Abstract
Summary: To date, most Leishmania and human immunodeficiency virus (HIV) coinfection cases reported to WHO come from Southern Europe. Up to the year 2001, nearly 2,000 cases of coinfection were identified, of which 90% were from Spain, Italy, France, and Portugal. However, these figures are misleading because they do not account for the large proportion of cases in many African and Asian countries that are missed due to a lack of diagnostic facilities and poor reporting systems. Most cases of coinfection in the Americas are reported in Brazil, where the incidence of leishmaniasis has spread in recent years due to overlap with major areas of HIV transmission. In some areas of Africa, the number of coinfection cases has increased dramatically due to social phenomena such as mass migration and wars. In northwest Ethiopia, up to 30% of all visceral leishmaniasis patients are also infected with HIV. In Asia, coinfections are increasingly being reported in India, which also has the highest global burden of leishmaniasis and a high rate of resistance to antimonial drugs. Based on the previous experience of 20 years of coinfection in Europe, this review focuses on the management of Leishmania-HIV-coinfected patients in low-income countries where leishmaniasis is endemic.
INTRODUCTION
Updated statistics on the human immunodeficiency virus (HIV)/AIDS situation in December 2006 have shown that an estimated 39.5 million people are living with HIV/AIDS, among whom approximately 95% reside in developing countries ([http://www.unaids.org/en/HIV_data/epi2006/default.asp]). Of 4.3 million new HIV infections in 2006, 2.8 million (65%) occurred in sub-Saharan Africa, which continues to be the most severely affected part of the world. In this region, HIV has had a marked negative impact, reducing adult life expectancy by 50% in several countries. Although lack of access to treatment remains a major challenge, the number of people receiving highly active antiretroviral therapy (HAART) in sub-Saharan Africa recently passed 1 million for the first time. Weakness within the health systems has been identified as a key obstacle to expanding treatment, care, and preventive services; in addition, poor adherence to long-term therapy contributes to the expansion of AIDS.
As recognized in the resolution of the 60th World Health Assembly (http://ftp.who.int/gb/ebwha/pdf_files/WHA60/A60_10-en.pdf), leishmaniasis is one of the most neglected tropical diseases, with more than 12 million people worldwide currently infected and 2 million new cases reported each year; 350 million people are considered at risk, and the number of new cases is increasing. The disease affects the poorest populations in 88 countries, particularly developing countries (12). Two basic clinical forms, namely, cutaneous leishmaniasis (CL), a disfiguring and stigmatizing disease, and visceral leishmaniasis (VL) or kala-azar, which is fatal without treatment, are recognized. VL is prevalent in 70 countries, with the largest focus in South Asia, accounting for an estimated 300,000 cases in 2006. East Africa has the second largest focus of VL, with approximately 30,000 cases per year, while Brazil is third, with 4,000 reported cases in 2006. There is an alarming occurrence of new foci and an increase in the incidence of VL in east Africa (8, 214, 278). The true incidence of VL is underestimated because surveillance systems are lacking and misdiagnosis, especially with malaria, is common; failure to diagnose the disease leads to an increased case fatality rate.
CL is present in at least 82 countries, with an estimated annual incidence of 1.5 million cases worldwide. Several clinical forms are possible, depending on the Leishmania species involved, including localized cutaneous leishmaniasis (LCL), which often heals without treatment; diffuse cutaneous leishmaniasis (DCL), which is very difficult to treat; and finally, mucocutaneous leishmaniasis (MCL), which is the most severe form, as it produces disfiguring lesions and mutilation of the face (204).
The first case of leishmaniasis associated with HIV infection was reported in 1985, while the number of cases has subsequently increased rapidly in southern Europe. Thirty-five countries have since reported cases of coinfection. After the introduction of HAART, the number of coinfected cases in European countries where the disease is endemic fell sharply. However, the problem has expanded to other major foci of leishmaniasis in the world due to increased overlap of the two diseases.
The HIV/AIDS pandemic has modified the natural history of leishmaniasis (9). HIV infection increases the risk of developing VL by 100 to 2,320 times in areas of endemicity, reduces the likelihood of a therapeutic response, and greatly increases the probability of relapse (107, 141, 189, 221). At the same time, VL promotes the clinical progression of HIV disease and the development of AIDS-defining conditions. Both diseases exert a synergistic detrimental effect on the cellular immune response because they target similar immune cells (177, 260).
Leishmania-HIV coinfection is currently reported for 2 to 9% of all VL cases in given countries of endemicity (267), but this proportion is likely to increase dramatically. In selected populations, such as in Humera, Ethiopia, the rate of coinfection in VL patients is 15 to 30% (143). In general, it is accepted that the reported global incidence of coinfection is underestimated, partly because VL occurs among neglected populations and because it is not on the CDC list of opportunistic infections, so it is rarely reported in AIDS notification systems. The introduction of HAART has totally changed the course of HIV/AIDS infections and the outcome of associated opportunistic infections. However, access to HAART in developing countries remains inadequate. In addition, there are many unresolved questions related to the management of Leishmania-HIV-coinfected patients that justify this review.
EPIDEMIOLOGICAL INFORMATION ON LEISHMANIA-HIV COINFECTION
Southern Europe
A dedicated surveillance network, consisting of 13 reporting institutions (268) that increased to 16 institutions in 1998 (266), has been monitoring the situation of Leishmania-HIV coinfection in southern Europe since 1994. Periodic case reports showed that four countries, i.e., France, Italy, Portugal, and Spain, were mainly involved (9). The largest number of cases was consistently detected in Spain, which may be related to the reactivation of asymptomatic infections due to a greater geographical overlap between leishmaniasis and HIV infections compared with that for other southern European countries. However, it has also been demonstrated that newly acquired infections occur among intravenous drug users (IVDU) sharing Leishmania-infected syringes (11, 70, 186, 187), and at the time of these studies, Spain had five to seven times more IVDU than the European average. However, the proportion of reactivated leishmaniasis cases in asymptomatic coinfected patients compared with coinfected cases due to contaminated syringes has not been established. Cumulative cases recorded in different year ranges (Table 1) show that an incidence peak (n = 717) occurred during January 1996 to June 1998, representing approximately 50% of the total number of cases (n = 1,440) reported during the period 1990-1998 (266). By early 2001, the cumulative number of cases recorded by the WHO was 1,911, of which 57% were from Spain (83). All case records were analyzed by a geographical information system, which showed that 75% of patients lived in coastal urban areas with relatively high population densities. The spatial pattern of coinfections mapped for the neighboring littorals of northeastern Spain and southern France suggested a progressive spread of cases from urban to rural areas (83).
TABLE 1.
Number of Leishmania-HIV coinfections recorded by the WHO for four countries in southern Europe
| Period | No. of coinfections
|
Reference | ||||
|---|---|---|---|---|---|---|
| France | Italy | Portugal | Spain | Total | ||
| January 1990-June 1998 | 259 | 229 | 117 | 835 | 1,440 | 266 |
| January 1996-June 1998 | 132 | 85 | 88 | 412 | 717 | 266 |
| January 1990-January 2001 | 318 | 335 | 159 | 1,099 | 1,911 | 83 |
| January 2001-December 2006 | 29a | 42 | 98 | 130 | 299 | WHO, unpublished data |
From January 2001 to December 2005.
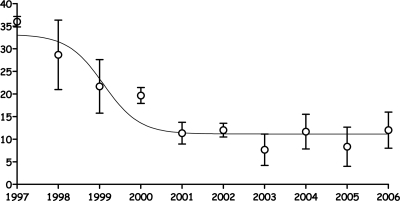
A clear decrease in the incidence of Leishmania-HIV coinfection was observed by the end of the 1990s (79, 138, 225), which can be attributed to the routine use of HAART since 1997 in most of southern Europe. In the Leishmaniasis Reference Centers of Madrid, Montpellier, and Rome, which are members of the WHO network for monitoring Leishmania-HIV coinfection, an average of 35 cases (95% confidence interval [CI], 34 to 38), which represented the incidence peak, were diagnosed in 1997. Cases began to steadily decrease during the period 1998-2001, and thereafter a low-incidence plateau was shown through 2006 (average of 12 cases; 95% CI, 8 to 16) (Fig. 1), except in Portugal; the reasons for the lack of decline in this country are unknown. An additional 241 new cases of primary infections from Spain (n = 95), Portugal (n = 64), Italy (n = 52), and France (n = 30) were reported to WHO during the period 2001-2006; some persistent cases were also reported. Other countries, such as Switzerland, Germany, United Kingdom, and Greece, reported sporadic imported cases (6).
FIG. 1.
Incidence trend of Leishmania-HIV coinfections recorded by three referral diagnosis centers, in France (1997-2005), Italy, and Spain (1997-2006). In these countries, HAART therapy for HIV treatment has been in routine use since 1997. Circles, means; bars, 95% confidence intervals.
Coinfected patients often have many episodes of active VL. More than 90% of these cases are confirmed by molecular methods to be relapses rather than reinfections (162). During 2001 to 2006, Spain and Portugal reported 95 primary infections versus 34 relapses (ratio of relapses to primary infections, 0.36) and 64 primary infections versus 21 relapses (ratio of relapses to primary infections, 0.33), respectively (WHO, unpublished data).
Epidemiological features and risk factors from cases reported during the period 1990-1998, representing the period of higher coinfection impact, and recently collated cases from the period 2001-2006, were analyzed and compared by WHO (266; WHO, unpublished data). The mean ages of patients were very similar in the two periods, i.e., 38.6 years (95% CI, 38.2 to 39.0 years) among 965 cases and 38.9 years (95% CI, 37.8 to 40.1 years) among 253 cases, respectively. Gender distributions were also similar, with male patients being highly prevalent in both periods (83.2% versus 88.5%, respectively). In contrast, the distributions by risk group for Leishmania-HIV coinfection showed significant differences between the earlier and more recent cases (Fig. 2). In both periods, three main risk factors, namely, IVDU and heterosexual and homosexual activities, accounted for about 94% of the analyzed cases. In the period 1990-1998, 781 cases that belonged to these risk groups were identified, among which IVDU accounted for 76% and heterosexual activity accounted for 12%, whereas among 95 cases analyzed during the period 2001-2006, the proportions of these groups were 67% and 23%, respectively (χ2 test; P = 0.01). This difference may reflect the general trend of AIDS decline among IVDU paralleled by an increase among heterosexuals in Western Europe (http://www.unaids.org). The rates of homosexual coinfected cases were similar in both periods (11% and 10%, respectively). With regard to immunological factors, coinfected patients were severely immunosuppressed in both periods. In the period 1990-1998, 624 of 682 patients (91%) had <200 CD4+ lymphocytes/μl, while during the period 2001-2006 (an HAART era) a similar situation was evident in 113 of 128 patients (88%).
FIG. 2.
Algorithm for the diagnosis of VL in HIV-infected patients.
South Asia
South Asia is currently the main focus for VL in the world, accounting for 67% of the total leishmaniasis disease burden (117). In 2005, Bangladesh reported 7,000 cases, India reported 32,800, and Nepal reported 3,000, figures that are known to be serious underestimations (34, 123, 230). In Bihar, India, a house-to-house survey demonstrated that only one in eight VL cases was counted in official government surveillance data (246). Additionally, there has been an upward trend in all three countries over the last several years, where 147 million people are estimated to be at risk of infection. More realistic estimates of annual incidence suggest approximately 250,000 cases in India, 40,000 in Bangladesh, and 3,000 in Nepal, which represents half of the VL burden in the world (41).
Interestingly, VL is concentrated in only 94 districts in all three countries and in four states in the northeast in India (Bihar, Uttar Pradesh, West Bengal, and Jharkhand). The state of Bihar accounts for >90% of cases and contributes to the spread of the disease into neighboring areas of Nepal. The reemergence of the disease in the 1970s was most likely due to residual post-kala-azar dermal leishmaniasis (PKDL) patients harboring parasites in the skin. Currently, PKDL is reported to occur in only 1% of Indian VL patients, but reliable data are lacking (228). In addition to this phenomenon, a loss of acquired immunity may partially explain the periodicity of VL incidence peaks every 10 to 15 years. In the past, most cases were in adults, although now there are reported to be many more children and adolescents, i.e., immune-naïve individuals, affected (41, 201).
The first case of HIV infection in India was reported in 1986 in Chennai (Madras) and was quickly followed by reports from all major cities; there has been a steady rise in the number of cases since (63, 164). The new 2006 estimates by the National AIDS Control Organization (http://www.nacoonline.org), supported by UNAIDS and WHO, indicate that the national adult HIV prevalence in India is approximately 0.36%, which corresponds to an estimated 2 million to 3.1 million people living with HIV in the country (http://www.nacoonline.org). The disease is concentrated in states in the south (Tamil Nadu, Andhra Pradesh, Maharashtra, and Karnataka), where effective interventions have caused HIV prevalence to begin to decline or stabilize, and to a lesser degree in the northeast (West Bengal, Orissa, Rajasthan, and Bihar), where overlap with leishmaniasis occurs. HAART was initially introduced in 25 centers in India during 2004, but because the implementation of the national HIV plan has been rapid, HAART is now widely available all over the country.
In Bangladesh, there are 11,000 people living with HIV; a national adult prevalence of <0.1% was estimated for 2006 (http://www.unaids.org/en/HIV_data/epi2006/default.asp). In Nepal, an estimated 75,000 people are living with HIV, and the national adult prevalence was estimated to be 0.5% for 2006 (http://www.unaids.org/en/HIV_data/epi2006/default.asp).
In India, the first Leishmania-HIV coinfection case was reported in 1999 from the sub-Himalayan region (Kumaon) (245). Various case reports of coinfection have since been published (150, 203). The problem of coinfection seems to be exacerbated by economic migrants who acquire HIV in urban settings and then return to their rural homes in areas where VL is endemic, where they acquire or reactivate leishmaniasis infection due to declining immunity. At the Kala-Azar Medical Research Centre in Muzaffarpur (Bihar), the number of HIV-positive patients increased from 339 in 2000 to 776 in 2006, and this was accompanied by an increase in the VL-HIV coinfection rate, from 0.88% in 2000 to 2.18% in 2006 (S. Sundar, personal communication). In a case series from India, rates of HIV positivity among VL-PKDL patients ranged from 1.5 to 6.3% (150, 258). One hospital-based study in India reported a VL prevalence of 2.84% among HIV-positive patients in 2006 (247).
In a study conducted in 39 hospitals in Nepal from June 2003 to May 2004, 140 of 854 febrile individuals studied had VL, and 8 of these were HIV positive (5.7%) (112). No data on Leishmania-HIV coinfection are available from Bangladesh.
As characterized by the PKDL patient, coinfected patients may represent an important reservoir of parasites with a high potential to maintain infection rates in sand flies at the community level (158). Although the extent of overlap between both infections is still limited, the potential for coinfection in this focus is very high, especially if one considers that these patients are a source of drug resistance due to their unresponsiveness to any antileishmania drug, in an area already threatened by a high rate of resistance to antimonials (251).
Brazil
In the 2006 Pan American Health Organization report for the Americas region, 62,000 cases of CL and 5,000 cases of VL were reported, of which the majority were from Brazil (http://www.paho.org/English/AD/DPC/CD/leish-2007.htm). However, linked databases from the National Surveillance Systems in Brazil for the period 2002-2003 yielded a corrected estimate of 10,207 VL cases for the same period, indicating that 40 to 50% of cases are underreported (http://www.aids.gov.br). Both CL and VL have been increasing for some years in Brazil; 32,000 (4.75 to 22.94 cases for every 100,000 inhabitants) and 3,500 (0.96 to 2.66 cases for every 100,000 inhabitants) cases of CL and VL, respectively, were reported in 2005. CL is widely distributed, whereas VL is endemic in the northeast areas, accounting for 87% of all VL cases, and is expanding to central west, north, and southeast areas of the country, and more worryingly, following a process of rural-to-urban transmission displacement, VL is spreading to important cities, such as Río de Janeiro, Belo Horizonte, Santarém, Teresina, Natal, and Fortaleza (47a).
Brazil is the epicenter of the HIV/AIDS epidemic in South America and accounts for one-third of all persons living with the virus in South America. AIDS was first reported in Brazil in 1983, and in the 2006 UNAIDS report, it is estimated that 620,000 (range, 370,000 to 1 million) people in Brazil are living with HIV (http://www.aids.gov.br). HIV/AIDS diagnostic and treatment services are provided free for all patients throughout Brazil. The country's emphasis on prevention and treatment has helped to keep the national adult prevalence steady at roughly 0.5% since 2000, although the spread of HIV transmission to regions with lower urbanization rates and to small- and medium-sized cities, where leishmaniasis can be transmitted, has been observed.
From 2001 to 2005, 16,210 cases of VL were reported in Brazil, and 315 (2%) patients were coinfected with HIV (92). Of the coinfected patients, 78% were male, and the median age was 38 years (86% of patients were in the 20- to 49-year age group); 56.3% of the HIV infections were attributed to heterosexual transmission, and 53% and 29% of the cases were reported from the northeastern and southeastern regions, respectively. The clinical forms found among coinfected cases are 43% MCL, 37% VL, and 20% CL (199), a clinical pattern that differs from that found in southern Europe, where typical VL represents 88% of coinfected cases; 8% of cases are atypical because of intestinal, lung, or other parasite colonizations, 4% are DCL, 0.4% are MCL, and 0.3% are combined cases of VL and CL (83). In the absence of HAART, the fatality rate during the first VL treatment course was 24%.
Of 150,000 CL cases reported from 2001 to 2005, 150 (0.1%) patients had HIV coinfection (92). MCL is frequently observed in HIV-coinfected patients in Brazil (43%), a clinical pattern rarely seen in southern Europe (0.4%).
In 2002, the Brazilian Leishmania-HIV Coinfection Network was established with the following aims (http://www.cpqrr.fiocruz.br/leish-hiv): (i) mapping of the geographical distribution of leishmaniasis-HIV coinfection; (ii) evaluation of the epidemiological, clinical, immunological, and therapeutic characteristics of each identified case; (iii) increasing the availability and ensuring appropriate usage of diagnostic tests for leishmaniasis; (iv) establishment of reference laboratories for the isolation and characterization of the parasites; (v) improvement in the dissemination of relevant information; (vi) enhanced training and provision of appropriate guidelines for the health system; (vii) broadening the participation of grassroots and nongovernmental organizations; and (viii) planning and evaluation of coinfection control interventions and follow-up activities. The Manual de Recomendações para Diagnóstico, Tratamento e Acompanhamento da Co-Infecção Leishmania-HIV was made available in 2004 by the Brazilian Ministry of Health (47a; http://www.saude.gov.br/bvs).
Sub-Saharan Africa
Burkina Faso.
The HIV seroprevalence in Burkina Faso is 2%. Sporadic cases of CL due to Leishmania major were reported from many localities from 1953 to 1984, but the number of cases has increased in recent years (61 cases in 1996, 552 cases in 1997, 1,218 cases in 1998, 1,595 cases in 1999, 712 cases in 2000, 1,063 cases in 2001, 1,152 cases in 2002, 1,194 cases in 2003, 901 cases in 2004, and 827 cases in 2005). A major increase in the number of cases since 2000 followed the development of a new district in a previously rural area near the capital Ougadougou; the disease is now known as “Ouaga 2000” (111). The peak incidence months are August and September, overlapping with the malaria peak season. Cases occur across all age groups and are equally prevalent among men and women.
Ten of 70 (14.3%) “Ouaga 2000” patients were coinfected with HIV. Many unusual clinical manifestations of CL, including lepromatous and diffuse (n = 15), ulcerative (n = 14), infiltrative (n = 12), papulonodular (n = 9), psoriasis-like (n = 5), Kaposi's sarcoma-like (n = 1), cheloid (n = 1), and histioid (n = 1) forms, were found in a prospective study of 32 coinfected patients. Treatment with a standard dosage regimen of meglumine antimoniate intramuscularly for 21 days achieved a 50% cure rate, but rapid relapses were observed in HIV-coinfected patients, for whom repeated courses of treatment were required (111, 172). Three treatment cycles increased the cure rate to 75%. Visceralization occurred in one HIV-positive patient, with disseminated papulonodular leishmaniasis and a bone marrow aspirate positive for L. major. Similar findings were observed in French Guiana, where nine coinfected patients had more lesions and less adenopathy or lymphangitis than immunocompetent patients, with a poorer response to treatment and higher recurrence and/or reinfection rates (66).
Ethiopia.
There is incomplete information on the epidemiology of leishmaniasis in Ethiopia, as no surveillance system is yet in place. However, reports of VL endemicity date back to the 1940s. The disease is prevalent mostly in lowland arid areas, and the parasite involved is mainly L. donovani, with an estimated annual incidence of 4,000 cases. The six areas of endemicity identified are northwestern Ethiopia (Metema, Humera, Wolkayit, and Libo/Fogera), northeastern Ethiopia (Awash Valley and Ethio-Djibouti border), south and southwest Ethiopia (Dawa, Genale, Gelana, Segen, Woito, Konso, and Omo River Valley), the Kenyan border, and the Gambella-Sudan border (113). However, leishmaniasis is spreading to areas where it was previously nonendemic, as exemplified by a recent outbreak in the Libo and Fogera districts (Amhara State), a highland area close to the focus in the northwest (8).
The first HIV-positive patient was reported in 1984, and the first AIDS case was reported in 1986. Based on antenatal sentinel surveillance projections, the estimated national HIV prevalence is 3.5% (10% in urban areas and 1.9% in rural areas). The urban prevalence is thought to have stabilized during the period 1999-2001, with a current estimation of 1.3 million HIV-positive people. HAART was introduced in 2003, but programs do not yet adequately address the needs of the rural poor. Approximately 65,000 HIV patients are now receiving HAART.
In Humera (northwest Ethiopia), the proportion of VL patients who were coinfected with HIV increased from 18.5% in 1998-1999 to 40% in 2006. In a retrospective review of 791 cases in Tigray, the case fatality rate among VL-HIV-coinfected patients was four times higher than that for VL patients not infected with HIV (143). In Libo, 15 to 18% of all VL patients are HIV positive (Médecins Sans Frontières (MSF)—Greece, personal communication). The groups at highest risk of coinfection are seasonal migrant laborers, sex workers, young adults in resettlement areas (particularly in the northwest and along the Sudan border), truck and other public transport drivers, and military personnel deployed in border areas (19).
Kenya, Uganda, and Somalia.
Data quality is poor for Kenya, Uganda, and Somalia. There are well-established foci in semiarid, poor, and remote districts where termite hills are colonized by the sandfly vector (Phlebotomus martini).
In Kenya, there are several historical foci, in West Pokot (representing 70% of all patients in Kenya), Baringo, Mandera, Garissa, and Mwingi. There was a recent outbreak in 2006 in northeast Kenya, at Wajir and Issiolo, which mainly affected children (n = 48; 95% of patients were <5 years of age). In 2006, 15 cases of VL-HIV coinfection were reported, but the risk of coinfection is increasing (268a).
In Uganda, the only documented area where VL is endemic is Pokot County, in the Nakapiripirit district in the northeastern region of Karamoja. This is an extension of the focus of endemicity of the West Pokot and Baringo districts of the Rift Valley province in Kenya. There is no national leishmaniasis control program, and most VL cases are monitored by MSF—Switzerland, who treated more than 2,500 patients in Amudat Hospital from 2000 to 2006. Approximately 70% of treated VL patients came from Kenya (West Pokot and Baringo districts). The male-to-female ratio of the patients was 3:1, and >60% of the patients were under 15 years of age. Eight cases of VL-HIV coinfection were confirmed (MSF—Switzerland, personal communication); no other data on VL-HIV coinfection are available. The HIV prevalence in Karamoja, on the Ugandan-Kenyan border, reached 3% in 2006; local conflicts, with associated rape, and cattle trading in towns may exacerbate the situation and elevate the potential for VL-HIV coinfection.
In Somalia, MSF—Belgium is currently dealing with an outbreak of VL and treated 263 and 1,300 cases in 2005 and 2006, respectively (MSF—Belgium, personal communication). No coinfection has been reported yet.
