Abstract
Inhaled Yersinia pestis produces a severe primary pneumonia known as pneumonic plague, which is contagious and highly lethal to humans and animals. In this study, we first determined the susceptibility of Y. pestis KIM6 to antimicrobial molecules of the airways. We found that (i) rat bronchoalveolar lavage fluid (rBALF) effectively killed KIM6 cells growing at 37°C; (ii) the antibacterial components of rBALF were small peptides (<10 kDa) that included two cationic antimicrobial peptides (CAMPs), the rat cathelicidin rCRAMP, and β-defensin RBD-1; (iii) the human cathelicidin LL-37 killed KIM6 cells as well as rBALF did; and (iv) the bactericidal property of LL-37 was synergistically amplified by human β-defensin 1, another constitutively expressed pulmonary CAMP. Second, the effects of three major surface proteins of Y. pestis, namely, the capsular antigen fraction 1 (F1), the pH 6 antigen (Psa fimbriae), and the outer membrane protease Pla, on the bactericidal effect of the antimicrobial rBALF peptides was determined with corresponding deletion mutants. We showed that (i) a Y. pestis psa mutant was only slightly more susceptible to rBALF than the parental KIM6 strain, (ii) a caf (F1 gene) mutant and a caf psa mutant were resistant to rBALF or LL-37, (iii) a caf pla mutant was as susceptible to the effect of rBALF or LL-37 as KIM6 was (caf+ pla+), and (iv) only the single caf mutant (pla+), but not KIM6 or the caf pla double mutant, degraded LL-37. The activity of Pla toward LL-37 was confirmed with pla mutants carrying a single-residue substitution affecting plasminogen cleavage. Taken together, our data indicated that Pla might act as a virulence factor not only by processing plasminogen but also by inactivating CAMPs, particularly when F1 is not expressed.
Yersinia pestis is transmitted by fleas or aerosol, causing bubonic or pneumonic plague by infecting regional lymph nodes or the lungs and septicemic plague when local containment is bypassed (45). Y. pestis uses an arsenal of virulence factors that render its entrance and rapid dissemination into the host as surreptitious as possible. These factors are thought to be most important during the first hours following infection to avoid alarming the innate immune system and to avoid phagocytosis. We recently found that in addition to being antiphagocytic (18, 27), the capsular antigen fraction 1 (F1) and the pH 6 antigen (Psa) inhibit bacterial uptake by respiratory tract epithelial cells (38), with the latter protein doing so by interacting with a host receptor that does not direct internalization (21). In addition, Y. pestis injects several antiphagocytic proteins directly into host cells through its type III secretion system (66). Some injected type III secretion system effector proteins, such as YopJ/YopP and YopH, have efficient anti-inflammatory properties (66), whereas the importance of the LcrV protein in activating interleukin-10 through Toll-like receptor 2 (TLR2) was recently contradicted (3, 47, 50). Y. pestis also makes a noninflammatory lipopolysaccharide (LPS) at mammalian body temperature, thereby escaping the typical LPS-induced stimulation of TLR4 (40, 48). After delivery through a fleabite, Y. pestis quickly spreads to the local lymph node, in a process that is facilitated by Psa and the plasminogen activator protein (Pla) (13). Pla is a bacterial outer membrane protein that acts as a protease that cleaves plasminogen to plasmin and degrades α2-antiplasmin, a plasmin inhibitor (6, 33, 57). Pla is also a mediator of bacterial binding to extracellular matrix proteins such as laminin (35). Pla is essential for bubonic plague (but not for septicemic plague) after flea-mediated transmission (53, 57, 68). Pla is also essential for the development of (but not dissemination of) primary pneumonic plague (36). Plague lethality is generally assumed to be due to sepsis.
Lung bronchoalveolar space contains a variety of molecules with antibacterial properties, such as lactoferrin, complement, collectins or surfactant proteins, and antimicrobial peptides (AMPs), particularly cationic AMPs (CAMPs), such as cathelicidins and β-defensins (37, 67, 70). Here we investigated the effect of airway antimicrobial molecules on Y. pestis and observed killing effects of rat bronchoalveolar lavage fluid (rBALF), mediated by AMPs. In addition, three surface-exposed bacterial molecules were found to modulate the susceptibility of Y. pestis to rBALF and the human cathelicidin LL-37.
MATERIALS AND METHODS
Reagents.
Survanta (Beractant; 25 mg phospholipids/ml and <1.0 mg/ml protein) (Ross Products Division, Abbott Laboratories, Columbus, OH) is a natural bovine lung extract containing phospholipids (with 80% of the total lipids being phosphatidylcholine [PC]), neutral lipids, fatty acids, surfactant protein B (SP-B), and SP-C. rBALF and Survanta were generously supplied by S. R. Bates (Institute for Environmental Medicine, University of Pennsylvania, PA). Synthetic LL-37 (human) cathelicidin and β-defensin 1 (human) were obtained from Phoenix Pharmaceuticals, Inc. (Burlingame, CA). A monoclonal antibody against human LL-37/CAP18 was obtained from Cell Sciences (Canton, MA). The rat cathelicidin rCRAMP, rat β-defensin-1 (RBD-1), and polyclonal rabbit antibodies against both peptides were obtained from Santa Cruz Biotechnology Inc. (Santa Cruz, CA).
Bacterial strains and plasmid constructs.
Y. pestis strains and plasmids used in this study are listed in Table 1. Y. pestis strains were grown overnight in brain heart infusion (BHI) broth at 26°C, diluted 1:100 in fresh BHI broth, and cultured overnight at 37°C. Under these conditions, the pH of the spent broth was 6.2 to 6.4, resulting in the expression of both the F1 and Psa structures on the bacterial surface. Appropriate antibiotics were used when required. DSY26 was constructed by allelic exchange, using strain JG153 and plasmid pLS009 (38). The pla gene was deleted from strain DSY9 to obtain strain DSY85 by using a lambda red recombination system (15). Briefly, the primer sequences were described previously (36), and the primers were used to prepare an amplified PCR product for the replacement of the pla gene with a kanamycin cassette. Strain DSY9 carrying the lambda red plasmid pSIM9 (16) was grown to log phase at 26°C, the red recombinase genes were induced for 15 min at 42°C, and the bacteria were transformed by electroporation with the gel-purified amplicons. Kanamycin-resistant recombinants were selected on BHI agar and grown for several cycles in BHI broth containing kanamycin (55 μg/ml) to select for bacteria containing only the pPCP1Ω aphA Δpla plasmid. The recombinant strain was cured of pSIM9 by growth of the bacteria overnight at 37°C, and removal of the kanamycin resistance gene was performed as described previously, using plasmid pCP20 (15). DSY87 and DSY88 were constructed by introducing pPCP1Ω aphA Δpla into JG153 and DSY50, respectively. The constructs were checked by agarose gel electrophoresis, restriction mapping of pPCP1 and its derivatives, PCR, and Pla activity. The in vitro growth rates of the mutants were comparable to that of the parental strain KIM6.
TABLE 1.
Bacterial strains and plasmids used in this study
| Strain or plasmid | Genotype or characteristics | Reference |
|---|---|---|
| Strains | ||
| KIM6 | KIM5 pCD1− (LCR−) pgm | 22 |
| JG153 | KIM6 pPCP1− (pla) | 57 |
| DSY9 | KIM6 Δcaf::blaM | 38 |
| DSY13 | KIM6 Δpsa::aphA | 38 |
| DSY14 | KIM6 Δcaf::blaM Δpsa::aphA | 38 |
| DSY26 | JG153 Δcaf::blaM | This study |
| DSY50 | JG153 Δcaf Δpsa | 38 |
| DSY85 | DSY9 Δpla | This study |
| DSY87 | JG153 pPCP1ΩaphA Δpla | This study |
| DSY88 | DSY50 Δcaf Δpsa pPCP1ΩaphA Δpla | This study |
| Plasmids | ||
| pDMS197 | oriT oriV (R6K) sacB Tcr | 20 |
| pLS009 | pDMS197 Δcaf::blaM | 38 |
| pSIM9 | pRK2 trfA(Ts) | 16 |
| pCP20 | FLP+ λci857+ λpR Rep(Ts) Apr Cmr | 15 |
| pBR322 | ori ColE1 Apr Tcr | 7 |
| pCS267 | pBR322-psaABC | 38 |
| pLG339 | pSC101 Kmr | 58 |
| pCS331 | pLG339-caf1M-caf1A-caf1 | 38 |
| pMRK1 | pla in pSE380 | 33 |
| pMRK1H101V | Pla(H101V) | 33 |
| pMRK1D206A | Pla(D206A) | 33 |
Fractionation of rBALF.
