Abstract
OBJECTIVE
To provide family physicians with an approach to the diagnosis and management of nonarthritic hip pain in young adults, which might occur as a result of femoroacetabular impingement syndrome.
SOURCES OF INFORMATION
A MEDLINE search from 1950 to April 2007 was carried out using the MeSH terms femoroacetabular, impingement, hip, and syndrome. The existing literature consists of level II studies. To date, randomized controlled trials have not been carried out.
MAIN MESSAGE
Nonarthritic hip pain in the active adult population has long been a difficult clinical problem to manage. Arthroplasty is rarely an appropriate option and the usual conservative therapies for musculoskeletal problems are frequently ineffective. Recently, abnormal impingement between the acetabulum and femoral head-neck junction, or femoroacetabular impingement syndrome, has been recognized as a relatively common and possibly prearthritic cause of these symptoms. Family physicians can identify these patients by recognizing the clinical history and through specific examination findings. Emerging evidence suggests that early surgical intervention improves function and perhaps prevents or delays the onset of degenerative changes in the hip joint.
CONCLUSION
Family physicians can identify patients with possible femoroacetabular impingement syndrome and play an important role in the appropriate management of these cases.
RÉSUMÉ
OBJECTIF
Présenter au médecin de famille une méthode de diagnostic et de traitement de la douleur de hanche non arthritique chez le jeune adulte pouvant résulter du syndrome du conflit fémoro-acétabulaire.
SOURCE DE L’INFORMATION
On a effectué une recherche dans MEDLINE entre 1950 et avril 2007 à l’aide des rubriques MeSH femoacetabular , inpingement , hip et syndrome . La littérature existante consiste en études de niveau II. Jusqu’à présent, aucun essai randomisé avec témoins n’a été effectuée.
PRINCIPAL MESSAGE
La douleur de hanche non arthritique chez l’adulte actif a longtemps été un problème clinique difficile. Il est rare que l’arthroplastie soit un choix approprié, et les thérapies conservatrices habituelles pour les problèmes musculosquelettiques sont souvent inefficaces. On s’est récemment aperçu qu’un conflit entre l’acétabulum et la jonction tête-col fémoral, ou syndrome du conflit fémoro-acétabulaire, pouvait être une cause relativement fréquente et possiblement préarthritique de ces symptômes. Le médecin de famille peut identifier ces patients à l’aide de l’histoire clinique et de certains examens spécifiques. Certaines données récentes suggèrent qu’une intervention chirurgicale précoce pourrait améliorer la fonction et prévenir ou retarder le début des changements dégénératifs de l’articulation de la hanche.
CONCLUSION
Le médecin de famille peut identifier les cas de conflit fémoro-acétabulaire et jouer un rôle important dans le traitement approprié de ce problème.
Case description
H.P. is a 38-year-old account manager who visits your office complaining of right hip pain. He is an otherwise healthy individual with no history of musculoskeletal problems. He describes his pain as primarily dull and achy and localized to his groin. The pain is present most days and is much worse after intense activity, especially after ice hockey, which he plays twice a week. Recently, he has had to stop playing, which has made him quite concerned. He states that the pain began about 3 years ago with no specific inciting event. Since then it has progressed slowly and now is interfering with his life, as he has difficulty tying his shoes, ascending stairs, and sitting for prolonged periods. He has seen a physiotherapist and a chiropractor, both of whom felt the pain was due to a groin pull. Prescribed exercises were of no help and actually made the pain worse. Two months ago, he was seen by a colleague of yours who ordered an x-ray investigation and prescribed anti-inflammatory medication. The x-ray results were reported as normal and the medication has provided little relief. H.P. asks what the problem could be and if there is anything that can help resolve his symptoms and allow him to play ice hockey again.
Femoroacetabular impingement syndrome
Femoroacetabular impingement (FAI) or hip impingement syndrome refers to the constellation of signs and symptoms brought about by abnormal contact between the acetabulum and femoral head-neck junction. This contact or impingement might occur within the normal physiologic range of motion as a result of subtle osseous abnormalities of the acetabulum or femur where the femoral neck transitions to the head. Alternatively, the impingement can occur in an otherwise morphologically normal hip as a result of extreme range of motion activities. This impingement can result in substantial pain and discomfort and frequently limits function in healthy and active patients.