Sudan.
The main area of endemicity is the southeast of the country, bordering Ethiopia. There have been recurrent epidemics with high mortality rates, most recently in 1989 (236). The number of VL cases in 2006 was unexpectedly low in the states of Gedaref (n = 1,918) and Sennar (n = 476), and similar figures were observed in Upper Nile, but the mean annual incidence in the whole country is approximately 15,000 to 20,000 VL cases (S. H. El-Safi, personal communication). The parasite identified is mainly L. donovani, although L. infantum also occurs (81). Transmission is basically anthroponotic, with PKDL cases occurring in up to 50% of VL patients, forming an important human reservoir (91).
The first case of AIDS was reported in 1986, and by December 2006, the adult national prevalence was 1.6%, indicating that Sudan is now in a generalized epidemic (http://www.unaids.org/en/HIV_data/epi2006/default.asp). The estimated number of HIV/AIDS cases is around 350,000 (range, 170,000 to 580,000). The transmission is mainly heterosexual (97%), and vertical transmission from mother to child also plays a role. The most affected areas are Khartoum and the eastern and southern states, due to population movements (refugees and internally displaced populations). The 19- to 39-year age group is the most affected, and among registered patients, males predominate (male-to-female ratio, 3:1). The prevalence of HIV infection in the surveillance sentinel clinics in 2002 and 2004 was 1.1% and 1.9%, respectively, for sexually transmitted infection clinics, 1.6% and 2.3%, respectively, for tuberculosis patients, and 2% and 0.95%, respectively, for antenatal care clinics (Sudan National AIDS Program). The prevalence in other groups was as follows: street children, 2.3%; university students, 1.1%; refugees, 4%; prisoners, 2.5%; and sex workers, 4.4%. The strategic objectives of the National Policies on HIV/AIDS are to maintain the prevalence of HIV/AIDS below 2% and to provide care, treatment, and support to infected patients. In 2006, there were 40 centers for treatment services (voluntary counseling and testing units) and around 1,000 patients receiving HAART. Screening of military personnel and students indicates that the number of cases of HIV is increasing.
By 1998, three cases of coinfection had been identified. Since then, the reported prevalence in hospital-based studies was 5% (3/60) in Khartoum between 1998 and 1999, 9.4% (5/53) in Khartoum in 2002, and 8.1% (3/37) and 3.6% (3/84) in 2002 and 2003, respectively, in Gedaref State (Sudan National AIDS Program).
MICROBIOLOGY
Since the first case of Leishmania-HIV coinfection (76), methods to identify Leishmania have greatly evolved. Beside multilocus enzyme electrophoresis, a large number of molecular methods have been introduced for the characterization of Leishmania from the genus to strain levels, but most of them lack standardization.
Three main cryobanks and identification centers, in France (Montpellier), Italy (Rome), and Spain (Madrid), which use the same reference identification technique by 15 enzymatic systems with starch gel electrophoresis, according to Rioux et al. (213), have identified a large series of isolates from Leishmania-HIV coinfection cases since 1986, on which the present review is focused. The data presented are based on a compilation of several papers, mainly three papers published in a 2003 special issue of Annals of Tropical Medicine and Parasitology, namely, those by Pratlong et al. (195) for southern France, Chicharro et al. (59) for Spain, and Gramiccia (108) for Italy, and a recent paper by Campino et al. (54) for Portugal.
A total of 1,037 Leishmania strains have been isolated and identified from HIV-positive patients, which represents the largest sample studied around the world. The majority of the isolates came from VL cases in southwest Europe, and a few isolates were obtained from other foci and other leishmaniasis forms (Table 2).
TABLE 2.
Zymodemes of L. infantum found in HIV-positive patients in southern Europe and North Africa
| Country | No. of isolates with zymodeme
|
Total no. of isolates | |||||
|---|---|---|---|---|---|---|---|
| MON-1 | MON-24 | MON-29 | MON-34 | MON-183 | Other (n = 23 zymodemes) | ||
| France | 158 | 5 | 1 | 5 | 169 | ||
| Greece | 2 | 1 | 3 | ||||
| Italy | 58 | 7 | 1 | 2 | 13 | 81 | |
| Portugal | 72 | 1 | 2 | 1 | 76 | ||
| Spain | 152 | 63 | 15 | 36 | 19 | 54 | 339 |
| Algeria | 12 | 9 | 1 | 22 | |||
| Morocco | 1 | 1 | |||||
| Tunisia | 3 | 1 | 4 | ||||
| Total | 458 | 87 | 19 | 38 | 19 | 74 | 695 |
Leishmania infantum Identification during Coinfection
Using isoenzyme electrophoresis, 695 isolates were identified as Leishmania infantum, mainly from patients infected in Spain (n = 339), France (n = 169), Italy (n = 81), and Portugal (n = 76), with a few isolates from patients in Algeria (n = 22), Tunisia (n = 4), Greece (n = 3), and Morocco (n = 1). Almost all of the leishmaniasis clinical forms were VL (99.6%), with occasional cases of CL (Table 2).
Of 28 different L. infantum zymodemes detected, MON-1 has the widest geographical distribution, being present in all eight countries mentioned above, and it is the most frequent zymodeme in the studied sample (65.9%), as also seen for immunocompetent VL patients and canine leishmaniasis cases from the Mediterranean countries. The MON-24 zymodeme is present in seven of eight countries and represents 12.5% of the isolates. Five zymodemes (MON-1, MON-24, MON-29, MON-34, and MON-183) account for 621 isolates (89.3%). The remaining 74 isolates (10.6%) are divided into 23 different zymodemes. The observed enzymatic polymorphism is based on the latter zymodemes, which are almost exclusively present in Spain (n = 21) and Italy (n = 15), indicating high enzymatic polymorphism, whereas enzymatic polymorphism is reduced in France (n = 5) and Portugal (n = 4).
Within the countries themselves, the polymorphism shows geographical variations. The best example is given by Gramiccia (108) in Italy, who showed that the polymorphism index (PI; the number of zymodemes detected divided by the number of patients investigated) for HIV-positive patients in the whole of Italy was higher (PI = 0.13) than that for HIV-negative patients (PI = 0.04). The PI for strains isolated from both HIV-positive and HIV-negative patients decreased from the south (Sicily) to the north (rest of Italy).
Zymodeme MON-1 is the usual agent of VL in both HIV-negative and -positive patients in the entire Mediterranean basin and can occasionally be responsible for CL in immunocompetent patients, although zymodeme MON-24 is the most frequent cause of CL in this area. However, several dermotropic zymodemes, usually causing CL in nonimmunodepressed patients (MON-11, MON-24, MON-29, MON-33, and MON-78), are directly responsible for VL in HIV-positive patients because of the anergic status of these patients (58).
The higher enzymatic polymorphism in HIV-positive than in HIV-negative patients implies that several zymodemes (MON-136, MON-183, MON-185, MON-188, MON-190, MON-198, MON-199, and MON-228) exist only in HIV-positive patients (120). Curiously, these zymodemes associated with HIV infection are located at the ends of the branches of the phylogenetic tree, as if they had recently appeared. The question is whether these zymodemes can survive and cause symptomatic disease in immunocompetent patients (195).
VL occurring during HIV infection cannot be cured, even after extensive antileishmanial treatment. The likelihood of a relapse occurring is dependent on the level of CD4+ cells in the patient. In patients (n = 80) from southern Europe, two or three stocks were isolated from each patient following successive episodes of relapse, with time intervals of 1 to 4 years, and were subsequently identified by enzymatic electrophoresis. All of the isolates were L. infantum, and 18 zymodemes were found repeatedly during the various episodes. They were mainly MON-1 (58.1%) and MON-24 (13.3%), but a large number of other zymodemes were also identified in the global sample (Table 3). These results suggest that there is no specific zymodeme related to a particular severity of VL, as several zymodemes are expressed in further relapses. However, all but two patients had the same L. infantum zymodeme during the successive episodes. In two patients, two distinct zymodemes were obtained, at time intervals of 20 months (MON-1 and MON-34) and 29 months (MON-1 and MON-33) (100). By using a more powerful tool for molecular tracking (seminested PCR-restriction fragment length polymorphism analysis) that is capable of discriminating within the same zymodeme, Morales et al. (162) showed that 7.5% of the so-called relapses in 40 patients with VL-HIV coinfection had a different band pattern from that found in the primary attack. From these studies, it appears that repeated leishmaniasis episodes in HIV-positive patients could be due mainly to relapses of the first infection. For the two cases of different zymodemes, these occurred due to either a reinfection or the existence of a mixed infection by two zymodemes which were differently selected during culture of the two episodes.
TABLE 3.
Numbers of isolates identified according to zymodemes found during VL relapses
| Regiona | No. of isolates with zymodeme
|
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 11 | 24 | 28 | 29 | 33 | 34 | 72 | 78 | 108 | 136 | 183 | 185 | 188 | 201 | 228 | 253 | 283 | |
| A | 13 | 2 | 2 | 1 | 1 | 1 | ||||||||||||
| B | 8 | 1 | 1 | 1 | 1 | 1 | ||||||||||||
| C | 20 | 10 | 1 | 5 | 1 | 2 | 1 | 2 | 1 | |||||||||
| D | 20 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||||
| Total | 61 | 1 | 14 | 3 | 4 | 2 | 6 | 1 | 1 | 2 | 1 | 2 | 1 | 1 | 1 | 1 | 2 | 1 |
More recently, L. infantum-L. major hybrid strains were described for HIV-coinfected patients from Portugal, by sequencing of the gene for polymerase II RNA and by isoenzymatic identification (202).
Other Leishmania Species during HIV Coinfection
No data from anthroponotic VL foci are available, with the exception of a single strain from Djibouti isolated and identified as L. donovani MON-268 (194).
Although Leishmania-HIV coinfection concerns mainly VL, some cases of CL have been reported from countries where it is endemic in Africa and South America. In the sub-Saharan Sahelian zone of Africa, several L. major isolates obtained from patients in Mali (n = 4), Burkina Faso (n = 7), Senegal (n = 1), and Mauritania (n = 1) belonged to zymodeme MON-26 and its small variants, MON-74 and MON-117, a group of zymodemes extending from west Africa to central Asia. An outbreak of CL in Ouagadougou (Burkina Faso) due to L. major MON-74 included HIV-positive patients (111).
Among Brazilian HIV-coinfected patients, Rabello et al. (199) reported eight cases of CL by L. braziliensis and L. guyanensis, three cases of MCL by L. braziliensis, and one case of VL by L. chagasi. In French Guiana, five strains isolated from HIV-positive patients with CL were typed by multilocus enzyme electrophoresis and shown to belong to L. guyanensis, and four zymodemes were detected, including MON-43 (n = 1), MON-45 (n = 1), MON-131 (n = 2), and MON-148 (n = 1) (66).
Moreover, various New World Leishmania dermotropic species, such as L. braziliensis, L. mexicana, and L. amazonensis, have been identified as causes of VL in HIV-positive patients (23, 24, 200, 241), while conversely, viscerotropic variants of L. infantum/L. chagasi have been found in cutaneous lesions or even in the healthy skin of HIV-positive patients (44, 105, 191).
The Trypanosomatidae family includes the protozoa of plants, insects, and mammals, but only Leishmania and Trypanosoma species are usually found in humans. However, in some cases, nonhuman monoxenous trypanosomatids have been isolated from HIV-positive patients, mimicing both VL (121, 180) and CL (40, 75, 227). These infections suggest that the immunocompromised patient could be vulnerable to other currently non-human-pathogenic trypanosomatids due to their anergic status (58, 74).
PATHOGENESIS
VL-HIV Coinfection
Early after the appearance and report of the first cases of Leishmania-HIV coinfection, it was evident that the presence of both pathogens concomitantly in the same host cell (the macrophage) might have enhanced reciprocal effects that influence the expression and multiplication of either one or both pathogens (36, 269). It is thought that the parasite infection found concurrently with HIV induces chronic immune activation, and therefore an increased HIV load and accelerated progression of AIDS (27), whereas immunological disturbances caused by HIV are particularly favorable for the uncontrolled multiplication of the parasite.
During the last 10 years, attempts have been made to discover those mechanisms that are involved in the immunopathogenesis of Leishmania-HIV coinfection and to confirm that there is a specific Leishmania-HIV interaction at the cellular level that might affect the course of infection for each pathogen. It has been determined that such interactions are patent in the macrophage as well in other cells, such as dendritic cells (DCs). The involvement of other cells might explain the systemic effects observed in coinfected patients.
The main problem of coinfection is that parasitic infection may induce the activation of latent virus. Clinical studies have shown that leishmaniasis promotes an increase in serum HIV type 1 (HIV-1) load (49, 196) and a more rapid progression to AIDS that reduces life expectancy in HIV-infected patients (72). Experimental studies have demonstrated the participation of Leishmania in the pathogenesis of HIV-1 through the induction of viral replication and disease progression. Initial reports proved that Leishmania can upregulate virus expression in two monocytoid cell lines latently infected with HIV-1 (36), and evidence was provided that Leishmania promastigotes (LPG) and the intramembrane structural component of LPG (core-PI) present in amastigotes were both capable of promoting virus replication in T cells through complex biochemical pathways that involve the translocation of the transcriptional factor NF-κβ to the nucleus (35). Although the exact mechanism remained unclear, it was thought that LPG molecules could interact with the HIV-infected T cell during antigenic presentation between the Leishmania-infected macrophage and the T cell (177). Furthermore, Leishmania may induce HIV replication in infected cells through antigen-specific and non-antigen-specific mechanisms in which tumor necrosis factor alpha (TNF-α) plays a key role (270).
More recently, it has been shown with human tonsillar tissue cultured ex vivo (275) and primary human monocyte-derived macrophages (274) that Leishmania does not directly affect virus gene expression but instead modulates the life cycle of HIV-1 through an indirect phenomenon that is linked to the induction or elevation of TNF-α and interleukin-1a (IL-1a) and that may function in an autocrine/paracrine manner to upregulate virus gene expression mediated through induction of NF-κβ (109).
For patients coinfected with HIV-1 and Leishmania, it has been proposed that the increase in cytokine production induced by the parasite will affect virus production not only in macrophages but also in HIV-1-infected CD4+ T cells (275).
Different clinical studies performed recently illustrate the complexity of the interplay between the pathogens. It has been observed that Leishmania infection may affect the life cycle of the virus through the increased expression of specific chemokine receptors. Leishmania-HIV-coinfected patients have a significantly higher level of CCR5+ CD3+ T cells than do HIV-negative patients with VL or HIV-positive patients without VL (176). CCR5 is a major coreceptor for HIV entry in target cells, and its high expression in subjects is related to a high virus load and accelerated progression to HIV disease (206). Another study with coinfected patients showed a marked increase in circulating levels of the soluble form of the human leukocyte antigen G (HLA-G), a nonclassical histocompatibility complex class I molecule with immunosuppressive properties (88).
Interactions between HIV and Leishmania are not only restricted to the replication of the virus. Clinical studies have demonstrated that the high incidence of disseminated leishmaniasis in AIDS patients (141) and the high peripheral parasitemia (45) are indicative of uncontrolled parasite growth. In concordance with this condition, experimental in vitro coinfection of monocyte-derived macrophages with HIV-1 and L. donovani (271) or L. infantum (276) promastigotes showed a significant enhancement of intracellular parasite growth compared with parasite infection alone. The lack of control of intracellular multiplication is probably related to the HIV-1-mediated impairment of an effector function carried out by macrophages, such as phagocytosis, intracellular killing, chemotaxis, and cytokine production (126). Despite the fact that HIV-1-infected monocyte-derived macrophages display an impaired capacity to phagocytose numerous pathogens, Leishmania uptake is increased following virus infection (276).
In immunocompetent individuals, the protective Leishmania-specific immune response is associated with a Th1 cytokine profile, while susceptibility to Leishmania infection and disease progression are related to a Th2 cytokine response (127). It has been confirmed that HIV-1 inhibits the proliferative response to L. donovani (269); this reduced cellular response might be because the known inductive signal for gamma interferon (IFN-γ) is lacking or could be due to the direct influence of anti-inflammatory Th2 cytokines. Wolday et al. (272) confirmed that HIV-1 can modulate in vitro and ex vivo cytokine production in response to Leishmania; the addition of HIV-1 to cultures decreased IFN-γ, IL-12, and IL-18 production and increased IL-4 and IL-10 production in response to Leishmania by peripheral blood monocytic cells from healthy donors, while cells from HIV-1-infected and coinfected patients failed to secrete IFN-γ in response to Leishmania. Analysis of the ex vivo production of cytokines by peripheral blood monocytic cells from coinfected patients showed that greater quantities of IL-4 and IL-10 were released than those from HIV-positive patients not infected with Leishmania, and production of IFN-γ showed no changes after stimulation with phytohemagglutinin (174). In addition, patients with VL and HIV-1 infection have decreased circulating levels of IL-15, a cytokine that enhances the Th1 response and potentiates the immune response to intracellular human pathogens (85). All of these data suggest that a shift toward the Th2 type of specific T-cell immune response to Leishmania occurs in patients with T-lymphocyte defects induced by HIV-1, which would partly explain the high susceptibility to Leishmania infection, the high severity of the disease, and why reactivations occur in these patients (49).
Barreto-de-Souza et al. (25) recently studied the role of the transcriptional transactivator (Tat) protein, an essential viral gene product for HIV-1 replication, in the exacerbation of Leishmania proliferation in human macrophages. Tat is secreted in large amounts by cells infected by HIV-1 and is able to stimulate secretion of IL-1β, IL-4, IL-6, IL-8, transforming growth factor beta (TGF-β), TNF-α, and TNF-β. The results showed that Tat protein was able to override the leishmanicidal effect of IFN-γ and to enhance Leishmania replication in human macrophages through the production of prostaglandin E2 in the macrophage, which in turn increases the synthesis of TGF-β1 and the augmentation of Leishmania growth.
A review of the literature confirms that there is a multifaceted interaction between Leishmania and HIV-1 in the macrophage host cell. But the macrophage is not the only cell type capable of hosting both pathogens; DCs can also be infected by Leishmania parasites and HIV-1 (168, 250). There is no information on the consequence of both pathogens being present in DCs, but it has been proposed that such coinfection might modify the course of infection for each pathogen (102). Furthermore, the ability of both Leishmania and HIV-1 to bind to the same DC receptor, DC-SIGN (DC-specific ICAM-3-grabbing nonintegrin), to gain entry into DCs (51, 65) might affect the life cycle of the other pathogen. It has been demonstrated that HIV-1 transmission to CD4+ T cells is diminished when DC-SIGN-expressing cells are preincubated with Leishmania amastigotes before being pulsed with virions (273). Nevertheless, the consequence of both parasite and virus competing for the same DC receptor is unknown, and the importance of DCs as a virus and parasite reservoir, as well as the impact of both pathogens being present in DCs at once in coinfected patients, remains to be determined.
CL-HIV Coinfection
CL occurs in humans as a localized (LCL), mucocutaneous (MCL), or diffuse (DCL) form, depending on the infecting species of Leishmania (2, 115) and the human host. The pathology of LCL in humans is similar to the pathology observed in experimental infections of resistant inbred mouse strains. The presence of amastigotes within infected macrophages is the hallmark of the disease. In early lesions, the dermal infiltrate consists mainly of macrophages filled with amastigotes (4), with lymphocytes and plasma cells appearing later, in association with edema in the superficial dermis and hyperkeratosis of the epidermis, followed by ulceration. Over the following months, a granulomatous infiltrate consisting of lymphocytes, epitheloid cells, and multinucleated giant cells emerges as the number of amastigotes and macrophages declines. Healing follows in most cases, occurring early (within 3 months) in lesions caused by species such as L. major or L. mexicana or being delayed (over 10 months) in lesions of L. tropica or L. braziliensis. Infection with a small number of parasites might lead to natural healing and immunization (2), which is the strategy applied in “leishmanization.”
Resolution of disease correlates with the development of a successful Th1 cellular immune response driven by IL-12- and IFN-γ-mediated expression of TNF-α (17) and inducible nitric oxide synthase (iNOS) (240), with production of NO and parasite killing (198). It is likely that sterile immunity is not achieved and parasite persistence promotes protection against reinfection. T regulatory cells have been demonstrated in LCL lesions due to L. braziliensis (52).
Atypical forms of CL appear in unusual locations not normally exposed to sandfly bites, such as the genitals, palms, and feet, and CL can exhibit unusual morphology (erysipeloid, verrucoid, psoriasiform, eczematoid, or zosteriform). Failure of the immune system to control parasite multiplication might lead to infection in the superficial layer of the papillary dermis in the eczematoid, erysipeloid, and psoriasiform forms or in the reticular dermis in sporotrichoid forms of CL (2). Multiple lesions of LCL can occur because of multiple inoculations by infected sand flies but can also result from parasite dissemination (130). A chronic form of LCL develops in cases where the protective response is insufficient and lesions persists for over 1 year (2).
CL has been compared to leprosy as a “spectral disease” (263). CL recidivans (2) and LCL would correspond to tuberculoid forms of leprosy, with a well-developed cell-mediated immune response characterized by a positive skin test, low levels of antibody, small numbers of parasites in the lesions, and a Th1 cytokine pattern dominated by IFN-γ and the presence of NO in lesions. At the other extreme of the cutaneous forms would be DCL, analogous to lepromatous leprosy, with a failure to mount a delayed-type hypersensitivity response characterized by a negative skin test, dissemination of lesions in the skin with large numbers of parasites, and a Th2 regulatory type of cellular response with increased IL-4 (14, 242), IL-10, and TGF-β (86), with the associated inflammatory dermal chemokines (217). Nevertheless, an explanation for the variable spectrum of CL based on the host response may only be valid within an area where the same species of Leishmania are distributed. Even then, the virulence of the parasite would be expected to play a role. It has been reported that CL caused by L. aethiopica manifests as either LCL or DCL depending on the propensity of the parasite strain to induce IFN-γ or IL-10 (3, 4), although this could not be substantiated in subsequent studies investigating the genetic variability of L. aethiopica strains (231).
HIV infection promotes a Th2 immune response (61) which is detrimental to leishmaniasis. In Leishmania-HIV coinfection, particularly in later stages of HIV disease with marked CD4+ T-cell depletion and reduced production of IFN-γ, lesion healing may be compromised because of the impaired capacity of macrophages to kill amastigotes. Appropriate recognition of Leishmania antigens and stimulation of B lymphocytes depend on an effective CD4+ T-cell response which, when compromised, manifests in an inhibition of the in vitro proliferative response to leishmanial antigens and a failure to mount a delayed-type hypersensitivity response in vivo, with a predominant humoral response from an oligoclonal B-cell population that favors parasite multiplication, dissemination, and unusual localization.
Most of the literature on the clinical course of CL-HIV coinfection highlights atypical presentations, usually of severe and unusual forms. It is likely that the impact of the HIV-driven Th2 shift on the pathogenesis of CL in coinfected patients depends on the degree of immunosuppression and the loss of CD4+ T cells. For example, the probability of ulceration is reduced in coinfected patients with low CD4+ T-cell counts (256). However, the relationship is not necessarily linear. Among six African HIV-positive patients with cutaneous L. major infection seen in an outpatient clinic in France between 1997 and 2002, five had DCL and none showed parasite dissemination beyond the lesion, despite a high viral load and very low CD4 levels in the peripheral blood (<10 cells/μl) (99). In DCL, where the tendency for a Th2 response is already established, synergy could emerge early with severe negative consequences for the course of leishmaniasis.
Unusual clinical presentations of CL have been reported from sites of endemicity for probably all Leishmania species. These are consistently associated with clinical polymorphism and difficulty in differential diagnoses (80) in the different geographical areas (111, 137, 151, 219, 244). Some patients manifest with several forms (papulonodular, ulcerative, infiltrative, lepromatous and diffuse, psoriasis-like, cheloid, histioid, or Kaposi's sarcoma-like) at the same time. “Dermotropic” variants of L. infantum as well as L. braziliensis, L. mexicana, and L. amazonensis have been reported to cause visceral disease in HIV-positive patients. Cutaneous involvement occurs in 8 to 12% of VL-HIV-coinfected patients (268). “Viscerotropic” Leishmania sp. variants, such as L. infantum or L. chagasi, can be found in cutaneous lesions and even in apparently healthy skin (181). In general, the dermatological manifestations of coinfection (reviewed in reference 197) tend toward dissemination and abundance of amastigotes in the dermis and in keratinocytes, with various histopathological findings depending on immune status, often with scarce mononuclear and lymphocyte infiltrates, and delayed healing.
