Abstract
The aim of this study was to determine whether impairment of sensory function after trigeminal nerve injury differs in severity among patients who report qualitatively different altered sensations. Data were obtained from 184 patients. Before and at 1, 3 and 6 months after orthognathic surgery, patients were grouped as having no altered sensation, negative sensations only (hypoesthetic), mixed sensations (negative + active), or active sensations only (paresthetic or dysesthetic). Bias-free estimates of contact detection and two-point discrimination were obtained to assess, via ANOVA, whether patients in the four groups exhibited different levels of sensory impairment. Impairment in contact detection and two-point discrimination was found to differ significantly among the groups at 6 months but not at 1 month. At 6 months, patients who reported negative sensations only exhibited the greatest impairment, on average, in contact detection; in contrast, patients who reported mixed sensations exhibited the greatest impairment in two-point discrimination. The least residual impairment at 6 months was observed in patients who reported no altered sensation. It is recommended that clinical judgments regarding nerve injury-associated sensory dysfunction not be based on threshold testing results without consideration of patients’ subjective reports of altered sensation.
Keywords: face, sensation, sensory impairment, orthognathic surgery, touch detection, two-point discrimination, tactile, threshold, sensitivity, trigeminal nerve injury
Contemporary maxillofacial surgical procedures pose significant risk (up to 100%) of injury to sensory branches of the trigeminal nerve. Sensation and sensory function are most often impaired, but seldom completely lost, and only a small percentage of patients develop post-traumatic neuropathic pain 6,14. Clinicians and clinical investigators vary in opinion regarding how patients should be evaluated for nerve injury following surgery. Most often, patients are questioned about the presence of altered sensation on the face and in the mouth. Less commonly, quantitative sensory testing methods are used to assess the severity of neurosensory impairment, and the time course and extent of the return of normal sensory function. There is growing consensus that patients’ subjective reports may provide a more sensitive indicator of the presence of post-traumatic nerve injury than neurosensory testing results, although testing is clearly required to determine the nature of the injury, e.g. whether sensory functions mediated by small versus large diameter fibers are mainly affected 6,9,13,14,24,25.
Anecdotal observations suggest that patients who report qualitatively different altered sensations provide different outcomes upon neurosensory testing. Cunningham et al. 3 noted that orthognathic surgery patients who reported tingling had lower thresholds for tactile detection and brush-stroke discrimination at 6 months after surgery than presurgically. In contrast, patients who reported only numbness tended to have higher thresholds postsurgically than presurgically. A similar observation was reported by Essick et al. 9, who showed that averaged data from trigeminal nerve-injured patients did not identify a deficit in cold pain detection. When patients who reported increased sensitivity to cold were excluded, re-analysis demonstrated the presence of substantial cold hypalgesia for the remaining group of individuals, i.e. lower temperatures were required for cold pain perception. Recently, Essick et al. 10 found that patients with cleft lip who reported altered sensation more akin to hyposensitivity exhibited higher two-point perception thresholds than patients whose altered sensations were more consistent with hypersensitivities.
The purpose of this study was to determine whether patients who report qualitatively different altered sensations after trigeminal nerve injury exhibit quantitatively different levels of impairment on two common threshold measures of sensory function. The altered sensation and sensory dysfunction that follow orthognathic surgery served as the experimental model. Based on the patients’ selection of words, sensation on the face was classified in one of four groups: no alteration, negative sensations only, mixed sensations (negative and active), or active sensations only. Using procedures that minimized response bias, thresholds for contact (touch) detection and two-point discrimination were obtained and compared among the four groups of patients defined by the differences in their altered sensations.
METHODS
Subjects
The data analyzed for this report came from 184 participants enrolled in a multi-center, double-blind, two-arm parallel group, stratified block randomized controlled clinical trial (Table 1) 19. The trial was designed to evaluate facial sensory re-training, a rehabilitative therapy that offers significant potential for patients who experience impaired sensory function as a result of trigeminal nerve injury. The analyses described in this report were exploratory since classification of altered sensation by the subject’s choice of words was not included in the design of the clinical trial. Consecutive patients with surgery dates after 1 December 2002 were eligible to be enrolled if they were scheduled for a bilateral sagittal split osteotomy to correct a severe malocclusion and/or a developmental disharmony. Inclusion and exclusion criteria are shown in Table 2.
Table 1.
Demographic Characteristics of Subjects Enrolled in the Sensory Retraining Clinical Trial
| Age (yrs.) |
|||||
|---|---|---|---|---|---|
| Surgery Performed | n | Mean | SD | % Female | % Male |
| Mandibular Only | 88 | 25.8 | 12.8 | 72 | 28 |
| + Genioplasty | 24 | 21.3 | 11.0 | 75 | 25 |
| Mandibular & Maxillary | 41 | 24.6 | 9.4 | 63 | 37 |
| + Genioplasty |
31 | 26.8 | 12.3 | 77 | 23 |
| Total | 184 | 25.1 | 11.8 | 71 | 29 |
Table 2.
