Abstract
Objective
To assess the effects of reducing television viewing and computer use on children’s body mass index (BMI) as a risk factor for the development of overweight in young children.
Design
Randomized controlled clinical trial.
Setting
University children’s hospital.
Participants
Seventy children aged 4 to 7 years whose BMI was at or above the 75th BMI percentile for age and sex.
Interventions
Children were randomized to an intervention to reduce their television viewing and computer use by 50% vs a monitoring control group that did not reduce television viewing or computer use.
Main Outcome Measures
Age- and sex-standardized BMI (zBMI), television viewing, energy intake, and physical activity were monitored every 6 months during 2 years.
Results
Children randomized to the intervention group showed greater reductions in targeted sedentary behavior (P < .001), zBMI (P < .05), and energy intake (P < .05) compared with the monitoring control group. Socioeconomic status moderated zBMI change (P = .01), with the experimental intervention working better among families of low socioeconomic status. Changes in targeted sedentary behavior mediated changes in zBMI (P < .05). The change in television viewing was related to the change in energy intake (P < .001) but not to the change in physical activity (P = .37).
Conclusions
Reducing television viewing and computer use may have an important role in preventing obesity and in lowering BMI in young children, and these changes may be related more to changes in energy intake than to changes in physical activity.
Trial Registration
clinical trials.gov Identifier: NCT00065052
Television viewing is cross-sectionally and prospectively related to obesity in children.1,2 There is limited research assessing the effect of reducing television viewing on the development of obesity.3–5 School-based interventions have shown that reducing television viewing in third- and fourth-grade students slowed the increase in body mass index (BMI) (calculated as weight in kilograms divided by height in meters squared)3 and that reduction in television viewing was related to success of a multicomponent obesity prevention program.4 Reducing television viewing in preschool children was associated with a reduction in parent-reported television viewing, but no changes in BMI were observed.5 Little research has involved children aged 4 to 7 years as they transition into their early school years.
For editorial comment see page 283
Reducing sedentary behavior could affect body weight by modifying energy intake or energy expenditure in several ways. Television viewing is related to consumption of fast food6 and foods and beverages that are advertised on television.7 Viewing cartoons with embedded food commercials can increase choice of the advertised item in preschoolers,8 and television commercials may prompt eating.9–11 Television viewing or related sedentary behavior may prompt eating by the association of these behaviors with eating, and television viewing and related behavior may impair the development of satiety by interfering with habituation to gustatory and olfactory cues.12–15 Reducing television viewing decreased energy and fat intake in lean adolescents.16 Television viewing and related sedentary behavior can compete with physical activity, lowering energy expenditure.11,17,18 When sedentary behavior is reduced, children may choose to engage in other sedentary behavior or to reallocate time to be more physically active,19–22 although the reallocation depends on child characteristics.23
The primary objective of this study was to determine the effects of reducing television viewing and computer use on age- and sex-standardized BMI (zBMI) changes in a sample of children aged 4 to 7 years who were at or above the 75th BMI percentile. Because BMI is positively associated with chronic disease risk factors in children24 and because childhood BMI predicts adult BMI,25 these young at-risk children are an appropriate target group for prevention programs. Secondary aims were to assess the effects of television viewing on energy intake and on energy expenditure. The study was approved by the Social and Behavioral Sciences Institutional Review Board at the State University of New York at Buffalo.
METHODS
PARTICIPANTS
Families were recruited through newspaper advertisements, flyers, and direct mailings targeting families with children aged 4 to 7 years. Inclusion criteria were a child aged 4 to 7 years at or above the 75th BMI percentile for age and sex,26 participation in at least 14 hours of television viewing and computer game playing per week in the primary household, no medical conditions that prevented or interfered with regular physical activity, unlimited access to television or television-related sedentary activities, and family agreement to have television monitoring devices (TV Allowance; Mindmaster Inc, Miami, Florida) attached to every television and computer monitor in the home for the duration of the study.
PROCEDURES
After completing a telephone screen, families attended an orientation, and, if interested, parents read and signed the informed consent and then completed a questionnaire that assessed the numbers of televisions, television video game units, VCR and DVD players, and computers in the home. Approximately 1 week later, a TV Allowance was attached to each television and computer monitor in the home by a research assistant (D.D.W. or J.H.F.), who recorded the numbers of televisions and computers and their locations in the home. The TV Allowance is an automated device that controls and monitors the use of televisions or computer monitors, including television, video game systems, DVD players, VCRs, and computers. The appliance was plugged into the TV Allowance, the plug was locked in, and the device was plugged into the wall. To turn on the television or computer monitor, each family member used an individually selected 4-digit code. To protect against the participating child watching television or playing a computer game on other family members’ time, the participating child was not informed of the codes of other family members. If the child learned the codes of another family member, these codes were changed. The TV Allowance sums the minutes of use for each code to objectively determine use of that device.