For L. aethiopica, recurrence was reported from healed LCL lesions in two cases, one where the LCL reappeared as MCL after 12 years and another where a successfully treated LCL lesion reappeared 5 years after healing (30). Recurrence of lesions in LCL due to L. aethiopica is estimated to occur in <1% of cases (20). It is not known whether the frequency of recurrence (reactivation or reinfection) is higher in HIV-coinfected patients.
Leishmania major was reported to cause DCL in a child with AIDS (104), in four coinfected patients with CD4 levels below 10/μl, with no visceralization and no relapse after successful treatment (99), and in a severely immunocompromised patient in Burkina Faso, who failed to respond to treatment courses of amphotericin B deoxycholate (AMB), sodium stibogluconate, and liposomal AMB (L-AMB) but responded to miltefosine (234). A longitudinal study in the same country reported clinical polymorphism and a variable treatment response for 32 CL-HIV patients followed over a period of 16 months, with some patients presenting with more than one clinical form (173). DCL in an HIV patient with a CD4 count of 98/μl responded dramatically to meglumine antimoniate treatment (171). In Sudan, L. major was identified in a Kaposi's sarcoma lesion in an HIV-coinfected patient (90).
In L. guyanensis infection, higher rates of recurrence (or reinfection) were observed for CL-HIV-coinfected patients. Coinfected patients with moderate immunosuppression (CD4 levels above 200 cells/μl) had more lesions and a lower rate of recovery after one treatment cycle with pentamidine than their HIV-negative counterparts (66). Relapse was reported after repeated cycles of treatment for one coinfected patient (CD4 count of 582/μl) who had mucosal and cutaneous involvement with abundant amastigotes, even in clinically healed lesions, and a negative skin test (84).
PKDL, a form of CL that generally appears after successful treatment of VL, is characterized by maculopapular or nodular lesions on the face, limbs, or trunk, with a heavy infiltrate of plasma cells and lymphocytes (118), and occurs in association with L. donovani. Leishmania infantum has also been incriminated in PKDL lesions in coinfected patients (223, 249).
In summary, HIV coinfection has the potential to negatively affect the course of CL as immunosuppression progresses by promoting parasite dissemination, atypical localization, unusual and more severe clinical presentations, delayed healing, poor responses to treatment, more frequent recurrences, and difficulty in diagnosis, irrespective of the etiologic species of Leishmania involved. The major pathophysiologic basis for this appears to involve an enhanced shift to a predominant Th2 response driven by the HIV-mediated immune dysregulation in the human host, which undermines the mainly Th1 response that is characteristic of CL in patients who are not immunocompromised. On the other hand, CL might be unmasked or show deterioration during the course of immune recovery following HAART (192) in HIV-coinfected patients.
DIAGNOSIS
For HIV patients, the diagnosis of leishmaniasis may be difficult because the clinical manifestations typical of the disease are not always present and/or patients may present with nonspecific clinical signs. Moreover, splenomegaly is less frequent in coinfected patients (189), and 42 to 68% of these patients have other associated opportunistic infections with similar symptoms, which further complicates the clinical diagnosis (224). The prevalence of different forms of leishmaniasis depends on the particular geographical area. VL is the most prevalent clinical form, especially in southwestern Europe and Ethiopia, where the majority of coinfection cases have been recorded, although cases of CL and MCL, with or without an association to VL, have been reported.
Parasitological Diagnosis
The detection of leishmanial parasites by microscopy or culture in different tissue samples is considered the gold standard for the diagnosis of leishmaniasis in HIV-coinfected patients and may be a useful way of detecting treatment failures.
Microscopy.
Bone marrow aspirate microscopy has been the most frequently employed diagnostic technique for VL-HIV cases, with reported sensitivities of 67 to 94% (7, 82, 160, 189). Observation of amastigotes in peripheral blood-stained smears is a noninvasive method that yields a positivity rate of 50 to 53% for coinfected patients (146, 153). Splenic aspiration is considered the most sensitive method for the diagnosis of VL, but the risk of hemorrhages cannot be discounted (approximately 0.1%). Therefore, this procedure has to be performed in equipped settings by experienced clinicians (124). Demonstration of the parasite in spleen or lymph node aspirates is a common procedure in countries where leishmaniasis is endemic and has also been applied to the diagnosis of coinfected patients (30, 143). Lymph node aspiration is less sensitive but still frequently used in Sudan, where lymph node enlargement is a common sign in VL patients (21, 277). Microscopic examination of hepatic biopsies has shown a sensitivity of 87% (160). Amastigotes can also be found in unusual locations, such as the lungs, larynx, tonsils, digestive tract, rectum, spinal fluid, and others (9, 175, 220).
A good microscopic diagnosis should be done on the basis of the observation of two slides of smears or touch preps from samples obtained by needle aspiration or biopsy stained with Giemsa stain or other Romanowsky-type stains. They should be examined for at least 1 hour, looking for amastigotes. The experience of the microscopist is crucial to the accurate diagnosis of VL. Nevertheless, false-negative results can be obtained due to the small number of Leishmania-infected cells as a consequence of pancytopenia. Parasitic load can also be affected by previous treatments with pentamidine or AMB against concomitant infections.
Culture.
The culture of splenic aspirates has shown a high sensitivity (63 to 100%) (141, 189) for Leishmania-HIV-coinfected patients, but due to the risk of internal bleeding, bone marrow aspiration is recommended because it is safer and has a similar sensitivity (50 to 100%) (9, 188). The culture of mononuclear peripheral blood cells reaches a sensitivity of 64 to 67% (140, 149). Cultures have to be examined every week by light microscopy, looking for promastigote forms, and subcultured into fresh medium. Cultures are considered negative if no flagellates are observed after 4 weeks.
One of the most remarkable features of coinfected patients is their tendency to relapse, which often causes them to refuse successive bone marrow aspirations, and therefore the option of noninvasive samples, such as blood, is extremely useful in the diagnosis of leishmaniasis for these patients.
Serological Diagnosis
Serological tests are simple, noninvasive methods but have limited diagnostic value because over 40% of coinfected individuals have no detectable specific antibody levels against Leishmania (9). This is probably the consequence of an oligoclonal B-cell response due to the absence of T cells that can recognize specific Leishmania antigens and make the presentation to the B cells. Nevertheless, seropositivity varies with the serological test employed. Therefore, it is recommended that at least two different serological tests are used for each patient in order to significantly increase the sensitivity of antibody detection (83).
The sensitivities of different serological techniques for the diagnosis of coinfected patients reported in the literature can be summarized as follows: 11 to 67% for indirect immunofluorescent antibody test (152, 163), 76 to 89% for enzyme-linked immunosorbent assay using crude antigen (80), 22 to 62% for enzyme-linked immunosorbent assay using rK39 antigen (80, 152), and 74 to 85% for immunoblotting (80, 152, 163). A high sensitivity (95%) of the direct agglutination test (DAT) for Ethiopian VL-HIV-coinfected patients has also been reported (114). Similar DAT results for Ethiopian patients were obtained by Oskam et al. (179) and Schoone et al. (233), using a fast agglutination screening test (a modified version of DAT performed within 3 hours with only one serum dilution), with sensitivities of 89% and 90% reported in the respective studies. The DAT has been validated in several areas of endemicity (57). Unfortunately, the technical requirements of the DAT procedure (e.g., micropipettes, microtiter plates, etc.) restrict its use to referral hospitals or well-supported health centers.
The rK39 dipstick test is a simple, fast, noninvasive serological method that has shown high sensitivity and specificity in the diagnosis of immunocompetent VL patients from different countries. Unfortunately, two different rK39 dipstick formats showed poor sensitivities, of 20% (CORIXA-IDRI, Seattle, WA) and 22% (ACON Laboratories, Bethlehem, PA), respectively, in the diagnosis of European coinfected patients (80). Studies on Leishmania-HIV-coinfected patients from countries where leishmaniasis is endemic are needed in order to assess the diagnostic value of the dipsticks under field conditions.
Serological cross-reactivity between Leishmania and other infectious agents, such as Trypanosoma and mycobacteria, has been reported widely for immunocompetent patients. Patients with visceral leishmaniasis can even have false-positive HIV test results. Nevertheless, a few false-positive results are less of a problem than are false-negative results, taking into account the high percentage of coinfected patients showing a partial, weak, or absent antibody response to Leishmania, as for other infections (152).
Antigen Detection
A new latex agglutination test (KAtex; Kalon Biological, United Kingdom), designed to detect Leishmania antigens in urine, was recently developed. KAtex was highly sensitive during clinical episodes when the parasitic load was high: in two studies of coinfected patients in Spain, the sensitivity was 85.7% and 100%, and the specificity in the second study was 96% (209, 264).
Riera et al. (209) found that KAtex was negative for coinfected patients who were considered cured (without amastigotes in bone marrow aspirates or blood after treatment), indicating that this test could be used as an infection marker. Furthermore, antigenuria becomes negative after successful chemotherapy, and no relapses were observed in the majority of these patients, showing that KAtex can be a useful tool for monitoring the efficacy of treatment. Coinfected patients usually suffer numerous relapses, and it is very difficult for them to achieve parasitological cure. Nevertheless, when antigen detection in urine was repeatedly negative after treatment, the probability of relapse was only 5% at 6 months. KAtex also detected Leishmania antigens in asymptomatic periods between relapses, indicating subclinical infection. These results are in agreement with those obtained by Sundar et al. (252) for immunocompetent VL patients from India, by El-Safi et al. (93) for Sudan, and by Cruz et al. (69) for pediatric patients from Spain. In a recent study undertaken in Spain, Leishmania antigen was undetected in the urine of HIV-positive asymptomatic Leishmania carriers by PCR, probably because of low levels of circulating parasites in these individuals (101).
Molecular Diagnosis
PCR is a useful technique that has been used for the detection of different Leishmania species. PCR protocols can be applied to numerous clinical samples, with a better performance than the classical parasitological methods. The analytical sensitivity is around 0.01 parasite per reaction, and homemade protocols are routinely used in many laboratories worldwide.
Leishmania PCR assays using bone marrow samples and peripheral blood as clinical specimens proved to be a reliable tool for the diagnosis of VL in HIV-positive patients. PCR sensitivity for bone marrow samples ranges from 82 to 100% (68, 131, 185), while blood samples offer a noninvasive alternative, with sensitivities ranging from 72 to 100% (53, 68, 97, 190). PCR is a useful technique for monitoring long-term efficacy of treatment and for prediction of relapses due to its high performance with noninvasive samples (16, 68, 210).
PCR has been applied to the detection and identification of Leishmania at different taxonomic levels and can even be used directly for clinical samples (232). Infections with other monoxenous trypanosomatids have been described for immunocompromised patients who displayed symptoms of CL or VL (58), which could contribute to false-positive results obtained by microscopy, culture, or even serological techniques, such as the indirect immunofluorescent antibody test. However, the excellent specificity associated with PCR overcomes this problem (58).
Real-time quantitative PCR (RTQ-PCR) was recently applied to the diagnosis and monitoring of Leishmania infections. Its main advantages include a reduction in the time needed for the assay and the possibility to quantify the parasitic load of the clinical sample. Based on small-subunit (SSU) rRNA gene amplification, Bossolasco et al. (45) obtained an analytical sensitivity of 0.625 parasite/ml and estimated that an increase in the parasitic load in peripheral blood above 10 parasites/ml preceded clinical relapse in Leishmania-HIV-coinfected patients after treatment. Using kinetoplast DNA as a target, Mary et al. (147) developed an RTQ-PCR with an analytical sensitivity of 0.001 parasite DNA equivalents/ml. RTQ-PCR analysis of blood samples from asymptomatic carriers of Leishmania in the Mediterranean area was able to detect disease in 58% of healthy subjects, compared with 16% detected by immunoblotting. Q-PCR with blood samples constitutes a noninvasive alternative to bone marrow aspiration in the diagnosis of leishmaniasis and represents a very sensitive tool for monitoring drug therapy and for follow-up in coinfected patients to confirm relapses.
An algorithm (Fig. 2) was recommended for the diagnosis of leishmaniasis in HIV-infected patients (WHO, presented at the Fifth Consultative Meeting on Leishmania-HIV Coinfection, Addis Ababa, Ethiopia, March 2007 [WHO/CDS/NTD/IDM/2007-7]).
CLINICAL ASPECTS OF LEISHMANIA-HIV COINFECTION
Clinical manifestations of leishmaniasis and Leishmania-HIV coinfection depend on both the infecting species of Leishmania and the cell-mediated immune response of the host. Data and studies on VL-HIV coinfection come mainly from Europe, where L. infantum is predominant: L. donovani is the infecting species in Africa and the Indian subcontinent. Data outside Europe are scarce, despite the increasing incidence of VL-HIV in these regions. Leishmania infection may remain asymptomatic, restricted to the skin in LCL and DCL and to the mucous membranes in MCL, but more commonly spreads systemically in VL. All forms, most notably VL, behave as opportunistic infections in immunocompromised HIV-infected people (9, 181).
In Southern Europe, 94% of patients with Leishmania-HIV coinfection suffered from VL, and 4% had CL (266). In East Africa and the Indian subcontinent, VL is the commonest form, but exact data are lacking. In Brazil, 43%, 37%, and 20% of the burden of coinfection are due to MCL, VL, and CL, respectively (199).
VL-HIV Coinfection
Clinical manifestations of VL caused by L. infantum and L. donovani in HIV-infected people are not significantly different from those in non-HIV-infected people (71, 133, 141, 143, 160, 166, 181, 188, 189, 205, 220, 224, 266). Classical features are fever, weight loss, hepatosplenomegaly, and pancytopenia. Localization of parasites in VL-HIV coinfection is broadly similar to that described for immunocompetent subjects (188, 189), although whether the frequency of leishmaniasis found in atypical locations is higher for VL-HIV-coinfected patients has not yet been confirmed with large comparative studies (220, 224).
At the time of diagnosis of the first episode of VL, 79 to 100% of HIV-positive patients coinfected with L. infantum had a CD4+ cell count of <200 cells/μl (133, 141, 166, 188, 189, 205, 224), and 42 to 72% of patients met the AIDS-defining criteria before or during the first episode of VL (133, 141, 160, 166, 189, 205). The CD4 counts of those with L. donovani infection are not published. The clinical presentations of VL in coinfected patients who have relapsed are comparable with initial episodes of VL (141, 189) and have not changed since HAART was introduced, except for the fact that the percentage of concomitant opportunistic infections has decreased (96, 265). Patients receiving HAART showed significantly lower frequencies of thrombocytopenia and leukopenia, as well as a lower frequency of increased liver enzyme levels, than did patients who did not receive HAART during episodes of VL (96).
In contrast to the clinical manifestations, the clinical course and prognosis of VL in HIV-infected individuals differ importantly from those in non-HIV-infected individuals. VL-HIV coinfection is characterized by significantly lower cure rates (143, 189, 216), higher drug toxicity (189, 215), higher relapse rates (9, 141, 188, 189, 215), and higher mortality rates (141, 189, 216) than those for VL in non-HIV-infected individuals.
In the period before HAART was available, cure rates in Europe and Africa after the first episode of VL in HIV-infected patients ranged from 56 to 90% (133, 141, 143, 189), but the impact of HAART on cure rates of VL in HIV-infected patients has not been established clearly.
Drug toxicity in HIV-related VL has become a well-documented problem. In an evaluation of pentavalent antimoniate treatment, adverse effects were observed in 56% of patients, and therapy had to be discontinued permanently due to serious adverse effects (mainly acute pancreatitis) in 28% of patients. A further 12% of patients died due to severe pancreatitis directly attributable to treatment (78). Although data from Africa and India are lacking, the high frequency of vomiting and mortality among antimonial-treated HIV-positive patients in Ethiopia suggests that similar toxicity occurs (215, 216). In addition, it has been demonstrated in vitro that sodium stibogluconate stimulates HIV-1 replication (22).
Relapses are an important feature of VL-HIV coinfection. If a patient does not receive HAART, relapse rates increase to 60% within 6 to 9 months posttreatment and to 90% within 12 months, with the mean interval length between subsequent relapses becoming shorter (138). In a comparative study by Pintado et al., a relapse rate of 56.6% occurred within 3 months after apparently successful treatment of VL (189). HAART with immune reconstitution and undetectable viral RNA loads does not prevent VL relapse (55, 96, 265). In patients receiving HAART, 80.6% had undetectable viral loads at the time of VL relapse (96). The exact impact of HAART and other factors on reducing relapse rates and the length of the interval between relapses has still to be determined. Some studies indicate that the period between relapses is prolonged by HAART (138, 156). Suffering a relapse increases the risk of a further relapse (265). This may be related to the poor increase in CD4+ cells observed in relapsing patients compared with that in nonrelapsing patients, despite complete suppression of HIV replication (77, 156).
HAART has greatly reduced the incidence of symptomatic first episodes of VL in Europe (89, 96, 222, 262), but this effect has not yet been seen in affected regions in South Asia or Africa, where access to free HAART is very limited. Demonstrated risk factors independently associated with the emergence of first episodes of VL, besides HAART, are CDC clinical category C and a CD4+ cell count of <300 cells/μl (262).
The mortality rate for VL-HIV-coinfected patients is much higher than that for HIV-negative VL patients. During a 1-year follow-up in a comparative study, 53.7% of HIV-positive patients died, compared with 7.5% of HIV-negative patients (P < 0.001). Factors that predicted survival of HIV-positive patients were HAART, a high CD4+ cell count, and the use of secondary prophylaxis for VL (189). Mortality during VL treatment is significantly higher among coinfected patients; a relative risk of 9.25 (P = 0.00005) was found in Ethiopia (216). Mortality during treatment is fourfold higher when antimonials are used than when miltefosine is used (215).
CL-HIV Coinfection
HIV-positive patients with CL should be examined carefully for the coexistence of VL. LCL in HIV-infected individuals tends to be associated with the initial stages of HIV infection and minimal immunosuppression and is clinically and histopathologically identical to LCL in non-HIV-infected individuals, with isolated papules or plaques observed on exposed areas. HIV-induced immunosuppression facilitates dissemination of amastigotes, leading to DCL that is usually, but not always (50, 62, 89), associated with VL (116, 170).
LCL and DCL are characterized by a higher rate of recurrence or reinfection and are more difficult to treat than CL in HIV-negative patients (29, 66). The incubation period does not seem to be affected by HIV status (99). The impact of HAART has not been studied.
MCL-HIV Coinfection
MCL is prevalent mainly in South America, but reports of coinfection with HIV are scarce. Sporadic cases have been described in Brazil (13, 42, 84) and other South American countries, as well as India (244), Spain (157), and Ethiopia (29). MCL may be severe in HIV-infected patients, with dissemination and a relapsing course.
PKDL and HIV Coinfection
PKDL is common in HIV-negative patients, appearing shortly after or even during treatment in 50% of VL cases in Sudan and, after a longer period, in 5 to 10% of VL cases in India (279). PKDL manifests as maculopapular or nodular lesions on the face, trunk, and limbs. Only a few cases of PKDL in HIV-positive patients have been reported in the literature (26, 211, 249). In Ethiopia, severe PKDL was more common in HIV-positive (27.3%) than in HIV-negative (13.3%) VL patients at a 6-month follow-up (216). Case reports of VL-HIV-coinfected patients have described cutaneous lesions that precede (159), accompany (18, 44, 64, 105), and follow (50, 56) VL after treatment. It is unclear whether these are forms of PKDL or parasitized skin lesions formed during the course of VL. In addition, an association between PKDL and immune reconstitution disease (IRD) soon after the start of HAART has been described (26, 103, 208). Interestingly, PKDL-IRD also occurs after VL caused by L. chagasi (38) and L. infantum (47, 208, 249), which are usually not associated with PKDL.
IRD in Leishmania-HIV Coinfection
One recent study suggests that patients with untreated subclinical VL do not develop symptomatic disease when started on HAART (77). There are, however, small numbers of reported possible cases of IRD. In France, two asymptomatic patients developed VL (L. infantum) within 2 weeks of HAART (37), while another report described a patient who had not been in a area of leishmaniasis endemicity for 8 years but who developed a first episode of VL following initiation of HAART (5). Furthermore, first episodes of VL were described for three severely immunocompromised patients, all with undetectable viral loads, who had just started HAART (122). A few possible cases of IRD with DCL (192), CL (128), and PKDL (26, 103, 208) have been described.
TREATMENT OF LEISHMANIASIS IN HIV-POSITIVE PATIENTS
The treatment of leishmaniasis in HIV-positive patients is characterized by a reduced number of therapeutic options. Drugs are inaccessible because of their price, lack of registration, toxicity, or ineffectiveness or because they have not yet been tested in these patients (Table 4) (10). There are few clinical trials analyzing the efficacy of the different treatments for Leishmania-HIV-coinfected patients (Table 5). In general, these patients have lower cure rates, higher drug toxicity rates, and higher fatality rates for leishmaniasis than do immunocompetent patients. Low CD4+ cell counts may prevent a full recovery, and multiple relapses often become unresponsive to all the previously used drugs. The treatment of coinfected patients is confounded by the scarcity of formalized clinical data. Another potential pitfall occurs when extrapolating treatment for L. donovani in Africa or Asia to the experience in Europe, where L. infantum probably has different drug susceptibilities and less virulence and seems to occur at lower CD4+ cell counts. Optimal treatment regimens have yet to be established for any region. A parasitological response to treatment is not indicative of an absence of future relapses (134, 135, 189), while a clinical response does not necessarily indicate parasitological clearance (141). Because recovery without relapses in immunodepressed patients has not yet been achieved, secondary prophylaxis must be considered, but there is little evidence of its efficacy.
TABLE 4.
Drugs used for treatment of VL
| Product | Brand name | Manufacturer | Areas of licensure for VLa | Price per unit | Standard treatment protocold |
|---|---|---|---|---|---|
| Sodium stibogluconate (pentavalent antimonial) | Pentostam | GlaxoSmithKline | Af, Am, Ind, Eur | 40 GBP (public sector price from GSK) per vial at 100 mg/ml (100 ml) | 20 MKD for 30 days |
| Albert David (India) | Af, Am, Ind, Eur | 3.25 Euros per vial at 100 mg/ml (30 ml) (via International Dispensary Association Amsterdam) | 20 MKD for 30 days | ||
| Meglumine antimoniate (pentavalent antimonial) | Glucantime | Sanofi-Aventis | Af, Am, Ind, Eur | US$1.20 per ampoule at 85 mg/5 ml (no profit-no loss price, agreed with WHO, for treatment of leishmaniasis) | 20 MKD for 30 days |
| AMB | Combinopharm (Spain) | Af, Am, Ind, Eur | US$1.91 per vial of 50 mg (236a) | 1 MKD for 15 days (alternate days) | |
| L-AMB | AmBisome | Gilead | US, Eur | US$20 per vial of 50 mg (reduced price, agreed with WHO, valid for public sector in developing countries for treatment of leishmaniasis) | 20-mg/kg total dose |
| ABLC | Abelcet | Zeneus | No | 82.13 GBP per vial of 100 mg/20 mlb | No standard treatment protocol but has been used in doses similar to those for L-AMB |
| L-AMB in colloidal suspension with cholesteryl sulfate | Amphocil | Beacon | No | 104.10 GBP per vial of 50 mgc | No standard treatment protocol but has been used in doses similar to those for L-AMB |
| L-AMB in emulsion | Amphomul | Bharat Serums and Vaccines (India) | Ind | US$10 per vial of 50 mg | 15-mg/kg total dose |
| Paromomycin | Gland Pharma (India) | Ind | US$10 for full course | 15 MKD for 21 days | |
| Miltefosine | Impavido | Aeterna Zentaris (Germany) | Af, Am, Ind, Eur | 108.50 Euros for 56 capsules of 50 mg for the public sector (www.medeor.org) | 100 mg/day for 28 days |
| Pentamidine mesylate | Pentamidine | Sanofi-Aventis | No | Pentamidine is free for the treatment of leishmaniasis (agreement with WHO) | Used for secondary prophylaxis (no known treatment protocol) |
Af, Africa; Am, America; In, Indian subcontinent; Eur, Europe; US, United States.
