Abstract
Cardiovascular disease represents the leading cause of morbidity and mortality in Western countries, and hypertension-related cardiovascular events affect about 37 million people per year, worldwide. In this perspective, hypertensive patients are at increased risk to experience cardiovascular events during life-long period, and treatment of high blood pressure represents one of the most effective strategies to reduce global cardiovascular risk. However, due to its multifactorial pathophysiology and its frequent association with other relevant risk factors and clinical conditions, treatment of hypertension requires an integrated approach, including lifestyle measures, antihypertensive drugs and other therapies. Yet, worldwide general practitioners continue to focus their attention on the management of a single risk factor, eg, blood pressure, rather than to global cardiovascular risk profile. In this view, modern strategies of cardiovascular prevention in hypertensive patients should move from a single risk factor based approach toward a more comprehensive risk evaluation in the individual patient. In other words, it is important to define the global cardiovascular risk to manage hypertensive patients at high-risk, rather than to focus on the high level of a single risk factor, for reducing cardiovascular morbidity and mortality in the general population, as well as in hypertensive population.
Keywords: hypertension, hypercholesterolemia, cardiovascular prevention, global cardiovascular risk
Introduction
Hypertension represents today a major public concern. In fact, it affects more than 20% of the adult population in Western countries and about a billion people worldwide (Collins et al 1990; MacMahon et al 1990). The presence of high blood pressure levels doubles the risk of ischemic heart disease and increases by four-fold incidence of stroke (Van den Hoogen et al 2000; Lewington et al 2002). On the other hand, treatment of hypertension reduces by approximately 40% stroke incidence and by about 14% coronary events (BPLTTC 2000). In spite of these evident benefits, only 20% of hypertensive patients receive an adequate treatment to keep blood pressure within the recommended threshold of normality (HDFPCG 1979; Wolf-Maier et al 2003). Together with the other modifiable cardiovascular risk factor, such as hyperglicemia, hypercholesterolemia, smoking and obesity, hypertension heavily contributes to the global cardiovascular burden of morbidity and mortality, as well as to increase individual absolute cardiovascular risk (Kannel 2000). In this view, modern strategies of cardiovascular prevention should consider a more comprehensive evaluation of risk factor profile in the individual patient (ESH/ESC 2003; WHO/ISH 2003; ADA 2003).
The clustering of cardiovascular risk factors in hypertensive patients is indeed an extremely frequent observation in both epidemiological studies and clinical practice, and less than 20% of hypertensive patients have no associated risk factors, whereas the remaining 80% have one or more associated risk factors (Kannel 2000). As addressed in the most recent European Guidelines on hypertension (ESH/ESC 2003), the concomitant presence of risk factors in hypertensive patients translates in progressively higher absolute cardiovascular risk, as clearly demonstrated about 15 years ago in the Framingham Heart Study (Andersson et al 1998). Depending upon the co-existence of none, one, two or more risk factors or diabetes, the level of added risk rises from low to moderate or high risk, as represented in Figure 1.
Figure 1.
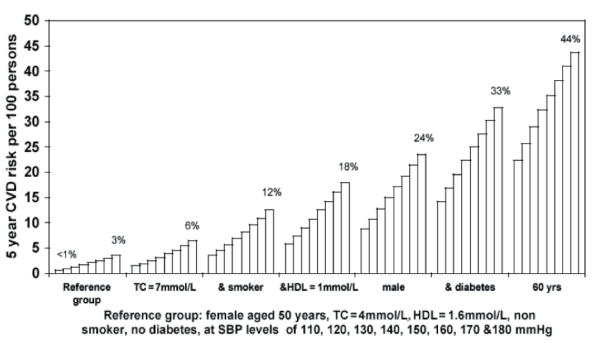
Absolute risk of cardiovascular disease over 5 years in patients by systolic blood pressure at specified levels of other risk factors. Copyright © 1991. Derived from Anderson KM, Odell PM, Wilson PW, et al 1991. Cardiovascular disease risk profiles. Am Heart J, 121(1 Pt 2):293–8.
