SYNOPSIS
Objective
We identified the risk factors associated with the anthrax outbreak of 2005 in animals in North Dakota.
Methods
Medical records of the 2005 anthrax outbreak were obtained from the Veterinary Diagnostic Laboratory at North Dakota State University. Additional data were obtained from the North Dakota state veterinarian's office, and supplemental questionnaires were administered to producers. The data obtained included ecological and environmental factors, animal health factors, and management factors.
Results
Anthrax occurred from July 1 to October 12, 2005. The cases were located in eastern North Dakota around the Red River Basin. Ransom, LaMoure, and Barnes counties reported most cases (71%). Species affected included cattle, bison, horses, sheep, elk, deer, pigs, and llamas. The predominant symptom was sudden death (38%) followed by bleeding from orifices (17%). Chi-square analysis indicated significant differences between case and control premises on the following variables: death reported on neighboring pasture, vaccination period, dry conditions, wet conditions, antibiotic use, multiple vaccination, and type of predator (coyote). Factors that significantly (p<0.05) predicted anthrax occurrences on the final logistic regression model were vaccination, use of antibiotics during an outbreak, and period of vaccine administration (before or during the outbreak).
Conclusion
The characteristics of the anthrax outbreak regarding time and place of occurrence, animals affected, clinical signs reported, and mortality rate were consistent with previous reports of natural anthrax outbreaks in animals. A number of factors that significantly predicted anthrax occurrence in animals in the 2005 outbreak in North Dakota were identified. This information is important in planning appropriate control and prevention measures for anthrax, including recommending the right vaccination and treatment regimens in managing future anthrax outbreaks.
Bacillus anthracis, the causative agent of anthrax, is a free-living bacterium commonly found as spores in alkaline soils.1–4 The spore is the resistant and avirulent form of the bacterium.2,3 Anthrax spores can live in the soil for several decades and still be viable when they enter a susceptible host.3–5 The ability of Bacillus anthracis to express virulent and avirulent phases in the course of its life cycle, under very different ecological conditions, is of epidemiologic importance. The bacterium produces edema and lethal toxins from a combination of three virulence factors: protective antigen, lethal factor, and edema factor.1,6–8 Virulence within the host is further enhanced by the antiphagocytic capsular antigen, which protects the bacterium from attack by the host's immune system.1,7 The toxins cause the primary clinical signs of necrosis, edema, and hemorrhage that are typically seen with infected hosts.1,6
Anthrax has a high fatality rate in herbivores and other susceptible hosts, with animal death being the final outcome in most cases.1,7,9,10 Susceptibility and high fatality has been reported in cattle, sheep, goats, horses, donkeys, pigs, and many warm-blooded domestic animals. Wildlife with high rates of disease include antelope, bison, gazelles, impalas, elephants, and hippopotami.11–13 Wild carnivores can also become infected through the consumption of dead animals infected with anthrax.11,12 However, birds have a natural resistance to the anthrax bacteria and cannot carry the bacteria to uninfected locations.12 Outbreaks of anthrax have been reported in animals after ingestion of feedstuffs containing meat and bone meal-based concentrates originating from carcasses contaminated with anthrax bacterial spores.1,10,14
The creation of a hostile environment by exhaustion of nutrients, exposure to oxygen, and death of host tissues causes the bacterium to revert to its spore form by sporulation.15,16 The spore is returned to the soil with the burial, decomposition, or rupture of the host carcass, where it can be picked up by other animals feeding in the same spot. The avirulent phase can last for many years.3,17,18 When soil conditions are favorable, the spores migrate through capillary action of soil water to the soil surface.3,18 Spores of Bacillus anthracis have a high buoyant density, which provides an opportunity for them to adhere to vegetation as the vegetation resurfaces during evaporation.3 In enzootic areas, animals grazing close to each other on fresh shoots of grass after high rainfall will often lead to outbreaks. These conditions favor disease occurrence because bacteria ingestion from contaminated soils and leaf blades is facilitated.3,19
Though the principal mode of transmission is ingestion of infective microorganisms, biting flies have been reported to transmit the disease from one animal to another. However, this mode of transmission plays a minor role in outbreaks. Nonbiting blowflies contaminate vegetation by depositing vomit droplets after feeding on carcasses infected with Bacillus anthracis. Animals feeding on such vegetation therefore have a higher chance of becoming infected. Another identified form of transmission is mechanical transmission by blood-feeding insects. A study by Turell and Knudson confirmed this mode when they showed that blood-feeding insects could mechanically transmit anthrax.17
