Abstract
Aims
Assessment of bronchodilator pharmacology in chronic obstructive pulmonary disease (COPD) may be improved by using more sensitive methods than spirometry, such as impulse oscillometry (IOS) and body plethysmography. We sought to compare salmeterol (S) and tiotropium (Tio) using these methods.
Methods
In this double-blind, randomized, four-way crossover study, 32 COPD patients received single doses of Tio (18 µg), S (50 and 100 µg) or placebo. Specific airway conductance (sGaw), forced expiratory volume in 1 s (FEV1) and IOS were measured pre- and up to 26 h postdose. Comparisons between treatments were analysed by weighted means (WM) between 0 and 12 (WM 0–12 h) and 12–24 h (WM 12–24 h) postdose. Data are expressed as mean difference (or geometric ratio for nonparametric data) with 95% confidence intervals.
Results
Tio and S100 significantly improved FEV1, sGaw and IOS parameters up to 26 h and S50 up to 16 h. WM analysis showed no difference between Tio and S100 in FEV1 for 0–12 h or 12–24 h. Maximum mid-expiratory flow (−0.06; −0.11, −0.01) and R35 (0.02; 0.01, 0.03) demonstrated superiority of S100 compared with Tio for WM 0–12 h sGaw (1.12; 1.02, 1.23), R5 (−0.06; −0.09, −0.02), R15 (−0.03; −0.05, −0.01), and resonant frequency (RF) (−2.30; −3.83, −0.77) showed superiority of Tio compared with S100 for WM 12–24 h. At 26 h, sGaw, R5, R15, X5 and RF also showed superiority of Tio compared with S100.
Conclusions
sGaw and IOS parameters sensitively differentiated between the effects of Tio and S when FEV1 measurements were similar. Clinical trials in patients with COPD should use IOS and sGaw to assess comprehensively bronchodilator pharmacology.
What is already known about this subject
Forced expiratory voume in 1 s (FEV1) is the standard measurement used to measure drug effects in chronic obstructive pulmonary disease (COPD) clinical trials.
Having previously shown that specific airway conductance (sGaw) measured using body plethysmography and impulse oscillometry (IOS) are more sensitive than FEV1 for assessing short-acting bronchodilator effects in patients with COPD, we conducted the first randomized, placebo-controlled study to compare long-acting bronchodilators in COPD patients using these techniques.
What this study adds
sGaw and IOS sensitively differentiated between the effects of tiotropium and salmeterol when FEV1 measurements were similar.
sGaw and IOS measurements are better than FEV1 for sensitively assessing bronchodilator pharmacology and differentiating between treatments in COPD clinical trials.
Keywords: body plethysmography, COPD, impulse oscillometry, long-acting bronchodilators
Introduction
Long-acting bronchodilators are widely used in the treatment of chronic obstructive pulmonary disease (COPD). Long-acting β agonists (e.g. salmeterol and formoterol) are usually taken twice daily, whereas the anticholinergic tiotropium is used once a day. These bronchodilators improve lung function and have beneficial effects on clinical end-points such as symptoms and exacerbation rates [1, 2].
The measurement of bronchodilation in COPD patients is usually by the spirometric measurement of forced expiratory volume in 1 s (FEV1), which has been extensively used, is easy to perform and reproducible. Importantly, in clinical trials it is a measurement required by drug regulatory authorities. However FEV1 is often insensitive to physiologically important changes in lung mechanics, such as those caused by a decrease in hyperinflation [3]. Consequently, it is recognized that patients may derive therapeutic benefits from bronchodilator therapies despite little change in FEV1. Understanding the therapeutic effects of bronchodilator treatments in COPD therefore requires a more comprehensive assessment of pulmonary function than spirometry alone, such as the additional measurement of lung volumes [4].
The lung function measurements of body plethysmography and the forced oscillation technique (FOT) are able to detect bronchodilator effects sensitively in patients with airflow obstruction, and it has been shown that these techniques are more sensitive than FEV1 for assessing short-acting bronchodilator effects in patients with COPD [5, 6]. The body plethysmograph is an enclosed constant-volume chamber in which volume and pressure changes resulting from expansion and compression of the lungs are used to calculate airway resistance and conductance and lung volumes. Oscillometry involves the application of small pressure oscillations at the mouth during spontaneous breathing to obtain a measure of respiratory impedance. Respiratory impedance (Z) is the ratio of pressure to flow and is composed of two components; resistance (R) and reactance (X) Multiple frequencies can be supplied as a continuous mixture of several sinusoidal waveforms by a programmed pseudorandom noise as used in FOT, or by rapidly recurring rectangular waveform impulses as used in impulse oscillometry (IOS). Body plethysmography and IOS have a practical advantage, as they both use tidal breathing, thus avoiding the possibility of bronchoconstriction during forced expiration in patients with airflow obstruction [7].
The magnitude and duration of effect of single doses of long-acting bronchodilators are usually assessed by FEV1. As FEV1 is a relatively insensitive measurement in COPD, we hypothesized that other pulmonary function measurements would provide a more sensitive assessment of long-acting bronchodilator pharmacology. Previous comparisons of body plethysmography, FOT and spirometry have not been performed in blinded, placebo-controlled clinical trials in patients with COPD [5, 6, 8]. We have therefore compared the effects of single doses of salmeterol and tiotropium in COPD patients over 26 h, using spirometry, IOS and body plethysmography with a placebo-controlled, double-blind, crossover study design. The aim of the study was to compare the ability of these pulmonary function methods to provide sensitive measurements of bronchodilator pharmacology in a clinical trial setting. The aim was to use the results to guide the choice of pulmonary function methodology for future clinical trials of novel bronchodilator drugs in COPD.