Equally important, recurrent impingement can result in injury to the acetabular labrum and adjacent cartilage. 1 – 4 Recent investigation has indicated that this abnormal impingement might lead to early degenerative changes in the hip joint and might, in fact, be the underlying etiology in most osteoarthritis cases previously identified as idiopathic. 1 , 5 – 9 Before the recent recognition of this clinical entity, young adult patients with radiographically normal yet symptomatic hips were managed expectantly. This frequently resulted in substantial functional limitations, persistent pain, and perhaps early joint degeneration. Fortunately, family physicians now have the opportunity to be actively involved in the diagnosis and appropriate management of these patients.
Sources of information
A MEDLINE search from 1950 to April 2007 was carried out using the MeSH terms femoroacetabular, impingement, hip, and syndrome. The search was restricted to studies published in the English language and limited to those with human subjects. Studies identified consisted primarily of level II evidence.
Main message
Recognition of FAI syndrome as a cause of nonarthritic hip pain and, perhaps, as a precursor to osteoarthritis is a fairly recent development. 1 , 5 – 9 A number of arthroscopic and open surgical techniques have been developed that appear promising in terms of symptom relief and functional improvement. 5 , 10 – 15 There is also some indication that early intervention might prevent or at least delay progression of degenerative changes leading to hip arthroplasty. 5 , 13 It is important to note, however, that the duration of follow-up in these studies is limited and that the natural history of the impinging hip has not yet been clearly defined. Randomized controlled trials with appropriate long-term follow-up could help to clarify many of the existing controversies, but to date have not been done.
A number of pre-existing hip abnormalities have been identified that might contribute to impingement, including acetabular retroversion, previous femoral neck fracture, slipped capital femoral epiphysis, and Legg-Calvé-Perthes disease. 2 – 7 , 10 Frequently, however, signs and symptoms of FAI syndrome are accompanied by a radiographic report of a normal hip. This might be because the evolution of the understanding of this condition is relatively recent or because of the subtlety of the radiographic findings. As a result, patients might be misdiagnosed and managed as having such conditions as groin strain, early osteoarthritis, low back disorder, or inguinal hernia. Such patients often continue to seek help from other health care providers, leading to a delay in diagnosis that not only affects quality of life but might also contribute to degeneration of the hip joint.
Fortunately, the constellation of demographic features, presenting symptoms, and clinical signs of hip impingement syndrome are fairly consistent and should allow family physicians to identify those who could benefit from appropriate referral and management.
Patients with FAI syndrome are typically healthy, active adults, frequently between the ages of 25 and 50. Many are involved in athletic activities that have been affected by their symptoms. Activities often involve extreme ranges of motion, such as ice hockey, martial arts, and some track and field events that require frequent deep hip flexion or pivoting maneuvers. Typically, such activities cause an increase in intensity or duration of symptoms.
Assessment
There are many common causes of hip pain that must be excluded before a diagnosis of FAI syndrome is considered ( Table 1 ). A careful history and physical examination can usually be relied upon to differentiate these causes.
Table 1 .
Common causes of adult hip pain
| CONDITION | COMMON COMPLAINTS AND CLINICAL FEATURES | PHYSICAL FIND INGS |
|---|---|---|
| Groin strain | Sudden onset groin pain, often following a specific event that can be recalled | Groin pain on active or passive abduction or extension |
| Osteoarthritis | Insidious onset of groin pain (less commonly buttock pain); worse with activity; occasionally, pain at night | More common in advanced stages; decreased range of motion (especially internal rotation); antalgic or gluteus medius gait; leg length discrepancy |
| Trochanteric bursitis | Lateral hip pain; worse with activity; difficulty lying on affected side | Tenderness on palpation of greater trochanter; lateral pain with resisted adduction |
The first step in the assessment involves a comprehensive pain history. Hip impingement pain is typically experienced anteriorly in the groin, but patients might also complain of associated lateral and posterior discomfort. Affected individuals might indicate the location of pain by gripping the lateral hip, just above the greater trochanter, between the abducted thumb and index finger. This is known as the C sign ( Figure 1 ). Pain is often described as dull or aching in nature and might become worse after prolonged periods of sitting. Occasionally, an exacerbation of sharp and catching pain with activity is reported. Duration of symptoms is variable, and patients might report an inciting event, although this is not always the case, as the onset is often insidious. Many times, a course of physiotherapy might have been completed. Owing to the mechanical nature of the impingement syndrome, however, this approach is usually ineffective, and inactivity might be the only effective way to relieve pain. Of course, any lumbosacral symptoms require close scrutiny, as do systemic conditions or medications having musculoskeletal manifestations.
Figure 1 . The C sign .