Agricultural regions with inadequate veterinary public health facilities have the most reported occurrence of anthrax.1,12,20 The incidence of anthrax is unknown in many countries, but it is assumed that the bacteria is present in most regions.12,18 The frequency of anthrax outbreaks in the U.S. is decreasing, even though records indicate incidence rates of the disease in animals and humans vary across the country.1 Outbreaks in the U.S. are generally considered to be sporadic in nature, though there are pockets of areas that are considered enzootic. It is also possible that the incidence of anthrax in enzootic areas peaks because of the ability to capture and report more cases as compared with the past. Areas considered enzootic in the U.S. include the states of North Dakota, Minnesota, South Dakota, and Texas. Other states that have reported outbreaks include Nebraska, Arkansas, Louisiana, and California. These are also areas with substantial livestock agricultural activity.1,13,14,21
North Dakota reported a large anthrax outbreak in 2005, which was considered the largest epizootic in the state to date. Animal health experts in the state believe the actual number of animal fatalities in 2005 easily reached the high hundreds. Environmental factors, seasonal patterns, and ecological conditions in North Dakota make it ideal for potential anthrax outbreaks. Additionally, exposure and frequent contact with the soil during open-pasture grazing increases the likelihood of infection and outbreaks.
We conducted a retrospective case-control study to identify risk factors associated with the anthrax outbreak of 2005 in animals in North Dakota. This information will be useful and indispensable in determining management and prevention strategies for future anthrax outbreaks.
METHODS
Case definition
For purposes of this study, we defined a positive or case premise as a location that housed animals meeting either the suspect, probable, or confirmed case definition of anthrax as defined hereafter. A confirmed case premise was one in which anthrax had been confirmed in the animals by clinical signs and appropriate laboratory tests. A probable case premise was one in which the animal showed classical clinical signs of anthrax, with no laboratory confirmation and/or history of positive case. A suspect case premise was one in which the animals showed clinical signs of anthrax with no laboratory confirmation. We defined a negative premise (control) as a premise in which the animals showed no clinical signs of anthrax, and/or had a negative laboratory diagnosis from a sample sent within 48 hours of animal death, and/or had never reported a case of anthrax in the past. A previous history of a positive anthrax case on the premise was included in our case premise definition because North Dakota is an enzootic state to the bacteria. This implies that there is a favorable probability of an animal dying from anthrax as indicated by a previous death.
Data sources
Data for this study were derived from three sources. Data for affected animals were retrieved in part from records for 2005 that were obtained from the North Dakota State University Veterinary Diagnostic Laboratory (VDL). Diagnostic samples consisting mainly of blood from respective premises were forwarded by local veterinarians. Blood collection was performed following guidelines outlined by the VDL and using specialized kits for sample collection. Diagnosis of anthrax from samples submitted to the VDL was performed by VDL staff. This ensured biases associated with diagnosis were minimized. Other sources of data included a producer survey conducted by the North Dakota state veterinarian's office. Additional data were obtained from a supplemental survey mailed to animal producers in the state between the months of May and August of 2006.
Laboratory procedures
Specimens (whole blood, serum) from animals showing clinical signs and suspected of having anthrax were submitted to the VDL. A laboratory culture was used to detect Bacillus anthracis infections following a standard procedure.6 Additional confirmatory diagnosis of anthrax cases was by polymerase chain reaction (PCR) using the University of Nebraska, Veterinary Diagnostic Center standard operating procedures manual for Bacillus anthracis PCR, and North Dakota State University VDL standard operating procedures manual for Bacillus anthracis PCR, both of which follow a published protocol for identification and characterization of Bacillus anthracis by multiplex PCR.6
Data analysis
Descriptive statistics of animal premises were computed using SAS.22 Characteristics of animals and premises that tested positive and negative to anthrax were compared using Chi-square tests of independence. Logistic regression analysis was run using SAS to identify premise characteristics that could significantly predict anthrax occurrence. The stepwise selection procedure was applied to select the best predictive variables to be included in the final logistic regression model.23 An assessment of goodness-of-fit statistic was conducted and the stability of the parameter estimates in the model was calculated. A parameter estimate with a value of p≤0.05 was considered significant for the model.
