SYNOPSIS
The threat of bioterrorism and emerging infectious diseases has prompted various public health agencies to recommend enhanced surveillance activities to supplement existing surveillance plans. The majority of emerging infectious diseases and bioterrorist agents are zoonotic. Animals are more sensitive to certain biological agents, and their use as clinical sentinels, as a means of early detection, is warranted.
This article provides design methods for a local integrated zoonotic surveillance plan and materials developed for veterinarians to assist in the early detection of bioevents. Zoonotic surveillance in the U.S. is currently too limited and compartmentalized for broader public health objectives. To rapidly detect and respond to bioevents, collaboration and cooperation among various agencies at the federal, state, and local levels must be enhanced and maintained. Co-analysis of animal and human diseases may facilitate the response to infectious disease events and limit morbidity and mortality in both animal and human populations.
Emerging infectious diseases are a threat to underdeveloped countries as well as industrialized countries as numerous risk factors for human disease emergence exist in both populations. Zoonoses are diseases transmittable between humans and animals. A 2001 report concluded that there are 1,415 species of infectious organisms known to be pathogenic to humans; of these, 868 (61%) are zoonotic. In addition, of the 175 pathogens considered to be emerging, 132 (75%) are zoonotic.1
Zoonoses can be introduced to the U.S. naturally or inadvertently (e.g., international travel, smuggled products, and animals) or via weaponized biological agents. Zoonotic agents may be considered for intentional release to cause damage and turmoil, as they can simultaneously target the health of both human and animal populations and have a serious socioeconomic impact.2
The U.S. General Accounting Office Report, West Nile Virus Outbreak, Lessons for Preparedness,3 indicated that the analysis of the West Nile virus (WNV) outbreak began as two separate investigations: one of sick people and the other of dying birds. It took almost three months to link the events to one disease. Recommendations in the report identified the need to address five areas, including coordination between public health and animal health efforts.
Based on publicly accessible state surveillance plans and disease reporting regulations, animal zoonotic surveillance activities are distinctly varied among states. Jurisdictional and geographical differences in surveillance activities impede a unified approach to an early detection system.4
ANIMALS AS SENTINELS OF ZOONOTIC ILLNESSES
Animal sentinels are defined by R.G. Stahl, Jr. as “any non-human organism that can react to. .. an environmental contaminant before the contaminant impacts people.”5 Animals are used in sentinel surveillance systems for the following reasons: (1) animals share environments with humans, (2) animals and humans respond to many toxic (or infectious) agents in analogous ways, and (3) clinical signs may manifest in animals prior to humans.6 There is scientific evidence that sentinel surveillance activities are predictive of human risk. For example, a report on dead crow density and WNV monitoring in New York confirmed that the elevated dead crow densities correlated to higher risk for disease in humans.7
An article by Rabinowitz et al. provides further support for the use of animals as sentinels, by reporting evidence that animals can: (1) provide early warning of an acute bioterrorist attack, (2) be markers for ongoing exposure risk, and (3) if mobile, propagate and maintain an epidemic.8 There is merit in using pets, farm animals, and wildlife as clinical sentinels, as each can serve a distinct role in disease detection and risk assessment.
PURPOSE OF THIS FRAMEWORK
This article provides design methods for the development of a local health department early-warning detection system for zoonotic bioevents. A bioevent is defined as a bioterror (BT) attack or large-scale, naturally occurring zoonotic event, such as pandemic influenza.
The objective of this reporting framework is to integrate veterinary health reporting with the human public health system. The local health department can provide educational materials and reporting instructions to supply veterinarians with the resources needed to facilitate the reporting of significant public health diseases. In addition to the early identification of an event, monitoring an outbreak is also integral to this plan's purpose, whether monitoring the geographic scope or maintaining vigilance of animal-propagated epidemics. The plan should reduce current gaps in data analyses and surveillance activities. The goal of animal-human integrated surveillance is to provide a means of early disease recognition and enhanced detection of human zoonoses, expedite a response to an outbreak or hazardous event, and consequently limit morbidity and mortality in both human and animal populations.
REPORTING SYSTEM DESCRIPTION
This framework was developed to be adaptable to emerging diseases and events so that it can be used as an “all-hazards” surveillance approach, with a focus on the threats that are of public health importance. This is a passive reporting system that relies on clinical signs demonstrated in animals to identify the initial manifestations of a bioevent or outbreak. Co-analysis of animal and human zoonotic disease events complements existing human health surveillance plans, may facilitate an early response, and may prevent widespread illness in both populations.
The plan proposes that local health departments request veterinarians to voluntarily report zoonotic animal diseases of potential public health threat to the local health department. Existing animal disease reporting requirements, and investigation and response procedures, will remain unchanged and carried out in accordance with the appropriate state and federal regulations.
