As the health crises of the developing world continue to attract concern, master of public health (MPH) students studying in the U.S. are becoming increasingly aware of and interested in international health studies.1 The University of Washington School of Public Health (UW SPH) in Seattle, Washington, has met this challenge by expanding and reorganizing its international public health teaching. We have established competencies for our global health MPH scholars, with a focus on addressing large public health problems with a social justice perspective.
The emergence of the global health concept over the last decade reflects heightened awareness of accelerating globalization processes that challenge the traditionally drawn boundaries between the international and domestic health professional worlds. While the precise definition of global health continues to be contested, it is widely agreed that increased global flows of resources, information, people, and infectious diseases, together with growing global inequality, have created new public health problems that require fresh and innovative approaches. With this recognition has come a spate of new global health centers, departments, institutes, and programs in American and European universities that seek to redefine approaches to public health and recalibrate training to new global health realities for the next generation of health researchers and practitioners. While the urgency for such redefined training is apparent, there is little in the current public health literature that attempts to identify just what this training should include.
In spite of new global health program proliferation, core professional global health competencies have yet to be defined, and no consensus for development of appropriate curricula has emerged in the public health field. The recent creation of a new Department of Global Health (DGH) at UW has presented curriculum planners, charged with developing new MPH, doctor of philosophy (PhD), and doctor of medicine programs, with these immediate challenges. This article describes the consensus-building process conducted by the DGH curriculum committee over a one-year period in which global health competencies were identified and curriculum needs redefined. While debates about the meaning and scope of global health will continue, basic guidelines for new kinds of training are urgently needed to prepare health workers for the rapidly changing environment they will soon confront.
Through this recently established DGH (which has received much of its new funding through an endowed grant from the Bill and Melinda Gates Foundation), UW is poised to rapidly expand its international health student enrollment, course offerings, and degree programs. Other prominent universities have launched similar efforts in just the last two years. In 2006, Duke University in Durham, North Carolina, which does not have a school of public health (SPH) to date, launched a new Global Health Institute, which started its education program with an undergraduate certificate. The Johns Hopkins University in Baltimore, Maryland, launched a Center for Global Health, bringing together its SPHs, medicine, and nursing schools in a collaborative effort. In addition, other schools such as The George Washington University in Washington, DC, have recently started offering MPH degrees in global health.
As UW prepared to launch its DGH—a collaboration between the SPH and the school of medicine—the curriculum committee of the existing international health program embarked on a complete review of UW's current course offerings in anticipation of growth and expansion. We found very little guidance for this effort in the public health literature. Patrick reported major gaps in public health training, along with the implication of inadequate coursework in SPHs and in medical schools.2 In a commentary on an international traineeship, Edwards and colleagues said medical students were generally being provided inadequate course electives to be competent enough in international settings.3 Hotez provided a thorough lament of the lack of global health content in U.S. and Canadian academic health centers compared with those in Europe, particularly in Britain.4 Dato and colleagues did provide a concept for helping discern our own capacity in course offerings to meet the challenge of global health training.5 And Drain and colleagues have published a call for more training and opportunities in global health, especially for medical students.6
The purpose of this article is to report on how we developed international health competencies to guide our curriculum development.
BACKGROUND
The U.S. has 37 accredited SPHs, which graduated 19,000 students in 2005.1 The schools are accredited by the Association of Schools of Public Health (ASPH), which has identified 10 areas of program concentration for public health training: biostatistics, epidemiology, administration, public health practice, health education, environmental sciences, maternal and child health, nutrition, biomedical/lab, and international.
Gaining entrance to a public health training program is competitive: slightly more than half (55%) of the 27,000 applicants for admission to all schools in 2005 were admitted. Applications have increased 53% since 1995. One-third of the students admitted in 2005 (34%) were members of minority groups, the largest component being Asian (14%). Women comprise 71% of the total enrolled population, and foreign nationals comprise 15%. From 1995 to 2005, the number of students enrolled in public health programs has increased 30%.
UW accepted 463 of its 940 public health program applicants in 2005, and actually enrolled 276 of these, or 60% of acceptances and 29% of applicants. The national average was to enroll 49% of acceptances and 27% of applicants.1 Our MPH degree in international health has been conferred on an average of 11 students per year for the last 10 years, with increasing numbers over time.
