Abstract
OBJECTIVE
Intrauterine devices (IUDs) for contraception are used infrequently in Canada despite their well-studied safety and efficacy. The purpose of this study was to investigate FPs’ perceptions of the risks of and indications for using IUDs, as these perceptions might be a key factor in why IUDs are underused.
DESIGN
Mailed survey.
SETTING
Kingston, a midsized city in Ontario.
PARTICIPANTS
All FPs practising in Kingston.
MAIN OUTCOME MEASURES
The primary outcome was the proportion of FPs who ranked the importance of risks of and contraindications to using IUDs in keeping with rankings in established clinical guidelines. Secondary outcomes were FP IUD prescription and insertion patterns, their perceptions of patients’ access to physicians who insert IUDs, and their interest in a course on IUD insertion.
RESULTS
Response rate was 81%. Contrary to the evidence, more than 60% of FPs thought pelvic inflammatory disease and ectopic pregnancy were major risks, and nearly half thought failure of IUDs was a major risk. Fewer than one-third would recommend IUDs as an option for nulliparous women, for postcoital contraception, for women with moderate-sized fibroids, or for women with pelvic inflammatory disease during the last year, though none of these are contraindications according to established clinical guidelines. About 82% of FPs prescribed IUDs, and 41% inserted them. Newer graduates were more likely than older graduates to prescribe only levonorgestrel IUDs (36% vs 8%). About 93% of survey respondents reported that patients’ access to physicians who insert IUDs was not a factor in recommendingIUDs to them.
CONCLUSION
A substantial proportion of surveyed FPs believed that the side effects of IUDs were more severe than is supported by clinical guidelines and were misinformed about the range of women who could benefit from IUDs. These misconceptions likely contribute to the low rate of IUD use in Canada.
RÉSUMÉ
OBJECTIF
Au Canada, le stérilet est peu souvent utilisé pour la contraception malgré les études démontrant clairement son efficacité et sa sécurité. Cette étude voulait connaître les perceptions qu’ont les MF des risques et indications du stérilet, puisque cela pourrait être un facteur clé expliquant sa sous-utilisation.
TYPE D’ÉTUDE
Enquête postale.
CONTEXTE
Kingston, une ville de moyenne dimension en Ontario.
PARTICIPANTS
Tous les MF pratiquant à Kingston.
PRINCIPAUX PARAMÈTRES À L’ÉTUDE
Le principal paramètre étudié était la proportion des MF qui évaluaient l’importance des risques et contre-indications du stérilet conformément à ce qu’indiquent les directives cliniques reconnues. Les paramètres secondaires étaient les modèles de prescription et d’installation du stérilet par les MF, leur perceptions concernant l’accessibilité des patients aux médecins qui les installent et leur intérêt pour un cours sur l’installation des stérilets.
RÉSULTATS
Le taux de réponse était de 81%. Contrairement aux données probantes, plus de 60% des MF pensaient que les maladies inflammatoires pelviennes et les grossesses ectopiques constituaient des risques majeurs, et près de la moitié pensaient que son inefficacité était un risque important. Moins d’un tiers recommanderaient le stérilet pour les nullipares, pour la contraception postcoïtale, pour celles qui ont des fibromes de dimension moyenne ou qui ont présenté une maladie inflammatoire pelvienne durant l’année précédente, même si aucune de ces situations ne constitue une contre-indication d’après les directives de pratique reconnues. Environ 82% des MF prescrivaient des stérilets et 41% les installaient. Les nouveaux diplômés étaient plus susceptibles que les autres de prescrire uniquement des stérilets au levonorgestrel (36% vs 8%). Environ 93% des répondants déclaraient que l’accès des patientes à un médecin qui installait des stérilets n’intervenait pas dans la décision de recommander le stérilet.
CONCLUSION
Une importante proportion des répondants jugeaient les effets indésirables du stérilet plus sévères que ce que les directives de pratique indiquent et étaient mal renseignés sur le type de patientes susceptibles de profiter du stérilet. Ces fausses perceptions contribuent vraisemblablement au faible taux d’utilisation du stérilet au Canada.