The rBALF was separated into two fractions after being centrifuged at 20,000 × g for 1 h. The pellet contained the large surfactant aggregates (phospholipids, SP-A, SP-B, SP-C, and SP-D), whereas all other soluble molecules remained in the supernatant. The latter fraction was subjected to gel filtration high-performance liquid chromatography through a Sephadex-G75 column. For proteinase K treatment of rBALF, the soluble fraction (0.125 mg/ml) was digested for 4 h at 56°C with proteinase K (5 μg; Roche Applied Science) in 50 μl digestion buffer (10 mM Tris, pH 7.8, 5 mM EDTA). To analyze the reducing effect of dithiothreitol (DTT), rBALF was treated with 10 mM DTT at room temperature for 1 h.
Antimicrobial assays.
Bacteria were grown to mid-log phase in BHI broth at 37°C. Twofold serial dilutions of rBALF (or its different fractions), LL-37, β-defensin 1, or polymyxin B were added to the bacteria grown in BHI broth to log phase, and the bacteria were diluted to approximately 2 × 106 CFU/ml or 2 × 107 CFU/ml in round-bottomed wells of 96-well microtiter plates. The plates were incubated on a rotary shaker at 37°C. After a 5-h or overnight incubation, aliquots were removed and serial 10-fold dilutions were plated onto TB (13 g tryptose [Difco], 2.5 g NaCl, 3.0 g Bacto beef extract paste in 1 liter) agar plates. The bactericidal activity was assessed after counting of colonies (CFU) on agar plates and by visual inspection of the growth. The minimal bactericidal concentration (MBC) was defined as the concentration of the antimicrobial at which no visible colonies were seen on the plate. All experiments were performed in duplicate. In some assays, purified F1 protein, isolated by heat extraction from the psa mutant strain DSY13 (38), or 987P fimbriae (30) were added at the same time as rBALF and were not removed during the incubation period. In other assays, rBALF or LL-37 was incubated with bacteria for 5 h before removal of the bacteria by centrifugation, filtration of the supernatants through 0.2-μm membranes, and assay of the filtrates for antimicrobial activity.
Western blotting.
For the detection of LL-37 and rCRAMP, samples were resolved by sodium dodecyl sulfate-polyacrylamide gel electrophoresis, using a Tris-Tricine discontinuous buffer system. The gels were electroblotted onto polyvinylidene difluoride membranes. Nonspecific binding sites on the membrane were blocked overnight in 5% dry milk. The blots were probed with a mouse monoclonal anti-LL-37 antibody and a goat polyclonal anti-rCRAMP antibody, using horseradish peroxidase-conjugated secondary antibodies and enhanced chemiluminescence for detection.
ELISA.
The amount of rCRAMP or RBD-1 in rBALF was determined by enzyme-linked immunosorbent assay (ELISA)-based inhibition assays. For this purpose, 96-well ELISA plates (Immulon 4A; Dynatech Laboratories Inc., Chantilly, VA) were coated with 0.1 μg (in 100 μl 0.1 M carbonate buffer, pH 9.6) of proprietary carboxy-terminal fragments of rCRAMP (molecular mass of 2.23; approximately 20 amino acids) or RBD-1 (sc-34170 P and sc-10851 P; Santa Cruz Biotechnology, Inc.). The plates were blocked with 5% bovine serum albumin (BSA) in phosphate-buffered saline (PBS) at 37°C for 30 min, washed three times with PBS containing 0.05% Tween 20, and incubated for 1 h at 37°C with donkey polyclonal anti-rCRAMP or anti-RBD-1 antibody (1/8,000 or 1/12,000, respectively, corresponding to the dilution showing 50% antibody binding to the coated peptides). For inhibition of binding, serial twofold dilutions of rBALF or the rCRAMP or RBD-1 fragments were preincubated for 1 h at 37°C with the diluted anti-rCRAMP or anti-RBD-1 antibody in 0.5% BSA. After being washed three times with PBS, the plates were incubated with horseradish peroxidase-conjugated anti-donkey immunoglobulin G for 1 h at 37°C. Following the last washing cycles, bound antibody was detected by using 1-Step Turbo TMB-ELISA (Pierce Biotechnology, Rockford, IL) and reading the absorbance at 450 nm.
Immunoadsorption assay.
rCRAMP and RBD-1 were removed from rBALF by immunoadsorption, using the following protocol. Goat anti-rCRAMP antibody (2.0 μg) and anti-RBD-1 antibody (2.0 μg) were adsorbed onto 60.0 μl of protein G magnetic beads (New England Biolabs Inc., Ipswich, MA) by overnight incubation in PBS, pH 7.4, at 4°C. After three washing steps with PBS, beads were blocked with 5% BSA in PBS for 1 h at 4°C. The magnetic beads were then washed three times with PBS and incubated with rBALF (125 μg protein) in PBS containing 1% BSA for 3 h at 4°C. The beads were removed, and the supernatant containing the remaining molecules of rBALF was assessed for antimicrobial activity. As a negative control, the unrelated goat anti-mouse immunoglobulin G antibody (4.0 μg) was adsorbed onto protein G magnetic beads as described above, and those beads were incubated with rBALF. The antimicrobial activity against Y. pestis KIM6 was determined by colony counts (CFU) after 5 h of incubation with untreated or rBALF-treated (2.5 μg/ml) bacteria. The percentage of antimicrobial activity was calculated by normalizing to 100% the antimicrobial activity of untreated rBALF.
Plasminogen activation.
Measurement of plasminogen activation was done as described by Kukkonen et al. (33). Briefly, 2 × 106 bacteria grown in BHI broth at 37°C were resuspended in PBS and incubated with 4 μg of human Glu-plasminogen and the chromogenic plasmin substrate Val-Leu-Lys-p-nitroanilide (0.45 mM) in a total volume of 200 μl at 37°C. Breakdown of the chromogenic substrate was measured at 405 nm for 30 min to 6 h.
RESULTS
rBALF contains antimicrobial molecules that kill Yersinia pestis.
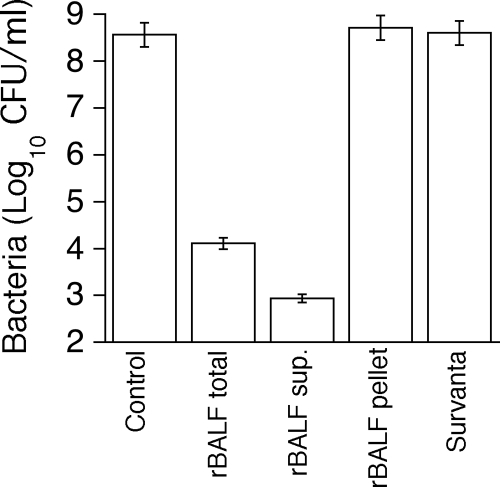
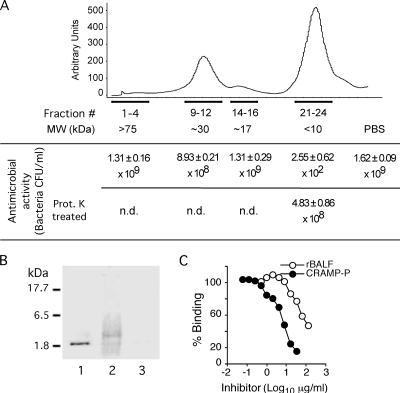
The susceptibility of Y. pestis to rBALF was evaluated to determine whether airway antimicrobial molecules affect the growth or survival of Y. pestis. Bacterial growth of Y. pestis KIM6 was significantly inhibited when bacteria were grown overnight at 37°C in the presence of rBALF (Fig. 1). The antimicrobial activity was present exclusively in the soluble fraction of rBALF. The rBALF and the soluble fraction of rBALF were bactericidal since they reduced bacterial counts of the inoculum 100- to 1,000-fold. Survanta, a commercially available surfactant extract from bovine BALF, did not affect bacterial growth. This extract is reported to lack only the hydrophilic SP-A. Therefore, assuming that the hydrophobic surfactant proteins SP-B and SP-C are effectively present in Survanta, our data indicate that these proteins do not affect Y. pestis, despite their antibacterial and/or LPS-binding properties (4, 51). To characterize the antimicrobial molecules present in rBALF, the soluble fraction was subjected to gel filtration chromatography. Only the fractions corresponding to peptides smaller than 10 kDa had an inhibitory effect on Y. pestis, reducing bacterial counts by over a millionfold (Fig. 2A). The antimicrobial components of rBALF were proteinase K sensitive, confirming that they were of a proteinaceous nature.