About 9% of applicants to SPHs sought admission to an international health track (up from nearly 8% in 1995); the other most popular programs were epidemiology (20%, up from 16% in 1995), administration (17%, a decline from 22% in 1995), and health education (15%, up from 13% in 1995).1 Nearly 9% of 6,656 public health degrees conferred in 2005 were with a focus on international health.1
Graduates from international public health programs have increased 69% since 1994 across the 37 schools, and comprise more than 6% of total enrolled students. In 2005, U.S. SPHs conferred 470 MPH degrees with concentrations in international health, and another 72 degrees of other types. For the 2005 entering class, there were 2,372 applicants to the nation's 13 currently operating international health programs, 81% female and 20% foreign nationals. Schools with international health programs, as measured by current students enrolled, include The Johns Hopkins University (317); George Washington University (184); Emory University (153) in Atlanta, Georgia; Boston University (140) in Boston, Massachusetts; University of San Francisco (108) in San Francisco, California; Harvard University (67) in Cambridge, Massachusetts; Loma Linda University (65) in Loma Linda, California; University of Texas Health Science Center—Houston (55) in Houston, Texas; New York Medical College (41) in Valhalla, New York; Yale University (34) in New Haven, Connecticut; UW (28); University of Michigan (22) in Ann Arbor, Michigan; and University of Arizona (17) in Tucson, Arizona. Tulane University's SPH in New Orleans, Louisiana, was closed for the fall semester 2005 subsequent to Hurricane Katrina, but conferred 113 degrees with an international health focus in June 2005.1
While small, our UW international health program is a vigorous and integral part of our SPH. Faculty members are known to be activists, involved in cutting-edge operational research on human immunodeficiency virus/acquired immunodeficiency syndrome treatment in low-income countries, workforce infrastructure strengthening, maternal and child health, malaria control, and nutrition.7–13 Our 20-year-old program has focused on social justice from its inception and attracts students from around the world who seek a critical approach to public health development efforts abroad. Additionally, we have two fellowship programs that have drawn 24 mid-career professionals from developing countries who take many of our classes.
METHODS
Literature search
In light of health competency concerns raised by Patrick,2 Edwards and colleagues,3 Hotez,4 and others, our own curriculum committee began with a literature search in an attempt to find a published set of such competencies we could modify and adapt for our program. Finding little of direct relevance, we turned to more generic public health competencies, produced by the Council on Linkages Between Academia and Public Health Practice (COL), which adopted a list of Core Competencies for Public Health Professionals on April 11, 2001.14
ASPH established MPH competencies in 2004, based on the five core discipline areas (biostatistics, environmental health, epidemiology, policy/management, and social and behavioral sciences) and seven cross-cutting domains. The domains include communication/informatics, diversity/culture, leadership, professionalism, program planning, biology, and systems thinking.15 This review provided helpful background, but included nothing specific to international or global health.
In addition, our own UW Department of Health Services developed curriculum competencies for its generic MPH program in 2005, based on the COL competencies. The United Nations' Millennium Development Goals offered another reference point, as we felt graduates of international health programs should direct their work toward the attainment of these internationally adopted goals.16
Strategic planning and establishing values
As a first step toward reorganizing our programming, UW prepared a situational assessment and strategic plan in early 2003, which involved surveying and interviewing our students and faculty. Through this process, we established the collective value system that drives our teaching and research. Some of these values included viewing health as a right, respect for other cultures, an abhorrence for the growing gap between the rich and poor, an appreciation for action-based science, creating partnerships (especially with institutions and organizations in low-income countries), and promoting the notion of the United States as a member of the global community. These values created the backdrop for our next steps.
Learning what other schools do
We next toured the websites of the largest programs to see what competencies are listed for global public health graduate training. George Washington University had posted global health competencies to its website. Boston University had produced international health department objectives, which read very much like competencies and seemed to fall within the COL categories. The University of San Francisco listed seven global health practice competencies, similar to others. Emory's school offered an MPH in international health with emphases on infectious disease, reproductive health, community health, or leadership. Each of Emory's areas of emphasis had its own competencies, which were detailed and came closest to UW's competencies by addressing some social justice concerns.
