Abstract
OBJECTIVE
To investigate whether patients’ expectations influence how they take their medications by looking at the expectations patients have of their medications and the factors that affect these expectations.
DESIGN
Qualitative study using in-depth interviews and a grounded-theory approach.
SETTING
A large city in Ontario.
PARTICIPANTS
A total of 18 community-dwelling adult patients taking medication for at least 6 months.
METHOD
Both purposive and convenience sampling techniques were used. The initial strategy comprised stratified, maximum variation, and typical case sampling. The research team developed a semistructured interview guide after a preliminary review of the literature. Individual, face-to-face, in-depth interviews were conducted and audiotaped. At the end of the interviews, basic demographic information was collected. Interviewers were debriefed following each interview and their comments on relevant contextual information, general impressions of the interview, and possible changes to the interview guide were audiotaped. Audiotapes of each interview, including the debriefing, were transcribed verbatim, cleaned, and given a unique identifying number. At least 2 team members participated in analyzing the data using an operational code book that was modified to accommodate emerging themes as analysis continued.
MAIN FINDINGS
Patients’ expectations were more realistic than idealistic. Many participants acted on their expectations by changing their medication regimens on their own or by seeking additional information on their medications. Expectations were affected by patients’ beliefs, past experiences with medications, relationships with their health care providers, other people’s beliefs, and the cost of medication. Patients actively engaged in strategies to confirm or modify their expectations of their medications.
CONCLUSION
A range of factors (most notably past experiences with medications and relationships with health care providers) influenced patients’ expectations of their medications. More comprehensive discussion between patients and their health care providers about these factors could affect whether medications are used optimally.
RÉSUMÉ
OBJECTIF
Examiner les attentes des patients concernant leur médication et les facteurs qui influencent ces attentes, et déterminer si cela influence leur utilisation des médicaments.
TYPE D’ÉTUDE
Étude qualitative utilisant des entrevues en profondeur et une méthode de théorie à base empirique.
CONTEXTE
Une grande ville d’Ontario.
PARTICIPANTS
Un total de 18 patients adultes vivant dans la communauté et prenant une médication depuis au moins 6 mois.
MÉTHODE
On a utilisé à la fois des techniques d’échantillonnage au jugé et de commodité. La stratégie initiale comprenait un échantillonnage de cas typiques, stratifiés et à variation maximale. Après une revue de la littérature, l’équipe de recherche a élaboré un guide d’entrevue semi-structurée. Des entrevues en profondeur individuelles en tête-à-tête ont été effectuées et enregistrées sur ruban magnétique. À la fin des entrevues, on a recueilli les données démographiques basales. Après chaque entrevue, l’interviewer faisait un compte-rendu, et ses commentaires sur l’information contextuelle pertinente, son impression générale de l’entrevue et les changements pouvant être apportés au guide d’entrevueétaient enregistrés sur bande sonore. Les enregistrements de chaque entrevue, y compris le compte-rendu final, ont été transcrits mot à mot, épurés et identifiés par un numéro unique. Au moins 2 membres de l’équipe ont participé à l’analyse des données à l’aide d’un manuel d’instruction modifié pour s’ajuster aux nouveaux thèmes à mesure que l’analyse progressait.
PRINCIPALES OBSERVATIONS
Les attentes des patients étaient plus réalistes qu’idéalistes. Plusieurs donnaient suite à leurs attentes en modifiant eux-mêmes la prise des médicaments ou en s’informant davantage sur leur médication. Les attentes des patients étaient influencées par leurs croyances, leur expérience des médicaments, leur relation avec le personnel soignant, les croyances d’autres personnes et le coût des médicaments. Les patients ont adopté des stratégies pour confirmer ou modifier leurs attentes concernant leur médication.
CONCLUSION
Divers facteurs (plus particulièrement leur expérience avec les médicaments et leur relation avec le personnel soignant) influencent les attentes des patients quant à leurs médicaments. Une discussion plus élaborée entre le patient et le personnel soignant au sujet de ces facteurs pourrait améliorer l’utilisation de la médication.
Several studies have established that medications are not always used optimally1–6 and that the medication prescribing and use system is multifaceted and complex.7 Although many health problems can be linked to the fact that medication prescribing practices are not standardized, these problems have also been attributed to underuse of medications, poor adherence to medication regimens, or lack of monitoring once medications are prescribed.7–10 Evaluation of prescription claims data shows that patients’ persistence with medications for chronic illnesses, such as antihypertensives,11 osteoporosis medications,12 oral diabetic medications,13 and antilipidemics,14–16 is poor. There is an obvious disconnect between prescribers’ intent to use medications to improve health outcomes and patients’ decisions on whether to continue taking their medications once their prescriptions have been dispensed.
Given the aging population and an increased focus on optimal medication prescribing and use practices, it is important to ascertain the factors that affect use of medications. In most clinical situations, patients make the final decision about whether they start or continue taking a medication. This decision is at least as complex as the assessments physicians, pharmacists, and other health care providers make when choosing or monitoring the effects of medications for patients. We set out to further explore patients’ perspectives on this issue.
Within the literature on use of medications, one underexplored area is patients’ expectations of their medications. An expectation, defined as “a thing that is expected to happen,”17 is likely to be an important contributor to decisions health care providers and patients make about whether to prescribe or use a medication. Disagreement between health care providers’ and patients’ expectations of medications could lead to inconsistent implementation of a medication-use plan and result in unintended adverse drug events or unrealized health benefits for patients. The aim of this study was to explain the influence of patients’ expectations on their use of medications.