Inclusion and Exclusion Criteria For Enrollment in the Sensory Retraining Clinical Trial
| Inclusion Criteria |
| 1. have a developmental dentofacial disharmony |
| 2. be 13-50 years of age |
| 3. be scheduled to receive a bilateral sagittal split either by mandibular osteotomy only or combined mandibular/maxillary surgery |
| Exclusion Criteria |
| 1. have a congenital anomaly or acute trauma |
| 2. have had previous facial surgery |
| 3. are pregnant at baseline |
| 4. do not have the ability to follow written English instructions |
| 5. are unwilling to sign informed consent |
| 6. report a moderate level of discomfort or problem caused by altered sensation of numbness or unusual feeling on the face at baseline |
| 7. report no altered sensation at one week post surgery |
| 8. have a medical condition associated with systemic neuropathy (e.g. diabetes, hypertension, kidney problems) |
Before a subject was enrolled, written consent (and assent if the subject was younger than 18) was obtained in accordance with the policies of the University of North Carolina Biomedical Institutional Review Board. Each subject enrolled and who consented after 14 April 2003 signed a Health Insurance Portability and Accountability Act consent form as well. Surgeries were performed by five attendants {AQ1}. Resident assistants were present during all surgeries.
Procedures
Subjects were appointed for data collection prior to surgery and at 1, 3 and 6 months after surgery. At each appointment the patient remained seated comfortably in a dental chair. Standard instructions were given prior to each procedure.
Assessment of Altered Sensation
At each appointment subjects were questioned about altered sensation on two cutaneous perioral sites: the chin and the upper lip. If no altered sensation was reported the patient was categorized as “no alteration”, i.e. as having normal sensation. If altered sensation was reported, the patient was asked to choose at least one word from a standardized list to describe the altered sensation that occurred spontaneously or when evoked by facial expression or touch anywhere on the site (Table 3) 20. A mirror was used to aid location of each site. More than one word could be selected for each site. Based on the words chosen, subjects were classified as reporting no alteration, negative (hypoesthetic) sensations only, mixed (negative + active) sensations or active (paresthetic or dysesthetic) sensations only. The categorization into four groups was based solely on the responses for the chin since very few subjects (29%, 11% and 6% at 1, 3 and 6 months, respectively) reported altered sensation on the upper lip (Figure 1). This was expected since only 72 of the 184 patients (39%) underwent LeFort surgery in close proximity to the infraorbital sensory nerves, supplying the innervation of the upper lip.
Table 3.
Words* on List Given to Patients for Selection to Describe Altered Sensations
| No Alteration: | No Words Selected |
| Hypoesthetic: | Numb, Warm, Wet, Rubbery, Cool, Swollen, Stretched, Wooden |
| Paresthetic: | Tickling, Tingling, Twitching, Pulling, Crawling, Vibrating, Drawing, Itching |
| Dysesthetic: | Prickling, Stinging, Electric, Painful, Cold, Hot, Tender, Excruciating, Sore, Burning, Shocking |
Adapted from Zuniga, J. R., Essick, G. K. A contemporary approach to the clinical evaluation of trigeminal nerve injuries. Atlas Oral Maxillofac Surg Clin North Am. 4:353-367, 1992.
1.
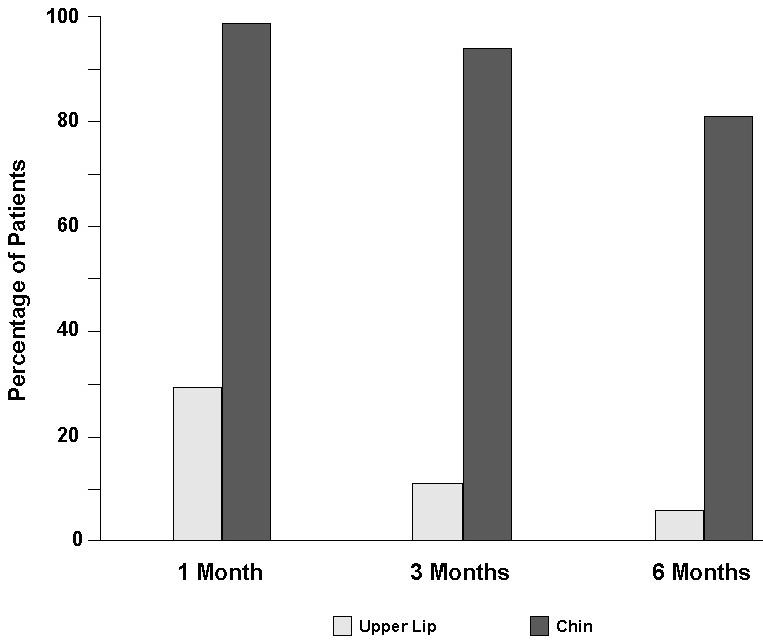
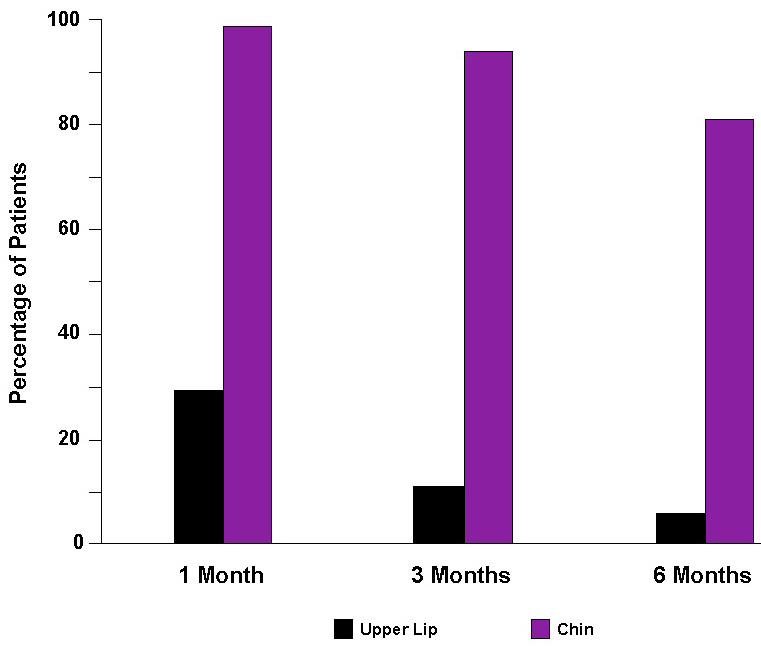
Percentage of patients who reported altered sensation on the chin and upper lip.
Assessment of Sensory Impairment
Following the self-assessments of altered sensation, sensory thresholds were estimated on four cutaneous perioral sites: the chin on the right and left sides, and the upper lip on the right and left sides. Given the low proportion of subjects who reported altered sensation on the upper lip, threshold data from the upper lip were not analyzed. Estimates for contact detection and two-point discrimination were obtained with a two-alternative, forced-choice test that minimized response bias.
