Abstract
Peroxisome proliferator-activated receptors (PPARs) are ligand-activated nuclear receptors controlling many important physiological processes, including lipid and glucose metabolism, energy homeostasis, inflammation, as well as cell proliferation and differentiation. In the past decade, intensive study of PPARs has shed novel insight into prevention and treatment of dyslipidemia, insulin resistance, and type 2 diabetes. Recently, a large body of research revealed that PPARs are also functionally expressed in reproductive organs and various parts of placenta during pregnancy, which strongly suggests that PPARs might play a critical role in reproduction and development, in addition to their central actions in energy homeostasis. In this review, we summarize recent findings elucidating the role of PPARs in female reproduction, with particular focus on evidence from gene knockout and transgenic animal model study.
1. INTRODUCTION
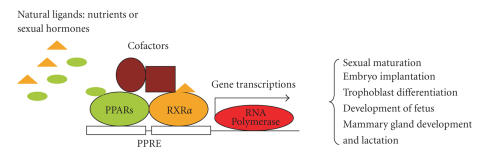
Peroxisome proliferator-activated receptors (PPARs) are members of the ligand-activated nuclear hormone receptor superfamily of 49 members that participate in many physiological functions [1]. To date, three isotypes, designated as PPARα, PPARβ/δ, and PPARγ, have been identified in many species, including frogs, rodents, and humans [2, 3]. PPARα is highly expressed in liver, kidney, heart, skeletal muscle, and other tissues involving fatty acid oxidation and it had been demonstrated to be the central regulator of fatty acid β-oxidation, fatty acid (FA) transport, and lipoprotein synthesis in these tissues. Activation of PPARα by its natural or synthetic ligands enhances FA uptake and oxidation in liver, which is beneficial for ameliorating dyslipidemia [4, 5]. PPARγ is predominantly expressed in adipose tissue and is a key regulator of adipocyte differentiation and triglyceride storage, whereas PPARβ/δ is ubiquitously expressed in almost all tissues and believed to be involved in lipid metabolism [4, 6]. In contrast to intensive research into PPARγ and PPARα, little exists for PPARβ/δ. After binding by their endogenous ligands, such as 15-deoxy-Δ12,14-prostaglandin J2 (15dPGJ2) and long-chain FAs, or exogenous synthetic agonists, such as thiazolidinediones (TZDs) and fibrates, PPARs will heterodimerize with another nuclear receptor called retinoid X receptor alpha (RXRα). The PPARs/RXRα heterodimer binds to a specific DNA sequence called PPAR-responsive element (PPRE) located in promoter regions of the target genes to initiate or silence gene transcription. A typical PPRE consists of a repeat AGGTCA separated by one nucleotide. However, activation of PPARs is far more complex than this, with complicated cross-talk among PPARs, RXRs, ligands, corepressors, coactivators, and many other factors [7, 8].
Because PPARs play key roles in regulating energy homeostasis, particularly FA oxidation and carbohydrate metabolism, numerous studies have been conducted in the past decade to develop synthetic PPAR agonists for therapeutic treatment of metabolic diseases, including dyslipidemia, insulin resistance, and type 2 diabetes. Long before being identified as PPARα agonists, fibrates were clinically prescribed for treatment of dyslipidemia. Subsequently, TZDs, structural analogues of fibrates, were shown to selectively activate PPARγ [7, 9–11]. To date, several TZDs, including pioglitazone and rosiglitazone, improve glycemic control in patients with type 2 diabetes or glucose intolerance via their insulin-sensitizing activity, mainly achieved by preventing FA uptake and adipose deposition in insulin-sensitive tissues such as liver, muscle, and pancreas [7, 9–11]. In addition, potent agonists for activation of multiple PPAR isotypes now in development, such as dual PPARα/γ agonists, have considerable promise for improving glycemic control with fewer side effects. As well, PPARβ/δ agonists are currently under development.
The nutrients glucose and FA and fuel sensors insulin and leptin have long been known to be critical in regulating female reproduction [12–14]. During the onset of puberty, molecules such as leptin and neuropeptide Y might function as energy sensors and initiate reproduction processes under conditions of sufficient body energy storage [13, 15, 16]. Given the well-documented central roles of PPARs in energy homeostasis and because energy status is directly linked to reproduction [13, 14], it is reasonable to speculate that PPARs may play important roles in female reproduction. In fact, many recent studies have examined the potential role of PPARs in reproduction. In rodents, PPAR knockout mouse models have provided direct evidence of a critical role of PPARs in reproduction and placenta development (Table 1). PPARγ-null mouse fetuses were shown to die by embryonic day 10 because of failed formation of the vascular labyrinth [17, 18], and PPARβ/δ-null mice also exhibited abnormal placenta during development [19]. In contrast to PPARγ- and PPARβ/δ-null mice, PPARα-null mice displayed no placental abnormality but, rather, increased risk of maternal abortion and offspring neonatal mortality [20]. Subsequent studies involving RT-PCR, in situ hybridization, immunohistochemistry, and Northern and Western blot analysis further revealed all three PPAR isotypes are expressed in reproductive tissues such as testis (sperm), ovary (oocyte), as well as various parts of the placenta of rat, mouse, and human [12, 21, 22]. Importantly, pregnant rats given oral troglitazone showed significantly increased placental PPARγ expression as well as reduced mortality of fetuses by about 50% [23]. Loss-of-function mutations of PPARs have provided excellent models for studying the roles of PPARs in human reproduction and placenta development. To date, three groups of loss-of-function mutations of PPARγ have been described [6, 24–26]. In one study, about 40% of female subjects with loss-of-function mutations of PPARγ had polycystic ovary syndrome (PCOS) [6], which has been believed to be associated with infertility in women. Consistent with these observations, administration of insulin-sensitizers TZDs and metformin improved ovulation function and fertility and enhanced growth hormone (GH) secretion in women with PCOS [27, 28]. Collectively, these findings imply an important role for PPARs in mammalian reproduction.