Methods
Thirty-two patients with moderate to severe COPD diagnosed according to Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria were recruited [9]. All patients were current or ex-smokers with at least a 10 pack year history. Inclusion criteria were postbronchodilator FEV1 40–80% predicted, FEV1/forced vital capacity (FVC) ratio <70%, and increase in FEV1 of ≥7% and ≥150 ml, 30 min after 80 µg of ipratropium bromide administered via dry powder inhaler. Patients were excluded from the study if they had a clinical diagnosis of asthma or if they had a respiratory tract infection within 4 weeks of the start of the study. All patients provided written informed consent and the study was approved by the South Manchester Medical Research Ethics Committee (Manchester, UK).
This was a double-blind, double-dummy, randomized, placebo-controlled, four-way crossover study performed at a single centre (Medicines Evaluation Unit, South Manchester University Hospitals NHS Trust). Patients received a single dose of tiotropium bromide 18 µg via HandiHaler™ (Tio), salmeterol 100 µg (S100) or 50 µg (S50) via Diskus™ dry powder inhaler or placebo on each of four study days separated by 10–14 days to allow adequate wash-out. Patients were given both of these inhaler devices on each study day, with at least one being placebo.
Short-acting bronchodilators were permitted during the study on an as-required basis and were withheld for 6 h before administration of study medication until 26 h post dose. Patients were required to withold tiotropium bromide for 10 days and from other long-acting inhaled bronchodilators for 72 h before administration of study medication until the end of the study. Patient adherence to non-use of medication was checked by questioning at each visit and the visit rescheduled in the event of non-adherence. Inhaled corticosteroids were allowed if the dose had been stable for at least 6 weeks prior to the study start.
Pulmonary function tests
IOS, body plethysmography and spirometry were performed predose and 2, 5, 8, 12, 16, 24 and 26 h post dose in that order, with patients having an overnight stay. All treatment period doses were scheduled between 08.00 and 10.00 h for all patients. For IOS (Masterscreen IOS; Erich Jaeger, Hoechberg, Germany) subjects supported their cheeks while impulses were applied during tidal breathing for 30 s. Respiratory resistance (R) and reactance (X) were calculated at 5–35 cycles s−1 (Hz). Resonant frequency (RF), the frequency at which reactance equals zero, was also recorded.
Specific airway conductance (sGaw), airway resistance (Raw), functional residual capacity (FRC), vital capacity (VC) and inspiratory capacity (IC) were measured in a constant volume plethysmograph (Vmax 6200; Sensormedics, Bilthoven, the Netherlands). IOS and body plethysmograph measurements were performed in triplicate. The mean FRC and IOS measurements and the highest IC and VC measurements were used for further analysis. Total lung capacity (TLC) and residual volume (RV) were then calculated from these parameters. Maximum expiratory flow volume measurements [FEV1, FVC and maximum mid-expiratory flow (MMEF)] were performed using the spirometry system on the plethysmograph. Readings were performed in triplicate, with the highest FEV1, MMEF and FVC used in further analysis.
Statistical analysis
The study sample size was based on the primary end-point of FEV1. Previous data estimated the within-subject variability of FEV1 to have a standard deviation (SD) between 0.08 and 0.21 l. A sample size of 32 subjects provided 81% power if the SD was 0.08 l, and 100% power if the SD was 0.21 l, to detect a difference of 0.15 l between treatments using a 5% two-sided significance level.
The data were analysed by serial time point analysis at 2, 5, 8, 12, 16, 24 and 26 h post dose compared with placebo. For each end-point, data were analysed by a mixed model including treatment, time, period, and a treatment by time interaction and baseline (a continuous covariate) fitted as fixed effects and subject fitted as a random effect. For comparisons between treatments, the data were principally analysed by weighted means between 0 and 12 (WM 0–12 h) and 12–24 h (WM 12–24 h) after dosing, in order to avoid issues with multiple testing at the multiple time points. Weighted means were analysed using a mixed model with baseline, period and treatment fitted as fixed effects and subject fitted as a random effect. Baseline was defined as the predose measurement for each treatment group. The Kenward and Roger method for approximating the denominator degrees of freedom and correcting for bias in the estimated variance–covariance of the fixed effects was used in the analyses.
FEV1, FVC, MMEF, IC, RV, FVC and IOS parameters were normally distributed. sGaw, Raw, FRC and TLC data were not normally distributed and were therefore analysed following natural logarithmic transformation. Normally distributed data are expressed as mean differences, whereas log transformed data are expressed as geometric ratios.
Results
Thirty-one patients completed all four treatment periods. One patient was withdrawn after the second treatment period (having received placebo and S50) due to a lower respiratory tract infection. The data from this subject are included in the statistical analysis. Baseline demographic and pulmonary function data are shown in Table 1. Patients had moderate to severe COPD with mean (SD) bronchodilator reversibility of 18% (8.9).