METHODS
Design
This study used qualitative research methods, and a grounded-theory approach was used to develop a model of factors linking patients’ expectations of medications with their behaviour regarding taking medications.18,19 The main research questions addressed in this study were as follows: what expectations do patients have of their medications and what factors influence patients’ expectations of their medications. This study received ethics approval from the St Joseph’s Healthcare Hamilton Research Ethics Board.
Study sample
Both purposive and convenience sampling were used. The initial sampling strategy consisted of stratified, maximum variation, and typical case sampling.18 An attempt was made to include patients who represented various age groups, who were taking a range of medications, and who had varying living arrangements (eg, living alone or living with others). We recognized that patients’ expectations would vary based on these factors.20,21
Participants were community-dwelling adults 18 years old and older who had been taking at least 1 medication for 6 months or longer and who had not been receiving formal assistance with their medications (eg, home care). Participants were recruited through notices posted in local newspapers, on hospital bulletin boards, in pharmacies, and in hospital volunteer offices, as well as through personal appeals to 4 local family doctors, of whom 2 provided patient contacts. Interviews continued until saturation was reached and no additional information was forthcoming.22
Data collection
Individual, face-to-face, in-depth interviews were conducted with each study participant. The research team developed a semistructured interview guide after a preliminary review of the literature. The guide was modified as interviews progressed to accommodate emerging themes. The interview began by asking patients for an inventory of all the medications they currently took. Patients were then asked to identify the 2 medications they would classify as their most important medications, and these were used to help participants orient their responses to the questions asked. At the end of each interview, basic demographic information, such as age, living arrangements, and level of education, was collected. After each interview, the interviewers completed a debriefing to discuss relevant contextual information, general impressions of the interview, and possible changes to the interview guide. These debriefings were audiotaped and became part of each transcript. Audiotapes of each interview, including the debriefing, were transcribed verbatim, cleaned, and given a unique identifying number. All the interviews were conducted by one researcher (K.N.) with another researcher (L.D. or C.S.) in attendance at some interviews.
Data analysis
Verbatim statements from transcripts and field notes were coded using an open coding process19 to identify common themes or categories. An operational code book was developed to guide analysis. Each transcript was coded independently by at least 2 members of the research team, using the code book. QSR NUD*IST, version 4,23 was used to retrieve and organize the data. Through axial coding,19 we developed a theoretical model that linked conditions thought to affect both patients’ expectations of medications and responses to conditions arising from use of medications. This model followed Strauss and Corbin’s description of grounded-theory model components: a central phenomenon (main focus of the study that emerges after coding), causal conditions (how the central phenomenon came about), strategies, intervening factors, contextual factors, and consequences.19 Strategies are ways of attending to the central phenomenon, and consequences are the effects of engaging in the strategies. Intervening and contextual factors are conditions that influence the strategies. Using theoretical sampling (ie, sampling so that data contributes to categories in an emerging theoretical model), we regularly assessed all components of the model to ensure the data had adequate depth and density.19 Both the code book and the model were updated regularly in an iterative fashion using information from each interview.
Rigour of the study
We used several methods to try to ensure the study was rigorous and trustworthy.18,24 Audiotaped and written verbatim versions of the interviews were compared to ensure accuracy and completeness of data. Debriefing and field notes were maintained and reviewed by team members. Member checking (sending written summaries of each interview to participants for their comments) was done to ensure we had interpreted their statements accurately. Triangulation was achieved through regular team meetings to discuss issues related to data collection and analysis. Finally, an audit trail or copies of all materials used to collect and analyse the data, as well as the analytical products, was maintained.
FINDINGS
Characteristics of the 18 study participants are shown in Table 1. More than half the participants (61%) were women. Mean age was 58.1 years (standard deviation = 18.7). The mean number of medications taken was 7.5 (standard deviation = 5.2). Nine respondents (50%) were taking cardiac medications, 8 (44%) were taking psychiatric medications, and 11 (61%) were taking medications for arthritis or other nonspecific pain. The 2 medications patients identified as their most important are listed in Table 2.
Table 1.
Demographic characteristics of participants
| CHARACTERISTIC | N (%)* |
|---|---|
| Women | 11 (61) |
| No. of medications taken† | |
| • 0–4 | 5 (28) |
| • 5–9 | 8 (44) |
| • ≥ 10 | 5 (28) |
| Marital status | |
| • Single | 6 (33) |
| • Divorced | 1 (6) |
| • Married | 5 (28) |
| • Widowed | 4 (22) |
| • Common law | 2 (11) |
| No. in household | |
| • 1 | 10 (56) |
| • 2 | 4 (22) |
| • 3 | 3 (17) |
| • 4 | 0 (0) |
| • 5 | 1 (6) |
| Occupation | |
| • Student | 1 (6) |
| • Working | 4 (22) |
| • On disability | 5 (28) |
| • Retired | 8 (44) |
| Highest level of education | |
| • High school | 8 (44) |
| • College | 4 (22) |
| • University undergraduate degree | 5 (28) |
| • University graduate degree | 1 (6) |
| Income ($) | |
| • 0–19 999 | 4 (22) |
| • 20 000–39 999 | 8 (44) |
| • 40 000–59 999 | 3 (17) |
| • 60 000–100 000 | 2 (11) |
| • Unknown | 1 (6) |
| Language spoken as a child | |
| • English | 16 (89) |
| • French | 1 (6) |
| • Prussian | 1 (6) |
| Religion | |
| • Christian | 16 (89) |
| • None | 2 (11) |
| • Other | 0 (0) |
Proportions might not add to 100% owing to rounding.
