Abstract
Objective: Chronic fatigue syndrome (CFS) is characterized by profound, debilitating fatigue and a combination of several other symptoms resulting in substantial reduction in occupational, personal, social, and educational status. CFS is often misdiagnosed as depression. The objective of this study was to evaluate and discuss different etiologies, approaches, and management strategies of CFS and to present ways to differentiate it from the fatigue symptom of depression.
Data Sources: A MEDLINE search was conducted to identify existing information about CFS and depression using the headings chronic fatigue syndrome AND depression. The alternative terms major depressive disorder and mood disorder were also searched in conjunction with the term chronic fatigue syndrome. Additionally, MEDLINE was searched using the term chronic fatigue. All searches were limited to articles published within the last 10 years, in English. A total of 302 articles were identified by these searches. Also, the term chronic fatigue syndrome was searched by itself. This search was limited to articles published within the last 5 years, in English, and resulted in an additional 460 articles. Additional publications were identified by manually searching the reference lists of the articles from both searches.
Study Selection and Data Extraction: CFS definitions, etiologies, differential diagnoses (especially depression) and management strategies were extracted, reviewed, and summarized to meet the objectives of this article.
Data Synthesis: CFS is underdiagnosed in more than 80% of the people who have it; at the same time, it is often misdiagnosed as depression. Genetic, immunologic, infectious, metabolic, and neurologic etiologies were suggested to explain CFS. A biopsychosocial model was suggested for evaluating, managing, and differentiating CFS from depression.
Conclusions: Evaluating and managing chronic fatigue is a challenging situation for physicians, as it is a challenging and difficult condition for patients. A biopsychosocial approach in the evaluation and management is recommended. More studies about CFS manifestations, evaluation, and management are needed.
“She is depressed,” her physician wrote when referring Ms. A, a 65-year-old married woman, for a psychiatric consult. “She has been feeling tired for more than a year and described being exhausted most of the time, with headaches, joint pain, and problems with her concentration and memory. Her fatigue is frustrating for her and for her family; she cannot function well even in the morning. She denied being depressed, and does not have any previous mental or medical illnesses. Every lab I checked was normal. I still think that she is hiding her depression and manifesting it with all these somatic complaints.”
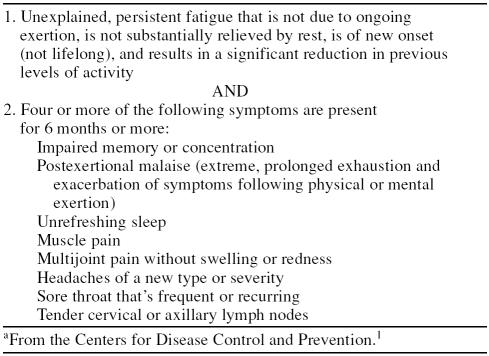
Prolonged fatigue is defined as self-reported, persistent fatigue of 1 month or longer.1 Chronic fatigue syndrome (previously known as myalgic encephalomyelitis2 or neurasthenia3) is characterized by profound, debilitating fatigue and a combination of symptoms resulting in substantial reduction in occupational, personal, social, and educational status1,2,4–7 (see Table 1). Diagnosis of the chronic fatigue syndrome (CFS) can be made only after alternate medical and psychiatric causes of chronic fatiguing illness have been excluded.
Table 1.
Chronic Fatigue Syndrome Criteriaa
At least 1 million Americans have CFS,1,8 more than have lung cancer or multiple sclerosis; yet more than 80% go undiagnosed. In the primary care setting, the prevalence of CFS ranges from 3% to 20% and from 80% to 90% at the end of life.9,10 There are no ethnic or racial differences. Previous reports have mentioned a female:male ratio of 1.3:1,6 but a recent report by the U.S. Centers for Disease Control and Prevention (CDC) showed a female:male ratio of 4:1. It occurs most often in the 40- to 59-year age group and in the geriatric population.1,9,10
Although the concept of neurasthenia was introduced in 1869 by George Miller Beard,3 CFS was defined in 1988 by the CDC, and while more than 3000 research studies have been done in this field, there is still some debate about the existence of this syndrome.1,11,12 The uncertainty about its existence and the lack of a specific laboratory test or marker to identify it, associated with hesitancy about making a diagnosis without knowing exactly how to treat it, all act as barriers to the diagnosis and treatment of CFS by primary care practitioners and psychiatrists.
Unlike the uncertainty about its existence, there is strong certainty about the impact of CFS. CFS patients, by definition, are functionally impaired and as disabled as patients with multiple sclerosis, heart disease, end-stage renal disease, and similar chronic conditions. The annual economic impact of CFS in the United States is estimated to be $9.1 billion in lost productivity.1
DATA SOURCES
A MEDLINE search was conducted to identify existing information about CFS and depression using the headings chronic fatigue syndrome AND depression. The alternative terms major depressive disorder and mood disorder were also searched in conjunction with the term chronic fatigue syndrome. Additionally, MEDLINE was searched using the term chronic fatigue. All searches were limited to articles published within the last 10 years, in English. A total of 302 articles were identified by these searches. Also, the term chronic fatigue syndrome was searched by itself. This search was limited to articles published within the last 5 years, in English, and resulted in an additional 460 articles. Additional publications were identified by manually searching the reference lists of the articles from both searches.
FATIGUE ETIOLOGIES
CFS cannot be considered either physical or psychological but instead requires a biopsychosocial approach to the illness. Numerous studies have tried to pinpoint specific etiologies by considering the following fields.
Genetic Etiologies
CFS is sometimes seen in members of the same family,13,14 but there is no evidence that it is contagious; instead, there may be a familial predisposition or a genetic link. The concordance rate was higher in monozygotic than in dizygotic female twins for chronic fatigue.15 Hickie et al.16 evaluated genetic and environmental determinants of prolonged fatigue in a twin study and found 44% (95% CI = 25% to 60%) of the genetic variance for fatigue was not shared by the other forms of psychological distress, and also found that environmental factors made negligible contributions to fatigue. On the other hand, Cho et al.17 found evidence of a partly genetic influence, but environmental effects continued to be predominant. Clearly, further research is needed to explore these possible relationships.
Immunologic Etiologies
Abnormal natural killer cell cytotoxicity,18 increase immune activation markers,19 greater numbers of CD16+/CD3− natural killer cells,20 and the presence of interferon in serum and cerebrospinal fluid in CFS patients21 have been identified. Staines22 suggested the loss of immunologic tolerance to vasoactive neuropeptides or their receptors following infection, other events, or de novo as a mechanism.
