During the past 10 years, human biological material—body fluids, cells, tissues, intracellular substances or DNA—and the related data have become an important resource for academic medical research, and for the industrial development of diagnostics and therapeutics (Godard et al, 2003). The increasing creation and use of biobanks that store both the material and the related data bears witness to their scientific value, but there is still no consensus—either internationally, or at the European or national levels—about the regulations that should govern biobanks in ethical or legal terms (Cambon-Thomsen et al, 2007; Kaye, 2005). In particular, consent models designed to appropriately regulate biobank-based research are characterized by a maze of laws, policies and ethical recommendations that range from strict (specific informed consent) to basically unrestricted use (broad consent; Boggio et al, 2007).
…consent models designed to appropriately regulate biobank-based research are characterized by a maze of laws, policies and ethical recommendations…
Many physicians, ethicists and policy-makers regard this fragmentation of the regulatory systems as a serious obstacle to biomedical research (Grizzle et al, 1999; Korn, 1999; Hirtzlin et al, 2003; Azarov et al, 2003; Trouet, 2004). Accordingly, many commentators have emphasized the need for international standardization, particularly in light of what the Council of Europe (COE; Strasbourg, France) described as the “increasing cross border flow of biological materials of human origin and data” (COE, 2006), and the interests of third parties, such as the pharmaceutical and biotechnology industries (Elger & Caplan, 2006; Anderlik, 2003).
Here, we propose a model and procedure for drafting, unified consent forms for the storage and use of human biological material and related data for the purpose of research. The resulting template, which was inspired by the partially restricted model proposed by the World Health Organization (WHO) in Geneva, Switzerland (WHO, 2003), was created for the Italian Biobank (IB) that operates in the context of a public university hospital, the Fondazione IRCCS Ospedale Maggiore Policlinico in Milano, Italy (Rebulla et al, 2007). This paper details the approach that eventually led to unified consent forms and procedures.
In February 2005, a multidisciplinary research group called the Italian Biobank User Group (IBUG) was formed. Its members were the Medical Director and Technical Director of the IB, two assistant biologists, a specialized legal expert, and 20 physicians and biologists from 14 clinical and laboratory units that use biobanking services. The IBUG held nine meetings between February 2005 and March 2006, each lasting 1–2 hours, which were dedicated to discussing the ethical and legal issues surrounding biobank-based research. The meetings also reviewed the drafts of informed consent templates that were drawn up by the legal expert, who applied an educational model involving both research and teaching tasks. The research tasks included: a comparative review of international, regional and national requirements for biobanking (Table 1)—laws, guidelines and ethical statements—to identify definitions of informed consent (Table 2); an analysis of articles about the ethical and legal aspects of biobanking research, which were mainly related to the available informed consent forms; the collection and review of consent models used by the biomedical staff at our hospital (Table 3); and the creation of a unified model of informed consent for biobanking (Fig 1).
Many physicians, ethicists and policy-makers regard this fragmentation of the regulatory systems as a serious obstacle to biomedical research
Table 1.
