Abstract
Background
Poor linkage with substance abuse treatment remains a problem, negating the benefits that can accrue to both substance abusers and the larger society. Numerous behavioral interventions have been tested to determine their potential role in improving linkage.
Methods
A randomized clinical trial of 678 substance abusers compared the linkage effect of two brief interventions with the referral standard of care (SOC) at a centralized intake unit (CIU). Interventions included five sessions of strengths-based case management (SBCM) or one session of motivational interviewing (MI). A priori hypotheses predicted that both interventions would be better than the standard of care in predicting linkage and that SBCM would be more effective than MI. We analyzed the effect of the two interventions on overall treatment linkage rates and by treatment modality. Logistic regression analysis examined predictors of treatment linkage for the sample and each group.
Results
Two hypotheses were confirmed in that SBCM (n = 222) was effective in improving linkage compared to the SOC (n = 230), 55.0% vs. 38.7% (p < .01). SBCM improved linkage more than MI (55.0% vs. 44.7%, p < .05). Motivational interviewing (n = 226) was not significantly more effective in improving linkage than the standard of care (44.7% vs. 38.7%; p > .05). The three trial groups differed only slightly on the client characteristics that predicted linkage with treatment.
Conclusions
The results of this study confirm a body of literature that supports the effectiveness of case management in improving linkage with treatment. The role of motivational interviewing in improving linkage was not supported. Results are discussed in the context of other case management and motivational interviewing linkage studies.
Keywords: Case management, Motivational interviewing, Linkage, Substance abuse treatment
1. Introduction
Substantial personal and societal benefits are associated with treatment for substance abusers (Farabee et al., 1998; Hubbard et al., 2003). The advent of widespread, evidence-based treatment interventions (e.g., cognitive behavioral treatments), may herald even better outcomes. No matter what the potential improvement in outcomes, substance abusers cannot benefit if they do not enter, or link with, treatment in the first place.
Linkage with substance abuse treatment is impeded by numerous influences that serve as obstacles, or barriers, to obtaining treatment (Cunningham et al., 1993). Andersen's model of health care utilization suggests three categories of barriers: predisposing characteristics such as gender and age; situational/illness factors such as motivation and perceived extent of substance abuse problem; and inhibiting factors such as homelessness and lack of social support for change (Andersen, 1995). Elements of the health care system pose formidable barriers as well, including waiting time, availability, affordability and accessibility. These barriers rarely operate independently; rather, they interact to interfere with linkage (Rapp, et al., 2006; Tsogia et al., 2001).
1.1. Intervening in Individual and System Barriers
1.1.1. Motivational Interviewing
Motivational Interviewing (MI) is intended to improve the willingness of substance abusers to consider change through a non-confrontive process that encourages them to assess the differences between their current and desired life situations (Miller, 1995). MI has been used to accomplish several treatment goals, including improving linkage with treatment. These studies have generally yielded poor results, although some unintended positive outcomes did occur. For example, clients randomly assigned to a single session of motivational interviewing were not more likely to link with treatment, although those who did link attended more treatment sessions, had more days of abstinence during treatment, and had fewer heavy drinking days 12 months after treatment (Connors et al., 2002). Similarly, dually diagnosed individuals who received MI had greater attendance and less tardiness once they entered treatment, although initial linkage rates were not different from a standard of care pre-admission group (Martino et al., 2002). Substance abusers on a waiting list following assessment at a CIU were no more likely to link with treatment if they had received a motivational intervention than if they had not (Donovan et al., 2001).
MI implemented outside of a drug treatment facility did improve linkage. Sixty parents at a child welfare agency who were referred for a substance abuse evaluation were randomly assigned to either a standard substance abuse evaluation or an evaluation enhanced by Motivational Interviewing techniques, each delivered in a single session (Carroll et al., 2001).
1.1.2. Case Management
Case management has become a ubiquitous social service intervention to assist persons with medical and psychosocial needs identify, access, and utilize community resources (Ballew & Mink, 1996). The core functions of case management—assessment, linking, monitoring, and advocacy—remain constant across almost all applications of case management. At the same time, functions are usually modified to fit specific health and social service systems (Center for Substance Abuse Treatment, 1998; Rapp, 2006). Case managers help clients identify personal impediments to linkage such as transportation, childcare, and lack of social support. Case managers may also advocate with treatment providers on behalf of clients. Broad system change is not usually the intent of case managers, although they do attempt to seek system accommodation on behalf of individual clients.
Clinical trials of case management have spanned diverse populations and settings. Positive linkage effects have been found in trials of injection drug users and methadone maintenance programs (Coviello et al., 2006; Zanis et al., 1996), centralized intake units (Scott et al., 2002), female welfare recipients (Morgenstern, et al., 2006), homeless substance abusers (Braucht, et al., 1995), dually diagnosed substance abusers (Morse, et al., 2006), and substance abusers involved in the criminal justice system (Rhodes & Gross, 1997). In a large retrospective cohort study (N = 7,776) case managed clients were more likely to enter some form of on-going treatment following detoxification than non-case managed clients (Shwartz et al., 1997).
The relative impact of case management combined with a fiscal incentive for treatment was explored elsewhere (Sorensen, et al., 2005). Case management without a voucher for free treatment improved linkage with a methadone maintenance program from 11% to 46%. When case management was coupled with vouchers the linkage rate increased to 93%.
Strengths-based case management (SBCM) has been consistent in improving linkage with treatment in a variety of settings. SBCM is function driven (e.g., monitoring), but is also based on five underlying principles that include an emphasis on strengths and teaching goal setting methods (Siegal, et al., 1995; Rapp, 2006). Linkage rates have been increased among a general population of substance abusers (Vaughan-Sarrazin et al., 2000), opioid dependent drug users entering agonist treatment programs (Strathdee, et al., 2006), and crack cocaine users aftercare treatment (Rapp et al., 1998; Siegal et al., 2002).
A recent meta-analysis examined the case management literature relative to substance abusing populations (Hesse et al., 2007). Studies of case management's role in improving linkage with treatment showed effect sizes that ranged from .08 to .89, with a mean effect size of .42.
1.1.3. Current study
The current study presents results from a clinical trial that tested the effectiveness of two brief clinical interventions on improving linkage and engagement with substance abuse treatment. Following assessment at a centralized intake unit (CIU), substance abusers were randomly assigned to a single session motivational interviewing (MI), up to five sessions of strengths-based case management (SBCM), or the referral standard of care (SOC) at a centralized intake unit. Although previous studies of MI have not demonstrated consistently positive effects on linkage, we still saw it as an appropriate intervention to examine in the context of a centralized intake unit. It is possible that substance abusers who have already made a decision to be assessed, but have not yet actually entered treatment, will be more amenable to MI's intended effects., Enhancing motivation, rather than developing it where it does not exist, may be a suitable role for such a brief intervention.
