Abstract
Objective: To determine the time to remission and recurrence in patients treated for acute mania and the predictive factors associated with these outcomes.
Method: This observational study, conducted in Turkey from April 2003 to January 2005, included patients with a DSM-IV diagnosis of bipolar I disorder, acute manic or mixed episode who were eligible to have an oral medication initiated or changed for the treatment of the episode. The patients were followed-up for 12 months.
Results: A total of 584 patients (mean ± SD age = 33.9 ± 11.2, 55.2% outpatients) were enrolled in 53 centers. Eighty-five percent of patients had a manic episode at baseline, with a mean ± SD duration of 21.6 ± 24.4 days. The baseline mean ± SD Clinical Global Impressions scale for use in bipolar disorder and Young Mania Rating Scale (YMRS) scores were 4.9 ± 0.9 (median = 5.0) and 33.2 ± 9.3 (median = 33), respectively. 539 patients achieved remission and, of those, 141 patients had recurrence. One-year remission and recurrence rates were 99.0% and 35.7%, respectively. Mean ± SD times to remission and recurrence in descriptive statistics were 80.9 ± 73.8 (median = 50) and 159.0 ± 95.5 (median = 156) days, respectively. In Cox regression analysis, psychiatric comorbidities (p = .048), a higher YMRS score (p < .001), and a higher number of previous depressive episodes (p = .009) were statistically significant predictors of a longer time to reach remission. Index episodes of longer duration (p = .033) and mixed type (p = 0.49) were significant predictors of a shorter time to recurrence. Confounding factors like concomitant treatment, comorbidities, and lack of blinding and randomization were other limitations.
Conclusion: Predictors for a longer time to remission were psychiatric comorbidities, a higher YMRS score, and a higher number of previous depressive episodes. Predictors for a shorter time to recurrence were episodes of longer duration and mixed type.
Bipolar disorder, occurring in 1.6% of the general population, results in distress, disability, suicide, and death and burdens relatives, caregivers, and society.1,2 Lithium has been shown to be effective for the treatment of acute manic episodes and for the long-term prevention of relapse3,4; however, a significant proportion of patients continue to experience relapse despite ongoing treatment.
In recent years, new treatment options for bipolar disorder, particularly for manic episodes, have been developed.5 These new medications include novel atypical antipsychotics and second- and third-generation anticonvulsants,6–10 with atypical antipsychotics being used increasingly for the treatment of acute bipolar mania.5,11,12
Despite the new treatment options for acute mania, data on their use and effects in daily clinical practice are limited, particularly regarding time to remission and recurrence and factors associated with these outcomes.13–16 Patients with mania exhibit extensive clinical variability, which is considered to have a substantial effect on prognosis.17,18 Yet because the strict patient selection criteria in clinical trials usually do not reflect this clinical variability, results of randomized clinical trials may not be generalized to all patients with acute mania.19 Information on the clinical course of bipolar disorder and manic episodes, focusing on time to remission and recurrence, will provide a valuable tool for incorporating the results of randomized clinical trials into daily practice and for planning and evaluating the health outcome results of treatment.
We conducted an observational, prospective, multicen-ter study in Turkey from April 2003 to January 2005 to determine the time to remission and recurrence after the treatment of a manic or mixed episode in inpatients and outpatients with bipolar disorder in a clinical setting. We also examined predictive factors associated with a longer time to remission and a shorter time to recurrence.
METHOD
Patients
Patients of at least 18 years of age with a Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnosis of bipolar I disorder who, in clinical practice, were eligible to have an oral medication started or changed for the treatment of an acute manic or mixed episode were entered in the study. Pregnant or breastfeeding women, patients who were participating in another study that included treatment intervention and/or an investigational drug, and patients who had initiated or changed an oral medication for the treatment of a manic or mixed episode before the first assessment for the study were excluded from the study. All patients or their legal representatives gave oral consent before entering the study. The Central Ethics Committee of the Ministry of Health approved the protocol, and the study was conducted according to local regulations.
Treatment
Because the study was designed as a noninterventional, observational study, all medication given to patients during the study period was determined solely at the discretion of the treating psychiatrists.
There were no study-specific procedures, and the investigator's decision regarding treatment and care of the patient was made during the course of normal clinical practice, separate from data collection or any other aspect of the study. All of the treatment decisions such as initiation, change, or discontinuation of a medication were determined by the clinicians themselves, according to the clinical course of the disease. Change of medication therapy or discontinuation of medication after the baseline observation was not a criterion for study discontinuation.