FIG. 1.
Bactericidal effect of rBALF on Yersinia pestis. Yersinia pestis KIM6 (1 × 106 CFU/ml) was grown overnight at 37°C in the presence of the rBALF total fraction (6.4 μg/ml protein), rBALF supernatant (small surfactant aggregates plus soluble molecules; 2.5 μg/ml protein), rBALF pellet (large surfactant aggregates; 43 μg/ml protein), or Survanta (bovine lung surfactant; diluted 1:100). Each bar represents the mean ± standard error for four independent experiments.
FIG. 2.
Presence of antimicrobial peptides in rBALF. (A) rBALF proteins separated by gel filtration chromatography (G75) and tested for antimicrobial activity against Y. pestis KIM6. Peak fractions were grouped as indicated and tested for their antimicrobial properties as described in the legend to Fig. 1, using the following protein concentrations: <1 μg/ml protein (fractions 1 to 4), 4.2 μg/ml protein (fractions 9 to 12), 2.3 μg/ml protein (fractions 14 to 16), and 3.3 μg/ml protein (fractions 21 to 24). Proteinase K treatment was done at 37°C for 4 h. n.d., not done. (B) Detection of rCRAMP in rBALF by Western blotting. Proteins were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis and detected by Western blot analysis using anti-rCRAMP antibody as indicated in Materials and Methods. Lane 1, C-terminal fragment of rCRAMP peptide (0.2 μg); lane 2, rBALF supernatant (2.5 μg); lane 3, fragment of RBD-1 peptide (0.2 μg). Molecular mass markers (in kDa) are indicated on the left. (C) Detection of rCRAMP in rBALF by ELISA. There was a concentration-dependent inhibition of anti-rCRAMP antibody binding to adsorbed rCRAMP by soluble rBALF or rCRAMP peptide.
Y. pestis is susceptible to the pulmonary CAMPs cathelicidin LL-37 and rCRAMP.
The cathelicidins and defensins are considered to be the major AMPs for host lung defense and are detectable in BALF (2, 37). A cathelicidin (LL-37 in humans and rCRAMP in rats) and β-defensin 1 (RBD-1 in rats) are both expressed constitutively in rodent lungs and human respiratory tract epithelial cells, with LL-37 being expressed specifically by pneumocytes (28, 37, 61, 67). In this study, the antimicrobial activity of the isolated small-peptide fraction of rBALF was not affected by DTT (data not shown), a treatment previously shown to disrupt the disulfide bridges of the defensins (31, 60). Moreover, the killing effect was still present when the bacteria were grown in RPMI (data not shown), a tissue culture medium containing salts at concentrations known to inhibit the antimicrobial properties of β-defensins (52). The possibility that BALF activity on Y. pestis might involve cathelicidin was consistent with previous reports indicating that the inhibitory activities of mammalian cathelicidins, including LL-37 and rCRAMP, are generally less sensitive to high salt concentrations than those of α- and β-defensins (61, 62). By investigating the activities of these CAMPs, commercially available synthetic LL-37 at a concentration of 40 μg/ml was found to efficiently kill Y. pestis KIM6 (Table 2). The same concentration of human β-defensin 1 did not demonstrate significant killing. However, a synergistic bactericidal activity was observed when both molecules were used together. Further comparative studies were undertaken with rBALF. Western blot analysis confirmed the presence of rCRAMP in rBALF (Fig. 2B). ELISA-based inhibition assays indicated that 10% and 0.5% of the rBALF proteins consisted of rCRAMP and RBD-1, respectively (Fig. 2C and data not shown). The contributions of the two antimicrobial peptides to the antimicrobial activity of rBALF toward Y. pestis were determined by removing them individually or together, using anti-RBD-1 and -rCRAMP antibodies adsorbed onto magnetic beads. Removal of RBD-1 showed no significant effect on the antimicrobial activity of rBALF (23.0% ± 1.5% decrease [mean ± standard error]; n = 3) compared to the control, using a nonspecific antibody (22.5% ± 2.4% decrease). In contrast, removal of rCRAMP alone or together with RBD-1 resulted in significant losses of antimicrobial activity (decreases of 61.0% ± 4.7% and 64.4% ± 6.5%, respectively). The fact that a significant synergistic loss of antimicrobial activity could not be detected after removing both rCRAMP and RBD-1 was not surprising, since the concentration of RBD-1 was 20 times lower than that of rCRAMP in rBALF.
TABLE 2.
Antimicrobial activities of LL-37 and β-defensin 1 against KIM6
| AMPa | KIM6 growth (CFU/ml)
|
|
|---|---|---|
| 5 h | 18 h | |
| None | 1.4 × 108 | 8.00 × 108 |
| LL-37 | 2.35 × 105 | 1.75 × 104 |
| β-defensin 1 | 9.14 × 107 | 3.25 × 108 |
| LL-37 plus β-defensin 1 | 1.30 × 104 | 2.10 × 103 |
The amount of AMP used for each condition was 40 μg/ml.
Taken together, our results strongly suggest that the cathelicidins LL-37 and rCRAMP are major antimicrobials against Y. pestis in the respiratory tract. The data also indicate the presence of other uncharacterized antimicrobial molecules. The detected synergistic activity of LL-37 with β-defensin 1 might be relevant for in vivo situations where inflammatory conditions activate the expression of certain antimicrobial peptides, including β-defensins.
F1 facilitates the activity of CAMPs against Y. pestis.
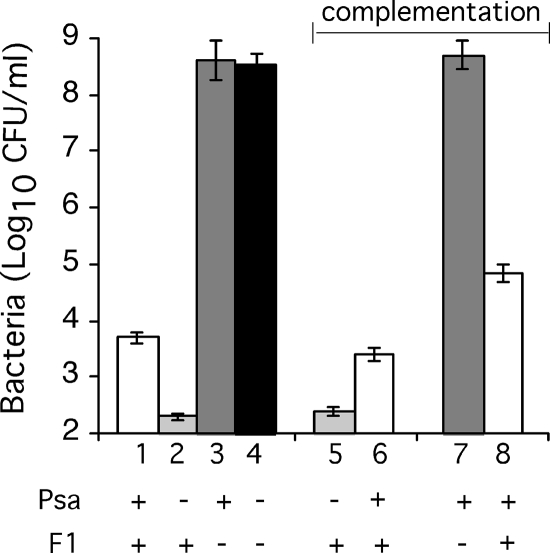
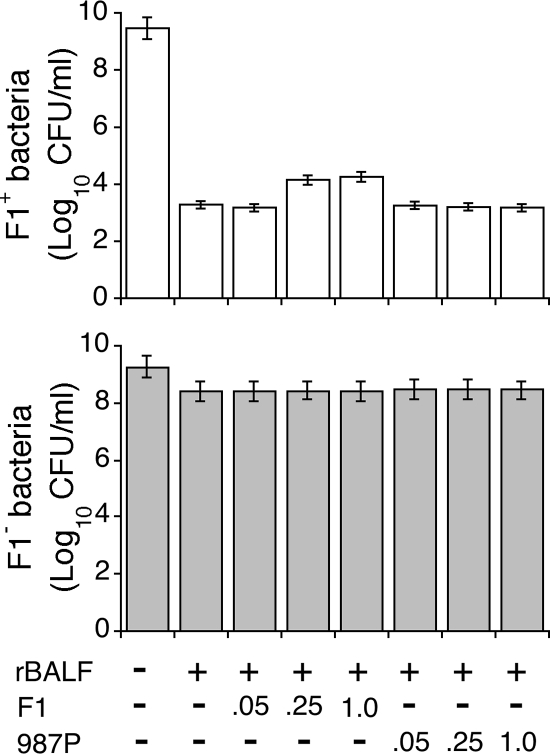
The possibility that the surface-exposed Psa or F1 protein has an effect on the growth and survival of rBALF-treated Y. pestis was analyzed by growing bacteria under conditions that allow the expression of Psa and F1 (BHI medium buffered to pH 6 at 37°C). Y. pestis expressing Psa was approximately 10 times less susceptible to the bactericidal effect of rBALF than the isogenic psa mutant strain (Fig. 3), suggesting that Psa partially protects bacteria against AMPs. trans-Complementation of the psa mutant with plasmid pCS267 resulted in Psa expression and lowered the killing effect of rBALF to wild-type levels. Surprisingly, the caf mutant and the psa caf double mutant were approximately 100,000 times more resistant to the effect of AMPs from rBALF than the isogenic strains expressing F1. Complementation of the caf mutant with the caf-containing plasmid pCS331 rendered Y. pestis again susceptible to the killing effect of rBALF (Fig. 3).