We hypothesized that: (1) substance abusers receiving SBCM would be more likely to link than the standard of care condition within 90 days following assessment; (2) substance abusers receiving MI would be more likely to link than the standard of care within the 90 days; and (3) substance abusers receiving SBCM would be more likely to link than those receiving MI. Hypotheses #1 and #2 were based on findings that have demonstrated motivational interviewing and strengths-based case management can be effective in improving linkage with treatment services (Carroll et al., 2001; Siegal, et al., 2002). The hypothesis that SBCM would demonstrate a higher linkage rate than MI was based on the broader objectives of SBCM which, in addition to addressing substance abusers' motivational barriers, also addresses tangible barriers such as lack of transportation, waiting lists, and need for childcare (Carr, et al., in press).
This study also considers the effectiveness of the two interventions in improving linkage with three treatment modalities—drug free outpatient, residential, and outpatient methadone maintenance. Finally, logistic regression was used to identify the characteristics of participants who linked with treatment in each study condition. Although we hypothesized that SBCM would be more effective overall, it is possible that MI, a shorter and less expensive intervention, could be just as effective as SBCM for some substance abusers. For example, substance abusers who have tenuous motivation and access to transportation and child care may not need case management, but could benefit from one session of MI.
2. Methods
2.1. Participants
Participants in this study were individuals who had undergone an assessment for a substance abuse problem at the centralized intake unit (CIU) in Montgomery County, OH. Centralized intake units provide standardized intake assessments for substance abusers, use protocols that match individuals with a continuum of appropriate treatment, and provide case management services to assist individuals in linking with services (Stephens, Scott, & Muck, 2003). The CIU is the required point of entry for persons seeking publicly subsidized substance abuse or mental health services. Approximately 5,000 substance abuse assessments are conducted at the CIU each year. CIU assessment therapists conducted a psychosocial and clinical assessment to determine the nature and extent of clients' substance abuse problems. Clients were then referred to an appropriate level of care based on American Society of Addiction Medicine (ASAM) placement criteria (American Society of Addiction Medicine, 2001). The criteria are nationally recognized guidelines for the placement of patients with alcohol and other drug problems. They include: early intervention, outpatient, intensive outpatient/partial hospitalization, residential/inpatient, and medically-managed intensive inpatient treatment. Situational factors such as treatment availability and client preference are also considered in treatment recommendations.
During the assessment interview, therapists conducted a pre-screening for the clinical trial and made referrals to the trial if a client agreed to meet with research staff. Eligibility criteria for inclusion in the study included: (1) 18 years of age or older; (2) diagnosed as having a substance abuse and/or dependence disorder using criteria from the Diagnostic and Statistical Manual (fourth edition) (American Psychiatric Association, 2001); (3) not diagnosed with schizophrenia or any other psychotic disorder; and (4) referred to a state certified specialty substance abuse treatment program, either residential, drug-free outpatient, or outpatient methadone maintenance. Participants were not eligible for the study if they were diagnosed with only alcohol abuse or alcohol dependence.
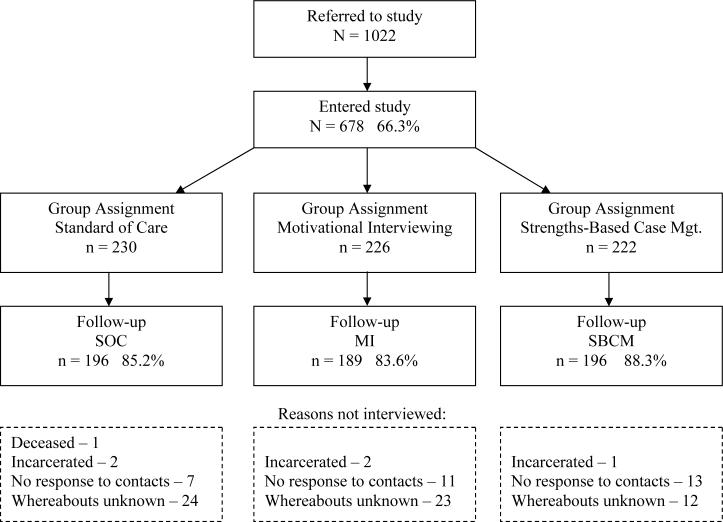
During the course of the present study (April 4, 2004 through June 31, 2006), assessment therapists at the CIU referred a total of 1022 eligible clients to the project. About two-thirds (66.3%, n = 678) of the individuals referred to the study agreed to participate in the baseline interview with a project research assistant (see Figure 1).
Figure 1.
Participant flow through referral, random assignment, and 3 month follow-up
2.2. Design and procedure
2.2.1. Procedure
After completing the CIU assessment process, eligible clients were referred to the study and met with a research assistant. Research assistants read a summary of the project and an informed consent approved by the university's institutional review board. Clients were also informed that this study involved two additional interviews, at three and six months, and were asked to provide follow-up locator information. Individuals who wished to participate in the study then completed a baseline interview lasting approximately 90 minutes. All questions in the baseline interview were read aloud to the participants and research assistants were trained to probe for clarity and completeness of responses. Participants received a $30 stipend for their time spent answering questions at each of the interview points.
After the baseline interview was completed, participants were randomly assigned to one of the three intervention groups, based on a list of random numbers created in advance by the project's research director.
2.2.2. Referral Standard of Care (SOC)
At the completion of their assessment, clients were informed of the recommendation for treatment level (residential, drug-free outpatient, or outpatient methadone maintenance) and the specific treatment program to which they were being referred. Clients were instructed to call the CIU after one week to obtain a specific date on which they could start treatment. When clients called, a CIU care coordinator provided a treatment start date to clients, and in some cases contacted treatment programs to resolve any scheduling difficulties. Care coordinators did not usually make face-to-face contact with the clients, or address barriers to linkage other than scheduling.
2.2.3. Motivational Interviewing (MI)
The Motivational Interviewing in the present study was based on previous studies that used MI as an adjunct to treatment rather than a stand alone treatment intervention such as Motivational Enhancement Therapy (Ball et al., 2007; Miller & Rollnick, 2002). MI was designed to help participants: (1) clarify their desire and motivation for treatment; and (2) reinforce behaviors and attitudes that were consistent with seeking treatment. Following assessment, MI counselors conducted a one hour session, consistent with the precepts of motivational interviewing. The counselor affirmed commitments to immediately seek treatment, as well as other positive steps toward that goal such as being willing to talk about substance use positives and negatives. The MI counselor used the participant's own reports, thoughts and behaviors concerning drug use and/or treatment to highlight discrepancies, the differences between a participant's current life and where they said they wanted to be.
