 | n = 23 | n = 21 | n = 23 | n = 20 | n = 22 | n = 24 | n = 22 |
| Mean Score and (SD) | 0.44 (0.12) | 0.25 (0.15) | 0.24 (0.13) | 0.23 (0.15) | 0.20 (0.16) | 0.23 (0.17) | 0.21 (0.15) | 0.22 (0.15) |
| Arthroplasty Surgery (AR) | ||||||||
| Number with data | n = 26 | n = 20 | n = 19 | n = 19 | n = 20 | n = 20 | n = 24 | n = 20 |
| Mean Score and (SD) | 0.44 (0.12) | 0.25 (0.12) | 0.22 (0.14) | 0.16 (0.08) | 0.19 (0.13) | 0.17 (0.10) | 0.23 (0.16) | 0.22 (0.15) |
| P-value for between-group difference | p = 0.99 | p = 0.33 | p = 0.95 | p = 0.37 | p = 0.79 | p = 0.50 | p = 0.86 | p = 0.92 |
| P-value for within-group improvement from baseline | NA | p < 0.0001 all groups |
p < 0.0001 all groups |
p < 0.0001 all groups |
p < 0.0001 all groups |
p < 0.0001 all groups |
p < 0.0001 all groups |
p < 0.0001 all groups |
Table 4.
Symptom Severity Index (SSI) for TMJ Pain (Observed Means and Standard Deviations by Treatment Group and Follow-up Interval)
| Treatment Groups | Baseline before Treatment, Mean Scores |
3 Mos Post-trt. |
6 Mos Post-trt. |
12 Mos Post-trt. |
18 Mos Post-trt. |
24 Mos Post-trt. |
60 Mos Intention- to-Treat |
60 Mos Treatment Received |
|---|---|---|---|---|---|---|---|---|
| Medical Management (MM) | ||||||||
| Number with data | n = 29 | n = 28 | n = 27 | n = 29 | n = 25 | n = 26 | n = 27 | n = 27 |
| Mean score and (SD) | 0.61 (0.23) | 0.33 (0.22) | 0.31 (0.20) | 0.28 (0.26) | 0.27 (0.21) | 0.21 (0.24) | 0.23 (0.25) | 0.23 (0.25) |
| Rehabilitation (NS) | ||||||||
| Number with data | n = 24 | n = 21 | n = 19 | n = 22 | n = 21 | n = 21 | n = 23 | n = 21 |
| Mean Score and (SD) | 0.72 (0.17) | 0.42 (0.27) | 0.34 (0.22) | 0.31 (0.24) | 0.29 (0.28) | 0.27 (0.23) | 0.23 (0.23) | 0.19 (0.21) |
| Arthroscopic Surgery (AS) | ||||||||
| Number with data | n = 26 | n = 22 | n = 22 | n = 21 | n = 19 | n = 22 | n = 24 | n = 21 |
| Mean Score and (SD) | 0.70 (0.19) | 0.34 (0.25) | 0.34 (0.22) | 0.30 (0.21) | 0.28 (0.22) | 0.25 (0.20) | 0.26 (0.20) | 0.29 (0.19) |
| Arthroplasty Surgery (AR) | ||||||||
| Number with data | n = 26 | n = 20 | n = 19 | n = 20 | n = 20 | n = 20 | n = 23 | n = 20 |
| Mean Score and (SD) | 0.76 (0.22) | 0.26 (0.24) | 0.19 (0.19) | 0.20 (0.22) | 0.26 (0.24) | 0.25 (0.24) | 0.28 (0.25) | 0.25 (0.21) |
| P-value for between-group difference | p = 0.06 | p = 0.23 | p = 0.083 | p = 0.37 | p = 0.97 | p = 0.86 | p = 0.83 | p = 0.50 |
| P-value for within-group improvement from baseline | NA | p < 0.0001 all groups |
p < 0.0001 all groups |
p < 0.0001 all groups |
p < 0.0001 all groups |
p < 0.0001 all groups |
p < 0.0001 all groups |
p < 0.0001 all groups |
Treatment compliance was inversely associated (p < 0.05) with SSI up to 18 mos but not later. The groups did not differ in compliance (p > 0.09); average compliance scores ranged from 1.1 for Rehabilitation to 1.7 for Medical Management. Adjustment for compliance did not produce group differences for CMI or SSI (p > 0.2). Groups differed in prescription medication use at 3 mos (p = 0.001), but not later. At 3 mos, proportions of participants requiring a prescription analgesic more than once weekly were 17/28 (61%), 2/21 (10%), 9/22 (23%), and 1/19 (5%) for Medical Management, Rehabilitation, Arthroscopy, and Arthroplasty, respectively. Numbers requiring muscle relaxants were 8/28 (29%) for Medical Management vs. 2/21 (10%), 0/22, and 0/19 for Rehabilitation, Arthroscopy, and Arthroplasty, respectively. Physical therapy visits averaged nine, seven, 12, and 16, respectively.
Each participant received the assigned initial treatment modality for at least 3 mos, after which some participants in each group needed additional interventions for persistent pain and reduced range of motion. Of 29 Medical Management participants, 12 received rehabilitation after 3 mos, and one received arthroscopy after 12 mos (total, 45% receiving a second modality). One Rehabilitation participant received arthroplasty after 6 mos. Two Arthroscopy participants and one Arthroplasty participant received repeat surgeries. One Arthroplasty participant experienced nerve injury that resolved completely.
DISCUSSION
The four treatment strategies did not differ in magnitude or timing of improved function or pain relief. Fifty-five percent of those initially treated with medical management alone had symptom resolution, consistent with natural history studies (Sato et al., 1997; Kurita et al., 1998). Just two of 52 Medical Management and Rehabilitation participants received surgery for persistent pain and restricted function.
An intervention study's generalizability derives from its treatments and its population. This effectiveness study compared treatment strategies defined by initial modality. The Medical Management group was not intended to simulate treatment with medical management alone; rather, it simulated a strategy beginning with medical management and using more invasive methods only if required. The study strategies matched clinical practice and are therefore generalizable.