Infectious Etiologies
Possible infectious etiologies have generated the most interest among CFS researchers. It has been postulated that chronic fatigue is a continuum ranging from cases with chronic viremia on the one hand to instances of frank psychiatric illness on the other.23 Multiple infectious agents have been linked to CFS, including Borna disease virus,24,25 parvovirus B19,26,27 glandular fever,28 Enterovirus,29 human herpesviruses 4, 6, and 7,30–32 infectious mononucleosis,33 Nipah virus encephalitis,34 and Q fever.35
Infections have not only played important etiologic roles, but also have been considered predictors of better prognoses when compared to noninfectious CFS cases.36 Human herpesvirus 6 reactivation has been suggested as an objective biomarker for fatigue.30
Endocrinology/Metabolism Etiologies
Hypothalamic-pituitary-adrenal (HPA) axis abnormalities have been studied as potential biological tests to diagnose CFS. Studies have shown HPA hypoactivity and higher chronic adrenocorticotropic hormone (ACTH) autoantibody levels as significant pathologic factors in CFS.37–39 Also reduced area under the ACTH response curve in CFS patients undergoing insulin tolerance test was significantly associated with the duration of CFS symptoms (r = −0.592, p = .005) and the severity of fatigue symptomatology.40 Other studies have suggested upregulation of hypothalamic 5-hydroxytryptamine receptors in patients with postviral fatigue syndrome but not in those with primary depression.41 However, another study showed no etiologic role for deficiency in central opioids or the HPA axis in the symptoms of CFS.42 Other biological factors have been investigated and considered as biological markers in CFS, including low magnesium level,43 low arachidonic acid level, low l-carnitine level,25 serum dehydroepiandrosterone (DHEA) sulfate deficiency,44 and impairments of the 2′,5′-oligoadenylate (2–5A) synthetase/RNase L pathway.45 Other studies showed no role of linoleic acid, eicosatrienoic acid (both p > .05),25 ferritin, vitamin B12, folate, or serum erythropoietin levels.46
Mental/Neurologic Etiologies
Psychosocial factors are frequently thought to contribute to fatigue. Rangel et al.13 found that CFS in childhood and adolescence is associated with higher levels of parental mental distress, emotional involvement, and family illness burden than those observed in association with juvenile rheumatoid arthritis, a chronic pediatric physical illness. Endicott14 described stressors including earlier mortality age and increased prevalence of cancer, autoimmune disorders, and CFS-like conditions in parents of psychiatric patients with CFS as compared to control groups. Thirty percent of the CFS patients and none of the controls reported dilemmas in the 3 months prior to the CFS onset in one study.47 History of abuse, particularly during childhood, may play a role in the development and perpetuation of chronic fatigue,48 and childhood trauma was associated with a 3- to 8-fold increased risk for CFS across different trauma types in one study.49 Sleep is also an interesting etiologic factor, as many patients with CFS have sleep disorders, and those with sleep disorders showed greater functional impairment independent of their psychiatric disorders.50–52
FATIGUE: DON'T ASSUME IT'S DEPRESSION
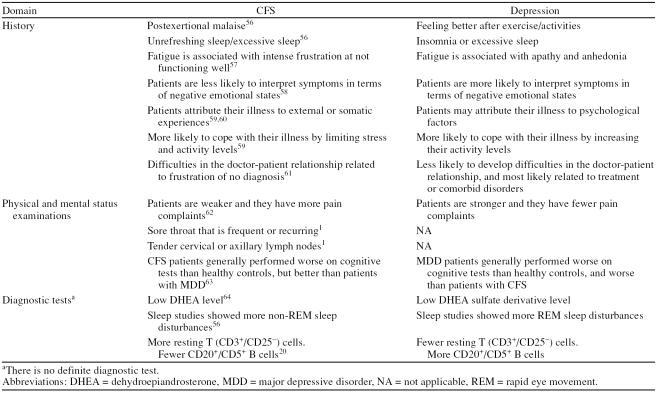
Fatigue is a part of a wide spectrum of diagnoses ranging from being a symptom in depression, anxiety, seasonal affective disorder,53 and multiple other diagnoses to being a full syndromal disorder in CFS, yet CFS goes undiagnosed in 80% of cases and is often misdiagnosed as depression. The Diagnostic and Statistical Manual of Mental Disorders doesn't list CFS as a diagnosis although the International Classification of Diseases, 10th Revision, does.12 In clinical practice, CFS presentations range from complicated cases associated with a psychotic state resulting in multiple murders in one case report54 to noncomplicated presentations with multiple psychiatric disorders, primarily depression.55 It is very important to understand the distinctive features between chronic fatigue and depressive disorder when evaluating a patient with a main complaint of fatigue. A full detailed history accompanied by questionnaire forms can be very helpful to differentiate CFS from major depressive disorder. There is still no specific test that can confidently differentiate between them. Multiple studies have tried to find distinctive factors and they are listed in Table 2.
Table 2.
Comparison Between Chronic Fatigue Syndrome (CFS) and Depression Across Different Studies
EVALUATION OF FATIGUE
Diagnosing CFS can be challenging for health care professionals for many reasons; the most important one is finding fatigue in a large number of illnesses and disorders. We reviewed information available about evaluation of chronic fatigue and discuss it in 3 parts: history, exam, and diagnostic tests.
History and Differentials
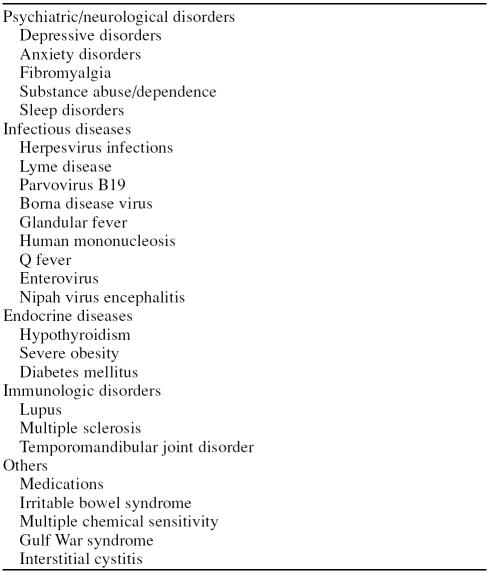
Because CFS is a diagnosis of exclusion,1 a full detailed history is considered essential. The history should include a detailed account of the symptoms, the associated disability, the choice of coping strategies, and importantly, the patient's own understanding of his/her illness.65 Every patient should be carefully evaluated for certain medical, psychiatric, and neurologic diseases that can cause fatigue as the most prominent symptom (Table 3). Two of the important differential diagnoses are depression and fibromyalgia. Although it is difficult to differentiate CFS from fibromyalgia confidently depending on the history or other reported differences of cognitive dysfunction components or clinical pain measures,66,67 CFS and fibromyalgia commonly co-occur within the concept of central sensitivity syndromes or functional somatic syndromes.68 This co-occurring increases functional impairment when compared to CFS individuals alone.69,70 Some of the distinguishing features between CFS and fibromyalgia include evidence for triggering viral infection and lower level of serum acylcarnitine observed in CFS patients, which is lacking in the majority of patients with fibromyalgia;71 slower information-processing in CFS patients compared to impaired control of attention in fibromyalgia patients;66 and lacking of the characteristic diffuse soft tissue pain and pain on palpation in at least 11 of 18 paired tender points in CFS patients.