The patient indicates location of pain by gripping the affected hip, just above the greater trochanter, between the abducted thumb and index finger.
Physical examination is very important in the assessment, as certain components, such as the impingement test, have been shown to be highly sensitive. Gait pattern is first observed for the presence of antalgic or gluteus medius gait. This involves the patient swaying the torso laterally over the affected hip in the stance phase as a result of abductor weakness or as an attempt to decrease the forces across the joint during the gait. Next, examine range of motion with the patient supine, comparing with the contralateral hip. Typically, internal rotation with the hip at 90° of flexion is markedly limited relative to the other side. Flexion and abduction are also frequently limited, though this is less consistent and might occur later in the development of the syndrome. Perhaps the most important finding indicating hip impingement is a positive impingement test, or the impingement sign, which has been shown to be present in more than 90% of patients who later have the diagnosis of FAI syndrome confirmed either radiographically or at the time of surgery. 4 , 10 , 11 The test involves having the patient supine on the examination table. The affected hip and knee are flexed to 90°. The hip is then adducted and internally rotated in this flexed position ( Figure 2 ). A positive test involves a sudden, often sharp, pain in the hip. Patients will often report that the maneuver recreates their typical symptoms.
Figure 2 . The impingement test .
With patient supine, the hip and knee of the affected limb are flexed to 90°. The leg is then adducted and internally rotated in this position. Occurrence of sudden exacerbation of pain, typically in the groin, is considered a positive test.
Imaging
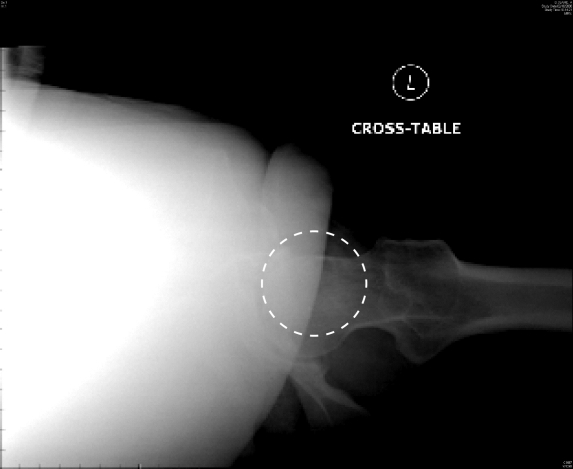
The next step in the assessment is appropriate imaging. If radiographs have not yet been completed, they should be arranged at this time. There are a number of specialized plain film views as well as other imaging modalities, including computed tomography scan and magnetic resonance arthrogram, which are used by orthopedic surgeons for surgical decision making and preoperative planning. At this stage, however, an anteroposterior view of the pelvis and a lateral view of the affected hip are all that is required, and more specialized imaging should be left to the discretion of the treating orthopedic surgeon. Morphologic abnormalities such as those listed above as well as the presence of any degenerative changes can be observed with this imaging. There are subtle findings on otherwise normal radiographs that might further support a diagnosis of impingement syndrome. These include a loss of the normal concavity at the head-neck junction, which can be seen on the anteroposterior view; posterior placement of the femoral head relative to the neck as seen on the cross-table lateral view; and presence of herniation pits on the anterolateral femoral neck, which might be seen on both views 1 ( Figure 3 ). It is important to be aware that hip impingement syndrome can, and often does, present with results of plain radiographs reported as normal. An inability to recognize these subtleties or a lack of access to the images should not overshadow a convincing history and physical examination findings, including a positive impingement test. The presence of degenerative changes on plain radiographs warrants discussion with the patient regarding a diagnosis of osteoarthritis and the appropriate management based on age, activity level, patient wishes, and his or her expectations. The presence of advanced degenerative changes precludes a diagnosis of impingement syndrome and, as such, the treatment options available.
Figure 3A . Anteroposterior scan of the pelvis in a patient with impingement syndrome .
Note the presence of abnormal prominence at the junction of the femoral head and neck on the superior aspect of the left hip, creating an abnormal contour (arrow).
Management
Having determined that the clinical presentation is consistent with impingement syndrome, family physicians are faced with the need for appropriate management and referral if necessary. As with many musculoskeletal problems, a brief course of conservative therapy is warranted. This should include activity modification or avoidance of exacerbating activities, rest, and anti-inflammatory medication (assuming no contraindications exist). Intensive physiotherapy is unlikely to be of benefit given the nature of the condition, and attempts to improve range of motion might continue the impinging process and aggravate the condition. Efforts should be made to continue with physical activity that does not aggravate symptoms so as to minimize muscular deconditioning. Given the mechanical nature of FAI, this symptomatic management will have little effect on the underlying cause, and attempts to return to previous activity will likely cause symptoms to recur. Therefore, concurrent referral to an orthopedic specialist is warranted.