Regarding the study population, the principal symptoms of closed lock are pain and limited opening. By these symptoms, our study population is comparable with closed-lock surgical groups in four other RCTs (Stegenga et al., 1993; Fridrich et al., 1996; Goudot et al., 2000; Holmlund et al., 2001). When the SSI's pain intensity scale was transformed to 0 to 10, mean baseline pain for this study's sample was 6.3, and mean maximum interincisal opening was 29.1 mm, compared with ranges of 5.6 to 7.1 and 27.6 to 30 mm in the other four studies.
Criteria for the closed-lock diagnosis included clinical and MRI evaluation, both having acceptable validity (Schiffman et al., 1989; Liedberg et al., 1996). For Arthroscopy and Arthroplasty participants, all diagnoses were confirmed during surgery.
We did not evaluate arthrocentesis, which was used infrequently when this study began. Two randomized trials have compared arthrocentesis and arthroscopic surgery for closed lock (Fridrich et al., 1996; Goudot et al., 2000). Pain reduction was similar for the two treatments, but the latter study found arthroscopic surgery superior for improving mouth opening. Finally, the present study cannot determine how individual modalities (self-care, medications, physical therapy, cognitive-behavioral therapy, splints, or surgery) contributed to a group's results.
This study provides a basis for advising closed-lock patients that, on average, short-term improvement with regard to pain and function, as measured at 3 mos, is similar for all four treatment strategies. Primary treatment for patients with closed lock should consist of medical management or rehabilitation. Within the context of this study, we were unable to detect any net benefit associated with surgery over that of medical management or rehabilitation at any follow-up period.
ACKNOWLEDGMENTS
We acknowledge Dr. Clyde Wilkes and, from the University of Minnesota, Pat Lenton, Amanda Jackson, Constance Bromaghim, Bruce Lindgren, and Drs. Gary Anderson, Jana Reinhart, and Greg Pelletier. This study was supported by NIH/NIDCR grants R29DEO8668, P30-DEO9737, N01-DE22635, and R01 DE13421-01, by HealthPartners of Minnesota, Allina, and by the University of Minnesota School of Dentistry.
APPENDIX
PARTICIPANTS
This study used strict and specific inclusion and exclusion criteria. Inclusion criteria included: (1) a definable time when the participants experienced an abrupt decrease in range-of-motion of the mandible, so that the chronicity of their condition could be determined; (2) a maximum active opening (incisor to incisor) equal to or less than 40 mm; and (3) pain in the affected joint with palpation, opening, and contralateral movements.
Exclusion criteria were assessed by history, beginning with systemic rheumatic diseases being ruled out. If the family history was positive for rheumatic diseases, or if the individual complained of generalized joint pain or stiffness in the joints, then laboratory studies were planned (CBC, electrolyte profile, ESR, and FANA), and had to be negative for the individual to be eligible for the study. No potential participant required this assessment. The Symptom Checklist (SCL-90R), a self-report questionnaire, screened for severe depression, anxiety, and other primary psychiatric illnesses, and normative scores were required for eligibility. Participants with controlled depression, taking antidepressant medications, and who had been on a steady maintenance dose for a minimum of 3 mos were eligible for this study. Controlled depression was defined by the patient's self-assessment as being currently normal, and a normative score for depression on the SCL-90R. For participants assigned to a treatment group involving a psychologist, this professional's evaluation was also considered in determining eligibility. If participants taking antidepressants did not fulfill these strict criteria, they were excluded. Primary craniofacial pain disorders other than closed lock were ruled out via history, examination, and MRIs of the entire head, including the TMJs. Pregnant women or those women desiring to become pregnant during the follow-up period were excluded due to the need for radiographs. If participants became pregnant prior to a follow-up appointment, then radiographic assessment was scheduled after the completion of the pregnancy.
EXAMINATION AND RANDOMIZATION
Sequential participants presenting to the clinicians involved in this study were asked to participate in the study if they: (1) met the above criteria, (2) had a presumed diagnosis of TMJ disc displacement without reduction, (3) had never had prior TMJ surgery, (4) had never been treated by any clinician involved in this study, and (5) agreed to be randomized to any treatment group. The clinician then suggested to all participants the use of over-the-counter aspirin, non-steroidal anti-inflammatory drugs (NSAIDs), or acetaminophen, soft diet, and home use of ice or heat to help control symptoms. Participants were referred to the Hennepin County Medical Center for bilateral TMJ tomography and bilateral MRI studies. If the MRI study was not sufficiently diagnostic, then TMJ arthrotomography was performed on the side with the presumed pathology. The latter was needed only once in this study sample.
At the conclusion of imaging, the participants returned to the evaluating clinician, the diagnosis of closed lock was confirmed, and all options were discussed with the participant based on a pre-determined script. If the participant agreed to the study, s/he was referred to the study coordinator at the University of Minnesota Clinical Dental Research Center for a complete discussion of all the details of the study, including the informed consent process. The consenting participants completed the study questionnaires, received a complete clinical examination, and were randomized to one of the four treatment groups, based on a concealed randomization schedule prepared by the study epidemiologist. The randomization had two strata defined by duration of decreased opening: “Non-chronic”, for durations under 6 mos, and “Chronic” for all others. Participants were then given copies of their TMJ MRIs and tomograms, and were referred to their assigned doctor for initiation of their randomly allocated treatment.