Table 3.
Chronic Fatigue Syndrome Differential Diagnoses
Exam
Every CFS evaluation should include a mental status examination to identify abnormalities in mood, intellectual function, memory, and personality. Particular attention should be directed toward current symptoms of depressive, anxious, self-destructive thoughts and observable signs such as psychomotor retardation.1 Although there is no definite physical finding, a full and thorough physical examination may be helpful in excluding other conditions. Multiple studies have suggested dysautonomia with greater increase in heart rate together with a more pronounced systolic blood pressure fall on standing in CFS patients compared to healthy individuals.46,72 Other studies found no statistically significant differences in either heart rate or galvanic skin resistance both during a normal day and before, during, and after exercise testing.73
Tests
The CDC has recommended the following initial screening tests when evaluating patients with CFS: urinalysis, total protein, glucose, C-reactive protein, phosphorus, electrolyte, complete blood count with leukocyte differential, alkaline phosphatase, creatinine, blood urea nitrogen, albumin, antinuclear antibody and rheumatoid factor, globulin, calcium, alanine aminotransferase or aspartate transaminase serum level, and thyroid function tests (thyroid stimulating hormone and free T4).1 Further tests or referral to specialists may be indicated to confirm or exclude a diagnosis that better explains the fatigue state or to follow up on results of the initial screening tests.
Multiple other studies have tried to find biomarkers or radiological markers for CFS. Erythrocyte sedimentation rate was normal in all 23 CFS patients in one study.74 Another study found that concentrations of C-reactive protein, β2-microglobulin, and neopterin were higher in patients with CFS (p ≤ .01).75 On the other hand, a study by Swanink et al.76 found that complete blood cell count, serum chemistry panel, C-reactive protein, and serologic tests were not different in 88 patients with CFS when compared to a control group. A potential role for DHEA in CFS, both therapeutically and as a diagnostic tool, was suggested in one study.64
Magnetic resonance imaging studies have been inconsistent, with some of them suggesting larger ventricular volumes.77–84 Functional magnetic resonance was more promising, as it showed quantitative and qualitative differences in activation of the working memory network,85 attenuation of the responsiveness to stimuli not directly related to the fatigue-inducing tasks,86 utilization of more extensive regions of the network associated with the verbal working memory system,87 impaired functioning and reduced gray-matter volume in the bilateral prefrontal cortex,88 and inactive ventral anterior cingulate after making an error.89
Single-photon emission computed tomography (SPECT) and brain electrical activity mapping scans were promising in one study,90 and SPECT scans showed more abnormalities than did magnetic resonance scans in one study (p < .025).91 Siessmeier et al.92 detected abnormalities in 18-fluorodeoxyglucose positron emission tomography in approximately half the CFS patients examined, but found that no specific pattern for CFS could be identified. Positron emission tomography showed an alteration of the serotonergic system in the rostral anterior cingulate in one study, which was suggested as an etiology.93 Recently, Puri94 described the application of proton neurospectroscopy and 31-phosphorus neurospectroscopy in chronic fatigue syndrome. It is essential to mention that evidence to date does not support routine use of the imaging modalities discussed above in evaluating potential CFS patients.
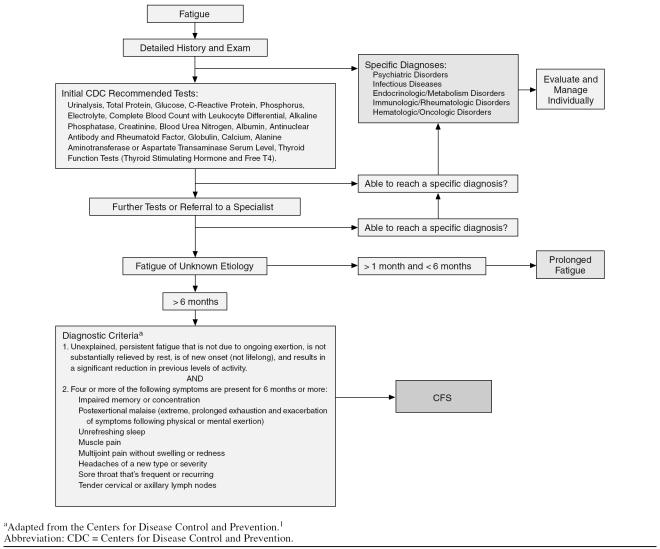
Finally, it is important to remember that a good history is more important than any available test to diagnose CFS and differentiate it from depression. The algorithm shown in Figure 1, which is based on the CDC recommendations and the results of the studies reviewed, is suggested for evaluating chronic fatigue.
Figure 1.
Algorithm for Evaluating Chronic Fatigue Syndrome (CFS)
MANAGEMENT OF FATIGUE
It is important to manage fatigue in the context of each patient suffering with it. Treatment of CFS, with its various major clinical and functional impacts, should be associated with a “biopsychosocial model” of management. Educating patients about their diagnoses is crucial. Physicians should emphasize distinction among factors that may have predisposed patients to develop, trigger, or perpetuate the illness.65 Progressive muscular rehabilitation, combined with behavioral and cognitive treatment, and appropriate choice of medications are essential parts of therapy.8
We will review the major concepts of CFS management and the evidence behind them.
Supportive and Symptomatic Treatment
Educating patients about CFS and validating their illness experience in addition to establishing a working alliance are the initial steps in the treatment.1,65 Direct the treatment toward the most problematic symptoms, as prioritized by the patient,1 and other illness-perpetuating factors.65 Encourage a well-balanced diet, and discuss with patients their nutritional habits. Advice about preventing over- and under-activity is essential. “Start low and go slow” is the correct advice for activities and exercise, the same as for using medications. Gear activities toward improving function in areas that are of greatest importance in achieving activities of daily living and remain open-minded about alternative therapies (electroacupuncture was helpful in one study95) and discuss them with your patients when appropriate.1 Consider referring or asking for consults and discuss that with patients early in the treatment.
Cognitive Behavioral Therapy
The short-term studies of cognitive behavioral therapy (CBT) in CFS have shown improvement in function and symptom management, especially in conjunction with other treatment modalities and in comparison to relaxation controls.96–99 Reports about good outcome following CBT ranged from 70%99 to none or even worsening of the symptoms.100 CBT was effective in treating symptoms of fatigue, mood, and physical fitness, but no improvement in cognitive function or quality of life was noticed in one study.101 Other studies showed limited effect on pain and fatigue.1 When treating CFS patients, the CBT therapist needs to be familiar with CFS, to be aware of the evidence for CFS as a biologically based disorder, and to validate the patient's experience of living with a misunderstood illness.
