Abstract
OBJECTIVE
To carry out initial psychometric testing on the Simple Lifestyle Indicator Questionnaire (SLIQ).
DESIGN
Self-administered questionnaire to obtain data for test-retest reliability, for Cronbach α testing on completed questionnaires, and for blinded external validity testing.
SETTING
Kingston, Ont, and surrounding area.
PARTICIPANTS
One hundred thirty-six family practice patients with an mean age of 68 years; 58% were women. Subjects were primarily white and living in a small city and itsrural surroundings.
MAIN OUTCOME MEASURES
Test-retest coefficients, Cronbach α values, and correlation coefficients.
RESULTS
Test-retest reliability on the 12 questions ranged from 0.63 to 0.97. The Cronbach α was 0.58 for questions on diet and 0.6 for questions on physical activity. We found a correlation coefficient of 0.77 between participants’ and blinded raters’ scores on the SLIQ.
CONCLUSION
The SLIQ, as currently tested, is likely suitable for use in research on people who are at least similar to those in our study population. It probably should not be used in clinical settings until further testing has been carried out.
RÉSUMÉ
OBJECTIF
Faire une première évaluation psychométrique du Questionnaire abrégé indicateur du mode de vie (QAIM).
TYPE D’ÉTUDE
Questionnaire auto-administré afin d’obtenir des données pour la fiabilité test-retest, pour l’évaluation du questionnaire par le Cronbach α et pour le test à l’aveugle de la validité externe.
CONTEXTE
Kingston, Ont, et environs.
PARTICIPANTS
Cent trente-six patients d’une clinique de médecine familiale âgés en moyenne de 68 ans, dont 58% de femmes. Les sujets étaient principalement de race blanche et habitaient une petite ville ou la campagne environnante.
PRINCIPAUX PARAMÈTRES À L’ÉTUDE
Coefficients test-retest, valeurs du Cronbach α et coefficients de corrélation.
RÉSULTATS
La fiabilité test-retest pour les 12 questions variait entre 0,63 et 0,97. Le Cronbach α était de 0,58 pour les questions sur l’alimentation et de 0,6 pour celles sur l’activité physique. On a trouvé un coefficient de corrélation de 0,77 entre les scores des participants et ceux des évaluateurs à l’aveugle pour le QQAIM.
CONCLUSION
D’après cette évaluation, le QAIM semble adéquat pour une recherche sur une population semblable à celle de notre étude. Il ne devrait probablement pas être utilisé dans des contextes cliniques avant d’avoir été davantage testé.
Those investigating cardiovascular disease often require assessment of the lifestyles of the participants in their research projects. While we found various scales that measured the individual components of lifestyle1–4 that affect cardiovascular disease (diet, activity, stress, smoking, alcohol consumption), we were unable to find a health-measurement scale that measured all these components at once.
Our research into hypertension5–7 required such a scale. It needed to be short, reliable, valid, and useful in both research and clinical settings. This paper reports on our initial psychometric testing of such a scale, the Simple Lifestyle Indicator Questionnaire (SLIQ).
METHODS
Figure 1 lists the 12 questions on the SLIQ and indicates the scoring procedure. The SLIQ has 5 components: diet (3 questions), activity (3 questions), alcohol consumption (3 questions), smoking (2 questions), and stress (1 question). For each component, a raw score and a category score can be calculated. To provide equal weighting for each component, the overall SLIQ score is based on the 5 category scores. Each component has a category score of 0, 1, or 2, so overall SLIQ scores can range from 0 to 10. The higher the score, the more healthy the lifestyle.
Figure 1.