In this view, as the benefits of reducing blood pressure are proportional to the levels of risk, in high-risk hypertensive patients a tighter control of blood pressure levels is recommended, and will result in a progressively greater benefit. In specific conditions, such as in the presence of concomitant diabetes, lower blood pressure targets are recommended to ensure a larger impact on outcomes, as it has been demonstrated in the United Kingdom Prospective Diabetes Study (UKPDS) (UKPDS 1998).
Recommendations derived from guidelines (ESH/ESC 2003) and recent observations from large international trials in hypertension (Yusuf et al 2002; Gaede et al 2003) clearly indicate that a prompt and tight control of blood pressure may reduce cardiovascular events in high-risk subjects. In this view, patients with hypertension and multiple concomitant risk factors, as those included in the Valsartan Antihypertensive Long-term Use Evaluation (VALUE) study (Julius et al 2004), deserve closer clinical observation and more prompt and aggressive therapeutic control of blood pressure levels aiming at the achievement of target levels of or below. In these patients multiple (two up to four) antihypertensive agents are often required to achieve the recommended targets. However, the achievement of blood pressure targets is difficult in such patients, and therefore, in order to adequately reduce the level of risk, other therapeutic strategies aimed at reducing the influence of concomitant risk factors (eg, lipid-lowering agents or aspirin) are helpful (HPS 2002; Sever et al 2003; Hansson et al 1998).
On the basis of these evidence, modern strategies of cardiovascular prevention in hypertensive patients should move from a single risk factor-based approach (eg, focusing on blood pressure) toward a more comprehensive evaluation and management of risk factor profile in the individual patient (Alderman et al 2002; Volpe et al 2004). In other words, it is important to adopt a more thorough approach aimed at reducing global cardiovascular risk. The decision to treat a patient should be based on the level of global risk, rather than on the level of a single risk factor. The decision about which risk factor, or factors, to treat should be also based primarily on the level of risk: the higher the absolute risk, the more intensive and extensive the treatment should be (Alderman et al 2002; Volpe et al 2004). This approach starts and ends with the patient’s global risk rather than on the basis of the level of a single risk factor.
Modern view of multiple risk management
Over the past two decades, observational studies have consistently demonstrated a strong and direct correlation between cardiovascular morbidity and mortality across the whole blood pressure spectrum, with no evidence of a threshold down to as low as 115/75 mmHg (Collins et al 1990; MacMahon et al 1990). For instance, the Framingham Heart Study showed that even slight elevations in blood pressure levels to the prehypertensive threshold (120–139/80–89 mmHg) is associated with a doubling of the incidence of cardiovascular events versus “normal” blood pressure levels (<120/80 mmHg) (Vasan et al 2001). Consistent evidence supporting a continuous relationship between blood pressure and cardiovascular risk can be derived from other large epidemiological studies and databases (Stamler et al 1986; Yusuf et al 2004). Moreover, nonhypertensive individuals with multiple risk factors or a history of cardiovascular disease are often at higher absolute risk of cardiovascular and renal events than hypertensive patients with few or no other additive risk factors (Conroy et al 2003).
As a consequence, guidelines have started to acknowledge the concept that other factors, besides high blood pressure levels, may further contribute to determine global cardiovascular risk profile of an individual patient. Although this process is still slow and incomplete, and in some representative sets of guidelines, such as in those issued in 2003 by Joint National Committee (JNC) VII (Chobanian et al 2003), this is not properly addressed in criteria for diagnosis and classification of essential hypertension.
Historically, therapeutic intervention thresholds for the treatment of cardiovascular risk factors, such as high blood pressure, blood cholesterol and glucose levels, have been based on different arbitrary threshold of each individual risk factor, which have been issued in different sets of guideline. Accordingly, physicians frequently persist to focus on the treatment of high blood pressure or cholesterol levels, rather than on the prevention of high blood pressure or high cholesterol-related cardiovascular disease. Because risk factors cluster in individuals (Kannel 2000), and there is a graded and continuous association between the sum of risk factors and overall cardiovascular risk (Stamler et al 1986; Anderson et al 1991), the contemporary approach to treatment should be unequivocally based on the assessment of the threshold, at least for cholesterol and blood pressure, based on the calculation of estimated coronary (Kannel 2000; Conroy et al 2003) or cardiovascular (coronary plus stroke) (ESH/ESC 2003, Grundy et al 1998, 1999) risk over a defined (usually 5 or 10 years) period.