Study Assessments
Data collection for the study occurred during the visits within the normal course of therapy. The patients were followed-up for 12 months, with visits performed approximately every 4 months (± 1–3 months). Additionally, patients were evaluated at the time of discharge and at the time of remission (remission visit) for inpatients, and at the time of remission and the first recurrence after remission (recurrence visit) for outpatients. Remission and recurrence visits had to be completed by the investigators when the patient met the a priori-defined criteria of remission and recurrence. The study was divided into 2 theoretical periods for the purpose of analysis; the first period started at the initial visit and ended at the remission visit, and the second period started at the remission visit and continued until the last observation visit—including any possible recurrence visit.
During the initial visit, sociodemographics and psychiatric history of the patients and characteristics of the current episode were recorded. Details of oral medication given or changed were recorded during the study. Based on the patient's and caregiver's reports, compliance with medication since last visit was evaluated using an explicit question with 4 possible answers (almost always, half of the time, almost never, never compliant). The Clinical Global Impressions scale for use in bipolar illness (CGI-BP)20 was used to quantify manic and depressive symptoms and to determine the recurrence of manic/mixed episodes. The CGI-BP severity scores range from 1 to 7, with 1 being normal/not at all ill and 7 being the most severely ill. The CGI-BP item 2 was used to make global assessment of improvement during treatment compared to baseline. The Young Mania Rating Scale (YMRS)21 was used to quantify the severity of mania in patients with bipolar disorder and to determine remission time. Definitions of remission and recurrence were defined a priori as a total YMRS score ≤ 12 and CGI-BP mania score ≥ 3 or CGI-BP depression score ≥ 3, respectively. The reliability and validity of the Turkish version of the YMRS has been demonstrated.22 Before the study, investigators were trained in YMRS administration. First, a fictitious patient film was rated together with investigators and experts in bipolar disorder. A second video film was rated individually by each investigator. A high correlation between investigators regarding YMRS scores was found (r = 0.78). The level of agreement between the investigators' and experts' ratings of the video film was also high (r = 0.90).
Statistical Analyses
All study data, including time to remission and recurrence, were summarized using descriptive statistics (e.g., mean, median, standard deviation, frequency, and percentage). The mean values were given as mean ± SD. The cumulative probabilities of remission and recurrence were calculated using Kaplan-Meier analysis, and the curves were compared using the log-rank test. Cox regression analysis, using the method of backward likelihood ratio, was performed to identify the following independent predictive factors for the dependent variables of longer time to remission and shorter time to recurrence: age; sex (male vs. female); presence of psychiatric comorbidities (yes vs. no); type of index episode (manic/mixed, first/multiple, and with psychotic/nonpsychotic features); duration of index episode; the number of past manic, mixed, and depressive episodes; treatment with olanzapine (patients treated with olanzapine at least 50% of the days until remission with or without adjunctive therapy vs. patients who were not given olanzapine until remission); and baseline YMRS score. For all tests, the level of significance was .05.
RESULTS
Baseline Characteristics of Patients and Current Episode
A total of 584 patients (51.3% were male; mean ± SD age = 33.9 ± 11.2), of which 55.2% were outpatients, were enrolled in 53 centers from 7 different regions of Turkey from April 2003 to January 2005. The numbers of patients who attended visits 2, 3, and 4 were 508, 516, and 502, respectively. Of the 584 patients enrolled, 17.8% had a psychiatric comorbidity in addition to bipolar disorder. The most frequent comorbidities (with ≥ 10%) were generalized anxiety disorder (33.7%), panic disorder (18.3%), obsessive-compulsive disorder (16.3%), attention-deficit/hyperactivity disorder (14.4%), eating disorders (10.6%), and social phobia (10.6%).