The contact detection threshold is the minimum force of contact against the skin that is felt. It was measured using nylon monofilaments (von Frey Hairs, Touch Test Sensory Evaluators, Stoelting, Wooddale, IL, USA) that differed in stiffness, and thus in the force applied to the skin. Each stimulus trial consisted of two intervals. A filament was pressed into the skin during one interval and no stimulus was applied during the other interval. Subjects identified the interval (first or second) during which the filament was delivered. No feedback was given as to the correctness of the response. A computer program specified the random sequence of the site to the tested, the random sequence of the interval for stimulus application, and the monofilament to be used for each of 30 trials for each site 12. The tracking algorithm predicted the threshold force that would be detected in the correct interval on 75% of the trials. Estimates < 0.003 g or > 25 g were censored to these boundary values due to uncertainly in extreme, small sample estimates calculated by the tracking algorithm.
The two-point discrimination threshold is the minimum separation between two points for which a subject discriminates two points from one point of contact. The hand-held Disk-Criminator TM (Lafayette Instrument Co., Lafayette, IN, USA) was used for testing. This instrument consists of two disks of miniature probes of 14 different separations between 2 and 15 mm. Two additional custom-built instruments provided separation of 20 and 25 mm (see Fig. 1 of Chen et al. 2, p. 540). The prongs of the instruments were oriented parallel to the floor and perpendicular to the skin surface of each site. Testing was identical to that for contact detection with the following exceptions. Two probes were pressed into the skin during one interval and one probe during the other interval. Subjects identified the interval (first or second) during which two probes were applied. The threshold tracking algorithm specified the separation between the two probes to be used on each trial. The algorithm also predicted the threshold separation that would be detected in the correct interval on 75% of the trials. Estimates < 2 mm or > 25 mm were censored to these boundary values based on the stimuli used during testing.
Statistical Analysis
For each threshold measure at each post-surgery visit, the log10 transformed threshold value of the right and left side of the chin was normalized by subtracting the side-matched log10 transformed pre-surgery value to obtain a side-specific impairment ratio. The maximum impairment ratio of the right and left side at each visit for each of the threshold measures was used as the outcome variable. Variation between right and left side values existed pre-surgically but paired t-tests indicated that the differences between the right and left side sensitivity were not statistically significant (t=0.66; df=1,183; P = 0.51 for contact detection; and t=-0.66; df=1,184; P = 0.52 for two-point discrimination).
Analysis of covariance (Proc GLM; SAS 23) was used to assess whether the average impairment ratio for each threshold measure at 1, 3 and 6 months was related to patients’ reports of altered sensations on the chin. The classification of subjects based on the types of sensations reported was the explanatory variable. The pre-surgery threshold value of the side used in the calculation of the maximum impairment ratio served as a covariate in the analyses. Level of significance was set at 0.05. When the impairment ratios differed significantly among the four groups of subjects, pairwise comparisons of the average impairment ratio values were performed using least squares means (Table 4). Patients in a given group were considered impaired, on average, if the 95% confidence intervals (CI) for their average value did not include ‘0.0’. An inverse transformation was used to convert the log10 values back to the original threshold units for tabular and graphical displays.