Includes both prescribed medications and those initiated by patients.
Table 2.
Most important medications named by each respondent
| PATIENT ID | AGE (Y) | MOST IMPORTANT MEDICATIONS |
|---|---|---|
| A011 | 58 | Isosorbide dinitrate and verapamil |
| B042 | 72 | Nitroglycerin and ASA |
| B051 | 33 | Birth control pills and ketorolac |
| B062 | 74 | Atenolol, hydrochlorothiazide, nitroglycerin spray, and ASA |
| B071 | 79 | Etidronate, both inhalers (salbutamol, beclomethasone), and ASA |
| B081 | 48 | Interferon β 1b; all others equally important |
| B091 | 37 | Valproic acid and antidepressants |
| B101 | 72 | Heart medication, but not sure as it was stopped |
| B111 | 24 | Birth control pills and antidepressants (both equally important) |
| B121 | 82 | Levothyroxine and hypertension medication |
| B132 | 84 | Amlodipine, isosorbide dinitrate, and ASA |
| B142 | 83 | Diabetic medications (metformin and glyburide) |
| B151 | 55 | Antidepressants and clonazepam |
| B162 | 42 | Acetaminophen (Tylenol No. 3) |
| B172 | 46 | Fluoxetine and clonazepam |
| B182 | 50 | Atorvastatin and enalapril |
| B191 | 62 | Moclobemide and domperidone |
| B201 | 44 | Levothyroxine and budesonide |
ASA—acetylsalicylic acid.
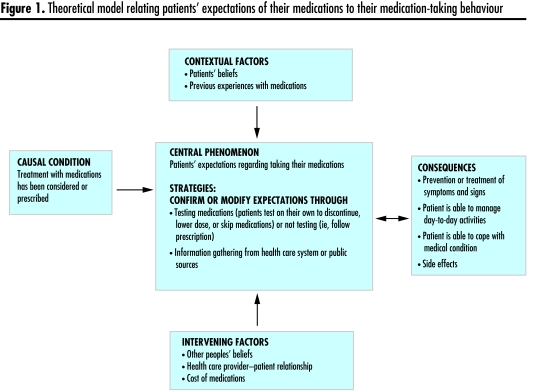
A theoretical model, using standard grounded-theory components, was developed to show the linkages between patients’ expectations of their medications and their behaviour regarding taking medications (Figure 1). This model centred on patients’ expectations and the strategies through which they arrived at them (eg, discontinuing medications on their own, lowering doses or skipping medications, or confirming their expectations by gathering information from health care system or public sources). The degree to which patients acted as a result of their expectations of their medications was influenced by various contextual and intervening factors. Each of these components is described below, and it should be noted that there is some overlap between components in this model. For clarity in presentation, each component is described separately. Where quotes are noted, participants’ ID numbers followed by text unit numbers are provided in parentheses.
Figure 1.
Theoretical model relating patients’ expectations of their medications to their medication-taking behaviour
Central phenomenon
The central phenomenon was patients’ expectations of their medications. These expectations were generally more realistic than idealistic. For example, most patients were not expecting their medications to be “miracle cures” but instead viewed them as one element that could help improve their medical conditions and daily lives. Patients’ expectations of their medications were primarily expressed in terms of testing out medications or validating them by gathering information on them.
Although many patients followed their physicians’ directions for taking medications, others tested their medications in various ways. Patients reporting testing medications on their own by discontinuing them, lowering doses, increasing doses, or skipping doses. This testing seemed to indicate an active response on patients’ part to try to maintain their health in a manner that worked for them, as the following quotes suggest:
I tried stopping everything [all medications]. Then in a couple of weeks, I knew I couldn’t stop the hypertension medicine because I could feel the effects of that. I don’t get a headache unless my pressure is up … and I was getting them again. So when I told my doctor [he said], “Oh, my goodness. You mustn’t stop that one.” And then when I went off the other, Synthroid, [he said], “Oh, you can’t stop that.” So those were the 2 that I went back on. (B121–242)
He [the doctor] said it wasn’t a strong enough dose and he was going to recommend either a higher dose or to go back to cisapride. So I had increased the dose myself. He was going to call, or somebody was going to call, but I hadn’t heard from him. So I’ve gone ahead because I wanted to be able to eat without discomfort. (B191–80)
Another manifestation of patients’ expectations of their medications (mentioned by 8 of 18 respondents) related to a lack of information on their medications. Patients often sought to confirm their expectations of what a medication could or could not do by seeking information from the health care system or public sources. In some cases, patients thought their physicians withheld information about side effects because they did not want patients to experience them. Yet patients expressed a desire to be more informed so that they would be able to develop accurate expectations of their medications. As one participant explained,
Not all patients are ignorant in the true sense of the word. I want to be told side effects and interactions and troubles or problems. I really want to understand things. (B201–160)
Physicians do not always tell us about side effects because they think people will think they have them. (B201–208)
Patients wanting information used several strategies to find it. For some patients, adverse events spurred them to seek out further information. Others gradually recognized that they could ask questions and get information as they continued to live with their medical conditions. Participants used a variety of information sources, such as doctors, pharmacists, the Internet, the library, and friends. Of particular note were positive comments about pharmacists and their accessibility with regard to information.