British National Formulary, March 2007.
P. Desjeux, Initiative for One World Health (www.iowh.org), personal communication.
MKD, milligrams per kilogram per day.
TABLE 5.
Treatment studies for Leishmania-HIV coinfection
| Region, parasite | Reference | Drugf | Regimen | No. of patients with initial cure (clinical and/or parasitological)/total no. of patients (%) | Severity of side effects | No. or % of dropouts | No. of recorded relapses/total no. of patients (%) | Study type |
|---|---|---|---|---|---|---|---|---|
| Europe, L. infantum | 134 | SbV | 20 mg/kg, 28 days | 29/44 (66) | Most serious (cardiotoxicity in six cases [one patient died] and pancreatitis in three cases) | 10 | 11/24 (46) | Randomized comparative trial |
| AMB | 28/45 (62) | Most serious (severe chills in 1 case, venous thrombosis in 1 case, and nephrotoxicity in 16 cases) | 15 | 8/24 (46) | ||||
| 78 | SbV | 20 mg/kg, 28 days | 5/25 (33)a | Most serious (pancreatitis in five cases, acute renal failure in one case, and leucopenia in one case) | 10 | 3/15 (20) | Retrospective study | |
| 135 | SbV | 20 mg/kg, 28 days | 7/19 (37) | Most serious (pancreatitis in four cases [all four patients died], renal failure in two cases [both patients died]) | 9 | 4/7 (57) | Randomized comparative trial | |
| ABLC | 3 mg/kg, 5 days | 6/18 (33) | Overall mild (seven cases of infusion-related reactions, one case of renal failure) | 1 | 2/4 (50) | |||
| ABLC | 3 mg/kg, 10 days | 8/20 (42) | Overall mild (eight cases of infusion-related reactions) | 2 | 3/8 (38) | |||
| 189 | SbV | 20 mg/kg, 3-4 weeks | 61b | Hyperamylasemia in 15.9% of patients, anemia in 14.7% of patients | 19% | No data per individual drug | Retrospective study | |
| AMB | 0.5-1 mg/kg, 3-4 weeks | 58b | Anemia in 29.4% of patients, renal failure in 17.6% of patients | 7% | No data per individual drug | |||
| Ethiopia, L. donovani | 31 | SbV | 20 mg/kg, 28 days | 17/23 (74) | No data | 0 | Not recorded | Prospective study |
| Europe, L. infantum | 141 | SbV | 20 mg/kg, 28 days | 42/51 (82)c | Hyperamylasemia in eight cases and cardiotoxicity in nine cases (one death) | Data not given | No data per individual drug | Retrospective study |
| AMB | At least 15-mg/kg total dose | 14/17 (82)d | Anemia in six cases and renal failure in five cases | Data not given | No data per individual drug | |||
| PENT | 4 mg/kg, 28 days | 2/3 (67) | One case of insulin-dependent diabetes | Data not given | No data per individual drug | |||
| 73 | L-AMB | 100 mg, 21 days | 11/11 (100) | No serious side effects; well tolerated | 0 | 8/11 (73) | Open-label dose finding | |
| 226 | L-AMB | 4 mg/kg on days 1 to 5, 10, 17, 24, 31, and 38 | 9/10 (100) | No serious side effects; well tolerated | 0 | 7/7 (100) | Open-label dose finding | |
| Ethiopia, L. donovani | 215 | MILT | 100 mg, 28 days | 56/63 (89) | Vomiting in 41 cases, 3 of which were serious; diarrhea in 34 cases | 3 | 16 of 52 (31) | Randomized comparative trial |
| SbV | 20 mg/kg, 40-60 days | 40/44 (90) | Vomiting in 20 cases, 7 of which were serious; diarrhea in 32 cases | 0 | 5/35 (14) | |||
| India, L. donovani | 243 | MILT | 100 mg, for a mean of 55 dayse | 25/39 (64) | Overall mild (vomiting in 10 cases, diarrhea in 4 cases) | Data not given | 22/25 (88) | Case series |
One of 25 cases was a relapse.
Fifty-one patients were started on pentavalent antimonials, and 17 were started on AMB, among whom 8 received L-AMB.
Allopurinol (three cases) and IFN-γ (one case) were added to therapy.
In four cases, L-AMB was used.
For two patients, the daily dose was 150 mg.
SbV, pentavalent antimonial; AMB, amphotericin B deoxycholate; L-AMB, liposomal AMB; ABLC, AMB lipid complex; PENT, pentamidine; MILT, miltefosine.
Antileishmania Drugs
Pentavalent antimonials.
Injectable pentavalent antimonials (sodium stibogluconate and meglumine antimoniate) (Table 4) have remained the mainstream treatment for VL since their introduction in the 1940s and are still highly effective, except in regions in India (Bihar) and Nepal, where resistance has rendered them almost useless (212, 255).
A first course of antimonials, at the WHO-recommended regimen of 20 mg/kg of body weight/day for 28 to 30 days, led to clinical and/or parasitological response in 33 to 82% of European coinfected patients, with relapses being common. The success rates in published studies vary greatly due to high levels of dropout and early death (78, 134, 135, 141, 189). Drug-induced pancreatitis was the most common cause of treatment discontinuation and death (78, 134, 135, 189). Serious electrocardiac changes have also been reported (135, 141). In Ethiopia, one-third of coinfected patients died during antimonial treatment (216). Mortality is clearly associated with antimonial therapy, which has a sixfold higher risk (P = 0.0003) of mortality than does miltefosine (215). Antimonials were also associated with a higher incidence of severe vomiting (215).
The cause of increased clinical pancreatitis with antimonials in coinfected patients is not clear (78). It is possible that antimonial toxicity selectively affects the sickest patients, such as those with VL-HIV coinfection, because the pentavalent antimonial is reduced to the toxic trivalent antimonial to a greater extent in these patients. Toxicity and high mortality during treatment render antimonials unsuitable as a first-line treatment for coinfected patients.
An additional disadvantage of antimonials is that they were shown to stimulate HIV-1 replication in vitro, a finding that merits further investigation (22).
AMB.
AMB has been used widely for the treatment of VL, mainly in India, where it is still highly effective after 10 years of extensive use (178). The risk of nephrotoxicity and hypokalemia necessitates hospitalization and, preferably, biochemical monitoring during treatment, which is difficult to achieve in resource-poor settings. AMB has already been abandoned in Western countries for the treatment of VL, in favor of safer and more effective lipid amphotericin preparations.
In vitro, AMB is a more potent antileishmanial than the antimonials, as its activity does not depend on the patient's immune response (9, 94, 169). However, in coinfected patients, its superiority over antimonials could not be demonstrated. Initial cure rates ranged from 58 to 82%, with regular relapses. The toxicity rates of both drugs were shown to be similar, with AMB causing renal toxicity in 18 to 36% of patients (134, 141, 189). As with the antimonials, the side effects of AMB in coinfected patients are more severe than those in noncoinfected patients.
Lipid formulations of AMB.
All lipid formulations of AMB show a better safety profile than that of AMB, with L-AMB (AmBisome; Gilead USA) considered superior to the other formulations. L-AMB has the highest therapeutic index of all antileishmanial drugs, including the other lipid AMB formulations (33). It is therefore indicated for the treatment of coinfected patients. The limited data on the use of L-AMB in coinfected patients were generated mostly in Europe. In other regions, L-AMB is prohibitively expensive, even though it is now available for a nonprofit cost of $20 per vial for VL in the developing world (Table 4).
For immunocompetent patients, no treatment failures have been observed with the currently recommended total dose of 20 mg/kg (33), except in Sudan. Sudanese patients without HIV were less responsive to L-AMB than were Europeans or Indians: the cure rates for total doses of ≤15 mg/kg, 16 to 20 mg/kg, and >20 mg/kg were 50%, 64%, and 88%, respectively (235). In another study, 10 of 64 Sudanese patients did not respond to treatment with L-AMB (20 mg/kg). This was thought to be related to high initial parasite loads and immunosuppressing underlying diseases (HIV infection and tuberculosis), and it was suggested that higher doses should have been used (165). In Europe, total doses of up to 30 to 40 mg/kg have been evaluated in small numbers of coinfected patients and were well tolerated, but they did not prevent relapses (73, 226). A dosing recommendation for coinfected patients cannot be made based on the limited data available. Since the half-life of L-AMB that has accumulated in the spleen, liver, and bone marrow is estimated to be at least 2 to 3 weeks (106), a prolonged high-dose regimen may be necessary to avoid the selection of resistant parasites.
Of the other lipid forms of AMB, AMB lipid complex (ABLC) has been used for secondary prophylaxis, administered every 21 days for 12 months. ABLC was well tolerated, and after 1 year, 22% of patients had relapsed, compared with 50% of patients without secondary prophylaxis (142). Data on secondary prophylaxis with L-AMB are anecdotal (161). An inexpensive lipid emulsion is manufactured in India (Amphomul; Bharat Sera and Vaccines) (Table 4), which is encouraging news for the treatment of VL, but it has not yet been evaluated in coinfected patients.
Miltefosine.
Treatment with miltefosine has consistently been shown to be safe and effective (255a). Relatively mild gastrointestinal side effects are common. A study of 299 Indian patients showed that vomiting occurred in 38% and diarrhea occurred in 20% of patients and generally lasted 1 to 2 days (253); none of these patients were coinfected. A major pitfall of miltefosine is its potential teratogenic effect, which impedes its use in pregnant or lactating women and women of childbearing potential not taking contraceptives.
In Ethiopia, side effects with miltefosine are worse in HIV-positive patients; vomiting occurred in 65% of coinfected patients, compared to 45% of noncoinfected patients. Miltefosine was used in 39 coinfected patients from Europe who had relapsed on previous treatments. Cure was achieved in 64% of patients, but almost all patients relapsed again and were retreated, with moderate success. It was found that prolonged treatment was safe, with one patient receiving treatment for 2 years (243). In Ethiopia, miltefosine was found to be less effective than antimonials in coinfected patients, with 18% versus 2% of patients failing initial treatment and 25% versus 11% relapsing within 6 months in the miltefosine and antimonial groups, respectively. Overall, mortality in the miltefosine group (6%) was lower than that in the antimonial group (12%) (215).
Miltefosine has a half-life of ∼1 week, so especially in relapsing coinfected patients, there is a risk of resistant parasites developing (32), as generated in vitro (239). As with other drugs, the use of miltefosine in coinfected patients should be prolonged until parasite clearance is achieved. In India, where large-scale miltefosine distribution is planned within the context of an elimination program, controlled use and knowledge of the HIV status of patients are of crucial importance (255a). In Europe and other zones where VL transmission is zoonotic, the use of miltefosine (and other first-line drugs) should not be allowed in dogs to prevent the development of primary resistant strains (255a).
Paromomycin.
Paromomycin sulfate was recently licensed for the treatment of VL on the basis of a large phase III trial, where it was shown to be as effective as AMB and was very well tolerated; the main side effects were a reversible elevation of liver enzymes, in approximately 1% of patients, and pain at the injection site (254). Paromomycin is the cheapest of all antileishmanial drugs (Table 4). Paromomycin has a good safety profile and is a broad-spectrum antibiotic active against some gram-positive and most gram-negative bacteria, many protozoa, and Mycobacterium tuberculosis (125). Its activity in coinfected patients has yet to be established. Acquired resistance may easily develop (67, 98, 144) and has been generated in vitro. There has been extensive, favorable experience with combinations of paromomycin plus sodium stibogluconate, with 224 patients receiving a combination in three randomized clinical trials (60, 237, 257), as have thousands of patients treated under field conditions (154). However, data for coinfected patients are lacking.
Pentamidine.
Pentamidine was used to treat VL mainly in India but has now been abandoned due to the severity of its side effects and to poor efficacy. Irreversible diabetes mellitus is a serious complication, occurring in 4 to 12% of cases (178). After a decade of use, the efficacy has declined to <70% (67). The scope of safe drugs to treat coinfected patients is limited, and thus these drugs are not to be used for secondary prophylaxis but reserved for treatment of acute cases. Pentamidine, although toxic in treatment doses, has been considered for use in secondary prophylaxis (183), as intermittent low-dose maintenance therapy is unlikely to show the toxicity seen with a therapeutic dosing regimen.
Following a recent agreement between WHO and the manufacturer (Sanofi-Aventis), pentamidine is now available for free for the treatment of all neglected diseases, including leishmaniasis (Table 4).
Combinations.
There is consensus that combination therapy for VL should urgently be introduced to minimize the development of resistant strains (48, 110). This is especially true for coinfected patients, as repeated exposure to single antileishmanial drugs will inevitably generate resistance, and incurable VL patients (158) or PKDL patients (1) may transmit drug-resistant parasites. Although no clinical trials to date have investigated combination therapies in coinfected patients, physicians may use combination therapy in patients with multiple relapses on a compassionate basis. Combinations of miltefosine plus paromomycin, pentavalent antimonials, and AMB were studied in vivo and in vitro; miltefosine plus paromomycin and miltefosine plus AMB were synergistic and should progress to clinical testing (238). In coinfected patients, even if these combinations do not prevent relapse, they may preserve drug sensitivity in individual patients and therefore prolong survival.
Antiretrovirals
Since 1996, the introduction of HAART in Europe has led to far fewer new VL infections in HIV-positive patients. HAART has reduced the risk of relapse in coinfected patients, although it is not clear to what extent (55, 77, 96, 138, 156, 265). These results cannot be extrapolated to the developing world, where the condition of patients is much worse and the L. donovani species is highly virulent. Nonetheless, it is clear that HAART reduces the morbidity and mortality of coinfected patients in all regions. In some areas with a high incidence of coinfection (Bihar, India; Ethiopia; and Eastern Sudan), access to HAART remains minimal. HAART is frequently restricted to nongovernmental organizations (NGOs), programs that cover small numbers of patients, while government programs are absent, malfunctioning, or at the first stage of implementation (e.g., in Ethiopia). Only relatively few coinfected patients in developing countries will be included in well-functioning HAART programs. Where CD4+ cell counts are difficult to obtain, VL should therefore be regarded as a valid entry point for HAART. For the African region, VL has been defined as an AIDS-defining disease, which is a pragmatic approach that should be adopted globally (http://www.who.int/hiv/pub/guidelines/clinicalstaging.pdf).
Indinavir and saquinavir show in vitro activity against L. infantum and L. major (33, 193, 229), but there is currently no clinical evidence of any HAART being more effective than others in preventing VL relapses in coinfected patients. Thus, the choice of HAART for coinfected patients does not differ from that in national programs for HIV.
Other Approaches
It has been suggested that in the absence of an adequate immune response, the addition of IFN-γ or recombinant IL-2 to VL therapy could be useful. However, both have not yet shown any additional benefit (46, 132). Selective splenectomy has been evaluated for relapsing coinfected patients, but despite being effective in restoring hematological parameters and reducing the need for blood transfusions, it did not prevent further relapses (261); in addition, this procedure should be avoided because of the risk of overwhelming sepsis and severe malaria.
MCL and CL
Evidence to support different treatments is very limited for HIV-negative CL patients (129, 145) and is absent for immunocompromised HIV-coinfected patients.
In general, to reduce the probability of dissemination and relapse in CL-HIV-coinfected patients, systemic treatment is recommended over local treatment, with close monitoring and follow-up of the patient. As long as evidence is lacking, the same treatment used for immunocompetent individuals will be offered to localized CL-HIV-coinfected patients. Reports of the treatment of HIV-associated MCL are scarce, although the cure of MCL following treatment with L-AMB has been described for a coinfected patient failing antimonial treatment (13). Miltefosine has been used effectively for treatment of PKDL in HIV-infected patients (26).
FOLLOW-UP OF PATIENTS AND MAINTENANCE THERAPY
Leishmania infection exacerbates the evolution of HIV through an increase of HIV replication and a decrease of the CD4+ lymphocyte count. In fact, about half of coinfected patients develop full AIDS criteria within 2 months after the diagnosis of VL. Furthermore, the course of VL in HIV-positive patients is characterized by the appearance of numerous relapses despite effective antileishmanial treatment. The number of relapses and the average time between them depend mainly on the immunological status of the patient (mainly defined by the CD4+ cell count and definitely influenced by HAART) and on the use of antileishmanial maintenance therapy. However, the different evolution of VL among patients suggests that other factors, such as parasitological variability, pathogenic strength of the infecting strain, or the existence of any resistance to antileishmanial drugs, can influence treatment success (87, 95, 218).
The mortality rate for European patients during a first episode of VL is 10 to 19%, which can increase to 24% during the month following the end of treatment, and is related to the toxicity of the treatment, complications arising during the VL episode, and concomitant opportunistic infections. The survival time varies from 3 to 24 months (average survival rate of 60% after 12 months) but can triple if the patient is treated with highly active HAART. After a correctly treated initial episode of VL, 25 to 61% of patients will relapse before 6 to 9 months, and 79 to 97% will relapse during the patient's lifetime (independent of the drug used to treat the first VL episode), with the average period between relapses becoming increasingly shorter (141, 188, 189).
There are three main points to consider in following up an HIV-positive patient who was recently diagnosed and treated for an episode of VL, as follows: (i) the need for test of cure after treatment and prediction/diagnosis of relapse, (ii) prompt initiation of effective HAART, and (iii) the convenience of secondary prophylaxis with an antileishmanial drug as maintenance therapy.
Test of Cure and/or Relapse
In treating immunocompetent patients, it is recognized that tests of cure are performed 1 month and 6 months after the finish of antileishmanial treatment in order to assess parasitological cure. Bone marrow or spleen aspiration is the technique usually performed, and diagnosis of VL is made when Leishmania sp. amastigotes are seen in Giemsa-stained samples or promastigotes are cultured in specific medium. For HIV-positive patients, though, parasitological cure is very difficult to achieve and relapses are very common, so the need for repeated invasive tests of cure could be very uncomfortable or dangerous for these patients. Repeated invasive diagnostic tests should be performed if there is no clinical improvement after treatment or whenever there is a suspicion of VL relapse.
PCR-based assays are useful tools for the diagnosis of VL in coinfected patients (16, 45, 68, 131, 185, 190, 210). The analysis of peripheral blood samples using PCR can be a useful noninvasive technique for monitoring patients posttreatment, which avoids unnecessary pain to the patient in evaluating the parasitic evolution during follow-up (16, 45, 68, 131, 185, 190, 210). PCR is a sensitive technique for detecting relapses several weeks before the clinical onset of disease. Leishmania DNA levels correlate with the clinical course of VL, and their measurement at diagnosis and during and after treatment seems to be useful in the clinical management of VL-HIV-coinfected patients. Positive nested PCR results during asymptomatic periods indicate the presence of the parasite, but not necessarily relapse (16, 45, 68, 131, 185, 190, 210). However, the presence of viable parasites during posttreatment follow-up increases the probability of relapse and could be a good marker of relapse (16, 45, 68, 131, 185, 190, 210). During relapse of VL, the parasite is detected more effectively in blood samples by nested PCR than by culture.
Antigen detection in urine with a latex agglutination test could represent an alternative noninvasive and easy-to-perform test for the diagnosis of leishmaniasis (sensitivity of 86%) and posttreatment follow-up in coinfected patients. In the absence of clinical symptoms, the detection of parasite antigens in urine samples is not associated with clinical disease in more than one-half of cases, and when antigen detection in urine is repeatedly negative, the probability of relapse is very low (5% at 6 months) (209).
Antiretroviral Therapy
HAART has dramatically modified the natural history of HIV infection and associated opportunistic infections. Despite the positive data associated with the use of these drugs, the benefits of HAART apply to only a minority of coinfected patients in the developing world. The effects of HAART on coinfected patients can be summarized as follows (77, 138, 139, 148, 156, 225, 262, 265). (i) The incidence of new VL cases in HIV-positive patients dropped about 50 to 65% in the Mediterranean area after HAART was introduced. HAART prevents future clinical VL in asymptomatic Leishmania sp.-infected patients. (ii) Coinfected patients who receive HAART have a higher survival rate than those who do not receive it (mean survival of 66 months). (iii) HAART modifies the pattern of VL relapse but is not sufficient to prevent the relapse of the disease. Relapsing VL is possible in HIV-infected patients receiving successful HAART, mainly when CD4+ cell levels are <200 cells/μl, but even if a very low viral load is achieved. About 40% (25 to 70%) of coinfected patients receiving HAART without VL maintenance therapy experience relapse, but HAART delays VL relapse, with a longer time between VL episodes (average of 7 months), in patients who receive HAART compared with those not receiving HAART. (iv) The whole possible clinical spectrum of leishmaniasis has been observed in HIV-positive patients, and atypical clinical forms have been observed no more frequently in patients receiving HAART. There is no correlation between the introduction of HAART and the occurrence of relapses, and the phenomenon of immune restoration syndrome is rarely observed (39, 122).
Maintenance Therapy (Secondary Prophylaxis)
Primary prophylaxis is not indicated. On the other hand, it seems advisable to use maintenance therapy systematically and soon after the first episode of VL to prevent early relapse, which would perpetuate a Th2-type response in cellular immunity and prevent the control of parasitization by Leishmania spp. despite effective HAART. The data about maintenance therapy come from the Mediterranean area, where VL is a zoonotic disease caused by L. infantum and where there are medical facilities for the follow-up of patients (136). Several questions arise when maintenance therapy is prescribed in other settings where medical care is insufficient for monitoring toxicity (mainly with antimonials) or where VL is an anthroponotic disease (Sudan, Ethiopia, and India) and there is the risk of inducing drug resistance (67). If maintenance therapy is provided in such situations, it should be conducted under a directly observed treatment program (particularly if miltefosine is the chosen drug).
There are enough accumulated data about the benefits of maintenance therapy in coinfected patients (156, 182, 188, 189, 207), but they are based on open-label, noncontrolled studies. In studies which failed to demonstrate the benefit of prophylaxis, patients tended to have more serious infection or had relapsed more often (133). In the only prospective and randomized study to investigate the effectiveness of a maintenance therapy, ABLC (3 mg/kg every 21 days) was compared with nonmaintenance therapy. At 12 months of follow-up, the benefit of the maintenance therapy was evident in the intention-to-treat analysis; the probability of being free of illness at 12 months was 50% and 22% for the groups with and without maintenance therapy, respectively (142).
Different regimens with several drugs have been used, mainly with pentavalent antimonials (20 mg/kg/day, given every 3 to 4 weeks), AMB (either L-AMB or ABLC) (3 to 5 mg/kg/day, given every 3 to 4 weeks), or pentamidine (4 mg/kg/day [300 mg for an adult], given every 3 to 4 weeks) (43).
Miltefosine is a very effective oral drug against VL (119, 234, 253, 259). There are no data about maintenance therapy with this drug for humans, but once- or twice-weekly oral administration to T-cell-deficient nude mice infected with L. donovani was useful as maintenance therapy (167). However, miltefosine requires a long treatment course (28 days) and has a long half-life (around 150 h), which might accelerate the emergence of drug resistance (184). Other oral drugs, such as itraconazole and allopurinol, have some therapeutic efficacy against Leishmania spp. and could hypothetically be used in maintenance therapy, together with miltefosine, to increase efficacy or prevent the appearance of resistance (15).
Once a patient's immune function has recovered with HAART and VL is quiescent, prophylaxis therapy could be suspended provided that the CD4+ cell count is maintained (>200 cells/μl) for more than 6 months (28, 248).