Harvard listed five brief concentration goals for its international health MPH, focusing on leadership, determinants of health, policy, evaluation, and research. Johns Hopkins had MPH core competencies and listed the required courses designed to meet those competencies, but none was specific to international health. Loma Linda reported having no formal competency listings beyond those offered by ASPH.
We also sought course listings from the largest international public health training programs as a proxy for a competency list. Understandably, the expansive university course listings in international health in the larger universities were substantially broader than our own list of courses.
Developing and circulating a draft
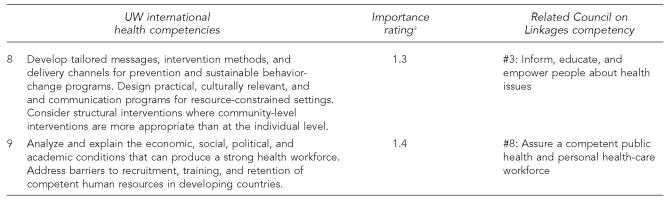
Next, we drafted competencies that (1) addressed the generic COL competencies, (2) were consistent with our international health program's sense of priorities and values, and (3) were set in the context of our own department's general MPH competencies. That process resulted in nine competencies unique to global health, all of which we considered equally important (Table 1).
Table 1.
University of Washington (UW) international health program competencies
Ratings were on a scale of 1 to 3, with 1 being “very important,” 2 “somewhat important,” and 3 “not important.” The competencies were broken into subparts for purposes of asking survey respondents to rank their importance. When there are two or more sentences in a competency, each sentence was offered as a separate ranking. The first competency, for example, as it has three sentences, had three rankings. We used the mean of the rankings within each section for reporting in this article. There were 44 survey respondents: 37 students and seven faculty members.
The World Health Organization's burden-of-disease categories include communicable, maternal, perinatal, and nutritional conditions, noncommunicable diseases, and injuries.
As part of this process, we also conducted an assessment of where our course offerings seemed to be out of alignment with our new competencies. A list of potential new courses was drafted and arrayed in order of priority, using our competencies as criteria.
Consulting curriculum experts
UW's Center for Instructional Development and Research reviewed the competencies and offered very helpful suggestions for ways to determine how students can demonstrate achievement of the competencies. The current trends in curriculum development favor interdisciplinary course offerings, student portfolios, and culminating projects (such as a thesis).
Surveying our faculty and students
For the final phase of our process in adopting competencies, we queried our faculty and students about the importance of each of the proposed competencies, using a scale of 1 to 3, with 1 being “very important” and 3 being “not important.” Beyond this initial objective to rate the relative importance of the competencies, we asked incoming students to rate their current competencies, as a baseline against which they will compare their self-ratings to their ratings as they exit the program in two years. For students who had completed a year of the program, we asked them which courses they had taken so far that they thought contributed most to the defined competencies. We also asked respondents to prioritize a list of potential new courses as part of the survey.
We obtained an approval from our UW Human Subjects Division to use these data on April 9, 2007 (#07-5644-E/G 01). A consent form was used to obtain permission from participating students.
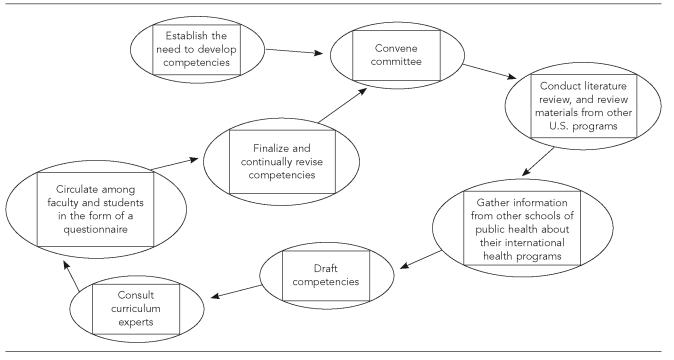
The Figure provides a schematic view of the steps in our process.
Figure.