Table 1.
Studies of reproductive phenotypes of female PPARα, PPARβ/δ, and PPARγ-null or transgenic mice.
| PPAR isotype | Reproductive phenotypes | References | |
|---|---|---|---|
| PPARα | KO | Maternal abortion and neonatal death; altered ovarian estradiol production | Yessoufou et al. [20], Lefebvre et al. [4] |
| TG | Defect in mammary gland development; defect in lactation during pregnancy | Yang et al. [50] | |
| PPARβ/δ | KO | Placental defects; frequent (>90%) midgestation lethality; placenta lipid accumulation defects | Barak et al. [19], Nadra et al. [57] |
| PPARγ | KO | Embryonic death at embryo day 10; embryonic lipid droplets lacking; placental malformed labyrinth zone; toxic milk | Barak et al. [17], Kubota et al. [18], Wan et al. [71] |
| TG | Exacerbates mammary gland tumor development | Saez et al. [73] |
KO: global or tissue-specific knockout; TG: tissue-specific transgenic.
In this review, we discuss PPARs expression in female reproductive tissues and their roles in female reproduction, with a focus on genetically manipulated mice.
2. PPARs: TISSUE DISTRIBUTION IN FEMALE REPRODUCTIVE SYSTEM
2.1. Hypothalamic-pituitary axis
All three PPAR isotypes have been detected in the mouse pituitary gland [29]. PPARγ is highly expressed in normal human pituitary gland and in all normal pituitary secreting cell lines [30]. Because of its antiproliferative effects in pituitary cells, activation of PPARγ by TZDs inhibited the development of pituitary adenomas in mice and humans [31]. Despite its presence in the hypothalamic-pituitary axis, the precise roles of PPARγ in reproductive cells remain poorly understood. Although PPARγ expression is evident in pituitary tissue, TZD treatment failed to affect the in vitro secretion of ovine pituitary hormones, including prolactin (PRL), growth hormone (GH), follicle-stimulating hormone (FSH), and luteinizing hormone (LH), and also no alteration of the LH secretion was observed in LbetaT2 cells, a murine gonadotropic pituitary tumor cell line [12].
2.2. Ovary
All three isotypes of PPAR are expressed in ovarian tissue. PPARα and PPARβ/δ are expressed primarily in the theca and stroma tissues [32], whereas PPARγ, more extensively studied, was detected in ovaries of mouse, rat, pig, sheep, cow, and human. In the ovaries of rodents and ruminants, PPARγ is highly expressed in granulosa cells, with lower expression in theca cells and the corpus luteum [12]. In humans, PPARγ was present in granulosa cells collected during oocyte aspiration from women undergoing treatment for in vitro fertilization [33]. Unlike the constant expression of PPARα and PPARβ/δ throughout follicular development and the ovarian cycle, the expression of PPARγ is downregulated in response to LH surge. PPARγ expression seems to be tightly regulated in the ovary, and its regulatory expression is the primary mechanism by which LH influences the activity of PPARγ [34].
2.3. Uterus and placenta
Although all three PPAR isotypes are functionally expressed in uterus, they display different expression profiles with the development of placenta in pregnancy [35–37]. In endometria of ewe, PPARα expression declines between day 7 and day 17 of pregnancy, whereas PPARβ/δ is constantly expressed at all developmental stages and PPARγ expression is erratically regulated. In addition, RXRs differ from that of PPARs, which suggests that different PPAR/RXR heterodimers might form and function distinctly as development proceeds [35]. All three PPAR isotypes have been reported in placenta in rodents and humans. PPARγ was the first to be detected in a human choriocarcinoma-derived JEG cell line by Northern blot analysis [34]. In human placenta, PPARγ is expressed in early and term villous trophoblasts and in extravillous trophoblasts in first-trimester placentas [21]. PPARγ was also detected in mouse placenta as early as embryonic day 8.5 [38] and in rat placenta by day 11 [23]. In mice, PPARγ is expressed in spongiotrophoblasts and in the vascular labyrinth that forms the interface between maternal and fetal circulation to control nutrient exchange [23]. In rodent placenta, PPARα and PPARβ/δ are present in the junctional zone, which has invasive and endocrine functions, and in the labyrinth, whereas in human placenta, they are in villous trophoblasts, particularly syncytiotrophoblasts [39]. However, in cultured villous trophoblasts of human term placenta, PPARα and PPARβ/δ transcript levels were higher in cytotrophoblasts than in syncytiotrophoblasts [40].
2.4. Mammary gland
All three isotypes of PPAR are detected in rodent mammary gland and human breast cell lines [41–44]. During pregnancy and lactation, the PPARα and γ mRNAs decreased while the PPARβ/δ mRNA remained relatively unchanged in mouse mammary gland [41].
3. PPARα AND FEMALE REPRODUCTION
During pregnancy, placental transfer of FA and other nutrients from the mother to the fetus is crucial for adequate fetal growth and development, and PPARα might play a crucial role in this process because of its central role in FA transport and oxidation [4, 10, 39]. Recently, gemfibrozil and clofibrate, two PPARα agonists, were shown to downregulate human chorionic gonadotrophin and upregulate progesterone secretion in human trophoblasts, which suggests that activation of PPARα might be beneficial for the secretion of these hormones, so essential for maintaining pregnancy [45]. More recently, evidence for a key role of PPARα in placenta development was demonstrated by increased abortion rate (by 20%) in PPARα-null mice without diabetes [4, 20]. In PPARα-null mice with diabetes, the mean abortion rate was approximately 50%, as compared with 8.3% for wild-type mice. Moreover, PPARα-null mice showed higher neonatal mortality than wild-type mice: for mice without diabetes, the rate was 13.3% versus 5.1%, respectively, and for mice with diabetes, 78.9% versus 27.7% [20]. Thus, PPARα might have an important role in maternal-fetal nutrient exchange, and its deficiency could be deleterious to fetal development. This study further supported that tight control of blood glucose is beneficial for improving the fertility of diabetic women and, as clearly indicated in this study, abortion rate and neonatal mortality were increased in both wild-type and PPARα-null mice with diabetes.