Exercise
CFS patients are very sensitive, and any treatment modality including exercise should start low and advance slowly. All exercises need to be followed by a rest period at a 1:3 ratio (i.e., 10 minutes of exercise: 30 minutes of rest). Review of the studies showed that exercise decreased the psychological stress102 and improved fatigue, functional capacity, and fitness significantly better than flexibility treatment,103 especially when associated with mood-enhancing, stress-reducing activities.104,105
Pharmacologic Treatment
Multiple studies have evaluated different treatment interventions, including recombinant erythropoietin, psychostimulants, corticosteroids, anti-inflammatory drugs, l-carnitine, and others.10,106 Antidepressants are the most common medications used in this regard; selegiline had a small but significant therapeutic effect independent of its antidepressant effect.107 Fluoxetine has been shown to improve overall symptoms and measures of immune function in one study,108 but failed in randomized, double-blind studies against placebo109 and graded exercise.110 Bupropion was effective for treatment of the fatigue and depressive symptoms associated with CFS in 9 fluoxetine-resistant patients111 and was also helpful in augmenting paroxetine in one case report.112 Venlafaxine was effective in 2 case reports.113 Moclobemide up to 600 mg a day for 6 weeks showed significant but small reductions in fatigue, depression, anxiety, and somatic amplification, as well as a modest overall improvement.114 Duloxetine may have a theoretical therapeutic benefit because of its characteristic of targeting pain. We could not find any study evaluating it in CFS patients. It is essential to mention that evidence to date does not support superiority of one medication over the others.
Other medications have been studied also. Clonidine enhanced both growth hormone (p = .028) and cortisol release (p = .021) and increased speed in the initial stage of a planning task (p = .023) only without affecting hormonal, physiologic, symptomatic, or neuropsychological measures.115 Low-dose hydrocortisone therapy caused increases in plasma leptin levels, with this biological response being more marked in those CFS subjects who showed a positive therapeutic response to hydrocortisone therapy.116 Essential fatty acid supplement rich in eicosapentaenoic acid was beneficial in a case report.117 Carnitine supplementation has been shown to reduce chronic inflammation and oxidative stress in hemodialysis patients and, in cancer patients, reduce fatigue and improve outcome.118 Treatment with modafinil was not beneficial in patients with CFS in one study.119
No therapeutic effects were found for natural killer cell stimulant,120 low-dose combination therapy of hydrocortisone and fludrocortisone,121 immunologic and antiviral substances, melatonin, or bright-light phototherapy.122
CONCLUSION
Evaluating and managing chronic fatigue is a challenging situation for physicians as it is a challenging and difficult condition for patients. A biopsychosocial approach in the evaluation and management is recommended. More studies about CFS manifestations, evaluation, and management are needed.
Drug names: bupropion (Wellbutrin and others), duloxetine (Cymbalta), clonidine (Catapres, Duraclon, and others), fluoxetine (Prozac and others), hydrocortisone (Cortef, Texacort, and others), modafinil (Provigil), paroxetine (Paxil, Pexeva, and others), selegiline (Eldepryl, Emsam, and others), venlafaxine (Effexor).
Footnotes
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
REFERENCES
- Centers for Disease Control and Prevention. Chronic Fatigue Syndrome. 26May2006 Available at: www.cdc.gov/cfs. Accessed Feb 3, 2007. [Google Scholar]
- Wessely S. The epidemiology of chronic fatigue syndrome. Epidemiol Rev. 1995;17:139–151. doi: 10.1093/oxfordjournals.epirev.a036170. [DOI] [PubMed] [Google Scholar]
- Schafer ML. On the history of the concept neurasthenia and its modern variants chronic fatigue syndrome, fibromyalgia, and multiple chemical sensitivities [in German] Fortschr Neurol Psychiatr. 2002;70(11):570–582. doi: 10.1055/s-2002-35174. [DOI] [PubMed] [Google Scholar]
- Holmes GP, Kaplan JE, and Gantz NM. et al. Chronic fatigue syndrome: a working case definition. Ann Intern Med. 1988 108:387–389. [DOI] [PubMed] [Google Scholar]
- Lloyd AR, Wakefield D, and Boughton C. et al. What is myalgic encephalomyelitis? Lancet. 1988 1:1286–1287. [DOI] [PubMed] [Google Scholar]
- Lloyd AR, Hickie I, and Boughton CR. et al. Prevalence of chronic fatigue syndrome in an Australian population. Med J Aust. 1990 153:522–528. [DOI] [PubMed] [Google Scholar]
- Sharpe MC, Archard LC, and Banatvala JE. et al. A report: chronic fatigue syndrome: guidelines for research. J R Soc Med. 1991 84:118–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maquet D, Demoulin C, Crielaard JM. Chronic fatigue syndrome: a systematic review. Ann Readapt Med Phys. 2006;49(6):337–347. 418–427. doi: 10.1016/j.annrmp.2006.03.011. [DOI] [PubMed] [Google Scholar]
- Lee S, Yu H, and Wing Y. et al. Psychiatric morbidity and illness experience of primary care patients with chronic fatigue in Hong Kong. Am J Psychiatry. 2000 157:380–384. [DOI] [PubMed] [Google Scholar]
- Davis MP, Khoshknabi D, Yue GH. Management of fatigue in cancer patients. Curr Pain Headache Rep. 2006;10(4):260–269. doi: 10.1007/s11916-006-0030-2. [DOI] [PubMed] [Google Scholar]
- Pearce JM. The enigma of chronic fatigue. Eur Neurol. 2006;56(1):31–36. doi: 10.1159/000095138. [DOI] [PubMed] [Google Scholar]
- Pichot P. Neurasthenia, yesterday and today [in French]. Encephale. 1994 20Spec No 3. 545–549. [PubMed] [Google Scholar]
- Rangel L, Garralda ME, and Jeffs J. et al. Family health and characteristics in chronic fatigue syndrome, juvenile rheumatoid arthritis, and emotional disorders of childhood. J Am Acad Child Adolesc Psychiatry. 2005 44(2):150–158. [DOI] [PubMed] [Google Scholar]