Tools are provided within this article to proactively educate veterinarians on rarely encountered emerging disease agents. This framework is meant to be dynamic, adaptable, and flexible. The plan includes a list of preliminary agents and animals under surveillance, and the lists may be customized by each locality.
Performing a region-specific analysis
An effective zoonotic reporting plan is based on the unique demographics, geography, animal populations, government infrastructure, and bioevent vulnerabilities of the region under surveillance. To tailor a plan to a specific region, the health department should gather the following information.
Demographics
The human population and household estimates should be obtained from U.S. Census Bureau records.
Farm and zoo animal populations
Livestock can be the target of an agroterrorism attack. Agriculture clubs, zoos, petting zoos, and equestrian activities can increase the risk of human-acquired zoonoses. Population estimates for the predominant farm and zoo animals in the region under consideration should be determined. Population estimates for farm animals may be obtained from the U.S. Department of Agriculture (USDA) census records available on the USDA website (http://www.nass.usda.gov/Census_of_Agriculture/index.asp). Zoo locations can be obtained through the yellow pages and/or the Internet.
Companion animal populations
Aside from the risk of humans and their companion animals transmitting infectious diseases to each other, pets that are free to roam outdoors can be at risk for acquiring numerous pathogens from both the environment and their interactions with wildlife. The American Veterinary Medical Association (AVMA) published formulae for determining pet populations for dogs, cats, and pet birds, based on household estimates.9 If other sources are available for determining pet populations, such as local Animal Control Services, they should also be utilized.
Predominant wildlife
Wild animals could be involved in the propagation of an epidemic due to their mobility and capability of contaminating a large geographical area.10 Wild animals usually do not receive veterinary care and surveillance activities are minimal. These animals are usually mobile and dispersed, and therefore the most prominent sentinel activities in wildlife are die-offs and neurological signs.11 Wildlife interfaces with humans, pets, and farm animals, and due to changing habitats and residential development, these interactions have increased.12 The U.S. Fish and Wildlife Services along with state wildlife services have data available to determine the predominant wildlife in a specific region.
Transportation
Major ports, international airports in particular, escalate the risks to a region and can be a critical factor in intentional or inadvertent novel disease introduction. There is also the possibility of the legal or illegal importation of animals, animal products, and other biologicals that may introduce a disease event. It is important to identify the ports in a region and be aware of the regulatory activities governing the importation and quarantine of animals and biological products.
Regulatory authority
Because state regulations vary, your current state regulations should be reviewed prior to the final determination of which agents and animals to include in the plan. The following disease reporting regulations should be evaluated as needed: human, livestock, pet, and wildlife diseases, as well as animal import regulations. Note any gaps in reportable diseases and surveillance programs. The proposed surveillance plan may be best instituted by the local health department as a voluntary reporting system.
Government infrastructure
It is imperative to evaluate communications and responsibilities within state and local departments with regard to both animal and human disease surveillance and control. Identify gaps or procedures that may interfere with the objectives of integrated surveillance. Determine if data can be timely collected and reported from other offices (e.g., State Veterinarian's Office) to enhance the data collection mechanisms of local surveillance activities. For example, state wildlife or agriculture agencies may be collecting serological sentinel data that can be used as an adjunct to the clinical data the local health department is collecting.
Also, assess the procedures and processes of the local animal control office and determine the information that can be obtained from this agency. Memoranda of understanding may be required for coordination among agencies.
Gather regional epidemiologic data
It is important for the local health department to gather epidemiologic data for the selected agents in the region to establish baseline rates. Knowledge of expected incidence rates will enhance the response to an outbreak. Once this plan is implemented, animal and human population estimates can also be used to determine the incidence of diseases reported during a given time period.
SELECTED AGENTS AND ANIMALS UNDER SURVEILLANCE
The selection of zoonotic agents for this framework was based on public health significance, severity, and preventability in the human population. Animal species were selected based on population estimates, which may not apply to every geographical area.
Agents
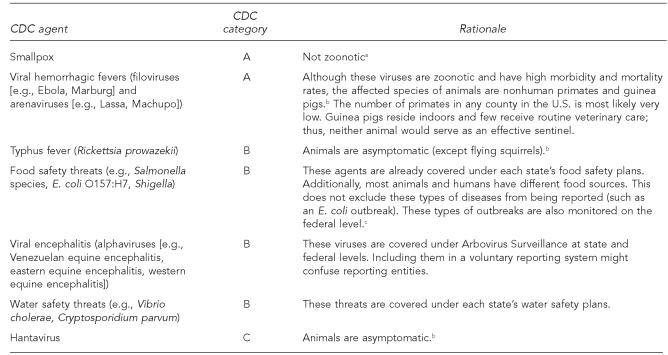
The Centers for Disease Control and Prevention's (CDC's) Potential Bioterror Agents were considered first.13 Those agents that are not zoonotic, are covered under other integrated surveillance activities, or are asymptomatic in animals were excluded from this framework. Figure 1 lists agents not included in this framework.
