Abstract
Objectives
The aim of the study was to identify the major heat waves that occurred in France from 1971 to 2003 and describe their impact on all-cause and cause-specific mortality.
Methods
Heat waves were defined as periods of at least 3 consecutive days when the maximum and the minimum temperature, averaged over the whole France, were simultaneously greater than their respective 95th percentile. The underlying causes of death were regrouped into 18 categories. Heatstroke, hyperthermia and dehydration were assigned to the “heat-related causes” (HRC) category.
The numbers of deaths observed (O) during the identified heat waves were compared to those expected (E) on the basis of the mortality rates reported for the three preceding years.
Results
Six heat waves (HW) were identified from 1971 to 2003. They were associated with great excess mortality (from 1300 to 13700 deaths). The observations are compatible with a moderate harvesting effect for four of the six HW. The mortality ratios increased with age for subjects aged over 55 years and were higher for women than for men over 75 years.
For the six HW, the excess mortality was significant for almost all the causes of death:
the greatest excess mortality (O-E) were observed for cardiovascular diseases, neoplasms, respiratory system diseases, HRC, ill-defined conditions and injury and poisoning,
the mortality ratios (O/E) were highest for HRC, respiratory diseases, nervous system diseases, mental disorders, infectious diseases, and endocrine and nutritional diseases.
Conclusions
Heat waves associated with excess mortality are not rare events in this temperate climate country. The excess mortality is much greater than HRC mortality. Some populations are particularly vulnerable to heat waves: the elderly, women and people with some specific diseases. However, no segment of the population may be considered protected from the risks associated with heat waves.
Keywords: Age, Cause of Death, gender, Heat wave, Mortality
Keywords: Adult, Age Factors, Aged, Cause of Death, trends, Female, France, epidemiology, Heat, adverse effects, Humans, Male, Middle Aged, Mortality, trends, Sex Factors
INTRODUCTION
The association between heat waves (HW) and mortality has been clearly established. (Basu and Samet, 2002; Besancenot, 2002) Some authors have described the association between the usual daily fluctuations in temperature and mortality using time series or a spatial approach. Others have focused on individual major heat episodes, in which an increase in mortality was observed concomitantly with an HW. Those authors described the characteristics of the mortality during or after the HW. (Applegate et al., 1981; Dessai, 2002; Ellis and Nelson, 1978; Ellis et al., 1980; Grize et al., 2005; Henschel et al., 1969; Katsouyanni et al., 1993; Naughton et al., 2002; Qiu et al., 2002; Rooney et al., 1998; Sartor et al., 1995; Schuman, 1972; Weisskopf et al., 2002; Whitman et al., 1997) Using the latter approach, we will particularly focus on the medical causes of death involved in such events.
Several studies considered heat-related deaths to be those for which heat was cited in the medical records.(2002; Nakai et al., 1999; Weisskopf et al., 2002; Wolfe et al., 2001) The resulting heat-related death count has been shown to be markedly smaller than the overall excess mortality observed during heat waves, particularly when the cause of death was not certified by specially trained physicians.(Shen et al., 1998) Excesses due to many causes of death other than heat-related causes occur during HW.
Some studies have systematically described the mortality or morbidity structure in terms of the causes of HW-related excess. (Applegate et al., 1981; Ellis and Nelson, 1978; Henschel et al., 1969; Michelozzi et al., 2005; Schuman, 1972; Semenza et al., 1999) Cardiovascular diseases (Applegate et al., 1981; Crawford et al., 2003; Ellis and Nelson, 1978; Ellis et al., 1980; Henschel et al., 1969; Huynen et al., 2001; Michelozzi et al., 2005; Rooney et al., 1998; Schuman, 1972; Semenza et al., 1999), respiratory diseases and causes directly related to heat (heatstroke, hyperthermia and dehydration) strongly contributed to the excess. A marked relative increase in the mortality or morbidity due to respiratory diseases, nervous system diseases and mental illnesses during HW has also been observed (Bark, 1998; Braga et al., 2002; Ellis and Nelson, 1978; Henschel et al., 1969; Huynen et al., 2001; Michelozzi et al., 2005; Rooney et al., 1998; Schuman, 1972; Semenza et al., 1999; Sharma, 2005). However, the maximum overall excess mortality observed in those studies was 2100 deaths, limiting the number of observable categories and the statistical precision of the analyses.
In the absence of any exceptional event, high temperatures are correlated with daily mortality,(Hales et al., 2000; Larsen, 1990; Zauli Sajani et al., 2002) but, more specifically, a marked increase in mortality is observed during HW characterized by the long duration of high temperatures.(Robinson, 2000; Smoyer, 1998) Other parameters than temperature have been shown to be linked to HW associated mortality, particularly pollution in urban areas(Basu and Samet, 2002; Besancenot, 2002), but are not available, to our knowledge, over a large period on the geographical scale of a whole temperate country with a population of more than 50 million inhabitants.
This paper addresses major HW because an increase in the frequency of such episodes is probable and has implications for public health, in the context of global climate change. Specially, it identifies HW in the whole France from 1971 to 2003 and details the all-cause and cause-specific structure of the excess mortality associated with those HW.
MATERIAL AND METHODS
Mortality data
The mortality data were derived from the Inserm (French National Institute for Medical Research) national database. Using the 8th (1971–1978), 9th (1979–1999) and 10th (2000–2003) updates of the International Classification of Diseases, the causes of death were classified using the 17 categories aggregated by Eurostat to ensure comparability over time and within the European Community (appendix l).(Jougla et al., 1998) An additional “Heat Related Causes” (HRC) category for deaths reported to be directly related to the HW by the physician, i.e.: dehydration, hyperthermia and heatstroke, was also considered.
The national mortality database generally includes more than one cause by death (the underlying cause and the contributing causes). The underlying cause of death is defined as the cause that originated the morbid process leading to the death. This cause is selected according to precise rules and recommendations from the International Classification of Diseases (more and more, this process of selection is done automatically).