- Endicott NA. Chronic fatigue syndrome in private practice psychiatry: family history of physical and mental health. J Psychosom Res. 1999;47(4):343–354. doi: 10.1016/s0022-3999(99)00013-6. [DOI] [PubMed] [Google Scholar]
- Buchwald D, Herrell R, and Ashton S. et al. A twin study of chronic fatigue. Psychosom Med. 2001 63(6):936–943. [DOI] [PubMed] [Google Scholar]
- Hickie I, Kirk K, Martin N. Unique genetic and environmental determinants of prolonged fatigue: a twin study. Psychol Med. 1999;29(2):259–268. doi: 10.1017/s0033291798007934. [DOI] [PubMed] [Google Scholar]
- Cho HJ, Skowera A, and Cleare A. et al. Chronic fatigue syndrome: an update focusing on phenomenology and pathophysiology. Curr Opin Psychiatry. 2006 19(1):67–73. [DOI] [PubMed] [Google Scholar]
- Klimas NG, Salvato FR, and Morgan R. et al. Immunologic abnormalities in the chronic fatigue syndrome. J Clin Microbiol. 1990 28:1403–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landay AL, Jessop C, and Lennette ET. et al. Chronic fatigue syndrome: a clinical condition associated with immune activation. Lancet. 1991 338:707–712. [DOI] [PubMed] [Google Scholar]
- Robertson MJ, Schacterle RS, and Mackin GA. et al. Lymphocyte subset differences in patients with chronic fatigue syndrome, multiple sclerosis and major depression. Clin Exp Immunol. 2005 141(2):326–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd A, Hickie I, and Brockman A. et al. Cytokine levels in serum and cerebrospinal fluid in patients with chronic fatigue syndrome and control subjects. J Infect Dis. 1991 164:1023–1024. [DOI] [PubMed] [Google Scholar]
- Staines DR. Postulated vasoactive neuropeptide autoimmunity in fatigue-related conditions: a brief review and hypothesis. Clin Dev Immunol. 2006;13(1):25–39. doi: 10.1080/17402520600568252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne E. The chronic fatigue syndrome: a reappraisal and unifying hypothesis. Clin Exp Neurol. 1991;28:128–138. [PubMed] [Google Scholar]
- Nakaya T, Kuratsune H, and Kitani T. et al. Demonstration on Borna disease virus in patients with chronic fatigue syndrome [in Japanese]. Nippon Rinsho. 1997 55(11):3064–3071. [PubMed] [Google Scholar]
- Li YJ, Wang DX, and Bai XL. et al. Clinical characteristics of patients with chronic fatigue syndrome: analysis of 82 cases [in Chinese]. Zhonghua Yi Xue Za Zhi. 2005 85(10):701–704. [PubMed] [Google Scholar]
- Matano S, Kinoshita H, and Tanigawa K. et al. Acute parvovirus B19 infection mimicking chronic fatigue syndrome. Intern Med. 2003 42(9):903–905. [DOI] [PubMed] [Google Scholar]
- Kerr JR. Pathogenesis of parvovirus B19 infection: host gene variability, and possible means and effects of virus persistence. J Vet Med B Infect Dis Vet Public Health. 2005;52(7–8):335–339. doi: 10.1111/j.1439-0450.2005.00859.x. [DOI] [PubMed] [Google Scholar]
- White PD, Thomas JM, and Amess J. et al. Incidence, risk and prognosis of acute and chronic fatigue syndromes and psychiatric disorders after glandular fever. Br J Psychiatry. 1998 173:475–481. [DOI] [PubMed] [Google Scholar]
- Chia JK. The role of enterovirus in chronic fatigue syndrome. J Clin Pathol. 2005;58(11):1126–1132. doi: 10.1136/jcp.2004.020255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo K. Human herpesvirus latency and fatigue. Uirusu. 2005;55(1):9–17. doi: 10.2222/jsv.55.9. [DOI] [PubMed] [Google Scholar]
- Komaroff AL. Chronic fatigue syndromes: a preliminary overview. Can Dis Wkly Rep. 1991;17:23–28. [PubMed] [Google Scholar]
- Ablashi DV. Viral studies of chronic fatigue syndrome. Clin Infect Dis. 1994 18suppl 1. S130–S133. [DOI] [PubMed] [Google Scholar]
- White PD, Thomas JM, and Sullivan PF. et al. The nosology of sub-acute and chronic fatigue syndromes that follow infectious mononucleosis. Psychol Med. 2004 34(3):499–507. [DOI] [PubMed] [Google Scholar]
- Ng BY, Lim CC, and Yeoh A. et al. Neuropsychiatric sequelae of Nipah virus encephalitis. J Neuropsychiatry Clin Neurosci. 2004 16(4):500–504. [DOI] [PubMed] [Google Scholar]
- Parker NR, Barralet JH, Bell AM. Q fever. Lancet. 2006;367(9511):679–688. doi: 10.1016/S0140-6736(06)68266-4. [DOI] [PubMed] [Google Scholar]
- Masuda A, Nakayama T, and Yamanaka T. et al. The prognosis after multi-disciplinary treatment for patients with postinfectious chronic fatigue syndrome and noninfectious chronic fatigue syndrome. J Behav Med. 2002 25(5):487–497. [DOI] [PubMed] [Google Scholar]
- Wheatland R. Chronic ACTH autoantibodies are a significant pathological factor in the disruption of the hypothalamic-pituitary-adrenal axis in chronic fatigue syndrome, anorexia nervosa and major depression. Med Hypotheses. 2005;65(2):287–295. doi: 10.1016/j.mehy.2005.02.031. [DOI] [PubMed] [Google Scholar]
- Gottschalk M, Kumpfel T, and Flachenecker P. et al. Fatigue and regulation of the hypothalamo-pituitary-adrenal axis in multiple sclerosis. Arch Neurol. February2005 62(2):277–280. [DOI] [PubMed] [Google Scholar]
- Wessely S. The neuropsychiatry of chronic fatigue syndrome. Ciba Found Symp. 1993 173:212–229.discussion 229–237. [DOI] [PubMed] [Google Scholar]
- Gaab J, Engert V, and Heitz V. et al. Associations between neuroendocrine responses to the Insulin Tolerance Test and patient characteristics in chronic fatigue syndrome. J Psychosom Res. 2004 56(4):419–424. [DOI] [PubMed] [Google Scholar]
- Bakheit AM, Behan PO, and Dinan TG. et al. Possible upregulation of hypothalamic 5-hydroxytryptamine receptors in patients with postviral fatigue syndrome. BMJ. 1992 304(6833):1010–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inder WJ, Prickett TC, Mulder RT. Normal opioid tone and hypothalamic-pituitary-adrenal axis function in chronic fatigue syndrome despite marked functional impairment. Clin Endocrinol (Oxf) 2005;62(3):343–348. doi: 10.1111/j.1365-2265.2005.02220.x. [DOI] [PubMed] [Google Scholar]