Comparative review of international laws, guidelines and regulations on biobank-based research and consent requirements
| Organization or country | Laws (L), guidelines (G) and regulations (R) | Informed consent requirements |
|---|---|---|
| World Health Organization | (G) Guideline for Obtaining Informed Consent for the Procurement and Use of Human Tissues, Cells and Fluids in Research (2003) (G) Proposed International Guidelines on Ethical Issues in Medical Genetics and Genetic Services (1997) | Specific informed consent Partially restricted consent Broad consent |
| Council for International Organizations of Medical Sciences | (G) International Ethical Guidelines for Biomedical Research Involving Human Subjects (2002) | Specific informed consent |
| United Nations Educational, Scientific and Cultural Organization | (G) International Declaration on Human Genetic Data (2003) | Partially restricted consent |
| Human Genome Organization | (G) Statement on DNA Sampling: Access and Control (1998) | Broad consent |
| Council of Europe | (L) Convention for the Protection of Human Rights and Dignity of the Human Being with Regard to the Application of Biology and Medicine (1997) (L) Treaty Series No. 195, Human Rights and Biomedicine. Protocol on Biomedical Research (2005) (G) Recommendation (2006) 4 on Research on Biological Materials of Human Origin (2006) | Specific informed consent |
| National Bioethics Advisory Commission | (G) Research Involving Human Biological Materials: Ethical Issues and Policy Guidance (1999) | Multi-layered consent |
| Australia | (G) National Statement on Ethical Conduct in Human Research (2007) | Specific informed consent Partially restricted consent Broad consent |
| Estonia | (L) Human Genes Research Act (2001) | Broad consent |
| France | (G) Ethical Issues Raised by Collections of Biological Materials and Associated Data: ‘Biobanks', ‘Biolibraries'—National Consultative Bioethics Committee for Health and Life Sciences (2003) | Specific informed consent |
| Germany | (G) Biobanks for Research—National Ethics Council Opinion (2004) | Broad consent |
| Italy | (G) Biobanks and Research on Human Biological Material—National Bioethics Committee Opinion (2006) (G) Guideline for Clinical Protocols of Genetic Research—Italian Society of Human Genetics (2006) | Partially restricted consent |
| (G) Guideline for Clinical Protocols of Genetic Research—Italian Society of Human Genetics (2006) | Specific informed consent | |
| (G) Guideline for Genetic Biobanks—Telethon (2003) | Specific informed consent | |
| (G) Guideline for the Establishment and Accreditation of Biobanks (2006) | Specific informed consent | |
| Japan | (G) Ethical Guidelines for Analytical Research on the Human Genome/ Genes (2001) | Broad consent |
| Switzerland | (G) Biobanks: Obtainment, Preservation and Utilization of Human Biological Material (2006) | Broad consent Specific informed consent |
| Spain | (R) Royal Decree 411/1996, by which Activities Regarding the Use of Human Tissues are Regulated (1996) | Informed expressed consent |
| United Kingdom | (L) Human Tissue Act (2004) (G) Human Tissue and Biological Samples for Use in Research—Medical Research Council (2001) | Broad consent |
| The Netherlands | (L) Civil code, article 467 (1994) (G) Code for Proper Secondary Use of Human Tissue in The Netherlands (2002) | Informed expressed consent |
| Iceland | (L) Act on Biobanks No. 110 (2000) | Broad consent |
| Denmark | (L) Law on Biobanks No. 312 (2003) | Informed expressed consent |
| Sweden | (L) Law No. 297 (2005) | Specific informed consent |
| Norway | (L) Act on Biobanks (2003) | Informed expressed consent |
Table 2.
Definition of informed consent models for biobank-based research according to the characterization used in international ethical and legal documents
| Model of informed consent | Definition |
|---|---|
| Broad consent | Allows the use of biological specimens and related data in immediate research and in future investigations of any kind at any time |
| Partially restricted consent | Allows the use of biological specimens and related data in specific immediate research and in future investigations directly or indirectly associated with them |
| Multi-layered consent | Requires several options to be explained to the research subject in a detailed form |
| Specific informed consent | Allows the use of biological specimens and related data only in immediate research; forbids any future study that is not foreseen at the time of the original consent |
Table 3.
Informed consent procedures to collect and store human biomaterials for research purposes applied in our hospital before the present study
| Specialty (number of procedures) | Reason for informed consent request | Type of information on the storage and future use of samples and related data |
|---|---|---|
| Clinical pathology (n = 3) | Diagnostic analysis | Absent |
| Haematology (n = 9) | Chemotherapy treatment Treatment with blood components Prenatal diagnosis of haemophilia A and B Participation in an international database on rare bleeding disorders Analysis of genetic heritage | Absent Absent Absent Absent Absent |
| Surgery (n = 7) | Removal of neoplastic tissues and organs Urethra reconstruction | Generic Generic |
| Neurology (n = 4) | Surgical biopsy | Generic |
| Gynaecology (n = 4) | Investigation on molecular markers | Specific |
| Medical genetics (n = 24) | Diagnostic analysis of fetal abnormalities Prenatal diagnosis | Generic Generic |
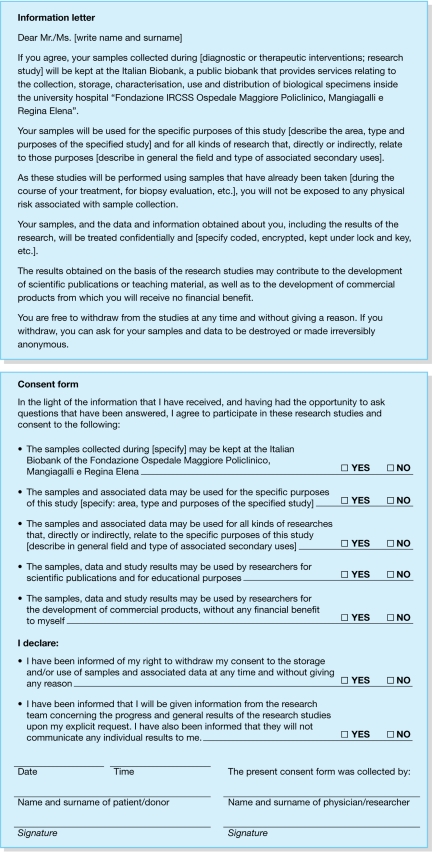
Figure 1.