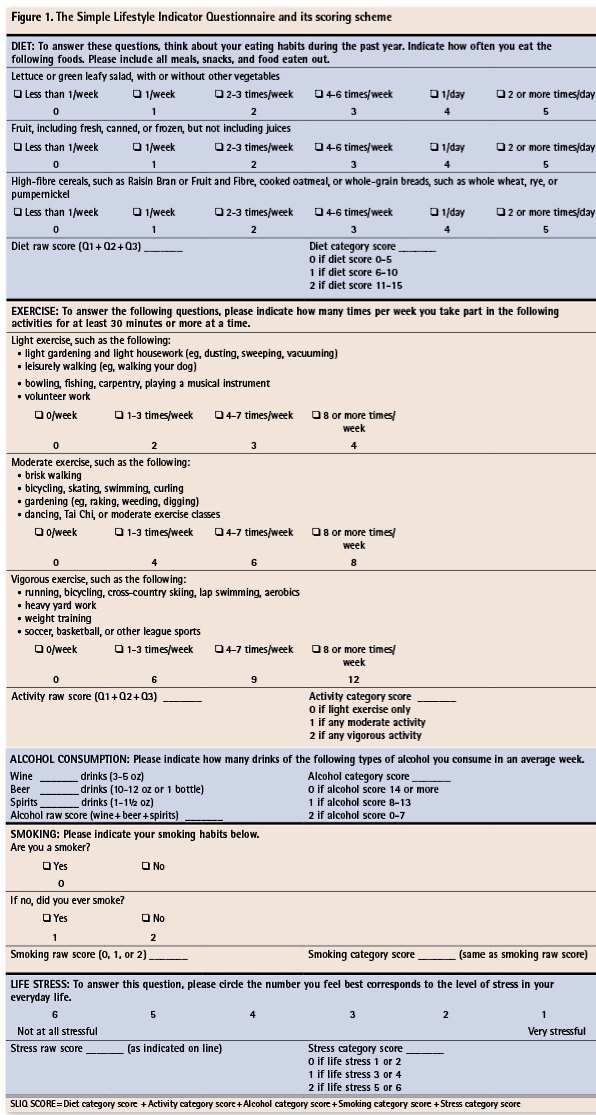
The Simple Lifestyle Indicator Questionnaire and its scoring scheme
Initial development and face and content validity
Originally, the SLIQ had 25 questions that had been drafted by 2 family physicians and a nutritionist. These were reviewed by a group, consisting of 3 family physicians, a nutritionist, and a nurse practitioner, which was asked to assess and comment on the content areas, the content of each item, and the structure of the questionnaire. Based on comments from this group and a factor analysis of the 9 original questions on diet, the final questions for the SLIQ were chosen. The factor analysis was done on 30 questionnaires completed by patients selected opportunistically in a family practice clinic.
Testing population
Once the content of the questions was final, and face and content validity had been assessed, formal evaluation of test-retest reliability, internal consistency, and external validity was undertaken. This testing was done on the first 136 people to be enrolled in a randomized study of home blood pressure monitoring. The eligibility criteria for that study included being 18 years old or older, having a diagnosis of hypertension, and not having achieved target blood pressure levels. People with diabetes, heart disease, or other comorbidity were not excluded.
Test-retest reliability
The 136 people were asked to complete the SLIQ and to complete it again 1 month later. Test-retest reliability coefficients were calculated for each question.
Internal consistency (Cronbach α)
Cronbach α indicates the degree to which the various questions are measuring the same construct. Only the questions on diet and activity were amenable to assessment by Cronbach α. These 2 components have 3 questions each. The component on stress has only 1 question and so cannot be assessed for Cronbach α. The questions on smoking and alcohol consumption are structured such that they are mutually exclusive and would not be expected to be scored in the same direction.
External validity
External validity was measured on a subsample of 60 questionnaires chosen randomly and assessed by 3 practitioners: a family doctor, a nurse practitioner, and a nutritionist. Without knowing how the questionnaires would have been scored on the SLIQ scoring template, these 3 health professionals were asked to review the responses and rank respondents’ lifestyles on a scale of 0 to 10, then to rank them categorically as unhealthy, intermediate, or healthy. These scores were then correlated with the SLIQ scores using the Pearson correlation coefficient as a measure of validity.