Evidence derived from large studies demonstrated that blood pressure lowering and lipid lowering agents may substantially reduce the risk of coronary or major cardiovascular events in a broad range of otherwise healthy subjects at high-risk profile, as well as in hypertensive or hypercholesterolemic patients at different thresholds of absolute risk (Daholf et al 2002, 2005; Cannon et al 2004; Julius et al 2004; LaRosa et al 2005). The absolute benefits of these regimens for such patients are substantially greater than those achieved in patients with uncomplicated hypertension or hypercholesterolemia. In this regard, even small reductions in blood pressure levels, as well as for any other traditional risk factor, may generate significant reduction of absolute risk in high-risk patients. As schematically shown in Figure 2, the treatment of multiple risk factors (eg, blood pressure and blood cholesterol) results in additive benefit, that clearly exceed the advantage of reducing aggressively one single risk factor (for instance, normalizing blood pressure).
Figure 2.
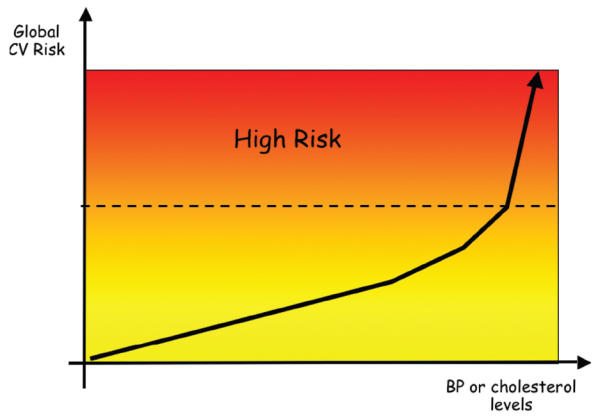
New paradigms in the management of cardiovascular disease: reduction of single or multiple risk factors generates a benefit proportional to the level of Risk. Risk increases in relation to clinical characteristics of individual, thus small reductions of each risk factor will produce larger absolute benefits in relation to level of absolute risk. Copyright © 2005. Modified from Volpe M, Ruilope LM, McInnes GT, et al 2005. Angiotensin-II receptor blockers: benefits beyond blood pressure reduction? J Hum Hypertens, 19:331 9.
Although arguments persist about the degree to which these effects relate to drug-specific properties, data suggest that the size of the risk factor reduction achieved is a more important determinant of outcome than the choice of drug, especially in high-risk individuals (Anderson et al 1991). In this type of patients, clinical outcomes trials, including the Perindopril pROtection aGainst REcurrent Stroke Study (PROGRESS) (PROGRESS 2001), the Antihypertensive and Lipid-Lowering treatment to prevent Heart Attack Trial (ALLHAT) (ALLHAT 2002), and the VALUE studies (Julius et al 2004), support the concept that “lower is better” for blood pressure. In addition, evidence derived from international, randomized, controlled trials, such as the Lipid-Lowering Arm of the Anglo- Scandinavian Cardiac Outcomes Trial (ASCOT-LLA) (Sever et al 2003), the Pravastatin or Atorvastatin Evaluation and Infection Therapy–Thrombolysis in Myocardial Infarction 22 (PROVE IT–TIMI 22) trial (Cannon et al 2004) and more recently the Treating to New Targets (TNT) trial (LaRosa et al 2005), strongly indicate that in hypertensive patients with very high cardiovascular risk an aggressive therapeutic approach aimed to lower the serum cholesterol concentrations with higher doses of statins rather than those commonly used in the clinical practice, significantly reduced the incidence of cardiovascular mortality and major cardiovascular events respect to conventional treatment. However, most patients worldwide are neither being treated effectively, nor achieving optimal blood pressure or cholesterol control (Mancia et al 1997; Libby 2005), according with recommendations of the recent guidelines (Grundy et al 1999; ESH/ESC 2003).