Table 1.
Patient demographics and baseline lung function [data are *mean (SD) or †median (range)]
| Number of patients | 32 |
| Sex M/F | 22/10 |
| Age (years) | 60.7 (8.14)* |
| Smokers (current/ex) | 13/19 |
| Pack years | 43.0 (22.4)* |
| Number on inhaled corticosteroids | 17 |
| Pre-bronchodilator FEV1 (l) | 1.60 (0.36)* |
| Pre-bronchodilator FEV1 (% predicted) | 54.1 (9.3)* |
| FEV1 reversibility after 80 µg ipratropium bromide (%) | 18.0 (8.94)* |
| FVC (l) | 3.05 (0.65)* |
| MMEF (l s−1) | 0.70 (0.27)* |
| FEV1/FVC | 0.53 (0.08)* |
| sGaw (kPa s−1) | 0.48 (0.23–1.01)† |
| Raw (kPa l−1 s−1) | 0.45 (0.27–0.75)† |
| RV (l) | 3.77 (1.06)* |
| RV (% predicted) | 167.6 (44.2)* |
| IC (l) | 2.48 (0.55)* |
| FRC (l) | 4.17 (2.20–7.22)† |
| TLC (l) | 7.07 (4.28–9.63)† |
| TLC (% predicted) | 109.4 (18.8)* |
| R5 (kPa l−1 s−1) | 0.67 (0.23)* |
| R20 (kPa l−1 s−1) | 0.41 (0.10)* |
| X5 (kPa l−1 s−1) | −0.33 (0.19)* |
| RF (Hz) | 26.10 (7.23)* |
FEV 1, Forced expiratory volume in 1 s; FVC, forced vital capacity; MMEF, maximum mid-expiratory flow; sGaw, specific airway conductance; Raw; RV, residual volume; IC, inspiratory capacity; FRC, functional residual capacity; TLC, total lung capacity; R, resistance; X, reactance; RF, resonant frequency.
Comparisons of active treatments vs. placebo (Figures 1–4)
Figure 1.
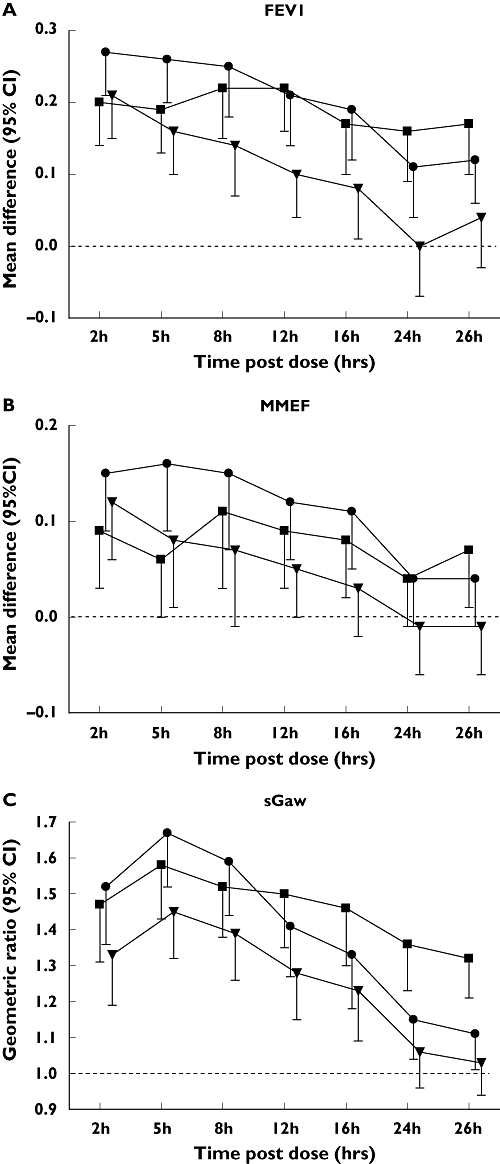
Active treatment vs. placebo (P) comparisons for (A) forced expiratory volume in 1 s (FEV1), (B) maximum mid-expiratory flow (MMEF) and (C) specific airway conductance (sGaw). Data for FEV1 and MMEF are mean difference [95% confidence intervals(CI)], data for sGaw are geometric mean ratio (one-sided 95% CIs shown). Tio vs P, (▪); S100 vs P, (•); S50 vs P, (▾)
Tio and S100 significantly improved FEV1, sGaw, R5, RF and X5 at all time points up to 26 h (Figures 1, 3 and 4). The duration of effect of S50 on these measurements was only 16 h (Figures 1, 3 and 4). IOS resistance measurements at higher frequencies showed a shorter duration of action for all treatments (Figure 3c). Tio significantly improved MMEF at all time points up to 26 h except 5 and 24 h, whereas S100 and S50 caused significant improvements up to 16 and 5 h, respectively (Figure 1b).
Figure 3.