The motivational counselor was trained by a nationally recognized expert in Motivational Interviewing, and had extensive experience working with clients in crisis. Training was reinforced throughout the study by masters-level clinical supervisors who had also received MI training. Fidelity was monitored and maintained through direct observation, review of a random sample of audiotapes of counselor-participant sessions, and review of case notes.
2.2.4. Strengths-Based Case Management
The brief strengths-based case management intervention (SBCM) was adapted from a long term intervention developed to help institutionalized mental health patients return to the community (Rapp & Chamberlain, 1985), and to help substance abusers link with and engage in aftercare services following residential treatment (Rapp, et al., 1998; Siegal, et al., 1995). The SBCM evaluated in this trial has been shown to be effective in helping persons recently diagnosed with HIV link with medical care (Gardner, et al., 2005).
SBCM has two broad components: case management functions and strengths-based principles. Functions include assessment, planning, linking, monitoring, and advocacy (Ballew & Mink, 1996). Strengths-based principles are: (1) help clients to use their strengths, abilities, and assets to facilitate linkage with treatment; (2) encourage client decision-making in plans to link with treatment; (3) promote the client and case manager relationship; (4) encourage client participation in informal sources of assistance; and (5) make contact with clients in their own environment (Rapp, 2006). The functions of case management and the principles that guide a strengths-based approach are operationalized in manuals created for this and previous studies (Gardner, et al., 2005). Each of the case management sessions are described in detail in the manual.
Participants in the SBCM condition met with their case managers for up to five sessions. Case managers helped clients identify personal skills, abilities, and assets through discussions guided by the SBCM manual. A detailed case management plan was developed that: (1) identified barriers to treatment and how to resolve them; and (2) taught participants a goal-setting process that included identifying personal goals, objectives, and strategies (Rapp, 2006).
The two study case managers were trained by clinical supervisors who emphasized how the strengths approach could be integrated into usual case management functions. The case managers also had extensive experience in working with substance abuse populations and in using community resources to improve clients' quality of life. Two masters-level supervisors assessed the fidelity with which the case managers delivered SBCM. Fidelity was monitored and maintained through direct observation of case manager/participant interactions using a fidelity scale keyed to the manual (Marty et al., 2001). Case managers' discussion of clients during supervision sessions and case manager case notes were also evaluated on a weekly basis using the fidelity scale.
2.2.5. Measurement of linkage with treatment
The primary outcome of the clinical trial was linkage with substance abuse treatment within 90 days of a CIU assessment. Linkage was defined as meeting with a treatment center counselor in individual, group, or family counseling. Administrative (pre-linkage) contacts spent in providing admission information were not counted as clinical contacts. The decision to use a 90-day period for linkage was based on State of Ohio administrative rules that require that a new assessment be conducted if treatment entry does not occur within 90 days. The focus of the current paper is linkage to treatment; results related to treatment engagement will be presented elsewhere.
3. Measures
An extensive baseline questionnaire contained questions regarding participant characteristics such as gender, race, age, education level, treatment history, and current legal system involvement. Information about situational and enabling/inhibiting characteristics included: drug use, housing, employment patterns, HIV risk behaviors, and critical life events. Data were collected for lifetime, six month, and 30 day periods. The interview included all items from the Addiction Severity Index (ASI), Version 5 (McLellan, 1992). Composite scores from each of the seven ASI areas are based on items representing functioning during the 30 days before the interview.
The baseline interview also included the Pre-treatment Readiness Scale (PRS) (Rapp et al., 2007) which was developed to determine readiness for treatment in substance abusers assessed and referred to treatment, but not yet in treatment. This instrument consists of four subscales. Summary scores for each of the readiness subscales were used in the analysis. These subscales with the number of items, summary score range, and reliability coefficient include: (a) Problem Recognition (10 items; 10−50; .90); (b) Desire for Change; (3 items; 3−15; .57); (c) Treatment Readiness (4 items; 4−20; .82); and (d) Treatment Reluctance (3 items; 3−15; .69).
Also included in the baseline interview was the 59-item Barriers to Treatment Inventory (Rapp et al., 2006), which was developed specifically for this trial to identify barriers that substance abusers experienced prior to treatment. Factors (with number of items, summary score range and reliability) include: (a) Problem Absence (6 items; 6−30;.86); (b) Negative Social Support (5 items; 5−25;.77); (c) Treatment Fear (4 items; 4−20; .76); (d) Privacy (3 items; 3−15;.80); (e) Committed Lifestyle (2 items; 2−10; .57); (f) Time Conflict (4 items; 4−20;.80); (g) Poor Treatment (4 items; 4−20; .66); (h) Admission Difficulty (2 items; 2−10;.65), and (i) Financial Problems (2 items; 2−10; .82). Participants were asked to indicate on a five-point Likert scale (1 = disagree strongly; 5 = agree strongly) how much they believed that each barrier would affect their entry into treatment.
The Reducing Barriers Project Services Tracking Record (STR) was used to gather data on treatment linkage, treatment retention (amount, duration, frequency), type of treatment contacts, medications prescribed, urinalysis results, ancillary services provided by the program, referrals to other services, and discharge status.
4. Results
The effectiveness of the two interventions was established by using intent-to-treat analyses, that is, all participants assigned to each group were retained in analyses whether they actually received the intervention or not. There were no missing data for linkage status.
4.1. Baseline sample
A total of 678 CIU clients consented to participate in the study and completed the baseline interview. The sample included 429 men (63.3%) and 249 women (36.7%). The sample was 51.0% Caucasian and 48.1% African American. The average age of the clients was 33.40 years (SD = 10.04, range 18−64). Only 58.0% of the clients were employed in the six months before coming to the CIU, and 20.2% of the clients were homeless. Half (50.3%) of the respondents described themselves as currently involved in the criminal justice system. The majority of the clients (70.1%) had prior treatment experience. Participants identified their most serious substance problem as: crack or powder cocaine (45.6%), heroin (22.0%), marijuana (14.9%), alcohol (11.6%), or other drugs (5.9%). The CIU referred approximately half (49.7%) of the participants to drug free outpatient treatment and another 31.9% were referred to residential programs. Only 18.4% of participants were referred to an outpatient methadone maintenance program. Despite random assignment, the intervention conditions did differ on two of the variables. Participants assigned to the MI condition were lower in psychiatric severity and were also more likely to say that they did not have a substance abuse problem. There were no other significant pre-existing differences among the groups. See Table 1 for a complete description of sample characteristics broken down by intervention condition.
Table 1.