Global cardiovascular risk assessment
As previously discussed, the presence of multiple cardiovascular risk factors rather than high level of any single risk factor in particular is usually the primary determinant of global risk of cardiovascular events in an individual. The absolute risk is the likelihood that a person will have a cardiovascular event over a given period of time (usually 5 to 10 years) (Grundy et al 1999). On the other hand, the relative risk is represented by the ratio of the absolute risk of a given patient (or group) to that of a low-risk group (Grundy et al 1999). Treatment decisions are based on the likelihood an individual will have a cardiovascular event over a given period of time (Grundy et al 1999). This replaces decision-making based on individual risk factor levels. It follows that at a given blood pressure, the risk of cardiovascular events can vary widely depending on the presence or absence of other nonblood pressure-related risk factors. Randomized clinical trials have also shown that in persons with a given blood pressure level, the relative risk reduction with antihypertensive treatment is similar in those with or without other risk factors (Alderman et al 2002). Two patients with the same systolic blood pressure may have very different global cardiovascular risk depending on the presence or absence of other risk factors (Volpe et al 2004). Their relative treatment benefit is the same, but the absolute risk benefit will be much greater in the higher-risk person.
In whom and when is it appropriate to do risk assessment?
As recommended by the most recent guidelines, risk assessments should be provided at the primary care level by health practitioners with appropriate training (Grundy et al 1999; Conroy et al 2003). Practitioners should be aware of the need to focus on population groups that have a high burden of cardiovascular disease. Accordingly, cardiovascular risk assessments are recommended:
◦ from the age of 45 years for asymptomatic men without other known risk factors
◦ from the age of 55 years for asymptomatic women without other known risk factors.
◦ from the age of 35 years for men with other known cardiovascular risk factors or at high risk of developing diabetes
◦ from the age of 45 years for women with other known cardiovascular risk factors or at high risk of developing diabetes.
◦ All those with cardiovascular disease should have comprehensive risk factor measurements to determine the best management approach.
How to perform the risk assessment?
In the clinical practice, the evaluation of the patient’s individual risk can be facilitated by the use of several tools. The application of risk charts, for instance, provide either advantages (quick and simple means to calculate the global cardiovascular risk; projection of the risk of an individual over time; comprehensible way to explain the risk factor modification concept to patients; etc), and limitations (limited number of risk factors that can be included; physicians should consider other risk factors and qualifiers when estimating individual risk profile; do not replace good clinical judgment about which and how much risk factors should be managed; no magic cut-point in defining classes of risk, as the cardiovascular risk is a continuum).
Risk charts generally identify major modifiable traditional risk factors (cigarette smoking, elevated blood pressure levels, elevated serum Total and LDL Cholesterol levels, low serum HDL Cholesterol levels, Diabetes Mellitus) and major not modifiable risk factors (age, sex, race). Other predisposing risk factors (abdominal obesity, physical inactivity, family history of premature coronary heart disease, psychosocial factors) or conditional risk factors (elevated serum triglycerides, small LDL particles, elevated serum homocysteine, elevated serum lipoprotein(a), C-reactive protein) are usually not considered. While major risk factors are strongly and independently related to increased incidence of major cardiovascular events, such as acute myocardial infarction, ischemic stroke or total cardiovascular mortality, which often represent the primary hard endpoints in the clinical trials, the other risk factors, even though a smaller quantitative contribution in determining the global risk profile and not a well-defined role in the pathogenesis of cardiovascular events, have been demonstrated to be of relevance in the clinical management of individual patients, and often represent direct targets of treatment in the clinical practice, characterizing the so-called secondary endpoints in the clinical trials. In addition, it is of note that the concomitant presence of other not modifiable risk factors, mostly age, represents a condition predisposing the development and enhancing the deleterious effects of concomitant modifiable risk factors.
A large body of risk charts and calculators to assess the coronary or global (coronary and cerebrovascular events) risk in individual patients have been proposed in the last two decades, since the Framingham experience (Kannel 2000). In this latter regard, the Framingham Score predicts either total coronary heart disease (CHD) (stable and unstable angina pectoris, myocardial infarction and CHD death), or major CHD events (myocardial infarction and CHD death) (Kannel 2000). However, this estimation of cardiovascular risk implies several limitations. In fact, it derives from old measurements, it does not consider significant differences among other populations, it indicates only an average value of risk (not individual variability), and it does not adequately account for severe abnormalities of risk factors (eg, severe hypercholesterolemia or hypertension or heavy smoking), leading to an underestimation of global cardiovascular risk.