I never realized how important pharmacists were because I never needed medication. But now I realize how very, very informed and very knowledgeable [they are] and [they] can be extremely helpful and supportive. (B191–362)
The doctor I have now will give me 2 versions. He’ll give me the quick simple …. If I’m not satisfied with number 1, then he gets into the real meat. So I like that about him. (B162–155)
The library, the Internet, the pharmacy, and lastly the doctors. I either trust the doctor or change doctors. But I also want to know more about the medication than they know. They’re not experts in the millions of drugs that are out there, so it pays to look it up and say, “Oh yeah, I’m having a side effect.” The Internet has a lot of garbage on it, but it has some good information [too]. (B172–91)
Consequences
Four main consequences resulted from patients following medication-use plans that aligned with their expectations of the medications: the medications prevented or treated symptoms or signs, patients’ ability to manage day-to-day activities improved, patients’ ability to cope with their medical conditions improved, and patients experienced side effects. Almost all participants talked about how their medications affected the symptoms or signs of their medical conditions. In some cases, this included slowing the progression of disease or alleviating the severity of symptoms: “Well, I expect them to do the job which the doctor says that I need. It does to a degree, I would imagine. It stops a heart attack, and it does bring my blood pressure down.” (B132–78)
For most people, medications were seen as a way to help manage life and conduct daily activities. Some participants also noted that taking their medications led to an improvement in health that also allowed them to do things that otherwise they might not have been able to do: “It allows me to do those things which I want to do, such as go on a vacation, or take a trip up to the northland, or go over to the seniors’ club, play some cards, or what have you. And [it] allows me to sit and do my carvings and … play music.” (B132–70)
For some patients, taking medications was seen as a way to cope with their medical conditions. Though somewhat related to the first expectation of prevention or treatment of symptoms and signs, some participants went on to comment further about how this allowed them to cope with their health concerns. This highlighted the emotional toll some medical conditions take on patients and the value patients ascribe to medications: “I think a lot of people don’t realize that it’s necessary to take a lot of medication. Sometimes, they [others] think, I think they think you take it because you’re not doing something else, you have an alternative, you could do something else. It is annoying, there’s no doubt. There are times when I say, ‘I’d like not to take it. Stick around and I’ll show you what will happen if I don’t.’” (A011–259)
Some patients were able to describe specifically what they wanted their medications to do. They were looking for a particular, tangible outcome from their medications (eg, reduce exacerbations of multiple sclerosis or alleviate depression). Not surprisingly, this was more evident among participants whose medical conditions greatly affected their daily lives: “They [medications] allow me to be on an equivalent level to other people. They allow me to handle things a bit better. For the first time in my life, I’m not at the mercy of my moods, and I’m not in the depths of depression, which is worth a million to me.” (B091–127)
Most respondents (15/18) reported some type of physical or emotional symptom that they thought was a side effect of medication and indicated that such experiences influenced their expectations of medications. Some adverse effects were tolerable, some were not: “[the medication] created heartburn so bad I thought I was dying” (B121–21); and “Side effects were as bad as the depression itself.” (B111–126) Some adverse effects were tolerated no matter how severe they were because participants knew they would eventually become comfortable with them or they thought that treating their medical conditions necessitated continuing the medication. Some side effects were considered a long-term concern that could give rise to problems in the future. Most physical signs and symptoms reported were systemic, usually related to the central nervous or gastrointestinal systems.
Some respondents discussed unexpected adverse effects. Participants who had these typically had not been informed about them or had not realized that adverse effects might occur, sometimes because they had too much information to process when they were ill. This situation seemed to heighten their emotional reactions to the situation: “This narcotic that I take for the pain, I didn’t ask [the pharmacist about it]. I ended up after taking one, (thinking), ‘Good God! What’s the matter with me?’ I felt it’s nauseating and almost disoriented.” (A011–219)
Contextual factors
Contextual factors are specific factors that influence the central phenomenon in a grounded-theory model. In this study, there were 2 main contextual factors associated with patients themselves that influenced their expectations of their medications: their beliefs about medications and their previous experiences with medications.
Patients’ beliefs
Participants mentioned 3 main beliefs about medications: taking medication is not optional if I want to live (or live well), medications allow me to take control over my own health, and it is important to question the need for medication. For most patients, taking their medications was seen as necessary if they were to maintain their current level of health and as not really optional:
Good grief! Eight pills for supper, wonderful! [sarcastic tone] But then I look at it the other way and I say, “Well, without those 8 pills, I can’t go for a walk, I can’t do the shopping.” You’re grateful in many ways that the medications are there. (A011–155)
The birth control pill makes it so that I can sort of function in society. Without it, it gets to a point where the frequency of changing a feminine hygiene product would interfere with class or work. So, again, it’s something that sort of keeps me a member of society. (B111–81)
The way in which medications affected patients’ control over their health also influenced their expectations of their medications. Some respondents noted that medications gave them control over their health; others thought that the act of taking medications took away control over their health. Perceptions about control over health affected whether patients expected medications to promote or reduce their chances of having good health. Some people described having to adapt their lives to their medications if they were taking a lot of medications or had many health problems. Others had incorporated taking medication into their lives so that they could still do everything they wanted to do: “I think it makes you feel somehow in control, because the medication can take control of your life very easily. And it’s not pleasant to feel that these bottles of pills determine where I’m going and what I’m going to do today.” (A011–163)
Although taking medications was associated with the concept of taking control over health, very few participants thought taking medications was unduly onerous.