- Durlach J, Pages N, and Bac P. et al. Chronopathological forms of magnesium depletion with hypofunction or with hyperfunction of the biological clock. Magnes Res. 2002 15(3–4):263–268. [PubMed] [Google Scholar]
- Kuratsune H, Yamaguti K, and Sawada M. et al. Dehydroepiandrosterone sulfate deficiency in chronic fatigue syndrome. Int J Mol Med. 1998 1(1):143–146. [DOI] [PubMed] [Google Scholar]
- Nijs J, De Meirleir K. Impairments of the 2–5 synthetase/RNase L pathway in chronic fatigue syndrome. In Vivo. 2005;19(6):1013–1021. [PubMed] [Google Scholar]
- Winkler AS, Blair D, and Marsden JT. et al. Autonomic function and serum erythropoietin levels in chronic fatigue syndrome. J Psychosom Res. 2004 56(2):179–183. [DOI] [PubMed] [Google Scholar]
- Hatcher S, House A. Life events, difficulties and dilemmas in the onset of chronic fatigue syndrome: a case-control study. Psychol Med. 2003;33(7):1185–1192. doi: 10.1017/s0033291703008274. [DOI] [PubMed] [Google Scholar]
- Taylor RR, Jason LA. Chronic fatigue, abuse-related traumatization, and psychiatric disorders in a community-based sample. Soc Sci Med. 2002;55(2):247–256. doi: 10.1016/s0277-9536(01)00168-x. [DOI] [PubMed] [Google Scholar]
- Heim C, Wagner D, and Maloney E. et al. Early adverse experience and risk for chronic fatigue syndrome: results from a population-based study. Arch Gen Psychiatry. 2006 63(11):1258–1266. [DOI] [PubMed] [Google Scholar]
- Morriss R, Sharpe M, and Sharpley AL. et al. Abnormalities of sleep in patients with the chronic fatigue syndrome. BMJ. 1993 306(6886):1161–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morriss RK, Wearden AJ, Battersby L. The relation of sleep difficulties to fatigue, mood and disability in chronic fatigue syndrome. J Psychosom Res. 1997;42(6):597–605. doi: 10.1016/s0022-3999(97)89895-9. [DOI] [PubMed] [Google Scholar]
- Friedlander AH, Mahler ME, Yagiela JA. Restless legs syndrome: manifestations, treatment and dental implications. J Am Dent Assoc. 2006;137(6):755–761. doi: 10.14219/jada.archive.2006.0287. [DOI] [PubMed] [Google Scholar]
- Terman M, Levine SM, and Terman JS. et al. Chronic fatigue syndrome and seasonal affective disorder: comorbidity, diagnostic overlap, and implications for treatment. Am J Med. 1998 1053A. 115S–124S. [DOI] [PubMed] [Google Scholar]
- Ghahramani M, Gooriah V. Chronic fatigue syndrome associated with a psychotic state resulting in multiple murders. Bull Am Acad Psychiatry Law. 1995;23(4):613–616. [PubMed] [Google Scholar]
- Skapinakis P, Lewis G, Mavreas V. Unexplained fatigue syndromes in a multinational primary care sample: specificity of definition and prevalence and distinctiveness from depression and generalized anxiety. Am J Psychiatry. 2003;160:785–787. doi: 10.1176/appi.ajp.160.4.785. [DOI] [PubMed] [Google Scholar]
- Hawk C, Jason LA, Torres-Harding S. Differential diagnosis of chronic fatigue syndrome and major depressive disorder. Int J Behav Med. 2006;13(3):244–251. doi: 10.1207/s15327558ijbm1303_8. [DOI] [PubMed] [Google Scholar]
- Moldofsky H. Nonrestorative sleep and symptoms after a febrile illness in patients with fibrositis and chronic fatigue syndromes. J Rheumatol Suppl. 1989;19:150–153. [PubMed] [Google Scholar]
- Dendy C, Cooper M, Sharpe M. Interpretation of symptoms in chronic fatigue syndrome. Behav Res Ther. 2001;39(11):1369–1380. doi: 10.1016/s0005-7967(00)00116-9. [DOI] [PubMed] [Google Scholar]
- Moss-Morris R, Petrie KJ. Discriminating between chronic fatigue syndrome and depression: a cognitive analysis. Psychol Med. 2001;31(3):469–479. doi: 10.1017/s0033291701003610. [DOI] [PubMed] [Google Scholar]
- White PD, Pinching AJ, and Rakib A. et al. A comparison of patients with chronic fatigue syndrome attending separate fatigue clinics based in immunology and psychiatry. J R Soc Med. 2002 95(9):440–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David AS. Postviral fatigue syndrome and psychiatry. Br Med Bull. 1991;47(4):966–988. doi: 10.1093/oxfordjournals.bmb.a072524. [DOI] [PubMed] [Google Scholar]
- Fulcher KY, White PD. Strength and physiological response to exercise in patients with chronic fatigue syndrome. J Neurol Neurosurg Psychiatry. 2000;69(3):302–307. doi: 10.1136/jnnp.69.3.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrie SM, MacHale SM, and Cavanagh JT. et al. The difference in patterns of motor and cognitive function in chronic fatigue syndrome and severe depressive illness. Psychol Med. 2000 30(2):433–442. [DOI] [PubMed] [Google Scholar]
- Scott LV, Salahuddin F, and Cooney J. et al. Differences in adrenal steroid profile in chronic fatigue syndrome, in depression and in health. J Affect Disord. 1999 54(1–2):129–137. [DOI] [PubMed] [Google Scholar]
- Sharpe M, Chalder T, and Palmer I. et al. Chronic fatigue syndrome: a practical guide to assessment and management. Gen Hosp Psychiatry. 1997 19(3):185–199. [DOI] [PubMed] [Google Scholar]
- Glass JM. Cognitive dysfunction in fibromyalgia and chronic fatigue syndrome: new trends and future directions. Curr Rheumatol Rep. 2006;8(6):425–429. doi: 10.1007/s11926-006-0036-0. [DOI] [PubMed] [Google Scholar]
- Geisser ME, Gracely RH, and Giesecke T. et al. The association between experimental and clinical pain measures among persons with fibromyalgia and chronic fatigue syndrome. Eur J Pain. 2007 11(2):202–207. [DOI] [PubMed] [Google Scholar]
- Yunus MB. Fibromyalgia and overlapping disorders: the unifying concept of central sensitivity syndromes. Semin Arthritis Rheum. 2007;36(6):339–356. doi: 10.1016/j.semarthrit.2006.12.009. [DOI] [PubMed] [Google Scholar]
- Brown MM, Jason LA. Functioning in individuals with chronic fatigue syndrome: increased impairment with co-occurring multiple chemical sensitivity and fibromyalgia. Dyn Med. 2007;6:9. doi: 10.1186/1476-5918-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook DB, Nagelkirk PR, and Poluri A. et al. The influence of aerobic fitness and fibromyalgia on cardiorespiratory and perceptual responses to exercise in patients with chronic fatigue syndrome. Arthritis Rheum. 2006 54(10):3351–3362. [DOI] [PubMed] [Google Scholar]