Recently, concerns have been raised about implementation of Framingham Risk Score in European populations Observational studies performed in Italy (2000), Denmark (2002) and Germany (2003) have clearly demonstrated that Framingham risk function overestimates coronary risk in European populations, due to a definition of nonfatal endpoints used in Framingham that is different from than in other cohort studies and clinical trials, and mostly to the objective difficulty in using local data to adjust the model for the use in individual European countries (Haq et al 1999; Menotti et al 2002; Thomsen et al 2002). In view of these evidence, European Society of Cardiology have carried out the Systematic COronary Risk Evaluation (SCORE) project (Conroy et al 2003) for the estimation of the 10-year risk of fatal cardiovascular disease in Europe, as reported in Figure 3 (Panel A and B). The SCORE risk predictor system introduces several differences with respect to the Framingham Risk Score. First of all, it considers the total cardiovascular mortality rather than total cardiovascular events as the primary endpoint, including all atherosclerotic deaths (coronary artery diseases and cerebrovascular diseases). Total cardiovascular risk gives a better estimate of individual risk, since noncoronary cardiovascular diseases represent a greater proportion of whole cardiovascular risk in European regions with low coronary artery disease. Secondly, it separates charts for lower (Belgium, France, Greece, Italy, Luxemburg, Spain, Switzerland, Portugal) and higher (United Kingdom, Sweden, Scotland, and other European regions) risk areas of Europe. These charts does not consider different algorithms for diabetic patients, in view of the facts that type 2 diabetes is associated per se with a 2-fold risk for men and 4-fold additive risk for women, determining itself an high-risk profile, as also highlighted in the most recent guidelines (ESH/ESC 2003).
Figure 3.
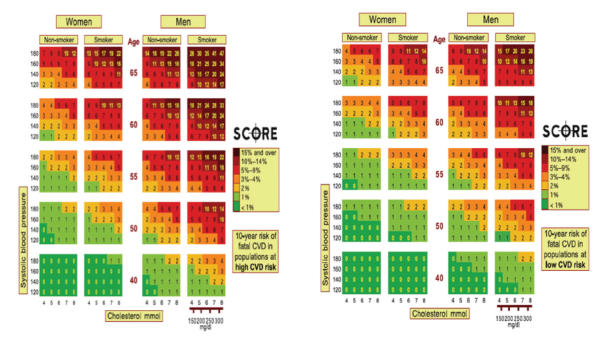
Risk charts in high risk and low risk populations, according to the SCORE Project. Copyright © 2003. Conroy RM, Pyorala K, Fitzgerald AP, et al for the SCORE project group. 2003. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 24:987Z 1003.
According to the SCORE, the definition of high total risk for developing a fatal cardiovascular events is represented by: 1) patients with established cardiovascular disease; 2) asymptomatic subjects who have: multiple risk factors resulting in a 10 year risk more than 5% now or if extrapolated to age 60 years, or markedly raised levels of single risk factors; 3) total cholesterol more than 320 mg/dl, LDL cholesterol more than 240 mg/dl, blood pressure more than 180/110 mmHg; 4) diabetes type 2 and diabetes type 1 with microalbuminuria. It is of note that total cardiovascular risk may also be higher than indicated in the chart in the following settings: a) in subjects approach the next age category; b) in asymptomatic subjects with preclinical evidence of atherosclerosis (eg, computerized tomography or ultrasonography); c) in subjects with a strong family history of premature cardiovascular disease; d) in subjects with low HDL cholesterol levels, with raised triglyceride levels, with impaired glucose tolerance, and with raised levels of C-reactive protein, homocysteine, apolipoprotein B or Lp(a); e) in obese and sedentary subjects.
After risk assessment: How to manage global risk?
Strict application of these recommendations should never replace the good clinical practice and personal experience of physicians, which should base their decisions on the evidence-based medicine, rather than simple application of risk calculator. In fact, most hypertension-related deaths come from patients with only modestly raised blood pressure, simply because they are so much more numerous. The same principles apply both to cholesterol and to total risk.
Multiple drug regimens to control risk are generally difficult to maintain and may be less practical and effective than an integrated approach to multiple risk targets by mixing antihypertensive drugs and other risk-lowering interventions, such as lipid-lowering agents and aspirin.