We set disease outcome status as either a positive premise (case) or a negative premise (control) to represent the dependent variable in the model. We also used several binary and multiple outcome variables as independent variables. These variables included: herd size (herd size greater than herd mean, and herd size less than herd mean), county of origin, vaccination time (before outbreak vs. during outbreak), vaccination history (no vaccination, one vaccination, two vaccinations, three vaccinations), vaccination and antibiotic use (with antibiotics vs. without antibiotics), pasture type (native long, other), pasture growth (short, other), unusual weather (yes vs. no), relative precipitation (dry, wet), standing water (present vs. absent), access to flowing water (yes vs. no), pasture water source (stock dam, creek, piped-in water, dug out, well, other), soil disturbance (yes vs. no), predators (present vs. absent), predator type (coyote vs. others), date put on pasture, time of death (first and last deaths on premise), antibiotic used (yes vs. no), disposal method (burned, buried, burned/buried, not burned/buried), biting flies (present vs. absent), closeness to burial site (yes vs. no), unknown carcass (present vs. absent), animal movement during period of outbreak (moved on or moved off premise), and animal species.
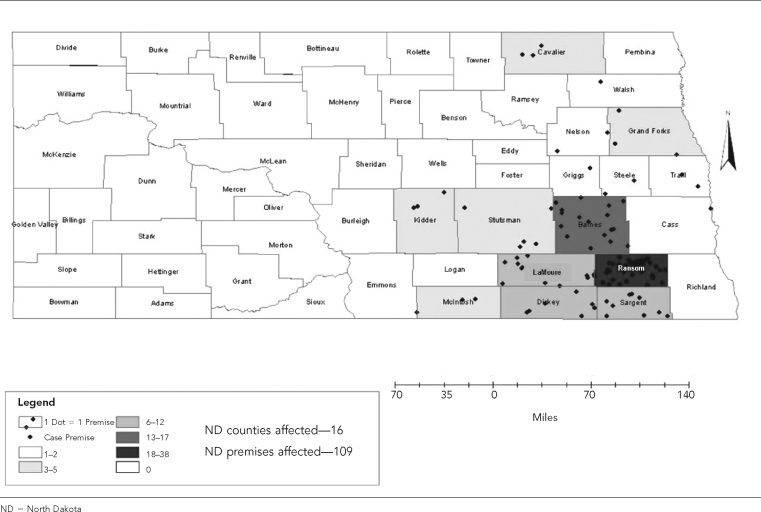
Geographic information system (GIS) was used to show the spatial distribution of case premises involved in the study. The large surface extent of the study area and other restrictions made visiting each premise difficult. The GIS technique of geocoding was employed to identify each location. Geocoding uses location information from street addresses of premises and converts these to longitudinal and latitudinal coordinates, which appear as specific points. These geocoded points were then superimposed on administrative and thematic map layers.
RESULTS
A detailed description of characteristics of the premises and animals affected with anthrax during the 2005 outbreak in North Dakota has been reported.24 Briefly, the outbreak involved 109 case premises spread over 16 counties. Geographically, the case premises were located in eastern North Dakota around the Red River of the North Basin. The counties affected are shown in the Figure, with most cases (71%) clustered around Ransom and LaMoure counties. The anthrax outbreak occurred from July 1 to October 12, 2005, with 243 positive cases. The peak period with most positive cases was the week of July 21 to July 27, with 48 positive cases. North Dakota was in the midst of a much wider regional outbreak, as anthrax was diagnosed in adjacent counties in Minnesota, South Dakota, and the province of Manitoba in Canada.
Figure.
Counties and number of premises affected by the Anthrax outbreak, 2005
A total of 576 specimens were sent to the VDL during the outbreak, and 243 (42%) were confirmed positive for anthrax. Species of animals affected were herbivores grazing on pastures and included: cattle (183, 75.0%), bison (32, 13.0%), horses (11, 5.0%), elk (11, 5.0%), sheep (5, 2.0%), and deer (1, 0.6%). The first cases reported were from bison bulls on pasture followed by cattle. The predominant clinical sign was sudden death (38%) followed by bleeding from orifices (17%). Other clinical signs included bloating and swelling, ataxia, recumbency, and edema. A total of 419 surveys were sent out by mail to producers in the state. This figure included the 109 premises with laboratory-diagnosed positive cases, and the 130 premises with negative laboratory diagnosis for anthrax. One hundred thirty-seven responses (33%) were returned. Fifty-two respondents were from premises with cases, and 85 respondents were from premises with no reported cases, giving a 1:1.6 ratio for case:control.