INTERVENTIONS
Medical Management
Those assigned to the medical management group saw only one clinician (ELS) 1 time per mo for 1/2 hr during 6 mos. This clinician provided education about the participant's condition and optimistic counseling about his/her prognosis, gave the participant prescription medications, and implemented a self-help program. Prescription medications offered included anti-inflammatories and muscle relaxants. The anti-inflammatories were initially a Medrol® dose pack for 6 days, followed typically with ibuprofen (800 mg), the latter to be used initially 3 times per day after meals. If the individual stated a preference for another type of prescription anti-inflammatory medication, that was allowed. Prescription muscle relaxants (diazepam, methocarbamol, cyclobenzaprine, or clonazepam) were used initially at bedtime to help reduce nocturnal muscle activity, again honoring any participant's preference. Medication use was monitored at monthly meetings between the participant and the doctor. The stated goal for all participants was to eliminate all prescription medications within a maximum of 2 mos or sooner, based on whether the medications either were not effective or were no longer needed for pain control. Over-the-counter anti-inflammatories were allowed as needed. Participants were also formally taught a self-help protocol by their doctor, with a standardized information sheet that they were given. This protocol included the use of self-applied heat or cold, a pain-free diet with bilateral chewing, and reminders that the tongue should be kept at the top of the mouth with the teeth apart and the muscles relaxed, and that they refrain from biting on lips, cheeks, or other anatomical structures, from biting on objects, from resting the jaw on the hand, and from sleeping on the stomach.
The rehabilitation group and both surgical treatment groups were given optimistic counseling about their prognosis and the same options for prescription and over-the-counter medications as the medical management group. The same self-help techniques used for medical management were implemented in the other three groups by the behavioral psychologist, and were reviewed and reinforced by the treating doctor.
Rehabilitation
Rehabilitation included splint therapy, physical therapy, cognitive-behavioral therapy, and medical management (Fricton et al., 1987). All participants assigned to the rehabilitation group were further randomized to one of two dental clinicians (ELS and JRF). All participants randomized to rehabilitation had the following: (1) The dentist implemented and monitored the medical management (the prescription medications) and inserted and adjusted a splint; (2) the registered physical therapists implemented and monitored the physical therapy rehabilitation, including a home exercise program; and (3) the licensed clinical psychologists ruled out significant psychopathology, evaluated for psychosocial and behavioral factors, and implemented and monitored all aspects of the cognitive-behavioral therapy, including the self-help techniques mentioned above, and oral habit-reversal techniques. All of these interventions were performed at the TMJ and Orofacial Pain Clinic at the University of Minnesota. With the exception of the assigned surgeries, all interventions for the Arthroscopy and Arthroplasty groups and the follow-up intervals were standardized and matched to the Rehabilitation group with regard to contact time with dentists, the extent of active physical therapy, and instruction on home exercises via the physical therapists, and the extent of cognitive-behavioral intervention with the behavioral psychologists.
Splint Therapy
All splint therapy was provided by one of the two dental clinicians. The dentist adjusted the passive, flat-plane splint in persons in both reclined and sitting positions, to create bilateral contacts on all posterior teeth with light to no contact on canines and incisors in the habitual closure position. Anterior guidance was maintained during protrusion and canine guidance during laterotrusion. A mandibular splint was used unless the individual was missing maxillary posterior teeth, in which case a maxillary splint was inserted and adjusted to the same parameters. The participants were instructed to use this splint as needed during the day and at bedtime, not to use it for eating, and to remove it during oral hygiene. If a participant stated that using the flat-plane splint was associated with his/her jaw being uncomfortable or painful, but having the mandible anterior to this position was comfortable, and if this position was no further than the edge-to-edge incisor position, then a mandibular orthopedic repositioning splint was fabricated for the maxillary teeth (Anderson et al., 1985). This latter splint was used only at bedtime so as not to result in any irreversible change in the maxillary/mandibular relation. Less than 5% of the participants received the latter splint. Regardless of the type of splint used, follow-up visits for splint adjustments were initially scheduled one time per mo for 6 mos as part of the 6 monthly follow-up visits with the dentist. After the sixth mo, the next planned visit was 3 mos later. If, at that time, the splint needed no significant adjustment, the individual was seen 6 mos later, and if, again, no significant adjustment was needed, the individual was then seen on an “as-needed” basis or yearly recall, whichever was less. At any time, the individual could return if he/she perceived a need for adjustment. The individual could also discontinue using the splint at any time if no differences were noted in symptoms when the splint was not used.
Physical Therapy
All evaluations and treatments for physical therapy were done by two physical therapists (Karen Decker, PT and Connie Bromaghim, PT) following published guidelines (Braun, 1987; Uriell et al., 1989; Seaton and Iglarsh, 1990). All those in the rehabilitation, arthroscopy, or arthroplasty groups were seen by the physical therapist for a one-hour initial evaluation. For the surgical groups, the initial evaluation was done pre-surgically. In all cases, the initial visit included a complete history of the participant's past and present head, jaw, and neck problem(s), including any past treatments, current pain complaints, and functional limitations. This was followed by an objective examination that included TMJ and cervical range of motion, quality of movement, strength testing, muscle palpation, and postural evaluation.
After the physical therapist's evaluation, a treatment plan was developed with specific goals, including decreased pain, increased function for both eating and talking, improved pain-free active range of motion (AROM) of the mandible, and improved relaxation. Specifically, short-term goals were to control inflammation and pain, and long-term goals were to achieve a functional TMJ AROM of 40 mm of incisal opening and 7 mm of lateral excursion, as well as incisal end-to-end protrusion. Once the goals were explained to the participant, he/she was scheduled for one-half hour in the clinic 3 times per wk for 4 wks for active and passive treatments with the physical therapist. Physical therapy interventions for those in the surgical groups followed post-surgical guidelines, and scheduled appointments started the first day after surgery (Rocabado, 1989; Uriel et al., 1989). During the active treatment phase, a home exercise program was initiated to rehabilitate the head, jaw, and neck musculature and to improve posture. These exercises were reviewed at subsequent visits and were modified as necessary. Modalities and the sequencing of modalities varied according to the subjective and objective findings assessed before each treatment. The overall physical therapy intervention was outcome-based, so when pain control and a functional AROM of the mandible were achieved, active treatment was discontinued. The participants were instructed to perform home exercises 6 times per day for 6 mos and daily thereafter.