An “underlying or contributing HRC” death category was thus defined as the deaths for which one of the causes cited was an HRC.
The analyses by cause of death were carried out by underlying cause and by dissociating the “underlying or contributing HRC” category, using a multiple-cause approach.(Redelings et al., 2006)
Meteorological data and identification of heat waves (HW)
Mainland France is administratively divided into 95 “départements”. The daily maximum and minimum temperatures from June to September, for the period 1971–2003, were obtained from one meteorological station per département, considered by Météo-France as representative of the population of the département. Daily average temperatures over the whole country were calculated as the population weighted average of the daily temperature observed in each of the 95 départements.
A HW was defined as a period of at least 3 consecutive days when the maximum (tmax) and minimum (tmin) temperatures were concomitantly greater than their respective 95th percentile: 30.0°C and 17.3°C, respectively.
Excess mortality estimation
On the basis of previous findings (Basu and Samet, 2002; Fouillet et al., 2006), we have defined the HW-associated mortality period as the HW period, plus 2 days after the last high-temperature day, in order to take the time lag between exposure and death into account. The mortality observed during those periods (O) was compared with the expected mortality (E) calculated on the basis of the observed mortality during the three preceding years. A log-linear Poisson model of the mortality rates, was used to estimate the expected number of deaths by month, year, age (ten-year groups), gender, and cause of death. Each parameter was systematically included in the model when the goodness of fit was significantly decreased. Finally, the model contained, for each age group, a linear annual trend, a specific month effect and a specific term for every cause of death by gender. The deviance divided by the number of degrees of freedom ranged from 1.48 to 3.45, depending on the HW considered. Over-dispersion was then taken into account in the calculation of confidence intervals and p-values. Using this model, an estimate of the expected number of deaths and its variance was obtained for each category.
On the basis of the fluctuations in the daily numbers of deaths that were observed during the reference period, “95% fluctuation intervals” were defined as intervals in which there was a 95% probability of observing the daily numbers of deaths in the future if they had the same expected value and variance as the deaths which were observed during the reference period. "Fluctuation intervals" are therefore prediction intervals.
The excess mortality (O-E) and mortality ratio (O/E) were calculated for each cause of death. The excess mortality (O-E) provides information on the importance of a given cause with respect to the overall excess mortality during an HW. The proportion of the excess for each cause in the overall excess was also calculated in order to compare the excess mortalities of different HW.
The mortality ratio (O/E) provides information on the impact of an HW on a particular cause of death. In order to compare the mortality ratios of different HW, the overall mortality ratio (O+/E+) was considered to be a measure of the impact of an HW on a population. Then, for each cause, relative mortality ratios were calculated:
where is the mortality ratio for a cause, “c”.
For each cause of death, the heterogeneity of the relative mortality ratios of the HW was tested, considering that the death counts for all the HW had independent multinomial distribution conditionally on the overall mortality ratio.
Standardization on age and gender structure
In order to compare the mortality structures by cause, the variations in the age and gender structure of the mortality in time were controlled.
Standard weights were calculated by age group “a” and gender “g” on the basis of the distribution of the sum of the expected mortalities due to that cause “c” for all the HW as follows:
, where “h” is a heat wave and “a’” and “g’” are age and gender indices of the sum.
Those weights, common to all the HW, were then used to obtain age- and gender-standardized mortality ratios as well as age- and gender-standardized proportions of the total expected mortality by cause.
Also, the age- and gender-standardized ratio for HW “h” and cause “c” was calculated as the weighted sum of age and gender specific mortality ratios as:
Similarly, for each HW and cause, the standardized proportions of the total excess mortality were calculated as the mean of the percentages by age and gender, weighted by the distribution of the sum of all causes of excess mortality by age and gender for all the HW.
RESULTS
General characteristics and temporal distribution of temperatures and mortality for the identified heat waves (HW)
Six HW were identified in France between 1971 and 2003 (table 1), their duration ranged from 3 days in 2001 to 11 days in 2003. During the first five HW, the average maximum temperature ranged from 30.8°C in 2001 to 33.5°C in 1990 and the average minimum temperature ranged from 17.7°C in 2001 to 18.5°C in 1990. In 2003, the average maximum and minimum temperatures during the HW were much higher than those for all the other HW, 36.4°C and 20.0°C, respectively.
Table 1.
Description of the major heat waves in France from 1971 to 2003
| Year: | 1975 | 1976 | 1983 | 1990 | 2001 | 2003 |
|---|---|---|---|---|---|---|
| Population | ||||||
| Total (million) | 52.7 | 52.9 | 54.8 | 56.7 | 59.2 | 59.8 |
| % <35 years | 53.8% | 54.0% | 53.1% | 50.3% | 45.7% | 45.1% |
| % 35 – 74 years | 41.1% | 40.8% | 40.8% | 43.0% | 46.8% | 47.1% |
| % 75 years or + | 5.1% | 5.2% | 6.1% | 6.7% | 7.5% | 7.8% |
| Temperatures (°C)a | ||||||
| Number of consecutive hot daysb | 5 | 9 | 4 | 5 | 3 | 11 |
| Average max. | 32.4 | 32.8 | 31.6 | 33.5 | 30.8 | 36.4 |
| Average min. | 18.2 | 17.9 | 18.4 | 18.5 | 17.7 | 20.0 |
| HW-associated mortality periodc | ||||||
| Begin | August 1st | June 28th | July 10th | August 1st | July 30th | August 3rd |
| End | August 7th | July 8th | July 15th | August 7th | August 3rd | August 15th |
| HW-associated mortality | ||||||
| Observed (O) | 12 507 | 20 560 | 10 301 | 10 838 | 7 814 | 31 431 |
| Expected (E) | 9 555 | 15 444 | 8 828 | 9 214 | 6 484 | 17 697 |
| Excess (O-E) | 2 952 | 5 116 | 1 473 | 1 624 | 1 330 | 13 734 |
| % <35 years | 5.6% | 3.1% | 4.4% | 5.5% | 2.0% | 0.6% |
| % 35 – 74 years | 32.6% | 32.7% | 26.5% | 26.6% | 21.6% | 19.8% |
| % 75 years or + | 61.7% | 64.3% | 69.1% | 67.9% | 76.4% | 79.6% |
| % female | 53.5% | 56.1% | 53.3% | 59.4% | 60.1% | 64.7% |
| Mortality ratio (O/E) | 1.31 [1.28;1.34] | 1.33 [1.31;1.35] | 1.17 [1.14;1.19] | 1.18 [1.15;1.20] | 1.21 [1.18;1.23] | 1.78 [1.75;1.80] |
| Harvestingd | ||||||
| O-E | −89 | −696 | 2131 | −1214 | −111 | 754 |
| O/E | 1.00 | 0.97 | 1.07 | 0.96 | 1.00 | 1.03 |
Average temperatures were calculated by weighting the temperatures of the 95 départements by their population;
At least 3 consecutive days where the maximum (tmax) and minimum (tmin) temperatures were concomitantly greater than their respective 95th percentile
HW period added by 2 days after the last hot day.