Intrauterine devices (IUDs) are an effective, safe, and reversible method of contraception supported by a growing body of evidence.1 They have been used by more than 100 million women worldwide.2 Two types of IUDs are available in Canada: copper IUDs (Nova-T and Flexi-T 300), and the levonorgestrel-releasing system (LNG-IUS), Mirena. Both have failure rates comparable to those of tubal ligation, and women return to normal fertility immediately after removal.3 Intrauterine devices do not increase risk of ectopic pregnancy (they primarily prevent fertilization) or pelvic inflammatory disease (PID) (rates of both of these are similar to rates in the general population), so are safe even for young, nulliparous women.2 They do not interfere with breastfeeding and can be inserted immediately after abortion or vaginal delivery, though risk of expulsion and perforation is lower if insertion is delayed by 4 weeks.2 Moderate-sized fibroids do not interfere with the efficacy of IUDs. Copper IUDs are effective as postcoital contraception for up to 7 days after intercourse.2 Copper IUDs might increase menstrual bleeding and cramping,4,5 and the LNG-IUS often causes oligomenorrhea6–10 and is increasingly being used instead of surgery for women with menorrhagia11,12 (Table 1). Intrauterine devices are effective for 5 years, and at $80 and $360, respectively, over time are the cheapest medical contraceptives except for surgery.3
Table 1.
Indications for and contraindications to use of IUDs
| INDICATIONS | CONTRAINDICATIONS |
|---|---|
| Multiparous and nulliparous women seeking reliable, reversible, coitally independent contraception | Pregnancy |
| Women seeking long-term contraception or a contraception method requiring less compliance | Current or recent (past 3 mo) pelvic inflammatory disease or sexually transmitted infection |
| Women with contraindications or sensitivities to estrogen (eg, women with thromboembolisms or migraines) | Cervical or endometrial cancer, malignant trophoblastic disease |
| Women who are breastfeeding | Severely distorted uterine cavity |
| Copper IUDs: postcoital contraception up to 7 days and women with current breast cancer or liver disease | Undiagnosed vaginal bleeding |
| Copper IUDs: women with human immunovirus infection | Allergy to copper |
| LNG-IUS: women with menorrhagia, dysmenorrhea, or bleeding disorders | Puerperal or postabortion sepsis |
Despite their well-accepted safety and efficacy, in North America, fewer than 1% of women use IUDs.2 The history of IUDs likely plays a role in their low use. They became popular in the 1960s and were used by up to 11% of American women using contraception. In the 1970s, however, reports of septic abortions and PID with the Dalkon Shield led to a class action suit, and all but 1 IUD were withdrawn from the market.1 (Studies have shown that the problems with the Dalkon Shield were unique to its design.13) Despite the safety of modern IUDs, a 2002 study looking at information in current medical textbooks found that the advantages of IUDs were under-represented and disadvantages exaggerated. For example, 9 of 13 American textbooks studied reported that using IUDs led to increased risk of PID, and 6 reported that use of IUDs led to increased risk of ectopic pregnancy. Most textbooks implied that use of IUDs should be a last resort.14
It is important for women to be well informed of their contraceptive options. In a Dutch study, women reported that their FPs were their most important source of information when they were making decisions regarding contraception.15 A few studies have looked at how many and to which patients FPs recommend IUDs. A 1990 American survey on copper IUDs found that only 17% of physicians, mostly gynecologists, were inserting IUDs and that 40% of physicians did not recommend IUDs owing to concerns about liability, safety, expense to patients, or failure necessitating abortion.16 An Australian study in 1994 found that 29% of physicians only discussed IUDs if specifically asked about them.17 A recent Dutch survey found that FPs mostly recommended IUDs to older, married or cohabiting patients with children. Urban physicians were more likely than their rural counterparts to recommend IUDs to young, nulliparous women.18 Women look to their FPs for information on contraception, and it would be unfortunate if FPs’ lack of awareness of the safety of IUDs is preventing women from knowing that IUDs are a valid option. We decided to investigate FPs’ misconceptions about IUDs to provide insight into how large a role they play in the low rate of IUD use in Canada.
Research objectives
The primary objective of the study was to determine the current perceptions of FPs in one Canadian city regarding the risks of and contraindications to using IUDs and how these perceptions compared with information in established clinical guidelines. Secondary objectives were to determine how many FPs prescribed and inserted IUDs and which types of IUDs they preferred, FPs’ perceptions as to whether access to physicians who insert IUDs was a deterrent to IUD prescription, and FPs’ interest in a course on IUD insertion.
METHOD
The survey was conducted in Kingston, Ont, a city of 150 000. It was approved by the Queen’s University Research Ethics Board in Kingston. A draft of the survey was pilot-tested on a group of residents and reviewed by 2 FPs. All FPs in the city were mailed a survey, a cover letter, and a postage-paid, addressed return envelope. A second survey was mailed to all nonrespondents 1 month later, then a third 2 months later in spring 2006. The first 2 mailings included the incentive of a draw for a gift certificate, and certificates for coffee were sent with the final mailing. Only physicians who were deceased or had moved were excluded. Data were compiled using numerical identifiers to ensure anonymity.