Figure 1.
CDC potential bioterrorist agents currently excluded from the framework
Aiello SE, editor. The Merck veterinary manual. 8th ed. Whitehouse Station (NJ): Merck – Co., Inc.; 1998.
The Center for Food Security and Public Health. Iowa State University. Animal disease information [cited 2005 Sep 5]. Available from: URL: www.cfsph.iastate.edu/DiseaseInfo/default.htm
Centers for Disease Control and Prevention (US). FoodNet—Foodborne Diseases Active Surveillance Network [cited 2005 Oct 16]. Available from: URL: www.cdc.gov/foodnet
CDC = Centers for Disease Control and Prevention
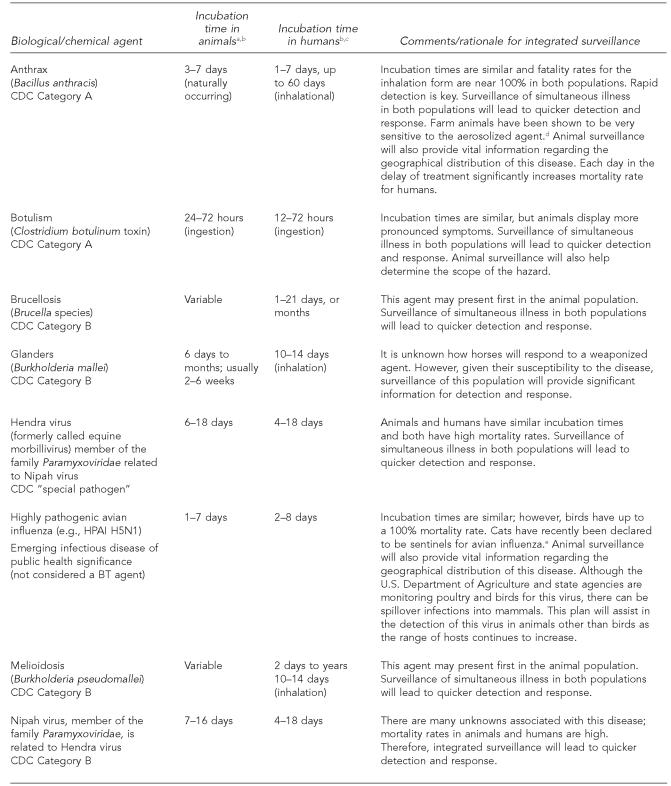
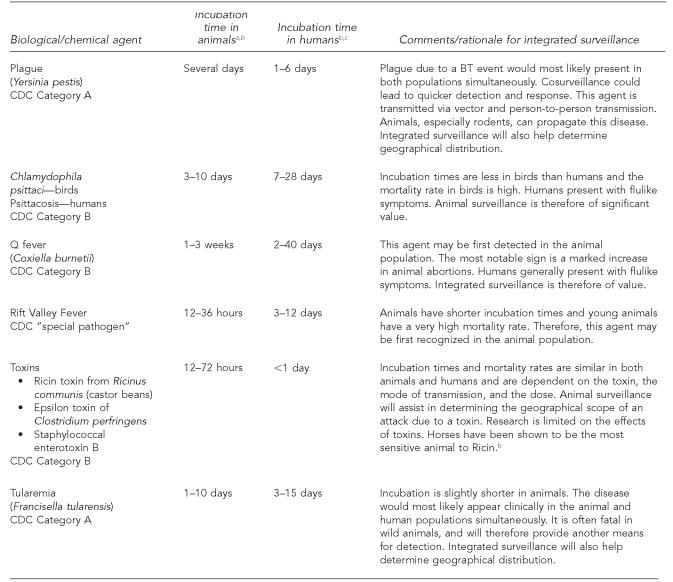
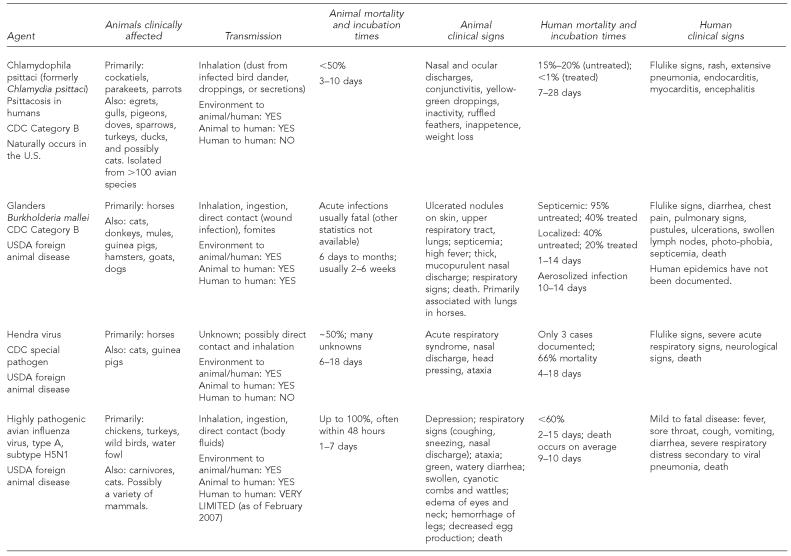
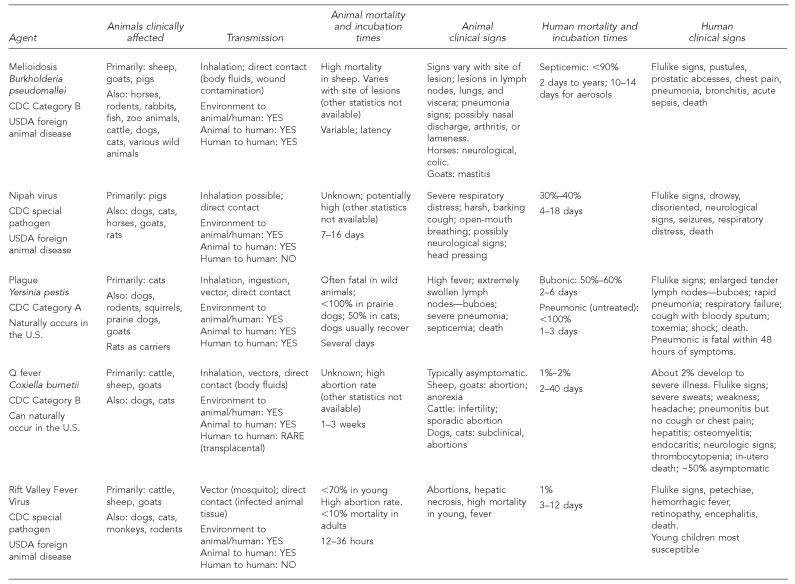
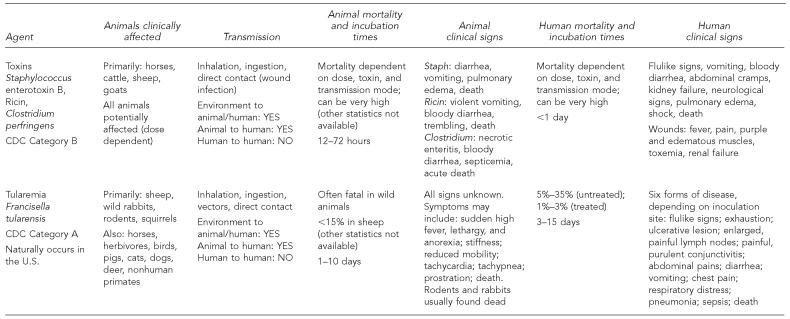
In addition to potential BT agents, this plan also includes highly pathogenic influenza viruses. The biological agents selected, and the rationale for surveillance of each, are included in Figure 2, and transmission routes are summarized in Figure 3. Agents under surveillance may be amended based on regional differences.
Figure 2.