Within the therapeutic strategy of the management of hypertension, especially in patients with concomitant risk factors, target organ damage or co-morbidities (left ventricular hypertrophy, microalbuminuria, atherosclerosis, left ventricular dysfunction, ischemic heart or cerebral disease and nephropathy), there is growing evidence supporting the use of newer antihypertensive drugs, such as those inhibiting the renin-angiotensin system (ACE Inhibitors or Angiotensin Receptor Blockers [ARB]) (Ruilope et al 2005). The beneficial effects of antihypertensive regimens, mostly based on ARBs, do not seem to be exclusively linked to the documented blood pressure lowering effect of these compounds, and therefore they have been at least partially attributed to other mechanisms (Volpe et al 2005). In addition, clinical research from prospective trials strongly support the benefit of using a lipid-lowering regimen in hypertensive patients, including those with other cardiovascular risk factors, even in patients who might not be candidates for such treatment, according to current guidelines on lipid-lowering treatment (Volpe et al 2005).
Conclusions
In conclusion, it is more appropriate to consider the global risk in arriving at decisions regarding clinical management of high-risk patients. In the modern strategies aimed at reducing global burden of cardiovascular disease, the overall risk reduction should represent the goal in the clinical practice, which is best achieved by establishing global risk profile, identifying modifiable components of risk, and then starting the most effective and tolerable therapeutic strategy. Recent evidence strongly support a more comprehensive strategy aimed at reducing all the components of the global cardiovascular risk rather than the level of each risk factor. In the clinical practice, this approach has been demonstrated to significantly reduce the global burden of disease in hypertensive patients at high risk (NCEP 2003). In this regard, it is important to define the global cardiovascular risk threshold to manage patients at high-risk, rather than to focus on the high level of a single risk factor, for achieving effective control of cardiovascular risk profile and reducing cardiovascular morbidity and mortality in the general population, as well as in hypertensive population.
References
- [ADA] American Diabetes Association. Hypertension management in adults with diabetes. Diabetes Care. 2004;27:S65–S67. doi: 10.2337/diacare.27.2007.s65. [DOI] [PubMed] [Google Scholar]
- Anderson KM, Odell PM, Wilson PW, et al. Cardiovascular disease risk profiles. Am Heart J. 1991;121(1 Pt 2):293–8. doi: 10.1016/0002-8703(91)90861-b. [DOI] [PubMed] [Google Scholar]
- Alderman MH, Furberg CD, Kostis JB, et al. Hypertension guidelines: criteria that might make them more clinically useful. Am J Hypertens. 2002;15(10 Pt 1):917–23. doi: 10.1016/s0895-7061(02)03001-7. [DOI] [PubMed] [Google Scholar]
- [ALLHAT] Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker versus diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) JAMA. 2002;288:2981–97. doi: 10.1001/jama.288.23.2981. [DOI] [PubMed] [Google Scholar]
- Andersson OK, Almgren T, Persson B, et al. Survival in treated hypertension: follow up study after two decades. Brit Med J. 1998;317:167–71. doi: 10.1136/bmj.317.7152.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [BPLTTC] Blood Pressure Lowering Treatment Trialists’ Collaboration. Effect of Angiotensin-converting enzyme inhibitors, calcium antagonists, and other blood pressure lowering drugs: results of prospectively designed overviews of randomized trials. Lancet. 2000;355:1955–1964. doi: 10.1016/s0140-6736(00)03307-9. [DOI] [PubMed] [Google Scholar]
- Cannon CP, Braunwald E, McCabe CH, et al. for the Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thromolysis in Myocardial Infarction 22 Investigators (PROVE IT-TIMI 22) Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004;350:1495–504. doi: 10.1056/NEJMoa040583. [DOI] [PubMed] [Google Scholar]