The initial physical therapy treatment depended on the individual's initial presentation. For those in the surgical groups, it was modified relative to their presentation on the first day after surgery. Those with acute inflammation were instructed in the use of cold packs and short-arc mobility exercises to be done frequently at home. Modalities used to reduce inflammation were iontophoresis, pulsed ultrasound, cold packs, and electrical stimulation. Regardless of group assignment, each participant had to present with decreased pain, decreased erythema, decreased edema, and decreased hyperthermia before the emphasis of treatment shifted to increasing the functional mobility. At this stage, the active treatments included ultrasound and hot packs to increase extensibility of the soft tissues in preparation for joint mobilization techniques. Mobilization techniques were used to increase the AROM, promote relaxation, and improve circulation. Electrical stimulation and cold packs were used to decrease muscle spasm and control pain as needed. Exercise was introduced at this stage to promote and improve coordination, strength, flexibility, and muscle re-education. These exercises included Rocabado's 6 × 6 exercises and a variety of active, active-assisted, and passive stretching of the muscles of mastication (Seeton and Iglarsh, 1990). The 6 × 6 exercises required 5 min to perform, and were initially to be done 6 times per day. While regaining the TMJ AROM, participants were also encouraged to use hot packs and stretching exercises 2-4 times per day. Participants were given instructions in self-care, joint protection, and relaxation.
After the planned four-week active treatment, the participants continued to see the same physical therapist for a monthly half-hour follow-up visit up to the sixth month. At these visits, the physical therapist reviewed exercises, reviewed compliance with the exercises, and reviewed the participant's ability to control symptoms. After the sixth month, participants were instructed to continue their exercises indefinitely at least once per day; they were also seen as needed. In summary, physical therapy for this study was outcome-based, with an emphasis on a home exercise program. Therapeutic intervention by the therapist was utilized, first, to reduce inflammation and, second, to increase functional mobility for eating and speaking. Every effort was made to rehabilitate the jaw within the participant's pain tolerance, and to restore function with the individual's compliance. Thus, the goal was to increase AROM and function within the individual's pain tolerance, while avoiding inflammation. Care was taken to provide, to each participant, a standardized physical therapy program that could be modified to meet that individual's needs.
Cognitive-behavioral Therapy
All evaluations and treatments for therapy were done by one of three, doctoral-level, licensed psychologists with specialty training in health psychology: Drs. Kate Hathaway, Greg Pelletier, and Jana Reinhart. All surgical patients had the first behavior therapy visit prior to surgery. Behavioral and psychological screening and intervention involved a standardized four-fold process:
(1) Evaluation for serious emotional disturbances that might interfere with successful treatment. This included psychological disorders defined by the Diagnostic and Statistical Manual IV, such as substance abuse, schizophrenia, or other psychotic disorders, and untreated mood or anxiety disorders (if evident at baseline, the individual was ineligible for the study; two persons were excluded due to uncontrolled depression);
(2) Screening for oral habits such as clenching/bruxing, biting lips or fingernails, leaning on chin, tongue or jaw thrusting, and gum or hard/chewy candy use. Clinicians also evaluated for postural habits, such as sleeping on the stomach, and maladaptive lifestyle habits, such as high levels of caffeine consumption, low levels of general physical exercise, or poor nutrition that could potentially contribute to orofacial pain, and for motivation-compliance levels.
(3) Implementation of self-help techniques, used also for medical management, such as eating a softer diet, applying moist heat, avoiding gum chewing, and avoiding other behaviors that stress jaw muscles and joints, such as bruxism.
(4) Implementation of cognitive-behavioral treatment and habit-reversal strategies for oral and maladaptive lifestyle habits. This included brief education about techniques for management of jaw pain, individual goal-setting, and optimistic counseling. During the first one-hour visit, participants were introduced to oral habit change techniques and were taught orofacial muscle relaxation (TONGUE UP, TEETH APART, MUSCLES RELAXED). The next two one-hour appointments involved in-depth cognitive-behavioral treatments designed to reduce oral habits, such as clenching, and to increase orofacial muscle relaxation. Techniques included: (a) didactic education regarding the relationship among oral habits, muscle strain, and discomfort; (b) information regarding the various roles of physical therapy, splint therapy, and oral habit change; (c) training in habit-reversal techniques (Hathaway, 1997), including instruction in orofacial muscle relaxation and self-monitoring techniques [Habit reversal had four goals: (1) to increase an individual's awareness of a behavior such as clenching, (2) to interrupt the chain of behaviors involved in the habit as soon as possible, (3) to teach the participant a behavior incompatible with the maladaptive habit (jaw relaxation), and (4) to eliminate reinforcement for the behavior (Azrin and Nunn, 1973).]; (d) assignment of home exercises to practice orofacial muscle relaxation and monitor oral habits per above [Participants were encouraged to monitor the tension in their jaw muscles, using structured and individualized prompts, and were told to practice the “mini-relaxation” of the jaw for 15-20 sec 3 or 4 times hourly.]; and (e) implementation of health education and cognitive-behavioral techniques to address maladaptive lifestyle habits (e.g., reduce caffeine and/or alcohol consumption, increase general exercise routines, improve nutrition and regularity of eating), address self-efficacy, and improve compliance. This intervention is similar to the stress management component of treatment described previously (Rudy et al., 1995).
Study participants were not routinely instructed in general relaxation techniques. Following this brief behavior therapy (3 sessions, 1 mo apart), progressive muscle relaxation or stress management was implemented only if the participant continued to report significant difficulties implementing orofacial relaxation, or if s/he complained of general body tension, and/or challenges with pain management. This happened in less than 5% of the participants. Instruction in relaxation techniques usually included both Progressive Muscle Relaxation (Jacobson, 1948) and Guided Imagery. An audio tape was made in the session, and appropriate instructions for practice were provided.