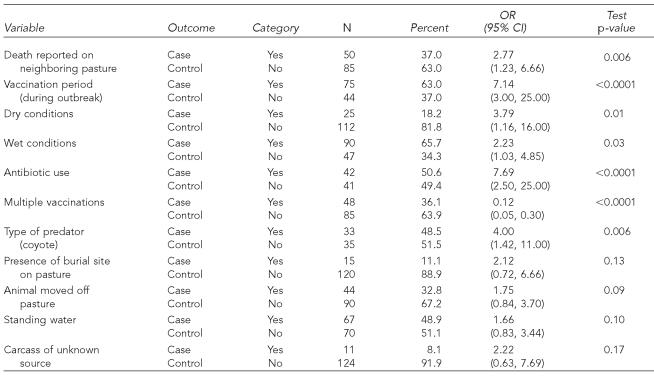
The Chi-square test results showed a number of factors that were significantly associated with anthrax occurrence (Table). These included presence of other deaths in nearby premises, the period producers were vaccinated, the number of times the animals were vaccinated, the concurrent use of antibiotics for treatment with vaccination, the presence of distinct very dry and wet conditions, and the type of predator reported on the pasture. The final logistic regression model retained three of the independent variables: vaccination, period of vaccine administration (before or during the outbreak), and the use of antibiotics with vaccination.
Table.
Chi-square comparison of case and control premises surveyed by select variables during the 2005 anthrax outbreak
OR = odds ratio
CI = confidence interval
Specifically, premises that vaccinated their animals more than one time a year were more likely to be protected case premises, as compared with premises that vaccinated only one time (odds ratio [OR] = 0.12, 95% confidence interval [CI] 0.05, 0.30, p<0.0001). Also, premises that vaccinated during the outbreak period instead of before were seven times more likely to be positive premises than those premises that initiated vaccination before the outbreak period (OR=7.14, 95% CI 3, 25, p<0.0001). Premises that reported using antibiotics along with vaccination were almost eight times more likely to be anthrax-positive premises as compared with those that did not use the antibiotic combination (OR=7.69, 95% CI 2.5, 25.0, p<0.0001). Premises that reported an animal death on a neighboring pasture were almost three times more likely to be positive-case premises as compared with premises that did not report an animal death on a neighboring pasture (OR=2.77, 95% CI 1.23, 6.66, p<0.006).
Premises that reported the presence of predators (coyotes) on their pasture were four times more likely to be positive case premises as compared with premises that did not report predators on their pasture (OR=4, 95% CI 1.42, 11.00, p<0.006). Premises that reported a distinct dry condition on their pasture were almost four times more likely to be positive case premises as compared with premises that did not report a distinct dry condition (OR=3.79, 95% CI 1.16, 16.00, p<0.01). Finally, premises that reported a distinct wet condition on their pasture were two times more likely to be positive case premises as compared with premises that did not report a distinct wet condition (OR=2.23, 95% CI 1.03, 4.85, p<0.03). The model had a concordance of 62.6% with a Hosmer and Lemeshow goodness-of-fit test statistic of 0.90 (p>0.05).
DISCUSSION
The anthrax outbreak of 2005 had similar characteristics to previous outbreaks in the state of North Dakota and elsewhere in the U.S. The reported clinical signs, type of species affected, and temporal and spatial distribution fit well with a classical outbreak. The endemic nature of the disease makes it an important veterinary threat not only to domesticated animals, but also to wildlife in the state. We used factors with plausible associations to the occurrence of the disease to identify significant factors. These factors, which influenced the outcome of the disease in the state, were broadly grouped into ecological and environmental factors, animal health factors, and management factors.
Results from the Chi-square test and logistic regression analyses indicated that vaccination was a very significant factor in predicting anthrax occurrence. The Sterne vaccine is the recommended vaccine against anthrax in the state. This is a live vaccine of the attenuated Sterne strain of the Bacillus anthracis bacterium. The vaccine has proven effective in protecting animals against the disease. Immunity derived from the use of this vaccine typically lasts for about six months to a little less than one year. The manufacturer of this vaccine recommends at least an annual vaccination for effectiveness to be achieved.25 Additionally, for the vaccine to be effective, the manufacturer recommends that each animal must be vaccinated at least twice, within two to three weeks of the first dose, to strengthen immunity in endemic areas. Our results suggested that a single dose of vaccination was not sufficient to elicit and maintain protective immunity from anthrax during the outbreak period. This is an indication that a second booster should be given during the outbreak period to protect animals during the next outbreak period.