PERSPECTIVES IN LEISHMANIA-HIV COINFECTION
The spread and overlap of both leishmaniasis and HIV infections in the major foci of leishmaniasis (India, Brazil, and Eastern Africa) make VL-HIV coinfection a serious worldwide concern. HIV and VL programs should develop integrated and well-coordinated intervention activities, particularly in areas where VL is endemic. Collaboration of the two programs should particularly be strengthened by local government at the district level to focus on the specific circumstances of each area of endemicity. The mobility of people, such as seasonal migrant laborers, urban migration from rural areas, resettlement activities from areas where disease is nonendemic to those where it is endemic, and the presence of refugees and internal population displacements due to war and conflicts constitute major factors for the spread of both diseases. There is a need to develop locally applicable strategies for appropriate intervention in migrant communities.
In areas where transmission is anthroponotic, VL-HIV-coinfected patients should be targeted as potential reservoirs of infection. Preventing the transmission of L. donovani is mandatory by providing bed nets. Furthermore, it may be prudent to encourage HIV-positive patients to move from areas of VL endemicity to prevent them from becoming infected with VL. In anthroponotic transmission areas, more studies are required to provide sufficient evidence to recommend maintenance/secondary prophylaxis treatment, and the risk of resistance must also be considered in this situation.
Both HIV and Leishmania infections induce a deficit in host humoral and cellular responses that limits the diagnostic value of serological tests for coinfected patients. Only 40 to 50% of VL-HIV-coinfected patients have detectable specific antibody levels against Leishmania. There is a need for comparative analysis studies from different geographical areas, using different serological techniques, including CD4+ counts, to characterize serum samples. The high parasitic burden of leishmaniasis in HIV-infected individuals permits the detection of Leishmania antigens, but there is only one technique currently available for antigen detection (KAtex, used for urine samples). Research into other antigen detection tests is needed to evaluate their use as active phase markers that allow the detection of parasitological cure and relapse. In addition, more research is needed to link the clinical and parasitological conditions and to establish better criteria for cure, considering the poor prognosis of coinfection and the high risk of relapse.
VL is an opportunistic infection in HIV-infected individuals and should be considered in the definition of stage IV in the WHO HIV/AIDS classification (stage C of the CDC classification). It is crucial to try to restore cell-mediated immunity with HAART as soon as possible to prevent further relapses of VL, even though HAART alone is not enough to prevent VL relapse.
All antileishmanial therapies are less effective in HIV-positive patients. There is a high mortality rate due to concurrent illness, complications, and drug toxicity. Pentavalent antimonials and AMB are more toxic to HIV patients, who require close monitoring for pancreatitis, cardiotoxicity, and nephrotoxicity, and these drugs should be avoided if better drugs, such as liposomal formulations of AMB, are available. In considering combination therapy, drugs should be administered sequentially (with the safest given first) rather than concurrently. Miltefosine is a safer drug for coinfected patients, although there are still problems of teratogenicity and adherence to consider. In general, patients who fail to clear the parasite will relapse, independent of the drug used. Relapses should be treated appropriately, and combination therapy may represent the best approach to avoid drug resistance while balancing benefit with drug toxicity. Drugs used for relapse treatment should be avoided for secondary prophylaxis, although the drug panoply is very limited. Secondary prophylaxis to prevent relapses in areas with zoonotic transmission of L. infantum has been reported in several publications, but more evidence from clinical trials is needed to establish a beneficial effect. Treatment options for secondary prophylaxis in VL-HIV-coinfected patients in anthroponotic transmission areas (L. donovani) are limited, and the risk of resistance must be taken into account. The use of promising new drugs, such as miltefosine, for canine leishmaniasis can also accelerate the development of resistance, and thus their use in dogs should be avoided to protect their efficacy in humans.
The priorities of treatment-related research should include the evaluation of efficacy and tolerability of alternative drugs, such as paromomycin, pentamidine (maintenance therapy only), and combinations with currently available drugs, in coinfected patients. Possible benefits to achieve include a shortened duration of treatment, improved efficacy, cost reduction, protection of drug resistance, and improved compliance. The toxicity of combination therapy may be enhanced in coinfected patients and so should be evaluated thoroughly in well-conducted clinical trials. The only combination that has demonstrated a positive result so far is sodium stibogluconate plus paromomycin. Confirmatory clinical trials are currently ongoing in East Africa to establish clear criteria on the use of maintenance therapy.
Acknowledgments
We are indebted to all of the participants of the Fifth Informal Consultative Meeting on Leishmania-HIV Coinfection, held in Addis Ababa, Ethiopia, in April 2007, and special thanks go to L. Campino, Portugal, A. N. Elkhoury, Brazil, S. Sundar, India, R. Guiguemdé, Burkina Faso, K. Ritmeijer, Holland, and R. Davidson, United Kingdom, for providing useful information or comments.
Special recognition is given to the Spanish Agency for International Cooperation (AECI) for supporting this initiative.
REFERENCES
- 1.Addy, M., and A. Nandy. 1992. Ten years of kala-azar in west Bengal. I. Did post-kala-azar dermal leishmaniasis initiate the outbreak in 24-Parganas? Bull. W. H. O. 70:341-346. [PMC free article] [PubMed] [Google Scholar]
- 2.Akilov, O. E., A. Khachemoune, and T. Hasan. 2007. Clinical manifestations and classification of Old World cutaneous leishmaniasis. Int. J. Dermatol. 46:132-142. [DOI] [PubMed] [Google Scholar]
- 3.Akuffo, H., K. Maasho, M. Blostedt, B. Hojeberg, S. Britton, and M. Bakhiet. 1997. Leishmania aethiopica derived from diffuse leishmaniasis patients preferentially induce mRNA for interleukin-10 while those from localized leishmaniasis patients induce interferon-gamma. J. Infect. Dis. 175:737-741. [DOI] [PubMed] [Google Scholar]
- 4.Akuffo, H., E. Schurr, G. Andersson, T. Yamaneberhan, and S. Britton. 1987. Responsiveness in diffuse versus local cutaneous leishmaniasis is due to parasite differences. Scand. J. Immunol. 26:717-721. [DOI] [PubMed] [Google Scholar]
- 5.Albrecht, H. 1998. Leishmaniosis—new perspectives on an underappreciated opportunistic infection. AIDS 12:2225-2226. [DOI] [PubMed] [Google Scholar]
- 6.Albrecht, H., I. Sobottka, C. Emminger, H. Jablonowski, G. Just, A. Stoehr, T. Kubin, B. Salzberger, T. Lutz, and J. van Lunzen. 1996. Visceral leishmaniasis emerging as an important opportunistic infection in HIV-infected persons living in areas nonendemic for Leishmania donovani. Arch. Pathol. Lab. Med. 120:189-198. [PubMed] [Google Scholar]
- 7.Altes, J., A. Salas, M. Riera, M. Udina, A. Galmes, J. Balanzat, A. Ballesteros, J. Buades, F. Salva, and C. Villalonga. 1991. Visceral leishmaniasis: another HIV-associated opportunistic infection? Report of eight cases and review of the literature. AIDS 5:201-207. [PubMed] [Google Scholar]
- 8.Alvar, J., S. Bashaye, D. Argaw, I. Cruz, P. Aparicio, A. Kassa, G. Orfanos, F. Parreno, O. Babaniyi, N. Gudeta, C. Canavate, and C. Bern. 2007. Kala-azar outbreak in Libo Kemkem, Ethiopia: epidemiologic and parasitologic assessment. Am. J. Trop. Med. Hyg. 77:275-282. [PubMed] [Google Scholar]
- 9.Alvar, J., C. Canavate, B. Gutierrez-Solar, M. Jimenez, F. Laguna, R. Lopez-Velez, R. Molina, and J. Moreno. 1997. Leishmania and human immunodeficiency virus coinfection: the first 10 years. Clin. Microbiol. Rev. 10:298-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alvar, J., S. Croft, and P. Olliaro. 2006. Chemotherapy in the treatment and control of leishmaniasis. Adv. Parasitol. 61:223-274. [DOI] [PubMed] [Google Scholar]
- 11.Alvar, J., B. Gutierrez-Solar, R. Molina, R. Lopez-Velez, A. Garcia-Camacho, P. Martinez, F. Laguna, E. Cercenado, and A. Galmes. 1992. Prevalence of Leishmania infection among AIDS patients. Lancet 339:1427. [DOI] [PubMed] [Google Scholar]
- 12.Alvar, J., S. Yactayo, and C. Bern. 2006. Leishmaniasis and poverty. Trends Parasitol. 22:552-557. [DOI] [PubMed] [Google Scholar]
- 13.Amato, V. S., A. C. Nicodemo, J. G. Amato, M. Boulos, and V. A. Neto. 2000. Mucocutaneous leishmaniasis associated with HIV infection treated successfully with liposomal amphotericin B (AmBisome). J. Antimicrob. Chemother. 46:341-342. [DOI] [PubMed] [Google Scholar]
- 14.Andrade-Narvaez, F. J., S. Medina-Peralta, A. Vargas-Gonzalez, S. B. Canto-Lara, and S. Estrada-Parra. 2005. The histopathology of cutaneous leishmaniasis due to Leishmania (Leishmania) mexicana in the Yucatan Peninsula, Mexico. Rev. Inst. Med. Trop. Sao Paulo 47:191-194. [DOI] [PubMed] [Google Scholar]
- 15.Angarano, G., P. Maggi, S. L. Coppola, and R. L. Cavaliere. 1998. Itraconazole as maintenance therapy for visceral leishmaniasis in HIV-infected patients. Eur. J. Clin. Microbiol. Infect. Dis. 17:365-367. [DOI] [PubMed] [Google Scholar]
- 16.Antinori, S., S. Calattini, E. Longhi, G. Bestetti, R. Piolini, C. Magni, G. Orlando, M. Gramiccia, V. Acquaviva, A. Foschi, S. Corvasce, C. Colomba, L. Titone, C. Parravicini, A. Cascio, and M. Corbellino. 2007. Clinical use of polymerase chain reaction performed on peripheral blood and bone marrow samples for the diagnosis and monitoring of visceral leishmaniasis in HIV-infected and HIV-uninfected patients: a single-center, 8-year experience in Italy and review of the literature. Clin. Infect. Dis. 44:1602-1610. [DOI] [PubMed] [Google Scholar]
- 17.Antonelli, L. R., W. O. Dutra, R. P. Almeida, O. Bacellar, E. M. Carvalho, and K. J. Gollob. 2005. Activated inflammatory T cells correlate with lesion size in human cutaneous leishmaniasis. Immunol. Lett. 101:226-230. [DOI] [PubMed] [Google Scholar]
- 18.Ara, M., C. Maillo, G. Peon, A. Clavel, J. Cuesta, M. P. Grasa, and F. J. Carapeto. 1998. Visceral leishmaniasis with cutaneous lesions in a patient infected with human immunodeficiency virus. Br. J. Dermatol. 139:114-117. [DOI] [PubMed] [Google Scholar]
- 19.Arya, S. C., and N. Agarwal. 2005. HIV/AIDS and leishmaniasis coinfection in Ethiopia. CMAJ 173:1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ashford, R. W., M. A. Bray, M. P. Hutchinson, and R. S. Bray. 1973. The epidemiology of cutaneous leishmaniasis in Ethiopia. Trans. R. Soc. Trop. Med. Hyg. 67:568-601. [DOI] [PubMed] [Google Scholar]
- 21.Babiker, Z. O., R. Davidson, C. Mazinda, S. Kipngetich, and K. Ritmeijer. 2007. Utility of lymph node aspiration in the diagnosis of visceral leishmaniasis in Sudan. Am. J. Trop. Med. Hyg. 76:689-693. [PubMed] [Google Scholar]
- 22.Barat, C., C. Zhao, M. Ouellette, and M. J. Tremblay. 2007. HIV-1 replication is stimulated by sodium stibogluconate, the therapeutic mainstay in the treatment of leishmaniasis. J. Infect. Dis. 195:236-245. [DOI] [PubMed] [Google Scholar]
- 23.Barral, A., R. Badaro, M. Barral-Netto, G. Grimaldi, Jr., H. Momem, and E. M. Carvalho. 1986. Isolation of Leishmania mexicana amazonensis from the bone marrow in a case of American visceral leishmaniasis. Am. J. Trop. Med. Hyg. 35:732-734. [DOI] [PubMed] [Google Scholar]
- 24.Barral, A., D. Pedral-Sampaio, G. Grimaldi Junior, H. Momen, D. McMahon-Pratt, A. Ribeiro de Jesus, R. Almeida, R. Badaro, M. Barral-Netto, E. M. Carvalho, et al. 1991. Leishmaniasis in Bahia, Brazil: evidence that Leishmania amazonensis produces a wide spectrum of clinical disease. Am. J. Trop. Med. Hyg. 44:536-546. [DOI] [PubMed] [Google Scholar]
- 25.Barreto-de-Souza, V., G. J. Pacheco, A. R. Silva, H. C. Castro-Faria-Neto, P. T. Bozza, E. M. Saraiva, and D. C. Bou-Habib. 2006. Increased Leishmania replication in HIV-1-infected macrophages is mediated by Tat protein through cyclooxygenase-2 expression and prostaglandin E2 synthesis. J. Infect. Dis. 194:846-854. [DOI] [PubMed] [Google Scholar]
- 26.Belay, A. D., Y. Asafa, J. Mesure, and R. N. Davidson. 2006. Successful miltefosine treatment of post-kala-azar dermal leishmaniasis occurring during antiretroviral therapy. Ann. Trop. Med. Parasitol. 100:223-227. [DOI] [PubMed] [Google Scholar]
- 27.Bentwich, Z. 2003. Concurrent infections that rise the HIV viral load. J. HIV Ther. 8:72-75. [PubMed] [Google Scholar]
- 28.Berenguer, J., J. Cosin, P. Miralles, J. C. Lopez, and B. Padilla. 2000. Discontinuation of secondary anti-leishmania prophylaxis in HIV-infected patients who have responded to highly active antiretroviral therapy. AIDS 14:2946-2948. [DOI] [PubMed] [Google Scholar]
- 29.Berhe, N., A. Hailu, and T. Gemetchu. 1995. Human immunodeficiency virus and recurrence of cutaneous leishmaniasis long after healed localized cutaneous leishmaniasis due to Leishmania aethiopica. Trans. R. Soc. Trop. Med. Hyg. 89:400-401. [DOI] [PubMed] [Google Scholar]
- 30.Berhe, N., A. Hailu, D. Wolday, Y. Negesse, P. Cenini, and D. Frommel. 1995. Ethiopian visceral leishmaniasis patients co-infected with human immunodeficiency virus. Trans. R. Soc. Trop. Med. Hyg. 89:205-207. [DOI] [PubMed] [Google Scholar]
- 31.Berhe, N., D. Wolday, A. Hailu, Y. Abraham, A. Ali, T. Gebre-Michael, P. Desjeux, A. Sonnerborg, H. Akuffo, and S. Britton. 1999. HIV viral load and response to antileishmanial chemotherapy in co-infected patients. AIDS 13:1921-1925. [DOI] [PubMed] [Google Scholar]
- 32.Berman, J., A. D. Bryceson, S. Croft, J. Engel, W. Gutteridge, J. Karbwang, H. Sindermann, J. Soto, S. Sundar, and J. A. Urbina. 2006. Miltefosine: issues to be addressed in the future. Trans. R. Soc. Trop. Med. Hyg. 100(Suppl. 1):S41-S44. [DOI] [PubMed] [Google Scholar]
- 33.Bern, C., J. Adler-Moore, J. Berenguer, M. Boelaert, M. den Boer, R. N. Davidson, C. Figueras, L. Gradoni, D. A. Kafetzis, K. Ritmeijer, E. Rosenthal, C. Royce, R. Russo, S. Sundar, and J. Alvar. 2006. Liposomal amphotericin B for the treatment of visceral leishmaniasis. Clin. Infect. Dis. 43:917-924. [DOI] [PubMed] [Google Scholar]
- 34.Bern, C., and R. Chowdhury. 2006. The epidemiology of visceral leishmaniasis in Bangladesh: prospects for improved control. Indian J. Med. Res. 123:275-288. [PubMed] [Google Scholar]
- 35.Bernier, R., B. Barbeau, M. J. Tremblay, and M. Olivier. 1998. The lipophosphoglycan of Leishmania donovani up-regulates HIV-1 transcription in T cells through the nuclear factor-kappaB elements. J. Immunol. 160:2881-2888. [PubMed] [Google Scholar]
- 36.Bernier, R., S. J. Turco, M. Olivier, and M. Tremblay. 1995. Activation of human immunodeficiency virus type 1 in monocytoid cells by the protozoan parasite Leishmania donovani. J. Virol. 69:7282-7285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berry, A., B. Abraham, J. Dereure, V. Pinzani, P. Bastien, and J. Reynes. 2004. Two case reports of symptomatic visceral leishmaniasis in AIDS patients concomitant with immune reconstitution due to antiretroviral therapy. Scand. J. Infect. Dis. 36:225-227. [DOI] [PubMed] [Google Scholar]
- 38.Bittencourt, A., N. Silva, A. Straatmann, V. L. Nunes, I. Follador, and R. Badaro. 2002. Post-kala-azar dermal leishmaniasis associated with AIDS. Braz. J. Infect. Dis. 6:313-316. [DOI] [PubMed] [Google Scholar]
- 39.Blanche, P., B. Gombert, O. Rivoal, S. Abad, D. Salmon, and A. Brezin. 2002. Uveitis due to Leishmania major as part of HAART-induced immune restitution syndrome in a patient with AIDS. Clin. Infect. Dis. 34:1279-1280. [DOI] [PubMed] [Google Scholar]
- 40.Boisseau-Garsaud, A. M., D. Cales-Quist, N. Desbois, J. Jouannelle, A. Jouannelle, F. Pratlong, and J. P. Dedet. 2000. A new case of cutaneous infection by a presumed monoxenous trypanosomatid in the island of Martinique (French West Indies). Trans. R. Soc. Trop. Med. Hyg. 94:51-52. [DOI] [PubMed] [Google Scholar]
- 41.Bora, D. 1999. Epidemiology of visceral leishmaniasis in India. Natl. Med. J. India 12:62-68. [PubMed] [Google Scholar]
- 42.Borges, A. S., A. A. Machado, M. S. Ferreira, J. F. de Castro Figueiredo, G. F. Silva, S. Cimerman, H. A. Bacha, and M. C. Teixeira. 1999. Concurrent leishmaniasis and human immunodeficiency virus (HIV) infection: a study of four cases. Rev. Soc. Bras. Med. Trop. 32:713-719. [PubMed] [Google Scholar]
- 43.Borrelli, P., A. Imperato, G. Murdaca, and M. Scudeletti. 2000. Liposomal amphotericin B as first line and secondary prophylactic treatment for visceral leishmaniasis in a patient infected with HIV. Ann. Ital. Med. Int. 15:169-171. [PubMed] [Google Scholar]
- 44.Bosch, R. J., A. B. Rodrigo, P. Sanchez, M. V. de Galvez, and E. Herrera. 2002. Presence of Leishmania organisms in specific and non-specific skin lesions in HIV-infected individuals with visceral leishmaniasis. Int. J. Dermatol. 41:670-675. [DOI] [PubMed] [Google Scholar]
- 45.Bossolasco, S., G. Gaiera, D. Olchini, M. Gulletta, L. Martello, A. Bestetti, L. Bossi, L. Germagnoli, A. Lazzarin, C. Uberti-Foppa, and P. Cinque. 2003. Real-time PCR assay for clinical management of human immunodeficiency virus-infected patients with visceral leishmaniasis. J. Clin. Microbiol. 41:5080-5084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bossolasco, S., S. Nozza, G. Gaiera, A. Bestetti, A. Lazzarin, and P. Cinque. 2007. Lack of immune recovery in HIV/Leishmania co-infection treated with human recombinant IL-2. AIDS 21:1223-1225. [DOI] [PubMed] [Google Scholar]
- 47.Boumis, E., P. Chinello, C. Della Rocca, M. G. Paglia, M. F. Proietti, and N. Petrosillo. 2006. Atypical disseminated leishmaniasis resembling post-kala-azar dermal leishmaniasis in an HIV-infected patient. Int. J. STD AIDS 17:351-353. [DOI] [PubMed] [Google Scholar]
- 47a.Brazilian Ministry of Health. 2004. Manual de recomendações para diagnóstico, tratamento e acompanhamento da co-infecção Leishmania-HIV. Brazilian Ministry of Health, Brasilia, Brazil.