Surgery
Both the arthroscopic and the arthroplasty (disc plication or removal) surgeries were done in combination with physical therapy, cognitive-behavioral therapy, and medical management, with splint therapy as needed. Before surgery, all surgical patients were seen one time by (1) the physical therapist, (2) the behavioral psychologist, and (3) the surgeon. Individuals were evaluated as to the indications for the planned surgical procedure. They underwent medical history procurement and physical evaluation, and they had to be able to tolerate general anesthetic of short duration. After surgery, all those in both surgical groups had physical therapy and behavioral therapy interventions identical overall, in time and content, to those of the rehabilitation group. Also, all patients were followed up by their surgeon once per month for 6 mos (the same as the follow-ups for the rehabilitation participants). The planned surgical patients' interventions were therefore identical with regard to content and timing relative to those of the rehabilitation participants, with one exception: An orthotic (splint) was used post-operatively only if the surgeon, physical therapist, health psychologist, or the patient believed that it was needed (see the criteria for a post-operative splint below).
Arthroscopy
All those assigned to the arthroscopic surgery group were further randomized to one of two oral and maxillofacial surgeons (JQS or RBT), according to a standardized surgical procedure consistent with a technique reported previously (Moses and Poker, 1989). The patients were taken to the operating room after a pre-operative evaluation by the Department of Anesthesiology, and were placed in a supine position on the operating table. None of the patients was given pre-medication that would affect the outcome of the procedure. General anesthesia was administered and modified for each individual, according to the purview of the anesthesiologist in charge. The type of anesthesia administered has never been shown to influence surgical outcome. Nasoendotracheal intubation was performed. The surgical site was prepared with Betadine soap and solution in the area of temporomandibular joint arthroscopy puncture. The patient was then appropriately draped for the procedure.
While the patient was affected by the muscle relaxant administered for the purpose of endotracheal intubation, the maximum inter-incisal opening was measured, recorded, and compared with the measurement obtained from the pre-surgical visit. No patient's maximum inter-incisal opening was seen to be significantly altered by the general anesthesia or the muscle relaxant, thus confirming that the reduced range of motion was due not to muscle guarding secondary to pain, but rather to actual mechanical obstruction. This clinical examination ensured that the clinical findings in the anesthetized patients corresponded with the findings from the pre-surgical imaging.
The surgical assistant manipulated the patient's jaw by placing his or her hand in the oral cavity and moving the lower jaw. The superior joint space was injected with 1 cc of 0.5% bupivacaine. The superior joint space was then infused with 4-6 cc of heparinized lactated Ringer's solution via the same needle puncture. The needle was then removed, and the superior joint space was entered with a cannula and trocar (Dyonics™, Smith and Nephew Endoscopy, Andover, MA, USA). The cannula was inserted to a depth of approximately 12 mm, until a puncturing through the temporomandibular joint capsule into the superior joint space was felt. A blunt trocar was then used to replace the sharp trocar, to facilitate further entry to approximately 20-25 mm, and the joint space was backwashed with heparinized lactated Ringer's solution to clear the joint space of debris and blood. The temporomandibular joint arthroscope (1.7 mm in diameter) (Dyonics™), connected to the appropriate light source and video camera, was inserted into the cannula. Positive entry into the superior joint space was noted, and the superior joint space was briefly examined. If there was a need for an outflow port for irrigation of the joint space, this outflow was accomplished with an 18-gauge short beveled needle placed by puncture through the skin inferior and anterior to the cannula puncture, and entering the superior joint space. The joint space was evaluated, and findings were recorded on videotape. After adequate evaluation, the trocar was removed, and the blunt trocar was replaced into the cannula. Lysis of adhesions was then performed with a trocar sweep of the superior joint space, with particular attention to the lateral capsular attachment to the disc. The joint space was again backwashed, and the arthroscopic cannula and outflow port were removed. One milliliter of betamethasone (i.e., 6 mg) was placed intra-articularly. The mandible was then moved passively through its full range of motion, to ensure the success of the procedure, and the patient was awakened from general anesthesia to be taken to the recovery area.
The technical difficulty of surgical arthroscopy was ascertained by the number of punctures required to enter the superior joint space and the amount of time required for the procedure. Sutures were not used in the surgical arthroscopy. All surgical start and finish times were recorded as per standard operating room protocol. Procedures were recorded via the standard operation dictation and placed in the patient's chart. All arthroscopic procedures were videotaped. Additionally, at least 4 views of the joint anatomy were recorded onto a color printer, and the prints were kept in the patient's chart. These records serve as evidence of adherence to surgical protocol and demonstration of temporomandibular joint pathology. Post-operatively, the patient was discharged from the hospital when fully recovered from the general anesthesia. This immediate discharge from the post-anesthesia recovery area is common in most applications of arthroscopy.
The patients were seen post-operatively by the surgeon performing the arthroscopy, with the first follow-up in 1 wk. The patient was then seen approximately once a month by the surgeon for 6 mos, and then annually. If there were any concerns by the physical therapist or the patient, more frequent or immediate follow-up evaluations were performed.
Arthroplasty
Patients received open-joint surgery under general anesthesia. All arthroplasties were performed by a single oral surgeon (Clyde Wilkes DDS, MD). A disc-repositioning procedure (discoplasty) was attempted whenever possible. If the surgeon judged, during surgery, that the case was too advanced and the joint tissues too degenerated, a disc removal procedure (discectomy) was performed, with necessary joint debridement and hard-tissue recontouring. Prior to surgery, no patient's maximum inter-incisal opening was found to be altered by the general anesthesia or the muscle relaxant, thus verifying that the reduced range of motion was due not to muscle guarding secondary to pain, but rather to actual mechanical obstruction.
The surgical protocol was standardized according to previously established procedures (Wilkes, 1991). The surgical joint was opened according to specifications, and the disc was determined to be dislocated anteriorly. The stretched posterior attachment was then re-sected, redundant tissue was removed, and the disc was manipulated and repositioned to its presumed correct position. Anterior release was usually necessary and involved release of the anterior attachment of the disc and/or partial myotomy of the superior head of the lateral pterygoid, to reposition the disc in a posterior direction without tension. This was accomplished with small sharp blades or a Holmium Laser (Lumenus, Santa Clara, CA, USA). A bilaminar repair was then carried out in the posterior attachment region, with continuous locking and/or multiple ties of non-absorbable suture and tieback suture from the lateral capsule to the posterior edge of the disc. Sutures used were either 4-0 Mersilene® (Ethicon, Inc, Somerville, NJ, USA) or 5-0 Nylon. The repair was tested with full forward excursions, and the disc was observed to move correctly with the condyle head. Adhesion barriers (i.e., gelfilm) were placed in the anterior and posterior recesses. The wound was then closed in layers as previously described.