Table 4.
P-values from the Analysis of Covariance and Least Squares Mean Procedures
| Ho: No | Comparisons of least squares means |
||||||
|---|---|---|---|---|---|---|---|
| Group Differences | Negative vs. No | Mixed vs. No | Active vs. No | Mixed vs. Negative | Active vs. Negative | Active vs. Mixed | |
| Contact Detection | |||||||
| 1 Month | 0.43 | ||||||
| 3 Months | 0.08 | ||||||
| 6 Months | 0.02 | 0.002 | 0.02 | 0.15 | 0.18 | 0.3 | 0.89 |
| 2-Point Discrimination | |||||||
| 1 Month | 0.87 | ||||||
| 3 Months | 0.03 | 0.02 | 0.03 | 0.45 | 0.53 | 0.04 | 0.06 |
| 6 Months | 0.001 | 0.28 | 0.0002 | 0.06 | 0.01 | 0.31 | 0.45 |
All overall models were statistically significant (P < 0.002). The pre-surgery side used to calculate the maximum of the right/left impairment ratio at each post-surgery visit was a statistically significant covariate in all models (P < 0.001).
RESULTS
The majority of the 184 participants were Caucasian and female (Table 1). All 184 patients underwent bilateral sagittal split surgery in close proximity to the inferior alveolar sensory nerves associated with the mandibular division of the trigeminal nerve. Thirty percent (30%) had a concurrent genioplasty procedure.
Altered sensation after surgery
Prior to surgery, practically none (2%) of the patients reported altered sensation on the chin. Upon questioning, those patients who reported altered sensation related it to the discomfort experienced upon adjustment of their orthodontic braces, and thus were not excluded from the study. However, at 1 month post surgery, nearly all (98%) of the patients reported some type of altered sensation on the chin. Most patients (81%) continued to experience altered sensation 6 months following surgery (Figure 1).
The percentages of patients whose post-surgical sensations on the chin were classified into the four categories of altered sensation are shown in Figure 2. The percentage of patients classified in the negative sensations only group remained constant at about 20% over the 6-month period while the percentage who reported a combination of negative and active (“mixed”) sensations decreased over time. The percentage who reported active sensations only tripled from 1 to 3 months and then decreased to 11% at 6 months.
2.
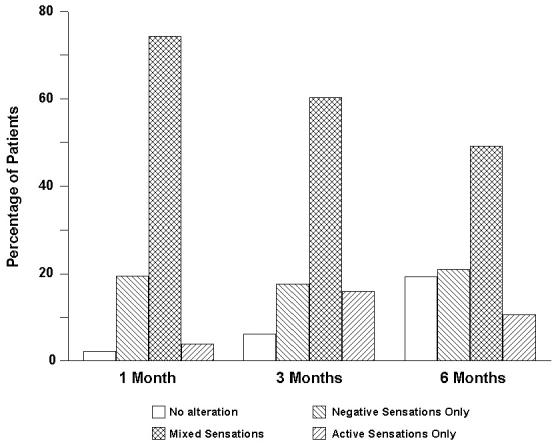
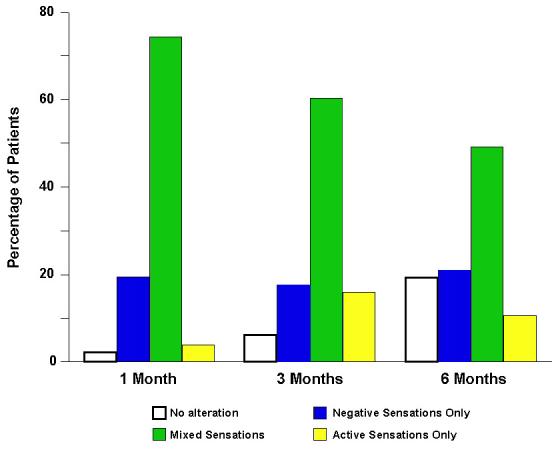
Percentage of patients classified into each of the four groups defined by the type of altered sensation reported on the chin.
Impairment in contact detection
The average threshold values for patients at 1, 3 and 6 months post surgery were elevated 62.7, 10.2, and 3.4 times the pre-surgical values, respectively (Figure 3). On average, those patients who reported no altered sensation at 6 months regained their pre-surgical capacity for detecting light touch on the skin. Those who reported some type of alteration in sensation at 6 months remained impaired, on average, regardless of the qualitative nature of the alteration.
3.