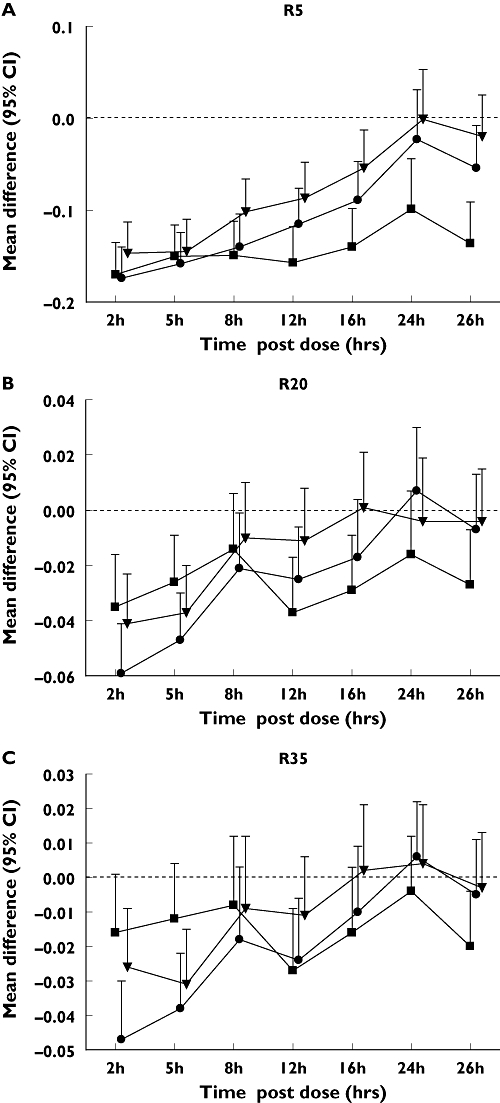
Active treatment vs. placebo (P) comparisons for (A) resistance (R) 5, (B) R20 and (C) R35. Data are mean difference (one-sided 95% confidence intervals shown). Tio vs P, (▪); S100 vs P (•); S50 vs P (▾)
Figure 4.
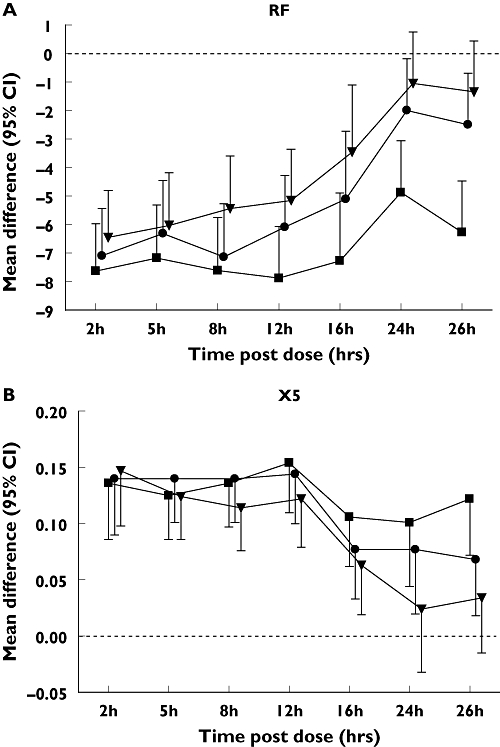
Active treatment vs. placebo (P) comparisons for (A) resonant frequency (RF) and (B) reactance (X) 5. Data are mean difference (one-sided 95% confidence intervals shown). Tio vs P, (▪); S100 vs P (•); S50 vs P (▾)
Tio significantly improved RV and IC at all time points up to 26 h and FRC up to 16 h (Figure 2). S100 significantly improved RV up to 24 h and IC and FRC up to 16 h (Figure 2). S50 significantly improved IC up to 16 h and RV and FRC up to 12 h (Figure 2). For TLC there were no statistically significant differences in any of the treatment comparisons against placebo at any time point (data not shown).
Figure 2.
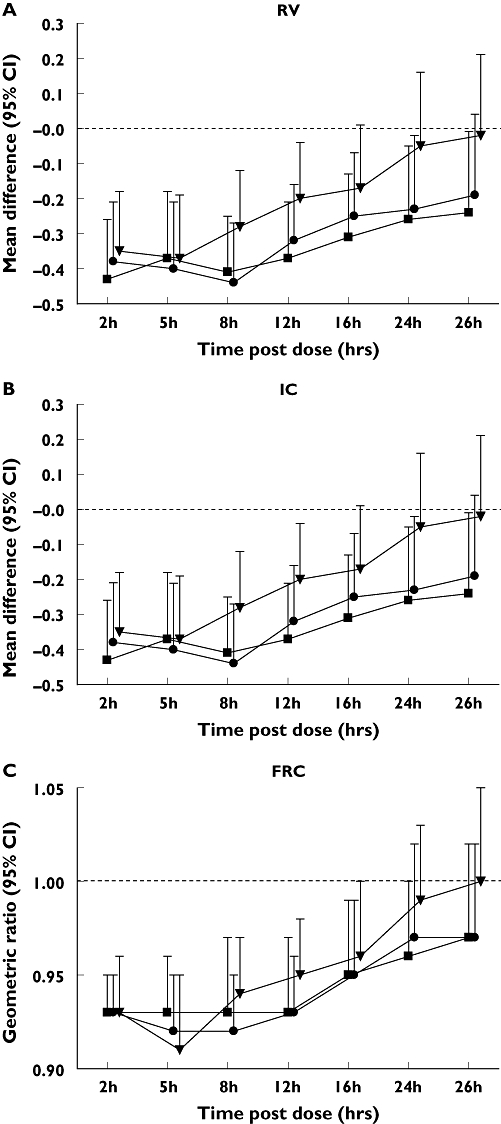
Active treatment vs. placebo (P) comparisons for (A) residual volume (RV), (B) functional residual capacity (FRC) and (C) inspiratory capacity (IC). Data for RV and IC forced expiratory volume in 1 s mean difference [95% confidence intervals (CI)], data for FRC are geometric mean ratio (one-sided 95% CIs shown). Tio vs P, (▪); S100 vs P (•); S50 vs P (▾)
Active treatment comparisons
Tiotropium bromide 18 µg vs. salmeterol 100 µg (Table 2a,b)
Table 2a.