Beliefs regarding the need for medications varied. Most participants valued their medications and identified a clear need for them, but some believed that they should not take too many medications or any medications at all. This typically resulted from a perception that prescription medications are not needed to improve health and that alternative medications are a better choice. For others, there simply seemed to be an artificial threshold that reflected an optimal number of medications. Overall, beliefs about taking medications seemed to reflect a feeling that taking fewer medications was better than taking more medications: “I wasn’t brought up like that, to take medication …. No, I was brought up to be as normal, as natural.” (B121–157)
Previous experiences with medications
Participants spoke of both positive and negative experiences with medications. Those who had positive experiences described how their medications had helped them and how this served as a reinforcement to continue taking them. Negative experiences sometimes caused patients to alter their approach to taking medications. Those who had side effects that they considered severe or serious often thought they had to deal with them on their own as they were not getting enough support from their health care providers or the health care system. Negative experiences shaped their expectations of what might happen to them in the future if they took the same or new medications. Most participants perceived that taking medications was an act of balancing benefits and risks: “I’m realistic. I think there are going to be some long-term side effects from taking the medication. What they are worries me a little bit, but I’ve resigned myself to the fact that I have to take those 2 [medications], that I expect to have side effects from [them]. I don’t want to have an asthma attack and end up in emergency, and without the thyroid medication, I would be really sick.” (B201–50)
Intervening factors
Intervening factors are a broader set of circumstances that affect the central phenomenon. Participants discussed 3 main intervening factors: other peoples’ beliefs about medications, their relationships with their health care providers, and the cost of medications.
Other people’s beliefs
A few patients talked about how other people’s beliefs and reactions affected their expectations and use of medications. In some cases, people had been prompted to start taking a medication on the suggestion of another person. One person taking alternative medications noted, “I really have no reason for taking them other than my mom said they would be great.” (B051–329) Two participants felt stigmatized by taking prescription medications. They thought they had a choice when it came to taking medications. One participant noted, “I feel stigma because I’ve had people say, ‘You really don’t need medication because you can control it yourself.’” (B091–103)
Another patient was taking 10 medications a day and told us how people close to her questioned whether taking so many medications was really necessary, the implication being that, if she just “tried harder,” she could rid herself of a supposed dependence on prescription medications. This patient very powerfully described how these views affected her life:
They [friends, family] used to hurt my feelings. They used to make me think that maybe I am taking too much medication, maybe I could cope with less. I try not to justify it any more. I try more just to say “Well, without it I can’t function.” It gets tense. They make you feel very, very, somehow inadequate, somehow less than everyone else. But unfortunately, [medication] carries a stigma with it. It takes a long time to get past that with so much medication. (A011–267)
Relationships with health care providers
Having a good relationship with a health care provider was an important indicator of whether respondents would discuss their need for information or their adverse effects with their health professionals. Some spoke of an almost adversarial or disconnected relationship with their physicians. Examples included thinking that the physician did not spend enough time with them, did not communicate well with them, did not listen well to them, and did not behave as if the relationship were a partnership. In most cases, participants’ experiences were related to relationships with their physicians or pharmacists rather than with other practitioners:
Well, I must say my physician that I have now is much more open. We talk about things. I told her I want a partnership .... I like this very much as an option [compared] to the old way of “I’m prescribing this, this is for you, you take this.” But it also puts responsibility on you. You have to be responsible if you’ve chosen something. And sometimes if you’re not feeling very well it puts you in a bind because you have trouble making decisions, so that’s tricky too. I guess, in a case like that, I would say, “I’m really not up to making a decision at this time. I would like you to make it and we can review it at a later time.” (B191–381)
Cost of medications
For many patients (13/18), the cost of a medication influenced whether they would actually take it. Several people noted problems with government insurance coverage of medications. They mentioned the length of time they had to wait before getting coverage and the high cost of paying for medications themselves in the interim. One respondent had recently declared bankruptcy owing to the high cost of medication. Having a drug plan was appreciated by those fortunate enough to have one. For others, it was important that costs be discussed at the time of prescribing. In most cases, patients were willing to handle the financial burden and administrative hassles because they expected the benefits of treatment to offset the difficulties involved in procuring medication: “I told her [the doctor] that I didn’t have one [drug plan], so she gave me a couple of inhalers to test. You just pay for it. You have to make that choice. I was fine with the pharmacist I usually deal with, and um, he let me wait till payday one time to pay for it.” (B201–65)
DISCUSSION
This study found that patients’ expectations of their medications are grounded in the reality of their experiences, beliefs, and health care or social situations rather than in idealistic ideas or beliefs. A preliminary model demonstrated that patients’ expectations were manifested through activities that helped them confirm or modify their belief that their medications were working as hoped. Such activities included testing the effectiveness of medications by independently discontinuing them, changing doses, or skipping medications, and by gathering information about medications from health care system or public sources.