RESULTS
Mean age of the 136 respondents was 68 years (standard deviation ±12 years), and 58% of them were women. They were primarily white and lived in a small city and its rural surroundings in southeastern Ontario. Table 1 shows the characteristics of the study population.
Table 1.
Characteristics of the study population: Mean age of subjects was 68 years (±12 years); N = 136.
| A) CHARACTERISTIC | N (%) |
|---|---|
| Female sex | 79 (58%) |
| With diabetes | 18 (14%) |
| With hyperlipidemia | 38 (28%) |
| B) CHARACTERISTIC | MEAN (STANDARD DEVIATION) |
| Body mass index | 30 (±5) |
| Waist circumference (cm) | 97 (±12) |
Face and content validity
The family physicians, nutritionist, and nurse practitioner who reviewed the final 12 questions thought that the content areas, content of items, and questionnaire structure covered the areas of lifestyle important in cardiovascular disease (content validity). They also thought that “on the face of it” the questions were reasonable and unambiguous (face validity).
Test-retest reliability
Table 2 shows test-retest reliability coefficients of each of the 12 questions on the SLIQ. The reliability coefficients for the alcohol and smoking components are quite good in the range of 0.87 to 0.97, and the reliability coefficient for the stress component is also reasonable at 0.75. The coefficients for the diet and activity components are lower, in the range of 0.63 to 0.74. These are still significant and acceptable correlations, given the less concrete nature of the domains being assessed.
Table 2. Test-retest reliability.
All coefficients significant at the .001 level.
| COMPONENT OF TEST | COEFFICIENT |
|---|---|
| Vegetables | 0.74 |
| Fruit | 0.72 |
| Fibre | 0.63 |
| Light exercise | 0.64 |
| Moderate exercise | 0.66 |
| Vigorous exercise | 0.71 |
| Wine | 0.88 |
| Beer | 0.87 |
| Spirits | 0.88 |
| Smoking | 0.97 |
| Former smoking | 0.89 |
| Stress | 0.75 |
Internal consistency (Cronbach α)
Cronbach α was measured separately on the 3 diet questions and the 3 activity questions. The coefficients for these questions were not excellent, but were reasonably good at the level of 0.58 for the diet questions and 0.6 for the questions on activity.
External validity
Comparison of SLIQ scores as measured by the scoring template with scores obtained by the health professionals’ blinded assessment of the questions validated our scoring scheme. We achieved a correlation coefficient of r = 0.77 (P = .001) between SLIQ scores and blinded reviewers’ scores. Interrater correlations between the health professionals were the following: nutritionist versus family doctor r = 0.6; nutritionist versus nurse practitioner r = 0.61; and nurse practitioner versus family doctor r = 0.73.
DISCUSSION
The SLIQ has very good test-retest reliability, good internal consistency, and, to the degree that we have tested it to date, good external validity. It requires further testing to delineate more clearly how well it correlates with a full clinical assessment (concurrent validity). The research question would be “How well does this 5-minute questionnaire correlate with a 30-minute clinical assessment aimed at rating a patient’s lifestyle?” There is also a need to compare each component’s score with a fully validated scale known to measure that component reliably. In essence, each component needs to be compared with the criterion standard measurement for that component (convergent validity). The SLIQ also needs to be tested on a range of populations. Our study population was primarily white, culturally Canadian, and living in and around a small Ontario city.
The most common question asked by people reviewing the SLIQ is how the 3 questions on diet, which ask about only salads, fruit, and fibre, can be used to assess a spectrum of dietary components. The factor analysis we did before this study strongly suggested that people who have good dietary practices related to salads, fruit, and fibre also have good dietary practices around eating fish, not eating junk food, and choosing food low in saturated fat. We do not need to ask questions about this other food because of the high correlation between dietary practices.
Conclusion
The SLIQ, as currently tested, is probably suitable for use in research on people who are at least similar to our study population. It probably should not be used in clinical settings until further testing has proved that it is a reliable instrument for measuring a range of lifestyle components.