Mortality during the 20 days following the HW-associated mortality period
All of the HW were associated with a significant excess mortality. The excess mortality during the HW-associated mortality period was about 3000 deaths for the 1975 HW, 5100 deaths for 1976, 1500 deaths for 1983, 1600 deaths for 1990, 1300 for 2001 and 13700 deaths for 2003 (table 1). The corresponding mortality ratios ranged from 1.17 in 1983 to 1.78 in 2003.
All the heat waves have shown a close concordance between the chronological variations in maximum daily temperature and daily mortality (figure 1). A progressive increase in mortality while temperatures were very high was followed by a fast decline when temperature fell towards the reference temperature. The 1983 HW had a somewhat different profile in that temperature and mortality were still greater than the reference values after fulfilling the heat criterion. However, the mortality increased over the HW period and decreased afterwards.
Figure 1.
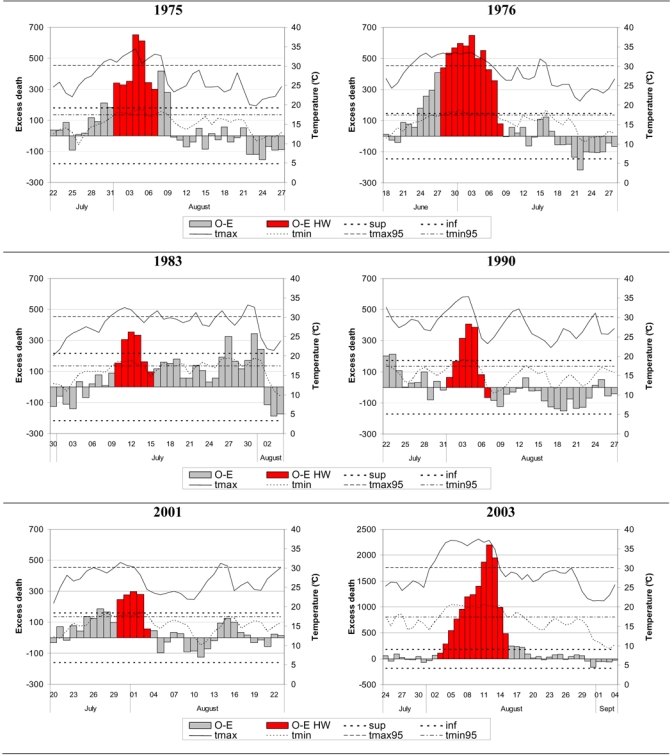
Temporal distributions of excess mortality in France during the 1975,1976, 1983,1990, 2001 and 2003 heat waves.
O-E: daily excess deaths; O-E HW: daily excess deaths during the HW-associated mortality period; sup, inf: upper and lower limit of the 95% fluctuation intervals of the daily number of deaths; tmax, tmin: average daily maximum and minimum temperatures; tmax95, tmin95: 95th percentile of the maximum and minimum temperatures.
Harvesting
On the 20 days following the HW-associated mortality period, the excess mortality was negative for four of the six HW (table 1). Except in 1990, the decrease in the mortality was much smaller than the excess mortality associated with the HW. However, except in 1983, on the 20 days following each HW-associated mortality period, a period of at least 5 consecutive days with a lower-than-expected mortality was observed. Those periods coincided with a decrease in the temperatures (figure 1).
Age and gender structure of HW associated mortality
The percentage of the population aged 75 years or more increased from 1975 to 2003 (table 1). The percentage of the overall excess deaths occurring among people aged 75 years or more increased from 62% in 1975 to 80% in 2003 while the percentage occurring among subjects under 35 decreased from 5.6% in 1975 to 0.6% in 2003 and the percentage occurring among women increased from 53% in 1975 to 65% in 2003.
For all the HW, the mortality ratios (O/E), by age and gender, showed similarities (figure 2):
Figure 2.
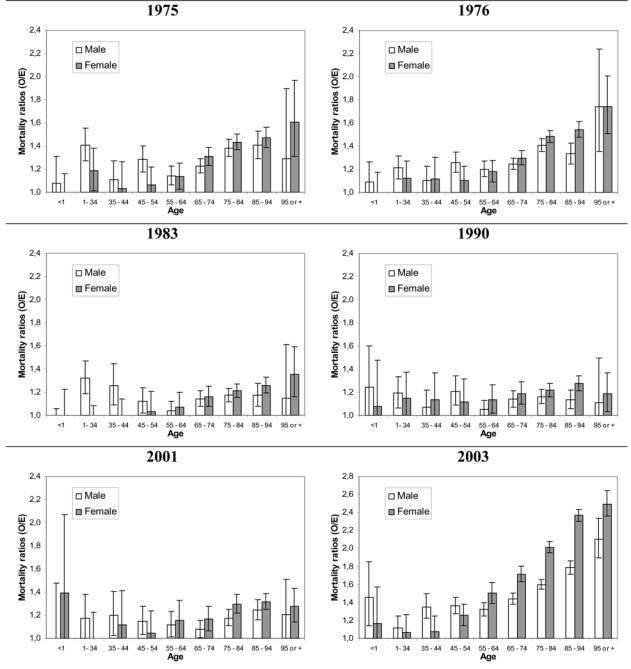
Mortality ratios by age (years) and gender in France during the 1975, 1976, 1983, 1990,2001 and 2003 heat waves.