Model of informed consent to store human biological materials for a specific study and associated future investigations
The teaching tasks involved developing short informative sessions for the IBUG on essential normative language to bridge the gap between bioethical and biomedical languages, and identifying the ethical and legal aspects of biobanking that needed to be considered. These were mainly related to: the ownership of human biological material derived from medical interventions or research projects; the potential use of human biological material and related data; the confidentiality of original and subsequent data; commercial developments, such as diagnostic procedures and drugs; and intellectual property rights, such as patents and licences.
The members of the working group reviewed the ethical and legal issues, and the draft consent templates. During these meetings, they raised many questions for discussion and resolution. The informed consent models were revised six times to address these comments. Finally, the informed consent model endorsed by the IBUG was examined and approved by the ethics committee at our hospital.
The review revealed the existence of a diverse range of views and policies regarding the appropriate consent required to store biological samples and data for future research (Maschke, 2005). Most regulations agree that consent should be free and explicit, and that the requirement for consent should be waived only in exceptional cases—usually when authorized by an ethics committee—or for unidentifiable samples or data (Knoppers, 2005a). However, the recommended nature and amount of information that should be given to a donor varies from broad or unrestricted to fully restricted or specific consent (Boggio et al, 2007; Hansson et al, 2006). The review also showed that the fragmentation in biobanking regulations regarding the use of biosamples and related data affects prospective research more than retrospective research (Knoppers, 2001).
Generally, international and regional regulations do not require informed consent when the biological samples and information are irreversibly anonymized or unlinked under certain conditions (Knoppers, 2005b). The WHO, for example, allows the use of such materials only when they are anonymized in such a way that the identification of a ‘sample source' is not possible (WHO, 1997). The Human Genome Organization (HUGO), the Council for International Organizations of Medical Sciences (CIOMS; Geneva, Switzerland) and the United Nations' Educational, Scientific and Cultural Organization (UNESCO; Paris, France) have adopted a less-restrictive approach, and allow stored samples and data to be used without re-consent if they are coded and if the research project is approved by an ethics committee (HUGO, 1998; CIOMS, 2002; UNESCO, 2003). Similarly, the COE recommends waiving informed consent for research that uses previously stored materials if they are unidentifiable, provided that “such use does not violate any restrictions placed by the person concerned before the anonymization of materials” (COE, 2006).
The national regulations governing research that makes use of stored materials and the associated data differ widely across a range of consent models. Canada, Germany, Norway, The Netherlands and the USA allow the use of stored samples without consent if they are not identifiable (Knoppers, 2005b; Merz, 2003). In Iceland, the National Bioethics Commission decides whether there is a need to ask donors for new consent to re-use samples (Knoppers, 2005b). In Estonia and the UK, consent is not required to re-use samples because donors are asked to give broad consent to future research when the samples are collected (Knoppers, 2005b).
When it comes to so-called secondary uses—research using human biosamples and related data specifically removed or collected for present and/or future uses—the various forms of informed consent recommended differ at international, European and national levels (Table 1). The CIOMS requires that subsequent studies should be circumscribed by the original consent, and that any conditions specified in the initial consent equally apply to secondary uses (CIOMS, 2002). In its Declaration on Human Genetic Data, UNESCO states that secondary uses that are incompatible with the clauses set out in the original consent form require renewed consent except in health emergencies; conversely, when the secondary uses involve related conditions, re-consent is not necessary (UNESCO, 2003). The WHO recognizes the possibility of a limited broad consent for future research, but only when data and samples are anonymized (WHO, 1997).