- Matsumoto Y. Fibromyalgia syndrome. Nippon Rinsho. 1999;57(2):364–369. [PubMed] [Google Scholar]
- Naschitz JE, Rosner I, and Rozenbaum M. et al. The head-up tilt test with haemodynamic instability score in diagnosing chronic fatigue syndrome. QJM. 2003 96(2):133–142. [DOI] [PubMed] [Google Scholar]
- Gallagher AM, Coldrick AR, and Hedge B. et al. Is the chronic fatigue syndrome an exercise phobia?: a case control study. J Psychosom Res. 2005 58(4):367–373. [DOI] [PubMed] [Google Scholar]
- Marshall GS, Gesser RM, and Yamanishi K. et al. Chronic fatigue in children: clinical features, Epstein-Barr virus and human herpesvirus 6 serology and long term follow-up. Pediatr Infect Dis J. 1991 10(4):287–290. [PubMed] [Google Scholar]
- Buchwald D, Wener MH, and Pearlman T. et al. Markers of inflammation and immune activation in chronic fatigue and chronic fatigue syndrome. J Rheumatol. 1997 24(2):372–376. [PubMed] [Google Scholar]
- Swanink CM, Vercoulen JH, and Bleijenberg G. et al. Chronic fatigue syndrome: a clinical and laboratory study with a well matched control group. J Intern Med. 1995 237(5):499–506. [DOI] [PubMed] [Google Scholar]
- Natelson BH, Cohen JM, and Brassloff I. et al. A controlled study of brain magnetic resonance imaging in patients with the chronic fatigue syndrome. J Neurol Sci. 1993 120(2):213–217. [DOI] [PubMed] [Google Scholar]
- Cope H, Pernet A, and Kendall B. et al. Cognitive functioning and magnetic resonance imaging in chronic fatigue. Br J Psychiatry. 1995 167(1):86–94. [DOI] [PubMed] [Google Scholar]
- Greco A, Tannock C, and Brostoff J. et al. Brain MR in chronic fatigue syndrome. AJNR Am J Neuroradiol. 1997 18(7):1265–1269. [PMC free article] [PubMed] [Google Scholar]
- Lange G, DeLuca J, and Maldjian JA. et al. Brain MRI abnormalities exist in a subset of patients with chronic fatigue syndrome. J Neurol Sci. 1999 171(1):3–7. [DOI] [PubMed] [Google Scholar]
- Cook DB, Lange G, and DeLuca J. et al. Relationship of brain MRI abnormalities and physical functional status in chronic fatigue syndrome. Int J Neurosci. 2001 107(1–2):1–6. [DOI] [PubMed] [Google Scholar]
- Lange G, Holodny AI, and DeLuca J. et al. Quantitative assessment of cerebral ventricular volumes in chronic fatigue syndrome. Appl Neuropsychol. 2001 8(1):23–30. [DOI] [PubMed] [Google Scholar]
- de Lange FP, Kalkman JS, and Bleijenberg G. et al. Gray matter volume reduction in the chronic fatigue syndrome. Neuroimage. 2005 26(3):777–781. [DOI] [PubMed] [Google Scholar]
- Daugherty SA, Henry BE, and Peterson DL. et al. Chronic fatigue syndrome in northern Nevada. Rev Infect Dis. 1991 13suppl 1. S39–S44. [DOI] [PubMed] [Google Scholar]
- Caseras X, Mataix-Cols D, and Giampietro V. et al. Probing the working memory system in chronic fatigue syndrome: a functional magnetic resonance imaging study using the n-back task. Psychosom Med. 2006 68(6):947–955. [DOI] [PubMed] [Google Scholar]
- Tanaka M, Sadato N, and Okada T. et al. Reduced responsiveness is an essential feature of chronic fatigue syndrome: a fMRI study. BMC Neurol. 2006 6:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange G, Steffener J, and Cook DB. et al. Objective evidence of cognitive complaints in chronic fatigue syndrome: a BOLD fMRI study of verbal working memory. Neuroimage. 2005 26(2):513–524. [DOI] [PubMed] [Google Scholar]
- Okada T, Tanaka M, and Kuratsune H. et al. Mechanisms underlying fatigue: a voxel-based morphometric study of chronic fatigue syndrome. BMC Neurol. 2004 4(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Lange FP, Kalkman JS, and Bleijenberg G. et al. Neural correlates of the chronic fatigue syndrome: an fMRI study [published online ahead of print July 7, 2004]. Brain. 2004 127pt 9. 1948–1957.doi:10.1093/brain/awh225. [DOI] [PubMed] [Google Scholar]
- Goldstein J. Chronic Fatigue Syndrome: The Struggle for Health. Beverly Hills, Calif: Chronic Fatigue Syndrome Institute. 1990 [Google Scholar]
- Schwartz RB, Garada BM, and Komaroff AL. et al. Detection of intracranial abnormalities in patients with chronic fatigue syndrome: comparison of MR imaging and SPECT. AJR Am J Roentgenol. 1994 162(4):935–941. [DOI] [PubMed] [Google Scholar]
- Siessmeier T, Nix WA, and Hardt J. et al. Observer independent analysis of cerebral glucose metabolism in patients with chronic fatigue syndrome. J Neurol Neurosurg Psychiatry. 2003 74(7):922–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto S, Ouchi Y, and Onoe H. et al. Reduction of serotonin transporters of patients with chronic fatigue syndrome. Neuroreport. 2004 15(17):2571–2574. [DOI] [PubMed] [Google Scholar]
- Puri BK. Proton and 31-phosphorus neurospectroscopy in the study of membrane phospholipids and fatty acid intervention in schizophrenia, depression, chronic fatigue syndrome (myalgic encephalomyelitis) and dyslexia. Int Rev Psychiatry. 2006;18(2):145–147. doi: 10.1080/09540260600581852. [DOI] [PubMed] [Google Scholar]
- Wang Q, Xiong JX. Clinical observation on electroacupuncture for treatment of chronic fatigue syndrome [in Chinese] Zhongguo Zhen Jiu. 2005;25(10):691–692. [PubMed] [Google Scholar]
- Price JR, Couper J. Cognitive behaviour therapy for adults with chronic fatigue syndrome. Cochrane Database Syst Rev. 2000;2:CD001027. doi: 10.1002/14651858.CD001027. [DOI] [PubMed] [Google Scholar]
- Akagi H, Klimes I, Bass C. Cognitive behavioral therapy for chronic fatigue syndrome in a general hospital: feasible and effective. Gen Hosp Psychiatry. 2001;23(5):254–260. doi: 10.1016/s0163-8343(01)00154-2. [DOI] [PubMed] [Google Scholar]