Weighted means (WM 0–12 h) for active treatment comparisons
| Tio vs. S100 | Tio vs. S50 | S100 vs. S50 | |
|---|---|---|---|
| FEV1‡ | −0.04 (−0.09, 0.01) | 0.05 (−0.001, 0.09) | 0.09 (0.04, 0.13)* |
| MMEF‡ | −0.06 (−0.11, −0.01)† | 0.01 (−0.05, 0.06) | 0.07 (0.02, 0.12)* |
| sGaw§ | 0.96 (0.89, 1.04) | 1.10 (1.02, 1.19)* | 1.14 (1.06, 1.23)* |
| RV‡ | −0.01 (−0.14, 0.12) | −0.08 (−0.21, 0.04) | −0.08 (−0.20, 0.05) |
| R5‡ | −0.01 (−0.03, 0.02) | −0.03 (−0.05, −0.01)* | −0.02 (−0.05, −0.001)* |
| R15‡ | 0.004 (−0.01, 0.02) | −0.01 (−0.02, 0.003) | −0.02 (−0.03, −0.001)* |
| R20‡ | 0.01 (0.00, 0.02) | −0.001 (−0.01, 0.01) | −0.01 (−0.02, −0.001)* |
| R25‡ | 0.01 (−0.01, 0.02) | −0.01 (−0.02, 0.004) | −0.02 (−0.03, −0.003)* |
| R35‡ | 0.02 (0.01, 0.03)† | 0.004 (−0.01, 0.02) | −0.01 (−0.02, −0.001)* |
| RF‡ | −0.79 (−1.99, 0.41) | −1.64 (−2.83, −0.45)* | −0.85 (−2.04, 0.34) |
| X5‡ | −0.01 (−0.04, 0.03) | 0.01 (−0.02, 0.04) | 0.01 (−0.02, 0.05) |
Tio, Tiotropium bromide 18 µg; S100, salmeterol 100 µg; S50, salmeterol 50 µg. Data are
mean difference (95% confidence intervals) or
geometric mean (95% confidence intervals).
Superiority of Tio over S100, Tio over S50 or S100 over S50.
Superiority of S100 over T. Data for TLC, FRC and IC are not shown as no significant differences seen.
FEV1, Forced expiratory volume in 1 s; MMEF, maximum mid-expiratory flow; sGaw, specific airway conductance; RV, residual volume; R, resistance; X, reactance.
Table 2b.
Weighted means (WM 12–24 h) for active treatment comparisons
| Tio vs. S100 | Tio vs. S50 | S100 vs. S50 | |
|---|---|---|---|
| FEV1† | 0.01 (−0.05, 0.06) | 0.12 (0.06, 0.17)* | 0.11 (0.06, 0.17)* |
| MMEF† | −0.02 (−0.07, 0.03) | 0.05 (−0.001, 0.09) | 0.07 (0.02, 0.11)* |
| sGaw‡ | 1.12 (1.02, 1.23)* | 1.23 (1.12, 1.34)* | 1.10 (1.00, 1.20)* |
| RV† | −0.04 (−0.20, 0.12) | −0.17 (−0.33, −0.02)* | −0.13 (−0.29, 0.02) |
| R5† | −0.06 (−0.09, −0.02)* | −0.09 (−0.12, −0.05)* | −0.03 (−0.06, 0.01) |
| R15† | −0.03 (−0.05, −0.01)* | −0.04 (−0.07, −0.02)* | −0.01 (−0.04, 0.01) |
| R20† | −0.02 (−0.03, 0.001) | −0.02 (−0.04, −0.01)* | −0.01 (−0.03, 0.01) |
| R25† | −0.02 (−0.03, 0.002) | −0.03 (−0.05, −0.02)* | −0.02 (−0.03, 0.00) |
| R35† | −0.01 (−0.02, 0.01) | −0.02 (−0.03, −0.002)* | −0.01 (−0.02, 0.01) |
| RF† | −2.30 (−3.83, −0.77)* | −3.64 (−5.16, −2.11)* | −1.33 (−2.86, 0.19) |
| X5† | 0.03 (−0.01, 0.06) | 0.06 (0.02, 0.09)* | 0.03 (−0.003, 0.06) |
Tio, Tiotropium bromide 18 µg; S100, salmeterol 100 µg; S50, salmeterol 50 µg. Data are
mean difference (95% confidence intervals) or
geometric mean (95% confidence intervals).
Superiority of Tio over S100, Tio over S50 or S100 over S50. Data for static lung volumes are not shown as no significant differences seen. FEV1, Forced expiratory volume in 1 s; MMEF, maximum mid-expiratory flow; sGaw, specific airway conductance; RV, residual volume; R, resistance; X, reactance.