Impingement syndrome is still a relatively new entity within orthopedic surgery. Surgical techniques for managing the problem are highly specialized and are unlikely to be undertaken by the general orthopedist. Most orthopedic surgeons will, however, have knowledge of a colleague experienced with impingement syndrome or hip surgery in general. Family physicians might wish to contact a local orthopedic surgeon and inquire about appropriate referral. Depending on practice location, such a referral might involve travel to another city or even province.
If, after specialist consultation and investigation, surgical intervention is offered, the various procedures must be discussed in detail with the patient. Briefly, these procedures involve addressing the intra-articular pathology leading to impingement between the acetabulum and proximal femur. Often, this involves carefully adjusting the contour of the femoral head-neck junction or the bony acetabular rim in addition to any intra-articular soft tissue problems such as labral tears. Such procedures can be carried out arthroscopically or via open surgical procedure, depending on the surgeon’s experience and the exact nature of the pathology. Both arthroscopic and open surgical treatment for FAI have been shown to substantially improve symptoms and hip function. 5 , 10 – 15
Case resolution
H.P. provides a history consistent with hip impingement. His activity certainly involves extreme ranges of flexion and rotation of the hip, both of which exacerbate his symptoms. His difficulty with tying his shoes could be related to a decreased range of motion due to pain or mechanical causes. Symptomatic treatment has been ineffective, as the underlying etiology has not been addressed. As is often the case, several other health care practitioners have been involved in his care without a correct diagnosis having been made. The report of a normal radiograph of the hip might lead many physicians to recommend continued symptomatic management or the pursuit of other possible sources of his pain. In the presence of clinical findings, such as decreased internal rotation and, in particular, a positive impingement test, this patient would certainly warrant further assessment and investigation by an orthopedic surgeon for possible hip impingement syndrome.
Conclusion
Nonarthritic hip pain due to impingement syndrome in young adult patients represents a difficult clinical problem. Such patients often respond poorly to symptomatic measures and are frequently unwilling to accept the functional limitations imposed by their symptoms. Furthermore, because of their young age, lack of degenerative changes, and functional expectations, joint replacement is inappropriate.
Hip impingement syndrome refers to a constellation of signs and symptoms brought about by abnormal contact between the acetabulum and femoral head-neck junction as a result of extreme range of motion activities or osseous abnormalities on either side of the hip joint. The presence of a consistent history and physical findings such as a positive impingement test should alert the family physician to the possibility of hip impingement syndrome. Radiographic studies might be reported as normal unless critically reviewed by specialists familiar with the subtleties of impingement syndrome. Referral to the appropriate specialist can provide the patient with options for treatment, which could result in substantial symptomatic relief and functional improvement and, perhaps, prevent or delay the onset of joint degeneration. Fortunately, with a general understanding of FAI syndrome, family physicians can recognize these patients and play an active role in their appropriate and timely management.
Figure 3B .
Lateral projection depicting lack of normal anterior offset of the femoral head (circle) relative to the neck
EDITOR’S KEY POINTS
Although there are many causes of nonarthritic hip pain in adults, impingement syndrome should be considered, as it could lead to degenerative changes.
The impingement test is positive in more than 90% of those with impingement syndrome.
Results of radiographs in the early stages might be normal.
If a brief course of conservative therapy fails to improve symptoms, referral to an orthopedic surgeon familiar with this condition is warranted.
POINTS DE REPÈRE DU RÉDACTEUR
Quoi qu’il existe plusieurs causes de douleur de hanche non arthritique chez l’adulte, on doit penser à un conflit fémoro-acétabulaire, une condition qui pourrait entraîner des changements dégénératifs.
Le test du conflit est positif chez plus de 90% des patients qui présentent ce syndrome.
Aux stades initiaux, les radiographies peuvent s’avérer normales.
Si les symptômes ne s’améliorent pas avec un traitement conservateur court, le patient doit être dirigé vers un chirurgien orthopédiste qui connaît bien cette condition.
Footnotes
Competing interests
None declared
This article has been peer reviewed.