An unanticipated finding in this study was discovering the extent to which many participants acted on their expectations without seeking the advice of their health care providers. For example, some changed their medication regimens before talking to a doctor or pharmacist after independently assessing how the medications seemed to help or harm their health. Patients’ independence was also discernable in their search for information about medications (eg, information on benefits and risks) that could confirm their preliminary expectations.
The patients in this sample used numerous sources of information to understand better what they could expect from their medications. Patients who thought they were not informed about a medication before taking it and then experienced side effects were dissatisfied that they had not been given enough information before initiating therapy. These negative experiences led to negative expectations (ie, patients thought they were more likely to experience side effects) of new medications. On the other hand, some patients expected that the medications they were prescribed were going to benefit them and so they did not as often act independently of the health care system to test their medications or seek more information about their therapy.
Many participants thought they lacked information or access to a reliable source of information about their medications. These patients likely made risk-benefit assessments without full knowledge of the medications’ known risk-benefit profiles. This finding is corroborated by numerous studies demonstrating that patients need more information about their medications.25–28 Despite this need for more information, participants easily identified their important medications, which were those that considerably decreased mortality and morbidity, prevented substantially undesirable outcomes (eg, seizures, unwanted pregnancy), or reduced or prevented debilitating symptoms.
Patients’ beliefs and other contextual factors that influenced their behaviour regarding taking medications were consistent with other theories that explain patients’ behaviour, such as the Health Belief Model,29 the Planned Behaviour theory,30 and the work of Horne and colleagues on beliefs about medications.31–33 The work of Horne and colleagues in particular reinforces the importance of examining how beliefs affect whether patients think they need a medication. The finding that use of medication is related to control over health is consistent with the findings of studies on what medications mean to people with epilepsy34 or schizophrenia.35 Some respondents in this study, however, believed instead that taking medications took away their control over their health. Thus, patients’ beliefs about how medications affect their control over their health could influence their expectations of their medications in many ways and might result in their independently testing medications or seeking more information about medications.
The literature has also documented the fact that patients test or make changes to their medication regimens. Dowell and Hudson found that patients often test medications before fully accepting the need for them.36 Benson and Britten found that patients who thought they were experiencing unwelcome effects from their medications adjusted them themselves to address the situation.37 Better communication between patients and health care providers could help patients be more engaged in monitoring their progress on therapy, be able to identify medication-induced adverse effects more effectively, feel more fully informed about the therapy they are receiving, and better understand why medications are prescribed (especially for medications that treat conditions that have no symptoms, such as hypertension or hyperlipidemia). Awareness of patients’ expectations can also help physicians, pharmacists, and other health care providers to identify and discuss situations where patients’ expectations are different from their own. This could help reduce gaps in information about drugs and make better plans for monitoring. It is also possible that, as physicians and patients discuss their expectations, physicians’ prescribing would become more aligned with particular patients’ needs. Britten and colleagues’ work has highlighted the need for physician-patient communication about medications and the need for a conscious recognition of the expectations that each brings to medication prescribing and use.38,39
Another notable finding was the mention of stigma related to medication use. Although only described by 2 participants, this finding highlights an emotional burden that influences expectations of medications and medication taking. Further research into how patients conceptualize and experience stigma around taking medications would add to the literature.
Limitations
Study participants were volunteers and thus could reflect people who want to have or have had more involvement in decisions about health care, who think they can take on more responsibility for their health themselves, or who are in some other way atypical of usual community-based adults taking medications long-term. Participants were purposefully sampled, however, to include patients with a range of diseases who were taking a variety of medications so that the study would benefit from gathering diverse ideas and thoughts.
Conclusion
A range of factors (most notably past experiences with medications and relationships with health care providers) influenced patients’ expectations of their medications. Increased discussion between patients and their health care providers about these factors could ultimately affect whether medications are used optimally.
Acknowledgment
This study was funded through grants from the Father Sean O’Sullivan Research Centre, St Joseph’s Healthcare, and the McMaster University Research and Aging Program in Hamilton, Ont. We thank the patients who gave their time to share their experiences with us
EDITOR’S KEY POINTS
Why do some patients take their medication as prescribed while others choose not to? In this qualitative study, 18 community-dwelling adults were asked about their expectations of their medications and about the factors that influenced those expectations.
Although a range of factors (eg, cost, beliefs about medications) affect patients’ expectations of their medications, past medication experiences and relationships with health care providers were very influential.
Many participants changed their medication regimens on their own or sought additional information about the drugs they were prescribed.
Talking with patients about what influences their decisions about use of medications could affect whether these medications are used optimally.
POINTS DE REPÈRE DU RÉDACTEUR
Pourquoi certains patients prennent-ils leur médication telle que prescrite alors que d’autres ne le font pas? Dans cette étude qualitative, on a demandé à 18 adultes vivant dans leur milieu naturel d’indiquer leurs attentes par rapport à leur médication et les facteurs qui influencent ces attentes.
Même si divers facteurs influencent les attentes relatives à la médication (par ex. coût, croyances au sujet de la médication), les expériences antérieures du patient avec les médicaments et la relation qu’il entretient avec l’équipe soignante avaient beaucoup d’importance.
Plusieurs patients ont changé d’eux-mêmes la façon de prendre leurs médicaments ou ont cherché des informations additionnelles sur ceux qu’on leur avait prescrits.