FIG. 3.
Effects of Psa and F1 expression on survival of Y. pestis exposed to BALF. The bactericidal effect of rBALF supernatant was assessed as described in the legend to Fig. 1. Wild-type Y. pestis KIM6 (bar 1) or isogenic psa (bar 2), caf (bar 3), and psa caf (bar 4) mutants were tested. For complementation studies, the psa strain was complemented with pCS267 (a plasmid expressing Psa) (bar 6) or the empty vector pBR322 (bar 5), and the caf strain was complemented with pCS331 (a plasmid expressing F1) (bar 8) or the empty vector pLG339 (bar 7). Each bar represents the mean ± standard error for three independent experiments.
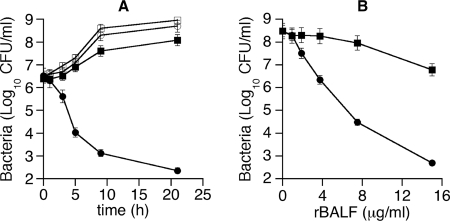
In a time course study, Y. pestis F1+ was gradually killed by rBALF over time, with the number of bacteria being reduced by about 4 to 5 log after 24 h (Fig. 4A). In contrast, Y. pestis F1− was able to multiply further in the presence of rBALF, albeit not as well as in the absence of rBALF. The addition of increasing amounts of rBALF to the bacterial culture had a significantly stronger killing effect on the F1-expressing bacteria than on the isogenic caf mutant (Fig. 4B). At the highest concentration of rBALF tested (15 μg/ml protein), the killing effect reduced the number of live Y. pestis F1+ cells by 6 log after 8 h, whereas the number of Y. pestis F1− cells had diminished by only 1.3 log by then. Comparable effects to those shown in Fig. 4 were obtained using 10-fold higher inocula (data not shown). These results showed that F1 renders Y. pestis sensitive to the action of the AMPs present in rBALF.
FIG. 4.
Time course and dose-response curves of rBALF antimicrobial activity to Y. pestis. Y. pestis KIM6 (F1+; circles) or its isogenic caf mutant (F1−; squares) was grown at 37°C in the presence (filled symbols) or absence (empty symbols) of rBALF supernatant (2.5 μg/ml), and survival was assessed at different time points (A) or the bacteria were grown in the presence of increasing concentrations of rBALF for 8 h (B). Comparable effects to those shown here (approximately 2 × 106 CFU/ml at time zero) were obtained using 10-fold higher inocula (data not shown). Each point represents the mean ± standard error for triplicate determinations for one of two reproducible experiments.
To determine whether F1 increased the susceptibility of Y. pestis by directly interacting with antimicrobial molecules, purified soluble F1 protein was added to a mixture of bacteria and rBALF. The addition of F1 protein did not modify the resistance of the Y. pestis caf mutant to the antimicrobial activity of rBALF (Fig. 5, bottom panel) and only slightly inhibited the killing of F1-expressing Y. pestis at the highest tested concentrations (Fig. 5, top panel). Similar amounts of the unrelated fimbrial protein 987P did not affect the antimicrobial activity of rBALF. These results indicated that F1 had to be expressed by the multiplying bacteria to exert its sensitizing effect with the AMPs of rBALF and that the latter molecules were not rendered potent by the presence of extraneous F1 protein.
FIG. 5.
Addition of soluble F1 does not interfere with Y. pestis susceptibility to rBALF. F1-expressing Y. pestis (top panel) or its isogenic caf mutant (bottom panel) were grown for 16 h at 37°C in the presence of rBALF supernatant (2.5 μg/ml) plus increasing concentrations of F1 or the unrelated 987P fimbriae as a control. The amount of soluble protein added is expressed as mg/ml. Each bar represents the mean ± standard error for three independent experiments.
Pla degrades CAMPs.
Since F1 needs to be expressed autogenously for its sensitizing effect with antimicrobial molecules, F1 might direct access of the antimicrobials to the site of action on Y. pestis, namely, the outer membrane. Alternatively, F1 might act indirectly by hindering access of antimicrobials to a surface-exposed inhibitor. Since the pPCP1 plasmid-encoded outer membrane protein Pla could possibly be capable of inhibiting AMPs, isogenic pla mutants of Y. pestis KIM6 and DSY9 (KIM6 caf) were constructed to evaluate the role of Pla. Both pla mutants were as susceptible as strain KIM6 to the AMPs of rBALF and to the cathelicidin LL-37 (Table 3), confirming that Pla was involved in the observed resistance of Y. pestis caf to AMPs, including LL-37. Interestingly, polymyxin B, a cyclic AMP, had the same bactericidal activity over all the strains tested, indicating that Pla exerted no inhibitory effect on this antibiotic.
TABLE 3.
MBCs of different antimicrobial compounds for KIM6 caf and/or pla mutants
| Bacterial strain | Phenotype | MBC (μg/ml)
|
||
|---|---|---|---|---|
| rBALF supernatant | LL-37 | Polymyxin B | ||
| KIM6 | F1+ Pla+ | 5.0 | 40.0 | 40.0 |
| DSY87 | F1+ Pla− | 5.0 | 40.0 | 40.0 |
| DSY9 | F1− Pla+ | 25.0 | >160.0 | 40.0 |
| DSY85 | F1− Pla− | 5.0 | 40.0 | 40.0 |
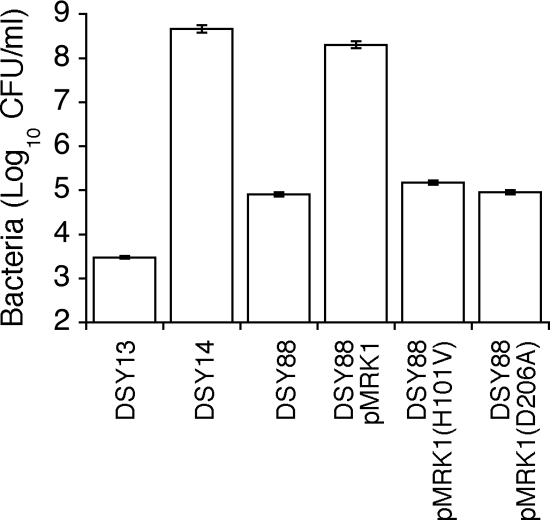
To determine whether the proteolytic activity of Pla was responsible for its inhibitory effect on rBALF and its AMPs, further studies were undertaken with Pla active-site mutants. For this purpose, the Y. pestis psa caf pla triple mutant DSY88 was transformed with a plasmid expressing the wild-type Pla protein (pMRK1) or expressing Pla proteins that had been mutated in their active sites (pMRK1H101V or pMRK1D206A). Plasmid pMRK1 caused an increased resistance of the Y. pestis psa caf pla triple mutant to rBALF, confirming that Pla could be complemented in trans for its antimicrobial inhibitory activity on the AMPs (Fig. 6). In contrast, the two plasmids carrying mutated pla genes demonstrated the same level of susceptibility to rBALF as the parental strain lacking these plasmids. This result indicated that the inhibitory effect of Pla on the AMPs of rBALF depended upon the proteolytic activity of Pla. As expected, strain DSY88 carrying pMRK1 showed similar levels of plasminogen activation to that of the Pla-expressing strain DSY14, whereas no plasminogen activation was detected with DSY88 containing pMRK1H101V or pMRK1D206A (data not shown). Bacterial viability was not affected by any of the plasmids used.
FIG. 6.