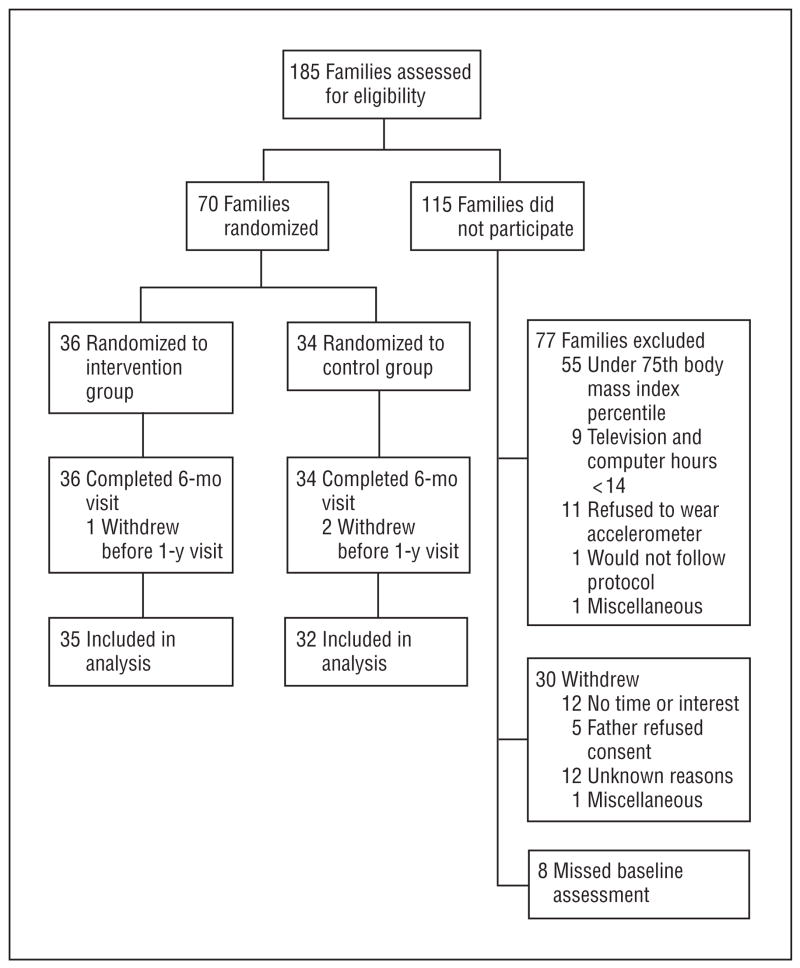
Baseline television and computer use was measured during a 3-week period. Seventy families met eligibility criteria and were randomized into intervention and control groups (Figure 1). Families were recruited in cohorts, were stratified by child sex, and were randomized by the study statistician (R.A.P.) in blocks of 2 without replacement using a random number generator limited to 2 numbers. Group assignments were provided to the project coordinator (J.L.R.).
Figure 1.
Overview of study flow.
Study staff (D.D.W. and J.H.F.) set the weekly time budgets for television viewing, computer use, and associated behaviors. Budgets were reduced by 10% of their baseline amount per month for children in the intervention group until the budget was reduced by 50%. When the budget was reached, the television or computer monitor could not be turned on for the remainder of the week. Study staff could set different amounts of time for each child in a household, if desired, to reduce conflict if another child was not on the program. Parents and non-participating family members could use their code to watch television or to use computers without being on a budget.
Children in the intervention group earned $0.25 for each half hour under budget,upto$2.00 per week .Parents were instructed to praise the participating child for reducing television viewing and for engaging in alternative behaviors. Decreases were also re-inforced by a star chart. At each home visit, a study staff member reviewed the star chart and praised the child for the number of stickers earned. When the child reached the 50% decrease at 6 months, the star charts were discontinued, and changes were supported through monthly newsletters and by parent al praise for behavior change. The intervention group received ideas for alternatives to sedentary behavior, a tailored monthly newsletter with parenting tips to reduce sedentary behavior, and information about how to rearrange the home environment to reduce access to sedentary behavior. Children in the control group were provided free access to television and computers and received $2.00 per week for participating, independent of their behavior change. Control families received a newsletter to provide parenting tips, sample praise statements, and child-appropriate activities and recipes.
MEASURES
Television and computer time were measured using the TV Allowance. Body mass index was calculated based on weight measured using a digital or calibrated balance beam scale and height measured using a calibrated stadiometer. The zBMI was calculated using age- (to the nearest month) and gender-specific median, standard deviation, and power of the Box-Cox transformation (LMS method).26 Physical activity was monitored using an activity monitor (ActiGraph; ActiGraph, LLC, Pensacola, Florida), a unidirectional accelerometer validated for children.27–29 Physical activity was recorded in 1-minute epochs on 3 randomly selected weekdays from after school until bedtime and all day for 1 randomly selected weekend day. The mean counts per minute during the 4 days was the measure of physical activity. Energy intake (in kilocalories per day) was measured for the month before the assessment using a validated30 85-item food frequency questionnaire completed by the participating parent. The numbers of televisions, computers, and pieces of exercise equipment were measured by interviews with the participating parent and child, as were the characteristics of the neighborhood environment (including distance in miles to the nearest park or playground, number of activities the child engaged in per week in the neighborhood environment, and perceived safety of the neighborhood on a scale of 1 to 5 [1, unsafe; 5, very safe]). Socioeconomic status (SES) was measured using the Four Factor Index of Social Status by Hollingshead,31 which provides a continuous measure based on parental occupation and education.
DATA ANALYSIS PLAN
t Tests and χ2 tests were used to assess comparability of groups. Mixed-effects regression models (MRMs) were used to assess zBMI, television viewing, energy intake, and physical activity over time. The MRMs do not assume compound symmetry but use separate estimates of variance at each measurement, which is important because variability often increases as follow-up is extended, and MRMs use all available data.32 The models for targeted sedentary behavior, energy intake, and physical activity included group, SES, and child age and sex as time-invariant fixed effects, as well as a random intercept. Child age and sex were excluded from the zBMI model because the zBMI values were standardized for age and sex. The usual pattern of change in behavioral studies is a decrease during the initial phases of intervention, followed by maintenance of change or relapse. To capture these patterns of change, linear (months) and quadratic (months×months) interactions with group were tested. Linear and quadratic interactions with group were evaluated for improvement of fit for the overall model by 2-tailed log likelihood tests using 2 df. If adding the quadratic term did not improve the fit of the model, it was not included to test the interaction of group × months. Group × months interactions were explored by examining between-group differences from baseline to 6, 12, 18, or 24 months.