Discuter avec le patient de ce qui influence sa décision concernant la prise des médicaments pourrait favoriser une prise optimale de ces médicaments.
Footnotes
Contributors
Dr Dolovich, Ms Sellors, and Dr Levine conceived and designed the study. Dr Dolovich, Ms Sellors, Ms Nair, and Ms Lee were involved in data collection. Dr Lohfeld provided methodologic expertise and guided analysis of the data. Dr Dolovich, Ms Sellors, Ms Nair, Ms Lee, and Dr Lohfeld analyzed the data. Dr Dolovich drafted the article and Ms Sellors and Ms Nair provided initial feedback and revisions. All the authors had input into the manuscript at various stages, and all the authors gave their approval to the final version submitted.
Competing interests
None declared
This article has been peer reviewed.
References
- 1.Kephart G, Sketris I, Smith M, Maheu A, Brown M. Coprescribing of nonsteroidal anti-inflammatory drugs and cytoprotective and antiulcer drugs in Nova Scotia’s senior population. Clin Ther. 1995;17(6):1159–73. doi: 10.1016/0149-2918(95)80095-6. [DOI] [PubMed] [Google Scholar]
- 2.Antani MR, Beyth RJ, Covinsky KE, Anderson PA, Miller DG, Cebul RD, et al. Failure to prescribe warfarin to patients with nonrheumatic atrial fibrillation. J Gen Intern Med. 1996;11(12):713–20. doi: 10.1007/BF02598984. [DOI] [PubMed] [Google Scholar]
- 3.Hanlon JT, Fillenbaum GG, Schmader KE, Kuchibhatla M, Horner RD. Inappropriate drug use among community-dwelling elderly. Pharmacotherapy. 2000;20(5):575–82. doi: 10.1592/phco.20.6.575.35163. [DOI] [PubMed] [Google Scholar]
- 4.Piecoro LT, Browning SR, Prince TS, Ranz TT, Scutchfield FD. A database analysis of potentially inappropriate drug use in an elderly medicaid population. Pharmacotherapy. 2000;20(2):221–8. doi: 10.1592/phco.20.3.221.34779. [DOI] [PubMed] [Google Scholar]
- 5.Rochon PA, Anderson GM, Tu JV, Clark JP, Gurwitz JH, Szalai JP, et al. Use of beta-blocker therapy in older patients after acute myocardial infarction in Ontario. CMAJ. 1999;161(11):1403–8. [PMC free article] [PubMed] [Google Scholar]
- 6.Rochon PA, Gurwitz JH. Prescribing for seniors: neither too much nor too little. JAMA. 1999;282(2):113–5. doi: 10.1001/jama.282.2.113. [DOI] [PubMed] [Google Scholar]
- 7.Leape LL, Bates DW, Cullen DJ, Cooper J, Demonaco HJ, Gallivan T, et al. Systems analysis of adverse drug events. ADE Prevention Study Group. JAMA. 1995;274(1):35–43. [PubMed] [Google Scholar]
- 8.Bates DW, Cullen DJ, Laird N, Petersen LA, Small SD, Servi D, et al. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group. JAMA. 1995;274(1):29–34. [PubMed] [Google Scholar]
- 9.Bergman U, Wiholm BE. Drug-related problems causing admission to a medical clinic. Eur J Clin Pharmacol. 1981;20(3):193–200. doi: 10.1007/BF00544597. [DOI] [PubMed] [Google Scholar]
- 10.Einarson TR. Drug-related hospital admissions. Ann Pharmacother. 1993;27(7–8):832–40. doi: 10.1177/106002809302700702. [DOI] [PubMed] [Google Scholar]
- 11.Caro JJ, Salas M, Speckman JL, Raggio G, Jackson JD. Persistence with treatment for hypertension in actual practice. CMAJ. 1999;160(1):31–7. [PMC free article] [PubMed] [Google Scholar]
- 12.Papaioannou A, Ioannidis G, Adachi JD, Sebaldt RJ, Ferko N, Puglia M, et al. Adherence to bisphosphonates and hormone replacement therapy in a tertiary care setting of patients in the CANDOO database. Osteoporosis Int. 2003;14(10):808–13. doi: 10.1007/s00198-003-1431-2. [DOI] [PubMed] [Google Scholar]
- 13.Catalan VS, Couture JA, LeLorier J. Predictors of persistence of use of the novel antidiabetic agent acarbose. Arch Intern Med. 2001;161(8):1106–12. doi: 10.1001/archinte.161.8.1106. [DOI] [PubMed] [Google Scholar]
- 14.Avorn J, Monette J, Lacour A, Bohn RL, Monane M, Mogun H, et al. Persistence of useof lipid-lowering medications:a cross-national study. JAMA. 1998;279(18):1458–62. doi: 10.1001/jama.279.18.1458. [DOI] [PubMed] [Google Scholar]
- 15.Benner JS, Glynn RJ, Mogun H, Neumann PJ, Weinstein MC, Avorn J. Long-term persistence in use of statin therapy in elderly patients. JAMA. 2002;288(4):455–61. doi: 10.1001/jama.288.4.455. [DOI] [PubMed] [Google Scholar]
- 16.Jackevicius CA, Mamdani M, Tu JV. Adherence with statin therapy in elderly patients with and without acute coronary syndromes. JAMA. 2002;288(4):462–7. doi: 10.1001/jama.288.4.462. [DOI] [PubMed] [Google Scholar]
- 17.Oxford paperback dictionary. 3. Oxford, UK: Oxford University Press; 1998. [Google Scholar]