Selected agents and sentinel attributes that will enhance current surveillance activities
Aiello SE, editor. The Merck veterinary manual. 8th ed. Whitehouse Station (NJ): Merck – Co., Inc.; 1998.
The Center for Food Security and Public Health. Iowa State University. Animal disease information [cited 2005 Sep 20]. Available from: URL: www.cfsph.iastate.edu/DiseaseInfo/default.htm
Chin JE, editor. Control of communicable diseases manual. 17th ed. Washington: American Public Health Association; 2000.
Glickman LT, Fairbrother A, Guarino AM, Bergman HL, Buck WB, Collins Cork L, et al. Animals as sentinels of environmental health hazards. Committee on Animals as Monitors of Environmental Hazards. Commission on Life Sciences. Washington: National Academy Press; 1991.
Rimmelzwaan GF, van Riel D, Baars M, Bestebroer TM, van Amerongen G, Fouchier RAM, et al. Influenza A virus (H5N1) infection in cats causes systemic disease with potential novel routes of virus spread within and between hosts. Am J Pathol 2006;168:176-83.
CDC = Centers for Disease Control and Prevention
BT = bioterror
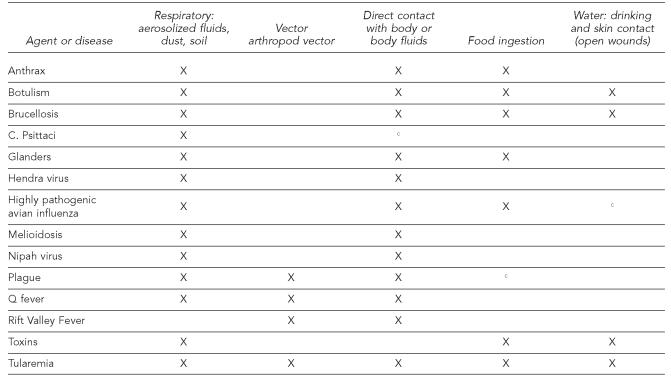
Figure 3.