Bactericidal effect of rBALF on Y. pestis pla mutants. Bacteria (1 × 106 CFU/ml) were grown for 5 h at 37°C in the presence of rBALF supernatant (2.5 μg/ml). DSY13 is a psa mutant strain, DSY14 is a psa caf mutant, and DSY88 is a psa caf pla mutant. Plasmid pMRK1 allowed the expression of an active Pla as a protease, whereas pMRK1H101V and pMRK1D206A directed the expression of an inactive form of Pla. Each bar represents the mean ± standard error for three independent experiments.
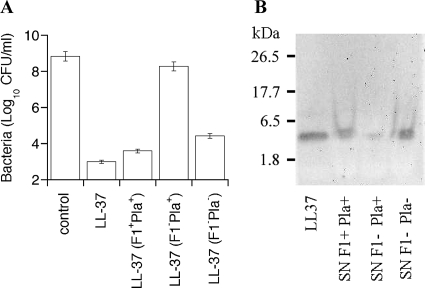
An additional experiment was undertaken to further investigate the proteolytic activity of Pla on an AMP and to determine whether F1 inhibits the activity of Pla, as predicted. For this, the cathelicidin LL-37 was exposed to strains with one of three phenotypes, namely, F1+ Pla+, F1− Pla−, or F1− Pla+. After 5 h of exposure, the bacteria were removed by centrifugation and the supernatant was inspected for its bactericidal activity on Y. pestis KIM6 (F1+ Pla+). Only LL-37 preincubated with Y. pestis F1− Pla+ lost its ability to kill Y. pestis KIM6 (Fig. 7A). Western blot analysis of the supernatant showed a significant decrease of LL-37 only after the preincubation step with Y. pestis F1− Pla+ (Fig. 7B). These data confirmed that the proteolytic activity of Pla on AMPs such as LL-37 is responsible for the increased resistance of Y. pestis strains lacking the F1 protein. The F1 protein was also shown to inhibit the degradation of LL-37 by Pla. Curiously, the activation of plasminogen by Pla was not considerably affected by the expression of F1 on the bacterial surface (data not shown), indicating that the F1-mediated inhibition of Pla activity was specific for the AMPs of rBALF and for LL-37.
FIG. 7.
Antibacterial activity and integrity of LL-37 preexposed to Y. pestis KIM6 and KIM6 mutants. Strain KIM6 (F1+ Pla+), the caf mutant (F1− Pla+), and the caf mutant without pPCP1 (F1− Pla−) were grown for 8 h at 37°C. After the bacteria were spun down, the supernatant was assayed for killing activity over strain KIM6 (A) or LL-37 was detected by Western blotting using a monoclonal anti-LL-37 antibody (B). For bacterial supernatants, the equivalent of 0.8 μg of LL-37 was applied per line; the amount of LL-37 standard was 0.25 μg. Each bar in panel A represents the mean ± standard error for three independent experiments.
DISCUSSION
Y. pestis is an agent that can survive on the epithelium of the respiratory tract or in the various skin layers after being deposited by aerosol or by a fleabite, respectively, before it initiates its invasive pathogenesis. Both environments contain antimicrobial molecules of the innate immune system. For this study, we wondered how Y. pestis resists the attack of these host factors in the respiratory tract. The effect of rBALF on the growth or survival of Y. pestis was used to evaluate the earliest type of interactions at the initiation of the infectious process. As predicted, rBALF could kill Y. pestis KIM6. The bactericidal molecules of rBALF were identified as small peptides. This result was consistent with the literature, since AMPs are ubiquitous components of the innate immune response and exhibit broad-range antimicrobial activities against gram-positive and gram-negative bacteria, fungi, parasites, and enveloped viruses (9). We further showed that our active rBALF fraction contained the cathelicidin rCRAMP and RBD-1, with the latter molecule being detected at a 20 times lower concentration than the former one. Similar to these two CAMPs, a corresponding cathelicidin and a β-defensin 1 were previously described to be expressed constitutively in human lungs. Among various mammalian cathelicidins, the human and rat peptides are most similar in terms of antimicrobial properties (62), supporting the relevance of our findings with rBALF for humans. Indeed, the bactericidal effect of rBALF on Y. pestis could be reproduced with the human cathelicidin LL-37 but not with human β-defensin 1, although the latter CAMP synergistically amplified the effect of LL-37. Thus, even though the inhibitory concentration of rBALF proteins was lower than that of LL-37 for Y. pestis, synergistic activities with other antimicrobial peptides, such as β-defensin 1, might explain our result. A literature review indicated that the inhibitory concentrations of LL-37 described here are in the expected range (19). CAMPs are produced by epithelial cells and are part of the phagocytic vacuole microbicidal mechanism. The pulmonary and alveolar microenvironment of an inhaled Y. pestis organism is expected to contain much higher concentrations of CAMPs than BALF does, and even more so when an inflammatory reaction that increases their expression is activated. These peptides have amphipathic structures that function to kill bacteria by permeabilization of their lipid bilayers. Thus, it is likely that CAMPs such as LL-37 interfere with the survival of inhaled Y. pestis cells in vivo. Whether certain Yop proteins of Y. pestis interfere with the expression of inducible CAMPs in the lungs remains to be determined.
Further studies were aimed at determining the potential modulating effect of the F1 and Psa proteins of Y. pestis. These two homopolymeric structures, which are exported by their respective chaperone-usher systems, cover the bacterial surface and might potentially serve as a protective layer against antimicrobials. Although rBALF was bactericidal for Y. pestis KIM6, it was surprising to find that this activity, which was barely inhibited by Psa, required the presence of the F1 protein on the bacterial surface. Investigations with isogenic mutants that lacked F1, Pla, or both indicated that Pla was responsible for the resistance of Y. pestis F1− to the antimicrobial molecules of rBALF. The fact that the proteolytic activity of Pla was responsible for this property was demonstrated with two pla mutants that had single amino acid substitutions known to affect only the enzymatic activity of Pla, with one of the mutations being in the active site. Moreover, adding the CAMP LL-37 to Y. pestis F1− Pla+ resulted in a decreased amount and reduced inhibitory activity of the peptide in the supernatant. These results strongly suggested that AMPs, which are effective against Y. pestis F1+, are Pla substrates in Y. pestis F1−, although an indirect effect involving intermediary factors cannot be ruled out.
The fibrinolytic activity of Y. pestis was originally linked to a plasmid, mapped, and characterized as the activity of an outer membrane protein designated Pla that cleaves plasminogen to plasmin (6, 55, 57). The Pla protease is an essential virulence factor for the invasion and dissemination of Y. pestis from the periphery. Although Pla was known to have additional substrates, such as the C3 complement factor and α2-antiplasmin (33, 57), the identification and characterization of its proteolytic inactivation of CAMPs herein are novel. Pla belongs to a family of outer membrane aspartate proteases, designated omptins, in Enterobacteriaceae (32, 64). Sequence particularities determine the differential substrate specificities of omptins. For example, the Salmonella omptin PgtE, unlike the Escherichia coli omptin OmpT, cleaves plasminogen to plasmin well, albeit 1,000 times less efficiently than Pla does (23, 32, 56). Access of plasminogen to omptins such as Pla and PgtE is inhibited by the addition and lengthening of the LPS O-chain repeats, respectively (34, 46). Y. pestis has a rough-type LPS that lacks an O-specific chain (54), resulting in efficient plasminogen activation by Pla. The inhibitory property of the LPS O chain on plasminogen cleavage by omptins can be compared to the inhibitory property of the F1 structure on the inactivation of CAMPs by the proteolytic activity of Pla, as described in this study. Surprisingly, the presence of F1 did not interfere with the activity of Pla on plasminogen, indicating substrate-specific interference of F1 on Pla. This specificity could not be due to different active sites on Pla, since a substitution mutation inactivating the enzymatic site of Pla for plasminogen cleavage also affected the inactivation of LL-37 or CRAMP. OmpT and PgtE cleave preferentially between two basic amino acid residues (14, 17), explaining why CAMPs such as cathelicidins, with their repeated pairs of Arg and/or Lys residues, are optimal targets for these omptins (24, 59). The efficiency (kcat/Km) of OmpT for a peptide with an Arg↓Arg cleavage site was fourfold better than that for a similar peptide with an Arg↓Val cleavage site (42, 65). Our results identifying the proteolytic activity of Pla on AMPs suggest that in addition to the previously described plasminogen cleavage site (… Gly-Arg↓Val-Val…), Pla probably cleaves cathelicidins between two basic residues. A recent study showed that small peptides are cleaved by hydrolysis between two positive residues (1). The tripeptide RK(I/G/S) was a particularly efficient substrate for Pla, supporting our results regarding cathelicidin degradation by Pla, since both LL-37 and rCRAMP contain such a tripeptide sequence twice. The F1 surface protein, thanks to its low isoelectric point (4.35), might sterically interfere with Pla access to the cleavage sites of cathelicidins by interacting with their positively charged residues. Alternatively, F1 might alter the substrate specificity of Pla. The fact that Pla specifically cleaves at sites found in tandem in cathelicidins and inactivates both the inhibitory activity of cathelicidins and rBALF AMPs further indicates that the rat cathelicidin rCRAMP is a major rBALF AMP acting against Y. pestis.