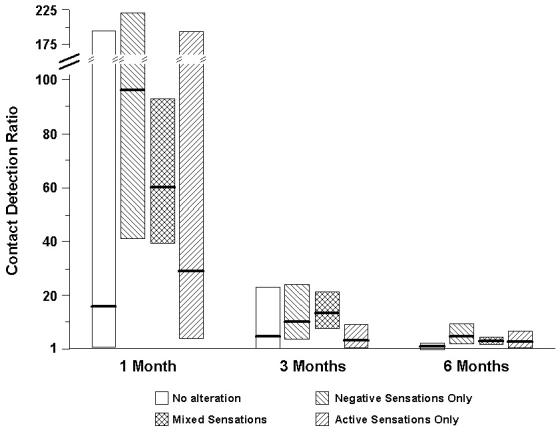
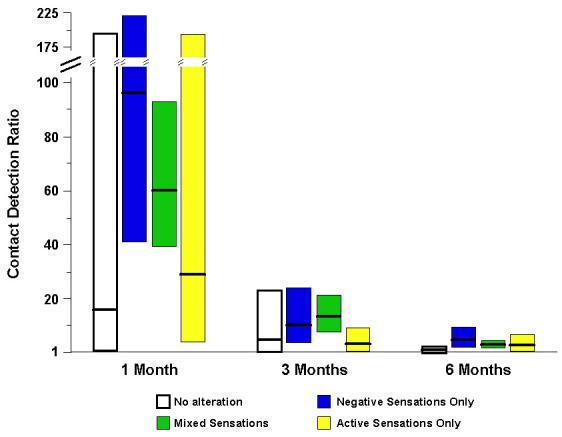
Impairment in contact (touch) detection on the chin. Shown are the geometric least squares means of the impairment ratio with 95% CI at 1, 3 and 6 months post surgery. The four groups of patients were defined by the words chosen to describe altered sensations on the chin.
The average impairment ratios did not differ statistically among the four groups of patients at 1 month post surgery (F=0.93; df=3,173; P=0.43) or 3 months post surgery (F=2.31; df=3,174; P=0.08). The groups did differ statistically at 6 months post surgery (F=3.29; df=3,170; P = 0.02; Figure 3). At 6 months, patients who reported only negative sensations (ratio = 5.7) were the most impaired, followed by patients who reported mixed sensations (ratio = 3.6). These two groups of patients were more impaired, on average, than patients who reported no altered sensation (ratio = 1.6; P = 0.002 and 0.02, respectively; see Table 4). On average, patients who reported only active sensations were slightly less impaired (ratio = 3.1) than patients who reported mixed sensations, and almost twice as impaired as patients with no alteration, but they did not differ statistically in impairment from any group (Table 4).
Impairment in two-point discrimination
Post-surgical impairment in two-point discrimination was substantially less than that for contact detection: The average threshold values for patients at 1, 3 and 6 months post-surgery were elevated 3.0, 2.0 and 1.7 times the pre-surgical values, respectively (Figure 4). Patients in all four groups, including those who reported no altered sensation, remained impaired, on average, in two-point discrimination throughout the 6-month post-surgery period. The average impairment ratios did not differ among the four groups of patients at 1 month post-surgery (F=0.24; df=3,174; P = 0.87), in contrast to 3 months post-surgery (F=2.98; df=3,175; P=0.03) and 6 months post-surgery (F=5.49; df=3,169; P=0.001). Patients who reported no altered sensation exhibited the mildest average impairment at all post-surgery visits. At 3 months, patients who reported only negative sensations were most impaired, on average; whereas, at 6 months, patients who reported mixed sensations were the most impaired.
4.
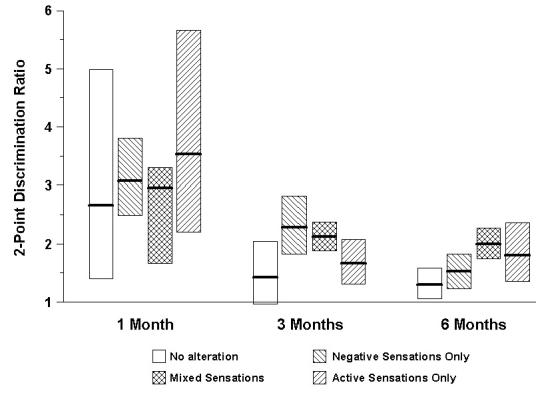
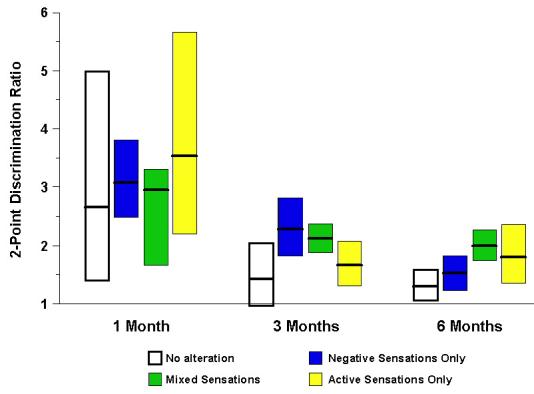
Impairment in two-point discrimination on the chin. Shown are the geometric least squares means of the impairment ratio with 95% CI at 1, 3 and 6 months post surgery. The four groups of patients were defined by the words chosen to describe altered sensations on the chin.