Furthermore, our results indicated premises that vaccinated during the outbreak period were seven times more likely to be positive premises than premises that initiated vaccination before the outbreak period. Anthrax outbreaks are common between the months of June and September in North Dakota and several other places in the U.S. Ideally, animals should be vaccinated at least a month before the outbreak period; that is, preferably in the month of May. Immunity to the bacteria typically sets in within 10 days to two weeks after vaccination. Booster doses are applied during the course of the outbreak to maintain protective immunity at very high levels. Most producers vaccinated their animals during the outbreak, specifically after a first case of anthrax death occurred on their premises or neighboring premises. It is very possible that the lack of a case on the premises, the lack of a case on the neighboring premises, the time, costs, and other priority activities on the premises may have influenced the producers' decision to vaccinate.
Use of antibiotics along with vaccination was a significant predictor of anthrax occurrence. Antibiotics are recommended in the literature as treatment for the anthrax disease both in humans and animals.26 The antibiotics used during the 2005 anthrax outbreak were penicillin and tetracycline, with penicillin being the antibiotic of choice among producers sampled. However, there are concerns that an antagonistic effect exists between the vaccine and any antibiotics administered during the immunogenic period.26,27 Also, increasing antibiotic resistance is another problem that needs more research focus for antibiotics used in treating anthrax. It has also been conclusively shown that antibiotic therapy during anthrax infection has prevented the development of an immune response in some animals. This study indicated that although the antibiotic treatment was effective, the risk of recurring disease persisted because of the possibility of delayed germination of spores.27 The results from our study, however, highlight the antagonistic effects associated with timing the use of antibiotics as treatment in joint use with the vaccine against anthrax.
Death of an animal on a neighboring premise was a significant predictor of anthrax occurrence on a premise. Producers that reported an anthrax death occurrence on a neighboring premise were almost three times more likely to be anthrax-positive premises, as compared with producers that reported there were no anthrax deaths on neighboring premises. This factor, though difficult to interpret within our anthrax occurrence context, became more plausible when we examined the presence of predators around the premises.
Producers that reported the presence of predators, specifically coyotes, were four times more likely to be anthrax-positive premises as compared with those that did not report the presence of predators. It is possible that predators played a role in disseminating anthrax infection to neighboring premises. Studies have shown that predators can be an effective and important means by which the anthrax bacteria are spread in the environment. Dragon et al. studied the natural dissemination of anthrax spores and found that scavengers were very effective at releasing and spreading contaminated fluids and viscera around the immediate area of the carcass.19 This was achieved mainly through adherence of the bacteria to fur and feathers, or by dragging tissues to other locations. This contributed heavily to the spread of spores beyond the carcass location. They also suggested that dissemination by intestinal carriage and fecal deposition was important in spore spread over wide areas. The authors also included water runoff from carcass sites as a major source of anthrax spores, though the extent of movement and the gradient needed were unknown. It is possible that the movement of predators from one premise to another transfers and spreads anthrax spores. This activity also makes the bacteria readily available for susceptible animals to ingest.
Environmental and ecological conditions play an important role in anthrax outbreaks.10,11,19 In our study, the presence of very wet conditions prior to the outbreak and dry conditions during the outbreak significantly predicted anthrax occurrence. This cycle of wet and dry conditions has been identified in several studies as a common requirement for an outbreak.3 Producers that reported very wet conditions were more likely to be anthrax-positive premises as compared with those that did not report very wet conditions. Producers that also reported very dry conditions were more likely to be anthrax-positive premises as compared with those that did not report very dry conditions.
The mean precipitation during the period was 3.05 inches with a median of 2.50 inches. Before the outbreak, the period between mid-May and June recorded a mean of about 7.10 inches of precipitation. Between the end of June and July, when most cases were reported, the region recorded a mean of just 1.90 inches of precipitation. The precipitation pattern agrees with the reported wet and dry weather phases needed for an outbreak to occur. It also indicates that weather conditions do play a significant role in anthrax outbreaks.