Three families moved out of state during the 2-year measurement period, so the primary analysis was based on 67 of 70 families (96%). Complete data were available for 66 of 67 families because 1 family withdrew before the 2-year follow-up, but all available data were included in the MRM analysis. The primary analysis was based on families who did not move because families who moved could not be provided with the intervention, as it required implementation of the TV Allowance and regular home monitoring. Intent-to-treat MRM analyses were also completed, including the 3 families who moved.
The MRMs were used to evaluate moderators, mediators of outcome, and nonspecific predictors.33 Moderators are baseline variables that differentially predict outcomes of the groups and were evaluated by the interaction of group × potential moderator × months (linear and quadratic models as appropriate). Potential moderators included sex, age, SES, energy intake, physical activity, baseline levels of targeted sedentary behavior, and the numbers of televisions and computers in the home and in the child’s bedroom. Moderators were chosen to represent baseline characteristics that could affect change but were not based on specific theoretical hypotheses.
Mediators are variables that differentially change between groups, and the differential change is related to change in the dependent variable. Only time-variant predictors that show between-group differences can be considered mediators, and these were tested by the interaction of group × potential mediator × months (linear and quadratic models as appropriate).
Nonspecific predictors are baseline or time variant variables that predict change in the dependent variable but do not interact with the group. Nonspecific predictors included variables assessed as moderators and mediators. The MRMs are particularly useful for studying mediators or nonspecific predictors over time because the MRM allows for time-variant (repeated) measures as independent and dependent variables.
The MRMs were used to estimate the elasticity between changes in television viewing and physical activity or energy intake. Elasticity is an economic construct that represents the relationships between proportional changes in television viewing and physical activity or energy intake. Elasticity coefficients are determined using log values in the regression models.34,35 The finding of a statistically significant positive relationship suggests that the 2 behaviors are complements. For example, energy intake would be a complement to television viewing and computer game playing if there was a statistically significant positive relationship between the change in television and computer use and energy intake. The finding of a statistically significant negative relationship suggests that the 2 behaviors are substitutes. Physical activity would be considered a substitute for watching television or playing computer games if physical activity increased in association with a reduction in television viewing and computer game playing.
Sample size estimates were based on research about the effects of reducing sedentary behavior on BMI changes.3 We estimated that with 30 subjects per group we had 80% power to detect a standardized effect size (Cohen d) of at least 0.23 at a 2-sided α level of .05 for the primary outcome variable of zBMI using a repeated-measures analysis of variance with 5 repeated measures (0, 6, 12, 18, and 24 months). Analyses were performed using commercially available software (SYSTAT 11.0; Systat Software, Inc, Richmond, California).36
RESULTS
There were no statistically significant differences in baseline characteristics among the participants (Table). Fifty-six of 70 children (80%) were above the 85th BMI percentile, and 31 of them (44%) were above the 95th BMI percentile.
Table.
Characteristics of Participants
| Characteristic | Control Group (n = 34) | Intervention Group (n = 36) |
|---|---|---|
| Age, mean (SD), y | 6.1 (1.3) | 5.8 (1.2) |
| Male to female ratio | 18:16 | 19:17 |
| BMI (SD) | 19.1 (3.5) | 19.3 (2.5) |
| Age- and sex-standardized BMI, mean (SD) | 1.51 (0.57) | 1.69 (0.58) |
| Television viewing and computer use, mean (SD), h/wk | 26.1 (10.1) | 24.2 (10.8) |
| Physical activity counts per min, mean (SD)a | 783.5 (249.1) | 757.0 (256.4) |
| Energy intake per day, mean (SD), kcal | 1562.6 (474.0) | 1551.4 (515.3) |
| Socioeconomic status, mean (SD)b | 42.0 (13.0) | 44.3 (10.6) |
| Minority race/ethnicity, No. (%)c | 9/34 (27) | 8/36 (22) |
| Home environment, No. (%) | ||
| Televisions | 2.9 (1.4) | 2.9 (1.2) |
| Computers | 1.0 (0.6) | 1.1 (0.6) |
| Pieces of home exercise equipment, mean (SD) | 1.4 (1.2) | 1.8 (1.1) |
| Neighborhood environment, mean (SD) | ||
| Blocks to nearest park or playground | 3.7 (2.8) | 3.3 (2.2) |
| Activities per wk in the neighborhood | 6.6 (3.6) | 6.4 (3.8) |
| Perceived safety on a scale of 1 (safe) to 5 (dangerous) | 3.4 (1.5) | 3.9 (1.2) |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
Based on accelerometer counts per minute.
Based on parental occupation and education.
Includes families of Hispanic, African American, Native American, and multiple races/ethnicities.
In the control group, the mean (SEM) number of hours of television viewing and computer games declined by −5.2 (11.1) hours per week at 24 months (Figure 2). In contrast, the mean (SEM) number of hours of television viewing and computer games in the intervention group declined by −17.5 (7.0) hours per week at 6 months and remained about the same through 24 months (P<.001 for group × months interaction). Statistically significant between-group differences (P<.001) were observed at 6 through 24 months.
Figure 2.
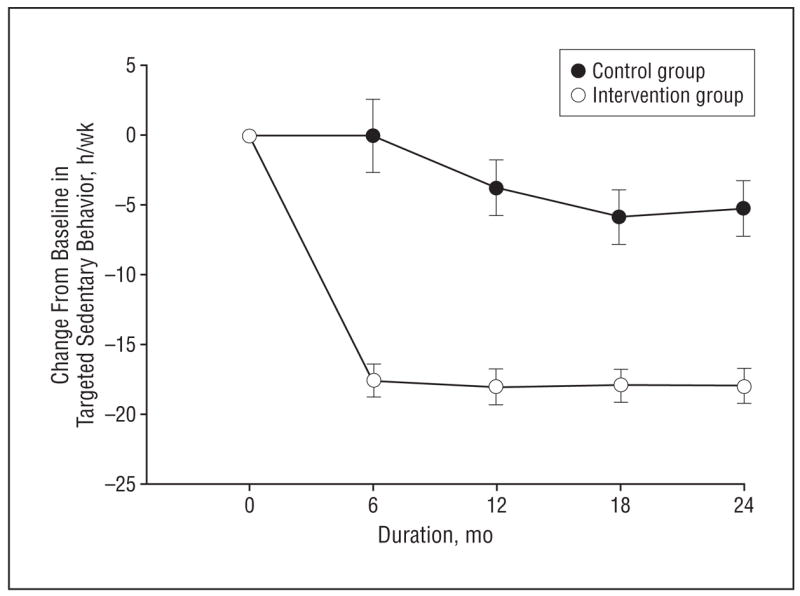
Reduction from baseline in targeted sedentary behavior (television viewing and computer use) for the intervention and control groups over time. A statistically significant difference in the rate of change by group was observed (P < .001). Data are given as mean (SEM).