Statistical analysis revealed that patients who reported only negative sensations at 3 months post surgery (ratio = 2.3) were more impaired, on average, than patients who reported no altered sensation (ratio = 1.6; P = 0.02) or only active sensations (ratio = 1.7; P = 0.04; see Table 4). Patients who reported mixed sensations were similarly impaired (ratio = 2.1) to those who reported only negative sensations. By 6 months the patients with mixed sensations exhibited significantly greater impairment (ratio = 2.0) than patients who reported only negative sensations (ratio = 1.5; P = 0.01) or no altered sensation (ratio = 1.3; P = 0.0002). Average levels of impairment were similar at 3 and 6 months for patients who reported mixed sensations, and for patients who reported only active sensations. Patients who reported only active sensations did not differ statistically in impairment from patients who reported no altered sensation, although their mean impairment ratio was greater (Table 4).
DISCUSSION
The relationship between qualitatively different altered sensations and sensory impairment has not been studied systematically in patients after trigeminal nerve injuries. Anecdotal observations (presented earlier in this paper) have demonstrated that patients who report different altered sensations exhibit different outcomes upon neurosensory testing. Previous studies have also shown that patients with neuropathic pain, secondary to damage of the trigeminal or spinal nerves, can be either hyposensitive or hypersensitive to mechanical stimulation of the skin. Combining their threshold values in clinical studies is known to mask differences in sensory function (i) between patients and control subjects 1,22 and (ii) between affected and non-affected sides of the patient’s body 4,17. The distinction offered by consideration of patients’ altered sensation is also prognostic for the individual patient. As an example, LaBanc and Gregg 16 reported that 521 patients with injured inferior alveolar or lingual nerves were classified as being hypoesthetic or as hyperesthetic/hyper-responsive during clinical examination and stimulus testing. All of the patients underwent nerve exploration and repair surgery. Surgical success was defined as minimal recovery of gross touch perception and a global pain reduction greater than 30%. The chance of success was found to be almost 1.5 times greater, on average, for patients classified as hypoesthetic compared to patients classified as hyperesthetic.
Most patients who experience iatrogenic injury to the trigeminal nerve do not develop neuropathic pain. Even so, a better understanding of the qualitative nature of the altered sensation and its relationship to impairments in sensory function, as assessed by neurosensory testing, is needed to appreciate the burden imposed on patients. For example, in a recent study the authors showed that patient-perceived difficulties in everyday life following orthognathic surgery are related to the type of altered sensation experienced 18. Patients whose sensations were uncomfortable or painful (dysesthetic sensations) reported the most difficulty followed by those who experienced non-painful sensations that are not normally present (i.e. positive or paresthetic sensations), than those who experienced only a simple loss in sensation (i.e. negative or hypoesthetic sensations).
Effect of time following surgery
A consistent finding in the present study was that the average threshold values obtained at 1 month after surgery did not vary systematically among the four groups of patients. Two hypothetical explanations can be offered to explain the lack of differentiation before 3 months post surgery. First, it is known that the variance in threshold measurements, both among subjects and within the same subject upon repeated measurement, increases with the mean magnitude of the measurement: the higher the threshold value, the less precisely it is usually measured 8,11. Less precision in the estimates of the thresholds at 1 month, estimates which were generally higher in value than those at 3 and 6 months, might have prevented detection of group differences in the values. Alternatively, with the passage of time after surgery, inflammation and swelling subside and residual altered sensation becomes more closely associated with nerve injury and its central consequences 21. Given this explanation, the relationship between qualitatively different altered sensations and impairments in threshold values is predicted to grow stronger with time following surgery, as was observed in the present study.
Impairment in contact detection
The use of contact detection thresholds in the evaluation of trigeminal nerve-injured patients is strongly supported by prior work 9,14,24. In a recent study, Teerijoki-Oksa et al. 24 showed that impairment in contact detection 2 weeks after orthognathic surgery correlates better with the severity of nerve damage, documented intraoperatively using nerve conduction methods, than does impairment in brush-stroke direction discrimination, spatial acuity, or warm/cold or sharp/blunt differentiation. The current study supports this finding. At every post-surgical visit, the contact detection thresholds relative to pre-surgery values were elevated to a greater extent than the two-point discrimination thresholds, on average. Of particular interest was the trend for impairment at 3 and 6 months post surgery to be less, on average, for patients who reported active (paresthetic or dysesthetic) sensations only than for patients who reported negative sensations only. This finding is generally consistent with that of Cunningham et al. 3 who noted that patients who reported tingling sensations did not have higher threshold values for tactile detection and brush-stroke discrimination at 6 months after orthognathic surgery than before, unlike patients who reported only numbness. In the present study, no evidence was found to suggest that the post-surgery threshold values of patients who reported active sensations were lower than the pre-surgery values.