The survey had 3 parts: questions on physicians’ characteristics, questions on their perceptions of the risks associated with use of IUDs, and questions on indications for use of IUDs. Information on physicians included demographics: sex, age, and years in practice. Respondents were asked if they prescribed or inserted IUDs, and which types. They were asked whether access to physicians who insert IUDs affected how often they recommended IUDs to patients and whether they would attend a course to increase their skill at insertion, if offered. The effect of sex and years in practice on prescription and insertion patterns was analyzed using χ2 tests with P <.05 considered significant.
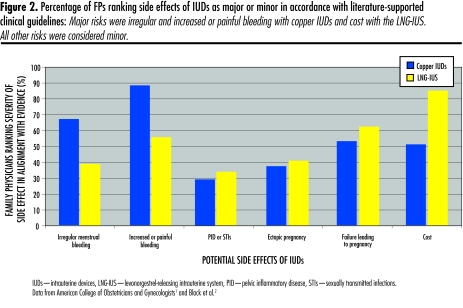
In the second part of the survey, FPs were asked to rank as major, intermediate, minor, or insignificant the risks associated with both copper IUDs and the LNG-IUS: irregular menstrual bleeding, increased or painful menstrual bleeding, amenorrhea, PID or sexually transmitted infections, ectopic pregnancy, failure leading to pregnancy, and cost. For ease of analysis, responses were grouped into major (major, intermediate) and minor (minor, insignificant). Responses were compared with the ranking of risks reported in recent practice guidelines from the Canadian and American societies of obstetrics and gynecology.1,2 These guidelines considered irregular and increased or painful bleeding with copper IUDs and the cost of the LNG-IUS to be major risks. All other risks were described as minor in both guidelines.
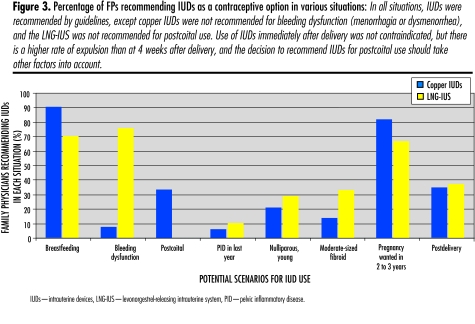
Family physicians were asked whether they would recommend either type of IUD as an option in 8 situations: breastfeeding; menorrhagia or dysmenorrhea; postcoital contraception; PID during the last year; young, nulliparous women; immediately after abortion or vaginal delivery; women hoping to conceive in 2 to 3 years; and women with moderate-sized fibroids. Again, responses were compared with information in clinical guidelines. Except for recommending copper IUDs for menorrhagia or dysmenorrhea and the LNG-IUS for postcoital contraception, all situations were appropriate for IUD use according to the guidelines (Table 1).
RESULTS
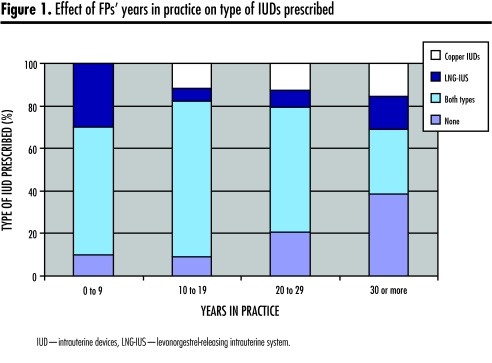
Of 131 surveys mailed, 12 were undeliverable because FPs had moved or died. A total of 96 active FPs (81%) responded to the survey. Among these, 56% were women, and 89% had practised for 10 or more years (Table 2). About 82% of respondents prescribed IUDs, and 41% inserted them; 57% prescribed both types of IUDs, 11% prescribed only the LNG-IUS, and 14% prescribed only copper IUDs. Family physicians in practice 0 to 9 years were more likely than those in practice longer to prescribe only the LNG-IUS (36% vs 8%, P = .037) (Figure 1). Women physicians were more likely than men to prescribe (89% vs 74%) and insert (43% vs 38%) IUDs, but this difference was not statistically significant (P = .06, P = .66). Only 7% of respondents thought access to physicians who insert IUDs was a consideration for whether they would recommend IUDs. About 50% reported being definitely or possibly interested in a course on IUD insertion.
Table 2.