Framework for developing competencies
FINDINGS
Comparison to other schools
We found only four international health master's degree training programs that had formally established competencies separate from their generic MPH programs. These programs were offered at George Washington University, Boston University, the University of San Francisco, and Emory. Only Emory's programs included competencies that could be described in terms of social justice.
Our survey
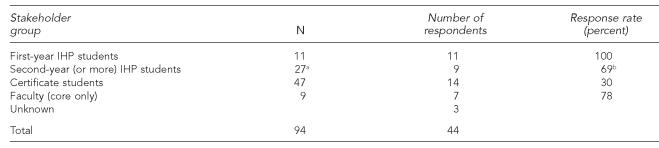
There were 44 respondents to our survey of students and faculty on their views of the proposed competencies for the UW international health program. Of these, 11 were incoming first-year students (100% of those eligible), nine were second- or third-year students (69% of those on campus and not abroad), 14 were certificate students (30% of those eligible), and seven were faculty (a little more than 75% of our core faculty). Three were unidentified. The survey results are detailed in Table 2.
Table 2.
Survey respondents
Only 13 were in residence.
Of those on campus
IHP = international health program
Respondents rated the competencies between 1.1 and 1.4 on the 1-to-3 scale, with lower numbers indicating higher importance. We concluded from these ratings that respondents had a fairly broad acceptance of the competencies, and that none of the competencies was considered unimportant.
When asked whether they would suggest additional competencies that we might have missed, the respondents offered nine suggestions, each different from the others and all of which could, arguably, be incorporated into the existing competencies. There were 35 respondents who had no additions to suggest.
Students entering both their first year and second year of MPH studies were asked to rate their own competencies in each area. Scores ranged from 1.4 to 2.8 on a scale of 1 to 3, with 1 for “firm grasp,” 2 for “some ability,” and 3 for “little comfort.” The mean score for incoming first-year students was 2.43, and for incoming second-year students was 2.05, suggesting some gain in competency in the first year of study, although this suggestive inference was not statistically significant.
The respondents' answers to questions about existing courses that contributed most to student learning of the competencies provided us with an initial sense of how well our courses deliver on our objectives, and helped to signal where we have weaknesses.
We also asked respondents to prioritize a set of possible new courses to meet the competencies. These priorities centered around courses that provide critical analysis of essential health services, health education and promotion, water and sanitation, resource allocation, reproductive health, and social inequalities.
Limitations
While this initial inquiry into the international health program curriculum was quite instructive, the process would have been assisted by a greater body of literature on competencies for international health training against which we could have compared our results. The response rate to our own internal baseline survey was reasonably high, and the responses received were fairly consistent. But additional responses would have made for a more robust dataset. Additionally, because there was no previous baseline survey, we had no data with which to compare these responses. As the only international health program in the Northwest states, we also had no regional peer group with which to make a comparison, which might have been instructive. Our program is also relatively young, especially when compared with our university counterparts in the East, and is relatively small.
CONCLUSIONS AND POLICY IMPLICATIONS
Core competencies have been an important part of public health training curriculum development for several years. However, these competencies mostly address the basic foundation of public health education, as few specific programs and tracks within the discipline have developed their own competencies within the broader frameworks offered by either the COL or ASPH.
UW competencies are very different from, for example, George Washington University competencies, suggesting that schools can use the publication of their competencies to convey to prospective students and faculty the unique identity and distinct values of their programs.
The UW program will now use these newly developed competencies to determine any gaps in curriculum and the priorities for new courses. This will provide a rational approach to making new faculty recruitment decisions.
Students will routinely be asked to rate their performance on the competencies as they enter the program, as they finish their first year, and as they graduate. These numbers will be tracked over time to measure program performance. Students will also be asked which courses contributed most to their competency development. The next phase in our development is to create a mechanism for students to assemble portfolios of their work that will demonstrate their proficiencies in each competency.
The process of developing competencies was a useful exercise for our curriculum committee and helped us set the stage for rapid and effective program expansion that is shaped by strategic and rational decision-making, rather than simply responding to current or prospective faculty interest areas. We were also able to articulate specific ways in which our program is unique among the other dozen international health programs across the country. We recommend this process to other SPHs as they seek to improve their program offerings in global health. This process not only will lead to a set of common expectations shared by all programs offering degrees in international and global health, but also will provide an objective means of differentiating programs from one another.