At the European level, both legislation and ethical recommendations tend towards requiring the consent to be as strict as possible. The COE, in its Convention for the Protection of Human Rights and Dignity of the Human Being, states that, “consent for using body parts for purposes other than that for which they were originally removed should be appropriate according to national laws”, but declares in the Additional Protocol to the Convention that consent for such uses should be specific (COE, 1997, 2005). Similarly, the COE recommendation about research on biological materials of human origin requires specific consent for any foreseen research use and as specific a consent form as possible for unplanned research studies (COE, 2006).
…the fragmentation in biobanking regulations regarding the use of biosamples and related data affects prospective research more than retrospective research
At a national level, every country has different requirements. The Common Rule in the USA calls for voluntary informed consent, and oversight of each research protocol and consent process by a local institutional review board (IRB; Merz, 2003). The US National Bioethics Advisory Commission (NBAC) report on Research Involving Human Biological Materials is more rigorous and requires that research consent forms provide the potential subject with several options, ranging from complete refusal for the use of samples in research, through a series of limited permissions, to allow the coded use of the materials for any type of future study (multi-layered consent; NBAC, 1999).
Germany, Iceland, the UK, Switzerland, Estonia, Japan and Latvia largely recommend broad consent models (Maschke, 2005). Other countries, such as Denmark, The Netherlands, Spain and Norway, recommend that consent should be informed, and express—but do not clarify—the type of consent that should be sought for biobank research (Knoppers, 2005b). Italy, France and Sweden explicitly require specific informed consent. Australia states that consent to the future use of data and tissue in research might be specific, extended or unspecified (Table 1).
Broad consent is not truly informed consent, but rather is a generic authorization that sacrifices the right of the donor to self-determination in favour of research interests
Our review of the consent forms used at our hospital (Table 3) revealed that no separate form was used specifically for the collection and storage of human biological samples and their related data for research, although a request for consent to store samples and data for future research was generally part of the informed consent used for diagnostic and/or therapeutic procedures. This consent section covers residual biomaterials, such as blood, tissues, organ parts or DNA, from routine or invasive diagnostic procedures (∼90%) and surgical interventions (∼10%).
The review also showed that the applied consent procedures did not differentiate between information and consent, but rather summarized them on a single sheet. In terms of the content and extent of the patient information, most consent forms provided some generally vague information about banking procedures, the purpose of future studies and privacy protection measures. A few provided specific information about the storage and future use of biological materials, the treatment of related data and the right of donors to refuse consent to the storage or future use of the collected samples.
On the basis of these reviews, the IBUG legal expert drafted a unified model of informed consent for the storage of biological samples for specific research studies and future investigations (Fig 1). The information letter that she produced contains: specific information about the storage of biological samples and related data, and about the nature and purposes of the studies to be carried out; general information about studies that could be developed in the future in association with the original research; specific information on privacy issues, and on donor authorization to use anonymous samples and data for scientific publications, teaching purposes or commercialization; specific information on the right of the donors to request and obtain details of the status of the work and general study results; and specific information about the right to withdraw consent and request the destruction or irreversible anonymization of samples and data. The consent form covers: the donor's consent to storing his or her samples and related data collected at the IB; consent to specific studies and associated future investigations; consent to use the results from these studies for scientific publications, teaching purposes or commercial products; the donor's declaration that he or she has been informed of the right to withdraw consent at any time; and the donor's declaration that he or she has been informed of the right to request the results obtained from using the biological samples and related data.
The final version of the model was approved by the IBUG, and the consent template was endorsed by the ethics committee at our hospital in which the IB is located. It has therefore become an officially approved procedure to be referred to for any research studies that use biological samples and related data.