Aiello SE, editor. The Merck veterinary manual. 8th ed. Whitehouse Station (NJ): Merck – Co., Inc.; 1998.
The Center for Food Security and Public Health. Iowa State University. Transmission routes [cited 2005 Nov 7]. Available from: URL: http://www.cfsph.iastate.edu/Handouts/resources_list.htm
Possible, depending on species
Animals
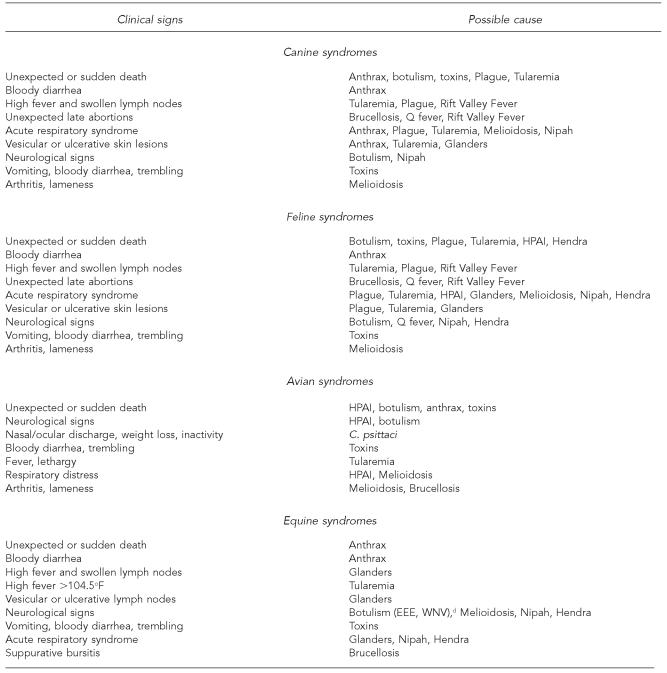
Once animal population estimates for a region are obtained, the animal species can be cross-referenced with the selected agents, using Figure 4 to determine the suitable sentinels. The preliminary agents and the susceptible species are captured in the educational quick reference charts (Figures 3 to 6). The following is a list of animals included as a base in this framework:
Companion animals (pets): Dogs, cats, ferrets, horses, and pet birds. Ferrets are included because they are common pets in the U.S. and are very susceptible to influenza.14,15
Livestock: Cattle, sheep, goats, poultry, and swine.
Wildlife: Deer, foxes, raccoons, and avian species. Although rodents and lagomorphs are affected by many of the agents, death in these populations would be difficult to detect; the carnivorous animals would therefore serve as more effective sentinels.
Figure 4.
Aiello SE, editor. The Merck veterinary manual. 8th ed. Whitehouse Station (NJ): Merck – Co., Inc.; 1998.
The Center for Food Security and Public Health. Iowa State University. Animal disease information [cited 2005 Sep 20]. Available from: URL: www.cfsph.iastate.edu/DiseaseInfo/default.htm
Orloski KA, Lathrop SL. Plague: a veterinary perspective. J Am Vet Med Assoc 2003;222:444-8.
Center for Infectious Disease Research and Policy, University of Minnesota. Bioterrorism [cited 2006 Feb 26]. Available from: URL: http://www.cidrap.umn.edu
Feldman KA. Tularemia. J Am Vet Med Assoc 2003;222:725-30.
American Veterinary Medical Association. Potential zoonotic agents of bioterrorism. Anthrax [cited 2006 Mar 8]. Available from: URL: www.avma.org/public_health/biosecurity/default.asp
Dependent on influenza strains and mutations
The effects of toxins are dependent on the toxin, the dose, and the mode of transmission.
Horses are the most sensitive animal to Ricin toxin.
H = high
M = moderate
L = low
U = potential/unknown
● = no evidence in the literature
Figure 6.
Centers for Disease Control and Prevention (US). Bioterrorism overview: bioterrorism agent categories [cited 2007 Feb 20]. Available from: URL: http://www.bt.cdc.gov/bioterrorism/overview.asp
Aiello SE, editor. The Merck veterinary manual. 8th ed. Whitehouse Station (NJ): Merck – Co., Inc.; 1998.
The Center for Food Security and Public Health. Iowa State University. Animal disease information [cited 2005 Sep 20]. Available from: URL: www.cfsph.iastate.edu/DiseaseInfo/default.htm
Center for Infectious Disease Research and Policy, University of Minnesota. Bioterrorism [cited 2006 Feb 26]. Available from: URL: http://www.cidrap.umn.edu
American Veterinary Medical Association. Potential zoonotic agents of bioterrorism. Anthrax [cited 2006 Mar 8]. Available from: URL: www.avma.org/public_health/biosecurity/default.asp
U.S. Department of Agriculture. Animal and Plant Health Inspection Service. Publications. Animal health [cited 2005 Mar 10].Available from: URL: http://www.aphis.usda.gov/publications/animal_health/index.shtml
World Health Organization. Avian influenza [cited 2006 Jan 10]. Available from: URL: http://www.who.int/csr/disease/avian_influenza/en
Beigel JH, Farrar J, Han AM, Hayden FG, Hyer R, de Jong MD, et al. Avian influenza A (H5N1) infection in humans. N Engl J Med 2005;353:1374-85.