Horizontal bars around each value represent the 95% confidence interval.
mortality ratios increased with age above 55 years, but the excess mortality was already significant for the aggregation of younger age groups (except in 2001, the mortality ratios were significantly greater than 1 for subjects aged less than 35 years);
except in 1976, the female mortality ratios were greater than the male mortality ratios above age 65 years for all the HW. This was significant only in 2003 when it was particularly marked. The age- and gender-standardized mortality ratios for the “over 75” age groups were from 5% higher for women in 1983 to 28% higher in 2003 as compared to men.
Excess mortality by cause of death
For all the HW, almost all the excess mortalities by cause of death were positive (table 2).
Table 2.
Proportion of expected and excess mortality by medical cause of death in France during the 1975, 1976, 1983, 1990, 2001 and 2003 heat waves.
| 1975
|
1976
|
1983
|
1990
|
2001
|
2003
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| %E | %(O-E) | %E | %(O-E) | %E | %(O-E) | %E | %(O-E) | %E | %(O-E) | %E | %(O-E) | |
| Underlying causes: | ||||||||||||
| 1. Infectious diseases | 3% | 4% | 3% | 4% | 1% | 4% | 2% | 4% | 2% | 6% | 2% | 3% |
| 2. Neoplasms | 23% | 16% | 23% | 8% | 24% | 9% | 28% | 17% | 30% | 12% | 30% | 7% |
| 4. Endocrine, nutritional diseasesa | 2% | 5% | 3% | 4% | 2% | 3% | 2% | 3% | 3% | 7% | 3% | 4% |
| 5. Mental disorders | 1% | 2% | 1% | 2% | 2% | 4% | 2% | 3% | 3% | 7% | 3% | 5% |
| 6. Nervous system diseases | 2% | 4% | 2% | 5% | 2% | 3% | 2% | 5% | 3% | 10% | 4% | 6% |
| 7. Cardiovascular diseases | 37% | 41% | 37% | 45% | 36% | 36% | 33% | 25% | 29% | 25% | 29% | 23% |
| 8. Respiratory system diseases | 4% | 6% | 5% | 10% | 5% | 10% | 5% | 13% | 6% | 7% | 5% | 9% |
| 9. Digestive system diseases | 7% | 5% | 7% | 2% | 6% | 4% | 6% | 3% | 5% | 3% | 5% | 2% |
| 10. Skin diseases | - | - | - | - | - | - | - | 2% | - | 1% | - | - |
| 11. Musculoskeletal diseases | - | - | - | - | - | - | - | - | - | 2% | - | - |
| 12. Genitourinary diseases | 2% | 1% | 2% | 1% | 2% | 2% | 1% | - | 1% | 3% | 1% | 3% |
| 14. Perinatal diseases | - | - | - | - | - | - | - | 1% | - | - | - | - |
| 16. Ill-defined conditionsb | 5% | 5% | 5% | 6% | 6% | 7% | 6% | 4% | 6% | 10% | 7% | 10% |
| 17. Injury, poisoningc | 11% | 11% | 10% | 6% | 10% | 14% | 10% | 11% | 9% | 3% | 8% | 3% |
| HRC (Heat Related Causes)d | - | 2% | - | 6% | - | 4% | - | 7% | - | 4% | - | 21% |
| Underlying or contributing HRCe | _ | 6% | _ | 15% | 1% | 13% | 2% | 21% | 2% | 17% | 2% | 44% |
| All causes | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% |
Excluding dehydration;
Excluding hyperthermia;
Excluding heatstroke;
Heat Related Causes: dehydration, hyperthermia and heatstroke;
Including deaths for which one of the coded causes was an HRC.
O: observed number of deaths, E: expected number of deaths, %E: Deaths as a percentage of overall expected mortality; %(O-E): Excess deaths as a percentage of overall excess mortality. “-”: percentage is less than 1%. Only the causes for which %E or %(O-E) are greater than 1% for at least one heat wave have been reported.
Heat Related Causes of death (HRC)
HRC as the underlying or contributing cause of death were very rare in the expected mortality for the six HW (table 2). During all the HW except that in 1975, the percentage of underlying HRC deaths expressed relative to the overall excess death count was greater than 4%. The percentage was particularly high in 2003: 21%.
The percentage of excess deaths with an underlying or contributing HRC, which ranged from 6% in 1975 to 44% in 2003, was more than two-fold greater than the percentage of excess deaths with an underlying HRC only for each of the HW.
Other causes of death
Cardiovascular diseases, respiratory system diseases, neoplasms, injury and poisoning, and ill-defined conditions accounted for a major percentage of the overall excess mortality for all six HW (table 2). For all the other causes except nervous system diseases, the contribution to excess mortality was lower than 10% for all the HW.
The percentage of cardiovascular-disease causes in the overall excess mortality fell from 41% in 1975 to 23% in 2003, while the percentage of cardiovascular disease-related expected mortality decreased from 37 to 29% of the overall mortality (table 2).
The results remained stable when the age- and gender-structure time trends were taken into account by considering standardized percentages.
Mortality ratios by cause of death
Heat-Related Causes (HRC)
The relative mortality ratios when HRC constituted the underlying cause of death ranged from 1.94 in 1983 to 18.15 in 2003 and were the greatest ratios for all underlying causes and for all HW. The relative mortality ratios when HRC constituted an underlying or contributing cause ranged from 2.19 in 1983 to 9.24 in 2003 and were less heterogeneous than the ratios when HRC constituted the underlying cause of death.