Controversially, some other reports indicated that activation of PPARα might be deleterious to development of female reproductive cells. PPARα can bind to estrogen response elements and act as a competitive inhibitor of estrogen receptor [46, 47]. Activation of PPARα decreased the expression and activity of aromatase in granulosa cells [48], thus resulting in decreased estradio synthesis. More recently, treatment with the PPARα agonist fenofibrate decreased the level of aromatase in wild-type mice but enhanced it in PPARα-null mice [49]. A critical role for PPARα in mammary gland function was supported by a recent study in which transgenic mice expressing a constitutively activated PPARα form (VP16PPARα) in the stratified epithelia had a severe defect in mammary gland development and lactation during pregnancy, resulting in 100% neonate mortality [50]. Taken together, these observations reveal that PPARα plays an important role in mammalian female reproduction, but further research work is required to clarify its definite role and underlying molecular mechanism(s).
4. PPARβ/δ AND FEMALE REPRODUCTION
PPARβ/δ is ubiquitously expressed in the ovary at a constant level during the estrous cycle and pseudopregnancy [51], which suggests that PPARβ/δ may be involved in normal ovarian function in theca, stroma, and luteal cells. One study showed that PPARβ/δ mRNA was almost absent on mouse embryo days 1–4 but was significantly expressed in the subluminal stroma surrounding blastocysts on day 5, just after embryo implantation. Subsequently, PPARβ/δ expression was increased in the decidua on days 6–8 [36, 52]. A similar process was observed in rat as well, intense PPARβ/δ immunostaining was observed in rat decidua under artificial decidualization but not in uninjected control horns [53]. These data suggest that PPARβ/δ expression at implantation sites requires an active blastocyst or analog and may play an essential role in blastocyst implantation.
A large body of research has indicated that PPARβ/δ mediates the important role of COX-2-derived prostaglandin I2 (prostacyclin, PGI2) in pregnancy. COX-2 knockout female mice displayed decreased fertility, in part due to deficiency of blastocyte implantation and decidualization [52, 54]. Treatment of these mice with a PGI2 analogue, carboprostacyclin, or the PPARβ/δ-selective agonist L-165041 restored implantation [52]. PGI2 is the most abundant prostaglandin at implantation sites where PPARβ/δ and COX-2 were colocalized and strongly upregulated during pregnancy in a similar manner [52]. As a potent endogenous PPARβ/δ ligand, PGI2 can act as a vasoactive agent to increase vascular permeability [55, 56] and blastocyst hatching [57], so the high expression of PPARβ/δ in the subluminal stroma at implantation sites might mediate this process, facilitating the implantation of the embryo [58]. This suggestion was further confirmed by placentas of PPARβ/δ-null mice displaying abnormal vascular development [19] and that giant-cell differentiation of placentas requires an intact PPARβ/δ signaling pathway [57].
In addition to the important roles of PPARβ/δ at implantation sites of the maternal body, the expression and function of PPARβ/δ in the embryo are of interest. Compared to the development of in vivo embryos, cultured embryos, such as in vitro fertilization (IVF) embryos, are retarded because they lack the protective environment of the maternal body [59]. Supplementing culture media with milepost, a stable analog of PGI2, enhanced mouse blastocyst hatching [60]. Recent work showed that preimplantation embryos express PPARβ/δ, which is essential for the enhancing effect of PGI2 and the spontaneous progression of the embryos. PGI2 promoted the development of wild-type embryos in vitro and enhanced their implantation potential but had no effect on PPARβ/δ-null embryos [61].
PPARβ/δ is expressed ubiquitously at higher levels during embryogenesis than in adulthood [62, 63]. In addition, homozygous loss of PPARβ/δ caused frequent embryonic lethality, but surviving PPARβ/δ-deficient offspring did not die postnatally, which suggests that the essential function of the receptor is restricted to the gestational period [19].
Given the roles of PPARβ/δ in embryo development and implantation, the activity of PPARβ/δ agonists under development should be carefully evaluated to avoid possible complications in pregnancy with their use.
5. PPARγ AND FEMALE REPRODUCTION
After ovulation, the expression of PPARγ in the corpus luteum increases, otherwise the corpus luteum regresses and PPARγ expression decreases if no fertilization or embryo implantation occurs [64, 65]. Thus, PPARγ might play a role in fertility control. Indeed, mice with specific deletion of PPARγ in granulosa cells exhibited reduced fertility [66]. Luteal expression of PPARγ might be important for the pregnancy, possibly via maintaining production of progesterone to support implantation and gestation [67].
PPARγ-null embryos were shown to die by embryonic day 10 [17], as a result of placenta alteration and malformed vascular labyrinth due to PPARγ deficiency, which disrupts the interface between trophoblasts and the fetal endothelium and leads to embryonic myocardial thinning. A tetraploid-rescued mutant overcame the placenta defect for survival to term. Consistent with this observation, an RXRα-(PPARγ hetero-partner) or RXRα/RXRβ-null mutant exhibited a similar phenotype to that of PPARγ-null mice [17, 68]. The expression of Mucin 1 (MUC1), a PPARγ target gene, is lost in PPARγ-null mice, whereas its expression in wild-type mice can be upregulated by PPARγ agonist treatment. MUC1 expressed in the apical surface of the labyrinth helps in differentiation of trophoblast stem cells and invokes developmental and functional analogies between the placental blood sinuses and luminal epithelia [69].
