SYNOPSIS
Bioterrorism is the deliberate release of viruses, bacteria, or other agents used to cause illness or death in people, animals, or plants. Only modest microbiologic skills are needed to produce and effectively use biologic weapons. And biological warfare has afflicted campaigns throughout military history, at times playing an important role in determining their outcomes.
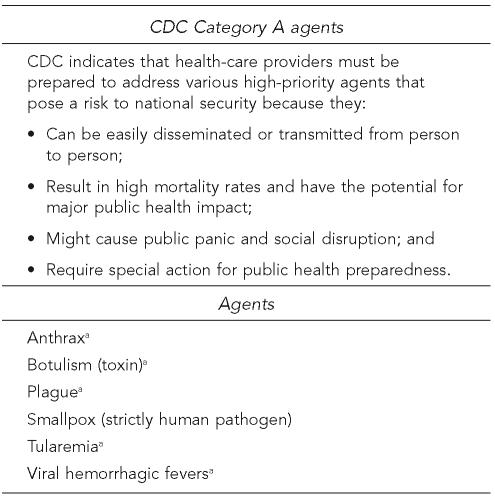
There is a long list of potential pathogens for use by terrorists, but only a few are easy to prepare and disperse. Of the infectious diseases, the vast majority are zoonoses. The Centers for Disease Control and Prevention's highest-priority bioterrorism agents are in Category A. The only disease that does not affect animals in Category A is smallpox, which was eliminated by a worldwide vaccination program in the late 1970s. Because these diseases can infect animals and humans, the medical and veterinary communities should work closely together in clinical, public health, and research settings.
The Model State Emergency Health Powers defines bioterrorism as the intentional use of any microorganism, virus, infectious substance, or biological product that may be engineered as a result of biotechnology—or any naturally occurring or bioengineered component of any such microorganism, virus, infectious substance, or biological product—to cause death, disease, or other biological malfunction in a human, animal, plant, or other living organism to influence the conduct of government or to intimidate or coerce a civilian population.1 Biological weapons (bioweapons) are relatively easy and inexpensive to produce, cause death or disabling disease, and can be aerosolized and distributed over large geographic areas.
There is a long list of potential pathogens for use by terrorists; however, only a few are easy to prepare and disperse. Traditional agents of offensive biological warfare (biowarfare) programs have included the causative organisms of anthrax, plague, tularemia, brucellosis, glanders, melioidosis, various foodborne illnesses, cryptosporidiosis, cryptococcosis, Q fever, psittacosis, dengue fever, smallpox, viral equine encephalitides, and the viral hemorrhagic fevers. All are seen in animals, except for smallpox and dengue fever.2
A Russian panel of bioweapons experts reviewed pathogens and determined the vast majority of pathogens were animal diseases transmissible to people, or zoonoses.3 A report in the Journal of the American Medical Association concluded that 80% of the common pathogens likely to be used in biowarfare are zoonoses.4 The Centers for Disease Control and Prevention (CDC) currently classifies bioterrorism diseases/agents most likely to be used into categories A, B, and C, with A having the highest priority.5 Of the infectious diseases in CDC's classification system, the majority are zoonoses. Of the Category A diseases, more than 80% are zoonoses (Figure 1). Category C includes emerging diseases, of which about 75% are zoonoses.
Figure 1.