- 48.Bryceson, A. 2001. A policy for leishmaniasis with respect to the prevention and control of drug resistance. Trop. Med. Int. Health 6:928-934. [DOI] [PubMed] [Google Scholar]
- 49.Cacopardo, B., L. Nigro, W. Preiser, A. Fama, M. I. Satariano, J. Braner, B. M. Celesia, B. Weber, R. Russo, and H. W. Doerr. 1996. Prolonged Th2 cell activation and increased viral replication in HIV-Leishmania co-infected patients despite treatment. Trans. R. Soc. Trop. Med. Hyg. 90:434-435. [DOI] [PubMed] [Google Scholar]
- 50.Calza, L., A. D'Antuono, G. Marinacci, R. Manfredi, V. Colangeli, B. Passarini, R. Orioli, O. Varoli, and F. Chiodo. 2004. Disseminated cutaneous leishmaniasis after visceral disease in a patient with AIDS. J. Am. Acad. Dermatol. 50:461-465. [DOI] [PubMed] [Google Scholar]
- 51.Cambi, A., F. de Lange, N. M. van Maarseveen, M. Nijhuis, B. Joosten, E. M. van Dijk, B. I. de Bakker, J. A. Fransen, P. H. Bovee-Geurts, F. N. van Leeuwen, N. F. Van Hulst, and C. G. Figdor. 2004. Microdomains of the C-type lectin DC-SIGN are portals for virus entry into dendritic cells. J. Cell Biol. 164:145-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Campanelli, A. P., A. M. Roselino, K. A. Cavassani, M. S. Pereira, R. A. Mortara, C. I. Brodskyn, H. S. Goncalves, Y. Belkaid, M. Barral-Netto, A. Barral, and J. S. Silva. 2006. CD4+CD25+ T cells in skin lesions of patients with cutaneous leishmaniasis exhibit phenotypic and functional characteristics of natural regulatory T cells. J. Infect. Dis. 193:1313-1322. [DOI] [PubMed] [Google Scholar]
- 53.Campino, L., S. Cortes, R. Pires, L. Oskam, and P. Abranches. 2000. Detection of Leishmania in immunocompromised patients using peripheral blood spots on filter paper and the polymerase chain reaction. Eur. J. Clin. Microbiol. Infect. Dis. 19:396-398. [DOI] [PubMed] [Google Scholar]
- 54.Campino, L., F. Pratlong, P. Abranches, J. A. Rioux, G. Santos-Gomes, C. Alves-Pires, S. Cortes, J. Ramada, J. M. Cristovao, M. O. Afonso, and J. P. Dedet. 2006. Leishmaniasis in Portugal: enzyme polymorphism of Leishmania infantum based on the identification of 213 strains. Trop. Med. Int. Health 11:1708-1714. [DOI] [PubMed] [Google Scholar]
- 55.Casado, J. L., R. Lopez-Velez, V. Pintado, C. Quereda, A. Antela, and S. Moreno. 2001. Relapsing visceral leishmaniasis in HIV-infected patients undergoing successful protease inhibitor therapy. Eur. J. Clin. Microbiol. Infect. Dis. 20:202-205. [DOI] [PubMed] [Google Scholar]
- 56.Catorze, G., J. Alberto, A. Afonso, R. Vieira, S. Cortes, and L. Campino. 2006. Leishmania infantum/HIV co-infection: cutaneous lesions following treatment of visceral leishmaniasis. Ann. Dermatol. Venereol. 133:39-42. [DOI] [PubMed] [Google Scholar]
- 57.Chappuis, F., S. Rijal, A. Soto, J. Menten, and M. Boelaert. 2006. A meta-analysis of the diagnostic performance of the direct agglutination test and rK39 dipstick for visceral leishmaniasis. BMJ 333:723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chicharro, C., and J. Alvar. 2003. Lower trypanosomatids in HIV/AIDS patients. Ann. Trop. Med. Parasitol. 97(Suppl. 1):75-78. [DOI] [PubMed] [Google Scholar]
- 59.Chicharro, C., M. I. Jimenez, and J. Alvar. 2003. Iso-enzymatic variability of Leishmania infantum in Spain. Ann. Trop. Med. Parasitol. 97(Suppl. 1):57-64. [DOI] [PubMed] [Google Scholar]
- 60.Chunge, C. N., J. Owate, H. O. Pamba, and L. Donno. 1990. Treatment of visceral leishmaniasis in Kenya by aminosidine alone or combined with sodium stibogluconate. Trans. R. Soc. Trop. Med. Hyg. 84:221-225. [DOI] [PubMed] [Google Scholar]
- 61.Clerici, M., and G. M. Shearer. 1993. A TH1→TH2 switch is a critical step in the etiology of HIV infection. Immunol. Today 14:107-111. [DOI] [PubMed] [Google Scholar]
- 62.Cnudde, F., C. Raccurt, F. Boulard, B. Terron-Aboud, M. Nicolas, and B. Juminer. 1994. Diffuse cutaneous leishmaniasis with visceral dissemination in an AIDS patient in Guadeloupe, West Indies. AIDS 8:559-560. [PubMed] [Google Scholar]
- 63.Cohen, J. 2007. HIV/AIDS. India slashes estimate of HIV-infected people. Science 317:179-181. [DOI] [PubMed] [Google Scholar]
- 64.Colebunders, R., K. Depraetere, T. Verstraeten, J. Lambert, E. Hauben, E. Van Marck, T. Maurer, A. L. Banuls, and J. C. Dujardin. 1999. Unusual cutaneous lesions in two patients with visceral leishmaniasis and HIV infection. J. Am. Acad. Dermatol. 41:847-850. [DOI] [PubMed] [Google Scholar]
- 65.Colmenares, M., A. Puig-Kroger, O. M. Pello, A. L. Corbi, and L. Rivas. 2002. Dendritic cell (DC)-specific intercellular adhesion molecule 3 (ICAM-3)-grabbing nonintegrin (DC-SIGN, CD209), a C-type surface lectin in human DCs, is a receptor for Leishmania amastigotes. J. Biol. Chem. 277:36766-36769. [DOI] [PubMed] [Google Scholar]
- 66.Couppie, P., E. Clyti, M. Sobesky, F. Bissuel, P. Del Giudice, D. Sainte-Marie, J. P. Dedet, B. Carme, and R. Pradinaud. 2004. Comparative study of cutaneous leishmaniasis in human immunodeficiency virus (HIV)-infected patients and non-HIV-infected patients in French Guiana. Br. J. Dermatol. 151:1165-1171. [DOI] [PubMed] [Google Scholar]
- 67.Croft, S. L., S. Sundar, and A. H. Fairlamb. 2006. Drug resistance in leishmaniasis. Clin. Microbiol. Rev. 19:111-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cruz, I., C. Canavate, J. M. Rubio, M. A. Morales, C. Chicharro, F. Laguna, M. Jimenez-Mejias, G. Sirera, S. Videla, and J. Alvar. 2002. A nested polymerase chain reaction (Ln-PCR) for diagnosing and monitoring Leishmania infantum infection in patients co-infected with human immunodeficiency virus. Trans. R. Soc. Trop. Med. Hyg. 96(Suppl. 1):S185-S189. [DOI] [PubMed] [Google Scholar]
- 69.Cruz, I., C. Chicharro, J. Nieto, B. Bailo, C. Canavate, M. C. Figueras, and J. Alvar. 2006. Comparison of new diagnostic tools for management of pediatric Mediterranean visceral leishmaniasis. J. Clin. Microbiol. 44:2343-2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cruz, I., M. A. Morales, I. Noguer, A. Rodriguez, and J. Alvar. 2002. Leishmania in discarded syringes from intravenous drug users. Lancet 359:1124-1125. [DOI] [PubMed] [Google Scholar]
- 71.Cruz, I., J. Nieto, J. Moreno, C. Canavate, P. Desjeux, and J. Alvar. 2006. Leishmania/HIV co-infections in the second decade. Indian J. Med. Res. 123:357-388. [PubMed] [Google Scholar]
- 72.Davidson, R. N. 1998. Practical guide for the treatment of leishmaniasis. Drugs 56:1009-1018. [DOI] [PubMed] [Google Scholar]
- 73.Davidson, R. N., L. Di Martino, L. Gradoni, R. Giacchino, R. Russo, G. B. Gaeta, R. Pempinello, S. Scott, F. Raimondi, A. Cascio, et al. 1994. Liposomal amphotericin B (AmBisome) in Mediterranean visceral leishmaniasis: a multi-centre trial. Q. J. Med. 87:75-81. [PubMed] [Google Scholar]
- 74.Dedet, J. P., and F. Pratlong. 2000. Leishmania, Trypanosoma and monoxenous trypanosomatids as emerging opportunistic agents. J. Eukaryot. Microbiol. 47:37-39. [DOI] [PubMed] [Google Scholar]
- 75.Dedet, J. P., B. Roche, F. Pratlong, D. Cales-Quist, J. Jouannelle, J. C. Benichou, and M. Huerre. 1995. Diffuse cutaneous infection caused by a presumed monoxenous trypanosomatid in a patient infected with HIV. Trans. R. Soc. Trop. Med. Hyg. 89:644-646. [DOI] [PubMed] [Google Scholar]
- 76.de la Loma, A., J. Alvar, E. Martinez Galiano, J. Blazquez, A. Alcala Munoz, and R. Najera. 1985. Leishmaniasis or AIDS? Trans. R. Soc. Trop. Med. Hyg. 79:421-422. [DOI] [PubMed] [Google Scholar]
- 77.de La Rosa, R., J. A. Pineda, J. Delgado, J. Macias, F. Morillas, J. A. Mira, A. Sanchez-Quijano, M. Leal, and E. Lissen. 2002. Incidence of and risk factors for symptomatic visceral leishmaniasis among human immunodeficiency virus type 1-infected patients from Spain in the era of highly active antiretroviral therapy. J. Clin. Microbiol. 40:762-767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Delgado, J., J. Macias, J. A. Pineda, J. E. Corzo, M. P. Gonzalez-Moreno, R. de la Rosa, A. Sanchez-Quijano, M. Leal, and E. Lissen. 1999. High frequency of serious side effects from meglumine antimoniate given without an upper limit dose for the treatment of visceral leishmaniasis in human immunodeficiency virus type-1-infected patients. Am. J. Trop. Med. Hyg. 61:766-769. [DOI] [PubMed] [Google Scholar]
- 79.del Giudice, P., M. Mary-Krause, C. Pradier, S. Grabar, P. Dellamonica, P. Marty, J. A. Gastaut, D. Costagliola, and E. Rosenthal. 2002. Impact of highly active antiretroviral therapy on the incidence of visceral leishmaniasis in a French cohort of patients infected with human immunodeficiency virus. J. Infect. Dis. 186:1366-1370. [DOI] [PubMed] [Google Scholar]
- 80.Deniau, M., C. Canavate, F. Faraut-Gambarelli, and P. Marty. 2003. The biological diagnosis of leishmaniasis in HIV-infected patients. Ann. Trop. Med. Parasitol. 97(Suppl. 1):115-133. [DOI] [PubMed] [Google Scholar]
- 81.Dereure, J., S. H. El-Safi, B. Bucheton, M. Boni, M. M. Kheir, B. Davoust, F. Pratlong, E. Feugier, M. Lambert, A. Dessein, and J. P. Dedet. 2003. Visceral leishmaniasis in eastern Sudan: parasite identification in humans and dogs; host-parasite relationships. Microbes Infect. 5:1103-1108. [DOI] [PubMed] [Google Scholar]
- 82.Dereure, J., J. Reynes, F. Pratlong, I. Lamaury, J. A. Rioux, F. Janbon, and J. P. Dedet. 1995. Visceral leishmaniasis in HIV-infected patients in the south of France. Bull. W. H. O. 73:245-246. [PMC free article] [PubMed] [Google Scholar]
- 83.Desjeux, P., and J. Alvar. 2003. Leishmania/HIV co-infections: epidemiology in Europe. Ann. Trop. Med. Parasitol. 97(Suppl. 1):3-15. [DOI] [PubMed] [Google Scholar]
- 84.de Souza e Souza, I., R. D. Naiff, T. C. Guimaraes, M. F. Naiff, E. Cupolillo, W. A. Rodrigues, and A. P. Schettini. 1998. American cutaneous leishmaniasis due to Leishmania (Viannia) guyanensis as an initial clinical presentation of human immunodeficiency virus infection. J. Eur. Acad. Dermatol. Venereol. 10:214-217. [DOI] [PubMed] [Google Scholar]
- 85.d'Ettorre, G., G. Ceccarelli, M. Carnevalini, G. Forcina, L. Zaffiri, A. P. Massetti, C. M. Mastroianni, and V. Vullo. 2006. Central role of interleukin-15 in human immunodeficiency virus (HIV)-infected patients with visceral leishmaniasis. Acta Trop. 99:83-87. [DOI] [PubMed] [Google Scholar]
- 86.Diaz, N. L., O. Zerpa, L. V. Ponce, J. Convit, A. J. Rondon, and F. J. Tapia. 2002. Intermediate or chronic cutaneous leishmaniasis: leukocyte immunophenotypes and cytokine characterisation of the lesion. Exp. Dermatol. 11:34-41. [DOI] [PubMed] [Google Scholar]
- 87.Di Giorgio, C., F. Faraut-Gambarelli, A. Imbert, P. Minodier, M. Gasquet, and H. Dumon. 1999. Flow cytometric assessment of amphotericin B susceptibility in Leishmania infantum isolates from patients with visceral leishmaniasis. J. Antimicrob. Chemother. 44:71-76. [DOI] [PubMed] [Google Scholar]
- 88.Donaghy, L., F. Gros, L. Amiot, C. Mary, A. Maillard, C. Guiguen, and J. P. Gangneux. 2007. Elevated levels of soluble non-classical major histocompatibility class I molecule human leucocyte antigen (HLA)-G in the blood of HIV-infected patients with or without visceral leishmaniasis. Clin. Exp. Immunol. 147:236-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Durand, I., M. Beylot-Barry, F. X. Weill, M. S. Doutre, and C. Beylot. 1998. Disseminated cutaneous leishmaniasis revealing human immunodeficiency virus infection. Ann. Dermatol. Venereol. 125:268-270. [PubMed] [Google Scholar]
- 90.Elamin, E. M., S. Guerbouj, A. M. Musa, I. Guizani, E. A. Khalil, M. M. Mukhtar, A. M. Elkadaro, H. S. Mohamed, M. E. Ibrahim, M. M. Abdel Hamid, M. El Azhari, and A. M. El Hassan. 2005. Uncommon clinical presentations of cutaneous leishmaniasis in Sudan. Trans. R. Soc. Trop. Med. Hyg. 99:803-808. [DOI] [PubMed] [Google Scholar]
- 91.el-Hassan, A. M., F. A. Hashim, M. S. Ali, H. W. Ghalib, and E. E. Zijlstra. 1993. Kala-azar in western Upper Nile province in the southern Sudan and its spread to a nomadic tribe from the north. Trans. R. Soc. Trop. Med. Hyg. 87:395-398. [DOI] [PubMed] [Google Scholar]
- 92.Elkhoury, A., M. Sousa, F. Lucena, W. Alves, J. Sena, and L. Paz. 2007. Co-infecção leishmaniose visceral e AIDS no Brasil. Rev. Soc. Bras. Med. Trop. 40:124. [Google Scholar]
- 93.El-Safi, S. H., A. Abdel-Haleem, A. Hammad, I. El-Basha, A. Omer, H. G. Kareem, M. Boelaert, M. Chance, and M. Hommel. 2003. Field evaluation of latex agglutination test for detecting urinary antigens in visceral leishmaniasis in Sudan. East Mediterr. Health J. 9:844-855. [PubMed] [Google Scholar]
- 94.Escobar, P., V. Yardley, and S. L. Croft. 2001. Activities of hexadecylphosphocholine (miltefosine), AmBisome, and sodium stibogluconate (Pentostam) against Leishmania donovani in immunodeficient scid mice. Antimicrob. Agents Chemother. 45:1872-1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Faraut-Gambarelli, F., R. Piarroux, M. Deniau, B. Giusiano, P. Marty, G. Michel, B. Faugere, and H. Dumon. 1997. In vitro and in vivo resistance of Leishmania infantum to meglumine antimoniate: a study of 37 strains collected from patients with visceral leishmaniasis. Antimicrob. Agents Chemother. 41:827-830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fernandez Cotarelo, M. J., J. Abellan Martinez, J. M. Guerra Vales, P. Martinez Sanchez, M. Rodrigo Gomez De La Barcena, and E. Salto Fernandez. 2003. Effect of highly active antiretroviral therapy on the incidence and clinical manifestations of visceral leishmaniasis in human immunodeficiency virus-infected patients. Clin. Infect. Dis. 37:973-977. [DOI] [PubMed] [Google Scholar]
- 97.Fisa, R., C. Riera, E. Ribera, M. Gallego, and M. Portus. 2002. A nested polymerase chain reaction for diagnosis and follow-up of human visceral leishmaniasis patients using blood samples. Trans. R. Soc. Trop. Med. Hyg. 96(Suppl. 1):S191-S194. [DOI] [PubMed] [Google Scholar]
- 98.Fong, D., M. M. Chan, R. Rodriguez, L. J. Gately, J. D. Berman, and M. Grogl. 1994. Paromomycin resistance in Leishmania tropica: lack of correlation with mutation in the small subunit ribosomal RNA gene. Am. J. Trop. Med. Hyg. 51:758-766. [DOI] [PubMed] [Google Scholar]
- 99.Foulet, F., A. Cosnes, S. Dellion, L. Blum, C. Bachmeyer, G. Raguin, C. Tourte-Schaeffer, M. Deniau, and S. Bretagne. 2006. Leishmania major cutaneous leishmaniasis in HIV-positive patients does not spread to extralesional sites. Arch. Dermatol. 142:1368-1369. [DOI] [PubMed] [Google Scholar]
- 100.Gallego, M., F. Pratlong, C. Riera, C. Munoz, E. Ribera, R. Fisa, J. A. Rioux, J. P. Dedet, and M. Portus. 2002. Isoenzymatic identification of Leishmania isolates from repeated clinical human leishmaniasis episodes in Catalonia (Spain). Trans. R. Soc. Trop. Med. Hyg. 96:45-47. [DOI] [PubMed] [Google Scholar]
- 101.Garcia-Garcia, J. A., J. Martin-Sanchez, M. Gallego, A. Rivero-Roman, A. Camacho, C. Riera, F. Morillas-Marquez, S. Vergara, J. Macias, and J. A. Pineda. 2006. Use of noninvasive markers to detect Leishmania infection in asymptomatic human immunodeficiency virus-infected patients. J. Clin. Microbiol. 44:4455-4458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Garg, R., N. Trudel, and M. J. Tremblay. 2007. Consequences of the natural propensity of Leishmania and HIV-1 to target dendritic cells. Trends Parasitol. 23:317-324. [DOI] [PubMed] [Google Scholar]
- 103.Gilad, J., A. Borer, D. Hallel-Halevy, K. Riesenberg, M. Alkan, and F. Schlaeffer. 2001. Post-kala-azar dermal leishmaniasis manifesting after initiation of highly active anti-retroviral therapy in a patient with human immunodeficiency virus infection. Isr. Med. Assoc. J. 3:451-452. [PubMed] [Google Scholar]
- 104.Gillis, D., S. Klaus, L. F. Schnur, P. Piscopos, S. Maayan, E. Okon, and D. Engelhard. 1995. Diffusely disseminated cutaneous Leishmania major infection in a child with acquired immunodeficiency syndrome. Pediatr. Infect. Dis. J. 14:247-249. [DOI] [PubMed] [Google Scholar]
- 105.Gonzalez-Beato, M. J., B. Moyano, C. Sanchez, M. T. Gonzalez-Beato, J. A. Perez-Molina, P. Miralles, and P. Lazaro. 2000. Kaposi's sarcoma-like lesions and other nodules as cutaneous involvement in AIDS-related visceral leishmaniasis. Br. J. Dermatol. 143:1316-1318. [DOI] [PubMed] [Google Scholar]
- 106.Gradoni, L., R. N. Davidson, S. Orsini, P. Betto, and M. Giambenedetti. 1993. Activity of liposomal amphotericin B (AmBisome) against Leishmania infantum and tissue distribution in mice. J. Drug Target. 1:311-316. [DOI] [PubMed] [Google Scholar]
- 107.Gradoni, L., A. Scalone, M. Gramiccia, and M. Troiani. 1996. Epidemiological surveillance of leishmaniasis in HIV-1-infected individuals in Italy. AIDS 10:785-791. [DOI] [PubMed] [Google Scholar]
- 108.Gramiccia, M. 2003. The identification and variability of the parasites causing leishmaniasis in HIV-positive patients in Italy. Ann. Trop. Med. Parasitol. 97(Suppl. 1):65-73. [DOI] [PubMed] [Google Scholar]
- 109.Griffin, G. E., K. Leung, T. M. Folks, S. Kunkel, and G. J. Nabel. 1989. Activation of HIV gene expression during monocyte differentiation by induction of NF-kappa B. Nature 339:70-73. [DOI] [PubMed] [Google Scholar]
- 110.Guerin, P. J., P. Olliaro, S. Sundar, M. Boelaert, S. L. Croft, P. Desjeux, M. K. Wasunna, and A. D. Bryceson. 2002. Visceral leishmaniasis: current status of control, diagnosis, and treatment, and a proposed research and development agenda. Lancet Infect. Dis. 2:494-501. [DOI] [PubMed] [Google Scholar]
- 111.Guiguemde, R. T., O. S. Sawadogo, C. Bories, K. L. Traore, D. Nezien, L. Nikiema, F. Pratlong, P. Marty, R. Houin, and M. Deniau. 2003. Leishmania major and HIV co-infection in Burkina Faso. Trans. R. Soc. Trop. Med. Hyg. 97:168-169. [DOI] [PubMed] [Google Scholar]
- 112.Gurubacharya, R. L., S. M. Gurubacharya, D. L. Gurubacharya, J. Quinkel, and V. L. Gurubacharya. 2006. Prevalence of visceral leishmania and HIV co-infection in Nepal. Indian J. Med. Res. 123:473-475. [PubMed] [Google Scholar]
- 113.Haile, T., and S. D. Anderson. 2006. Visceral leishmaniasis in northern Ethiopia. East Afr. Med. J. 83:389-392. [DOI] [PubMed] [Google Scholar]
- 114.Hailu, A., and N. Berhe. 2002. The performance of direct agglutination tests (DAT) in the diagnosis of visceral leishmaniasis among Ethiopian patients with HIV co-infection. Ann. Trop. Med. Parasitol. 96:25-30. [DOI] [PubMed] [Google Scholar]
- 115.Hepburn, N. C. 2003. Cutaneous leishmaniasis: an overview. J. Postgrad. Med. 49:50-54. [DOI] [PubMed] [Google Scholar]
- 116.Herrera, E., P. Sanchez, and R. J. Bosch. 1995. Disseminated cutaneous leishmaniasis in an HIV-infected patient. Int. J. STD AIDS 6:125-126. [DOI] [PubMed] [Google Scholar]
- 117.Hotez, P. J., J. H. Remme, P. Buss, G. Alleyne, C. Morel, and J. G. Breman. 2004. Combating tropical infectious diseases: report of the Disease Control Priorities in Developing Countries Project. Clin. Infect. Dis. 38:871-878. [DOI] [PubMed] [Google Scholar]
- 118.Ismail, A., A. F. Gadir, T. G. Theander, A. Kharazmi, and A. M. El Hassan. 2006. Pathology of post-kala-azar dermal leishmaniasis: a light microscopical, immunohistochemical, and ultrastructural study of skin lesions and draining lymph nodes. J. Cutan. Pathol. 33:778-787. [DOI] [PubMed] [Google Scholar]
- 119.Jha, T. K., S. Sundar, C. P. Thakur, P. Bachmann, J. Karbwang, C. Fischer, A. Voss, and J. Berman. 1999. Miltefosine, an oral agent, for the treatment of Indian visceral leishmaniasis. N. Engl. J. Med. 341:1795-1800. [DOI] [PubMed] [Google Scholar]
- 120.Jimenez, M., M. Ferrer-Dufol, C. Canavate, B. Gutierrez-Solar, R. Molina, F. Laguna, R. Lopez-Velez, E. Cercenado, E. Dauden, J. Blazquez, et al. 1995. Variability of Leishmania (Leishmania) infantum among stocks from immunocompromised, immunocompetent patients and dogs in Spain. FEMS Microbiol. Lett. 131:197-204. [DOI] [PubMed] [Google Scholar]
- 121.Jimenez, M. I., R. Lopez-Velez, R. Molina, C. Canavate, and J. Alvar. 1996. HIV co-infection with a currently non-pathogenic flagellate. Lancet 347:264-265. [DOI] [PubMed] [Google Scholar]
- 122.Jimenez-Exposito, M. J., C. Alonso-Villaverde, P. Sarda, and L. Masana. 1999. Visceral leishmaniasis in HIV-infected patients with non-detectable HIV-1 viral load after highly active antiretroviral therapy. AIDS 13:152-153. [PubMed] [Google Scholar]
- 123.Joshi, D. D., M. Sharma, and S. Bhandari. 2006. Visceral leishmaniasis in Nepal during 1980-2006. J. Commun. Dis. 38:139-148. [PubMed] [Google Scholar]