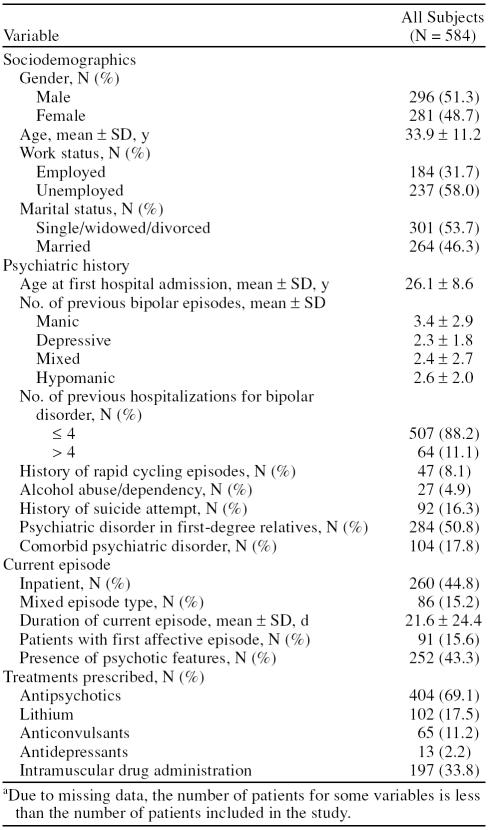
Regarding current episodes, 84.8% of patients had a manic episode and 15.2% had a mixed episode. The mean ± SD duration of the episode was 21.6 ± 24.4 days. Ninety-one patients (15.6%) were recorded as having their first bipolar episode, whereas 84.4% had a mean ± SD number of 3.4 ± 2.9 previous manic, 2.3 ± 1.8 previous depressive, and 2.4 ± 2.7 previous mixed episodes. Psychotic features, which include delusions (false ideas about what is taking place or who one is) and hallucinations (seeing or hearing things that aren't there), were present in 43.3% of patients. The sociodemographics and psychiatric history of the patients and characteristics of the current episode are summarized in Table 1.
Table 1.
Sociodemographics, Psychiatric History, Current Episode Characteristics, and Treatments Prescribed in the First Visit (N = 584)a
The mean ± SD CGI-BP score of patients was 4.9 ± 0.9 (median = 5.0) and the mean ± SD total YMRS score was 33.2 ± 9.3 (median = 33) at baseline. The severity of the index episode ranged from moderate to severely ill (CGI-BP score ≥ 5) in 94.5% of patients.
Drug Treatment
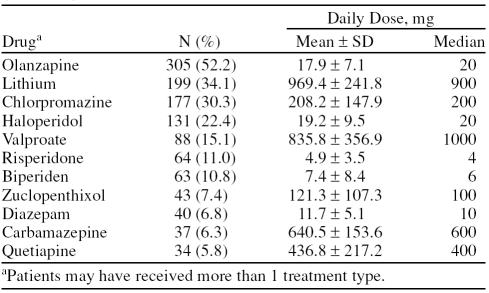
Classes of medication prescribed in the first visit (post-baseline) are summarized in Table 1. Forty-four percent of patients were given other treatments including anticholinergics (28.6%), anxiolytics/hypnotics (19.0%), and antihistaminics (1.7%). Intramuscular drugs were administered in 33.8% of patients (Table 1). The most commonly prescribed oral drugs at the first visit for the treatment of the current episode were olanzapine (52.2%), lithium (34.1%), chlorpromazine (30.3%), and haloperidol (22.4%) (Table 2). The rate of reported noncompliance with prescribed medication (almost never or never compliant) ranged from 0.8% to 12.4% during the study. The rate of noncompliance in relapsed patients was similar to the overall sample (12.4%).
Table 2.
Drugs Prescribed to Patients at the First Visit (N = 584)
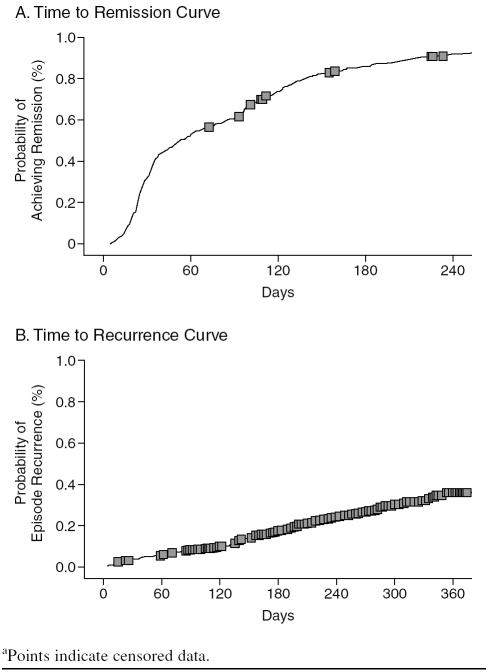
Time to Remission
A total of 539 patients achieved remission in a mean ± SD time of 80.9 ± 73.8 days after the initiation or change of an oral medication; the median time to reach remission criteria was 50 days. The Kaplan-Meier curve for remission is presented in Figure 1A. Ninety-one percent of patients were found to be normal or minimally ill (CGI-BP severity score of 1 or 2) at the remission visit. Of the 539 patients, 92.5% were rated as much or very much improved at the remission visit according to the CGI-BP item 2 (change from baseline). The mean ± SD total YMRS score at the remission visit was 5.2 ± 3.6 (median = 5). Cumulative probabilities of remission by months 3, 6, 9, and 12 were 60.6%, 86.2%, 94.0%, and 99.0%, respectively.