MMEF and R35 demonstrated superiority of S100 compared with Tio for WM 0–12 h (Table 2a). There was also some evidence for superiority of S100 over Tio for FEV1 at 2 h and 5 h [mean difference −0.07 (95% confidence interval −0.13, −0.01 for both time points)], although there was no difference for WM 0–12 h.
WM 12–24 h showed superiority of Tio compared with S100 for sGaw, R5, R15 and RF (Table 2b). At 26 h, sGaw (1.19; 1.09, 1.31), R5 (−0.08; −0.13, −0.04), R15 (−0.04; −0.06, −0.01), X5 (0.05; 0.004, 0.10) and RF (−3.78; −5.59, −1.96) demonstrated superiority of Tio compared with S100.
Tiotropium bromide 18 µg vs. salmeterol 50 µg (Table 2a,b)
Weighted means analysis showed superiority of Tio compared with S50 at 0–12 h for sGaw, R5 and RF, and at 12–24 h for FEV1, sGaw, R5–R35, RF, X5 and RV.
Salmeterol 100 µg vs. salmeterol 50 µg (Table 2a,b)
Weighted means analysis showed superiority of S100 compared with S50 at 0–12 h for FEV1, MMEF, sGaw and R5–R35, and at 12–24 h for FEV1, MMEF and sGaw.
Discussion
This is the first randomized, placebo-controlled study to compare long-acting bronchodilator drugs in COPD patients using a comprehensive range of techniques that measure forced expired volumes, static volumes, airway conductance, pulmonary resistance and pulmonary reactance. Our main findings were that FEV1 showed the effects of Tio and S100 to be very similar over 26 h, and superior to S50. However, MMEF and R35 showed some evidence of superiority of S100 over Tio within the first 12 h post dose, whereas sGaw, R5, R15 and RF demonstrated superiority of Tio over S100 from 12 to 26 h. The pharmacological differences between Tio and S100 were demonstrated by body plethysmography and IOS, whereas measurement of FEV1 revealed no difference. Clinical trials in COPD that rely on FEV1 measurements alone may lack sensitivity to define differences between inhaled drugs accurately.
Comparing the active treatments against placebo, FEV1, sGaw, R5, RF and X5 all showed that the duration of action of Tio and S100 were 26 h, whereas the duration of S50 was shorter at 16 h. Any changes in other lung function measurements were of shorter duration than those observed for FEV1. This suggests that sGaw, R5, RF and X5 are measuring physiologically relevant changes in pulmonary function that are closely associated with changes in FEV1. Our previous study has also shown that sGaw, R5 and IOS compliance measurements are the most sensitive assessments of bronchodilator effects in COPD patients [5].
There was some evidence from MMEF and R35 measurements of a benefit in favour of S100 over Tio from 0 to 12 h, and individual FEV1 time point analysis suggested this benefit was within 5 h post dose. FEV1 and high-frequency IOS resistance measurements are representative of changes in large airway tone [10], and these findings suggest that S100 has a greater effect at early time points on the large airways. In contrast, S50 demonstrated no superiority over Tio. This indicates that any bronchodilator superiority of salmeterol compared with Tio during the first 12 h post dose is a dose-related phenomenon, occurring only with the S100 dose. The dose–response effect of salmeterol was further confirmed by the longer duration of action of S100 compared with S50.
After 12 h post dose, sGaw, R5, R15, RF and X5 provided evidence for a superior effect of Tio over S100, even while FEV1 measurements were similar. There is some evidence that changes in RF and X5 reflect peripheral bronchodilation [11, 12] and that sGaw measurements are also indicative of small airway tone [13]. It is possible that the differences between Tio and S100 were due to a prolonged effect of Tio on the small airways. The lack of ability of FEV1 to differentiate between the two treatments after 12 h further underscores our previous findings that using FEV1 alone may not provide a comprehensive evaluation of the effects of drugs, and that sGaw and IOS provide additional sensitive assessments of physiologically relevant parameters [5].
The differences observed between the treatments may be explained by differences between the degree of peripheral vs. central deposition of the bronchodilators studied, and the location and activity within the bronchial tree of the specific receptors targeted. The findings may also be attributed to differences in drug distribution following inhalation from the different delivery devices.
MMEF was not a robust method for differentiating between treatments, consistent with results from our previous COPD study [5]. The lack of improvement of MMEF in COPD studies may be explained by the fact that as the FVC improves, MMEF shifts along the flow volume loop and may even decline. It is possible to correct MMEF for changes in FVC [14], although this is not routinely performed.
We have shown that higher frequency resistance measurements did not demonstrate bronchodilation with the sensitivity demonstrated by the lower frequency measurements. This is consistent with results from our previous COPD study [5]. Previous studies in asthma patients have also shown that R20 is less sensitive than R5 [15, 16]. IOS measurements in COPD patients demonstrate frequency dependence of resistance, i.e. the resistance at low frequencies is raised to a greater extent than that at high frequencies [16]. This may explain why low-frequency resistance measurements show more significant improvement in COPD. However, studies in healthy volunteers have shown similar changes across the range of frequencies between R5 and R25 [15–17]. This may reflect changes in large airways seen in healthy volunteers without associated change in peripheral airway resistance.