Comparison of Sample Characteristics by Total Sample and Intervention Condition
| SOC n = 230 |
MI n = 226 |
SBCM n = 222 |
Total Sample n=678 |
|
|---|---|---|---|---|
| Age | 33.6 | 32.9 | 33.8 | 33.4 |
| Gender (%) | ||||
| Male | 63.0 (145) | 63.3 (143) | 63.5 (141) | 63.3 (429) |
| Female | 37.0 (85) | 36.7 (83) | 36.5 (81) | 36.7 (249) |
| Ethnicity (%) | ||||
| White | 51.3 (118) | 52.7 (119) | 49.1 (109) | 51.0 (346) |
| African American | 47.4 (109) | 46.9 (106) | 50.0 (111) | 48.1 (326) |
| Other | 1.3 (3) | 0.4 (1) | 0.9 (2) | 0.9 (6) |
| Involved in CJ system (%) | ||||
| Yes | 50.0 (115) | 52.2 (118) | 48.6 (108) | 50.3 (341) |
| Homeless (%) | ||||
| Yes | 18.7 (43) | 16.8 (38) | 25.2 (56) | 20.2 (137) |
| Prior Treatment (%) | ||||
| Yes | 68.7 (158) | 69.5 (157) | 72.14 (160) | 70.1 (475) |
| Education Level | 11.4 | 11.2 | 11.0 | 11.2 |
| Drug of Choice (%) | ||||
| Alcohol | 12.7 (29) | 13.8 (31) | 8.2 (18) | 11.6 (78) |
| Heroin | 19.3 (44) | 22.7 (51) | 24.1 (53) | 22.0 (148) |
| Cocaine/Crack | 47.4 (108) | 39.6 (89) | 50.0 (110) | 45.6 (307) |
| Cannabis | 14.0 (32) | 17.8 (40) | 12.7 (28) | 14.9 (100) |
| Other | 6.6 (15) | 6.2 (14) | 5.0 (11) | 5.9 (40) |
| Barriers to Treatment | ||||
| Absence Problem* | 10.67 | 11.52 | 10.13 | 10.77 |
| Negative Social Support | 8.11 | 7.98 | 8.12 | 8.07 |
| Treatment Fear | 7.47 | 7.18 | 7.01 | 7.22 |
| Privacy Concerns | 8.18 | 7.77 | 8.16 | 8.02 |
| Committed Lifestyle | 4.97 | 4.88 | 5.05 | 4.96 |
| Time Conflict | 3.93 | 3.85 | 3.74 | 3.87 |
| Poor Treatment Availability | 5.40 | 5.32 | 5.28 | 5.33 |
| Admission Difficulties | 5.25 | 4.98 | 5.06 | 5.10 |
| Financial Problem | 7.59 | 7.75 | 7.48 | 7.61 |
| Pre-Treatment Readiness | ||||
| Problem Recognition | 39.28 | 37.64 | 39.50 | 38.81 |
| Desire for Change | 13.71 | 13.61 | 13.90 | 13.74 |
| Treatment Readiness | 17.53 | 17.37 | 17.76 | 17.55 |
| Treatment Reluctance | 6.45 | 6.50 | 6.17 | 6.37 |
| ASI Composites | ||||
| Psychiatric * | .278 | .226 | .285 | .263 |
| Alcohol | .153 | .124 | .160 | .146 |
| Drug | .195 | .201 | .205 | .200 |
| Medical | .199 | .211 | .251 | .220 |
| Family/Social Support | .195 | .183 | .201 | .193 |
| Legal | .202 | .223 | .200 | .209 |
| Employment | .772 | .771 | .792 | .778 |
| Modality Referred to (%) | ||||
| Residential | 33.5 | 29.2 | 32.9 | 31.9 (216) |
| Outpatient | 50.0 | 50.0 | 49.1 | 49.7 (337) |
| Methadone | 16.5 | 20.8 | 18.0 | 18.4 (125) |
p < .05
There were no significant differences in the three month follow-up interview rate for the three study groups: SOC, 85.2%; MI, 83.6%; SBCM, 88.3%. Participants in the SBCM group attended a mean of 2.3 sessions; linkers attended 2.9 sessions and non-linkers, 1.6 sessions.
4.2. Linkage to treatment by condition
The linkage rate for the total sample was 46.0%. The relationship between intervention condition (SOC, MI, or SBCM) and linkage was examined using a Chi-Square test of association. There was a significant relationship between the type of intervention participants received and whether they linked with treatment, χ2 (2, N = 678) = 12.26, p < .01. To test the specific a priori hypotheses about differences between the interventions, a series of z-tests of proportions was conducted. Results revealed that there was no significant difference between the proportion of participants in the SOC group who linked (38.7%) when compared with participants in the MI group who linked (44.7%), z = 1.30, p > .05. However, participants in the SBCM group (55.0%) did link at a significantly higher rate than the SOC group, z = 3.46, p < .001. There was also a significant difference in linkage rate between the MI group and the SBCM group, z = 2.17, p < .05. Table 2 contains the linkage rate for each study condition.
Table 2.
Percent of Participants Who Linked by Intervention Condition and Treatment Modality
| SOC | MI | SBCM | Total | |
|---|---|---|---|---|
| Modality | ||||
| Residential | 39.0 | 43.9 | 56.2 | 46.3a |
| Outpatient | 28.7c | 43.4 | 52.3c | 41.2b |
| Methadone |
68.4 |
48.9 |
60.0 |
58.4a, b |
| Total | 38.7d | 44.7e | 55.0d, e | 46.0 |
Note. All values are percentages. Percentages with the same superscript are significantly different. a, e p < .05, c p < .01, b, d p < .001
4.3. Linkage by treatment modality
After assessment at the CIU, participants received referrals to one of three types of programs: inpatient residential treatment (n = 216), outpatient drug-free (n = 337), or methadone maintenance (n = 125). Linkage rates for the three modalities were: inpatient residential (46.3%), outpatient drug free (41.2%), and methadone maintenance (58.4%). A Chi-Square test of association showed that there was a relationship between treatment modality and linkage with treatment, χ2 (2, N = 678) = 10.81, p < .01.
Chi-Square analysis was also used to look at the effect of group assignment (SOC, MI, or SBCM) on linkage in each of the treatment modalities. For the residential treatment modality there was no relationship between group assignment and whether participants linked, χ2 (2, N = 216) = 4.67, p > .05. Nor was there a relationship between assignment and linkage for participants assigned to methadone maintenance, χ2 (2, N = 125) = 3.35, p > .05. There was, however, a significant relationship in the outpatient treatment modality, χ2 (2, N = 337) = 13.17, p < .01. These results were further examined with a series of post hoc z-tests of proportions with Bonferroni correction for familywise error. There was no significant difference in the proportion of participants in the SOC group who linked with outpatient treatment (28.7%) and participants in the MI group who linked (43.4%), z = 2.31, p > .05. Participants in the SBCM group, however did link at a significantly higher rate (52.3%) than participants in the SOC group, z = 3.60, p < .01. Finally, there was no significant difference between the MI group and the SBCM group in linkage to outpatient treatment, z = 1.33, p > .05. See Table 2 for modality linkage rates.