- Deale A, Husain K, and Chalder T. et al. Long-term outcome of cognitive behavior therapy versus relaxation therapy for chronic fatigue syndrome: a 5-year follow-up study. Am J Psychiatry. 2001 158:2038–2042. [DOI] [PubMed] [Google Scholar]
- Deale A, Chalder T, and Marks I. et al. Cognitive behavior therapy for chronic fatigue syndrome: a randomized controlled trial. Am J Psychiatry. 1997 154:408–414. [DOI] [PubMed] [Google Scholar]
- Masuda A, Nakayama T, and Yamanaka T. et al. Cognitive behavioral therapy and fasting therapy for a patient with chronic fatigue syndrome. Intern Med. 2001 40(11):1158–1161. [DOI] [PubMed] [Google Scholar]
- O'Dowd H, Gladwell P, and Rogers CA. et al. Cognitive behavioural therapy in chronic fatigue syndrome: a randomised controlled trial of an outpatient group programme. Health Technol Assess. 2006 10(37):iii–iv. ix,–x. 1–121. [DOI] [PubMed] [Google Scholar]
- Coutts R, Weatherby R, Davie A. The use of a symptom “self-report” inventory to evaluate the acceptability and efficacy of a walking program for patients suffering with chronic fatigue syndrome. J Psychosom Res. 2001;51(2):425–429. doi: 10.1016/s0022-3999(00)00220-8. [DOI] [PubMed] [Google Scholar]
- Fulcher KY, White PD. Randomised controlled trial of graded exercise in patients with the chronic fatigue syndrome. BMJ. 1997;314(7095):1647–1652. doi: 10.1136/bmj.314.7095.1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedberg F. Does graded activity increase activity?: a case study of chronic fatigue syndrome. J Behav Ther Exp Psychiatry. 2002;33(3–4):203–215. doi: 10.1016/s0005-7916(02)00038-1. [DOI] [PubMed] [Google Scholar]
- Powell P, Bentall RP, and Nye FJ. et al. Patient education to encourage graded exercise in chronic fatigue syndrome: 2-year follow-up of randomised controlled trial. Br J Psychiatry. 2004 184:142–146. [DOI] [PubMed] [Google Scholar]
- Goodnick PJ, Sandoval R. Psychotropic treatment of chronic fatigue syndrome and related disorders. J Clin Psychiatry. 1993;54:13–20. [PubMed] [Google Scholar]
- Natelson BH, Cheu J, and Hill N. et al. Single-blind, placebo phase-in trial of two escalating doses of selegiline in the chronic fatigue syndrome. Neuropsychobiology. 1998 37(3):150–154. [DOI] [PubMed] [Google Scholar]
- Klimas NG, Morgan R, and Van Rid F. et al. Observations regarding use of an antidepressant, fluoxetine, in chronic fatigue syndrome. In: Goodnick PJ, Klimas NG, eds. Chronic Fatigue and Related Immune Deficiency Syndromes. Washington, DC: American Psychiatric Press. 1993 95–108. [Google Scholar]
- Vercoulen JH, Swanink CM, and Zitman FG. et al. Randomised, double-blind, placebo-controlled study of fluoxetine in chronic fatigue syndrome. Lancet. 1996 347(9005):858–861. [DOI] [PubMed] [Google Scholar]
- Wearden AJ, Morriss RK, and Mullis R. et al. Randomised, double-blind, placebo-controlled treatment trial of fluoxetine and graded exercise for chronic fatigue syndrome. Br J Psychiatry. 1998 172:485–490. [DOI] [PubMed] [Google Scholar]
- Goodnick PJ, Sandoval R, and Brickman A. et al. Bupropion treatment of fluoxetine-resistant chronic fatigue syndrome. Biol Psychiatry. 1992 32:834–838. [DOI] [PubMed] [Google Scholar]
- Schonfeldt-Lecuona C, Connemann BJ, and Wolf RC. et al. Bupropion augmentation in the treatment of chronic fatigue syndrome with coexistent major depression episode [letter]. Pharmacopsychiatry. 2006 39(4):152–154. [DOI] [PubMed] [Google Scholar]
- Lecrubien Y. Antidepressant drugs: similar but different? In: Mendlewicz J, Brunello N, Langer SZ, et al, eds. New Pharmacological Approaches to the Therapy of Depressive Disorders. Basel, Switzerland: Karger. 1993 83–91. [Google Scholar]
- White PD, Cleary KJ. An open study of the efficacy and adverse effects of moclobemide in patients with the chronic fatigue syndrome. Int Clin Psychopharmacol. 1997;12(1):47–52. doi: 10.1097/00004850-199701000-00007. [DOI] [PubMed] [Google Scholar]
- Morriss RK, Robson MJ, Deakin JF. Neuropsychological performance and noradrenaline function in chronic fatigue syndrome under conditions of high arousal. Psychopharmacology (Berl) 2002;163(2):166–173. doi: 10.1007/s00213-002-1129-8. [DOI] [PubMed] [Google Scholar]
- Cleare AJ, O'Keane V, Miell J. Plasma leptin in chronic fatigue syndrome and a placebo-controlled study of the effects of low-dose hydrocortisone on leptin secretion. Clin Endocrinol (Oxf) 2001;55(1):113–119. doi: 10.1046/j.1365-2265.2001.01341.x. [DOI] [PubMed] [Google Scholar]
- Puri BK, Holmes J, Hamilton G. Eicosapentaenoic acid–rich essential fatty acid supplementation in chronic fatigue syndrome associated with symptom remission and structural brain changes. Int J Clin Pract. 2004;58(3):297–299. doi: 10.1111/j.1368-5031.2004.00073.x. [DOI] [PubMed] [Google Scholar]
- Laviano A, Meguid MM, and Guijarro A. et al. Antimyopathic effects of carnitine and nicotine. Curr Opin Clin Nutr Metab Care. 2006 9(4):442–448. [DOI] [PubMed] [Google Scholar]
- Randall DC, Cafferty FH, and Shneerson JM. et al. Chronic treatment with modafinil may not be beneficial in patients with chronic fatigue syndrome. J Psychopharmacol. 2005 19(6):647–660. [DOI] [PubMed] [Google Scholar]
- McDermott C, Richards SC, and Thomas PW. et al. A placebo-controlled, double-blind, randomized controlled trial of a natural killer cell stimulant (BioBran MGN-3) in chronic fatigue syndrome. QJM. 2006 99(7):461–468. [DOI] [PubMed] [Google Scholar]
- Blockmans D, Persoons P, and Van Houdenhove B. et al. Combination therapy with hydrocortisone and fludrocortisone does not improve symptoms in chronic fatigue syndrome: a randomized, placebo-controlled, double-blind, crossover study. Am J Med. 2003 114(9):736–741. [DOI] [PubMed] [Google Scholar]
- Williams G, Waterhouse J, and Mugarza J. et al. Therapy of circadian rhythm disorders in chronic fatigue syndrome: no symptomatic improvement with melatonin or phototherapy. Eur J Clin Invest. 2002 32(11):831–837. [DOI] [PubMed] [Google Scholar]