Impairment in two-point discrimination
Measures of two-point discrimination are complex and are determined not only by spatial information, but by intensity and temporal information as well 15. In addition to spatial cues, subjects are thought to attend to the greater force, the greater area of skin contact, and differences in the timing of the pressures from two points in discriminating two points from one point of contact. Overall, at 3 and 6 months following surgery the threshold values, relative to the pre-surgery values, were highest for patients who reported mixed sensations. The authors hypothesize that the active, i.e. additional, sensations added noise to both weakened spatial and non-spatial cues from the loss in innervation. This resulted in greater impairment in the two-point thresholds for patients who experienced mixed sensations than for patients who experienced negative sensations only, active sensations only, or no alteration in sensation.
Similarity of sensory impairments in patients with only active sensations and patients with no alteration
For both threshold measures at 1, 3 and 6 months post surgery, the average impairment ratio of patients who reported active sensations only was typically higher than that of patients who reported no alteration in sensation, but the differences between these two groups were not statistically significant. This indicates that patients who report only active sensations do not consistently, on average, exhibit greater impairment than that observed in patients who report no alteration in sensation. These observations further suggest at least partial segregation in the neural processes that results in negative versus active sensations, and that different processes are associated with different levels of impairment in sensory function.
Neurosensory status at 6 months post surgery
At 6 months post surgery, contact detection thresholds for only the group of patients who reported no altered sensation had, on average, returned to the pre-surgery values, but the ability to discriminate two points from one point of contact was still impaired in this group. All of the groups that reported an alteration in sensation showed impairment, although to different extents. Similar differences, unidentified in previous studies, may underlie the controversial relationship between neurosensory testing results and patients’ subjective reports of altered sensation that have been reported in the literature 3,5-7,9.
Clinical implications
The current study confirms the usefulness of patients’ reports of altered sensation and of threshold measures of sensory function in the evaluation of patients with trigeminal nerve injuries. It also indicates that changes in threshold measures of sensory function during the first 6 months post-surgery cannot be understood fully in the absence of patients’ subjective reports of altered sensations. Impairment in contact detection and two-point discrimination cannot be attributed to altered response biases associated with altered skin sensation, but rather to differences in patients’ abilities to detect and discriminate tactile stimuli. Further work is required to determine how group differences in mean threshold values over time can be used to interpret the changes in neurosensory function observed in individual patients. One can anticipate, for example, a better understanding of patients who report greater or more debilitating altered sensation than reflected by assessment of sensory thresholds on affected versus non-affected facial skin sites. By studying the relationship between altered sensation and sensory impairment longitudinally for 1-2 years, it may be possible to better predict during the first few postoperative months which patients are likely to have favorable or unfavorable sensory recoveries.
Acknowledgements
The authors wish to thank Atousa Safavi, Colleen Ellett Farmer, Harold Jennings, Debora Price, and Akshya Patel for their efforts in patient enrollment and data collection.
Source of support: National Institute of Dental and Craniofacial Research (NIH grant DE01367).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Greg K. Essick, Department of Prosthodontics and Center for Neurosensory Disorders.
Ceib Phillips, Department of Orthodontics.
Timothy A. Turvey, Department of Oral and Maxillofacial Surgery, University of North Carolina, Chapel Hill, NC 27599-7450.
Myron Tucker, Private Practice, 411 Billingsley Road, Charlotte, NC 28211.
References
- 1.Baumgärtner U, Magerl W, Klein T, Hopf HC, Treede RD. Neurogenic hyperalgesia versus painful hypoalgesia: two distinct mechanisms of neuropathic pain. Pain. 2002;96:141–151. doi: 10.1016/s0304-3959(01)00438-9. doi: 10.1016/S0304-3959(01)00438-9. [DOI] [PubMed] [Google Scholar]
- 2.Chen CC, Essick GK, Kelly DG, Young MG, Nestor JM, Masse B. Gender-, side- and site-dependent variations in perioral spatial resolution. Arch Oral Biol. 1995;40:539–548. doi: 10.1016/0003-9969(94)00202-m. doi: 10.1016/0003-9969(94)00202-M. [DOI] [PubMed] [Google Scholar]