4.4. Predictors of linkage to treatment
A logistic regression analysis was conducted to identify the predictors of linkage to treatment. Predictor variables included: gender, race, age, education level, homelessness, involvement in the criminal justice system, problem severity, and prior treatment experience. Participant perceptions of barriers to treatment and pre-treatment motivation were also included in the model. Finally, dummy variables were included to indicate whether or not participants received case management or motivational interviewing.
The results of the analysis, presented in Table 3, clearly indicated that the set of predictors successfully distinguished between participants who linked with treatment and those who did not, χ2 = 85.58, p < .001, Nagelkerke R2 = .16. The model also demonstrated the ability to correctly predict participants' outcome category (linkage vs. no linkage). Specifically, the model correctly predicted the outcome category of 73.0% of the participants who did not link and 59.9% of those who did link. The overall prediction success rate was 67.0%.
Table 3.
Significant Predictors of Linkage for Overall Sample and Each Intervention Condition
| Overall |
SOC |
MI |
SBCM |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | B | Wald χ2 | Odds Ratio | B | Wald χ2 | Odds Ratio | B | Wald χ2 | Odds Ratio | B | Wald χ2 | Odds Ratio |
| Male | -.37 | 4.04* | .69 | -.73 | 4.54* | .48 | ||||||
| Higher Education Level | .10 | 4.43* | 1.11 | .21 | 4.32* | 1.23 | ||||||
| Prior Treatment | .56 | 8.06** | 1.75 | |||||||||
| Homeless | -.47 | 3.98* | .63 | |||||||||
| Problem Recognition | −.08 | 5.61* | .93 | |||||||||
| Alcohol Severity | −1.62 | 14.77*** | .20 | −2.75 | 7.28** | .06 | −1.84 | 6.46* | .16 | |||
| Intervention Groups | ||||||||||||
| Reference Group: SOC | ||||||||||||
| Motivational Interviewing | ||||||||||||
| Strengths-Based Case Mgmt. | .76 |
13.45*** |
2.13 |
|
|
|
|
|
|
|
|
|
| χ2 = 86.58, p < .001, Nagelkerke R2 = .16 | χ2 = 39.72, p = .054, Nagelkerke R2 = .22 | χ2 = 37.37, p = .088, Nagelkerke R2 = .20 | χ2 = 36.25, p = .110, Nagelkerke R2 = .20 | |||||||||
p < .05
p < .01
p < .001
Six different variables included in the model were significant predictors of linkage across the entire sample. The strongest predictor was whether participants were in the SBCM condition [z = 13.45, p < .001, odds ratio (OR) = 2.13]. Participants in the SBCM condition were 2.13 times more likely to link with treatment than those who were not in the SBCM condition. MI, however, was not a significant predictor of linkage (z = 1.08, p > .05). Men were less likely to link (z = 4.04, p < .05, OR = .69). Participants with more years of education were more likely to link (z = 4.43, p < .05, OR = 1.11). Participants who were homeless were less likely to link with treatment (z = 3.98, p < .05, OR = .68) while participants who had prior treatment experience were more likely to link with treatment (z = 8.06, p < .01, OR = 1.75). None of the scales from the BTI or the PRS were significant predictors in this model; however, the ASI composite score which measures alcohol use was, (z = 14.77, p < .001, OR = .20).
4.5. Predictors of linkage by type of intervention
To examine whether the pattern of predictors of linkage differed depending on the type of intervention participants received, three separate logistic regressions were conducted. The same set of predictors used for the entire sample was also included in logistic regression analyses for each study condition. Results are presented in Table 3.
4.5.1. SOC group
For participants who were randomly assigned to receive the standard of care by the CIU, the logistic regression model indicated that the set of predictors did not successfully distinguish between those who linked to treatment and those who did not, χ2 = 39.72, p = .05; Nagelkerke R2 = .22. There were only two significant predictors of linkage for participants in the SOC group. The first of these was gender, z = 4.54, p < .05, OR = .48. Men were less likely to link with treatment than were women. The second predictor was Problem Recognition, one of the scales from the PTR, z = 5.61, p < .05, OR = .927. Participants who showed less problem recognition were more likely to link with treatment.
4.5.2. MI group
There were two significant predictors of linkage for the MI group. First, participants with higher levels of education were more likely to link with treatment, z = 4.32, p < .05, OR = 1.23. Second, participants who had higher alcohol use problems, as measured by the ASI, were less likely to link with treatment, z = 7.28, p < .01, OR = .064.
4.5.3. SBCM group
There was only one significant predictor of linkage to treatment in the SBCM group. Participants who had more severe alcohol use problems, as measured by the ASI, were less likely to link with treatment, z = 6.46, p < .05, OR = .16.
5. Discussion
The current study describes the results of a clinical trial of two interventions that were intended to help substance abusers link with substance abuse treatment. Strengths-based case management was designed to help substance abusers identify and resolve barriers to treatment entry; motivational interviewing was designed to develop or build on existing motivation. The hypotheses that predicted SBCM would be more effective than the SOC and MI groups were supported; the remaining hypothesis that MI would be more effective than the SOC group in improving linkage was not supported.
Six of the seven predictors included in the overall model, including case management assignment, affected the odds of a participant linking with treatment. Having had prior treatment, being female, not homeless, having more education, and having less alcohol severity all predicted a better chance of linking with treatment. No client characteristics were consistent predictors of linkage across the three study groups, although alcohol severity did predict linkage in the MI and SBCM groups.
5.1. Strengths-Based Case Management
Substance abusers who were assessed at a centralized intake unit and received SBCM linked with treatment 18% more often than a standard of care group; the odds of linking with treatment were doubled. These findings are consistent with a sizable body of literature that has found a positive effect for case management in facilitating linkage with treatment. Our findings also point to three themes found in other case management studies, including models of case management, length of case management interventions, and contextual issues surrounding case management.