Results from the logistic regression analysis indicated that vaccination, period of vaccination, and the use of antibiotics with vaccination were the three variables that best predicted anthrax occurrence. Prevention by vaccination is vital to protect susceptible animals and to stop huge losses from animal deaths. A comparison between the 2005 outbreak period with a few animals vaccinated and the 2006 period, when most producers properly vaccinated, supports the contributory role of vaccination. For effective control and prevention, the vaccine must be administered before the outbreak season, and vaccination should be administered preferably a month before the season. This increases the likelihood that the animals will develop protective immunity against the bacteria before infection sets. Booster doses of the vaccine are recommended and should be administered in the course of the outbreak to keep immunity high.25
Producers that administered antibiotics during the outbreak did not report any adverse effects from their use. Antibiotics such as penicillin and tetracycline are effective against anthrax, and the use of antibiotics has been identified as an important control strategy in other studies; thus, it should be considered. However, our model suggests that the joint application of both vaccination and antibiotics is not effective. And more studies on the effects of administering the vaccine and antibiotics together need to be conducted.
CONCLUSION
The characteristics of the anthrax outbreak regarding time and place of occurrence, animals affected, clinical signs reported, and mortality rate were consistent with previous reports of natural anthrax outbreaks in animals. Some risk factors that significantly predicted anthrax occurrence in animals in the 2005 outbreak in North Dakota were identified. These included the period the vaccine was administered, wet weather conditions, dry weather conditions, the joint use of antibiotics and vaccination to treat animals, the number of times the animals were vaccinated, reported animal death on a neighboring pasture, and the presence and type of predator roaming around the premises. Vaccination status, period of vaccine administration (before or during the outbreak), and use of antibiotics with vaccination during an outbreak were the variables that predicted anthrax occurrence. This is an indication that following the right vaccination and treatment strategies is beneficial in managing the outbreak. These data are useful in determining and mapping out future policy, research, and control strategies for anthrax in animals.
Acknowledgments
The authors thank the North Dakota State Veterinarians Office, veterinarians, county agents, and producers in North Dakota for participating in the study, and Mathew Theis, Great Plains Institute of Food Safety, North Dakota State University, Fargo, North Dakota, as well as Dr. Sara Friedrich, Hovland Veterinary Clinic, Lisbon, North Dakota, for assisting with data collection.
Footnotes
Funding was provided by a grant from the North Dakota State Board of Agricultural Research and Education.
REFERENCES
- 1.Murray PR, Pfaller MA, Rosenthal KS. Medical microbiology. 5th ed. Philadelphia: Mosby; 2005. [Google Scholar]
- 2.Ryu C, Lee K, Seong WK, Oh HB. Sensitive and rapid quantitative detection of anthrax spores isolated from soil samples by real-time PCR. Microbiol Immunol. 2003;47:693–9. doi: 10.1111/j.1348-0421.2003.tb03434.x. [DOI] [PubMed] [Google Scholar]
- 3.Dragon DC, Rennie RP. The ecology of anthrax spores: tough but not invincible. Can Vet J. 1995;36:295–301. [PMC free article] [PubMed] [Google Scholar]
- 4.Ryan KJ, Ray CG, editors. Sherris medical microbiology. 4th ed. New York: McGraw Hill; 2004. [Google Scholar]
- 5.World Health Organization. Guidelines for the surveillance and control of anthrax in humans and animals. 1998. [cited 2007 Feb 14]. Available from: URL: http://www.who.int/csr/resources/publications/anthrax/WHO_EMC_ZDI_98_6/en.
- 6.Ramisse V, Patra G, Garrigue H, Guesdon JL, Mock M. Identification and characterization of Bacillus anthracis by multiplex PCR analysis of sequences on plasmids pX01 and pX02 and chromosomal DNA. FEMS Microbiol Let. 1996;145:9–16. doi: 10.1111/j.1574-6968.1996.tb08548.x. [DOI] [PubMed] [Google Scholar]
- 7.Hanna PC, Ireland JA. Understanding Bacillus anthracis pathogenesis. Trends Microbiol. 1999;7:180–2. doi: 10.1016/s0966-842x(99)01507-3. [DOI] [PubMed] [Google Scholar]
- 8.The virulence of cultivated anthrax virus. Science. 1884;4:276–7. doi: 10.1126/science.ns-4.85.276. [DOI] [PubMed] [Google Scholar]
- 9.Bales ME, Dannenberg AL, Brachman PS, Kaufmann AF, Klatsky PC, Ashford DA. Epidemiologic response to anthrax outbreaks: field investigations, 1950–2001. Emerg Infect Dis. 2002;8:1163–74. doi: 10.3201/eid0810.020223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.U.S. Department of Agriculture: Animal and Plant Health Inspection Service, Veterinary Services, Centers for Epidemiology and Animal Health, Center for Emerging Issues (US) Epizootiology and ecology of anthrax. [cited 2007 Feb 14]. Available from: URL: http://www.aphis.usda.gov/vs/ceah/cei/taf/emerginganimalhealthissues_files/anthrax.text.pdf.