A statistically significant interaction of group × months was observed for zBMI (P<.05), as zBMI decreased a mean (SEM) of −0.24 (0.32) at 24 months for the intervention group, while the control group demonstrated a mean (SEM) zBMI increase of 0.05 (0.29) at 6 months, a return to baseline at 12 months, and a gradual mean (SEM) zBMI decrease of −0.13 (0.37) at 24 months after baseline (Figure 3). Statistically significant between-group differences were observed from baseline to 6 months (P=.02) and 12 months (P=.03).
Figure 3.
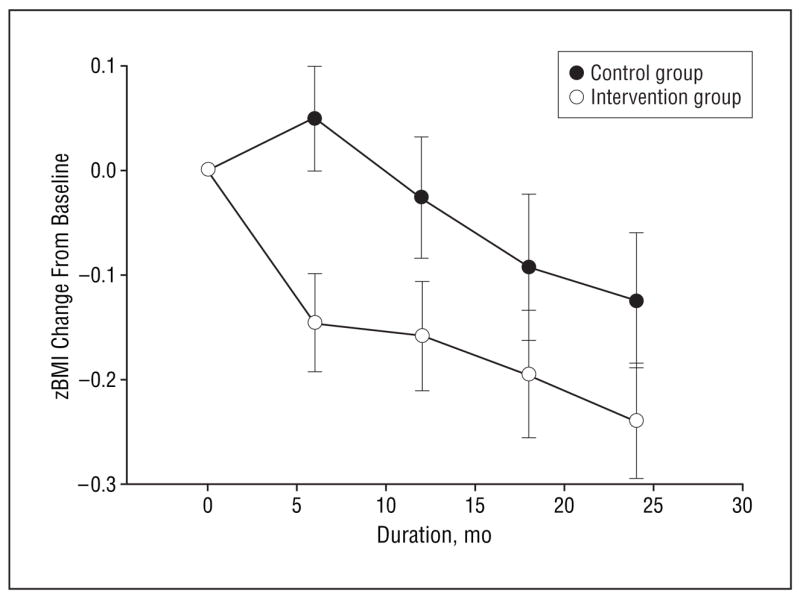
Reduction in age- and sex-standardized body mass index (zBMI) values relative to baseline for the intervention and control groups over time. A statistically significant difference in the rate of change in zBMI by group was observed (P < .05). Data are given as mean (SEM).
Energy intake data showed a greater reduction for the intervention group than for the control group (P < .05), with statistically significant between-group differences from baseline to 18 months and 24 months (P = .047) (Figure 4). No statistically significant between-group changes over time were observed for changes in physical activity, as the control group demonstrated mean (SEM) changes in physical activity counts per minute of 43.7 (302.2), 7.8 (316.9), −23.5 (262.4), and −62.7 (189.7) at 6, 12, 18, and 24 months, respectively, while the intervention group demonstrated mean (SEM) changes in physical activity counts per minute of 36.2 (381.3), 63.7 (288.8), 111.8 (603.0), and 31.4 (275.4) at the same time points, respectively.
Figure 4.
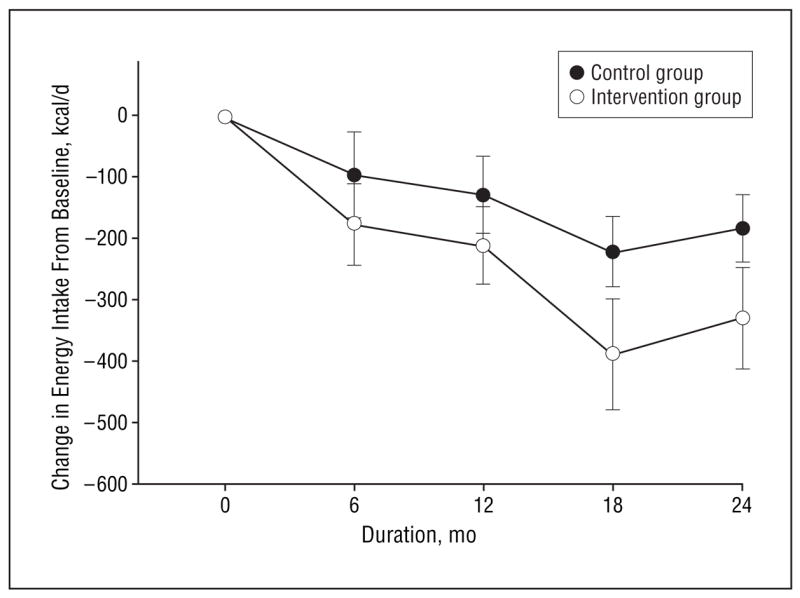
Reduction in energy intake for the intervention and control groups over time. A statistically significant difference in the rate of change in energy intake by group was observed (P < .05). Data are given as mean (SEM).