Previous studies had reported that Y. pestis was resistant to linear CAMPs, such as cecropin P1 and mastoparan (43). The results of these studies, which were done at 21°C to 28°C, were later found to be temperature dependent, with resistance to CAMPs being significantly lower at 37°C (48). This temperature-dependent decrease of resistance to CAMPs was originally attributed to a modified LPS, consisting predominantly of molecules with increased levels of tetra-acylated lipid A lacking C12 and C16:1 acyl groups. Surprisingly, later studies showed that mutants that lacked the corresponding acyltransferase genes (msbB and lpxP, respectively) did not significantly affect the susceptibility to cecropin A (49), suggesting that another temperature-dependent modification of LPS or another factor was responsible for the observed temperature effect. Our results identified two other factors involved, namely, Pla and F1. At a lower temperature, when the F1 protein is not (or very poorly) expressed, Pla is still present and proteolytically active on a linear CAMP such as LL-37, explaining the resistance toward similar linear CAMPs. In contrast, at 37°C, F1 is expressed and inhibits Pla, rendering Y. pestis more susceptible toward LL-37. Interestingly, Pla did not affect polymyxin B susceptibility at the lower temperature. It was suggested that Pla cannot cleave polymyxin B because of the cyclic structure of this antibiotic, the nature of the basic residues, which are five α,γ-diaminobutyric acid residues out of a total of 10 amino acids, and/or the presence of an attached fatty acid. This is consistent with the reported polymyxin B resistance of Y. pestis, which was previously found to result from the addition of 4-aminoarabinose to the lipid A of Y. pestis LPS at growth temperatures near 25°C or from the activation of the PhoPQ and PmrAB two-component regulatory systems (48, 69).
CAMP inhibition by Pla at temperatures near 25°C might be important in the flea gut environment, which most likely includes CAMPs, as described for a variety of insects (8, 11). Interestingly, the blood used to feed and infect fleas under laboratory conditions must contain high concentrations of Y. pestis (∼5 × 108 CFU/ml) to achieve infection of a majority of fleas (25). Since the blood meal of a flea averages ∼0.5 μl per meal, probably every 4 to 5 days (12), a flea meal needs to contain ∼2.5 × 105 bacteria to ensure 100% infection. This indicates that Y. pestis cells that are ingurgitated from bacteremic mammals cannot survive or multiply successfully in the flea digestive tract if they do not amount to the tens if not hundreds of thousands. Considering that the intravenous or subcutaneous 50% lethal dose is <10 for mice (63), one has to assume that Y. pestis coming from mammalian blood (37°C) is not ready for the novel environment of the flea digestive tract (ambient temperature). We suggest that in the early stage of Y. pestis infection of fleas, the F1 protein is still present, rendering bacteria susceptible to CAMPs of the flea gut (10, 26). Stochastic variability in gene expression might favor the presence of a few cells that express less or no F1 in a large population of Y. pestis cells grown at 37°C (29). Thus, the ingestion of a great number of bacteria by fleas would permit the few cells that express little F1 to survive and replicate successfully, thanks to Pla. At a later stage, survival in the flea gut and blockage of the proventriculus require the hms genes, which are expressed at ambient temperature and involved in biofilm formation (26). At this stage of flea infestation, Pla would become superfluous, consistent with previous findings showing that Pla was dispensable for Xenopsylla cheopis flea blockage after fleas were fed with blood containing 5 × 108 Y. pestis cells per ml (25).
Although Y. pestis grown at 37°C in vitro expresses F1 and is sensitive to CAMPs, this bacterium is known to multiply well extracellularly in mammals, despite expressing F1. This suggests that CAMPs are not present in sufficient amounts to kill the bacteria or that these peptides are inactivated extracellularly. The former possibility is unlikely, since Y. pestis multiplies efficiently to high numbers in mammalian lungs during pneumonic plague, despite the influx of large numbers of polymorphonuclear cells and the concomitant expression and probable release of CAMPs by these cells. An alternative explanation for the in vivo resistance of Y. pestis to CAMPs might be the activation of novel bacterial resistance genes (5, 41). Oligopeptide transporters have been shown to be involved in bacterial resistance to CAMPs in Enterobacteriaceae and other gram-negative bacteria (39, 44). It is thought that these transporters “inactivate” the membrane-active CAMPs by directing them to the bacterial cytoplasm, where they are inactivated by proteases. Whether such transporters play a role in Y. pestis resistance to CAMPs remains to be studied.
Acknowledgments
We thank Jon Goguen for Y. pestis strains, Timo Korhonen and Don Court for plasmids, Sandra Bates for the gifts of rBALF and Survanta, Hani Boshra and Oriol Sunyer for high-performance liquid chromatography, and Len Bello and Ron Harty for reading the manuscript.
This work was supported by NIH grant 1R21 AI053343-01A1, a University of Pennsylvania Research Foundation grant, and research initiative funds from the University of Pennsylvania Veterinary Center for Infectious Disease.
Editor: J. B. Bliska
Footnotes
Published ahead of print on 28 January 2008.
REFERENCES
- 1.Agarkov, A., S. Chauhan, P. J. Lory, S. R. Gilbertson, and V. L. Motin. 2008. Substrate specificity and screening of the integral membrane protease Pla. Bioorg. Med. Chem. Lett. 18427-431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agerberth, B., J. Grunewald, E. Castanos-Velez, B. Olsson, H. Jornvall, H. Wigzell, A. Eklund, and G. H. Gudmundsson. 1999. Antibacterial components in bronchoalveolar lavage fluid from healthy individuals and sarcoidosis patients. Am. J. Respir. Crit. Care Med. 160283-290. [DOI] [PubMed] [Google Scholar]
- 3.Auerbuch, V., and R. R. Isberg. 2007. Growth of Yersinia pseudotuberculosis in mice occurs independently of Toll-like receptor 2 expression and induction of interleukin-10. Infect. Immun. 753561-3570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Augusto, L. A., J. Li, M. Synguelakis, J. Johansson, and R. Chaby. 2002. Structural basis for interactions between lung surfactant protein C and bacterial lipopolysaccharide. J. Biol. Chem. 27723484-23492. [DOI] [PubMed] [Google Scholar]
- 5.Bader, M. W., S. Sanowar, M. E. Daley, A. R. Schneider, U. Cho, W. Xu, R. E. Klevit, H. Le Moual, and S. I. Miller. 2005. Recognition of antimicrobial peptides by a bacterial sensor kinase. Cell 122461-472. [DOI] [PubMed] [Google Scholar]
- 6.Beesley, E. D., R. R. Brubaker, W. A. Janssen, and M. J. Surgalla. 1967. Pesticins. 3. Expression of coagulase and mechanism of fibrinolysis. J. Bacteriol. 9419-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bolivar, F., R. L. Rodriguez, P. J. Greene, M. C. Betlach, H. L. Heyneker, and H. W. Boyer. 1977. Construction and characterization of new cloning vehicles. II. A multipurpose cloning system. Gene 295-113. [PubMed] [Google Scholar]
- 8.Boulanger, N., R. J. Munks, J. V. Hamilton, F. Vovelle, R. Brun, M. J. Lehane, and P. Bulet. 2002. Epithelial innate immunity. A novel antimicrobial peptide with antiparasitic activity in the blood-sucking insect Stomoxys calcitrans. J. Biol. Chem. 27749921-49926. [DOI] [PubMed] [Google Scholar]
- 9.Bowdish, D. M., D. J. Davidson, and R. E. Hancock. 2006. Immunomodulatory properties of defensins and cathelicidins. Curr. Top. Microbiol. Immunol. 30627-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brey, P. T., W. J. Lee, M. Yamakawa, Y. Koizumi, S. Perrot, M. Francois, and M. Ashida. 1993. Role of the integument in insect immunity: epicuticular abrasion and induction of cecropin synthesis in cuticular epithelial cells. Proc. Natl. Acad. Sci. USA 906275-6279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bulet, P., and R. Stocklin. 2005. Insect antimicrobial peptides: structures, properties and gene regulation. Protein Pept. Lett. 123-11. [DOI] [PubMed] [Google Scholar]
- 12.Busvine, J. R. 1976. The harmful effects of parasites, p. 62. In Insects, hygiene and history. Athlone Press, London, United Kingdom.