- 11.Lindeque PM, Turnbull PC. Ecology and epidemiology of anthrax in Etosha National Park, Namibia. Onderstepoort J Vet Res. 1994;61:71–83. [PubMed] [Google Scholar]
- 12.Food and Agriculture Organization of the United Nations, Agriculture and Consumer Protection Department. Anthrax in animals. [cited 2007 Feb 14]. Available from: URL: http://www.fao.org/ag/magazine/0112sp.htm.
- 13.Human anthrax associated with an epizootic among livestock—North Dakota, 2000. MMWR Morb Mortal Wkly Rep. 2001;50(32):677–80. [PubMed] [Google Scholar]
- 14.Human ingestion of Bacillus anthracis-contaminated meat—Minnesota, August 2000. JAMA. 2000;284:1644–6. [PubMed] [Google Scholar]
- 15.Titball RW, Turnbull PC, Hutson RA. The monitoring and detection of Bacillus anthracis in the environment. Soc Appl Bacteriol Symp Ser. 1991;20:S9–S18. [PubMed] [Google Scholar]
- 16.Turnbull PC, Lindeque PM, Le Roux J, Bennett AM, Parks SR. Airborne movement of anthrax spores from carcass sites in the Etosha National Park, Namibia. J Appl Microbiol. 1998;84:667–76. doi: 10.1046/j.1365-2672.1998.00394.x. [DOI] [PubMed] [Google Scholar]
- 17.Turell MJ, Knudson GB. Mechanical transmission of Bacillus anthracis by stable flies (Stomoxys calcitrans) and mosquitoes (Aedes aegypti and Aedes taeniorhynchus) Infect Immun. 1987;55:1859–61. doi: 10.1128/iai.55.8.1859-1861.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Friedlander AM. Microbiology: tackling anthrax. Nature. 2001;414:160–1. doi: 10.1038/35102660. [DOI] [PubMed] [Google Scholar]
- 19.Dragon DC, Bader DE, Mitchell J, Wollen N. Natural dissemination of Bacillus anthracis spores in northern Canada. Appl Environ Microbiol. 2005;71:1610–5. doi: 10.1128/AEM.71.3.1610-1615.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Madigan M, Martinko J. Brock biology of microorganisms. 11th ed. Carbondale (IL): Prentice Hall; 2005. [Google Scholar]
- 21.Inglesby TV, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Friedlander AM, et al. Anthrax as a biological weapon: medical and public health management. JAMA. 1999;281:1735–45. doi: 10.1001/jama.281.18.1735. [DOI] [PubMed] [Google Scholar]
- 22.SAS Institute Inc. SAS: Version 8. Cary (NC): SAS Institute Inc.; 1999. [Google Scholar]
- 23.Hosmer DW, Lemeshow S. Applied logistic regression. 2nd ed. New York: John Wiley – Sons; 2000. [Google Scholar]
- 24.Ndiva Mongoh M, Dyer NW, Stoltenow CL, Khaitsa ML. Characterization of an outbreak of anthrax in animals in North Dakota: 243 cases. Bov Pract. 2007;41:101–9. [Google Scholar]
- 25.North Dakota State University, Extension Service. Stoltenow CL, Hammer CJ, editors. Anthrax. V-561 (revised) 2006 Mar [Google Scholar]
- 26.Inglesby TV, O'Toole T, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, et al. Anthrax as a biological weapon, 2002: updated recommendations for management. JAMA. 2002;287:2236–52. doi: 10.1001/jama.287.17.2236. [DOI] [PubMed] [Google Scholar]
- 27.Friedlander AM, Welkos SL, Pitt ML, Ezzell JW, Worsham PH, Rose KJ, et al. Postexposure prophylaxis against experimental inhalation anthrax. J Infect Dis. 1993;167:1239–43. doi: 10.1093/infdis/167.5.1239. [DOI] [PubMed] [Google Scholar]