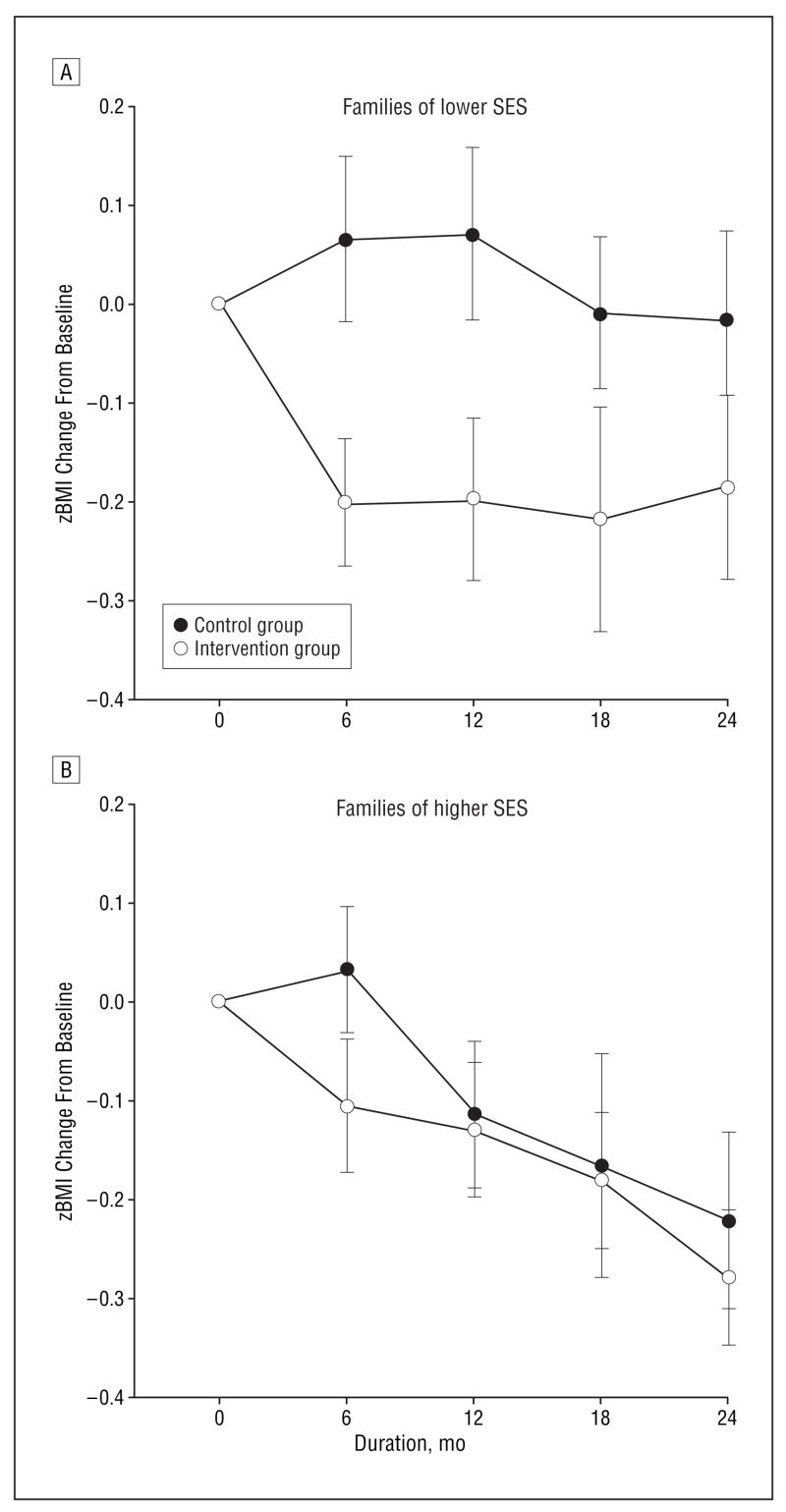
Socioeconomic status was a statistically significant moderator of zBMI change (group × SES × months; P = .01) (Figure 5). This effect was explored by dividing the sample based on SES into 2 groups at the mean SES and by examining changes in zBMI by group. For the low SES group, statistically significant between-group differences were observed from baseline to 6 months (P = .002), 12 months (P = .02), 18 months (P = .04), and 24 months (P = .05), while no statistically significant between-group differences in zBMI change were observed for the high SES group. Tele vision and computer use mediated the effect of group on zBMI values over time (group ×targeted sedentary behavior×months; P < .05). Baseline zBMI was a nonspecific predictor of zBMI change (coefficient, 0.008; P < .001), with lower zBMI baseline values associated with greater change. However, care should be used in interpreting the direction of the relationship between baseline zBMI values and zBMI change over time because of the distribution of zBMI values.37 Log changes in targeted sedentary behavior were complemented by log changes in energy intake (coefficient [SE], 0.10 [0.03]; P < .001), while physical activity was not a substitute for targeted sedentary behavior (coefficient [SE], −0.03 [0.03]; P = .37).
Figure 5.
Change in age- and sex-standardized body mass index (zBMI) values relative to baseline for the intervention and control groups over time. A statistically significant difference in the rate of change in zBMI by group for families divided into lower (A) and higher (B) socioeconomic status (SES) was observed (P = .01). Data are given as mean (SEM).
COMMENT
This randomized controlled trial showed a statistically significant and sustained reduction in television viewing and computer use that was associated with decreases in zBMI for children whose BMI was at or above the 75th percentile for age and sex. Results of the mediator analyses suggest that zBMI changes were mediated by targeted sedentary behavior changes. Our findings show that television viewing and computer use can be modified in young children using behavioral engineering technology that provides parental control over a child’s screen time budget while giving the child the opportunity to choose how to spend this budget.