Other causes of death
With regard to the other underlying causes, the mortality ratios were greatest for all six HW for respiratory system diseases, nervous system diseases and mental disorders, infectious diseases, and endocrine and nutritional diseases.
Some other causes had lower relative mortality ratios. This was the case for ill-defined conditions, genitourinary diseases (except in 1990), injury and poisoning (except in 2001), digestive system diseases, cardiovascular diseases and neoplasms.
For each of the causes of death, the relative mortality ratios were of the same order for all the HW (table 3). However, for almost all causes, the relative mortality ratios showed statistically-significant between-HW heterogeneity, most often related to the particular characteristics of the 2003 HW. The relative mortality ratios for HRC, ill-defined conditions and genitourinary diseases were greater for the 2003 HW than for the other five HW.
Table 3.
Relative mortality ratiosa by medical cause of death in France during the 1975, 1976, 1983, 1990, 2001 and 2003 heat waves
| 1975 | 1976 | 1983 | 1990 | 2001 | 2003 | |
|---|---|---|---|---|---|---|
| Underlying causes: | ||||||
| 1. Infectious diseases | 1.03 | 1.13 | 1.21 | 1.19 | 1.38 | 1.31 * |
| 2. Neoplasms | 0.93 | 0.84 | 0.91 | 0.94 | 0.90 | 0.66 * |
| 3. Blood diseases | - | - | - | - | - | 0.92 |
| 4. Endocrine, nutritional diseasesb | 1.23 | 1.18 | 1.10 | 1.07 | 1.22 | 1.18 |
| 5. Mental disorders | 1.21 | 1.25 | 1.23 | 1.02 | 1.25 | 1.23 * |
| 6. Nervous system diseases | 1.19 | 1.35 | 1.07 | 1.23 | 1.33 | 1.26 * |
| 7. Cardiovascular diseases | 1.02 | 1.05 | 1.00 | 0.96 | 0.98 | 0.91 * |
| 8. Respiratory system diseases | 1.09 | 1.25 | 1.11 | 1.20 | 1.03 | 1.34 * |
| 9. Digestive system diseases | 0.92 | 0.84 | 0.95 | 0.93 | 0.93 | 0.77 * |
| 10. Skin diseases | - | - | - | 1.45 | 1.26 | 0.88 * |
| 11. Musculoskeletal diseases | - | - | - | - | 1.29 | 1.06 |
| 12. Genitourinary diseases | 0.92 | 0.93 | 1.03 | - | 1.21 | 1.33 * |
| 13. Pregnancy, childbirth | - | - | - | 3.68 | - | - * |
| 14. Perinatal diseases | 0.55 | 0.59 | - | 1.49 | - | 0.80 * |
| 15. Congenital malformations | - | - | - | - | - | 0.89 |
| 16. Ill-defined conditionsc | 0.99 | 1.05 | 1.02 | 0.95 | 1.10 | 1.27 * |
| 17. Injury, poisoningd | 1.00 | 0.90 | 1.04 | 1.02 | - | 0.74 * |
| HRC (Heat Related Causes)e | 3.37 | 10.74 | 1.94 | 2.67 | 2.06 | 18.15 * |
| Underlying or contributing HRCf | 3.66 | 7.38 | 2.19 | 2.82 | 2.36 | 9.24* |
| All causes | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00* |
Relative O/E: cause-specific mortality ratio divided by the overall “All causes” mortality ratio. O: observed number of deaths; E: expected number of deaths;
Excluding dehydration
Excluding hyperthermia
Excluding heatstroke;
Heat Related Causes: dehydration, hyperthermia and heatstroke;
Including deaths for which one of the coded causes was an HRC.
“-” O/E is not significantly different from 1 at the 5% level.
the relative mortality ratios for 1975, 1976, 1983, 1990, 2001 and 2003 are statistically heterogeneous at the 1% level.
Conversely, the ratios were lower during the 2003 HW for neoplasms, cardiovascular diseases and injury and poisoning.
When considering the underlying medical cause of death only for death certificates without any contributing HRC, similar mortality ratios by cause were observed.
The age- and gender-standardized mortality ratios were very similar to the non-standardized ratios.
Causes of death by age and gender
Similar results were obtained for the age groups: “35–74 years” and “≥ 75 years”. Considering the underlying causes of death, for the “under 35 years” age group, except in 2001 and 2003, the majority of the excess mortality was due to injury and poisoning. This cause of death is also the main expected cause for that age group. Except in 2001, there was a significant excess of underlying HRC.
Except for the 1975 and the 1983 HW, the all-cause mortality ratios, standardized on age structure, were significantly greater for females for all the HW and ranged from a 5% excess in 1976 to a 20% excess in 2003. For all six HW, the female age-standardized mortality ratios were markedly higher for infectious diseases and genitourinary diseases reported as underlying causes, and for deaths with an underlying or contributing HRC. For genitourinary diseases, the difference was significant for the 1975, 1990, 2001 and 2003 HW. For all the other causes, the age-standardized mortality ratios showed no significant between-gender difference for at least three of the six HW.
DISCUSSION
Six heat waves (HW) were identified in France from 1971 to 2003. They were associated with great excess mortality (from 1300 to 13700 deaths) and shown to exhibit close chronological concordance between daily temperature and mortality time course over the HW. The mortality ratios increased with age for subjects aged over 55 years and were 5 to 28% higher for women than for men over 75 years.
Considering the underlying causes of death for the six HW, the excess mortality was significant for almost all the causes:
the greatest excess mortality (O-E) were observed for cardiovascular diseases, neoplasms, respiratory system diseases, HRC, ill-defined conditions, and injury and poisoning,
the mortality ratios (O/E) were highest for heat-related causes (HRC), respiratory diseases, nervous system diseases, mental disorders, infectious diseases, and endocrine and nutritional diseases.