- 124.Kager, P. A., and P. H. Rees. 1983. Splenic aspiration. Review of the literature. Trop. Geogr. Med. 35:111-124. [PubMed] [Google Scholar]
- 125.Kanyok, T. P., M. V. Reddy, J. Chinnaswamy, L. H. Danziger, and P. R. Gangadharam. 1994. In vivo activity of paromomycin against susceptible and multidrug-resistant Mycobacterium tuberculosis and M. avium complex strains. Antimicrob. Agents Chemother. 38:170-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kedzierska, K., and S. M. Crowe. 2002. The role of monocytes and macrophages in the pathogenesis of HIV-1 infection. Curr. Med. Chem. 9:1893-1903. [DOI] [PubMed] [Google Scholar]
- 127.Kemp, K. 2000. Cytokine-producing T cell subsets in human leishmaniasis. Arch. Immunol. Ther. Exp. (Warsaw) 48:173-176. [PubMed] [Google Scholar]
- 128.Kerob, D., J. D. Bouaziz, C. Sarfati, J. Pavie, M. D. Vignon-Pennamen, J. Menotti, S. Hamane, F. Pralong, P. Buffet, P. Morel, and C. Lebbe. 2006. First case of cutaneous reconstitution inflammatory syndrome associated with HIV infection and leishmaniasis. Clin. Infect. Dis. 43:664-666. [DOI] [PubMed] [Google Scholar]
- 129.Khatami, A., A. Firooz, F. Gorouhi, and Y. Dowlati. 2007. Treatment of acute Old World cutaneous leishmaniasis: a systematic review of the randomized controlled trials. J. Am. Acad. Dermatol. 57:335.e1-335.e29. [DOI] [PubMed] [Google Scholar]
- 130.Kubba, R., Y. al-Gindan, A. M. el-Hassan, A. H. Omer, M. K. Kutty, and M. B. Saeed. 1988. Dissemination in cutaneous leishmaniasis. II. Satellite papules and subcutaneous induration. Int. J. Dermatol. 27:702-706. [DOI] [PubMed] [Google Scholar]
- 131.Lachaud, L., J. Dereure, E. Chabbert, J. Reynes, J. M. Mauboussin, E. Oziol, J. P. Dedet, and P. Bastien. 2000. Optimized PCR using patient blood samples for diagnosis and follow-up of visceral leishmaniasis, with special reference to AIDS patients. J. Clin. Microbiol. 38:236-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Laguna, F. 2003. Treatment of leishmaniasis in HIV-positive patients. Ann. Trop. Med. Parasitol. 97(Suppl. 1):135-142. [DOI] [PubMed] [Google Scholar]
- 133.Laguna, F., M. Adrados, J. Alvar, V. Soriano, M. E. Valencia, V. Moreno, R. Polo, J. Verdejo, M. I. Jimenez, P. Martinez, M. L. Martinez, and J. M. Gonzalez-Lahoz. 1997. Visceral leishmaniasis in patients infected with the human immunodeficiency virus. Eur. J. Clin. Microbiol. Infect. Dis. 16:898-903. [DOI] [PubMed] [Google Scholar]
- 134.Laguna, F., R. Lopez-Velez, F. Pulido, A. Salas, J. Torre-Cisneros, E. Torres, F. J. Medrano, J. Sanz, G. Pico, J. Gomez-Rodrigo, J. Pasquau, and J. Alvar. 1999. Treatment of visceral leishmaniasis in HIV-infected patients: a randomized trial comparing meglumine antimoniate with amphotericin B. AIDS 13:1063-1069. [DOI] [PubMed] [Google Scholar]
- 135.Laguna, F., S. Videla, M. E. Jimenez-Mejias, G. Sirera, J. Torre-Cisneros, E. Ribera, D. Prados, B. Clotet, M. Sust, R. Lopez-Velez, and J. Alvar. 2003. Amphotericin B lipid complex versus meglumine antimoniate in the treatment of visceral leishmaniasis in patients infected with HIV: a randomized pilot study. J. Antimicrob. Chemother. 52:464-468. [DOI] [PubMed] [Google Scholar]
- 136.Laguna-del-Estal, P., and M. S. Moya-Mir. 1997. Prophylaxis of visceral leishmaniasis in human immunodeficiency virus-infected patients. Am. J. Med. 102:222. [DOI] [PubMed] [Google Scholar]
- 137.Lartey, M., L. Adusei, L. Hanson-Nortey, and J. Addy. 2006. Coinfection of cutaneous leishmaniasis and HIV infection. Ghana Med. J. 40:110-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Lopez-Velez, R. 2003. The impact of highly active antiretroviral therapy (HAART) on visceral leishmaniasis in Spanish patients who are co-infected with HIV. Ann. Trop. Med. Parasitol. 97(Suppl. 1):143-147. [DOI] [PubMed] [Google Scholar]
- 139.Lopez-Velez, R., J. L. Casado, and V. Pintado. 2001. Decline of a visceral leishmaniasis epidemic in HIV-infected patients after the introduction of highly active antiretroviral therapy (HAART). Clin. Microbiol. Infect. 7:394-395. [DOI] [PubMed] [Google Scholar]
- 140.Lopez-Velez, R., F. Laguna, J. Alvar, J. A. Perez-Molina, R. Molina, P. Martinez, and J. Villarrubia. 1995. Parasitic culture of buffy coat for diagnosis of visceral leishmaniasis in human immunodeficiency virus-infected patients. J. Clin. Microbiol. 33:937-939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Lopez-Velez, R., J. A. Perez-Molina, A. Guerrero, F. Baquero, J. Villarrubia, L. Escribano, C. Bellas, F. Perez-Corral, and J. Alvar. 1998. Clinicoepidemiologic characteristics, prognostic factors, and survival analysis of patients coinfected with human immunodeficiency virus and Leishmania in an area of Madrid, Spain. Am. J. Trop. Med. Hyg. 58:436-443. [DOI] [PubMed] [Google Scholar]
- 142.Lopez-Velez, R., S. Videla, M. Marquez, V. Boix, M. E. Jimenez-Mejias, M. Gorgolas, J. R. Arribas, A. Salas, F. Laguna, M. Sust, C. Canavate, and J. Alvar. 2004. Amphotericin B lipid complex versus no treatment in the secondary prophylaxis of visceral leishmaniasis in HIV-infected patients. J. Antimicrob. Chemother. 53:540-543. [DOI] [PubMed] [Google Scholar]
- 143.Lyons, S., H. Veeken, and J. Long. 2003. Visceral leishmaniasis and HIV in Tigray, Ethiopia. Trop. Med. Int. Health 8:733-739. [DOI] [PubMed] [Google Scholar]
- 144.Maarouf, M., M. T. Adeline, M. Solignac, D. Vautrin, and M. Robert-Gero. 1998. Development and characterization of paromomycin-resistant Leishmania donovani promastigotes. Parasite 5:167-173. [DOI] [PubMed] [Google Scholar]
- 145.Mahajan, V. K., and N. L. Sharma. 2007. Therapeutic options for cutaneous leishmaniasis. J. Dermatol. Treat. 18:97-104. [DOI] [PubMed] [Google Scholar]
- 146.Martinez, P., E. de la Vega, F. Laguna, V. Soriano, S. Puente, V. Moreno, M. J. Sentchordi, C. Garcia-Aguado, and J. Gonzalez-Lahoz. 1993. Diagnosis of visceral leishmaniasis in HIV-infected individuals using peripheral blood smears. AIDS 7:227-230. [DOI] [PubMed] [Google Scholar]
- 147.Mary, C., F. Faraut, M. P. Drogoul, B. Xeridat, N. Schleinitz, B. Cuisenier, and H. Dumon. 2006. Reference values for Leishmania infantum parasitemia in different clinical presentations: quantitative polymerase chain reaction for therapeutic monitoring and patient follow-up. Am. J. Trop. Med. Hyg. 75:858-863. [PubMed] [Google Scholar]
- 148.Mastroianni, C. M., G. d'Ettorre, G. Forcina, A. Corpolongo, S. Dell'Isola, M. Lichtner, C. D'Agostino, V. Trinchieri, P. Santopadre, and V. Vullo. 2000. Long-term remission of human immunodeficiency virus-associated visceral leishmaniasis after initiation of potent combination antiretroviral treatment: report of two cases. J. Infect. 40:94-96. [DOI] [PubMed] [Google Scholar]
- 149.Mathis, A., and P. Deplazes. 1995. PCR and in vitro cultivation for detection of Leishmania spp. in diagnostic samples from humans and dogs. J. Clin. Microbiol. 33:1145-1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Mathur, P., J. C. Samantaray, M. Vajpayee, and P. Samanta. 2006. Visceral leishmaniasis/human immunodeficiency virus co-infection in India: the focus of two epidemics. J. Med. Microbiol. 55:919-922. [DOI] [PubMed] [Google Scholar]
- 151.Mattos, M., A. Caiza, O. Fernandes, A. J. Goncalves, C. Pirmez, C. S. Souza, and M. P. Oliveira-Neto. 1998. American cutaneous leishmaniasis associated with HIV infection: report of four cases. J. Eur. Acad. Dermatol. Venereol. 10:218-225. [PubMed] [Google Scholar]
- 152.Medrano, F. J., C. Canavate, M. Leal, C. Rey, E. Lissen, and J. Alvar. 1998. The role of serology in the diagnosis and prognosis of visceral leishmaniasis in patients coinfected with human immunodeficiency virus type-1. Am. J. Trop. Med. Hyg. 59:155-162. [DOI] [PubMed] [Google Scholar]
- 153.Medrano, F. J., E. Jimenez-Mejias, E. Calderon, C. Regordan, and M. Leal. 1993. An easy and quick method for the diagnosis of visceral leishmaniasis in HIV-1-infected individuals. AIDS 7:1399. [DOI] [PubMed] [Google Scholar]
- 154.Melaku, Y., S. M. Collin, K. Keus, F. Gatluak, K. Ritmeijer, and R. N. Davidson. 2007. Treatment of kala-azar in southern Sudan using a 17-day regimen of sodium stibogluconate combined with paromomycin: a retrospective comparison with 30-day sodium stibogluconate monotherapy. Am. J. Trop. Med. Hyg. 77:89-94. [PubMed] [Google Scholar]
- 155.Reference deleted.
- 156.Mira, J. A., J. E. Corzo, A. Rivero, J. Macias, F. L. De Leon, J. Torre-Cisneros, J. Gomez-Mateos, R. Jurado, and J. A. Pineda. 2004. Frequency of visceral leishmaniasis relapses in human immunodeficiency virus-infected patients receiving highly active antiretroviral therapy. Am. J. Trop. Med. Hyg. 70:298-301. [PubMed] [Google Scholar]
- 157.Miralles, E. S., M. Nunez, Y. Hilara, A. Harto, R. Moreno, and A. Ledo. 1994. Mucocutaneous leishmaniasis and HIV. Dermatology 189:275-277. [DOI] [PubMed] [Google Scholar]
- 158.Molina, R., J. M. Lohse, F. Pulido, F. Laguna, R. Lopez-Velez, and J. Alvar. 1999. Infection of sand flies by humans coinfected with Leishmania infantum and human immunodeficiency virus. Am. J. Trop. Med. Hyg. 60:51-53. [DOI] [PubMed] [Google Scholar]
- 159.Mondain-Miton, V., M. Toussaint-Gari, P. Hofman, P. Marty, M. Carles, F. De Salvador, F. Miton, Y. Le Fichoux, and P. Dellamonica. 1995. Atypical leishmaniasis in a patient infected with human immunodeficiency virus. Clin. Infect. Dis. 21:663-665. [DOI] [PubMed] [Google Scholar]
- 160.Montalban, C., J. L. Calleja, A. Erice, F. Laguna, B. Clotet, D. Podzamczer, J. Cobo, J. Mallolas, M. Yebra, and A. Gallego. 1990. Visceral leishmaniasis in patients infected with human immunodeficiency virus. J. Infect. 21:261-270. [DOI] [PubMed] [Google Scholar]
- 161.Montana, M., N. Chochoi, P. Monges, I. Ravaux, F. Faraut, S. Gensollen, M. C. Bongrand, P. Timon-David, and H. Gallais. 2004. Liposomal amphotericin B in secondary prophylaxis of visceral leishmaniasis in HIV-infected patients: report of five clinical cases. Pathol. Biol. (Paris) 52:66-75. [DOI] [PubMed] [Google Scholar]
- 162.Morales, M. A., I. Cruz, J. M. Rubio, C. Chicharro, C. Canavate, F. Laguna, and J. Alvar. 2002. Relapses versus reinfections in patients coinfected with Leishmania infantum and human immunodeficiency virus type 1. J. Infect. Dis. 185:1533-1537. [DOI] [PubMed] [Google Scholar]
- 163.Moreno, J., C. Canavate, C. Chamizo, F. Laguna, and J. Alvar. 2000. HIV-Leishmania infantum co-infection: humoral and cellular immune responses to the parasite after chemotherapy. Trans. R. Soc. Trop. Med. Hyg. 94:328-332. [DOI] [PubMed] [Google Scholar]
- 164.Mudur, G. 2007. India reduces estimated count of people with HIV. BMJ 335:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Mueller, M., K. Ritmeijer, M. Balasegaram, Y. Koummuki, M. R. Santana, and R. Davidson. 2007. Unresponsiveness to AmBisome in some Sudanese patients with kala-azar. Trans. R. Soc. Trop. Med. Hyg. 101:19-24. [DOI] [PubMed] [Google Scholar]
- 166.Murray, H. W. 1999. Kala-azar as an AIDS-related opportunistic infection. AIDS Patient Care STDs 13:459-465. [DOI] [PubMed] [Google Scholar]
- 167.Murray, H. W. 2000. Suppression of posttreatment recurrence of experimental visceral leishmaniasis in T-cell-deficient mice by oral miltefosine. Antimicrob. Agents Chemother. 44:3235-3236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Murray, H. W., J. D. Berman, C. R. Davies, and N. G. Saravia. 2005. Advances in leishmaniasis. Lancet 366:1561-1577. [DOI] [PubMed] [Google Scholar]
- 169.Murray, H. W., J. Hariprashad, and R. E. Fichtl. 1993. Treatment of experimental visceral leishmaniasis in a T-cell-deficient host: response to amphotericin B and pentamidine. Antimicrob. Agents Chemother. 37:1504-1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Ndiaye, P. B., M. Develoux, M. T. Dieng, and M. Huerre. 1996. Diffuse cutaneous leishmaniasis and acquired immunodeficiency syndrome in a Senegalese patient. Bull. Soc. Pathol. Exot. 89:282-286. [PubMed] [Google Scholar]
- 171.Niamba, P., O. Goumbri-Lompo, A. Traore, F. Barro-Traore, and R. T. Soudre. 2007. Diffuse cutaneous leishmaniasis in an HIV-positive patient in western Africa. Australas. J. Dermatol. 48:32-34. [DOI] [PubMed] [Google Scholar]
- 172.Niamba, P., A. Traore, O. Goumbri-Lompo, C. Labreze, F. Traore-Barro, M. Bonkoungou, L. Ilboudo, A. Gaulier, and B. R. Soudre. 2006. Cutaneous leishmania in HIV patient in Ouagadougou: clinical and therapeutic aspects. Ann. Dermatol. Venereol. 133:537-542. [DOI] [PubMed] [Google Scholar]
- 173.Niamba, P. A., A. Traoré, O. Goumbri-Lompo, B. F. Traoré, M. Bonkoungou, L. Ilboudo, A. Gaulier, and C. Boileau. 2005. Cutaneous leishmania and HIV co-infection: clinical and evolutionary aspects, abstr. TuPe1.4C17. Third Int. AIDS Conf. HIV Pathog. Treat., Rio de Janiero, Brazil, 24 to 27 July 2005.
- 174.Nigro, L., B. Cacopardo, W. Preiser, J. Braner, J. Cinatl, F. Palermo, R. Russo, H. W. Doerr, and A. Nunnari. 1999. In vitro production of type 1 and type 2 cytokines by peripheral blood mononuclear cells from subjects coinfected with human immunodeficiency virus and Leishmania infantum. Am. J. Trop. Med. Hyg. 60:142-145. [DOI] [PubMed] [Google Scholar]
- 175.Nigro, L., A. Montineri, R. La Rosa, M. Zuccarello, C. Iacobello, C. Iacobello, C. Vinci, R. Pulizia, and F. Fatuzzo. 2003. Visceral leishmaniasis and HIV co-infection: a rare case of pulmonary and oral localization. Infez. Med. 11:93-96. [PubMed] [Google Scholar]
- 176.Nigro, L., M. L. Rizzo, C. Vancheri, R. La Rosa, C. Mastruzzo, V. Tomaselli, A. Ragusa, R. Manuele, and B. Cacopardo. 2007. CCR5 and CCR3 expression on T CD3+ lymphocytes from HIV/Leishmania co-infected subjects. Med. Microbiol. Immunol. 196:253-255. [DOI] [PubMed] [Google Scholar]
- 177.Olivier, M., R. Badaro, F. J. Medrano, and J. Moreno. 2003. The pathogenesis of Leishmania/HIV co-infection: cellular and immunological mechanisms. Ann. Trop. Med. Parasitol. 97(Suppl. 1):79-98. [DOI] [PubMed] [Google Scholar]
- 178.Olliaro, P. L., P. J. Guerin, S. Gerstl, A. A. Haaskjold, J. A. Rottingen, and S. Sundar. 2005. Treatment options for visceral leishmaniasis: a systematic review of clinical studies done in India, 1980-2004. Lancet Infect. Dis. 5:763-774. [DOI] [PubMed] [Google Scholar]
- 179.Oskam, L., J. L. Nieuwenhuijs, and A. Hailu. 1999. Evaluation of the direct agglutination test (DAT) using freeze-dried antigen for the detection of anti-Leishmania antibodies in stored sera from various patient groups in Ethiopia. Trans. R. Soc. Trop. Med. Hyg. 93:275-277. [DOI] [PubMed] [Google Scholar]
- 180.Pacheco, R. S., M. C. Marzochi, M. Q. Pires, C. M. Brito, F. Madeira Mde, and E. G. Barbosa-Santos. 1998. Parasite genotypically related to a monoxenous trypanosomatid of dog's flea causing opportunistic infection in an HIV positive patient. Mem. Inst. Oswaldo Cruz 93:531-537. [DOI] [PubMed] [Google Scholar]
- 181.Paredes, R., J. Munoz, I. Diaz, P. Domingo, M. Gurgui, and B. Clotet. 2003. Leishmaniasis in HIV infection. J. Postgrad. Med. 49:39-49. [DOI] [PubMed] [Google Scholar]
- 182.Pasquau, F., J. Ena, R. Sanchez, J. M. Cuadrado, C. Amador, J. Flores, C. Benito, C. Redondo, J. Lacruz, V. Abril, and J. Onofre. 2005. Leishmaniasis as an opportunistic infection in HIV-infected patients: determinants of relapse and mortality in a collaborative study of 228 episodes in a Mediterreanean region. Eur. J. Clin. Microbiol. Infect. Dis. 24:411-418. [DOI] [PubMed] [Google Scholar]
- 183.Perez-Molina, J. A., R. Lopez-Velez, P. Montilla, and A. Guerrero. 1996. Pentamidine isethionate as secondary prophylaxis against visceral leishmaniasis in HIV-positive patients. AIDS 10:237-238. [DOI] [PubMed] [Google Scholar]
- 184.Perez-Victoria, F. J., M. P. Sanchez-Canete, K. Seifert, S. L. Croft, S. Sundar, S. Castanys, and F. Gamarro. 2006. Mechanisms of experimental resistance of Leishmania to miltefosine: implications for clinical use. Drug Resist. Updat. 9:26-39. [DOI] [PubMed] [Google Scholar]
- 185.Piarroux, R., F. Gambarelli, H. Dumon, M. Fontes, S. Dunan, C. Mary, B. Toga, and M. Quilici. 1994. Comparison of PCR with direct examination of bone marrow aspiration, myeloculture, and serology for diagnosis of visceral leishmaniasis in immunocompromised patients. J. Clin. Microbiol. 32:746-749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Pineda, J. A., J. Macias, F. Morillas, J. Fernandez-Ochoa, J. Cara, R. de La Rosa, J. A. Mira, J. Martin-Sanchez, M. Gonzalez, J. Delgado, C. Acedo, and E. Lissen. 2001. Evidence of increased risk for Leishmania infantum infection among HIV-seronegative intravenous drug users from southern Spain. Eur. J. Clin. Microbiol. Infect. Dis. 20:354-357. [DOI] [PubMed] [Google Scholar]
- 187.Pineda, J. A., J. Martin-Sanchez, J. Macias, and F. Morillas. 2002. Leishmania spp. infection in injecting drug users. Lancet 360:950-951. [DOI] [PubMed] [Google Scholar]
- 188.Pintado, V., and R. Lopez-Velez. 2001. HIV-associated visceral leishmaniasis. Clin. Microbiol. Infect. 7:291-300. [DOI] [PubMed] [Google Scholar]
- 189.Pintado, V., P. Martin-Rabadan, M. L. Rivera, S. Moreno, and E. Bouza. 2001. Visceral leishmaniasis in human immunodeficiency virus (HIV)-infected and non-HIV-infected patients. A comparative study. Medicine (Baltimore) 80:54-73. [DOI] [PubMed] [Google Scholar]
- 190.Pizzuto, M., M. Piazza, D. Senese, C. Scalamogna, S. Calattini, L. Corsico, T. Persico, B. Adriani, C. Magni, G. Guaraldi, G. Gaiera, A. Ludovisi, M. Gramiccia, M. Galli, M. Moroni, M. Corbellino, and S. Antinori. 2001. Role of PCR in diagnosis and prognosis of visceral leishmaniasis in patients coinfected with human immunodeficiency virus type 1. J. Clin. Microbiol. 39:357-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Ponce, C., E. Ponce, A. Morrison, A. Cruz, R. Kreutzer, D. McMahon-Pratt, and F. Neva. 1991. Leishmania donovani chagasi: new clinical variant of cutaneous leishmaniasis in Honduras. Lancet 337:67-70. [DOI] [PubMed] [Google Scholar]
- 192.Posada-Vergara, M. P., J. A. Lindoso, J. E. Tolezano, V. L. Pereira-Chioccola, M. V. Silva, and H. Goto. 2005. Tegumentary leishmaniasis as a manifestation of immune reconstitution inflammatory syndrome in 2 patients with AIDS. J. Infect. Dis. 192:1819-1822. [DOI] [PubMed] [Google Scholar]
- 193.Pozio, E., and M. A. Morales. 2005. The impact of HIV-protease inhibitors on opportunistic parasites. Trends Parasitol. 21:58-63. [DOI] [PubMed] [Google Scholar]
- 194.Pratlong, F., T. Debord, E. Garnotel, E. Garrabe, P. Marty, G. Raphenon, and J. P. Dedet. 2005. First identification of the causative agent of visceral leishmaniasis in Djibouti: Leishmania donovani. Ann. Trop. Med. Parasitol. 99:21-25. [DOI] [PubMed] [Google Scholar]
- 195.Pratlong, F., J. Dereure, M. Deniau, P. Marty, F. Faraut-Gambarelli, and J. P. Dedet. 2003. Enzymatic polymorphism during Leishmania/HIV co-infection: a study of 381 Leishmania strains received between 1986 and 2000 at the international cryobank in Montpellier, France. Ann. Trop. Med. Parasitol. 97(Suppl. 1):47-56. [DOI] [PubMed] [Google Scholar]
- 196.Preiser, W., B. Cacopardo, L. Nigro, J. Braner, A. Nunnari, H. W. Doerr, and B. Weber. 1996. Immunological findings in HIV-Leishmania coinfection. Intervirology 39:285-288. [DOI] [PubMed] [Google Scholar]
- 197.Puig, L., and R. Pradinaud. 2003. Leishmania and HIV co-infection: dermatological manifestations. Ann. Trop. Med. Parasitol. 97(Suppl. 1):107-114. [DOI] [PubMed] [Google Scholar]
- 198.Qadoumi, M., I. Becker, N. Donhauser, M. Rollinghoff, and C. Bogdan. 2002. Expression of inducible nitric oxide synthase in skin lesions of patients with American cutaneous leishmaniasis. Infect. Immun. 70:4638-4642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Rabello, A., M. Orsini, and J. Disch. 2003. Leishmania/HIV co-infection in Brazil: an appraisal. Ann. Trop. Med. Parasitol. 97(Suppl. 1):17-28. [DOI] [PubMed] [Google Scholar]
- 200.Ramos-Santos, C., O. Hernandez-Montes, G. Sanchez-Tejeda, and A. Monroy-Ostria. 2000. Visceral leishmaniasis caused by Leishmania (L.) mexicana in a Mexican patient with human immunodeficiency virus infection. Mem. Inst. Oswaldo Cruz 95:733-737. [DOI] [PubMed] [Google Scholar]
- 201.Ranjan, A., D. Sur, V. P. Singh, N. A. Siddique, B. Manna, C. S. Lal, P. K. Sinha, K. Kishore, and S. K. Bhattacharya. 2005. Risk factors for Indian kala-azar. Am. J. Trop. Med. Hyg. 73:74-78. [PubMed] [Google Scholar]