- 18.Creswell JW. Qualitative inquiry and research design: choosing among five traditions. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 19.Strauss A, Corbin J. Basics of qualitative research: techniques and procedures for developing grounded theory. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 20.Koecheler JA, Abramowitz PW, Swim SE, Daniels CE. Indicators for the selection of ambulatory patients who warrant pharmacist monitoring. Am J Hosp Pharm. 1989;46(4):729–32. [PubMed] [Google Scholar]
- 21.Ellis SL, Billups SJ, Malone DC, Carter BL, Covey D, Mason B, et al. Types of interventions made by clinical pharmacists in the IMPROVE study. Impact of Managed Pharmaceutical Care on Resource Utilization and Outcomes in Veterans Affairs Medical Centers. Pharmacotherapy. 2000;20(4):429–35. doi: 10.1592/phco.20.5.429.35055. [DOI] [PubMed] [Google Scholar]
- 22.Willms D, Johnson NA. Essentials in qualitative research: a notebook for the field. Hamilton, ON: McMaster University Department of Anthropology; 1999. [Google Scholar]
- 23.Qualitative Solutions and Research Pty Ltd. QSR NUD*IST. Cambridge, MA: Qualitative Solutions and Research Pty Ltd; 1997. [Google Scholar]
- 24.Lincoln YS, Guba EG. Naturalistic inquiry. Newbury Park, CA: Sage; 1985. [Google Scholar]
- 25.Wiederholt JB, Clarridge BR, Svarstad BL. Verbal consultation regarding prescription drugs: findings from a statewide study. Med Care. 1992;30(2):159–73. doi: 10.1097/00005650-199202000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Berry DC, Michas IC, Gillie T, Forster M. What do patients want to know about their medicines and what do doctors want to tell. Psychol Health. 1997;12:467–80. [Google Scholar]
- 27.Chelf JH, Agre P, Axelrod A, Cheney L, Cole DD, Conrad K, et al. Cancer-related patient education: an overview of the last decade of evaluation and research. Oncol Nurs Forum. 2001;28(7):1139–47. [PubMed] [Google Scholar]
- 28.Couldridge L, Kendall S, March A. A systematic overview—a decade of research. The information and counselling needs of people with epilepsy. Seizure. 2001;10(8):605–14. doi: 10.1053/seiz.2001.0652. [DOI] [PubMed] [Google Scholar]
- 29.Strecher V, Champion V, Rosenstock I. The health belief model and health behavior. In: Gochman D, editor. Handbook of health behavior research. New York, NY: Plenum Press; 1997. pp. 71–91. [Google Scholar]
- 30.Ajzen I. The theory of planned behaviour. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 31.Buick D, Crook D, Horne R. Women’s perceptions of hormone replacement therapy: risks and benefits (1980–2002) Climacteric. 2005;8(1):24–35. doi: 10.1080/13697130500062654. [DOI] [PubMed] [Google Scholar]
- 32.Cooper A, Jackson G, Weinman J, Horne R. A qualitative study investigating patients’ beliefs about cardiac rehabilitation. Clin Rehab. 2005;19(1):87–96. doi: 10.1191/0269215505cr818oa. [DOI] [PubMed] [Google Scholar]
- 33.Cooper V, Buick D, Horne R, Lambert N, Gellaitry G, Leake H, et al. Perceptions of HAART among gay men who declined a treatment offer: preliminary results from an interview-based study. AIDS Care. 2002;14(3):319–28. doi: 10.1080/09540120220123694. [DOI] [PubMed] [Google Scholar]
- 34.Conrad P. The meaning of medications: another look at compliance. Soc Sci Med. 1985;20(1):29–37. doi: 10.1016/0277-9536(85)90308-9. [DOI] [PubMed] [Google Scholar]
- 35.Rogers A, Day JC, Williams B, Randall F, Wood P, Healy D, et al. The meaning and management of neuroleptic medication: a study of patients with a diagnosis of schizophrenia. Soc Sci Med. 1998;47(9):1313–23. doi: 10.1016/s0277-9536(98)00209-3. [DOI] [PubMed] [Google Scholar]
- 36.Dowell J, Hudson H. A qualitative study of medication-taking behaviour in primary care. Fam Pract. 1997;14(5):369–75. doi: 10.1093/fampra/14.5.369. [DOI] [PubMed] [Google Scholar]
- 37.Benson J, Britten N. What effects do patients feel from their antihypertensive tablets and how do they react to them? Qualitative analysis of interviews with patients. Fam Pract. 2006;23(1):80–7. doi: 10.1093/fampra/cmi081. [DOI] [PubMed] [Google Scholar]
- 38.Jenkins L, Britten N, Stevenson F, Barber N, Bradley C. Developing and using quantitative instruments for measuring doctor-patient communication about drugs. Patient Educ Couns. 2003;50:273–8. doi: 10.1016/s0738-3991(03)00049-1. [DOI] [PubMed] [Google Scholar]
- 39.Britten N, Ukoumunne O, Boulton M. Patients’ attitudes to medications and expectations for prescriptions. Health Expect. 2002;5(3):256–69. doi: 10.1046/j.1369-6513.2002.00187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]