The percentage of cardiovascular diseases in the overall excess mortality decreased over the six HW. During the 2003 HW, the percentage of HRC (as an underlying or contributing cause) was higher.
This study was performed on the whole French territory by using averaged temperature weighted by the population of the départements. The spatial precision of temperatures, one meteorological station per département, may be considered questionable. However, the temporal correlation between the population-weighted temperature average at the département level and the population-weighted temperature average derived from a 10km-step grid (4145 points) provided by Météo-France for the period 1993-2003 was greater than 0.99. This finding probably reflects the strong spatial correlation of the temporal variations in temperature over the whole country.
The criteria used to identify temporally major HW as well as HW-associated mortality periods addressed in this study were somewhat arbitrary and are not proposed as a formal definition of HW. This is particularly obvious for the 1983 HW, in which temperatures were still high and mortality was still in excess after the identified period. Such criteria enabled clear differentiation of six HW with major excess mortality in a large temperate country from the daily fluctuations in mortality associated with high temperatures. Those fluctuations can be observed before or after all HW. For the six identified HW, the overall associated excess mortalities were strong and enabled the elucidation of fine categories of age and medical causes of the excess mortality during HW.
A three-year reference period was chosen to ensure both comparability of the cause-specific mortality structure and statistical stability. For the 1976 and 2003 HW, a HW is present in the reference period. However, the HW do not affect the estimation of the expected mortality in either case: in 1976, because the months of their respective occurrences are not the same and the months are individualized; in 2003, for the same reason, since the excess mortality during August for the 2001 HW is negligible.
The daily mortality course follows the same characteristic shape during each identified HW with a progressive increase in mortality while temperatures were very high and a fast decline when temperatures fell toward the reference temperatures. In line with previous studies (Braga et al., 2002; Dessai, 2002; Huynen et al., 2001; Rooney et al., 1998; Sartor et al., 1995), our observations are compatible with a moderate harvesting effect during the 20 days following the mortality associated with HW period. Indeed, a lower than expected mortality was observed for four of the six HW, although the magnitude of this effect was generally much smaller than the excess mortality during the HW.
The very high proportion of excess deaths occurring in subjects aged 75 years or more reflect both the age structure of the expected mortality and the marked increase of the mortality ratios with age.
For all six HW, higher mortality ratios were observed for women age over 65 than for men in the same age group. This finding has not been systematically reported in other studies of HW.(Rooney et al., 1998; Whitman et al., 1997) The difference appeared to be particularly great for genitourinary system diseases, for infectious diseases as underlying causes, and for underlying or contributing HRC.
Except for the 2001 HW, significant excess mortality in the “under 35 years” age group was observed for all the HW. The excess was statistically significant only for males. Injury and poisoning constituted the main underlying cause of expected and excess mortality for subjects under 35. Thus, even though the elderly constitute the most vulnerable subpopulation during a HW and the percentage of the overall excess death occurring among subjects under 35 is lower than 1% during the 2003 HW, it should be stressed that no sub-population can be considered devoid of risk.
HRC have been reported to constitute the most specific medical cause of death associated with HW and have been shown to be a major medical cause of death during other HW.(Applegate et al., 1981; Henschel et al., 1969) Monitoring that type of cause, especially during heat episodes, may constitute an important component of a mortality surveillance system.
The contribution of HRC to overall excess mortality increased dramatically during the 2003 HW, compared with the other five HW. As a matter of fact, the intensity and duration of the 2003 HW were much greater than had ever been observed in the same country.(Bessemoulin et al., 2004) Additionally, the 2003 HW developed into a major crisis situation that was of much greater magnitude and had a markedly-higher profile than the five preceding HW. The connection between mortality and heat exposure was therefore more immediately obvious, and so we cannot exclude a modification of the certification of HRC during this episode. This particular increase was observed for underlying HRC and for contributing HRC as well.
Infectious, endocrine and nutritional diseases gave rise to high mortality ratios for all six HW and have rarely been described in studies which were based on smaller excess mortalities.(Ellis and Nelson, 1978; Michelozzi et al., 2005) The analyses were conducted on a period covered by three different updates of the ICD (8, 9 and 10). This fact makes more precise cause-of-death analysis difficult. However, the mortality ratios for infectious diseases mainly appear to be high because of the high mortality ratios for septicaemia. This cause is coded as an underlying cause when there is a lack of information, but it is generally a terminal cause of death. It is thus likely that HW induce complications in some cases of infection, leading to acute septicaemia and resulting in death.
No cause of death in the “endocrine and nutritional disease” category seems to have increased specifically. Diabetes is the most frequent disease in that category. The incidence of diabetes clearly cannot increase in such a short period. Endocrine and nutritional disease thus probably constitute vulnerability factors during HW.
The mortality ratios by underlying cause of death observed for deaths with no mention of heat, i.e. without underlying or contributing HRC, were similar to those observed for all deaths during all the HW. In consequence, one may considered that description of the major mortality ratios by underlying cause of death, except for HRC, may help to identify the preexisting diseases that may be considered to constitute major risks during HW.
Except for HRC, the causes associated with the highest excess mortality were essentially those giving rise to the highest percentages of the usual mortality. Moreover, the relative ratios were similar for the six HW. This suggests that the proportions of some causes of the overall expected mortality, such as cardiovascular disease, nervous system disease and mental illness, may reflect the vulnerability of a given population. An analysis on a finer geographical scale may contribute to further elucidating that aspect.
As a conclusion, this study showed that, despite the exceptional impact of the 2003 HW on the population, the HW and its effects on mortality share many common epidemiological characteristics with the five other HW that have occurred in France since 1971. Some populations are particularly vulnerable to heat waves: the elderly, women and people with some specific diseases. However, no segment of the population may be considered protected from the risks associated with heat waves.