Footnotes
This study was funded by the University of Washington (UW) Department of Health Services, School of Public Health and Community Medicine (SPHCM) in Seattle, Washington.
REFERENCES
- 1.Ramiah K, Silver GB, Sow M-SK. Washington: ASPH; 2005. Association of Schools of Public Health 2005 annual data report; p. 72. [Google Scholar]
- 2.Patrick WK. Global health challenges: trends in public health training, research and advocacy. Asia Pac J Public Health. 2000;(12 Suppl):S8–12. [PubMed] [Google Scholar]
- 3.Edwards N, DiCenso A, Degner L, O'Brien-Pallas L, Lander J. Burgeoning opportunities in nursing research. Can J Nurs Res. 2002;34:139–48. [PubMed] [Google Scholar]
- 4.Hotez PJ. Should we establish a North American school of global health sciences? Am J Med Sci. 2004;328:71–7. doi: 10.1097/00000441-200408000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Dato VM, Potter MA, Fertman CI, Pistella CL. A capacity mapping approach to public health training resources. Public Health Rep. 2002;117:20–7. doi: 10.1093/phr/117.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Drain PK, Primack A, Hunt DD, Fawzi WW, Holmes KK, Gardner P. Global health in medical education: a call for more training and opportunities. Acad Med. 2007;82:226–30. doi: 10.1097/ACM.0b013e3180305cf9. [DOI] [PubMed] [Google Scholar]
- 7.Bezruchka S. Income inequality and population health. Hierarchy and health are related. BMJ. 2002;324:978. [PubMed] [Google Scholar]
- 8.Gloyd S, Suarez Torres J, Mercer MA. Immunization campaigns and political agendas: retrospective from Ecuador and El Salvador. Int J Health Serv. 2003;33:113–28. doi: 10.2190/25BV-JW2P-22CN-WNRR. [DOI] [PubMed] [Google Scholar]
- 9.Hagopian A, Ofosu A, Fatusi A, Biritwum R, Essel A, Gary Hart L, et al. The flight of physicians from West Africa: views of African physicians and implications for policy. Soc Sci Med. 2005;61:1750–60. doi: 10.1016/j.socscimed.2005.03.027. [DOI] [PubMed] [Google Scholar]
- 10.Pfeiffer J. International NGOs and primary health care in Mozambique: the need for a new model of collaboration. Soc Sci Med. 2003;56:725–38. doi: 10.1016/s0277-9536(02)00068-0. [DOI] [PubMed] [Google Scholar]
- 11.Spigner C. African Americans, democracy, and biomedical and behavioral research: contradictions or consensus in community-based participatory research? Int Q Community Health Educ. 1999–2000;19:259–84. doi: 10.2190/XBWT-G9RF-4B35-KBNM. [DOI] [PubMed] [Google Scholar]
- 12.Gorstein J, Bhaskaram P, Khanum S, Hossaini R, Balakrishna N, Goodman TS, et al. Safety and impact of vitamin A supplementation delivered with oral polio vaccine as part of the immunization campaign in Orissa, India. Food Nutr Bull. 2003;24:319–31. doi: 10.1177/156482650302400402. [DOI] [PubMed] [Google Scholar]
- 13.Mercer MA, Liskin L, Scott SJ. The role of non-governmental organizations in the global response to AIDS. AIDS Care. 1991;3:265–70. doi: 10.1080/09540129108253072. [DOI] [PubMed] [Google Scholar]
- 14.Council on Linkages Between Academia and Public Health Practice. Core competencies for public health professionals. 2001. Apr 11, [cited 2007 Apr 17]. Available from: URL: http://www.phf.org/competencies.htm.
- 15.Association of Schools of Public Health. MPH core competency development project. [cited 2006 Dec 6]. Available from: URL: http://www.asph.org/document.cfm?page=851.
- 16.United Nations. UN millennium development goals. [cited 2007 Apr 17]. Available from: URL: http://www.un.org/millenniumgoals.