In the current study, IOS reactance measurements (RF and X5) were able to demonstrate significant bronchodilation, with RF being the most sensitive for differentiating between treatments. This is similar to our previous findings using IOS to assess bronchodilation in COPD patients [5]. The improvements in RF and X5 in this study may be due to a reduction of expiratory flow limitation [18], and/or improvements in respiratory compliance and peripheral bronchodilation [11, 12]. Together with the changes observed in R5 in the current study, it appears that IOS through R5 and RF allows for sensitive assessment of bronchodilator effects in COPD.
It has been previously shown that many COPD patients show significant improvements in static lung volumes after administration of a bronchodilator despite little change in FEV1[3]. In our previous COPD study it was shown that both IC an RV improved significantly after high doses of salbutamol in a group of patients with hyperinflation, as evidenced by increased RV [5]. In the current study, RV, IC and FRC significantly improved, although the results were less consistent than those of sGaw, FEV1 and IOS. In contrast, TLC showed no significant improvement in any of the active vs. placebo comparisons. Patients in this study were not preselected for hyperinflation and had a mean RV of 168% predicted, but a relatively normal mean TLC. The current data suggest that lung volume measurements in reversible patients do not add any further information to distinguish between long-acting bronchodilators.
The current study preselected patients according to FEV1 reversibility, to allow the drug treatments to be compared using different techniques. It is recognized that reversibility to bronchodilators in COPD varies over time and according to the bronchodilator used [19, 20]. Subjects were included who responded to a short-acting anticholinergic, and we recognize that a different population may have been selected if β agonist-responsive patients had been included.
Care was taken in this study to exclude patients with a previous diagnosis of asthma. All the patients included had symptoms and lung function compatible with COPD as defined by the GOLD guidelines. However, COPD patients with reversibility to ipratopium were not recruited; the mean reversibility was 18% expressed as a change from baseline, or 9% expressed as a percentage of predicted. Our patients therefore had ‘poorly reversible airflow obstruction’ in keeping with the GOLD definition [9], as the mean FEV1 improved from 54% to only 63% predicted after the inhalation of ipratopium.
Clinical trials in COPD have previously included only patients exhibiting FEV1 reversibility in order to maximize the chance of observing bronchodilator drug effects [21]. It should be noted that the level of reversibility observed in this study is compatible with published data regarding bronchodilator reversibility in COPD patients. In a study of >1000 COPD patients, a post-bronchodilator increase in FEV1 of ≥15% compared with baseline was observed in >80% of patients [20]. In another large study, the mean change in FEV1 post bronchodilator was 15% expressed as a change from baseline or 5% when expressed as percentage of predicted [22]. Further studies are required to determine whether our results are also applicable to a less reversible group of COPD patients. This would also allow assessment of whether changes in body plethysmography and IOS can be seen in patients with little change in FEV1.
There are practical factors to consider when determining the optimum lung function tests for use in clinical trials. Spirometry is easy to perform, but is effort dependent and the deep inspiration required can lead to changes in bronchomotor tone. Plethysmography requires only tidal breathing, but is more complex to perform for both operator and subject. Practically, IOS is a simpler procedure for measuring respiratory resistance and has the advantage of measuring resistance over a range of frequencies, as well as measuring respiratory reactance.
FEV1 is currently the standard measurement used in COPD clinical trials. However, we have shown that sGaw and IOS measurements can differentiate between the effects of tiotropium and salmeterol when FEV1 measurements are similar. The pharmacology of bronchodilators in COPD can be more fully understood by using a range of pulmonary function measurements. Inclusion of effort-independent IOS end-points and sGaw in clinical trials may help in the comprehensive assessment of bronchodilator pharmacology in COPD patients.
Acknowledgments
The authors thank Stephanie Lasenby and Nigel Dallow for statistical analysis and Angus Henderson for study operational support. This work was funded by GlaxoSmithKline (GSK Study ACH100539).