Our review of ethical and legal documents confirmed the current lack of unified regulations about biobank-based research. Although some academics criticize the importance attributed to informed consent for biobanking (Brekke & Sirnes, 2006), the review also showed that defining consent requirements for the collection, storage and use of biological samples and related information for research remains one of the most controversial issues in the international debate (Cambon-Thomsen, 2004). The root of the controversy is the differing international, European and national regulations. Retrospective research is more efficiently regulated by adopting the rule of waiving informed consent when the samples and data are made anonymous and other conditions are met, whereas prospective research is governed by a patchwork of ethical and legal provisions (Maschke, 2005). In this regard, both US and European legislations and guidelines are moving towards a model that requires a specific consent form, at least for identified or identifiable biomaterials and data. By contrast, national laws and regulations in Europe and elsewhere tend to rely on broad consent if the samples and data are made anonymous, if the research project is approved by an ethics committee or other competent body and if it is possible for participants to ‘opt out' (Elger & Caplan, 2006).
The review of the consent procedures used at our hospital confirmed the tendency to adopt a broad consent model, and showed that most consent forms provide generic information about the storage and future use of the specimens. On the basis of these reviews, the IBUG approved an informed consent model for the collection and storage of human biological samples and data for research purposes, which is consistent with the partially restricted model proposed by the WHO; it respects individual autonomy while facilitating research using biological materials. A model that allows specified research and related future—and often unplanned—investigations allows donors to make informed decisions about the handling of their samples and related data, and therefore respects their right to self-determination. The decision of a subject to allow or refuse the use of his or her samples and data for research is based on sufficiently detailed information about future studies, while, simultaneously, the model allows research to proceed and therefore promotes the interests of donors in improving the healthcare system. In other words, a partially restricted form of consent for biobank research balances the sometimes conflicting interests of donor autonomy and medical research.
In agreement with several academics (Arnason, 2004; Beskow et al, 2001), the IBUG felt that other consent templates did not adequately achieve this crucial balance. Broad consent is not truly informed consent, but rather is a generic authorization that sacrifices the right of the donor to self-determination in favour of research interests. Multi-layered and fully restricted consent, by contrast, protects donor autonomy at the expense of research and the interest of the donor in biomedical progress. The IBUG makes no claim that its choice and reasoning represent the only way of dealing with the subject of informed consent, but it is certainly a practical and ethical option.
Other groups are also developing regulatory systems for biobanks. Lundberg & Lindblad (2001) used a self-administered questionnaire to evaluate the attitudes and perceptions of potential donors of biological samples, by asking random samples of the general public, blood donors and patients to rate the risks and benefits associated with different uses of biological samples. Their analysis of 2,928 responses showed that public trust in authorities to balance the risks and benefits of genetic research varied, although most respondents showed a positive attitude towards genetic research, and 86% declared their willingness to donate a blood sample for this purpose on the basis of generic consent. A similar study showed that most potential tissue-sample donors (72%) preferred general consent when they had to balance these values (Hoeyer et al, 2004).
A further study used a biobank model that was based on the role of a ‘medical archivist' (Aurays-Blais & Patenaude, 2006). Such an archivist would have several responsibilities including: verifying the informed consent of participants in accordance with the protocol and consent form; advising the local ethics committee on coding the samples; giving a secondary code to the stored samples; and being the key-holder of the secondary code. The type of informed consent recommended by the analysis depended on the nature of the study to be carried out. For specified research projects the consent was strictly informed, whereas for future unspecified studies the type of consent was to be decided by the ethics committee. Setting aside their methodological differences, these projects confirm the remarkable variability in the regulatory requirements for existing informed consent procedures. In particular, comparing these studies highlighted the tendency to support broad consent as a model that promotes research while respecting donor autonomy.
In line with these studies, the decision of the IBUG to opt for a partially restricted consent template was justified on the basis of respecting individual autonomy. In this view, the development of biomedical research including biobanking and the subsequent promotion of the interests of donors necessarily goes through the hierarchy of the ethical value scale of each donor—autonomy, beneficence and justice (Engelhardt, 1986). However, this is just one of the factors at stake in biobank research, and the choice of what might be ‘appropriate' ethics remains controversial and highlights the need for further study (Cambon-Thomsen et al, 2007; Williams, 2005).
We acknowledge that some limitations need to be overcome before our approach can be translated into other settings. First, our project originated in a hospital department with a long experience of cell, tissue and organ collection/donation, which facilitated the generally positive attitude of the operators. Second, we are still in the early phase of monitoring the efficacy of the model implemented in our hospital, and we do not yet know if the level of the information provided to donors has been improved by our informed consent model.