Discectomy procedures were utilized when a repositioning repair procedure was either inappropriate or impossible. The discectomy procedure consisted of resecting anterior, posterior, lateral, and medial attachments of the disc and removing the disc. Bleeding was controlled with electrocautery and the Holmium Laser, and/or by direct small sutures consisting of interrupted 5-0 Vicryl. The wound was then closed in layers.
No intra-articular steroids were used with the arthroplasty procedures. We emphasize that all patients were given careful post-operative instructions, to avoid overload of the operated joint. Patients were seen at approximately 1 wk post-operatively, and then on a monthly basis for the first 6 mos, and then annually.
The decision as to whether an individual should have unilateral or bilateral TMJ surgery, in either surgical group, was determined by the treating surgeon, based on pre-surgical symptoms, signs, and MRI/tomography findings, and in consultation with the patient. Contralateral TMJ surgery was performed if the individual had a positive current history of symptoms and signs of TMJ involvement, and an MRI diagnosis of TMJ disc displacement for the contralateral joint. If the individual had a positive current history of symptoms and signs, but the MRI diagnosis showed a normal disc position for the contralateral joint, the contralateral TMJ surgery was not performed. Unilateral TMJ surgery was also planned if the individual had a negative current history of symptoms for the contralateral joint. If contralateral surgery was required, it was an arthroscopic surgery for those in the arthroscopic group and an open-joint procedure for those in the repair group. There were 15 bilateral and 8 unilateral arthroscopies, and 13 bilateral and 8 unilateral arthroplasties. In all, 34 joints received arthroplasty, with 24 discoplasties and 10 discectomies.
Treatment modalities provided to Medical Management participants were extended to the other groups; the surgical groups also received post-operative narcotics. Surgical patients saw the physical therapist, psychologist, and surgeon once after randomization but before surgery. Post-operatively, Arthroscopy and Arthroplasty patients saw the same physical therapists and psychologists and received the same treatments as the Rehabilitation participants.
The criteria specified for surgical patients to receive a splint post-operatively were that the individual: (1) reported pain upon awakening, (2) noted that s/he was clenching or grinding his/her teeth at any time during the day or night, (3) noticed any other oral habit(s), (4) had a significant post-operative skeletal malocclusion (either anterior or posterior open bite), or (5) desired to have a splint. The need for a splint in the surgical group could be determined by the surgeon, the physical therapist, the psychologist, and/or the patient. This decision was made after the options were discussed with the patient at either the pre- or post-surgical visit. The need for a splint was typically decided pre-surgically, and the splint was then inserted post-operatively as soon as the patient could tolerate opening the mouth long enough to have the splint adjusted properly (usually within 1 wk of surgery). The type and use of a post-operative splint were identical to those described in the Splint Therapy section above for rehabilitation, with one exception: if the person had a posterior open bite following arthroplasty. In this situation, a maxillary orthotic with an anterior bite-plate design (Dahlström and Haraldson, 1985) was used until the posterior teeth came into contact, after which this splint was changed to a flat-plane design. In all cases, the splint treatment was performed by one clinician (ELS). Follow-up visits for splint adjustments were limited to only the time it took to adjust the splint. Splint adjustment was initially once per month until the splint no longer needed adjustment (usually 3 mos). The patient was then seen 3 mos later and, if no significant adjustment was needed, then 6 mos later, and finally on an “as needed” basis or yearly recall, whichever was less. The individual could discontinue using the splint at any time when its use no longer made any difference in the symptoms. All but two of the Arthroscopy and five of the Arthroplasty surgical patients received splints post-surgically.
OBJECTIVES FOR ALL FOUR TREATMENT STRATEGIES
General guidelines of the program expected for all participants included:
(1) elimination of all prescription medication for pain;
(2) reduction of pain behaviors, including verbalization of pain and avoidance of tasks due to pain; and
(3) restoration of normal work and home activity.
Education of the participant to ensure proper understanding and compliance was emphasized from the beginning with all participants. Regardless of whether a participant was assigned to Rehabilitation, Arthroscopy, or Arthroplasty, s/he was seen for follow-up by the surgeon or dentist (once per month for 6 mos), the physical therapist (4 wks of active treatment, then once per month for 6 mos total), and the psychologist (3 behavior therapy sessions one month apart, followed by any additional sessions needed).
The three objectives for all interventions included:
(1) reduction of joint pain and associated myalgia, at rest and with function;
(2) improvement in the range of motion of the mandible without deviation; and
(3) reduction in the need for future health care for the problem.
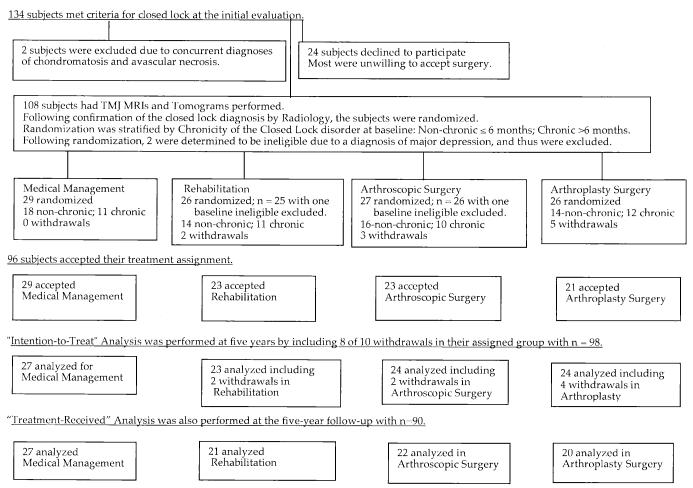
Appendix Figure.