- Chobanian A, Bakris G, Black H, et al. The Seventh Report of the Joint National Committee (JNC) on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. JAMA. 2003;289:2560–2571. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- Collins R, Peto R, MacMahon S, et al. Blood pressure, stroke, and coronary heart disease. Part 2, Short-term reductions in blood pressure: overview of randomised drug trials in their epidemiological context. Lancet. 1990;335:827–839. doi: 10.1016/0140-6736(90)90944-z. [DOI] [PubMed] [Google Scholar]
- Conroy RM, Pyorala K, Fitzgerald AP, et al. for the SCORE Project Group. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24:987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]
- Dahlof B, Devereux RB, Kjeldsen SE, et al. for the LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention For End-point reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359:995–1003. doi: 10.1016/S0140-6736(02)08089-3. [DOI] [PubMed] [Google Scholar]
- Dahlof B, Sever PS, Poulter NR, et al. for the ASCOT Investigators. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005;366(9489):895–906. doi: 10.1016/S0140-6736(05)67185-1. [DOI] [PubMed] [Google Scholar]
- [ESH/ESC] European Society of Hypertension/European Society of Cardiology. European Society of Hypertension (ESH)/European Society of Cardiology (ESC) guidelines for the management of arterial hypertension. J Hypertens. 2003;21:1011–1053. doi: 10.1097/00004872-200306000-00001. [DOI] [PubMed] [Google Scholar]
- Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348:383–93. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]
- Grundy SM, Balady GJ, Criqui MH, et al. American Heart Association. Primary prevention of coronary heart disease: guidance from Framingham: a statement for healthcare professionals from the AHA Task Force on Risk Reduction. Circulation. 1998;97:1876–87. doi: 10.1161/01.cir.97.18.1876. [DOI] [PubMed] [Google Scholar]
- Grundy SM, Pasternak R, Greenland P, et al. Assessment of Cardiovascular Risk by use of multiple-risk-factor assessment equations. A Statement for Healthcare Professional from the American Heart Association and the American College of Cardiology. J Am Coll Cardiol. 1999;34:1348–59. doi: 10.1016/s0735-1097(99)00387-3. [DOI] [PubMed] [Google Scholar]
- Hansson L, Zanchetti A, Carruthers SG, et al. for the HOT Study Group. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet. 1998;351:1755–1762. doi: 10.1016/s0140-6736(98)04311-6. [DOI] [PubMed] [Google Scholar]
- Haq IU, Ramsay LE, Yeo WW, et al. Is the Framingham risk function valid for northern European populations? A comparison of methods for estimating absolute coronary risk in high-risk men. Heart. 1999;81:40–6. doi: 10.1136/hrt.81.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [HDFPCG] Hypertension Detection and Follow-up Program Cooperative Group. Five-year findings of the hypertension detection and follow-up program. Reduction in mortality of persons with high blood pressure, including mild hypertension. Hypertension Detection and Follow-up Program Cooperative Group. JAMA. 1979;242:2562–71. [PubMed] [Google Scholar]
- [HPS] Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20 536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–22. [Google Scholar]
- Julius S, Kjeldsen SE, Weber M, et al. for the VALUE Trial Group. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the Valsartan Antihypertensive Long-term Use Evaluation (VALUE) randomised trial. Lancet. 2004;363:2022–31. doi: 10.1016/S0140-6736(04)16451-9. [DOI] [PubMed] [Google Scholar]
- Kannel WB. Risk stratification in hypertension: new insights from the Framingham Study. Am J Hypertens. 2000;13(1 Pt 2):3S–10S. doi: 10.1016/s0895-7061(99)00252-6. [DOI] [PubMed] [Google Scholar]
- LaRosa JC, Grundy SM, Waters DP, et al. for the Treating to New Targets (TNT) Investigators. Intensive Lipid Lowering with Atorvastatin in Patients with Stable Coronary Disease. N Engl J Med. 2005;352:1425–35. doi: 10.1056/NEJMoa050461. [DOI] [PubMed] [Google Scholar]
- Lewington S, Clarke R, Qizilbash N, et al. for the Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- Libby P. The forgotten majority. Unfinished business in cardiovascular risk reductionJ. Am Coll Cardiol. 2005;46:1225–8. doi: 10.1016/j.jacc.2005.07.006. [DOI] [PubMed] [Google Scholar]