During early term pregnancy, placental trophoblasts invade the uterine wall and establish the maternal-fetal exchange. PPARγ plays a dominant role in this process. The differentiation of the placenta is characterized by fusion of cytotrophoblasts into syncytiotrophoblasts, which are more resistant than cytotrophoblasts to hypoxic injury. Activation of PPARγ stimulates this differentiation process [21]. PPARγ agonists increase FA uptake and adipose accumulation in trophoblasts [70], and PPARγ-null or RXRα-null murine embryos show fewer lipid droplets than wild-type embryos [17, 68], which suggests an important role of PPARγ in providing sufficient nutrients for embryo development. Moreover, it is indicated in one latest study that PPARγ deletion in mammary gland resulted in the production of “toxic milk” containing elevated levels of inflammatory lipids, which results in inflammation, alopecia, and growth retardation in the nursing neonates [71]. Peroxisome proliferator-activated receptor-binding protein (PBP) serves as an anchor for recruiting PPAR mediator complexes, and is necessary for activation of PPARs. Moreover, specific knockout of PBP in mouse mammary gland resulted in a severe defect in mammary gland development, indeed the PBP-null mammary gland failed to produce milk for nursing neonates during lactation [72]. These studies clearly indicated that PPARγ/PPAR-binding protein expression are also vital for providing high-quality milk for nursing the neonates and protecting them from inflammatory lipids [71]. Interestingly and unexpectedly, constitutive expression of an active form of PPARγ (Vp16PPARγ) in mammary gland exacerbated mammary gland tumor development via enhanced Wnt signaling [73].
Proinflammatory proteins and cytokines are associated with term and preterm labor and stimulate uterine contraction [74]; PPARγ might be implicated in this process because of its ability to suppress inflammatory cytokine secretion [75]. The natural ligands of placental PPARγ may be present in maternal circulation, which could be naturally occurring prostanoids or FAs and some reproductive hormones. This hypothesis is supported by the observation that serum from pregnant women activated PPARγ expression in JEG-3 cells, while serum from nonpregnant women having no such effect [76].
In addition, as a target gene of PPARγ, another nuclear receptor, liver X receptor (LXR), participates in regulation of female reproduction. The two isforms, α and β, both act as transcription factors activated by binding of specific cholesterol metabolites [77]. LXRs play important roles in many metabolic pathways, such as cholesterol, lipid, and carbohydrate metabolism. In addition to these regulatory actions, LXRs affect reproductive function. Mice deficient in LXRα, LXRβ, or both showed decreased ability to conceive and fewer pups per litter as compared with wild-type mice [78]. As well, both LXRα and β are expressed in mouse oocytes and seem to affect ovarian function [78]. Lipid distribution in the uterus plays a critical role for its function. LXR prevents accumulation of cholesteryl esters in the mouse myometrium by controlling the expression of genes (ABCA1 and ABCG1) involved in cholesterol efflux and storage. As well, mice lacking LXRβ showed a contractile activity defect induced by oxytocin or PGF2α [79]. Taken together, gene knockout results suggest that PPARγ/LXR might participate in embryonic development by sensing changes in levels of nutrients, hormones, and/or other signals.
6. CONCLUSION
A large body of research has revealed that in addition to their central roles in regulating FA oxidation and glucose homeostasis, PPARs are highly expressed in reproductive tissues and placenta, so PPARs might also be key regulators of reproduction and development (Table 1). At the early stage of sexual maturation, PPARs might be activated in response to energy status and/or circulating hormones for involvement in maturation of reproductive cells. During gestation, PPARs are highly expressed in trophoblasts and directly involved in cytotrophoblast differentiation and function, possibly functioning as energy-signal sensors and transporters for nutrients and gases between maternal and fetus circulation to provide sufficient nutrients for development of the fetus (see Figure 1). Moreover, PPARs also play important roles in mammary gland development and maternal PPARs are vital for producing high-quality milk for nursing neonates. However, further research is required to address the following questions. (1) What are the natural ligands for activation of PPARs in reproduction and development, nutrients, sexual hormones, or other factors? (2) What are the underlying molecular mechanisms of PPAR activation in response to their natural ligands? Given the critical roles of all three PPAR isotypes in female reproduction, caution should be taken in the clinical use of PPARα and PPARγ agonists in young women.
Figure 1.
Schematic presentation of regulatory roles of PPARs in reproduction and development.
ACKNOWLEDGMENTS
The authors thank Dr. Jing Li and Dr. Dan Pu for their assistance in manuscript preparation. This work was supported by grants from the Natural Science Foundation of China (Grant no. NSFC 30670766, 30530340, 30771030) and the Ministry of Science and Technology of China (Grant no. 2006CB503907 to Y. Guan).