Flow of participants through each stage of the randomized clinical trial.
APPENDIX REFERENCES
- Anderson GC, Schulte JK, Goodkind RJ. Comparative study of two treatment methods for internal derangement of the temporomandibular joint. J Prosthet Dent. 1985;53:392–397. doi: 10.1016/0022-3913(85)90520-7. [DOI] [PubMed] [Google Scholar]
- Azrin NH, Nunn RG. Habit-reversal: a method of eliminating nervous habits and tics. Behav Res Ther. 1973;11:619–628. doi: 10.1016/0005-7967(73)90119-8. [DOI] [PubMed] [Google Scholar]
- Braun BL. The effect of physical therapy intervention on incisal opening after temporomandibular joint surgery. Oral Surg Oral Med Oral Pathol. 1987;64:544–548. doi: 10.1016/0030-4220(87)90030-2. [DOI] [PubMed] [Google Scholar]
- Dahlström L, Haraldson T. Bite plates and stabilization splints in mandibular dysfunction. A clinical and electromyographic comparison. Acta Odontol Scand. 1985;43:109–114. doi: 10.3109/00016358509046495. [DOI] [PubMed] [Google Scholar]
- Fricton JR, Hathaway KM, Bromaghim C. Interdisciplinary management of patients with TMJ and craniofacial pain: characteristics and outcome. J Craniomandib Disord. 1987;1:115–122. [PubMed] [Google Scholar]
- Hathaway KM. Evaluation and management of maladaptive behaviors and psychological issues in temporomandibular disorder patients. Dent Clin North Am. 1997;41:341–354. [PubMed] [Google Scholar]
- Jacobson E. Progressive relaxation: a physiological and clinical investigation of muscular states and their significance in psychology and medical practice. The University of Chicago Press; Chicago: 1948. [Google Scholar]
- Moses JJ, Poker ID. TMJ arthroscopic surgery: an analysis of 237 patients. J Oral Maxillofac Surg. 1989;47:790–794. doi: 10.1016/s0278-2391(89)80035-7. [DOI] [PubMed] [Google Scholar]
- Rocabado M. Physical therapy for the postsurgical TMJ patient. J Craniomandib Disord. 1989;3:75–82. [PubMed] [Google Scholar]
- Rudy TE, Turk DC, Kubinski JA, Zaki HS. Differential treatment responses of TMD patients as a function of psychological characteristics. Pain. 1995;61:103–112. doi: 10.1016/0304-3959(94)00151-4. [DOI] [PubMed] [Google Scholar]
- Seaton MR, Iglarsh ZA. The musculoskeletal approach to maxillofacial pain. Lippincott; Philadelphia: 1990. [Google Scholar]
- Uriell P, Bertolucci L, Swaffer C. Physical therapy in the postoperative management of temporomandibular joint arthroscopic surgery. J Cranio. 1989;7:27–32. doi: 10.1080/08869634.1989.11678265. [DOI] [PubMed] [Google Scholar]
- Wilkes CH. Surgical treatment of internal derangements of the temporomandibular joint. A long-term study. Arch Otolaryngol Head Neck Surg. 1991;117:64–72. doi: 10.1001/archotol.1991.01870130070019. [DOI] [PubMed] [Google Scholar]
Footnotes
A supplemental appendix to this article is published electronically only at http://www.dentalresearch.org.
REFERENCES
- Derogatis LR. SCL-90-R: administration, scoring and procedures manual-II for the revised version. Clinical Psychometric Research; Towson, MD: 1992. [Google Scholar]
- Dimitroulis G. The role of surgery in the management of disorders of the temporomandibular joint: a critical review of the literature. Int J Oral Maxillofac Surg. 2005;34(Part 2):231–237. doi: 10.1016/j.ijom.2004.06.006. [DOI] [PubMed] [Google Scholar]
- Drangsholt M, LeResche L. In: Temporomandibular disorder pain. In: Epidemiology of pain. Crombie IK, Croft PR, Linton SJ, LeResche L, Von Korff M, editors. IASP Press; Seattle: 1999. pp. 203–233. [Google Scholar]
- Fricton JR. Musculoskeletal measures of orofacial pain. Anesth Prog. 1990;37:136–143. [PMC free article] [PubMed] [Google Scholar]
- Fricton JR, Schiffman EL. Reliability of a craniomandibular index. J Dent Res. 1986;65:1359–1364. doi: 10.1177/00220345860650111701. [DOI] [PubMed] [Google Scholar]
- Fricton JR, Schiffman EL. The craniomandibular index: validity. J Prosthet Dent. 1987;58:222–228. doi: 10.1016/0022-3913(87)90181-8. [DOI] [PubMed] [Google Scholar]
- Fricton JR, Hathaway KM, Bromaghim C. Interdisciplinary management of patients with TMJ and craniofacial pain: characteristics and outcome. J Craniomandib Disord. 1987a;1:115–122. [PubMed] [Google Scholar]
- Fricton JR, Nelson A, Monsein M. IMPATH: microcomputer assessment of behavioral and psychosocial factors in craniomandibular disorders. Cranio. 1987b;5:372–381. doi: 10.1080/08869634.1987.11678214. [DOI] [PubMed] [Google Scholar]
- Fricton JR, Look JO, Schiffman E, Swift J. Long-term study of temporomandibular joint surgery with alloplastic implants compared with nonimplant surgery and nonsurgical rehabilitation for painful temporomandibular joint disc displacement. J Oral Maxillofac Surg. 2002;60:1400–1411. doi: 10.1053/joms.2002.36091. [DOI] [PubMed] [Google Scholar]
- Fridrich KL, Wise JM, Zeitler DL. Prospective comparison of arthroscopy and arthrocentesis for temporomandibular joint disorders. J Oral Maxillofac Surg. 1996;54:816–820. doi: 10.1016/s0278-2391(96)90526-1. [DOI] [PubMed] [Google Scholar]