CDC classification of critical biological agents
Seen in animals and people
CDC = Centers for Disease Control and Prevention
The majority of biological agents (especially type A) are most effectively used as aerosols. Effective delivery of an aerosolized agent requires that the particle size be 1 to 10 microns to be able to reach the terminal bronchioles and alveoli. Aerosol sprays are the most likely method to be used in a potential bioterrorism attack because they are the most effective means of widespread dissemination.6 CDC defines bioterrorism as the deliberate release of viruses, bacteria, or other agents used to cause illness or death in people, animals, or plants.7 The death and illness in a community can have financial repercussions. The monetary cost related to human causalities during a release of aerosolized anthrax spores in 1998 was conservatively estimated to be $26.2 billion per 100,000 people exposed.8
COWPOX LEADS TO SMALLPOX PREVENTION
As previously mentioned, the only disease that does not affect animals in Category A is smallpox, which was eliminated by a worldwide vaccination program. The World Health Organization (WHO) officially declared smallpox eradicated in 1979.9 Elimination was possible because there was no animal reservoir. The global eradication of smallpox was a tremendous achievement made possible by the development of an effective vaccine. As a result, routine vaccination of the general population is no longer recommended. Stocks of smallpox still exist in two secure laboratories. There was concern that the threat of smallpox could be used as a bioterrorist weapon, which in 2002 led to a vaccination campaign in U.S. military and civilian health-care workers and first responders.10
Interestingly, the control of smallpox began with the observation that people exposed to cowpox, a zoonosis, were later immune to smallpox. Effective control of smallpox began in the late 16th century when Dr. Edward Jenner, an English physician, became intrigued with farmers' reports that people who caught cowpox didn't develop smallpox later. He used an animal pox virus (cowpox) to immunize people against the smallpox virus. Jenner published his research in 1798; however, great opposition arose in the medical community and in the general public to using cowpox to provide immunity to smallpox. His initial report to the Royal Society was rejected as the concept conflicted with established knowledge. With time, his research was accepted and Jenner spent much of the rest of his life traveling the world to demonstrate his technique and distribute cowpox material to others.11
The WHO has calculated that the net world economic return from smallpox eradication is $1 billion a year, with billions of lives saved. The number of lives saved by Jenner's technique of vaccination is said to be higher than by any other individual in history.11 During his time, the vaccination process involved deliberately giving people smallpox by scratching into their skin scab material from someone who had a mild form of smallpox (later called “variolation”). Deaths from this procedure were not uncommon, but many physicians built up lucrative businesses administering it.12
Cowpox is a mild infection of cows that causes weeping ulcers on their mammary glands but little discomfort. Most cows in a milking herd may become affected, developing a fever and lesions on the hands, arms, or face. Although once common in cattle, cowpox is now rare. Jenner concluded that cowpox not only protected against smallpox, but also could be transmitted from one person to another as a deliberate mechanism of protection.
ZOONOSES' IMPACT ON MILITARY CAMPAIGNS IN HISTORY
Zoonoses have afflicted campaigns throughout military history. The attack of the Tatars on the city of Caffa, a well-fortified port, was recorded during the Middle Ages. The Tatar soldiers surrounded the city and placed it under siege. Soldiers catapulted plague cadavers into the city, where the inhabitants died of plague. It is unknown if the catapulted bodies led to the development of plague in Caffa or if the event was coincidental. Because plague-transmitting fleas quickly leave cadavers to find living hosts, the corpses catapulted over the city walls may not have been carrying competent plague vectors. The tactic of hurling bodies of dead plague victims over city walls occurred in other conflicts and was also reportedly used by Russian troops battling Swedish forces in 1710.2,13,14
Animal diseases are the leading agents of biowarfare. One advantage of biowarfare is that it can kill combatants, while leaving their equipment and supplies intact. Furthermore, only modest microbiological skills are needed to produce and effectively use bioweapons. The potency, cost-effectiveness, and ability to manufacture and deploy bioweapons with little sophistication, or under the semblance of legitimate commercial endeavors, will ensure that bioweapons remain a constant threat to public health.14
In 1925, Poland was a leader in developing the Geneva Protocol, a treaty that also prohibited the use of bioweapons. However, the usefulness of treaties in preventing the future development and use of bioweapons is questionable, and the issue of verification remains unresolved and controversial. For example, Poland was among the first countries to use bioweapons in sabotage operations against the Germans in World War II.13
The Japanese also began one of history's most notorious bioweapons programs in 1932, and numerous human experiments were conducted at the infamous Unit 731 throughout the war. Located in Manchuria, Unit 731 sprawled across 150 buildings and five satellite camps, and had a staff of more than 3,000 scientists and technicians.2,14 Unit 731 allegedly experimented with biological agents on at least 3,000 prisoners of war. Of these prisoners of war, more than 1,000 were estimated to have died following experiments using such zoonoses as anthrax, botulism, brucellosis, and plague. These allegations were supported during a military tribunal held in the former Soviet Union in December 1949.