- 13.Cathelyn, J. S., S. D. Crosby, W. W. Lathem, W. E. Goldman, and V. L. Miller. 2006. RovA, a global regulator of Yersinia pestis, specifically required for bubonic plague. Proc. Natl. Acad. Sci. USA 10313514-13519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen, H., and D. M. Schifferli. 2003. Construction, characterization and immunogenicity of an attenuated Salmonella enterica serovar Typhimurium pgtE vaccine expressing fimbriae with integrated viral epitopes from the spiC promoter. Infect. Immun. 714664-4673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Datsenko, K. A., and B. L. Wanner. 2000. One-step inactivation of chromosomal genes in Escherichia coli K-12 using PCR products. Proc. Natl. Acad. Sci. USA 976640-6645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Datta, S., N. Costantino, and D. L. Court. 2006. A set of recombineering plasmids for gram-negative bacteria. Gene 379109-115. [DOI] [PubMed] [Google Scholar]
- 17.Dekker, N., R. C. Cox, R. A. Kramer, and M. R. Egmond. 2001. Substrate specificity of the integral membrane protease OmpT determined by spatially addressed peptide libraries. Biochemistry 401694-1701. [DOI] [PubMed] [Google Scholar]
- 18.Du, Y., R. Rosqvist, and A. Forsberg. 2002. Role of fraction 1 antigen of Yersinia pestis in inhibition of phagocytosis. Infect. Immun. 701453-1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Durr, U. H., U. S. Sudheendra, and A. Ramamoorthy. 2006. LL-37, the only human member of the cathelicidin family of antimicrobial peptides. Biochim. Biophys. Acta 17581408-1425. [DOI] [PubMed] [Google Scholar]
- 20.Edwards, R. A., L. H. Keller, and D. M. Schifferli. 1998. Improved allelic exchange vectors and their use to analyze 987P fimbria gene expression. Gene 207149-157. [DOI] [PubMed] [Google Scholar]
- 21.Galván, E. M., H. Chen, and D. M. Schifferli. 2007. The Psa fimbriae of Yersinia pestis interact with phosphatidylcholine on alveolar epithelial cells and pulmonary surfactant. Infect. Immun. 751272-1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goguen, J. D., J. Yother, and S. C. Straley. 1984. Genetic analysis of the low-calcium response in Yersinia pestis mu d1(Ap lac) insertion mutants. J. Bacteriol. 160842-848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grodberg, J., and J. J. Dunn. 1989. Comparison of Escherichia coli K-12 outer membrane protease OmpT and Salmonella typhimurium E protein. J. Bacteriol. 1712903-2905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guina, T., E. C. Yi, H. Wang, M. Hackett, and S. I. Miller. 2000. A PhoP-regulated outer membrane protease of Salmonella enterica serovar Typhimurium promotes resistance to alpha-helical antimicrobial peptides. J. Bacteriol. 1824077-4086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hinnebusch, B. J., E. R. Fischer, and T. G. Schwan. 1998. Evaluation of the role of the Yersinia pestis plasminogen activator and other plasmid-encoded factors in temperature-dependent blockage of the flea. J. Infect. Dis. 1781406-1415. [DOI] [PubMed] [Google Scholar]
- 26.Hinnebusch, B. J., R. D. Perry, and T. G. Schwan. 1996. Role of the Yersinia pestis hemin storage (hms) locus in the transmission of plague by fleas. Science 273367-370. [DOI] [PubMed] [Google Scholar]
- 27.Huang, X. Z., and L. E. Lindler. 2004. The pH 6 antigen is an antiphagocytic factor produced by Yersinia pestis independent of Yersinia outer proteins and capsule antigen. Infect. Immun. 727212-7219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jia, H. P., J. N. Mills, F. Barahmand-Pour, D. Nishimura, R. K. Mallampali, G. Wang, K. Wiles, B. F. Tack, C. L. Bevins, and P. B. McCray, Jr. 1999. Molecular cloning and characterization of rat genes encoding homologues of human beta-defensins. Infect. Immun. 674827-4833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kaern, M., T. C. Elston, W. J. Blake, and J. J. Collins. 2005. Stochasticity in gene expression: from theories to phenotypes. Nat. Rev. Genet. 6451-464. [DOI] [PubMed] [Google Scholar]
- 30.Khan, A. S., and D. M. Schifferli. 1994. A minor 987P protein different from the structural fimbrial subunit is the adhesin. Infect. Immun. 624233-4243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim, C., N. Gajendran, H. W. Mittrucker, M. Weiwad, Y. H. Song, R. Hurwitz, M. Wilmanns, G. Fischer, and S. H. Kaufmann. 2005. Human alpha-defensins neutralize anthrax lethal toxin and protect against its fatal consequences. Proc. Natl. Acad. Sci. USA 1024830-4835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kukkonen, M., and T. K. Korhonen. 2004. The omptin family of enterobacterial surface proteases/adhesins: from housekeeping in Escherichia coli to systemic spread of Yersinia pestis. Int. J. Med. Microbiol. 2947-14. [DOI] [PubMed] [Google Scholar]
- 33.Kukkonen, M., K. Lahteenmaki, M. Suomalainen, N. Kalkkinen, L. Emody, H. Lang, and T. K. Korhonen. 2001. Protein regions important for plasminogen activation and inactivation of alpha2-antiplasmin in the surface protease Pla of Yersinia pestis. Mol. Microbiol. 401097-1111. [DOI] [PubMed] [Google Scholar]
- 34.Kukkonen, M., M. Suomalainen, P. Kyllonen, K. Lahteenmaki, H. Lang, R. Virkola, I. M. Helander, O. Holst, and T. K. Korhonen. 2004. Lack of O-antigen is essential for plasminogen activation by Yersinia pestis and Salmonella enterica. Mol. Microbiol. 51215-225. [DOI] [PubMed] [Google Scholar]
- 35.Lahteenmaki, K., R. Virkola, A. Saren, L. Emody, and T. K. Korhonen. 1998. Expression of plasminogen activator Pla of Yersinia pestis enhances bacterial attachment to the mammalian extracellular matrix. Infect. Immun. 665755-5762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lathem, W. W., P. A. Price, V. L. Miller, and W. E. Goldman. 2007. A plasminogen-activating protease specifically controls the development of primary pneumonic plague. Science 315509-513. [DOI] [PubMed] [Google Scholar]
- 37.Laube, D. M., S. Yim, L. K. Ryan, K. O. Kisich, and G. Diamond. 2006. Antimicrobial peptides in the airway. Curr. Top. Microbiol. Immunol. 306153-182. [DOI] [PubMed] [Google Scholar]
- 38.Liu, F., H. Chen, E. M. Galván, M. A. Lasaro, and D. M. Schifferli. 2006. The effects of Psa and F1 on the adhesive and invasive interactions of Yersinia pestis with human respiratory tract epithelial cells. Infect. Immun. 745636-5644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mason, K. M., M. E. Bruggeman, R. S. Munson, and L. O. Bakaletz. 2006. The non-typeable Haemophilus influenzae Sap transporter provides a mechanism of antimicrobial peptide resistance and SapD-dependent potassium acquisition. Mol. Microbiol. 621357-1372. [DOI] [PubMed] [Google Scholar]
- 40.Montminy, S. W., N. Khan, S. McGrath, M. J. Walkowicz, F. Sharp, J. E. Conlon, K. Fukase, S. Kusumoto, C. Sweet, K. Miyake, S. Akira, R. J. Cotter, J. D. Goguen, and E. Lien. 2006. Virulence factors of Yersinia pestis are overcome by a strong lipopolysaccharide response. Nat. Immunol. 71066-1073. [DOI] [PubMed] [Google Scholar]