Figure 1.
Kaplan-Meier Curves for Cumulative (A) Remission and (B) Recurrence Rates for the Patients Who Achieved Remission (N = 539) Over 12 Monthsa
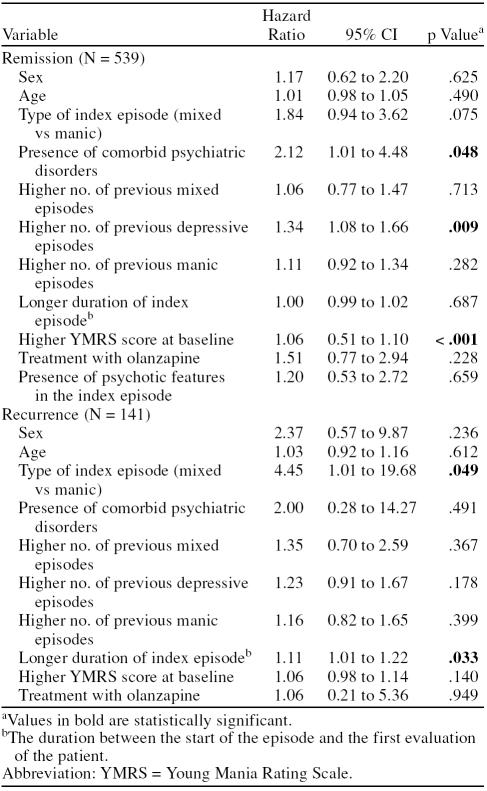
In Cox regression analysis, the presence of psychiatric comorbidities (hazard ratio [HR] = 2.12, 95% confidence interval [CI] = 1.01 to 4.48), a higher baseline YMRS score (HR = 1.06, 95% CI = 0.51 to 1.10), and a higher number of previous depressive episodes (HR = 1.34, 95% CI = 1.08 to 1.66) were found to be statistically significant predictors for a longer time to achieve remission (Table 3).
Table 3.
Independent Variables Associated With a Longer Time to Remission or Shorter Time to Recurrence in Cox Regression Analysis
Time to Recurrence
Of the 539 patients who achieved remission, 141 experienced recurrence of a manic episode within the 1-year observation period, and the mean ± SD time to recurrence was 159.0 ± 95.5 days (median = 156 days). The Kaplan-Meier curve for recurrence is presented in Figure 1B. Of the patients who had recurrence, 71.5% were outpatients. The majority of patients (63.4%) were moderately or severely ill (CGP-BP severity score ≥ 5) at the recurrence visit. The mean ± SD CGI-BP severity score was 3.84 ± 1.22. The types of recurrence were manic (50.0% of patients), mixed (19.6% of patients), depressive (19.6% of patients), and hypomanic (10.9% of patients). Psychotic symptoms were present in 68.3% of the recurrences. The most commonly prescribed drugs after the recurrence visit were olanzapine (19.9%), lithium (16.2%), and chlorpromazine (11.8%). Cumulative probabilities of recurrence by months 3, 6, 9, and 12 were 3.5%, 7.7%, 25.7%, and 35.7%, respectively.
In a Cox regression analysis for recurrence, index episodes of a longer duration and mixed type were found to be predictors for a shorter time to manic or depressive recurrence (HR = 1.11, 95% CI = 1.01 to 1.22 and HR = 4.45, 95% CI = 1.01 to 19.68, respectively) (Table 3).