With World War II came increased development of bioweapons, most of which were zoonoses. The Allies created bioweapons for potential retaliatory use in response to German biological attack.14 The U.S. offensive bioweapons program began in 1942 with the establishment of the War Research Service, a civilian agency that conducted research and development at Camp Detrick, Maryland. It was reported that approximately 5,000 anthrax bombs were prepared at Camp Detrick, but none were used during the war.2
Adolf Hitler reportedly issued orders prohibiting bioweapons development in Germany. However, with the support of high-ranking Nazi party officials, German scientists began bioweapons research, although their results lagged far behind that of other countries.14
Research in the U.S. on bioweapons reportedly climaxed from 1950 to 1969. Vigo, Indiana, became home to a bioweapons plant that, if it were put into use, would have been capable of producing 100 tons of anthrax spores per month.14 By the late 1960s, the U.S. military had developed an arsenal that included lethal zooonotic diseases such as anthrax, brucellosis, tularemia, Q fever, and Venezuelan equine encephalitis.2
In addition, the U.S. started a program in 1953 to develop countermeasures, including vaccines, antisera, and therapeutic agents, that would protect troops from possible biological attack. President Nixon terminated the U.S. offensive bioweapons program in 1969 and 1970. Given the available conventional, chemical, and nuclear weapons, bioweapons were not considered essential for national security.2,14 In 1971, the U.S. military released to the civilian population a Venezuelan equine encephalomeningitis (VEE) vaccine developed to protect troops during biowarfare.
EXOTIC SLEEPING SICKNESS OUTBREAK
An epizootic of an exotic sleeping sickness spread into the U.S. in 1971, with 400,000 horses quarantined in Texas in an attempt to halt expansion of the outbreak. The disease was called VEE and was an extension of an epidemic that involved thousands of humans and equids, which appeared to have begun in 1969 at the Peru-Ecuador border.15 The disease had a high fatality rate (>50%) in horses and was debilitating in humans, producing flulike symptoms and a case fatality rate of about 1%. The virus has been responsible for large outbreaks of the disease in horses and people over large geographic areas in the New World.16
In July 1971, the Agriculture Secretary declared a national emergency to fight the sleeping sickness epidemic. In most equine arboviruses, the horse is not an efficient amplification host. The significance of infected horses in maintaining epizootic VEE, however, is illustrated by the observation that human disease has never been demonstrated in the absence of equine disease. Horses with VEE develop a sufficient level of viremia to act as a reservoir or amplifying hosts and are considered the most important species for amplification of virus in VEE epizootics.16
The U.S. Army released stockpiles of an attenuated live-strain vaccine, TC-83, developed to protect troops in biowarfare.17 Mandatory vaccination of horses was required in the southern-border states (Alabama, Arizona, California, Georgia, Florida, and Mississippi) to create a wall of immunity to halt the northward spread of the outbreak.
In this situation, a vaccine developed for use in humans was released for use on horses to halt the spread of the zoonosis around the U.S. The declaration of a national emergency, the release of a biowarfare vaccine, and the mandatory vaccination of horses created panic in the nation, and various local and state governments were put on alert.18 However, with the use of the vaccine, the outbreak was quickly resolved.
ANIMALS AS COMMUNITY SENTINELS
Like people, domestic animals and wildlife are exposed to infectious diseases and environmental contaminants in the air, soil, water, and food, and they can suffer from acute and chronic diseases from such exposure. Often, animals serve as disease sentinels, or early-warning systems, for the community. Animals can alert the public to infectious and noninfectious diseases.
Canaries were used for more than 75 years in Great Britain as a biological sentinel to detect toxic gases in mines. If the canary became acutely ill or died, the miners would quickly evacuate the mine. Today, the expression “canary in a coal mine” is used to refer to an indicator or event that serves as a warning that a potentially detrimental change has taken place and immediate intervention is mandated.19 An assault on human populations with a bioterrorism agent would likely pose a health risk to animal populations in the target area; therefore, integrating veterinary and human public health surveillance efforts is essential.