References
- 1.Yang X, Downes M, Yu R, et al. Nuclear receptor expression links the circadian clock to metabolism. Cell. 2006;126(4):801–810. doi: 10.1016/j.cell.2006.06.050. [DOI] [PubMed] [Google Scholar]
- 2.Lehrke M, Lazar MA. The many faces of PPARγ . Cell. 2005;123(6):993–999. doi: 10.1016/j.cell.2005.11.026. [DOI] [PubMed] [Google Scholar]
- 3.Balakumar P, Rose M, Singh M. PPAR ligands: are they potential agents for cardiovascular disorders? Pharmacology. 2007;80(1):1–10. doi: 10.1159/000102594. [DOI] [PubMed] [Google Scholar]
- 4.Lefebvre P, Chinetti G, Fruchart J-C, Staels B. Sorting out the roles of PPARα in energy metabolism and vascular homeostasis. Journal of Clinical Investigation. 2006;116(3):571–580. doi: 10.1172/JCI27989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beaven SW, Tontonoz P. Nuclear receptors in lipid metabolism: targeting the heart of dyslipidemia. Annual Review of Medicine. 2006;57:313–329. doi: 10.1146/annurev.med.57.121304.131428. [DOI] [PubMed] [Google Scholar]
- 6.Semple RK, Chatterjee VK, O'Rahilly S. PPARγ and human metabolic disease. Journal of Clinical Investigation. 2006;116(3):581–589. doi: 10.1172/JCI28003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang Y, Guan Y. PPAR-γ agonists and diabetic nephropathy. Current Diabetes Reports. 2005;5(6):470–475. doi: 10.1007/s11892-005-0057-5. [DOI] [PubMed] [Google Scholar]
- 8.Zoete V, Grosdidier A, Michielin O. Peroxisome proliferator-activated receptor structures: ligand specificity, molecular switch and interactions with regulators. Biochimica et Biophysica Acta. 2007;1771(8):915–925. doi: 10.1016/j.bbalip.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 9.Staels B, Fruchart J-C. Therapeutic roles of peroxisome proliferator-activated receptor agonists. Diabetes. 2005;54(8):2460–2470. doi: 10.2337/diabetes.54.8.2460. [DOI] [PubMed] [Google Scholar]
- 10.Guan Y. Peroxisome proliferator-activated receptor family and its relationship to renal complications of the metabolic syndrome. Journal of the American Society of Nephrology. 2004;15(11):2801–2815. doi: 10.1097/01.ASN.0000139067.83419.46. [DOI] [PubMed] [Google Scholar]
- 11.Wang G, Wei J, Guan Y, Jin N, Mao J, Wang X. Peroxisome proliferator-activated receptor-γ agonist rosiglitazone reduces clinical inflammatory responses in type 2 diabetes with coronary artery disease after coronary angioplasty. Metabolism. 2005;54(5):590–597. doi: 10.1016/j.metabol.2004.11.017. [DOI] [PubMed] [Google Scholar]
- 12.Froment P, Gizard F, Defever D, Staels B, Dupont J, Monget P. Peroxisome proliferator-activated receptors in reproductive tissues: from gametogenesis to parturition. Journal of Endocrinology. 2006;189(2):199–209. doi: 10.1677/joe.1.06667. [DOI] [PubMed] [Google Scholar]
- 13.Cervero A, Domínguez F, Horcajadas JA, Quiñonero A, Pellicer A, Simón C. The role of the leptin in reproduction. Current Opinion in Obstetrics & Gynecology. 2006;18(3):297–303. doi: 10.1097/01.gco.0000193004.35287.89. [DOI] [PubMed] [Google Scholar]
- 14.The ESHRE Capri Workshop Group. Nutrition and reproduction in women. Human Reproduction Update. 2006;12(3):193–207. doi: 10.1093/humupd/dmk003. [DOI] [PubMed] [Google Scholar]
- 15.Kiess W, Blum WF, Aubert ML. Leptin, puberty and reproductive function: lessons from animal studies and observations in humans. European Journal of Endocrinology. 1998;138(1):26–29. doi: 10.1530/eje.0.1380026. [DOI] [PubMed] [Google Scholar]
- 16.Kiess W, Reich A, Meyer K, et al. A role for leptin in sexual maturation and puberty? Hormone Research. 1999;51(supplement 3):55–63. doi: 10.1159/000053163. [DOI] [PubMed] [Google Scholar]
- 17.Barak Y, Nelson MC, Ong ES, et al. PPARγ is required for placental, cardiac, and adipose tissue development. Molecular Cell. 1999;4(4):585–595. doi: 10.1016/s1097-2765(00)80209-9. [DOI] [PubMed] [Google Scholar]
- 18.Kubota N, Terauchi Y, Miki H, et al. PPARγ mediates high-fat diet-induced adipocyte hypertrophy and insulin resistance. Molecular Cell. 1999;4(4):597–609. doi: 10.1016/s1097-2765(00)80210-5. [DOI] [PubMed] [Google Scholar]
- 19.Barak Y, Liao D, He W, et al. Effects of peroxisome proliferator-activated receptor δ on placentation, adiposity, and colorectal cancer. Proceedings of the National Academy of Sciences of the United States of America. 2002;99(1):303–308. doi: 10.1073/pnas.012610299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yessoufou A, Hichami A, Besnard P, Moutairou K, Khan NA. Peroxisome proliferator-activated receptor α deficiency increases the risk of maternal abortion and neonatal mortality in murine pregnancy with or without diabetes mellitus: modulation of T cell differentiation. Endocrinology. 2006;147(9):4410–4418. doi: 10.1210/en.2006-0067. [DOI] [PubMed] [Google Scholar]
- 21.Fournier T, Tsatsaris V, Handschuh K, Evain-Brion D. PPARs and the placenta. Placenta. 2007;28(2-3):65–76. doi: 10.1016/j.placenta.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 22.Schaiff WT, Barak Y, Sadovsky Y. The pleiotropic function of PPARγ in the placenta. Molecular and Cellular Endocrinology. 2006;249(1-2):10–15. doi: 10.1016/j.mce.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 23.Asami-Miyagishi R, Iseki S, Usui M, Uchida K, Kubo H, Morita I. Expression and function of PPARγ in rat placental development. Biochemical and Biophysical Research Communications. 2004;315(2):497–501. doi: 10.1016/j.bbrc.2004.01.074. [DOI] [PubMed] [Google Scholar]