- MacMahon S, Peto R, Cutler J, et al. Blood pressure, stroke, and coronary heart disease Part 1, Prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet. 1990;335:765–774. doi: 10.1016/0140-6736(90)90878-9. [DOI] [PubMed] [Google Scholar]
- Mancia G, Sega R, Milanesi C, et al. Blood pressure control in the hypertensive population. Lancet. 1997;349:454–7. doi: 10.1016/s0140-6736(96)07099-7. [DOI] [PubMed] [Google Scholar]
- Menotti A, Puddu PE, Lanti M. Comparison of the Framingham risk function-based coronary chart with risk function from an Italian population study. Eur Heart J. 2000;21:365–70. doi: 10.1053/euhj.1999.1864. [DOI] [PubMed] [Google Scholar]
- [NCEP] National Cholesterol Education Program. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). Final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- Ruilope LM, Rosei EA, Bakris GL, et al. Angiotensin receptor blockers: therapeutic targets and cardiovascular protection. Blood Press. 2005;14(4):196–209. doi: 10.1080/08037050500230227. [DOI] [PubMed] [Google Scholar]
- Sever PS, Dahlof B, Poulter NR, et al. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm (ASCOT-LLA): A multicentre randomised controlled trial. Lancet. 2003;361:1149–58. doi: 10.1016/S0140-6736(03)12948-0. [DOI] [PubMed] [Google Scholar]
- Stamler J, Wentworth D, Neaton JD. Is the relationship between serum cholesterol and risk of premature death from coronary heart disease continuous and graded? Findings in 356.222 primary screeners of the Multiple Risk Factor Intervention Trial (MRFIT) JAMA. 1986;256:2823–2828. [PubMed] [Google Scholar]
- [PROGRESS] The Perindopril pROtection aGainst REcurrent Stroke Study Collaborative Group. Randomized trial of perindopril-based blood-pressure-lowering regimen among 6105 individuals with previous stroke or transient ischemic attack. Lancet. 2001;358:1033–1041. doi: 10.1016/S0140-6736(01)06178-5. [DOI] [PubMed] [Google Scholar]
- Thomsen TF, McGee D, Davidsen M, et al. A cross-validation of risk-scores for coronary heart disease mortality based on data from the Glostrup Population Studies and Framingham Heart Study. Int J Epidemiol. 2002;31:817–22. doi: 10.1093/ije/31.4.817. [DOI] [PubMed] [Google Scholar]
- [UKPDS] United Kingdom Prospective Diabetes Study Group. Tight Blood Pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS38. Brit Med J. 1998;317:703–713. [PMC free article] [PubMed] [Google Scholar]
- Van den Hoogen PC, Feskens EJ, Nagelkerke NJ, et al. The relation between blood pressure and mortality due to coronary heart disease among men in different parts of the world. Seven Countries Study Research Group. N Engl J Med. 2000;342:1–8. doi: 10.1056/NEJM200001063420101. [DOI] [PubMed] [Google Scholar]
- Vasan RS, Larson MG, Leip EP, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001;345(18):1291–7. doi: 10.1056/NEJMoa003417. [DOI] [PubMed] [Google Scholar]
- Volpe M, Alderman MH, Furberg CD, et al. Beyond hypertension toward guidelines for cardiovascular risk reduction. Am J Hypertens. 2004;17(11 Pt 1):1068–74. doi: 10.1016/j.amjhyper.2004.06.017. [DOI] [PubMed] [Google Scholar]
- Volpe M, Ruilope LM, McInnes GT, et al. Angiotensin-II receptor blockers: benefits beyond blood pressure reduction? J Hum Hypertens. 2005;19:331–9. doi: 10.1038/sj.jhh.1001831. [DOI] [PubMed] [Google Scholar]
- Wolf-Maier K, Cooper RS, Banegas JR, et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA. 2003;289:2363–9. doi: 10.1001/jama.289.18.2363. [DOI] [PubMed] [Google Scholar]
- [WHO/ISH] World Health Organization/International Society of Hypertension. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21:1983–1992. doi: 10.1097/00004872-200311000-00002. [DOI] [PubMed] [Google Scholar]
- Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- Yusuf S, Sleight P, Dagenais G, et al. for the Hearth Outcomes Prevention Evaluation (HOPE) Study Group. Effects of angiotensin-converting enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2002;342:145–53. doi: 10.1056/NEJM200001203420301. [DOI] [PubMed] [Google Scholar]