- 3.Cunningham LL, Tiner BD, Clark GM, Bays RA, Keeling SD, Rugh JD. A comparison of questionnaire versus monofilament assessment of neurosensory deficit. J Oral Maxillofac Surg. 1996;54:454–459. doi: 10.1016/s0278-2391(96)90120-2. doi: 10.1016/S0278-2391(96)90120-2. [DOI] [PubMed] [Google Scholar]
- 4.Eide PK, Jørum E, Stenehjem AE. Somatosensory findings in patients with spinal cord injury and central dysaesthesia pain. J Neurol Neurosurg Psychiatry. 1996;60:411–415. doi: 10.1136/jnnp.60.4.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Essick GK. Comprehensive clinical evaluation of perioral sensory function. Oral Maxillofac Surg Clin North Am. 1992;4:503–526. [Google Scholar]
- 6.Essick GK. Psychophysical assessment of patients with posttraumatic neuropathic trigeminal pain. J Orofac Pain. 2004;18:345–354. [PubMed] [Google Scholar]
- 7.Essick GK, Austin S, Phillips C, Kiyak HA. Short-term sensory impairment following orthognathic surgery. Oral Maxillofac Surg Clin North Am. 2001;13:295–313. [Google Scholar]
- 8.Essick G, Guest S, Martinez E, Chen C, McGlone F. Site-dependent and subject-related variations in perioral thermal sensitivity. Somatosens Mot Res. 2004;21:159–175. doi: 10.1080/08990220400012414. doi: 10.1080/08990220400012414. [DOI] [PubMed] [Google Scholar]
- 9.Essick GK, Patel S, Trulsson M. Mechanosensory and thermosensory changes across the border of impaired sensitivity to pinprick after mandibular nerve injury. J Oral Maxillofac Surg. 2002;60:1250–1266. doi: 10.1053/joms.2002.35721. doi: 10.1053/joms.2002.35721. [DOI] [PubMed] [Google Scholar]
- 10.Essick GK, Phillips C, Trotman C-A. Factors affecting lip vermillion sensory thresholds. 2006. Functional outcomes of cleft lip surgery: Part IV. Submitted. {AQ2} [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Feldman JA, Essick GK, Zuniga JR, Phillips C. Inter-examiner reliability of three subjective clinical neurosensory tests. Int J Adult Orthod Orthognath Surg. 1997;12:273–285. [Google Scholar]
- 12.Harvey L. Efficient estimation of sensory thresholds. Behav Res Methods Instrum Comput. 1986;18:623–632. [Google Scholar]
- 13.Jääskeläinen SK. The utility of clinical neurophysiological and quantitative sensory testing for trigeminal neuropathy. J Orofac Pain. 2004;18:355–359. [PubMed] [Google Scholar]
- 14.Jääskeläinen SK, Teerijoki-Oksa T, Virtanen A, Tenovuo O, Forssell H. Sensory regeneration following intraoperatively verified trigeminal nerve injury. Neurology. 2004;62:1951–1957. doi: 10.1212/01.wnl.0000129490.67954.c2. [DOI] [PubMed] [Google Scholar]
- 15.Johnson KO, Van Boven RW, Hsiao SS. The perception of two points is not the spatial resolution threshold. In: Bovie J, Hansson P, Lindblom U, editors. Touch, Temperature, and Pain in Health and Disease: Mechanisms and Assessments. IASP Press; Seattle: 1994. p. 389. [Google Scholar]
- 16.LaBanc JP, Gregg JM. Trigeminal Nerve Injury: basic problems, historical perspectives, early successes, and remaining challenges. Oral Maxillofac Surg Clin North Am. 1992;4:277–284. [Google Scholar]
- 17.Lindblom U, Verrillo RT. Sensory functions in chronic neuralgia. J Neurol Neurosurg Psychiatry. 1979;42:422–435. doi: 10.1136/jnnp.42.5.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Phillips C, Essick G, Blakey G, Tucker M. Relationship between patients’ perception of postsurgical sequelae and altered sensations following BSSO. J Oral Maxillofac Surg. 2006 doi: 10.1016/j.joms.2005.12.078. In Press. {AQ2} [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Phillips C, Essick G, Preisser JS, Turvey TA, Tucker M, Lin D. Sensory retraining following orthognathic surgery: Effect on patient perception of altered sensation. J Oral Maxillofac Surg. 2006 doi: 10.1016/j.joms.2006.09.035. Accepted. {AQ2} [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Phillips C, Essick G, Zuniga J, Tucker M, Blakey G. Qualitative Descriptors Used by Patients following Orthognathic Surgery to Portray Altered Sensation. J Oral Maxillofac Surg. 2006;64:1751–1760. doi: 10.1016/j.joms.2005.11.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rood JP. Degrees of injury to the inferior alveolar nerve sustained during the removal of impacted mandibular third molars by the lingual split technique. Br J Oral Surg. 1983;21:103–116. doi: 10.1016/0007-117x(83)90054-9. doi: 10.1016/0007-117X(83)90054-9. [DOI] [PubMed] [Google Scholar]
- 22.Rowbotham MC, Petersen KL, Fields HL. Is postherpetic neuralgia more than one disorder? Pain Forum. 1998;7:231–237. [Google Scholar]
- 23.SAS Institute, Inc . SAS/STAT ® User’s Guide, Version 9.1. SAS Institute, Inc; Cary, NC: 2004. [Google Scholar]
- 24.Teerijoki-Oksa T, Jääskeläinen S, Forssell K, Virtanen A, Forssell H. An evaluation of clinical and electrophysiologic tests in nerve injury diagnosis after mandibular sagittal split osteotomy. Int J Oral Maxillofac Surg. 2003;32:15–23. doi: 10.1054/ijom.2002.0325. doi: 10.1054/ijom.2002.0325. [DOI] [PubMed] [Google Scholar]
- 25.Westermark A, Englesson L, Bongenhielm U. Neurosensory function after sagittal split osteotomy of the mandible: A comparison between subjective evaluation and objective assessment. Int J Adult Orthod Orthognath Surg. 1999;14:268–275. [PubMed] [Google Scholar]