5.1.1. Models of case management
Several models of case management are routinely identified in the case management literature, whether applied to substance abuse or other problems. This study demonstrated a positive linkage effect from strengths-based case management. Other models that have been used to facilitate linkage include brokerage, general, intensive, and assertive (Center for Substance Abuse Treatment, 1998). Case managers help substance abusers assess their own situation, as well as identify, link, and stay involved in services. Positive linkage outcomes have been attributed to each of these models. In a recent metaanalysis, effect sizes were calculated for several of these models, including: assertive community treatment, .74; strengths-based, .70; brokerage, .68; and, general, .20 (Hesse, et al., 2007).
The cross model success of case management suggests that different case management models may have some mechanism in common that leads to successful linkage. Transportation related variables including distance to treatment, having access to a car, and having a case manager to provide transportation to treatment, have been suggested as one mechanism of action (Strathdee, et al., 2006). Using a manual-based case management intervention also predicted linkage with treatment (Coviello, et al., 2006; Hesse, et al., 2007; Strathdee, et al., 2006). Clients of strengths-based case managers identified the focus on strengths and a powerful working alliance as factors in staying involved with their case managers (Brun & Rapp, 2001; Redko et al., in press).
5.1.2. Case management duration
Historically, case management has been implemented as a long-term intervention, lasting many months (Rapp, et al., 1998). The long-term perspective may have originated from two sources. First, substance abusers have generally been viewed as having a chronic and relapsing condition (McLellan et al., 2000) and as such are in need of a long-term, supportive intervention. Second, most models of case management, including strengths-based and assertive community treatment, were derived from case management used to support persons with chronic mental illness over long periods of time.
More recently, case management has been designed to help with very specific goals such as linkage. In line with this more limited focus, case management has been shortened to a brief intervention in some settings. In the current study, substance abusers could receive between one and five sessions of SBCM over a 60 day period. Elsewhere, case management has consisted of one session (Braucht et al., 1995, Morgenstern, et al., 2006) or 2 weeks (Zanis, et al., 1996). While brief interventions cannot hope to address all of the problems of a given client, they can be valuable in helping clients accomplish specific, critical goals.
Taking a cue from brief case management, it may be useful to re-conceptualize long-term case management. Rather than a general source of support for indefinite periods, case management could be implemented in such a way that it helps substance abusers with a series of specific goals. Examples include: completing the first week (or month) of treatment, getting a job, and linking with aftercare treatment.
5.1.3. Case management context
Clinical trials of case management have spanned diverse populations and settings. Positive linkage effects have been found with injection drug users entering methadone maintenance programs (Coviello, et al., 2006; Zanis, et al., 1996), centralized intake units (Scott, et al., 2002), female welfare recipients (Morgenstern, et al., 2006), homeless substance abusers (Braucht, et al., 1995), dually diagnosed substance abusers (Morse, et al., 2006), and substance abusers involved in the criminal justice system (Rhodes & Gross, 1997). This once again suggests that the positive effects of case management are generalizable to a number of settings and populations.
Case management studies that have taken place at methadone treatment programs are most common. In our study SBCM did not have a positive effect on linkage to methadone maintenance treatment. This contrasts with consistent findings that show positive, sometimes striking improvements in linkage. In two instances a generalist model of case management improved the linkage rate with methadone treatment from 8% to 29% and in another, 11% to 46.7% (Coviello, et al., 2006; Sorensen, et al., 2005).
Much less is known about the relationship between case management and linkage with other treatment modalities. Only one non-methadone study has reported results by treatment modality (Morgenstern, et al., 2006). Women receiving public welfare support who were referred to inpatient treatment did not benefit from intensive case management (Morgenstern, et al., 2006). Those who were referred to outpatient treatment did link at a higher rate. Our results showed the same pattern; SBCM improved linkage with drug free outpatient treatment while linkage with residential treatment improved, but not to statistical significance.
While there is a large body of literature that addresses influences on linkage, we know little about the factors that, in combination with case management, predict linkage. In our study only one client characteristic, alcohol severity, predicted linkage with treatment among case managed clients. A limited number of other studies have found that transportation and distance issues affect linkage (Strathdee, et al., 2006), as does drug and alcohol severity, stage of change, homelessness, and outreach contact (Corsi, et al., 2007).
5.1.4. Future case management research
Case management is an important component of treatment for many substance abusers (National Institute on Drug Abuse, 1999). As such, repeated positive findings about its role in improving treatment linkage suggest the need for multi-site implementation trials. These trials will reveal whether community-based organizations can implement case management as it was intended, and whether these programs demonstrate the same improvements in linkage that have been found in clinical trials. Implementation trials can also further our understanding of how community organizations and local context affect case management.
Many of the remaining questions about the value of strengths-based and other models of case management can be addressed in multiple settings as well. These questions include: What is the mechanism of action in various models of case management? What system and individual characteristics are most amenable to the effects of case management? What interventions can be paired with case management to reach substance abusers that do not benefit from case management alone?
5.2. Motivational Interviewing
The motivational interviewing tested in this trial was not effective in improving the linkage rate of substance abusers referred to treatment, disproving one of the study's hypotheses. These findings are congruent with a limited literature that has also found that MI does not have an effect on treatment entry. In the only adequately powered study of an MI intervention, two in-person sessions and one follow-up telephone call were tested at a centralized intake unit (Donovan, et al., 2001). MI did not improve treatment entry, treatment completion, or drug related outcomes. The sole affirmative study of MI and linkage was conducted at a non-treatment program site with a small sample (Carroll, et al., 2001).
The lack of an MI effect in this study may have been due to relatively high levels of motivation in participants. This would be consistent with the fact that all participants had already received an assessment, the first step in entering treatment. Poor linkage may also have been the result of waiting for treatment an average of 65 days (Carr, et al., in press). Even if MI had an initial positive influence on motivation, its impact could have diminished during the two months of waiting. Had prior information been available about the length of the waiting time following CIU referral, a longer MI intervention may have been proposed for this study.
The lengthy waiting period also suggests another potential limitation of MI. Substance abusers experiencing a wide range of tangible barriers such as transportation difficulties, childcare obligations, or a job, may have been dissuaded from linking no matter what their motivation. Motivational interviewing, coupled with contingency management or case management, may be useful in mediating some lifestyle barriers to linkage and thereby improve linkage (Donovan, et al., 2001).
5.2.1. Future MI study
MI's potential value stems from its brief, low cost design and its non-confrontive but directive approach. Despite these appealing features, few studies have empirically examined its ability to facilitate linkage with treatment. In order to thoroughly assess the efficacy of MI in improving linkage, adequately powered studies, including multi-site trials, need to be conducted. An existing platform for such a study is the National Institute on Drug Abuse's Clinical Trials Network. MI studies of retention and other outcomes are already taking place in several of the CTN's nodes (Carroll, et al., 2006). The large participant base offered by the CTN may provide researchers with the opportunity to identify individual and system influences that mediate linkage with treatment among persons who receive MI.