- 41.Navarre, W. W., T. A. Halsey, D. Walthers, J. Frye, M. McClelland, J. L. Potter, L. J. Kenney, J. S. Gunn, F. C. Fang, and S. J. Libby. 2005. Co-regulation of Salmonella enterica genes required for virulence and resistance to antimicrobial peptides by SlyA and PhoP/PhoQ. Mol. Microbiol. 56492-508. [DOI] [PubMed] [Google Scholar]
- 42.Olsen, M. J., D. Stephens, D. Griffiths, P. Daugherty, G. Georgiou, and B. L. Iverson. 2000. Function-based isolation of novel enzymes from a large library. Nat. Biotechnol. 181071-1074. [DOI] [PubMed] [Google Scholar]
- 43.Oyston, P. C., J. L. Prior, S. Kiljunen, M. Skurnik, J. Hill, and R. W. Titball. 2003. Expression of heterologous O-antigen in Yersinia pestis KIM does not affect virulence by the intravenous route. J. Med. Microbiol. 52289-294. [DOI] [PubMed] [Google Scholar]
- 44.Parra-Lopez, C., M. T. Baer, and E. A. Groisman. 1993. Molecular genetic analysis of a locus required for resistance to antimicrobial peptides in Salmonella typhimurium. EMBO J. 124053-4062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Perry, R. D., and J. D. Fetherston. 1997. Yersinia pestis—etiologic agent of plague. Clin. Microbiol. Rev. 1035-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pouillot, F., A. Derbise, M. Kukkonen, J. Foulon, T. K. Korhonen, and E. Carniel. 2005. Evaluation of O-antigen inactivation on Pla activity and virulence of Yersinia pseudotuberculosis harbouring the pPla plasmid. Microbiology 1513759-3768. [DOI] [PubMed] [Google Scholar]
- 47.Pouliot, K., N. Pan, S. Wang, S. Lu, E. Lien, and J. D. Goguen. 2007. Evaluation of the role of LcrV-Toll-like receptor 2-mediated immunomodulation in the virulence of Yersinia pestis. Infect. Immun. 753571-3580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rebeil, R., R. K. Ernst, B. B. Gowen, S. I. Miller, and B. J. Hinnebusch. 2004. Variation in lipid A structure in the pathogenic yersiniae. Mol. Microbiol. 521363-1373. [DOI] [PubMed] [Google Scholar]
- 49.Rebeil, R., R. K. Ernst, C. O. Jarrett, K. N. Adams, S. I. Miller, and B. J. Hinnebusch. 2006. Characterization of late acyltransferase genes of Yersinia pestis and their role in temperature-dependent lipid A variation. J. Bacteriol. 1881381-1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Reithmeier-Rost, D., J. Hill, S. J. Elvin, D. Williamson, S. Dittmann, A. Schmid, G. Wilharm, and A. Sing. 2007. The weak interaction of LcrV and TLR2 does not contribute to the virulence of Yersinia pestis. Microbes Infect. 9997-1002. [DOI] [PubMed] [Google Scholar]
- 51.Ryan, M. A., H. T. Akinbi, A. G. Serrano, J. Perez-Gil, H. Wu, F. X. McCormack, and T. E. Weaver. 2006. Antimicrobial activity of native and synthetic surfactant protein B peptides. J. Immunol. 176416-425. [DOI] [PubMed] [Google Scholar]
- 52.Schutte, B. C., and P. B. McCray, Jr. 2002. β-Defensins in lung host defense. Annu. Rev. Physiol. 64709-748. [DOI] [PubMed] [Google Scholar]
- 53.Sebbane, F., C. O. Jarrett, D. Gardner, D. Long, and B. J. Hinnebusch. 2006. Role of the Yersinia pestis plasminogen activator in the incidence of distinct septicemic and bubonic forms of flea-borne plague. Proc. Natl. Acad. Sci. USA 1035526-5530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Skurnik, M., and J. A. Bengoechea. 2003. The biosynthesis and biological role of lipopolysaccharide O-antigens of pathogenic yersiniae. Carbohydr. Res. 3382521-2529. [DOI] [PubMed] [Google Scholar]
- 55.Sodeinde, O. A., and J. D. Goguen. 1988. Genetic analysis of the 9.5-kilobase virulence plasmid of Yersinia pestis. Infect. Immun. 562743-2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sodeinde, O. A., and J. D. Goguen. 1989. Nucleotide sequence of the plasminogen activator gene of Yersinia pestis: relationship to ompT of Escherichia coli and gene E of Salmonella typhimurium. Infect. Immun. 571517-1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sodeinde, O. A., Y. V. Subrahmanyam, K. Stark, T. Quan, Y. Bao, and J. D. Goguen. 1992. A surface protease and the invasive character of plague. Science 2581004-1007. [DOI] [PubMed] [Google Scholar]
- 58.Stoker, N. G., N. F. Fairweather, and B. G. Spratt. 1982. Versatile low-copy-number plasmid vectors for cloning in Escherichia coli. Gene 18335-341. [DOI] [PubMed] [Google Scholar]
- 59.Stumpe, S., R. Schmid, D. L. Stephens, G. Georgiou, and E. P. Bakker. 1998. Identification of OmpT as the protease that hydrolyzes the antimicrobial peptide protamine before it enters growing cells of Escherichia coli. J. Bacteriol. 1804002-4006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Taylor, K., B. McCullough, D. J. Clarke, R. J. Langley, T. Pechenick, A. Hill, D. J. Campopiano, P. E. Barran, J. R. Dorin, and J. R. Govan. 2007. Covalent dimer species of beta-defensin Defr1 display potent antimicrobial activity against multidrug-resistant bacterial pathogens. Antimicrob. Agents Chemother. 511719-1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Termen, S., M. Tollin, B. Olsson, T. Svenberg, B. Agerberth, and G. H. Gudmundsson. 2003. Phylogeny, processing and expression of the rat cathelicidin rCRAMP: a model for innate antimicrobial peptides. Cell. Mol. Life Sci. 60536-549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Travis, S. M., N. N. Anderson, W. R. Forsyth, C. Espiritu, B. D. Conway, E. P. Greenberg, P. B. McCray, Jr., R. I. Lehrer, M. J. Welsh, and B. F. Tack. 2000. Bactericidal activity of mammalian cathelicidin-derived peptides. Infect. Immun. 682748-2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Une, T., and R. R. Brubaker. 1984. In vivo comparison of avirulent Vwa− and Pgm− or Pstr phenotypes of yersiniae. Infect. Immun. 43895-900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vandeputte-Rutten, L., R. A. Kramer, J. Kroon, N. Dekker, M. R. Egmond, and P. Gros. 2001. Crystal structure of the outer membrane protease OmpT from Escherichia coli suggests a novel catalytic site. EMBO J. 205033-5039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Varadarajan, N., J. Gam, M. J. Olsen, G. Georgiou, and B. L. Iverson. 2005. Engineering of protease variants exhibiting high catalytic activity and exquisite substrate selectivity. Proc. Natl. Acad. Sci. USA 1026855-6860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Viboud, G. I., and J. B. Bliska. 2005. Yersinia outer proteins: role in modulation of host cell signalling responses and pathogenesis. Annu. Rev. Microbiol. 5969-89. [DOI] [PubMed] [Google Scholar]
- 67.Wah, J., A. Wellek, M. Frankenberger, P. Unterberger, U. Welsch, and R. Bals. 2006. Antimicrobial peptides are present in immune and host defense cells of the human respiratory and gastrointestinal tracts. Cell Tissue Res. 324449-456. [DOI] [PubMed] [Google Scholar]
- 68.Welkos, S. L., A. M. Friedlander, and K. J. Davis. 1997. Studies on the role of plasminogen activator in systemic infection by virulent Yersinia pestis strain C092. Microb. Pathog. 23211-223. [DOI] [PubMed] [Google Scholar]
- 69.Winfield, M. D., T. Latifi, and E. A. Groisman. 2005. Transcriptional regulation of the 4-amino-4-deoxy-l-arabinose biosynthetic genes in Yersinia pestis. J. Biol. Chem. 28014765-14772. [DOI] [PubMed] [Google Scholar]
- 70.Wright, J. R. 2005. Immunoregulatory functions of surfactant proteins. Nat. Rev. Immunol. 558-68. [DOI] [PubMed] [Google Scholar]