The trend for zBMI in the intervention group was a gradual reduction during the 2 years of observation, while the control group demonstrated an increase followed by gradual decreases. Differential changes from baseline to 6 and 12 months were statistically significant. The largest zBMI difference between groups was −0.19 at 6 months, which decreased to −0.13, −0.10, and −0.11 at 12, 18, and 24 months, respectively. Although the changes were modest, a small effect of this simple and inexpensive intervention (approximately $100 for each TV Allowance) magnified across the population may produce important reductions in the prevalence of obesity and obesity-related comorbidities.38
The changes in zBMI were moderated by child SES, with the intervention working best for families of lower SES. Children from families of higher SES showed reductions in zBMI whether they were in the intervention group or the control group. Families of lower SES showed large and sustained zBMI differences between the intervention and control families throughout the 2 years of measurement of −.0.17, −0.20, −0.17, and −0.26 at 6, 12, 18, and 24 months, respectively. The observation that the intervention worked better for families of lower SES than of higher SES is important because children of low SES are at greater risk of becoming obese adults than children of higher SES.39,40 Perhaps families of higher SES were more aware than families of lower SES of information linking television viewing to weight in children, and perhaps families of higher SES had the familial resources and parenting skills needed to modify television viewing without use of the TV Allowance. No differences in family characteristics between groups of lower SES vs higher SES were found, including no differences in the breakdown among families of minority races/ethnicities in the lower (22.6%) and higher (22.2%) SES groups. Future re search should explore differences between SES groups that may mediate these effects.
Changes in energy intake, but not changes in physical activity, were differentially related to changes in the targeted sedentary behavior. Reducing television viewing could affect energy intake by minimizing cues to eat and by decreasing exposure to television advertising.6–11 Patterns of change in energy intake16 and physical activity23 were consistent with findings of experimental research in which targeted sedentary behavior was modified in older children. If the intervention works primarily by complementary changes in energy intake, then youth who eat while watching television would benefit more from the intervention. Previous research showed that decreases in energy intake were not observed for youth who infrequently ate in association with television viewing, while a decrease in energy intake of more than 600 kcal was observed for youth who ate in association with television viewing for at least 50% of their eating episodes.16 Television viewing reduction technology can also be used as part of a comprehensive obesity treatment program.19,41 The association of television viewing with eating supports the need to explore the reduction of television advertising as a way to avoid overeating and obesity in youth.42
The behavioral engineering technology of the TV Allowance may simplify the modification of child television viewing. It is possible that family rules regarding television viewing could have similar effects, but there may be important differences in technology vs parental control. Using technology to modify television viewing eliminates parental vigilance needed to enforce family rules and reduces the disciplinary action needed if a child exceeds his or her sedentary behavior limits. Perhaps most important, the device puts the choice of when to watch television in the child’s control, as opposed to a rule such as no television time until homework is completed. Although the TV Allowance and family rules can reduce sedentary behavior, there may be child differences in the perception of control that may relate to intervention effectiveness.
The TV Allowance was placed on all televisions and computers in the home. Without this technology, there would be additional parental demands to monitor use, especially in the case of televisions in children’s bedrooms. Placement of a television in a child’s bedroom may increase the risk of obesity more than televisions in family spaces43 and may make parental monitoring difficult.44
The intervention used in children aged 4 to 7 years is applicable to older children. It has previously been shown that the TV Allowance can be used to reduce home television viewing and computer use among older children and adolescents just as among younger children in the present study.3,16,45,46 A major difference is that older children may have more opportunities to visit friends and to accumulate additional television viewing and computer use at friends’ homes.
This study included children who were at or above the 75th BMI percentile; therefore, the results cannot be generalized to the prevention of at-risk children who were less overweight. Data on use of the television and computer, such as to entertain children or for educational purposes, may provide insight into how reducing television and computer use moderated the effects of the intervention among families of lower SES. There were limitations to the measurement of television viewing and energy intake. The TV Allowance accumulates television time until it is reset but does not provide downloadable information about when the television is watched. Energy intake data were collected using a food frequency questionnaire that assesses eating during the past month. Food diaries would be more labor intensive for subjects, but they would provide a detailed assessment of how television viewing affects behaviors that influence energy balance and body weight.
These results show that changes in the home environment may be important targets for reducing BMI in children and that the home environment as arranged by parents may contribute to the risk of pediatric obesity.47 In addition to complementary changes in energy intake that may accompany reductions in television viewing,16 an environment in which parents provide easy access to fruits and vegetables is related to children’s fruit and vegetable consumption,48 and parent and sibling models can maximize occasions to teach healthy eating habits to young children.49 There may be unique advantages to environmental manipulations that modify the shared family environment, including television and computer use, in which children develop positive behaviors that provide the basis for lifetime good eating and physical activity habits and a healthy body weight.
Acknowledgments
Funding/Support: This study was supported by grant DK63442 from the National Institute of Diabetes and Digestive Diseases (Dr Epstein) and by the Behavioral Medicine Laboratory, Department of Pediatrics, School of Medicine and Biomedical Sciences, State University of New York at Buffalo (Dr Roemmich).
Footnotes
Financial Disclosure: Dr Epstein is a consultant to Kraft Foods.
Author Contributions: Study concept and design: Epstein, Roemmich, and J. Robinson. Acquisition of data: Epstein, J. Robinson, Paluch, Winiewicz, and Fuerch. Analysis and interpretation of data: Epstein, J. Robinson, Paluch, and T. Robinson. Drafting of the manuscript: Epstein. Critical revision of the manuscript for important intellectual content: Epstein, Roemmich, J. Robinson, Paluch, Winiewicz, Fuerch, and T. Robinson. Statistical analysis: Epstein and Paluch. Obtained funding: Epstein and Roemmich. Administrative, technical, and material support: Epstein, J. Robinson, Winiewicz, and Fuerch.