5.3. SBCM and MI
The third hypothesis of this study was confirmed. SBCM was significantly better at improving linkage with treatment than MI. We speculate that a prominent reason for this finding can be found in the broader focus of the SBCM intervention. SBCM activities such as active referral to services and direct assistance with linkage may help substance abusers negotiate such problems as a lengthy waiting period before treatment. It is possible that merging the two study interventions may address two major areas that improve linkage: poor motivation and lifestyle barriers to linkage. A fourth study group in this trial, one that combined MI and SBCM, would have allowed us to more fully understand the relative contribution of the two interventions on linkage.
5.4. Limitations
Interpretation of these results should take into account study limitations. The generalizability of our findings may be limited by several factors. First, the substance abusers in this study were self-selected, having made decisions to: (1) be assessed for treatment; (2) be referred to the study; and (3) participate in the study baseline interview. Each of these steps may indicate that participants had more motivation than substance abusers who were not involved with the treatment continuum and had resolved at least some of their barriers to care.
As in other clinical trials, the generalizability of our findings is compromised somewhat by restrictions imposed by eligibility criteria. In this study substance abusers who were alcohol dependent only, without other drug dependence or abuse, were not eligible.
6. Conclusion
Results of this clinical trial were generally consistent with previous studies that supported the value of case management in improving linkage with treatment. The findings that motivational interviewing did not improve linkage were also similar to most previous studies. The future research that is called for with these two interventions is different as well. Case management appears ready for real-world implementation trials and a careful assessment of how it may be modified by community programs. In order to fully determine the value of motivational interviewing in facilitating linkage, it will be necessary to design and implement controlled clinical trials that have adequate power to identify potential effects.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders-IV-R. Fourth ed. American Psychiatric Association; Washington, DC: 2001. [Google Scholar]
- American Society of Addiction Medicine . Patient placement criteria for the treatment for substance-related disorders. Second ed. American Society of Addiction Medicine; Chevy Chase, MD: 2001. [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- Ball SA, Van Horn D, Crits-Cristoph P, Woody GE, Farentinos C, Martino S, Nich C, Frankforter TL, Obert JL, Carroll KM. Site matters: Multisite randomized trial of motivational enhancement therapy in community drug abuse clinics. J Consult Clin Psychol. 2007;75(4):556–567. doi: 10.1037/0022-006X.75.4.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballew JR, Mink G. Case management in social work. second edition Charles C Thompson; Springfield, IL: 1996. [Google Scholar]
- Braucht GN, Reichardt CS, Geissler LJ, Bormann CA, Kwiatkowski CF, Kirby MW., Jr. Effective services for homeless substance abusers. J Addict Dis. 1995;14(4):87–109. doi: 10.1300/j069v14n04_06. [DOI] [PubMed] [Google Scholar]
- Brun C, Rapp RC. Strengths-based case management: Individual's perspectives on strengths and the case manager relationship. Soc Work. 2001;46(3):278–288. doi: 10.1093/sw/46.3.278. [DOI] [PubMed] [Google Scholar]
- Carr CA, Xu J, Redko C, Lane DT, Rapp RC, Goris J, Carlson RG. Individual and system influences on waiting time for substance abuse treatment. J Subst Abuse Treat. doi: 10.1016/j.jsat.2007.03.005. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Nich C, Martino S, Frankforter TL, Farentinos C, Kunkel LE, Mikulich-Gilbertson SK, Morgenstern J, Obert JL, Polcin D, Snead N, Woody GE. Motivational interviewing to improve treatment engagement and outcome in individuals seeking treatment for substance abuse: A multisite effectiveness study. Drug Alcohol Depend. 2006;81(3):301–312. doi: 10.1016/j.drugalcdep.2005.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Libby B, Sheehan J, Hyland N. Motivational interviewing to enhance treatment initiation in substance abusers: An effectiveness study. Am J Addict. 2001;10:335–339. doi: 10.1080/aja.10.4.335.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment . Comprehensive case management for substance abuse treatment. Treatment Improvement Protocol (TIP) Series 27 (DHHS Publication No. [SMA] 98−3222) Substance Abuse and Mental Health Services Administration; Rockville, MD: 1998. [PubMed] [Google Scholar]
- Connors GJ, Walitzer KS, Dermen KH. Preparing clients for alcoholism treatment: Effects on treatment participation and outcomes. J Consult Clin Psychol. 2002;70(5):1161–1169. doi: 10.1037//0022-006x.70.5.1161. [DOI] [PubMed] [Google Scholar]
- Corsi KF, Kwiatkowski CF, Booth RE. Treatment entry and predictors among opiate-using injection drug users. Am. J. Drug Alcohol Abuse. 2007;33:121–127. doi: 10.1080/00952990601091093. [DOI] [PubMed] [Google Scholar]
- Coviello DM, Zanis DA, Wesnoski SA, Alterman AI. The effectiveness of outreach case management in re-enrolling discharged methadone patients. Drug Alcohol Depend. 2006;85(1):56–65. doi: 10.1016/j.drugalcdep.2006.03.009. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Sobell LC, Sobell MB, Agrawal S, Toneatte T. Barriers to treatment: Why alcohol and drug abusers delay or never seek treatment. Addict Behav. 1993;18(3):347–353. doi: 10.1016/0306-4603(93)90036-9. [DOI] [PubMed] [Google Scholar]
- Donovan DM, Rosengren DB, Downey L, Cox GB, Sloan KL. Attrition prevention with individuals awaiting publicly funded drug treatment. Addiction. 2001;96(8):1149–1160. doi: 10.1046/j.1360-0443.2001.96811498.x. [DOI] [PubMed] [Google Scholar]
- Farabee D, Leukefeld CG, Hays L. Accessing drug-abuse treatment: Perceptions of out-of-treatment injectors. J Drug Issues. 1998;28(2):381–394. [Google Scholar]
- Gardner L, Metsch LR, Anderson-Mahoney P, Loughlin AM, Del Rio C, Strathdee S, Sansom SL, Siegal HA, Greenberg AE, Holmberg SD, Antiretroviral Treatment and Access (ARTAS) Study Group. Efficacy of a brief case management intervention to link recently diagnosed HIV-infected persons to care. AIDS. 2005;19:423–431. doi: 10.1097/01.aids.0000161772.51900.eb. [DOI] [PubMed] [Google Scholar]