Multi-layered and fully restricted consent […] protects donor autonomy at the expense of research and the interest of the donor in biomedical progress
Nevertheless, we believe that our informed consent model will facilitate future biobank-based research while appropriately balancing the conflicting interests and principles, although we are aware that the rapid expansion of biobanks and related research will inevitably give rise to new issues. It is therefore likely that the clauses proposed here will require modification or adaptation in the future. Finally, we believe that enhancing the public trust in research is vital to accomplish important social aims. In this regard, we look towards the analysis of perceptions of, and attitudes towards, donating biological samples for biobank-based research.
Acknowledgments
The project was supported by: a grant for the development of a participative model for umbilical cord blood donation for research and therapeutical applications from the Swiss Foundation for Research on Transfusion and Transplantation; the Italian Ministry of Health; the Telethon project GTF02008; the Eurobiobank project QLTR-2001-02769; the Eurogentest-Network of Excellence; and the Fondazione Il Sangue. The authors are grateful to Jon F. Merz and Lisa Miranda for helpful discussions of the manuscript.
Footnotes
The authors declare that they have no conflict of interest.
References
- Anderlik MR (2003) Commercial biobanks and genetic research: ethical and legal issues. Am J Pharmacogenomics 3: 203–215 [DOI] [PubMed] [Google Scholar]
- Arnason V (2004) Coding and consent: moral challenges of the database project in Iceland. Bioethics 18: 27–49 [DOI] [PubMed] [Google Scholar]
- Aurays-Blais C, Patenaude J (2006) A biobank management model applicable to biomedical research. BMC Med Ethics 4: 1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azarov KS, Olmstead FL, Hume RF, Myers J, Calhoun BC, Martin LS (2003) Ethical use of tissue samples in genetic research. Mil Med 168: 437–441 [PubMed] [Google Scholar]
- Beskow LM, Burke W, Merz JF, Barr PA, Terry S, Penchaszadeh VB, Gostin LO, Gwinn M, Khoury MJ (2001) Informed consent for population-based research involving genetics. JAMA 18: 2315–2321 [DOI] [PubMed] [Google Scholar]
- Boggio A, Adorno NB, Bernice E, Mauron A, Capron AM (2007) Comparing Guidelines on Biobanks: Emerging Consensus and Unresolved Controversies. Geneva, Switzerland: Réseau Universitaire International de Genève [Google Scholar]
- Brekke OA, Sirnes T (2006) Population biobanks: the ethical gravity of informed consent. Biosocieties 1: 385–398 [Google Scholar]
- Cambon-Thomsen A (2004) The social and ethical issues of post-genomic human biobanks. Nat Rev Genet 5: 866–873 [DOI] [PubMed] [Google Scholar]
- Cambon-Thomsen A, Rial-Sebbag E, Knoppers BM (2007) Trends in ethical and legal frameworks for the use of human biobanks. Eur Respir J 30: 373–382 [DOI] [PubMed] [Google Scholar]
- CIOMS (2002) International Ethical Guidelines for Biomedical Research Involving Human Subjects. Geneva, Switzerland: Council for International Organizations of Medical Sciences [PubMed] [Google Scholar]
- COE (1997) Convention for the Protection of Human Rights and Dignity of the Human Being with Regard to the Application of Biology and Biomedicine. Strasbourg, France: Council of Europe [DOI] [PubMed] [Google Scholar]
- COE (2005) Treaty Series No. 195, Human Rights and Biomedicine. Protocol on Biomedical Research. Strasbourg, France: Council of Europe [Google Scholar]
- COE (2006) Recommendation of the Committee of Ministers to Member States on Research on Biological Materials of Human Origin. Strasbourg, France: Council of Europe [Google Scholar]
- Elger BS, Caplan AL (2006) Consent and anonymization in research. EMBO Rep 7: 661–666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelhardt HT (1986) The Foundations of Bioethics. Oxford, UK: Oxford University Press [Google Scholar]