Chin JE, editor. Control of communicable diseases manual. 17th ed. Washington: American Public Health Association; 2000.
Morrison G. Zoonotic infections from pets. Postgrad Med 2001;110. Also available from: URL: http://www.postgradmed.com/issues/2001/07_01/morrison.htm [cited 2006 Jan 19].
CDC = Centers for Disease Control and Prevention
GI = gastrointestinal
USDA = U.S. Department of Agriculture
SYSTEM DESIGN AND REPORTING MECHANISMS
The essential components of an integrated zoonotic surveillance system include: rapid identification of a disease threat; rapid reporting of a disease event; monitoring and analysis of reported diseases; assessment of human exposures or concurrent infections; communication and collaboration; and a rapid and coordinated response. It was determined that the sensitivity of disease surveillance and the rapidity of a response are the most valuable attributes of this system. Positive predictive value may suffer when sensitivity is increased. Case definitions should be employed to subdivide cases as suspect, probable, and confirmed to better qualify the reports submitted.
Local health departments should determine the best means for gathering animal zoonotic data. Because timeliness is extremely important, veterinarians should be requested to report cases potentially attributable to the selected agents (or other possible threats) within 24 hours to the health department.
Analyze infrastructure and reporting mechanisms
Once your region has evaluated governmental infrastructures and determined the factions from where additional animal disease data can be obtained, enhancing methods for vertical and horizontal government communication can be planned. Relationships among agriculture, wildlife, and human health departments may need to be strengthened.
The local health department should be prepared to receive reports in the form of written, oral, or electronic communications, from the veterinary sector as well as intra- and interagency partners; at times, data may need to be actively collected.
Awareness
A reporting form may be developed, or veterinarians and others could be asked to report via telephone. Materials sent to veterinarians should include a purpose statement for this surveillance activity; instructions for reporting; contacts for laboratory testing, specimen collection, and quarantine procedures; and contacts to call for suspected illnesses.
Figures 3 to 6 provide information on the agents, the animals affected, and clinical and epidemiologic features for both animal and human populations. These figures can be provided to veterinarians or used as a foundation for educational materials. Quick reference charts, such as these, should prepare veterinarians, the health department, and others to recognize the early signs of these uncommon disease events and respond more rapidly. These materials will also assist veterinarians with counseling pet owners and managing occupational exposures.
INVESTIGATION, RESPONSE, AND OTHER CONSIDERATIONS
Although an event concerning an animal case or outbreak will be reported to the health department, the appropriate authorities should investigate (e.g., State Veterinarian's Office) according to existing protocol. Details of the investigation should be communicated to the health department. A response to an agroterror or BT event would be conducted by various government levels and agencies and would require multi-institutional collaboration and coordination.
A reporting plan is the first step in an integrated zoonotic surveillance system. Other activities that a local health department may need to consider and address include:
Identification of the consortia, industries, and agencies that will be asked to report
Review of regulations and agency responsibilities
Definition of official responsibilities and points of contact at local and state levels
Determination of responsibilities for evaluation and analysis of data, report dissemination, risk communication, and consequence management
Allocation of resources
Identification of the most effective communication channels for the various partners
Enhancing relationships within and with other offices and agencies as needed
Determining thresholds for intervention
Performing active educational outreach to veterinarians and various animal groups
Determining any barriers to veterinary and intra- or interagency reporting
Coordination with adjoining jurisdictions
Review of information technology capabilities
Other logistical, administrative, and training issues
LIMITATIONS AND ASSUMPTIONS
This framework is designed to be a passive system. The plan can become active for a specific agent(s) during a time of perceived or actual crisis. Epidemiologic and clinical data in the educational materials are based on the published literature for naturally occurring diseases and may not represent the clinical or epidemiologic features of a weaponized agent. The educational materials and information in this plan are based on scientific data as of February 2007. The plan is limited to the potential BT and emerging zoonotic agents of greatest human threat at the time this article was written.
This framework is limited to select agents. If an unanticipated agent causes an outbreak, or a bioengineered terror agent is dispersed, the educational materials will be of limited use. However, having a plan in place for effective management of a zoonotic outbreak will facilitate and expedite response activities.
If there is population dispersion of wild animals crossing county and state lines, clusters or trends may not be recognized. In addition, residents who do not provide veterinary care for their animals will not be captured by this system.