- Hesse M, Vanderplasschen W, Rapp RC, Broekaert E, Fridell M. Case management for persons with substance use disorders. Cochrane Database of Systematic Review. 2007;(Issue 4) doi: 10.1002/14651858.CD006265.pub2. [DOI] [PubMed] [Google Scholar]
- Hubbard RL, Craddock SG, Anderson J. Overview of 5-year follow-up outcomes in the drug abuse treatment outcome studies (DATOS). J Subst Abuse Treat. 2003;25:125–134. doi: 10.1016/s0740-5472(03)00130-2. [DOI] [PubMed] [Google Scholar]
- Martino S, Carroll K, Kostas D, Perkins J, Rounsaville B. Dual diagnosis motivational interviewing: A modification of motivational interviewing for substance-abusing patients with psychotic disorders. J Subst Abuse Treat. 2002;23(4):297–308. doi: 10.1016/s0740-5472(02)00295-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marty D, Rapp CA, Carlson L. The experts speak: The critical ingredients of strengths model case management. Psychiatr Rehabil J. 2001;24(3):214–221. doi: 10.1037/h0095090. [DOI] [PubMed] [Google Scholar]
- McLellan AT. The fifth edition of the addiction severity index. J Subst Abuse Treat. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O'Brien CP, Kleber HD. Drug Dependence, a chronic medical illness Implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- Miller WR. Motivational enhancement therapy with drug abusers. National Institute on Drug Abuse; Washington, DC: 1995. [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2 ed. Guilford Press; New York, NY: 2002. [Google Scholar]
- Morgenstern J, Blanchard KA, McCrady BS, McVeigh KH, Morgan TJ, Pandina RJ. Effectiveness of intensive case management for substance-dependent women receiving temporary assistance for needy families. Am. J. Public Health. 2006;96(11):2016–2023. doi: 10.2105/AJPH.2005.076380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse GA, Calsyn RJ, Klinkenberg WD, Helminiak TW, Wolff N, Drake RE, Yonker RD, Lama G, Lemming MR, McCudden S. Treating homeless clients with severe mental illness and substance use disorders: Costs and outcomes. Community Ment Health J. 2006;42(4):377–404. doi: 10.1007/s10597-006-9050-y. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse Principles of drug addiction treatment: A research-based guide. Retrieved NIH publication number 99−4180. 1999 from http://www.drugabuse.gov/PODAT/PODATIndex.html.
- Rapp CA, Chamberlain R. Case management services for the chronically mentally ill. Soc Work. 1985;30(5):417–422. doi: 10.1093/sw/30.5.417. [DOI] [PubMed] [Google Scholar]
- Rapp RC. The strengths perspective and persons with substance abuse problems. In: Saleebey D, editor. The strengths perspective in social work practice. fourth edition Longman; New York: 2006. pp. 128–147. [Google Scholar]
- Rapp RC, Siegal HA, Li L, Saha P. Predicting post-primary treatment services and drug use outcome: A multivariate analysis. Am. J. Drug Alcohol Abuse. 1998;24(4):603–615. doi: 10.3109/00952999809019610. [DOI] [PubMed] [Google Scholar]
- Rapp RC, Xu J, Carr CA, Lane DT, Wang J, Carlson RG. Treatment barriers identified by substance abusers assessed at a centralized intake unit. J Subst Abuse Treat. 2006;30:227–235. doi: 10.1016/j.jsat.2006.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapp RC, Xu J, Carr CA, Lane DT, Redko C, Wang J, Carlson RG. Understanding treatment readiness in recently assessed, pre-treatment substance abusers. Subst Abuse. 2007;28(1):11–23. doi: 10.1300/J465v28n01_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redko C, Rapp RC, Elms C, Snyder M, Carlson RG. Understanding the working alliance between persons with substance abuse problems and strengths-based case managers. J Psychoactive Drugs. doi: 10.1080/02791072.2007.10400610. in press. [DOI] [PubMed] [Google Scholar]
- Rhodes W, Gross M. Case management reduces drug use and criminality among drug-involved arrestees: An experimental study of an HIV prevention intervention. (Final summary report presented to the National Institute of Justice and the National Institute on Drug Abuse) U.S. Department of Health and Human Services; Rockville, MD: 1997. [Google Scholar]
- Scott CK, Sherman RE, Foss MA, Godley M, Hristova L. Impact of centralized intake on case management services. J Psychoactive Drugs. 2002;34(1):51–57. doi: 10.1080/02791072.2002.10399936. [DOI] [PubMed] [Google Scholar]
- Siegal HA, Li L, Rapp RC. Case management as a therapeutic enhancement: Impact on post-treatment criminality. J Addict Dis. 2002;21(4):37–46. doi: 10.1300/J069v21n04_04. [DOI] [PubMed] [Google Scholar]
- Siegal HA, Rapp RC, Kelliher CW, Fisher JH, Wagner JH, Cole PA. The strengths perspective of case management: A promising inpatient substance abuse treatment enhancement. J Psychoactive Drugs. 1995;27(1):67–72. doi: 10.1080/02791072.1995.10471674. [DOI] [PubMed] [Google Scholar]
- Shwartz M, Baker G, Mulvey KP, Plough A. Improving publicly funded substance abuse treatment: The value of case management. Am. J. Public Health. 1997;87(10):1659–1664. doi: 10.2105/ajph.87.10.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen J, Masson C, Delucchi K, Sporer K, Barnett P, Mitsuishi F, Lin C, Song Y, Chen T, Hall S. Randomized trial of drug abuse treatment-linkage strategies. J Consult Clin Psychol. 2005;73(6):1026–1035. doi: 10.1037/0022-006X.73.6.1026. [DOI] [PubMed] [Google Scholar]
- Stephens RC, Scott CK, Muck RD. Clinical assessment and substance abuse treatment. State University of New York Press; Albany: 2003. [Google Scholar]
- Strathdee S, Ricketts E, Huettner S, Cornelius L, Bishai D, Havens J, Beilenson P, Rapp C, Lloyd J, Latkin C. Facilitating entry into drug treatment among injection drug users referred from a needle exchange program: Results from a community-based behavioral intervention trial. Drug Alcohol Depend. 2006;83(3):225–232. doi: 10.1016/j.drugalcdep.2005.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsogia D, Copello A, Orford J. Entering treatment for substance misuse: A review of the literature. J Ment Health. 2001;10(5):481–499. [Google Scholar]
- Vaughan-Sarrazin MS, Hall JA, Rick GS. Impact of case management on use of health services by rural clients in substance abuse treatment. J Drug Issues. 2000;30(2):435–463. [Google Scholar]
- Zanis DA, McLellan AT, Alterman AI, Cnaan RA. Efficacy of enhanced outreach counseling to reenroll high-risk drug users 1 year after discharge from treatment. Am J Psychiatry. 1996;153(8):1095–1096. doi: 10.1176/ajp.153.8.1095. [DOI] [PubMed] [Google Scholar]