- Goudot P, Jaquinet AR, Hugonnet S, Haefliger W, Richter M. Improvement of pain and function after arthroscopy and arthrocentesis of the temporomandibular joint: a comparative study. J CranioMaxillofac Surg. 2000;28:39–43. doi: 10.1054/jcms.1999.0103. [DOI] [PubMed] [Google Scholar]
- Holmlund AB, Axelsson S, Gynther GW. A comparison of discectomy and arthroscopic lysis and lavage for the treatment of chronic closed lock of the temporomandibular joint: a randomized outcome study. J Oral Maxillofac Surg. 2001;59:972–977. doi: 10.1053/joms.2001.25818. [DOI] [PubMed] [Google Scholar]
- Kropmans JB, Dijkstra PU, Stegenga B, de Bont LG. Therapeutic outcome assessment in permanent temporomandibular joint disc displacement. J Oral Rehabil. 1999;26:357–363. doi: 10.1046/j.1365-2842.1999.00417.x. [DOI] [PubMed] [Google Scholar]
- Kurita K, Westesson PL, Yuasa H, Toyama M, Machida J, Ogi N. Natural course of untreated symptomatic temporomandibular joint disc displacement without reduction. J Dent Res. 1998;77:361–365. doi: 10.1177/00220345980770020401. [DOI] [PubMed] [Google Scholar]
- LeResche L. Research diagnostic criteria for temporomandibular disorders. In: Fricton JR, Dubner R, editors. Orofacial pain and temporomandibular disorders. Raven Press; New York: 1995. pp. 189–203. [Google Scholar]
- Liedberg J, Panmekiate A, Petersson A, Rohlin M. Evidence-based evaluation of three imaging methods for the temporomandibular disc. Dentomaxillofac Radiol. 1996;25:234–241. doi: 10.1259/dmfr.25.5.9161176. [DOI] [PubMed] [Google Scholar]
- Mercuri LG, Laskin DM. Indications for surgical treatment of internal derangements of the temporomandibular joint. Current controversies in surgery for internal derangements of the temporomandibular joint/Indications for surgical treatment of internal derangements of the TMJ. Oral Maxillofac Surg Clin North Am. 1994;6(2):223–226. [Google Scholar]
- Minakuchi H, Kuboki T, Matsuka Y, Maekawa K, Yatani H, Yamashita A. Randomized controlled evaluation of treatments for temporomandibular joint anterior disk displacement without reduction. J Dent Res. 2001;80:924–928. doi: 10.1177/00220345010800031501. [DOI] [PubMed] [Google Scholar]
- Moses JJ, Poker ID. TMJ arthroscopic surgery: an analysis of 237 patients. J Oral Maxillofac Surg. 1989;47:790–794. doi: 10.1016/s0278-2391(89)80035-7. [DOI] [PubMed] [Google Scholar]
- Sato S, Goto S, Kawamura H, Motegi K. The natural course of nonreducing disc displacement of the TMJ: relationship of clinical findings at initial visit to outcome after 12 months without treatment. J Orofac Pain. 1997;11:315–320. [PubMed] [Google Scholar]
- Schiffman E, Anderson G, Fricton J, Burton K, Schellhas K. Diagnostic criteria for intraarticular TM disorders. Community Dent Oral Epidemiol. 1989;17:252–257. doi: 10.1111/j.1600-0528.1989.tb00628.x. [DOI] [PubMed] [Google Scholar]
- Schiffman EL, Fricton JR, Haley DP, Shapiro BL. The prevalence and treatment needs of subjects with temporomandibular disorders. J Am Dent Assoc. 1990;120:295–303. doi: 10.14219/jada.archive.1990.0059. [DOI] [PubMed] [Google Scholar]
- Shaefer JR, Jackson DL, Schiffman EL, Anderson QN. Pressure-pain thresholds and MRI effusions in TMJ arthralgia. J Dent Res. 2001;80:1935–1939. doi: 10.1177/00220345010800101401. [DOI] [PubMed] [Google Scholar]
- Stegenga B, de Bont LG, Dijkstra PU, Boering G. Short-term outcome of arthroscopic surgery of temporomandibular joint osteoarthrosis and internal derangement: a randomized controlled clinical trial. Br J Oral Maxillofac Surg. 1993;31:3–14. doi: 10.1016/0266-4356(93)90089-f. [DOI] [PubMed] [Google Scholar]
- Turk DC, Rudy TE, Sorkin BA. Neglected topics in chronic pain treatment outcome studies: determination of success. Pain. 1993;53:3–16. doi: 10.1016/0304-3959(93)90049-U. [DOI] [PubMed] [Google Scholar]
- Wilkes CH. Internal derangements of the temporomandibular joint. Pathological variations. Arch Otolaryngol Head Neck Surg. 1989;115:469–477. doi: 10.1001/archotol.1989.01860280067019. [DOI] [PubMed] [Google Scholar]
- Wilkes CH. Surgical treatment of internal derangements of the temporomandibular joint. A long-term Study. Arch Otolaryngol Head Neck Surg. 1991;117:64–72. doi: 10.1001/archotol.1991.01870130070019. [DOI] [PubMed] [Google Scholar]
- Wright EF, Schiffman EL. Treatment alternatives for patients with masticatory myofascial pain. J Am Dent Assoc. 1995;125:1030–1039. doi: 10.14219/jada.archive.1995.0281. [DOI] [PubMed] [Google Scholar]
- Wright E, Anderson G, Schulte J. A randomized clinical trial of intraoral soft splints and palliative treatment for masticatory muscle pain. J Orofac Pain. 1995;9:192–199. [PubMed] [Google Scholar]
- Wright EF, Domenech MA, Fischer JR., Jr Usefulness of posture training for patients with temporomandibular disorders. J Am Dent Assoc. 2000;131:202–210. doi: 10.14219/jada.archive.2000.0148. [DOI] [PubMed] [Google Scholar]