Acknowledgments
We would like to express our gratitude to the institutions that afforded us various forms of assistance in this study: Inserm, INSEE and Météo-France, and to the members of those institutions with whom we worked: F. Laurent, C. Jacquart and A. Le Toullec, with Inserm-CépiDc-IFR69; G. Desplanques with INSEE; JM. Veysseire and G. Gayraud with Météo-France. We also are very grateful to A. Mullarky for his skilful assistance in the preparation of the English version of this manuscript.
Funding
This work was financed by Inserm (French National Institute for Health and Medical Research), InVS (Institut de Veille Sanitaire) and DGS (Direction Générate de la Santé).
Appendix 1. ICD8 (1971–1978), ICD9 (1979–1999) and ICD10 (2000–2003) codes of the 17 categories and the HRC category
| ICD8 | ICD9 | ICD10 | |
|---|---|---|---|
| 1.Infectious diseases | 000-136 | 001-139 | A00 – B99 |
| 2.Neoplasms | 140-239 | 140-239 | C00 – D48 |
| 3.Blood diseases | 280-289 | D50-D89 | D50 – D89 |
| 4.Endocrine and nutritional diseasesa | 240-279 | 240-276.4,276.6-278.9 | E00 – E859,E87 – E90 |
| 5.Mental disorders | 290-315 | 290-319 | F00 – F99 |
| 6.Nervous system diseases | 320-389 | 320-389 | G00 – H95 |
| 7.Cardiovascular diseases | 390-444.1,444.3-458,782.4 | 390-459 | I00 – 199 |
| 8.Respiratory system diseases | 460-519 | 460-519 | J00 – J99 |
| 9.Digestive system diseases | 520-577,444.2 | 520-579 | K00 – K93 |
| 10.Skin diseases | 680-709 | 680-709 | L00 – L99 |
| 11.Musculoskeletal diseases | 710-738 | 710-739 | M00 – M99 |
| 12.Genitourinary diseases | 580-629,792 | 580-629 | N00 – N99 |
| 13.Pregnancy, childbirth | 630-678 | 630-676 | O00 – O99 |
| 14.Perinatal diseases | 760-779 | 760-779 | P00 – P96 |
| 15.Congenital malformations | 740-759 | 740-759 | Q00 – Q99 |
| 16.111-defined conditionsb | 780-782.3,782.5-787, 788.1-788.7,788.9-791,793-796 | 780-780.5,780.7-799 | R00-R50.8,R51-R99 |
| 17.Injury, poisoningc | E800-E899,E901-E999 | E800-E899,E901-E999 | V01-X29,X31-Y89 |
| HRC (Heat Related Causes)d | 788.0,788.8,E900 | 276.5,780.6,E900 | E86, R50.9, X30 |
Excluding dehydration;
Excluding hyperthermia;
Excluding heatstroke;
Heat Related Causes: dehydration, hyperthermia and heatstroke
References
- 1.Heat-related deaths--four states, July-August 2001, and United States, 1979–1999. MMWR Morb Mortal Wkly Rep. 2002;51:567–70. [PubMed] [Google Scholar]
- 2.Applegate WB, Runyan JW, Jr, Brasfield L, et al. Analysis of the 1980 heat wave in Memphis. J Am Geriatr Soc. 1981;29(8):337–42. doi: 10.1111/j.1532-5415.1981.tb01238.x. [DOI] [PubMed] [Google Scholar]
- 3.Bark N. Deaths of psychiatric patients during heat waves. Psychiatr Serv. 1998;49(8):1088–90. doi: 10.1176/ps.49.8.1088. [DOI] [PubMed] [Google Scholar]
- 4.Basu R, Samet JM. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol Rev. 2002;24(2):190–202. doi: 10.1093/epirev/mxf007. [DOI] [PubMed] [Google Scholar]
- 5.Besancenot J. Vagues de chaleur et mortalité dans les grandes agglomérations urbaines. Environnement, risques et santé. 2002;4(1):229–240. [Google Scholar]
- 6.Bessemoulin P, Bourdette N, Courtier P, Manach J. La canicule d’août 2003 en France et en Europe. La météorologie. 2004;46:25–33. [Google Scholar]
- 7.Braga AL, Zanobetti A, Schwartz J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ Health Perspect. 2002;110(9):859–63. doi: 10.1289/ehp.02110859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crawford VL, McCann M, Stout RW. Changes in seasonal deaths from myocardial infarction. Qjm. 2003;96(1):45–52. doi: 10.1093/qjmed/hcg005. [DOI] [PubMed] [Google Scholar]
- 9.Dessai S. Heat stress and mortality in Lisbon part I. model construction and validation. Int J Biometeorol. 2002;47(1):6–12. doi: 10.1007/s00484-002-0143-1. [DOI] [PubMed] [Google Scholar]
- 10.Ellis FP, Nelson F. Mortality in the elderly in a heat wave in New York City, August 1975. Environ Res. 1978;15(3):504–12. doi: 10.1016/0013-9351(78)90129-9. [DOI] [PubMed] [Google Scholar]
- 11.Ellis FP, Prince HP, Lovatt G, Whittington RM. Mortality and morbidity in Birmingham during the 1976 heatwave. Q J Med. 1980;49(193):1–8. [PubMed] [Google Scholar]
- 12.Fouillet A, Rey G, Laurent F, et al. Excess mortality related to the August 2003 heat wave in France. Int Arch Occup Environ Health. 2006;80(1):16–24. doi: 10.1007/s00420-006-0089-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grize L, Huss A, Thommen O, Schindler C, Braun-Fahrlander C. Heat wave 2003 and mortality in Switzerland. Swiss Med Wkly. 2005;135(13–14):200–5. doi: 10.4414/smw.2005.11009. [DOI] [PubMed] [Google Scholar]
- 14.Hales S, Salmond C, Town GI, Kjellstrom T, Woodward A. Daily mortality in relation to weather and air pollution in Christchurch, New Zealand. Aust N Z J Public Health. 2000;24(1):89–91. doi: 10.1111/j.1467-842x.2000.tb00731.x. [DOI] [PubMed] [Google Scholar]