EDITOR’S KEY POINTS
While there are various scales for measuring the individual components of lifestyle that affect cardiovascular disease, the authors were unable to find a scale for measuring several components at once.
This paper reports on initial psychometric testing of such a scale, the Simple Lifestyle Indicator Questionnaire.
The Simple Lifestyle Indicator Questionnaire, as currently tested, is probably suitable for use in research on people who are at least similar to the population in this study. It likely should not be used in clinical settings until further testing has been carried out.
POINTS DE REPÈRE DU RÉDACTEUR
Même s’il existe plusieurs échelles pour mesurer les diverses composantes du mode de vie qui influencent les maladies cardiovasculaires, les auteurs n’en ont trouvé aucune capable de mesurer plusieurs composantes à la fois.
Cet article décrit l’évaluation psychométrique initiale d’une de ces échelles, le Questionnaire abrégé indicateur du mode de vie.
Dans son état actuel, le Questionnaire abrégé indicateur du mode de vie convient probablement pour une recherche sur une population semblable à celle de l’étude présente. Il ne devrait vraisemblablement pas être utilisé dans un contexte clinique avant d’avoir été davantage testé.
Footnotes
Contributors
Dr Godwin, Ms Streight, Dr Dyachuk, Ms van den Hooven, Ms Ploemacher, Ms Seguin, and Ms Cuthbertson contributed to concept and design of the study, analysis and interpretation of data, and preparing the manuscript for publication.
Competing interests
None declared
*Full text is available in English at www.cfp.ca.
This article has been peer reviewed.
References
- 1.Newby PK, Hu FB, Rimm EB, Smith-Warner SA, Feskanich D, Sampson L, et al. Reproducibility and validity of the Diet Quality Index Revised as assessed by use of a food-frequency questionnaire. Am J Clin Nutr. 2003;78(5):941–9. doi: 10.1093/ajcn/78.5.941. [DOI] [PubMed] [Google Scholar]
- 2.Haines PS, Siega-Riz AM, Popkin BM. The Diet Quality Index revised: a measurement instrument for populations. J Am Diet Assoc. 1999;99(6):697–704. doi: 10.1016/S0002-8223(99)00168-6. [DOI] [PubMed] [Google Scholar]
- 3.Tudor-Locke C, Burkett L, Reis JP, Ainsworth BE, Macera CA, Wilson DK. How many days of pedometer monitoring predict weekly physical activity in adults? Prev Med. 2005;40(3):293–8. doi: 10.1016/j.ypmed.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 4.Levenstein S, Prantera C, Varvo V, Scribano ML, Berto E, Luzi C, et al. Development of the Perceived Stress Questionnaire: a new tool for psychosomatic research. J Psychosom Res. 1993;37(1):19–32. doi: 10.1016/0022-3999(93)90120-5. [DOI] [PubMed] [Google Scholar]
- 5.Godwin M, Delva D, Seguin R, Casson I, MacDonald S, Birtwhistle R, et al. Relationship between blood pressure measurements recorded on patients’ charts in family physicians’ offices and subsequent 24 hour ambulatory blood pressure monitoring [abstract] BMC Cardiovasc Disord. 2004;4:2. doi: 10.1186/1471-2261-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Birtwhistle RV, Godwin MS, Delva MD, Casson RI, Lam M, MacDonald SE, et al. Randomised equivalence trial comparing three month and six month follow up of patients with hypertension by family practitioners. BMJ. 2004;328(7433):204. doi: 10.1136/bmj.37967.374063.EE. Epub 2004 Jan 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Godwin M, Ruhland L, Casson I, MacDonald S, Delva D, Birtwhistle R, et al. Pragmatic controlled clinical trials in primary care: the struggle between external and internal validity [abstract] BMC Med Res Methodol. 2003;3:28. doi: 10.1186/1471-2288-3-28. [DOI] [PMC free article] [PubMed] [Google Scholar]