- 24.Barroso I, Gurnell M, Crowley VEF, et al. Dominant negative mutations in human PPARγ associated with severe insulin resistance, diabetes mellitus and hypertension. Nature. 1999;402(6764):880–883. doi: 10.1038/47254. [DOI] [PubMed] [Google Scholar]
- 25.Agarwal AK, Garg A. A novel heterozygous mutation in peroxisome proliferator-activated receptor-γ gene in a patient with familial partial lipodystrophy. Journal of Clinical Endocrinology & Metabolism. 2002;87(1):408–411. doi: 10.1210/jcem.87.1.8290. [DOI] [PubMed] [Google Scholar]
- 26.Hegele RA, Cao H, Frankowski C, Mathews ST, Leff T. PPARG F388L, a transactivation-deficient mutant, in familial partial lipodystrophy. Diabetes. 2002;51(12):3586–3590. doi: 10.2337/diabetes.51.12.3586. [DOI] [PubMed] [Google Scholar]
- 27.Glintborg D, Støving RK, Hagen C, et al. Pioglitazone treatment increases spontaneous growth hormone (GH) secretion and stimulated GH levels in polycystic ovary syndrome. Journal of Clinical Endocrinology & Metabolism. 2005;90(10):5605–5612. doi: 10.1210/jc.2005-0615. [DOI] [PubMed] [Google Scholar]
- 28.Seli E, Duleba AJ. Optimizing ovulation induction in women with polycystic ovary syndrome. Current Opinion in Obstetrics & Gynecology. 2002;14(3):245–254. doi: 10.1097/00001703-200206000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Bookout AL, Jeong Y, Downes M, Yu RT, Evans RM, Mangelsdorf DJ. Anatomical profiling of nuclear receptor expression reveals a hierarchical transcriptional network. Cell. 2006;126(4):789–799. doi: 10.1016/j.cell.2006.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bogazzi F, Russo D, Locci MT, et al. Peroxisome proliferator-activated receptor (PPAR)γ is highly expressed in normal human pituitary gland. Journal of Endocrinological Investigation. 2005;28(10):899–904. doi: 10.1007/BF03345321. [DOI] [PubMed] [Google Scholar]
- 31.Heaney AP, Fernando M, Melmed S. PPAR-γ receptor ligands: novel therapy for pituitary adenomas. Journal of Clinical Investigation. 2003;111(9):1381–1388. doi: 10.1172/JCI16575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee SS, Pineau T, Drago J, et al. Targeted disruption of the α isoform of the peroxisome proliferator-activated receptor gene in mice results in abolishment of the pleiotropic effects of peroxisome proliferators. Molecular and Cellular Biology. 1995;15(6):3012–3022. doi: 10.1128/mcb.15.6.3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Komar CM. Peroxisome proliferator-activated receptors (PPARs) and ovarian function—implications for regulating steroidogenesis, differentiation, and tissue remodeling. Reproductive Biology and Endocrinology. 2005;3:41. doi: 10.1186/1477-7827-3-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Banerjee J, Komar CM. Effects of luteinizing hormone on peroxisome proliferator-activated receptor γ in the rat ovary before and after the gonadotropin surge. Reproduction. 2006;131(1):93–101. doi: 10.1530/rep.1.00730. [DOI] [PubMed] [Google Scholar]
- 35.Cammas L, Reinaud P, Bordas N, Dubois O, Germain G, Charpigny G. Developmental regulation of prostacyclin synthase and prostacyclin receptors in the ovine uterus and conceptus during the peri-implantation period. Reproduction. 2006;131(5):917–927. doi: 10.1530/rep.1.00799. [DOI] [PubMed] [Google Scholar]
- 36.Ding N-Z, Teng C-B, Ma H, et al. Peroxisome proliferator-activated receptor δ expression and regulation in mouse uterus during embryo implantation and decidualization. Molecular Reproduction and Development. 2003;66(3):218–224. doi: 10.1002/mrd.10348. [DOI] [PubMed] [Google Scholar]
- 37.Lord E, Murphy BD, Desmarais JA, Ledoux S, Beaudry D, Palin M-F. Modulation of peroxisome proliferator-activated receptor δ and γ transcripts in swine endometrial tissue during early gestation. Reproduction. 2006;131(5):929–942. doi: 10.1530/rep.1.00657. [DOI] [PubMed] [Google Scholar]
- 38.Cutando A, Gil-Montoya JA. The dental patient with hemostatic disorders. A review of hemostasia physiopathology for dental professionals. Medicina Oral. 1999;4(3):485–493. [PubMed] [Google Scholar]
- 39.Wang Q, Fujii H, Knipp GT. Expression of PPAR and RXR isoforms in the developing rat and human term placentas. Placenta. 2002;23(8-9):661–671. doi: 10.1053/plac.2002.0855. [DOI] [PubMed] [Google Scholar]
- 40.Daoud G, Simoneau L, Masse A, Rassart E, Lafond J. Expression of cFABP and PPAR in trophoblast cells: effect of PPAR ligands on linoleic acid uptake and differentiation. Biochimica et Biophysica Acta. 2005;1687(1–3):181–194. doi: 10.1016/j.bbalip.2004.11.017. [DOI] [PubMed] [Google Scholar]
- 41.Gimble JM, Pighetti GM, Lerner MR, et al. Expression of peroxisome proliferator activated receptor mRNA in normal and tumorigenic rodent mammary glands. Biochemical and Biophysical Research Communications. 1998;253(3):813–817. doi: 10.1006/bbrc.1998.9858. [DOI] [PubMed] [Google Scholar]