References
- 1. Ganz R , Parvizi J , Beck M , Leunig M , Notzli H , Siebenrock KH . Femoroacetabular impingement: a cause for osteoarthritis of the hip . Clin Orthop Rel Res . 2003 ; 417 : 112 – 20 . doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 2. Kassarjian A , Yoon LS , Belzile E , Connolly SA , Millis MB , Palmer WE . Triad of MR arthrographic findings in patients with cam-type femoroacetabular impingement . Radiology . 2005 ; 236 : 588 – 92 . doi: 10.1148/radiol.2362041987. [DOI] [PubMed] [Google Scholar]
- 3. Ito K , Minka MA , Leunig M , Werlen S , Ganz R . Femoroacetabular impingement and the cam effect: a MRI based quantitative anatomical study of the femoral head neck offset . J Bone Joint Surg Br . 2001 ; 83 : 171 – 6 . doi: 10.1302/0301-620x.83b2.11092. [DOI] [PubMed] [Google Scholar]
- 4. Ito K , Leunig M , Ganz R . Histopathologic features of the acetabular labrum in femoroacetabular impingement . Clin Orthop Rel Res . 2004 ; 429 : 262 – 71 . doi: 10.1097/01.blo.0000144861.11193.17. [DOI] [PubMed] [Google Scholar]
- 5. Beck M , Leunig M , Parvizi J , Boutier V , Wyss D , Ganz R . Anterior femoroacetabular impingement: part 2. Midterm results of surgical treatment . Clin Orthop . 2004 ; 418 : 67 – 73 . [PubMed] [Google Scholar]
- 6. Goodman DA , Feighan JE , Smith AD , Latimer B , Buly RL , Cooperman DR . Subclinical slipped capital femoral epiphysis . J Bone Joint Surg . 1997 ; 79 : 1489 – 97 . doi: 10.2106/00004623-199710000-00005. [DOI] [PubMed] [Google Scholar]
- 7. Lavigne M , Parvizi J , Beck M , Siebenrock KA , Ganz R , Leunig M . Anterior femoroacetabular impingement: part 1. Techniques of joint preserving surgery . Clin Orthop Rel Res . 2004 ; 418 : 61 – 6 . [PubMed] [Google Scholar]
- 8. Tanzer M , Noiseux N . Osseous abnormalities and early osteoarthritis: the role of hip impingement . Clin Orthop Rel Res . 2004 ; 429 : 170 – 7 . [PubMed] [Google Scholar]
- 9. Wagner S , Hofstetter W , Chiquet M , Mainil-Varlet P , Stauffer E , Ganz R , et al. Early osteoarthritic changes of human femoral head cartilage subsequent to femoroacetabular impingement . Osteoarthritis Cartilage . 2003 ; 11 ( 7 ): 508 – 18 . doi: 10.1016/s1063-4584(03)00075-x. [DOI] [PubMed] [Google Scholar]
- 10. Peters CL , Erickson JA . Treatment of femoro-acetabular impingement with surgical dislocation and debridement in young adults . J Bone Joint Surg . 2006 ; 88A : 1735 – 41 . doi: 10.2106/JBJS.E.00514. [DOI] [PubMed] [Google Scholar]
- 11. Murphy S , Tannast M , Kim YJ , Buly R , Millis MB . Debridement of the adult hip for femoroacetabular impingement: indication and preliminary clinical results . Clin Orthop Rel Res . 2004 ; 429 : 178 – 81 . doi: 10.1097/01.blo.0000150307.75238.b9. [DOI] [PubMed] [Google Scholar]
- 13. Espinosa N , Rothenfluh D , Beck M , Ganz R , Leunig M . Treatment of femoroacetabular impingement: preliminary results of labral refixation . J Bone Joint Surg Am . 2006 ; 88A : 925 – 35 . doi: 10.2106/JBJS.E.00290. [DOI] [PubMed] [Google Scholar]
- 14. Beaule P , LeDuff M , Zaragoza E . Quality of life following femoral head-neck osteoplasty for femoroacetabular impingement . J Bone Joint Surg Am . 2007 ; 89 : 773 – 9 . doi: 10.2106/JBJS.F.00681. [DOI] [PubMed] [Google Scholar]
- 15. Burnett RS , Della Rocca GJ , Prather H , Curry M , Maloney WJ , Clohisy JC . Clinical presentation of patients with tears of the acetabular labrum . J Bone Joint Surg Am . 2006 ; 88A : 1448 – 57 . doi: 10.2106/JBJS.D.02806. [DOI] [PubMed] [Google Scholar]