RECOMMENDATIONS
Educational and reporting materials should initially be disseminated to veterinarians and Animal Control Services. Increasing awareness in other sectors is strongly recommended for pet stores, zoos, wildlife rehabilitation groups, pet owner groups, animal rescue societies, animal shelters, academic institutions, and U.S. Customs/USDA stationed at ports. Evaluation of animal diagnostic laboratory reporting can also be performed for supplemental reporting.
The framework can be expanded to include additional agents and hazards separately covered under other state or federal systems, such as Lyme disease. For harmonization purposes, zoonotic diseases covered under other animal-human health surveillance systems, such as rabies and WNV, may be considered for inclusion in this plan.
A task force consisting of representatives of the local health department; Animal Control Services; the state health, agriculture, and wildlife departments; the regional veterinary diagnostics laboratory; academia; and community veterinarians would be an effective collaborative team for ensuring the success of an animal-human integrated zoonotic surveillance program. The task force can also help establish case definitions, identify reporting sources and mechanisms, address barriers to reporting, and instigate interdisciplinary networking. Although resources may be limited, having a broad array of partners will contribute greatly to a responsive local public health system.16
CHALLENGES
Novel surveillance systems face many challenges and it may take time before the proposed system operates as expected. Incentives to report suspected diseases are limited and confidentiality must be ensured to prevent potential economic losses to the various animal industries. Additionally, jurisdictional issues (animal health agencies vs. human health) may also serve as a barrier to this reporting system. Collaboration and coordination among various agencies and stakeholders are crucial and need to be addressed for the optimal implementation, maintenance, and expansion of surveillance activities. Information sharing and interdisciplinary partnerships via a task force could serve as an incentive to partake in the voluntary system.
There may be a need to sustain veterinary interest, especially when the threat of bioterrorism is perceived to be low, and/or if no significant zoonotic events are encountered after a period of time. However, it should be noted that over time, a zero incidence (i.e., no reported cases) does not equate to a failure of the surveillance plan.
Local health departments may not have the information technology and the budget for electronic reporting. A paper system may overwhelm and challenge some health departments, especially in the event of an emergency situation. Staff available to respond to emergencies might also be limited.
There exists a need for more research on the effects of weaponized biological agents. Also, several emerging agents, such as Hendra and Nipah viruses, are poorly understood given the rarity of outbreaks. This shortcoming of information can have a significant influence on recognition and response activities. The plan will require updating as new scientific evidence becomes available.
CONCLUSION
Strengthening the U.S. public health infrastructure must include bringing human and veterinary medicine together. Improved interagency communication and collaboration will facilitate the response to various types of outbreak situations. Aggregate data analyzed from diverse sources may be as significant and effective as the astute physician for early detection. Because BT attacks can occur in any place and at any time, and zoonoses can unpredictably emerge in our society and rapidly spread to other regions, the authors recommend that state and/or national integrated zoonotic surveillance plans be considered to uniformly capture these essential data throughout the U.S.
Figure 5.
NOTE: All symptoms are primarily based on naturally acquired infections. Research on weaponized agents is limited.
Aiello SE, editor. The Merck veterinary manual. 8th ed. Whitehouse Station (NJ): Merck – Co., Inc.; 1998.
Rimmelzwaan GF, van Riel D, Baars M, Bestebroer TM, van Amerongen G, Fouchier RAM, et al. Influenza A virus (H5N1) infection in cats causes systemic disease with potential novel routes of virus spread within and between hosts. Am J Pathol 2006;168:176-83.
Massachusetts Department of Agricultural Resources. Bureau of Animal Health. Bioterrorism and animals: preparedness and response workshops [cited 2006 Mar 2]. Available from: URL: www.mass.gov/agr/animalhealth/bioterrorism/Workshops.htm
Diseases in parentheses are important to consider but are not formally included in this reporting plan.
EEE = Eastern Equine Encephalitis
WNV = West Nile virus
HPAI = highly pathogenic avian influenza
Acknowledgments
The authors acknowledge the following individuals for their technical advice: Rebecca Parkin, PhD, MPH, The George Washington University School of Public Health and Health Services (GWU-SPHHS), Washington; Julia Murphy, DVM, MS, DACVPM, Virginia Department of Health; Linda M. Amendt, MS, MT, U.S. Food and Drug Administration (USFDA); Philip Snoy, DVM, USFDA; Katherine Hunting, PhD, MPH, GWU-SPHHS; Ronald G. King, DVM, Office of Veterinary Services, Virginia Department of Agriculture and Consumer Services; Jonathan Sleeman, MA, VetMB, Dipl. ACZM, MRCVS, Virginia Department of Game and Inland Fisheries; Officer Becky Keenan, Animal Control Division, Falls Church, VA; Gillian Anne Comyn, DVM, MPH, DACVPM, U.S. Department of Agriculture (USDA)/Animal and Plant Health Inspection Service (APHIS)/Veterinary Services (VS); and Dr. Terry L. Taylor, USDA/APHIS/VS. Appreciation is also expressed to the veterinarians who took the time to answer questions and provide feedback.