- 202.Ravel, C., S. Cortes, F. Pratlong, F. Morio, J. P. Dedet, and L. Campino. 2006. First report of genetic hybrids between two very divergent Leishmania species: Leishmania infantum and Leishmania major. Int. J. Parasitol. 36:1383-1388. [DOI] [PubMed] [Google Scholar]
- 203.Redhu, N. S., A. Dey, V. Balooni, and S. Singh. 2006. Leishmania-HIV co-infection: an emerging problem in India. AIDS 20:1213-1215. [DOI] [PubMed] [Google Scholar]
- 204.Reithinger, R., J. C. Dujardin, H. Louzir, C. Pirmez, B. Alexander, and S. Brooker. 2007. Cutaneous leishmaniasis. Lancet Infect. Dis. 7:581-596. [DOI] [PubMed] [Google Scholar]
- 205.Reus, S., R. Sanchez, J. Portilla, V. Boix, M. Priego, E. Merino, and F. Roman. 1999. Visceral leishmaniasis: a comparative study of patients with and without human immunodeficiency virus infection. Enferm. Infecc. Microbiol. Clin. 17:515-520. [PubMed] [Google Scholar]
- 206.Reynes, J., P. Portales, M. Segondy, V. Baillat, P. Andre, O. Avinens, M. C. Picot, J. Clot, J. F. Eliaou, and P. Corbeau. 2001. CD4 T cell surface CCR5 density as a host factor in HIV-1 disease progression. AIDS 15:1627-1634. [DOI] [PubMed] [Google Scholar]
- 207.Ribera, E., I. Ocana, J. de Otero, E. Cortes, I. Gasser, and A. Pahissa. 1996. Prophylaxis of visceral leishmaniasis in human immunodeficiency virus-infected patients. Am. J. Med. 100:496-501. [DOI] [PubMed] [Google Scholar]
- 208.Ridolfo, A. L., C. Gervasoni, S. Antinori, M. Pizzuto, S. Santambrogio, D. Trabattoni, M. Clerici, and M. Galli. 2000. Post-kala-azar dermal leishmaniasis during highly active antiretroviral therapy in an AIDS patient infected with Leishmania infantum. J. Infect. 40:199-202. [DOI] [PubMed] [Google Scholar]
- 209.Riera, C., R. Fisa, P. Lopez, E. Ribera, J. Carrio, V. Falco, I. Molina, M. Gallego, and M. Portus. 2004. Evaluation of a latex agglutination test (KAtex) for detection of Leishmania antigen in urine of patients with HIV-Leishmania coinfection: value in diagnosis and post-treatment follow-up. Eur. J. Clin. Microbiol. Infect. Dis. 23:899-904. [DOI] [PubMed] [Google Scholar]
- 210.Riera, C., R. Fisa, E. Ribera, J. Carrio, V. Falco, M. Gallego, L. Moner, I. Molina, and M. Portus. 2005. Value of culture and nested polymerase chain reaction of blood in the prediction of relapses in patients co-infected with leishmania and human immunodeficiency virus. Am. J. Trop. Med. Hyg. 73:1012-1015. [PubMed] [Google Scholar]
- 211.Rihl, M., M. Stoll, K. Ulbricht, F. C. Bange, and R. E. Schmidt. 2006. Successful treatment of post-kala-azar dermal leishmaniasis (PKDL) in a HIV infected patient with multiple relapsing leishmaniasis from Western Europe. J. Infect. 53:e25-e27. [DOI] [PubMed] [Google Scholar]
- 212.Rijal, S., F. Chappuis, R. Singh, P. A. Bovier, P. Acharya, B. M. Karki, M. L. Das, P. Desjeux, L. Loutan, and S. Koirala. 2003. Treatment of visceral leishmaniasis in south-eastern Nepal: decreasing efficacy of sodium stibogluconate and need for a policy to limit further decline. Trans. R. Soc. Trop. Med. Hyg. 97:350-354. [DOI] [PubMed] [Google Scholar]
- 213.Rioux, J. A., G. Lanotte, E. Serres, F. Pratlong, P. Bastien, and J. Perieres. 1990. Taxonomy of Leishmania. Use of isoenzymes. Suggestions for a new classification. Ann. Parasitol. Hum. Comp. 65:111-125. [DOI] [PubMed] [Google Scholar]
- 214.Ritmeijer, K., and R. N. Davidson. 2003. Royal Society of Tropical Medicine and Hygiene joint meeting with Medecins Sans Frontieres at Manson House, London, 20 March 2003: field research in humanitarian medical programmes. Medecins Sans Frontieres interventions against kala-azar in the Sudan, 1989-2003. Trans. R. Soc. Trop. Med. Hyg. 97:609-613. [DOI] [PubMed] [Google Scholar]
- 215.Ritmeijer, K., A. Dejenie, Y. Assefa, T. B. Hundie, J. Mesure, G. Boots, M. den Boer, and R. N. Davidson. 2006. A comparison of miltefosine and sodium stibogluconate for treatment of visceral leishmaniasis in an Ethiopian population with high prevalence of HIV infection. Clin. Infect. Dis. 43:357-364. [DOI] [PubMed] [Google Scholar]
- 216.Ritmeijer, K., H. Veeken, Y. Melaku, G. Leal, R. Amsalu, J. Seaman, and R. N. Davidson. 2001. Ethiopian visceral leishmaniasis: generic and proprietary sodium stibogluconate are equivalent; HIV co-infected patients have a poor outcome. Trans. R. Soc. Trop. Med. Hyg. 95:668-672. [DOI] [PubMed] [Google Scholar]
- 217.Ritter, U., and H. Korner. 2002. Divergent expression of inflammatory dermal chemokines in cutaneous leishmaniasis. Parasite Immunol. 24:295-301. [DOI] [PubMed] [Google Scholar]
- 218.Rivas, L., J. Moreno, C. Canavate, and J. Alvar. 2004. Virulence and disease in leishmaniasis: what is relevant for the patient? Trends Parasitol. 20:297-301. [DOI] [PubMed] [Google Scholar]
- 219.Rosatelli, J. B., C. S. Souza, F. A. Soares, N. T. Foss, and A. M. Roselino. 1998. Generalized cutaneous leishmaniasis in acquired immunodeficiency syndrome. J. Eur. Acad. Dermatol. Venereol. 10:229-232. [PubMed] [Google Scholar]
- 220.Rosenthal, E., P. Marty, P. del Giudice, C. Pradier, C. Ceppi, J. A. Gastaut, Y. Le Fichoux, and J. P. Cassuto. 2000. HIV and Leishmania coinfection: a review of 91 cases with focus on atypical locations of Leishmania. Clin. Infect. Dis. 31:1093-1095. [DOI] [PubMed] [Google Scholar]
- 221.Rosenthal, E., P. Marty, I. Poizot-Martin, J. Reynes, F. Pratlong, A. Lafeuillade, D. Jaubert, O. Boulat, J. Dereure, F. Gambarelli, et al. 1995. Visceral leishmaniasis and HIV-1 co-infection in southern France. Trans. R. Soc. Trop. Med. Hyg. 89:159-162. [DOI] [PubMed] [Google Scholar]
- 222.Rosenthal, E., S. Tempesta, P. Del Giudice, P. Marty, P. Desjeux, C. Pradier, Y. Le Fichoux, and J. P. Cassuto. 2001. Declining incidence of visceral leishmaniasis in HIV-infected individuals in the era of highly active antiretroviral therapy. AIDS 15:1184-1185. [DOI] [PubMed] [Google Scholar]
- 223.Roustan, G., J. A. Jimenez, B. Gutierrez-Solar, J. L. Gallego, J. Alvar, and M. Patron. 1998. Post-kala-azar dermal leishmaniasis with mucosal involvement in a kidney transplant recipient: treatment with liposomal amphotericin B. Br. J. Dermatol. 138:526-528. [DOI] [PubMed] [Google Scholar]
- 224.Russo, R., F. Laguna, R. Lopez-Velez, F. J. Medrano, E. Rosenthal, B. Cacopardo, and L. Nigro. 2003. Visceral leishmaniasis in those infected with HIV: clinical aspects and other opportunistic infections. Ann. Trop. Med. Parasitol. 97(Suppl. 1):99-105. [DOI] [PubMed] [Google Scholar]
- 225.Russo, R., L. Nigro, G. Panarello, and A. Montineri. 2003. Clinical survey of Leishmania/HIV co-infection in Catania, Italy: the impact of highly active antiretroviral therapy (HAART). Ann. Trop. Med. Parasitol. 97(Suppl. 1):149-155. [DOI] [PubMed] [Google Scholar]
- 226.Russo, R., L. C. Nigro, S. Minniti, A. Montineri, L. Gradoni, L. Caldeira, and R. N. Davidson. 1996. Visceral leishmaniasis in HIV infected patients: treatment with high dose liposomal amphotericin B (AmBisome). J. Infect. 32:133-137. [DOI] [PubMed] [Google Scholar]
- 227.Sabbatani, S., A. Isuierdo Calzado, A. Ferro, A. M. Lopez Goudiaby, V. Borghi, G. P. Zanchetta, and O. E. Varnier. 1991. Atypical leishmaniasis in an HIV-2-seropositive patient from Guinea-Bissau. AIDS 5:899-901. [PubMed] [Google Scholar]
- 228.Salotra, P., and R. Singh. 2006. Challenges in the diagnosis of post kala-azar dermal leishmaniasis. Indian J. Med. Res. 123:295-310. [PubMed] [Google Scholar]
- 229.Savoia, D., T. Allice, and P. A. Tovo. 2005. Antileishmanial activity of HIV protease inhibitors. Int. J. Antimicrob. Agents 26:92-94. [DOI] [PubMed] [Google Scholar]
- 230.Schenkel, K., S. Rijal, S. Koirala, S. Koirala, V. Vanlerberghe, P. Van der Stuyft, M. Gramiccia, and M. Boelaert. 2006. Visceral leishmaniasis in southeastern Nepal: a cross-sectional survey on Leishmania donovani infection and its risk factors. Trop. Med. Int. Health 11:1792-1799. [DOI] [PubMed] [Google Scholar]
- 231.Schonian, G., H. Akuffo, S. Lewin, K. Maasho, S. Nylen, F. Pratlong, C. L. Eisenberger, L. F. Schnur, and W. Presber. 2000. Genetic variability within the species Leishmania aethiopica does not correlate with clinical variations of cutaneous leishmaniasis. Mol. Biochem. Parasitol. 106:239-248. [DOI] [PubMed] [Google Scholar]
- 232.Schonian, G., A. Nasereddin, N. Dinse, C. Schweynoch, H. D. Schallig, W. Presber, and C. L. Jaffe. 2003. PCR diagnosis and characterization of Leishmania in local and imported clinical samples. Diagn. Microbiol. Infect. Dis. 47:349-358. [DOI] [PubMed] [Google Scholar]
- 233.Schoone, G. J., A. Hailu, C. C. Kroon, J. L. Nieuwenhuys, H. D. Schallig, and L. Oskam. 2001. A fast agglutination screening test (FAST) for the detection of anti-Leishmania antibodies. Trans. R. Soc. Trop. Med. Hyg. 95:400-401. [DOI] [PubMed] [Google Scholar]
- 234.Schraner, C., B. Hasse, U. Hasse, D. Baumann, A. Faeh, G. Burg, F. Grimm, A. Mathis, R. Weber, and H. F. Gunthard. 2005. Successful treatment with miltefosine of disseminated cutaneous leishmaniasis in a severely immunocompromised patient infected with HIV-1. Clin. Infect. Dis. 40:e120-e124. [DOI] [PubMed] [Google Scholar]
- 235.Seaman, J., C. Boer, R. Wilkinson, J. de Jong, E. de Wilde, E. Sondorp, and R. Davidson. 1995. Liposomal amphotericin B (AmBisome) in the treatment of complicated kala-azar under field conditions. Clin. Infect. Dis. 21:188-193. [DOI] [PubMed] [Google Scholar]
- 236.Seaman, J., A. J. Mercer, and E. Sondorp. 1996. The epidemic of visceral leishmaniasis in western Upper Nile, southern Sudan: course and impact from 1984 to 1994. Int. J. Epidemiol. 25:862-871. [DOI] [PubMed] [Google Scholar]
- 237.Seaman, J., D. Pryce, H. E. Sondorp, A. Moody, A. D. Bryceson, and R. N. Davidson. 1993. Epidemic visceral leishmaniasis in Sudan: a randomized trial of aminosidine plus sodium stibogluconate versus sodium stibogluconate alone. J. Infect. Dis. 168:715-720. [DOI] [PubMed] [Google Scholar]
- 238.Seifert, K., and S. L. Croft. 2006. In vitro and in vivo interactions between miltefosine and other antileishmanial drugs. Antimicrob. Agents Chemother. 50:73-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Seifert, K., S. Matu, F. Javier Perez-Victoria, S. Castanys, F. Gamarro, and S. L. Croft. 2003. Characterisation of Leishmania donovani promastigotes resistant to hexadecylphosphocholine (miltefosine). Int. J. Antimicrob. Agents 22:380-387. [DOI] [PubMed] [Google Scholar]
- 240.Serarslan, G., and E. Atik. 2005. Expression of inducible nitric oxide synthase in human cutaneous leishmaniasis. Mol. Cell Biochem. 280:147-149. [DOI] [PubMed] [Google Scholar]
- 241.Silva, E. S., R. S. Pacheco, C. M. Gontijo, I. R. Carvalho, and R. P. Brazil. 2002. Visceral leishmaniasis caused by Leishmania (Viannia) braziliensis in a patient infected with human immunodeficiency virus. Rev. Inst. Med. Trop. Sao Paulo 44:145-149. [DOI] [PubMed] [Google Scholar]
- 242.Silveira, F. T., R. Lainson, and C. E. Corbett. 2004. Clinical and immunopathological spectrum of American cutaneous leishmaniasis with special reference to the disease in Amazonian Brazil: a review. Mem. Inst. Oswaldo Cruz 99:239-251. [DOI] [PubMed] [Google Scholar]
- 243.Sindermann, H., K. R. Engel, C. Fischer, and W. Bommer. 2004. Oral miltefosine for leishmaniasis in immunocompromised patients: compassionate use in 39 patients with HIV infection. Clin. Infect. Dis. 39:1520-1523. [DOI] [PubMed] [Google Scholar]
- 244.Singh, S. 2004. Mucosal leishmaniasis in an Indian AIDS patient. Lancet Infect. Dis. 4:660-661. [DOI] [PubMed] [Google Scholar]
- 245.Singh, S., A. Biswas, N. Wig, P. Aggarwal, R. Sood, and J. P. Wali. 1999. A new focus of visceral leishmaniasis in sub-Himalayan (Kumaon) region of northern India. J. Commun. Dis. 31:73-77. [PubMed] [Google Scholar]
- 246.Singh, S. P., D. C. Reddy, M. Rai, and S. Sundar. 2006. Serious underreporting of visceral leishmaniasis through passive case reporting in Bihar, India. Trop. Med. Int. Health 11:899-905. [DOI] [PubMed] [Google Scholar]
- 247.Sinha, P. K., V. N. Rabidas, K. Pandey, N. Verma, A. K. Gupta, A. Ranjan, P. Das, and S. K. Bhattacharya. 2003. Visceral leishmaniasis and HIV coinfection in Bihar, India. J. Acquir. Immune Defic. Syndr. 32:115-116. [DOI] [PubMed] [Google Scholar]
- 248.Soriano, V., C. Dona, R. Rodriguez-Rosado, P. Barreiro, and J. Gonzalez-Lahoz. 2000. Discontinuation of secondary prophylaxis for opportunistic infections in HIV-infected patients receiving highly active antiretroviral therapy. AIDS 14:383-386. [DOI] [PubMed] [Google Scholar]
- 249.Stark, D., S. Pett, D. Marriott, and J. Harkness. 2006. Post-kala-azar dermal leishmaniasis due to Leishmania infantum in a human immunodeficiency virus type 1-infected patient. J. Clin. Microbiol. 44:1178-1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Stebbing, J., B. Gazzard, and D. C. Douek. 2004. Where does HIV live? N. Engl. J. Med. 350:1872-1880. [DOI] [PubMed] [Google Scholar]
- 251.Sundar, S. 2001. Drug resistance in Indian visceral leishmaniasis. Trop. Med. Int. Health 6:849-854. [DOI] [PubMed] [Google Scholar]
- 252.Sundar, S., S. Agrawal, K. Pai, M. Chance, and M. Hommel. 2005. Detection of leishmanial antigen in the urine of patients with visceral leishmaniasis by a latex agglutination test. Am. J. Trop. Med. Hyg. 73:269-271. [PubMed] [Google Scholar]
- 253.Sundar, S., T. K. Jha, C. P. Thakur, J. Engel, H. Sindermann, C. Fischer, K. Junge, A. Bryceson, and J. Berman. 2002. Oral miltefosine for Indian visceral leishmaniasis. N. Engl. J. Med. 347:1739-1746. [DOI] [PubMed] [Google Scholar]
- 254.Sundar, S., T. K. Jha, C. P. Thakur, P. K. Sinha, and S. K. Bhattacharya. 2007. Injectable paromomycin for visceral leishmaniasis in India. N. Engl. J. Med. 356:2571-2581. [DOI] [PubMed] [Google Scholar]
- 255.Sundar, S., D. K. More, M. K. Singh, V. P. Singh, S. Sharma, A. Makharia, P. C. Kumar, and H. W. Murray. 2000. Failure of pentavalent antimony in visceral leishmaniasis in India: report from the center of the Indian epidemic. Clin. Infect. Dis. 31:1104-1107. [DOI] [PubMed] [Google Scholar]
- 255a.Sundar, S., and P. L. Olliaro. Miltefosine in the treatment of leishmaniasis: clinical evidence for informed clinical risk management. Ther. Clin. Risk Manag., in press. [PMC free article] [PubMed]
- 256.Terabe, M., T. Kuramochi, M. Ito, T. Hatabu, C. Sanjoba, K. P. Chang, T. Onodera, and Y. Matsumoto. 2000. CD4+ cells are indispensable for ulcer development in murine cutaneous leishmaniasis. Infect. Immun. 68:4574-4577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Thakur, C. P., T. P. Kanyok, A. K. Pandey, G. P. Sinha, A. E. Zaniewski, H. H. Houlihan, and P. Olliaro. 2000. A prospective randomized, comparative, open-label trial of the safety and efficacy of paromomycin (aminosidine) plus sodium stibogluconate versus sodium stibogluconate alone for the treatment of visceral leishmaniasis. Trans. R. Soc. Trop. Med. Hyg. 94:429-431. [DOI] [PubMed] [Google Scholar]
- 258.Thakur, C. P., S. Narayan, and A. Ranjan. 2003. Kala-azar (visceral leishmaniasis) and HIV coinfection in Bihar, India: is this combination increasing? J. Acquir. Immune Defic. Syndr. 32:572-573. [DOI] [PubMed] [Google Scholar]
- 259.Thakur, C. P., P. K. Sinha, R. K. Singh, S. M. Hassan, and S. Narain. 2000. Miltefosine in a case of visceral leishmaniasis with HIV co-infection; and rising incidence of this disease in India. Trans. R. Soc. Trop. Med. Hyg. 94:696-697. [DOI] [PubMed] [Google Scholar]
- 260.Tremblay, M., M. Olivier, and R. Bernier. 1996. Leishmania and the pathogenesis of HIV infection. Parasitol. Today 12:257-261. [DOI] [PubMed] [Google Scholar]
- 261.Troya, J., A. Casquero, G. Muniz, M. L. Fernandez-Guerrero, and M. Gorgolas. 2007. The role of splenectomy in HIV-infected patients with relapsing visceral leishmaniasis. Parasitology 134:621-624. [DOI] [PubMed] [Google Scholar]
- 262.Tumbarello, M., E. Tacconelli, S. Bertagnolio, and R. Cauda. 2000. Highly active antiretroviral therapy decreases the incidence of visceral leishmaniasis in HIV-infected individuals. AIDS 14:2948-2949. [DOI] [PubMed] [Google Scholar]
- 263.Turk, J. L., and A. D. Bryceson. 1971. Immunological phenomena in leprosy and related diseases. Adv. Immunol. 13:209-266. [DOI] [PubMed] [Google Scholar]
- 263a.UNICEF/UNAIDS/WHO/MSF. June 2005. Sources and prices of selected medicines and diagnostics for people living with HIV/AIDS: a joint UNICEF, UNAIDS, WHO, MSF project, 6th ed. WHO, Geneva, Switzerland.
- 264.Vilaplana, C., S. Blanco, J. Dominguez, M. Gimenez, V. Ausina, C. Tural, and C. Munoz. 2004. Noninvasive method for diagnosis of visceral leishmaniasis by a latex agglutination test for detection of antigens in urine samples. J. Clin. Microbiol. 42:1853-1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Villanueva, J. L., A. Alarcon, M. Bernabeu-Wittel, E. Cordero, D. Prados, C. Regordan, and J. Alvar. 2000. Prospective evaluation and follow-up of European patients with visceral leishmaniasis and HIV-1 coinfection in the era of highly active antiretroviral therapy. Eur. J. Clin. Microbiol. Infect. Dis. 19:798-801. [DOI] [PubMed] [Google Scholar]
- 266.WHO. 2000. Leishmania/HIV co-infection in south-western Europe 1990-1998: restrospective analysis of 965 cases, p. 14, vol. WHO/LEISH/2000.42. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 267.WHO. 1997. Leishmania/HIV co-infection. Epidemiological analysis of 692 restrospective cases. Wkly. Epidemiol. Rec. 72:49-54. [PubMed] [Google Scholar]
- 268.WHO. 1995. Report on the consultative meeting on Leishmania/HIV co-infection, p. 1-14, vol. WHO/LEISH/95.35. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 268a.WHO. May 2000. WHO fact sheet no. 116. World Health Organization, Geneva, Switzerland.
- 269.Wolday, D., H. Akuffo, S. Britton, A. Hathaway, and B. Sander. 1994. HIV-1 inhibits Leishmania-induced cell proliferation but not production of interleukin-6 and tumour necrosis factor alpha. Scand. J. Immunol. 39:380-386. [DOI] [PubMed] [Google Scholar]
- 270.Wolday, D., H. Akuffo, A. Demissie, and S. Britton. 1999. Role of Leishmania donovani and its lipophosphoglycan in CD4+ T-cell activation-induced human immunodeficiency virus replication. Infect. Immun. 67:5258-5264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Wolday, D., H. Akuffo, G. Fessahaye, A. Valantine, and S. Britton. 1998. Live and killed human immunodeficiency virus type-1 increases the intracellular growth of Leishmania donovani in monocyte-derived cells. Scand. J. Infect. Dis. 30:29-34. [DOI] [PubMed] [Google Scholar]
- 272.Wolday, D., N. Berhe, S. Britton, and H. Akuffo. 2000. HIV-1 alters T helper cytokines, interleukin-12 and interleukin-18 responses to the protozoan parasite Leishmania donovani. AIDS 14:921-929. [DOI] [PubMed] [Google Scholar]
- 273.Zhao, C., R. Cantin, M. Breton, B. Papadopoulou, and M. J. Tremblay. 2005. DC-SIGN-mediated transfer of HIV-1 is compromised by the ability of Leishmania infantum to exploit DC-SIGN as a ligand. J. Infect. Dis. 191:1665-1669. [DOI] [PubMed] [Google Scholar]
- 274.Zhao, C., B. Papadopoulou, and M. J. Tremblay. 2004. Leishmania infantum enhances human immunodeficiency virus type-1 replication in primary human macrophages through a complex cytokine network. Clin. Immunol. 113:81-88. [DOI] [PubMed] [Google Scholar]
- 275.Zhao, C., B. Papadopoulou, and M. J. Tremblay. 2004. Leishmania infantum promotes replication of HIV type 1 in human lymphoid tissue cultured ex vivo by inducing secretion of the proinflammatory cytokines TNF-alpha and IL-1 alpha. J. Immunol. 172:3086-3093. [DOI] [PubMed] [Google Scholar]
- 276.Zhao, C., S. Thibault, N. Messier, M. Ouellette, B. Papadopoulou, and M. J. Tremblay. 2006. In primary human monocyte-derived macrophages exposed to human immunodeficiency virus type 1, does the increased intracellular growth of Leishmania infantum rely on its enhanced uptake? J. Gen. Virol. 87:1295-1302. [DOI] [PubMed] [Google Scholar]
- 277.Zijlstra, E. E., M. S. Ali, A. M. el-Hassan, I. A. el-Toum, M. Satti, H. W. Ghalib, and P. A. Kager. 1992. Kala-azar: a comparative study of parasitological methods and the direct agglutination test in diagnosis. Trans. R. Soc. Trop. Med. Hyg. 86:505-507. [DOI] [PubMed] [Google Scholar]
- 278.Zijlstra, E. E., and A. M. el-Hassan. 2001. Leishmaniasis in Sudan. Visceral leishmaniasis. Trans. R. Soc. Trop. Med. Hyg. 95(Suppl. 1):S27-S58. [DOI] [PubMed] [Google Scholar]
- 279.Zijlstra, E. E., A. M. Musa, E. A. Khalil, I. M. el-Hassan, and A. M. el-Hassan. 2003. Post-kala-azar dermal leishmaniasis. Lancet Infect. Dis. 3:87-98. [DOI] [PubMed] [Google Scholar]