DISCUSSION
In this observational study, we explored the time to remission and recurrence after the treatment of a manic episode in both inpatients and outpatients with bipolar disorder. The course of remission from a manic episode can be unpredictable due to high clinical variability in patients with mania.17,18 The short follow-up times of clinical trials prevent the assessment of time to remission and recurrence. Therefore, observational studies have a particular importance for the evaluation of time to remission and recurrence in daily clinical practice. The observational study design and limited patient selection criteria of our study enabled us to recruit patients who were representative of the general population of patients with acute mania and to follow up with them in daily practice, while avoiding the strict selection, treatment, and follow-up guidelines used in randomized clinical trials.19
Limitations of the study were exclusion of patients who were not treated, had no change in treatment, or had a change in treatment before the first evaluation of the study, since only patients who initiated or changed an oral medication were enrolled. Because psychiatrists initiate or change the medication for most patients with acute mania during the course of daily practice, however, this limitation does not affect the generalizability of our study population. Other limitations of the study were polypharmacy and comorbidities, both of which are the results of the naturalistic and observational design of the study and are almost always present in patients with bipolar disorder.23,24 Measuring blood levels or using a valid compliance questionnaire might be a more precise method for assessing compliance in the treatment groups; however, no difference was found in compliance among treatment groups in this study.
Bromet et al.16 determined the time to remission in 123 psychotic first admission patients with bipolar disorder (74% of them were manic) in epidemiologically defined samples followed for 4 years. They found that 74.8% of patients achieved remission by 1 year, and 83.7% by 4 years. In another study by Tohen et al.,25 the 2-year remission rate of a manic or mixed episode after the first hospitalization was 72.0%. The remission rate of our study population was higher by 1 year (99.0%) than the previously reported rates, which may be the result of different remission criteria than those of the previous studies. Bromet et al.16 studied remissions lasting at least 2 months, and Tohen et al.25 described symptomatic remission as a YMRS score ≤ 5, whereas our criteria for remission was a total YMRS score ≤ 12. Median time to recovery was reported 2 weeks shorter (5.3 weeks) in a Dutch case register study that included only hospitalized patients. This disparity may arise from methodological differences between studies (e.g., definition of recovery/remission, visit intervals) and/or characteristics of the patients in the sample (e.g., inpatient-outpatient status, treatment patterns, comorbidities).
We found that the presence of psychiatric comorbidities, a higher baseline YMRS score, and a higher number of previous depressive episodes were statistically significant predictors for a longer time to remission. These predictive factors differ slightly from those of previous studies. In previous studies, younger age at onset, history of childhood psychopathology, higher Brief Psychiatric Rating Scale (BPRS) anxiety/depression scores,16 male sex, longer hospitalization time, and high initial depression ratings15 were significantly associated with a longer time to remission. Contrary to the findings of Tohen et al.,15 we did not find that gender was a predictive factor for late remission. The predictive value of higher YMRS scores at baseline for late remission is a finding, relevant with the clinical observations. Kessing26 reported factors affecting remission rates in bipolar patients from a Dutch case register; patients with severe mania and with accompanying psychotic features were found to take longer to reach remission than the patients with mild or moderate forms of mania. In a previous analysis of the register, younger age, longer previous episodes, and female gender were also found to be associated with slower rate of recovery.27
Recurrence of the disorder occurred in 35.7% of patients by 1 year, which is a similar recurrence rate to that of previous studies. A prospective, naturalistic, lithium follow-up study examining recurrence after recovery13 reported cumulative recurrence risks of 24% by the first 6 months and 43% by 1 year. Within 2 years, 40% of patients had experienced a new episode of mania after the first episode in the study by Tohen et al.15 Bromet et al.16 found recurrence in 35.9% of patients within 1 year and Saka et al.28 in 31.2% of patients within 1 year.
Consistent to the findings of previous studies, our data show that index episodes of a longer duration and mixed type were significant risk factors for a shorter time to recurrence. In previous studies, childhood internalizing-type problems, higher BPRS anxiety/depression and Hamilton Rating Scale for Depression scores, an admission episode not involving mania,16 initial mood-congruent psychosis, lower premorbid occupational status, initial manic presentation,15 and number of past episodes29 were associated with a shorter time to recurrence. In our study, although statistically insignificant, female sex and the presence of psychiatric comorbidities were risk factors for a shorter time to recurrence with high hazard ratios (HR = 2.37, 95% CI = 0.57 to 9.87 and HR = 2.00, 95% CI = 0.28 to 14.27, respectively).