The views expressed in this article do not necessarily represent the views of the USFDA or the U.S. government.
REFERENCES
- 1.Taylor LH, Latham SM, Woolhouse ME. Risk factors for human disease emergence. Philos Trans R Soc Lond B Biol Sci. 2001;356:938–89. doi: 10.1098/rstb.2001.0888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blancou J, Chomel BB, Belotto A, Meslin FX. Emerging or reemerging bacterial zoonoses: factors of emergence, surveillance and control. Vet Res. 2005;36:507–22. doi: 10.1051/vetres:2005008. [DOI] [PubMed] [Google Scholar]
- 3.General Accounting Office (US) Washington: The Office; 2000. [cited 2006 Apr 6]. West Nile virus outbreak. Lessons for the public health preparedness. GAO/HEHS-00-180. Also available from: URL: http://www.gao.gov/archive/2000/he00180.pdf. [Google Scholar]
- 4.Tucker JB. Washington: Senate Committee on Appropriations; 2001. Oct 3, [cited 2007 Mar 6]. Improving infectious disease surveillance to combat bioterrorism and natural emerging infections. Testimony before the Subcommittee on Labor, Health and Human Services, Education, and related agencies of the U.S. Also available from: URL: http://cns.miis.edu/research/cbw/testtuck.htm. [Google Scholar]
- 5.Stahl RG., Jr Can mammalian and non mammalian “sentinel species” data be used to evaluate the human health implications of environmental contaminants? Hum Ecol Risk Assess. 1997;3:329–35. Quoted in: van der Schalie WH, Gardner HS Jr., Bantle JA, De Rosa CT, Finch RA, Reif JS, et al. Animals as sentinels of human health hazards of environmental chemicals. Environ Health Perspect 1999;107:309–15. [Google Scholar]
- 6.Glickman LT, Fairbrother A, Guarino AM, Bergman HL, Buck WB, Collins Cork L, et al. Commission on Life Sciences. Washington: National Academy Press; 1991. Animals as sentinels of environmental health hazards. Committee on Animals as Monitors of Environmental Hazards. [Google Scholar]
- 7.Eidson M, Schmit K, Hagiwara Y, Anand M, Backenson PB, Gotham I, et al. Dead crow density and West Nile virus monitoring, New York. [cited 2006 Apr 5];Emerg Infect Dis. 2005 11:1370–5. doi: 10.3201/eid1109.040712. Also available from: URL: http://www.cdc.gov/ncidod/EID/vol11no09/04-0712.htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rabinowitz P, Gordon Z, Chudnov D, Wilcox M, Odofon L, Liu A, et al. Animals as sentinels of bioterrorism agents. Emerg Infect Dis. 2006;12:647–52. doi: 10.3201/eid1204.051120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Veterinary Medical Association. U.S. pet ownership and demographics sourcebook. 2002. [cited 2008 Jan 10]. Available from: URL: http://www.avma.org/reference/marketstats/ownership.asp.
- 10.The Center for Food Security and Public Health. Iowa State University. Bioterrorism awareness: protection of human and animal health—companion animal veterinarians [Google Scholar]
- 11.Vourc'h G, Bridges VE, Gibbens J, De Groot BD, McIntyre L, Poland R, et al. Detecting emerging diseases in farm animals through clinical observations. Emerg Infect Dis. 2006;12:204–10. doi: 10.3201/eid1202.050498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Friend M, McLean RG. The role of native birds and other wildlife on the emergence of zoonotic diseases. In: Burroughs T, Knobler S, Lederberg J, editors. The emergence of zoonotic diseases: understanding the impact on animal and human health—workshop summary. Institute of Medicine Workshop Summary; 2000 Jun 7–8. Washington: National Academy Press; 2002. [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention (US) Bioterrorism overview: bioterrorism agent categories. [cited 2007 Feb 20]. Available from: URL: http://www.bt.cdc.gov/bioterrorism/overview.asp.
- 14.Morrison G. Zoonotic infections from pets. [cited 2006 Jan 19];Postgrad Med. 2001 110 doi: 10.3810/pgm.2001.07.970. Also available from: URL: http://www.postgradmed.com/issues/2001/07_01/morrison.htm. [DOI] [PubMed] [Google Scholar]
- 15.Govorkova EA, Rehg JE, Krauss S, Yen HL, Guan Y, Peiris M, et al. Lethality to ferrets of H5N1 influenza virus isolated from humans and poultry in 2004. J Virol. 2005;79:2191–8. doi: 10.1128/JVI.79.4.2191-2198.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zahner SJ. Local public health system partnerships. Public Health Rep. 2005;120:76–83. doi: 10.1177/003335490512000113. [DOI] [PMC free article] [PubMed] [Google Scholar]