- 42.Suchanek KM, May FJ, Jae Lee W, Holman NA, Roberts-Thomson SJ. Peroxisome proliferator-activated receptor β expression in human breast epithelial cell lines of tumorigenic and non-tumorigenic origin. The International Journal of Biochemistry & Cell Biology. 2002;34(9):1051–1058. doi: 10.1016/s1357-2725(02)00025-0. [DOI] [PubMed] [Google Scholar]
- 43.Suchanek KM, May FJ, Robinson JA, et al. Peroxisome proliferator-activated receptor α in the human breast cancer cell lines MCF-7 and MDA-MB-231. Molecular Carcinogenesis. 2002;34(4):165–171. doi: 10.1002/mc.10061. [DOI] [PubMed] [Google Scholar]
- 44.Bonofiglio D, Aquila S, Catalano S, et al. Peroxisome proliferator-activated receptor-γ activates p53 gene promoter binding to the nuclear factor-κB sequence in human MCF7 breast cancer cells. Molecular Endocrinology. 2006;20(12):3083–3092. doi: 10.1210/me.2006-0192. [DOI] [PubMed] [Google Scholar]
- 45.Hashimoto F, Oguchi Y, Morita M, et al. PPARα agonists clofibrate and gemfibrozil inhibit cell growth, down-regulate hCG and up-regulate progesterone secretions in immortalized human trophoblast cells. Biochemical Pharmacology. 2004;68(2):313–321. doi: 10.1016/j.bcp.2004.03.024. [DOI] [PubMed] [Google Scholar]
- 46.Keller H, Givel F, Perroud M, Wahli W. Signaling cross-talk between peroxisome proliferator-activated receptor/retinoid X receptor and estrogen receptor through estrogen response elements. Molecular Endocrinology. 1995;9(7):794–804. doi: 10.1210/mend.9.7.7476963. [DOI] [PubMed] [Google Scholar]
- 47.Nuñez SB, Medin JA, Braissant O, et al. Retinoid X receptor and peroxisome proliferator-activated receptor activate an estrogen responsive gene independent of the estrogen receptor. Molecular and Cellular Endocrinology. 1997;127(1):27–40. doi: 10.1016/s0303-7207(96)03980-9. [DOI] [PubMed] [Google Scholar]
- 48.Lovekamp-Swan T, Jetten AM, Davis BJ. Dual activation of PPARα and PPARγ by mono-(2-ethylhexyl) phthalate in rat ovarian granulosa cells. Molecular and Cellular Endocrinology. 2003;201(1-2):133–141. doi: 10.1016/s0303-7207(02)00423-9. [DOI] [PubMed] [Google Scholar]
- 49.Toda K, Okada T, Miyaura C, Saibara T. Fenofibrate, a ligand for PPARα, inhibits aromatase cytochrome P450 expression in the ovary of mouse. Journal of Lipid Research. 2003;44(2):265–270. doi: 10.1194/jlr.M200327-JLR200. [DOI] [PubMed] [Google Scholar]
- 50.Yang Q, Kurotani R, Yamada A, Kimura S, Gonzalez FJ. Peroxisome proliferator-activated receptor α activation during pregnancy severely impairs mammary lobuloalveolar development in mice. Endocrinology. 2006;147(10):4772–4780. doi: 10.1210/en.2006-0437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Komar CM, Curry TE., Jr Localization and expression of messenger RNAs for the peroxisome proliferator-activated receptors in ovarian tissue from naturally cycling and pseudopregnant rats. Biology of Reproduction. 2002;66(5):1531–1539. doi: 10.1095/biolreprod66.5.1531. [DOI] [PubMed] [Google Scholar]
- 52.Lim H, Gupta RA, Ma W-G, et al. Cyclo-oxygenase-2-derived prostacyclin mediates embryo implantation in the mouse via PPARδ . Genes & development. 1999;13(12):1561–1574. doi: 10.1101/gad.13.12.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ding N-Z, Ma X-H, Diao H-L, Xu L-B, Yang Z-M. Differential expression of peroxisome proliferator-activated receptor δ at implantation sites and in decidual cells of rat uterus. Reproduction. 2003;125(6):817–825. doi: 10.1530/rep.0.1250817. [DOI] [PubMed] [Google Scholar]
- 54.Lim H, Paria BC, Das SK, et al. Multiple female reproductive failures in cyclooxygenase 2-deficient mice. Cell. 1997;91(2):197–208. doi: 10.1016/s0092-8674(00)80402-x. [DOI] [PubMed] [Google Scholar]
- 55.Wheeler-Jones C, Abu-Ghazaleh R, Cospedal R, Houliston RA, Martin J, Zachary I. Vascular endothelial growth factor stimulates prostacyclin production and activation of cytosolic phospholipase A2 in endothelial cells via p42/p44 mitogen-activated protein kinase. FEBS Letters. 1997;420(1):28–32. doi: 10.1016/s0014-5793(97)01481-6. [DOI] [PubMed] [Google Scholar]
- 56.Murohara T, Horowitz JR, Silver M, et al. Vascular endothelial growth factor/vascular permeability factor enhances vascular permeability via nitric oxide and prostacyclin. Circulation. 1998;97(1):99–107. doi: 10.1161/01.cir.97.1.99. [DOI] [PubMed] [Google Scholar]
- 57.Nadra K, Anghel SI, Joye E, et al. Differentiation of trophoblast giant cells and their metabolic functions are dependent on peroxisome proliferator-activated receptor β/δ . Molecular and Cellular Biology. 2006;26(8):3266–3281. doi: 10.1128/MCB.26.8.3266-3281.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Psychoyos A. Uterine receptivity for nidation. Annals of the New York Academy of Sciences. 1986;476(1):36–42. doi: 10.1111/j.1749-6632.1986.tb20920.x. [DOI] [PubMed] [Google Scholar]
- 59.Hardy K. Cell death in the mammalian blastocyst. Molecular Human Reproduction. 1997;3(10):919–925. doi: 10.1093/molehr/3.10.919. [DOI] [PubMed] [Google Scholar]
- 60.Huang J-C, Wun W-SA, Goldsby JS, Wun IC, Falconi SM, Wu KK. Prostacyclin enhances embryo hatching but not sperm motility. Human Reproduction. 2003;18(12):2582–2589. doi: 10.1093/humrep/deg490. [DOI] [PubMed] [Google Scholar]