Public health policy is, by nature, an interprofessional endeavor. The veterinary practitioner sees animals on a daily basis and would likely see the impact of the agent in their patients. As such, they can function as the eyes and ears of government agencies when an atypical disease situation occurs. Such an event could be the release of a biological agent.
For example, in 1979 an epidemic of anthrax occurred in April among people who lived or worked within a distance of 4 km in a narrow zone downwind of a Soviet military microbiology facility. In addition, livestock died of anthrax along the extended axis of the epidemic zone out to a distance of 60 km. Anthrax of cattle and sheep is characterized by sudden onset and a rapidly fatal course. Often, the course of disease in these animals is so rapid that illness is not observed and animals are found dead. Such a sudden die-off of animals is an alert to the community that a problem exists.2,14
On Long Island, New York, in 1999, West Nile virus was first isolated from horses with an atypical neurological disease. As the mortality rate in horses was about 35%, veterinarians searched for unusual causes. The first alert that something atypical was occurring was in 1999 when birds, particularly crows, began dying of an unknown neurologic disease.16
Some advantages of using animals as sentinels include lower cost, shorter latency of disease development, and greater ease of obtaining tissue samples and autopsy data. To understand what is happening in animals requires regular and systematic data analysis to identify health hazards. Sick animals can alert people to environmental dangers in much the same way that a barking dog alerts its owner of an intruder. Animal surveillance for such infectious diseases as bubonic plague, equine viral encephalomyelitis, hantavirus, and rabies is conducted routinely by public health departments. Animal outbreaks of these diseases typically precede human outbreaks, allowing time for preventive action to reduce or prevent human cases.
ANIMALS AS EVIDENCE OF BIOTERRORISM
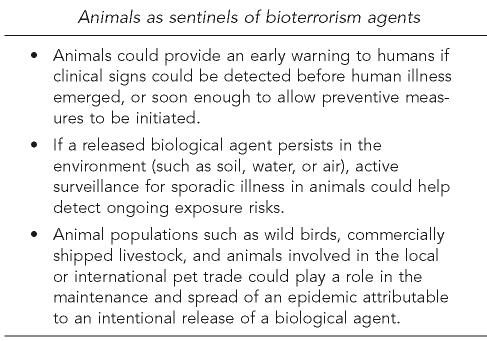
A review of the scientific literature from 1966 to 2005 was conducted to obtain evidence for public health decisions on the use of animals in early warning of a bioterrorism attack, markers for ongoing exposure risk, and propagation of a bioterrorism outbreak. The review found evidence that, for certain bioterrorism agents, pets, wildlife, or livestock could provide early warning, and that for other agents, humans would likely manifest symptoms before illness could be detected in animals.20 Three of the major conclusions support what was earlier thought to be the case (Figure 2). Some general conclusions that came out of the research include:
(1)Public health should build capacity for active surveillance and intervention efforts to detect and control ongoing outbreaks of disease in domestic and wild animal populations.
(2)Integrating veterinary and human public health surveillance efforts is essential in dealing with bioterrorism. This effort will require improved communication and collaboration.
(3)Physicians and veterinarians should work closely together in clinical, public health, and research settings. Comparative medicine looks at disease processes across species, and the majority of diseases are not limited to a single species.21
(4)Epidemiologic principles and diagnostic criteria are similar regardless of the animal species involved.
(5)Early identification of zoonotic disease occurrence, through simultaneous monitoring of human and animal disease surveillance systems, is critical to protect health in both populations.22
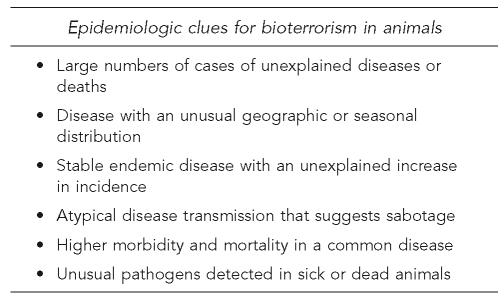
(6)Coordinated and cohesive efforts by scientists, health-care providers, veterinarians, and epidemiologists are needed to control the global impact of biowarfare.6 Animals hold several epidemiologic clues for possible bioterrorism (Figure 3).