Participants’ prescription, insertion, and referral patterns for intrauterine devices (IUDs) in relation to their sex and number of years in practice: N = 96.
| YEARS IN PRACTICE
|
SEX
|
||||||
|---|---|---|---|---|---|---|---|
| PATTERNS* | 0–9 N = 11 | 10–19 N = 38 | 20–29 N = 33 | 30 OR MORE N = 14 | MALE N = 42 | FEMALE N = 54 | TOTAL |
| Prescribe IUDs | |||||||
| • Yes | 10 | 34 | 26 | 9 | 31 | 48 | 79 |
| • No | 1 | 4 | 7 | 5 | 11 | 6 | 17 |
| Insert IUDs | |||||||
| • Yes | 3 | 20 | 11 | 5 | 16 | 23 | 39 |
| • No | 8 | 18 | 22 | 9 | 26 | 31 | 57 |
| Thought that access to physicians who insert IUDs was a problem | |||||||
| • Yes | 0 | 3 | 2 | 1 | 2 | 4 | 6 |
| • No | 10 | 26 | 24 | 12 | 32 | 40 | 72 |
| • Maybe | 0 | 0 | 3 | 0 | 1 | 2 | 3 |
| Interested in a course on IUD insertion | |||||||
| • Yes | 4 | 8 | 6 | 0 | 5 | 13 | 18 |
| • No | 5 | 16 | 17 | 8 | 22 | 24 | 46 |
| • Maybe | 2 | 10 | 6 | 6 | 12 | 15 | 27 |
Totals for all patterns do not equal N value in each category owing to lack of response.
Figure 1.
Effect of FPs’ years in practice on type of IUDs prescribed
More than 60% of respondents ranked ectopic pregnancy and PID as major risks of IUDs, and 47% and 38% thought there was major risk of failure with copper IUDs and the LNG-IUS, respectively (Figure 2). About 45% thought increased or painful bleeding was a major risk of the LNG-IUS. Only in the 3 categories classified as major risks—irregular bleeding, increased or painful bleeding with copper IUDs, and cost of the LNG-IUS—were at least two-thirds of respondents in keeping with clinical guidelines.
Figure 2.
Percentage of FPs ranking side effects of IUDs as major or minor in accordance with literature-supported clinical guidelines: Major risks were irregular and increased or painful bleeding with copper IUDs and cost with the LNG-IUS. All other risks were considered minor.
With regard to indications for IUDs, most respondents would not recommend them to nulliparous women (79% would not recommend copper IUDs, and 71% would not recommend the LNG-IUS), for postcoital contraception (67% would not recommend copper IUDs), for patients with moderate-sized fibroids (87% would not recommend copper IUDs, and 68% would not recommend the LNG-IUS), or for patients with PID during the last year (94% would not recommend copper IUDs, and 90% would not recommend the LNG-IUS). Immediately after abortion or vaginal delivery, only 35% and 36% would recommend copper IUDs and the LNG-IUS, respectively. In all these conditions, clinical guidelines support the safety of IUDs (Figure 3).
Figure 3.
Percentage of FPs recommending IUDs as a contraceptive option in various situations: In all situations, IUDs were recommended by guidelines, except copper IUDs were not recommended for bleeding dysfunction (menorrhagia or dysmenorrhea), and the LNG-IUS was not recommended for postcoital use. Use of IUDs immediately after delivery was not contraindicated, but there is a higher rate of expulsion than at 4 weeks after delivery, and the decision to recommend IUDs for postcoital use should take other factors into account.
DISCUSSION
This is the first study to quantify Canadian FPs’ misconceptions about IUDs. Results of this study show the gap between FPs’ perceptions of the risks of and indications for use of IUDs and those described in established clinical guidelines. Despite guidelines describing the safety of IUDs, PID and ectopic pregnancy were ranked as major risks by more than 60% of surveyed FPs. Even with an efficacy similar to that of tubal ligation,3 between 38% and 47% of respondents still thought failure was a major risk. The LNG-IUS is increasingly recommended as a treatment for menorrhagia and dysmenorrhea,11,12 yet 46% of FPs thought increased or painful bleeding was a major risk of the device. Though not contraindicated in clinical guidelines, more than two-thirds of respondents said they would not recommend IUDs to nulliparous women, women with moderate-sized fibroids, or women with PID during the last year. Even though postcoital contraception is listed as an indication for copper IUDs owing to their low failure rate when used within 7 days of intercourse,2 fewer than two-thirds of respondents would recommend them. These findings were in keeping with a 2002 study of American medical textbooks, where 9 of 13 textbooks reported that IUDs increase the risk of PID, and 6 of 13 reported that ectopic pregnancy was a risk.14
Investigating whether access to physicians willing to insert IUDs was a factor in the low use of IUDs in Canada, we found that 82% of respondents prescribed IUDs, and 41% inserted them. Few recent studies indicate the number of FPs inserting IUDs for comparison. One study in 1990 found that about 17% inserted them.16 Despite our findings, only 7% of respondents thought that access to physicians willing to insert IUDs was a factor in whether they would recommend IUDs to patients.