- 61.Huang J-C, Wun W-SA, Goldsby JS, Wun IC, Noorhasan D, Wu KK. Stimulation of embryo hatching and implantation by prostacyclin and peroxisome proliferator-activated receptor δ activation: implication in IVF. Human Reproduction. 2006;22(3):807–814. doi: 10.1093/humrep/del429. [DOI] [PubMed] [Google Scholar]
- 62.Braissant O, Foufelle F, Scotto C, Dauça M, Wahli W. Differential expression of peroxisome proliferator-activated receptors (PPARs): tissue distribution of PPAR-α, -β, and -γ in the adult rat. Endocrinology. 1996;137(1):354–366. doi: 10.1210/endo.137.1.8536636. [DOI] [PubMed] [Google Scholar]
- 63.Braissant O, Wahli W. Differential expression of peroxisome proliferator-activated receptor-α, -β, and -γ during rat embryonic development. Endocrinology. 1998;139(6):2748–2754. doi: 10.1210/endo.139.6.6049. [DOI] [PubMed] [Google Scholar]
- 64.Löhrke B, Viergutz T, Shahi SK, et al. Detection and functional characterisation of the transcription factor peroxisome proliferator-activated receptor γ in lutein cells. Journal of Endocrinology. 1998;159(3):429–439. doi: 10.1677/joe.0.1590429. [DOI] [PubMed] [Google Scholar]
- 65.Viergutz T, Loehrke B, Poehland R, Becker F, Kanitz W. Relationship between different stages of the corpus luteum and the expression of the peroxisome proliferator-activated receptor γ protein in bovine large lutein cells. Journal of Reproduction and Fertility. 2000;118(1):153–161. [PubMed] [Google Scholar]
- 66.Cui Y, Miyoshi K, Claudio E, et al. Loss of the peroxisome proliferation-activated receptor γ (PPARγ) does not affect mammary development and propensity for tumor formation but leads to reduced fertility. Journal of Biological Chemistry. 2002;277(20):17830–17835. doi: 10.1074/jbc.M200186200. [DOI] [PubMed] [Google Scholar]
- 67.Lebovic DI, Kir M, Casey CL. Peroxisome proliferator-activated receptor-γ induces regression of endometrial explants in a rat model of endometriosis. Fertility and Sterility. 2004;82(supplement 3):1008–1013. doi: 10.1016/j.fertnstert.2004.02.148. [DOI] [PubMed] [Google Scholar]
- 68.Sapin V, Dollé P, Hindelang C, Kastner P, Chambon P. Defects of the chorioallantoic placenta in mouse RXRα null fetuses. Developmental Biology. 1997;191(1):29–41. doi: 10.1006/dbio.1997.8687. [DOI] [PubMed] [Google Scholar]
- 69.Shalom-Barak T, Nicholas JM, Wang Y, et al. Peroxisome proliferator-activated receptor γ controls Muc1 transcription in trophoblasts. Molecular and Cellular Biology. 2004;24(24):10661–10669. doi: 10.1128/MCB.24.24.10661-10669.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Elchalal U, Humphrey RG, Smith SD, Hu C, Sadovsky Y, Nelson DM. Troglitazone attenuates hypoxia-induced injury in cultured term human trophoblasts. American Journal of Obstetrics and Gynecology. 2004;191(6):2154–2159. doi: 10.1016/j.ajog.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 71.Wan Y, Saghatelian A, Chong L-W, Zhang C-L, Cravatt BF, Evans RM. Maternal PPARγ protects nursing neonates by suppressing the production of inflammatory milk. Genes & Development. 2007;21(15):1895–1908. doi: 10.1101/gad.1567207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jia Y, Qi C, Zhang Z, Zhu YT, Rao SM, Zhu Y-J. Peroxisome proliferator-activated receptor-binding protein null mutation results in defective mammary gland development. Journal of Biological Chemistry. 2005;280(11):10766–10773. doi: 10.1074/jbc.M413331200. [DOI] [PubMed] [Google Scholar]
- 73.Saez E, Rosenfeld J, Livolsi A, et al. PPARγ signaling exacerbates mammary gland tumor development. Genes & Development. 2004;18(5):528–540. doi: 10.1101/gad.1167804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm delivery. The New England Journal of Medicine. 2000;342(20):1500–1507. doi: 10.1056/NEJM200005183422007. [DOI] [PubMed] [Google Scholar]
- 75.Pascual G, Fong AL, Ogawa S, et al. A SUMOylation-dependent pathway mediates transrepression of inflammatory response genes by PPAR-γ . Nature. 2005;437(7059):759–763. doi: 10.1038/nature03988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Waite LL, Person EC, Zhou Y, Lim K-H, Scanlan TS, Taylor RN. Placental peroxisome proliferator-activated receptor-γ is up-regulated by pregnancy serum. Journal of Clinical Endocrinology & Metabolism. 2000;85(10):3808–3814. doi: 10.1210/jcem.85.10.6847. [DOI] [PubMed] [Google Scholar]
- 77.Lehrke M, Pascual G, Glass CK, Lazar MA. Gaining weight: the keystone symposium on PPAR and LXR. Genes & Development. 2005;19(15):1737–1742. doi: 10.1101/gad.1341005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Steffensen KR, Robertson K, Gustafsson J-Å, Andersen CY. Reduced fertility and inability of oocytes to resume meiosis in mice deficient of the LXR genes. Molecular and Cellular Endocrinology. 2006;256(1-2):9–16. doi: 10.1016/j.mce.2006.03.044. [DOI] [PubMed] [Google Scholar]
- 79.Mouzat K, Prod'homme M, Volle DH, et al. Oxysterol nuclear receptor LXRβ regulates cholesterol homeostasis and contractile function in mouse uterus. Journal of Biological Chemistry. 2007;282(7):4693–4701. doi: 10.1074/jbc.M606718200. [DOI] [PubMed] [Google Scholar]