Figure 2.
Conclusions based on actual bioterrorism events, as well as naturally occurring epizootics
Figure 3.
Evidence to guide disease detectives when investigating an outbreak
CONCLUSIONS
With zoonoses as the most likely infectious diseases to be used by bioterrorists, human and veterinary medicine can benefit from cross-collaboration. As barriers between animal species collapse, it expands the knowledge base of human and veterinary medicine.23 This concept was recognized with the recent development of the “one medicine” concept by the American Medical Association and the American Veterinary Medical Association. By breaking down the walls between the two fields, we will help fight diseases that jump between animals and humans and ultimately advance both human and animal health.24,25
The majority of the emerging infectious diseases, including those caused by bioterrorist agents, are zoonoses. Because these diseases can infect animals and humans, the medical and veterinary communities should work closely together in clinical, public health, and research settings. These efforts would increase our understanding of how zoonoses expand their host range and would, ultimately, improve prevention and control strategies.21
Public health, health-care, and veterinary communities have an enormous challenge in the early recognition, reporting, treatment, and prevention of zoonotic diseases. As such, a transformed system of disease surveillance that is predicated on seamless integration of a diverse set of capabilities is required. A one-medicine perspective enhances zoonoses detection and control by surveillance and communication. This practice extends to earlier concepts of not restricting medicine to species barriers in the search for better health and to generate added value to common disciplinary health. The one-medicine viewpoint also requires sensitivity to specific contexts of societies, cultures, and health systems.26
A community surveillance system that is reliant solely on humans will not provide early health warning, but will instead record history.2 A truly comprehensive national early health-warning system will rely upon the vertical integration of local, state, federal, and international officials, as well as the horizontal integration of animal health, human health, public safety, communication, transportation, intelligence, and national security professionals and institutions.
Dr. Edward Jenner (1749–1823) is famous as the pioneer of vaccination against smallpox.
REFERENCES
- 1.Center for Law and the Public's Health at Georgetown and Johns Hopkins Universities. The Model State Emergency Health Powers Act. Centers for Disease Control and Prevention (US) 2001. [cited 2007 Dec 18]. Available from: URL: www.publichealthlaw.net/MSEHPA/MSEHPA2.pdf.
- 2.Noah DL, Huebner KD, Darling RG, Waeckerle JF. The history and threat of biological warfare and terrorism. Emerg Med Clin North Am. 2002;20:255–71. doi: 10.1016/s0733-8627(01)00002-5. [DOI] [PubMed] [Google Scholar]
- 3.Vorobyov A. Criterion rating as a measure of probable use of bio agents as biological weapons. Papers presented to the Working Group on Biological Weapons Control of the Committee on International Security and Arms Control; Washington: National Academy of Sciences; 1994. [Google Scholar]
- 4.Franz DR, Jahrling PB, Friedlander AM, McClain DJ, Hoover DL, Bryne WR, et al. Clinical recognition and management of patients exposed to biological warfare agents. JAMA. 1997;278:399–411. doi: 10.1001/jama.278.5.399. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (US) Bioterrorism agents/diseases. [cited 2007 Dec 18]. Available from: URL: http://www.bt.cdc.gov/agent/agentlist-category.asp#b.
- 6.Khardori N. Bioterrorism and bioterrorism preparedness: historical perspective and overview. Infect Dis Clin North Am. 2006;20:179–211. doi: 10.1016/j.idc.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (US) Bioterrorism overview. [cited 2007 Dec 18]. Available from: URL: http://www.bt.cdc.gov/bioterrorism/overview.asp.
- 8.Kaufmann AF, Meltzer MI, Schmid GP. The economic impact of a bioterrorist attack: are prevention and postattack intervention programs justifiable? [cited 2007 Dec 18];Emerg Infect Dis. 1997 3:83–94. doi: 10.3201/eid0302.970201. Also available from: URL: http://www.cdc.gov/ncidod/eid/vol3no2/kaufman.htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Smallpox: historical significance. [cited 2007 Dec 18]. Available from: URL: http://www.who.int/mediacentre/factsheets/smallpox/en.