References
- 1.Mahler DA, Donohue JF, Barbee RA, Goldman MD, Gross NJ, Wisniewski ME, Yancey SW, Zakes BA, Rickard KA, Anderson WH. Efficacy of salmeterol xinafoate in the treatment of COPD. Chest. 1999;115:957–65. doi: 10.1378/chest.115.4.957. [DOI] [PubMed] [Google Scholar]
- 2.Vincken W, van Noord JA, Greefhorst AP, Bantje TA, Kesten S, Korducki L, Cornelissen PJ. Dutch/Belgian Tiotropium Study Group. Improved health outcomes in patients with COPD during 1 yr's treatment with tiotropium. Eur Respir J. 2002;19:209–16. doi: 10.1183/09031936.02.00238702. [DOI] [PubMed] [Google Scholar]
- 3.Newton MF, O'Donnell DE, Forkert L. Response of lung volumes to inhaled salbutamol in a large population of patients with severe hyperinflation. Chest. 2002;121:1042–50. doi: 10.1378/chest.121.4.1042. [DOI] [PubMed] [Google Scholar]
- 4.Celli B, ZuWallack R, Wang S, Kesten S. Improvement in resting inspiratory capacity and hyperinflation with tiotropium in COPD patients with increased static lung volumes. Chest. 2003;124:1743–8. doi: 10.1378/chest.124.5.1743. [DOI] [PubMed] [Google Scholar]
- 5.Borrill ZL, Houghton CM, Woodcock AA, Vestbo J, Singh SD. Measuring bronchodilation in COPD clinical trials. Br J Clin Pharmacol. 2005;59:379–94. doi: 10.1111/j.1365-2125.2004.02261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Noord JA, Smeets J, Clement J, van de Woestijne KP, Demedts M. Assessment of reversibility of airflow obstruction. Am J Respir Crit Care Med. 1994;150:551–4. doi: 10.1164/ajrccm.150.2.8049845. [DOI] [PubMed] [Google Scholar]
- 7.Burns GP, Gibson GJ. A novel hypothesis to explain the bronchoconstrictor effect of deep inspiration in asthma. Thorax. 2002;57:116–9. doi: 10.1136/thorax.57.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh D, Tal-Singer R, Faiferman I, Lasenby S, Henderson A, Wessels D, Goosen A, Dallow N, Vessey R, Goldman M. Plethysmography and impulse oscillometry assessment of tiotropium and ipratropium bromide; a randomized, double-blind, placebo-controlled, cross-over study in healthy subjects. Br J Clin Pharmacol. 2006;61:398–404. doi: 10.1111/j.1365-2125.2006.02594.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2006. [1 June 2006]. Available at http://www.goldcopd.org.
- 10.Kjeldgaard JM, Hyde RW, Speers DM, Reichert WW. Frequency dependence of total respiratory resistance in early airway disease. Am Rev Respir Dis. 1976;114:501–8. doi: 10.1164/arrd.1976.114.3.501. [DOI] [PubMed] [Google Scholar]
- 11.Bouaziz N, Beyaert C, Gauthier R, Monin P, Peslin R, Marchal F. Respiratory system reactance as an indicator of the intrathoracic airway response to methacholine in children. Pediatr Pulmonol. 1996;22:7–13. doi: 10.1002/(SICI)1099-0496(199607)22:1<7::AID-PPUL2>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 12.Kaczka DW, Ingenito EP, Israel E, Lutchen KR. Airway and lung tissue mechanics in asthma. Effects of albuterol. Am J Respir Crit Care Med. 1999;159:169–78. doi: 10.1164/ajrccm.159.1.9709109. [DOI] [PubMed] [Google Scholar]
- 13.Bassiri AG, Girgis RE, Doyle RL, Theodore M. Detection of small airway dysfunction using specific airway conductance. Chest. 1997;111:1533–5. doi: 10.1378/chest.111.6.1533. [DOI] [PubMed] [Google Scholar]
- 14.Cockcroft DW, Berscheid BA. Volume adjustment of maximal midexpiratory flow. Importance of changes in total lung capacity. Chest. 1980;78:595–600. doi: 10.1378/chest.78.4.595. [DOI] [PubMed] [Google Scholar]
- 15.Houghton CM, Woodcock AA, Singh D. A comparison of lung function measurements for assessing dose–response effects of salbutamol. Br J Clin Pharmacol. 2004;58:134–41. doi: 10.1111/j.1365-2125.2004.02105.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Houghton CM, Woodcock AA, Singh D. A comparison of plethysmography, spirometry and oscillometry for assessing the pulmonary effects of inhaled ipratropium bromide in healthy subjects and patients with asthma. Br J Clin Pharmacol. 2005;59:152–9. doi: 10.1111/j.1365-2125.2004.02262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kjeldgaard JM, Hyde RW, Speers DM, Reichert WW. Frequency dependence of total respiratory resistance in early airways disease. Am Rev Resp Dis. 1976;114:501–8. doi: 10.1164/arrd.1976.114.3.501. [DOI] [PubMed] [Google Scholar]
- 18.Dellaca RL, Santus P, Aliverti Z, Stevenson N, Centanni S, Macklem PT, Pedotti A, Calverley PMA. Detection of expiratory flow limitation in COPD using the forced oscillation technique. Eur Respir J. 2004;23:232–40. doi: 10.1183/09031936.04.00046804. [DOI] [PubMed] [Google Scholar]
- 19.Calverley PM, Burge PS, Spencer S, Anderson JA, Jones PW. Bronchodilator reversibility testing in chronic obstructive pulmonary disease. Thorax. 2003;58:659–64. doi: 10.1136/thorax.58.8.659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dorinsky PM, Reisner C, Ferguson GT, Menjoge SS, Serby CW, Witek TJ. The combination of ipratropium and albuterol optimizes pulmonary function reversibility testing in patients with COPD. Chest. 1999;115:966–71. doi: 10.1378/chest.115.4.966. [DOI] [PubMed] [Google Scholar]
- 21.Maesen FP, Smeets JJ, Sledsens TJ, Wald FD, Cornelissen PJ. Tiotropium bromide, a new long-acting antimuscarinic bronchodilator: a pharmacodynamic study in patients with chronic obstructive pulmonary disease (COPD). Dutch Study Group. Eur Respir J. 1995;8:1506–13. [PubMed] [Google Scholar]
- 22.Anthonisen NR, Wright EC. Bronchodilator response in chronic obstructive pulmonary disease. Am Rev Respir Dis. 1986;133:814–9. [PubMed] [Google Scholar]