References
- 1.Dietz WH, Jr, Gortmaker SL. Do we fatten our children at the television set? obesity and television viewing in children and adolescents. Pediatrics. 1985;75(5):807–812. [PubMed] [Google Scholar]
- 2.Gortmaker SL, Must A, Sobol AM, Peterson K, Colditz GA, Dietz WH. Television watching as a cause of increasing obesity among children in the United States, 1986–1990. Arch Pediatr Adolesc Med. 1996;150(4):356–362. doi: 10.1001/archpedi.1996.02170290022003. [DOI] [PubMed] [Google Scholar]
- 3.Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282(16):1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 4.Gortmaker SL, Peterson K, Wiecha J, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med. 1999;153(4):409–418. doi: 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]
- 5.Dennison BA, Russo TJ, Burdick PA, Jenkins PL. An intervention to reduce television viewing by preschool children. Arch Pediatr Adolesc Med. 2004;158(2):170–176. doi: 10.1001/archpedi.158.2.170. [DOI] [PubMed] [Google Scholar]
- 6.Taveras EM, Sandora TJ, Shih MC, Ross-Degnan D, Goldmann DA, Gillman MW. The association of television and video viewing with fast food intake by preschool-age children. Obesity (Silver Spring) 2006;14(11):2034–2041. doi: 10.1038/oby.2006.238. [DOI] [PubMed] [Google Scholar]
- 7.Utter J, Scragg R, Schaaf D. Associations between television viewing and consumption of commonly advertised foods among New Zealand children and young adolescents. Public Health Nutr. 2006;9(5):606–612. doi: 10.1079/phn2005899. [DOI] [PubMed] [Google Scholar]
- 8.Borzekowski DL, Robinson TN. The 30-second effect: an experiment revealing the impact of television commercials on food preferences of preschoolers. J Am Diet Assoc. 2001;101(1):42–46. doi: 10.1016/S0002-8223(01)00012-8. [DOI] [PubMed] [Google Scholar]
- 9.Jeffrey DB, McLellam RW, Fox DT. The development of children’s eating habits: the role of television commercials. Health Educ Q. 1982;9(2–3):174–189. [PubMed] [Google Scholar]
- 10.Galst JP. Television food commercials and pro-nutritional public service announcements as determinants of young children’s snack choices. Child Dev. 1980;51(3):935–938. [Google Scholar]
- 11.Taras HL, Sallis JF, Patterson PR, Nader PR, Nelson JA. Television’s influence on children’s diet and physical activity. J Dev Behav Pediatr. 1989;10(4):176–180. [PubMed] [Google Scholar]
- 12.Epstein LH, Rodefer JS, Wisniewski L, Caggiula AR. Habituation and dishabituation of human salivary response. Physiol Behav. 1992;51(5):945–950. doi: 10.1016/0031-9384(92)90075-d. [DOI] [PubMed] [Google Scholar]
- 13.Epstein LH, Paluch R, Smith JD, Sayette M. Allocation of attentional resources during habituation to food cues. Psychophysiology. 1997;34(1):59–64. doi: 10.1111/j.1469-8986.1997.tb02416.x. [DOI] [PubMed] [Google Scholar]
- 14.Wisniewski L, Epstein LH, Caggiula AR. Effect of food change on consumption, hedonics, and salivation. Physiol Behav. 1992;52(1):21–26. doi: 10.1016/0031-9384(92)90428-5. [DOI] [PubMed] [Google Scholar]
- 15.Temple JL, Giacomelli AM, Kent KM, Roemmich JN, Epstein LH. Television watching increases motivated responding and energy intake in children. Am J Clin Nutr. 2007;85(2):355–361. doi: 10.1093/ajcn/85.2.355. [DOI] [PubMed] [Google Scholar]
- 16.Epstein LH, Roemmich JN, Paluch RA, Raynor HA. The influence of changes in sedentary behavior on energy and macronutrient intake in youth. Am J Clin Nutr. 2005;81(2):361–366. doi: 10.1093/ajcn.81.2.361. [DOI] [PubMed] [Google Scholar]
- 17.Buchowski MS, Sun M. Energy expenditure, television viewing and obesity. Int J Obes Relat Metab Disord. 1996;20(3):236–244. [PubMed] [Google Scholar]
- 18.DuRant RH, Baranowski T, Johnson M, Thompson WO. The relationship among television watching, physical activity, and body composition of young children. Pediatrics. 1994;94(4 pt 1):449–455. [PubMed] [Google Scholar]
- 19.Epstein LH, Valoski AM, Vara LS, et al. Effects of decreasing sedentary behavior and increasing activity on weight change in obese children. Health Psychol. 1995;14(2):109–115. doi: 10.1037//0278-6133.14.2.109. [DOI] [PubMed] [Google Scholar]
- 20.Epstein LH, Saelens BE, O’Brien JG. Effects of reinforcing increases in active behavior versus decreases in sedentary behavior for obese children. Int J Behav Med. 1995;2(1):41–50. doi: 10.1207/s15327558ijbm0201_4. [DOI] [PubMed] [Google Scholar]
- 21.Epstein LH, Smith JA, Vara LS, Rodefer JS. Behavioral economic analysis of activity choice in obese children. Health Psychol. 1991;10(5):311–316. doi: 10.1037//0278-6133.10.5.311. [DOI] [PubMed] [Google Scholar]
- 22.Saelens BE, Epstein LH. The rate of sedentary activities determines the reinforcing value of physical activity. Health Psychol. 1999;18(6):655–659. doi: 10.1037//0278-6133.18.6.655. [DOI] [PubMed] [Google Scholar]
- 23.Epstein LH, Roemmich JN, Paluch RA, Raynor HA. Physical activity as a substitute for sedentary behavior in youth. Ann Behav Med. 2005;29(3):200–209. doi: 10.1207/s15324796abm2903_6. [DOI] [PubMed] [Google Scholar]