- 15.Henschel A, Burton LL, Margolies L, Smith JE. An analysis of the heat deaths in St. Louis during July, 1966. Am J Public Health Nations Health. 1969;59(12):2232–42. doi: 10.2105/ajph.59.12.2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huynen MM, Martens P, Schram D, Weijenberg MP, Kunst AE. The impact of heat waves and cold spells on mortality rates in the Dutch population. Environ Health Perspect. 2001;109(5):463–70. doi: 10.1289/ehp.01109463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jougla E, Pavillon G, Rossollin F, De Smedt M, Bonte J. Improvement of the quality and comparability of causes-of-death statistics inside the European Community. EUROSTAT Task Force on “causes of death statistics”. Rev Epidemiol Sante Publique. 1998;46(6):447–56. [PubMed] [Google Scholar]
- 18.Katsouyanni K, Pantazopoulou A, Touloumi G, et al. Evidence for interaction between air pollution and high temperature in the causation of excess mortality. Arch Environ Health. 1993;48(4):235–42. doi: 10.1080/00039896.1993.9940365. [DOI] [PubMed] [Google Scholar]
- 19.Larsen U. The effects of monthly temperature fluctuations on mortality in the United States from 1921 to 1985. Int J Biometeorol. 1990;34(3):136–45. doi: 10.1007/BF01048710. [DOI] [PubMed] [Google Scholar]
- 20.Michelozzi P, de Donate F, Bisanti L, et al. The impact of the summer 2003 heat waves on mortality in four Italian cities. Euro Surveill. 2005;10(7) [PubMed] [Google Scholar]
- 21.Nakai S, Itoh T, Morimoto T. Deaths from heat-stroke in Japan: 1968–1994. Int J Biometeorol. 1999;43(3):124–7. doi: 10.1007/s004840050127. [DOI] [PubMed] [Google Scholar]
- 22.Naughton MP, Henderson A, Mirabelli MC, et al. Heat-related mortality during a 1999 heat wave in Chicago. Am J Prev Med. 2002;22(4):221–7. doi: 10.1016/s0749-3797(02)00421-x. [DOI] [PubMed] [Google Scholar]
- 23.Qiu D, Tanihata T, Aoyama H, et al. Relationship between a high mortality rate and extreme heat during the summer of 1999 in Hokkaido Prefecture, Japan. J Epidemiol. 2002;12(3):254–7. doi: 10.2188/jea.12.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Redelings MD, Sorvillo F, Simon P. A comparison of underlying cause and multiple causes of death: US vital statistics, 2000–2001. Epidemiology. 2006;17(1):100–3. doi: 10.1097/01.ede.0000187177.96138.c6. [DOI] [PubMed] [Google Scholar]
- 25.Robinson P. On the definition of a heat wave. J Appl Meteorol. 2000;40(4):762–75. [Google Scholar]
- 26.Rooney C, McMichael AJ, Kovats RS, Coleman MP. Excess mortality in England and Wales, and in Greater London, during the 1995 heatwave. J Epidemiol Community Health. 1998;52(8):482–6. doi: 10.1136/jech.52.8.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sartor F, Snacken R, Demuth C, Walckiers D. Temperature, ambient ozone levels, and mortality during summer 1994, in Belgium. Environ Res. 1995;70(2):105–13. doi: 10.1006/enrs.1995.1054. [DOI] [PubMed] [Google Scholar]
- 28.Schuman SH. Patterns of urban heat-wave deaths and implications for prevention: data from New York and St. Louis during July, 1966. Environ Res. 1972;5(1):59–75. doi: 10.1016/0013-9351(72)90020-5. [DOI] [PubMed] [Google Scholar]
- 29.Semenza JC, McCullough JE, Flanders WD, McGeehin MA, Lumpkin JR. Excess hospital admissions during the July 1995 heat wave in Chicago. Am J Prev Med. 1999;16(4):269–77. doi: 10.1016/s0749-3797(99)00025-2. [DOI] [PubMed] [Google Scholar]
- 30.Sharma HS. Heat-related deaths are largely due to brain damage. Indian J Med Res. 2005;121(5):621–3. [PubMed] [Google Scholar]
- 31.Shen T, Howe HL, Alo C, Moolenaar RL. Toward a broader definition of heat-related death: comparison of mortality estimates from medical examiners’ classification with those from total death differentials during the July 1995 heat wave in Chicago, Illinois. Am J Forensic Med Pathol. 1998;19(2):113–8. doi: 10.1097/00000433-199806000-00003. [DOI] [PubMed] [Google Scholar]
- 32.Smoyer KE. Putting risk in its place: methodological considerations for investigating extreme event health risk. Soc Sci Med. 1998;47(11):1809–24. doi: 10.1016/s0277-9536(98)00237-8. [DOI] [PubMed] [Google Scholar]
- 33.Weisskopf MG, Anderson HA, Foldy S, et al. Heat wave morbidity and mortality, Milwaukee, Wis, 1999 vs 1995: an improved response? Am J Public Health. 2002;92(5):830–3. doi: 10.2105/ajph.92.5.830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Whitman S, Good G, Donoghue ER, et al. Mortality in Chicago attributed to the July 1995 heat wave. Am J Public Health. 1997;87(9):1515–8. doi: 10.2105/ajph.87.9.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wolfe MI, Kaiser R, Naughton MP, et al. Heat-related mortality in selected United States cities, summer 1999. Am J Forensic Med Pathol. 2001;22(4):352–7. doi: 10.1097/00000433-200112000-00004. [DOI] [PubMed] [Google Scholar]
- 36.Zauli Sajani S, Garaffoni G, Goldoni CA, et al. Mortality and bioclimatic discomfort in Emilia-Romagna, Italy. J Epidemiol Community Health. 2002;56(7):536–7. doi: 10.1136/jech.56.7.536. [DOI] [PMC free article] [PubMed] [Google Scholar]