In conclusion, in this large observational study, the median time to remission and recurrence after the treatment of a manic episode was 50 and 156 days, respectively. Factors associated with a longer time to achieve remission such as the presence of psychiatric comorbidities, high baseline YMRS score, and higher number of previous depressive episodes and factors associated with a shorter time to recurrence such as episodes of longer duration and mixed type might be taken into account when treating manic patients in acute and maintenance phases. These data on remission and recurrence patterns in bipolar disorder may provide opportunities to develop new alternatives for medication, which should primarily focus on difficult issues like depressive symptomatology, mixed states, and psychotic features. Additionally, efforts to reveal factors associated with remission and recurrence will yield benefit in areas that have vital importance for bipolar patients such as adherence and social and occupational functionality. Many other potential variables that were not investigated in this study, such as adherence to medication or treatment and neurobiological factors, may constitute focal points for future studies.
Drug names: biperiden (Akineton), carbamazepine (Carbatrol, Equetro, and others), chlorpromazine (Thorazine, Sonazine, and others), diazepam (Diastat, Valium, and others), haloperidol (Haldol and others), lithium (Eskalith, Lithobid, and others), olanzapine (Zyprexa), quetiapine (Seroquel), risperidone (Risperdal).
Footnotes
Funding for this study was provided by Eli Lilly and Co.
The authors acknowledge Selda Emre-Aydingoz, M.D., Ph.D., E.L.S. (funded by Eli Lilly and Co. through Omega CRO) as a medical writer for drafting the manuscript and Ayca Aptik, M.Sc. (Eli Lilly and Co.) and Seniz Pekmen, M.Sc. (Eli Lilly and Co.) for their assistance in the preparation of this manuscript.
Dr. Saylan is an employee of Eli Lilly. Dr. Oral has received grant/research support from Eli Lilly, AstraZeneca, and Pfizer; has received honoraria from Eli Lilly, AstraZeneca, Janssen, and Lundbeck; and has participated in speakers/advisory boards for Eli Lilly, AstraZeneca, Pfizer, Lundbeck, Janssen, and Bristol-Myers Squibb. Drs. Kora, Akkaya, Karamustafalioglu, Tomruk, and Yasan report no additional financial or other relationships relevant to the subject of this article.
REFERENCES
- Kessler RC, McGonagle KA, and Zhao S. et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994 51:8–19. [DOI] [PubMed] [Google Scholar]
- Woods SW. The economic burden of bipolar disease. J Clin Psychiatry. 2000 61suppl 13. 38–41. [PubMed] [Google Scholar]
- Bowden CL. Clinical correlates of therapeutic response in bipolar disorder. J Affect Disord. 2001;67(1–3):257–265. doi: 10.1016/s0165-0327(98)00160-8. [DOI] [PubMed] [Google Scholar]
- Baldessarini RJ, Tondo L, and Hennen J. et al. Is lithium still worth using?: an update of selected recent research. Harv Rev Psychiatry. 2002 10:59–75. [PubMed] [Google Scholar]
- Mensink GJ, Slooff CJ. Novel antipsychotics in bipolar and schizoaffective mania. Acta Psychiatr Scand. 2004;109:405–419. doi: 10.1111/j.1600-0047.2004.00295.x. [DOI] [PubMed] [Google Scholar]
- Bowden CL, Brugger AM, and Swann AC. et al. Efficacy of divalproex vs lithium and placebo in the treatment of mania: The Depakote Mania Study Group. JAMA. 1994 271:918–924. [PubMed] [Google Scholar]
- Bowden CL. Novel treatments for bipolar disorder. Expert Opin Investig Drugs. 2001;10:661–671. doi: 10.1517/13543784.10.4.661. [DOI] [PubMed] [Google Scholar]
- Yatham LN, Kusumakar V, and Calabrese JR. et al. Third generation anticonvulsants in bipolar disorder: a review of efficacy and summary of clinical recommendations. J Clin Psychiatry. 2002 63:275–283. [DOI] [PubMed] [Google Scholar]
- Yatham LN. The role of novel antipsychotics in bipolar disorders. J Clin Psychiatry. 2002 63suppl 3. 10–14. [PubMed] [Google Scholar]