- 10.Parrino J, Graham BS. Smallpox vaccines: past, present, and future. J Allergy Clin Immunol. 2006;118:1320–6. doi: 10.1016/j.jaci.2006.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stewart AJ, Devlin PM. The history of the smallpox vaccine. J Infect. 2006;52:329–34. doi: 10.1016/j.jinf.2005.07.021. [DOI] [PubMed] [Google Scholar]
- 12.The Jenner Museum. [cited 2007 Dec 18]. Available from: URL: http://www.jennermuseum.com.
- 13.Lesho ME, Dorsey MD, Bunner D. Feces, dead horses, and fleas. Evolution of the hostile use of biological agents. West J Med. 1998;168:512–6. [PMC free article] [PubMed] [Google Scholar]
- 14.Christopher GW, Cieslak TJ, Pavlin JA, Eitzen EM., Jr Biological warfare: a historical perspective. JAMA. 1997;278:412–7. [PubMed] [Google Scholar]
- 15.Calisher CH. Medically important arboviruses of the United States and Canada. Clin Microbiol Rev. 1994;7:89–116. doi: 10.1128/cmr.7.1.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gibbs EP, Long MT. Equine alphaviruses. In: Sellon DC, Long MT, editors. Equine infectious diseases. Philadelphia: W.B. Saunders Co.; 2006. pp. 191–7. [Google Scholar]
- 17.French GR, Plotkin SA. Miscellaneous limited-use vaccines. In: Plotkin SA, Orenstein WA, editors. Vaccines. 3rd ed. Philadelphia: W.B. Saunders Co.; 1999. pp. 728–42. [Google Scholar]
- 18.Texas embargoes horses in epidemic; thousands expected to die; 34 humans infected. Los Angeles Times. 1971. Jul 15,
- 19.Cheatham ML. Is the canary still singing? Crit Care Med. 2007;35:320–1. doi: 10.1097/01.CCM.0000251843.34578.F2. [DOI] [PubMed] [Google Scholar]
- 20.Rabinowitz P, Gordon Z, Chudnov D, Wilcox M, Odofin L, Liu A, et al. Animals as sentinels of bioterrorism agents. [cited 2007 Dec 18];Emerg Infect Dis. 2006 12:647–52. doi: 10.3201/eid1204.051120. Also available from: URL: http://www.cdc.gov/ncidod/eid/vol12no04/05-1120.htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kahn LH. Confronting zoonoses, linking human and veterinary medicine. [cited 2007 Dec 18];Emerg Infect Dis. 2006 12:556–61. doi: 10.3201/eid1204.050956. Also available from: URL: http://www.cdc.gov/ncidod/eid/vol12no04/05-0956.htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mauer WA, Kaneene JB. Integrated human-animal disease surveillance. [cited 2007 Dec 18];Emerg Infect Dis. 2005 11:1490–1. doi: 10.3201/eid1109.050180. Also available from: URL: http://www.cdc.gov/ncidod/eid/vol11no09/05-0180.htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kahn LH. The zoonotic connection. Bull Atom Scientists. 2007 [Google Scholar]
- 24.Enserink M. Medicine. Initiative aims to merge animal and human health science to benefit both. Science Magazine. 2007;316:1553. doi: 10.1126/science.316.5831.1553a. [DOI] [PubMed] [Google Scholar]
- 25.Zinsstag J, Schelling E, Wyss K, Mahamat MB. Potential of cooperation between human and animal health to strengthen health systems. Lancet. 2005;366:2142–5. doi: 10.1016/S0140-6736(05)67731-8. [DOI] [PubMed] [Google Scholar]
- 26.Mattix ME, Zeman DH, Moeller R, Jackson C, Larsen T. Clinicopathologic aspects of animal and zoonotic diseases of bioterrorism. Clin Lab Med. 2006;26:445–89. doi: 10.1016/j.cll.2006.03.010. [DOI] [PubMed] [Google Scholar]