- Godard B, Schmidtke J, Cassiman JJ, Aymé S (2003) Data storage and DNA banking for biomedical research: informed consent, confidentiality, quality issues, ownership, return of benefits. A professional perspective. Eur J Human Genet 11 (Suppl 2): 88–122 [DOI] [PubMed] [Google Scholar]
- Grizzle W, Grody WW, Noll WW, Sobel ME, Stass SA, Trainer T, Travers H, Weedn V, Woodruff K (1999) Recommended policies for uses of human tissue in research, education, and quality control. Ad hoc Committee on Stored Tissue, College of American Pathologists. Arch Pathol Lab Med 123: 296–300 [DOI] [PubMed] [Google Scholar]
- Hansson MG, Dillner J, Bartram CR, Carlson JA, Helgesson G (2006) Should donors be allowed to give broad consent to future biobank research? Lancet Oncol 7: 266–269 [DOI] [PubMed] [Google Scholar]
- Hirtzlin I et al. (2003) An empirical survey on biobanking of human genetic material and data in six EU countries. Eur J Hum Genet 6: 475–488 [DOI] [PubMed] [Google Scholar]
- Hoeyer K, Oloffson BE, Mjorndal T, Lynoe N (2004) Informed consent and biobanks: a population-based study of attitudes towards tissue donation for genetic research. Scand J Public Health 3: 224–229 [DOI] [PubMed] [Google Scholar]
- HUGO (1998) Statement on DNA Sampling: Control and Access. London, UK: Human Genome Organization [Google Scholar]
- Kaye J (2005) Do we need a uniform regulatory system for biobanks across Europe? Eur J Hum Genet 14: 245–248 [DOI] [PubMed] [Google Scholar]
- Knoppers BM (2001) Ethical aspects of genome research and banking. In Genomics and Bioinformatics, Rehm HJ, Reed G (eds), pp 418–429. Weinheim, Germany: Wiley [Google Scholar]
- Knoppers BM (2005a) Consent revisited: points to consider. Health Law Rev 13: 33–38 [PubMed] [Google Scholar]
- Knoppers BM (2005b) Biobanking: international norms. J Law Med Ethics 33: 7–14 [DOI] [PubMed] [Google Scholar]
- Korn D (1999) Contribution of the human tissue archive to the advancement of medical knowledge and the public health. In National Bioethics Advisory Commission, Research involving Human Biological Materials: Ethical Issues and Policy Guidance, Vol II, pp E1–E30. Rockville, MD, USA: National Bioethics Advisory Commission [Google Scholar]
- Lundberg L, Lindblad A (2001) Empirical research on informed consent and biobanks. In The Use of Human Biobanks. Ethical, Social, Economical and Legal Aspects, Hansson MG (ed), pp 53–54. Uppsala, Sweden: Uppsala University [Google Scholar]
- Maschke KJ (2005) Navigating an ethical patchwork—human gene banks. Nat Biotechnol 5: 539–545 [DOI] [PubMed] [Google Scholar]
- Merz JF (2003) On the intersection of privacy, consent, commerce and genetic research. In Populations and Genetics: Legal Socio-Ethical Perspectives, Knoppers BM (ed), pp 257–268. New York, NY, USA: Kluwer Legal International [Google Scholar]
- NBAC (1999) Research Involving Human Biological Materials: Ethical Issues and Policy Guidance, Vol I. Rockville, MD, USA: National Bioethics Advisory Commission [Google Scholar]
- Rebulla P, Lecchi L, Giovanelli S, Butti B, Salvaterra E (2007) Biobanking in the year 2007. Transfus Med Hemother 34: 284–192 [Google Scholar]
- Trouet C (2004) New European guidelines for the use of stored human biological materials in biomedical research. J Med Ethics 30: 99–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNESCO (2003) International Declaration on Human Genetic Data. Paris, France: United Nations Educational, Scientific and Cultural Organization [Google Scholar]
- WHO (1997) Proposed International Guidelines on Ethical Issues in Medical Genetics and Genetic Services. Geneva, Switzerland: World Health Organization [Google Scholar]
- WHO (2003) Guideline for Obtaining Informed Consent for the Procurement and Use of Human Tissues, Cells, and Fluids in Research. Geneva, Switzerland: World Health Organization [Google Scholar]
- Williams G (2005) Bioethics and large scale biobanking: individualistic ethics and collective projects. Genomics Soc Policy 2: 50–66 [Google Scholar]