- Calabrese JR, Shelton MD, and Rapport DJ. et al. Bipolar disorders and the effectiveness of novel anticonvulsants. J Clin Psychiatry. 2002 63suppl 3. 5–9. [PubMed] [Google Scholar]
- Sachs GS, Grossman F, and Ghaemi SN. et al. Combination of a mood stabilizer with risperidone or haloperidol for treatment of acute mania: a double-blind, placebo-controlled comparison of efficacy and safety. Am J Psychiatry. 2002 159:1146–1154. [DOI] [PubMed] [Google Scholar]
- Sajatovic M, Brescan DW, and Perez DE. et al. Quetiapine alone and added to a mood stabilizer for serious mood disorders. J Clin Psychiatry. 2001 62:728–732. [DOI] [PubMed] [Google Scholar]
- Coryell W, Endicott J, and Maser JD. et al. The likelihood of recurrence in bipolar affective disorder: the importance of episode recency. J Affect Disord. 1995 33:201–206. [DOI] [PubMed] [Google Scholar]
- Suppes T, Dennehy EB, and Gibbons EW. The longitudinal course of bipolar disorder. J Clin Psychiatry. 2000 61suppl 9. 23–30. [PubMed] [Google Scholar]
- Tohen M, Zarate CA JR, and Hennen J. et al. The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence. Am J Psychiatry. 2003 160:2099–2107. [DOI] [PubMed] [Google Scholar]
- Bromet EJ, Finch SJ, and Carlson GA. et al. Time to remission and relapse after the first hospital admission in severe bipolar disorder. Soc Psychiatry Psychiatr Epidemiol. 2005 40:106–113. [DOI] [PubMed] [Google Scholar]
- Geddes J, Goodwin G. Bipolar disorder: clinical uncertainty, evidence-based medicine and large-scale randomised trials. Br J Psychiatry Suppl. 2001;41:S191–S194. [PubMed] [Google Scholar]
- Krabbendam L, Myin-Germeys I, and De Graaf R. et al. Dimensions of depression, mania, and psychosis in the general population. Psychol Med. 2004 34:1117–1186. [DOI] [PubMed] [Google Scholar]
- Storosum JG, Fouwels A, and Gispen-de Wied CC. et al. How real are patients in placebo-controlled studies of acute manic episode? Eur Neuropsychopharmacol. 2004 14:319–323. [DOI] [PubMed] [Google Scholar]
- Spearing MK, Post RM, and Leverich GS. et al. Modification of the Clinical Global Impressions (CGI) scale for use in bipolar illness (BP): the CGI-BP. Psychiatry Res. 1997 73(3):159–171. [DOI] [PubMed] [Google Scholar]
- Young RC, Biggs JT, and Ziegler VE. et al. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978 133:429–435. [DOI] [PubMed] [Google Scholar]
- Karadag F, Oral T, and Yalcin FA. et al. Young Mani Derecelendirme Olceginin Turkiye'de gecerlilik ve guvenilirligi [Reliability and Validity of Turkish Translation of Young Mania Rating Scale]. Turk Psikiyatri Derg. 2002 13:107–114. [PubMed] [Google Scholar]
- Kupfer DJ, Frank E, and Grochocinski VJ. et al. Demographic and clinical characteristics of individuals in a bipolar disorder case registry. J Clin Psychiatry. 2002 63(2):120–125. [DOI] [PubMed] [Google Scholar]
- Lin D, Mok H, Yatham LN. Polytherapy in bipolar disorder. CNS Drugs. 2006;20(1):29–42. doi: 10.2165/00023210-200620010-00003. [DOI] [PubMed] [Google Scholar]
- Tohen M, Ketter TA, and Zarate CA. et al. Olanzapine versus divalproex sodium for the treatment of acute mania and maintenance of remission: a 47-week study. Am J Psychiatry. 2003 160:1263–1271. [DOI] [PubMed] [Google Scholar]
- Kessing LV. Subtypes of manic episodes according to ICD-10-prediction of time to remission and risk of relapse. J Affect Disord. 2004;81(3):279–285. doi: 10.1016/S0165-0327(03)00191-5. [DOI] [PubMed] [Google Scholar]
- Kessing LV, Mortensen PB. Recovery from episodes during the course of affective disorder: a case-register study. Acta Psychiatr Scand. 1999;100(4):279–287. doi: 10.1111/j.1600-0447.1999.tb10862.x. [DOI] [PubMed] [Google Scholar]
- Saka MC, Ozer S, Ulusahin A. Bipolar bozukluk bir yillik izlem calismasi [Bipolar disorder: one year follow up] Turk Psikiyatri Derg. 2001;12:282–292. [Google Scholar]
- Kessing LV, Hansen MG, Andersen PK. Course of illness in depressive and bipolar disorders. Br J Psychiatry. 2004;185:372–377. doi: 10.1192/bjp.185.5.372. [DOI] [PubMed] [Google Scholar]