- 24.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103(6 pt 1):1175–1182. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 25.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337(13):869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 26.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002;246(246):1–90. [PubMed] [Google Scholar]
- 27.Pate RR, Baranowski T, Dowda M, Trost SG. Tracking of physical activity in young children. Med Sci Sports Exerc. 1996;28(1):92–96. doi: 10.1097/00005768-199601000-00019. [DOI] [PubMed] [Google Scholar]
- 28.Trost SG, Ward DS, Moorehead SM, Watson PD, Riner W, Burke JR. Validity of the Computer Science and Applications (CSA) activity monitor in children. Med Sci Sports Exerc. 1998;30(4):629–633. doi: 10.1097/00005768-199804000-00023. [DOI] [PubMed] [Google Scholar]
- 29.Ekelund U, Sjöström M, Yngve A, et al. Physical activity assessed by activity monitor and doubly labeled water in children. Med Sci Sports Exerc. 2001;33(2):275–281. doi: 10.1097/00005768-200102000-00017. [DOI] [PubMed] [Google Scholar]
- 30.Blum RE, Wei EK, Rockett HR, et al. Validation of a food frequency questionnaire in Native American and Caucasian children 1 to 5 years of age. Matern Child Health J. 1999;3(3):167–172. doi: 10.1023/a:1022350023163. [DOI] [PubMed] [Google Scholar]
- 31.Hollingshead AB. Four Factor Index of Social Status. New Haven, CT: Yale University; 1975. [Google Scholar]
- 32.Hedeker D, Gibbons RD. Longitudinal Data Analysis. Hoboken, NJ: John Wiley & Sons; 2006. [Google Scholar]
- 33.Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59(10):877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 34.Epstein LH, Raja S, Gold SS, Paluch RA, Pak Y, Roemmich JN. Reducing sedentary behavior: the relationship between park area and the physical activity of youth. Psychol Sci. 2006;17(8):654–659. doi: 10.1111/j.1467-9280.2006.01761.x. [DOI] [PubMed] [Google Scholar]
- 35.Epstein LH, Handley EA, Dearing KK, et al. Purchases of food in youth: influence of price and income. Psychol Sci. 2006;17(1):82–89. doi: 10.1111/j.1467-9280.2005.01668.x. [DOI] [PubMed] [Google Scholar]
- 36.Systat Software, Inc. SYSTAT 11.0. Richmond, CA: Systat Software Inc; 2004. [Google Scholar]
- 37.Paluch RA, Epstein LH, Roemmich JN. Comparison of methods to evaluate changes in relative body mass index in pediatric weight control. Am J Hum Biol. 2007;19(4):487–494. doi: 10.1002/ajhb.20608. [DOI] [PubMed] [Google Scholar]
- 38.Rose G. Strategy of prevention: lessons from cardiovascular disease. Br Med J (Clin Res Ed) 1981;282(6279):1847–1851. doi: 10.1136/bmj.282.6279.1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Parsons TJ, Power C, Logan S, Summerbell CD. Childhood predictors of adult obesity: a systematic review. Int J Obes Relat Metab Disord. 1999;23(suppl 8):S1–S107. [PubMed] [Google Scholar]
- 40.Janssen I, Boyce WF, Simpson K, Pickett W. Influence of individual- and area-level measures of socioeconomic status on obesity, unhealthy eating, and physical inactivity in Canadian adolescents. Am J Clin Nutr. 2006;83(1):139–145. doi: 10.1093/ajcn/83.1.139. [DOI] [PubMed] [Google Scholar]
- 41.Epstein LH, Paluch RA, Gordy CC, Dorn J. Decreasing sedentary behaviors in treating pediatric obesity. Arch Pediatr Adolesc Med. 2000;154(3):220–226. doi: 10.1001/archpedi.154.3.220. [DOI] [PubMed] [Google Scholar]
- 42.Caraher M, Landon J, Dalmeny K. Television advertising and children: lessons from policy development. Public Health Nutr. 2006;9(5):596–605. doi: 10.1079/phn2005879. [DOI] [PubMed] [Google Scholar]
- 43.Dennison BA, Erb TA, Jenkins PL. Television viewing and television in bedroom associated with overweight risk among low-income preschool children. Pediatrics. 2002;109(6):1028–1035. doi: 10.1542/peds.109.6.1028. [DOI] [PubMed] [Google Scholar]
- 44.Robinson JL, Winiewicz DD, Fuerch JH, Roemmich JN, Epstein LH. Relationship between parental estimate and an objective measure of child television watching. [May 3, 2007];Int J Behav Nutr Phys Act. 2006 3:e43. doi: 10.1186/1479-5868-3-43. http://www.ijnpa.org/content/3/1/43. [DOI] [PMC free article] [PubMed]
- 45.Ford BS, McDonald TE, Owens AS, Robinson TN. Primary care interventions to reduce television viewing in African-American children. Am J Prev Med. 2002;22(2):106–109. doi: 10.1016/s0749-3797(01)00410-x. [DOI] [PubMed] [Google Scholar]
- 46.Robinson TN, Killen JD, Kraemer HC, et al. Dance and reducing television viewing to prevent weight gain in African-American girls: the Stanford GEMS pilot study. Ethn Dis. 2003;13(1 suppl 1):S65–S77. [PubMed] [Google Scholar]
- 47.Davison KK, Birch LL. Obesigenic families: parents’ physical activity and dietary intake patterns predict girls’ risk of overweight. Int J Obes Relat Metab Disord. 2002;26(9):1186–1193. doi: 10.1038/sj.ijo.0802071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baranowski T, Cullen KW, Baranowski J. Psychosocial correlates of dietary intake: advancing dietary intervention. Annu Rev Nutr. 1999;19:17–40. doi: 10.1146/annurev.nutr.19.1.17. [DOI] [PubMed] [Google Scholar]
- 49.Harper LV, Sanders KM. The effect of adults’ eating on young children’s acceptance of unfamiliar foods. J Exp Child Psychol. 1975;20(2):206–214. [Google Scholar]