There was a significant difference in type of IUD used by younger and older practitioners. Younger FPs (in practice 0 to 9 years) preferred the LNG-IUS, with 36% prescribing only this type (versus 8% of older practitioners), and none prescribing only copper IUDs. The LNG-IUS is the more appropriate IUD in certain situations as it decreases menstrual cramping and bleeding. The LNG-IUS is newer (approved in the United States in 2000), and it is possible that younger FPs were completing residency while the LNG-IUS was on the market. There was some interest in more training in use of IUDs; 50% of respondents indicated a possible or definite interest in a course on IUD insertion. This suggested that they knew they needed further training in insertion, but whether or not they were also aware of the need for education in the risks of and indications for use of IUDs was not addressed.
Limitations and strengths
Conducting the study in a single city might have limited the degree to which findings can be generalized. A Dutch study, however, found urban physicians were more likely to prescribe IUDs to young, nulliparous women than rural ones were,18 so misconceptions might be even more widespread in rural Canada. One survey question asked respondents to rank risks from major to insignificant, and this might have been interpreted either as a measure of severity or as a rate of incidence. It was analyzed as a combination of the 2 (see Method). The study was strengthened by the high response rate of 81% of all FPs in the city. This was likely due to the many mailings, gift certificate incentives, and perhaps because both investigators were residents of the city asking for FPs’ participation for educational purposes. The 19% who did not respond might have been less interested in IUDs and less well informed, and their responses might have supported our conclusions. Family physicians’ perceptions were compared with opinions expressed in 2 well established guidelines, which we found to be in keeping with opinions found in an extensive literature search on the safety of IUDs. We found no literature questioning the validity of the guidelines. Finally, the breadth of the survey questions allowed a thorough picture of FPs’ perceptions of IUDs to emerge.
Conclusion
Our findings are relevant to FPs, medical educators, and patients seeking accurate information. The study quantifies FPs’ substantial misconceptions about IUDs, such as their association with risk of PID and ectopic pregnancy and their failure rates. Results of this study point to areas where education is needed, both for FPs in practice and residents currently in training. Further research into patients’ perceptions of IUDs and other potential barriers to use, such as access to physicians willing to insert IUDs, is needed.
EDITOR’S KEY POINTS
Despite their well-accepted safety and efficacy, intrauterine devices (IUDs) are used by fewer than 1% of women in North America. An American survey found that only 17% of physicians, mostly gynecologists, were inserting copper IUDs and that 40% of physicians did not recommend IUDs to patients.
This study presents the perceptions of FPs in one Canadian city regarding the risks of and contraindications to use of IUDs, and looks at whether these perceptions are in keeping with clinical guidelines.
Results of the study showed that 82% of respondents prescribed IUDs, and 41% inserted them. They also showed the gap between FPs’ perceptions of the risks of and indications for IUDs, and actual risks and indications as described in established clinical guidelines. Despite guidelines describing the safety of IUDs, pelvic inflammatory disease and ectopic pregnancy were incorrectly ranked as major risks by more than 60% of surveyed physicians.
POINTS DE REPÈRE DU RÉDACTEUR
Même si les stérilets sont reconnus sécuritaires et efficaces, moins de 1% des femmes les utilisent en Amérique du Nord. Une enquête américaine a révélé que seulement 17% des médecins, principalement des gynécologues, installaient des stérilets de cuivre et que 40% des médecins ne conseillaient pas le stérilet à leurs patientes.
Cette étude présente l’opinion de MF d’une ville canadienne sur les risques et contre-indications du stérilet, et évalue si ces perceptions sont conformes aux directives cliniques.
Les résultats de cette étude montrent que 82% des répondants prescrivaient des stérilets et que 41% les installaient. Ils illustrent aussi la disparité qui existe entre la perception qu’ont les MF des risques et indications des stérilets et les véritables risques et indications décrits dans les directives de pratique reconnues. Même si les directives confirment la sécurité du stérilet, plus de 60% des répondants estimaient à tort que les maladies inflammatoires pelviennes et les grossesses ectopiques constituaient des risques majeurs.
Footnotes
Contributors
Drs Stubbs and Schamp contributed equally to concept and design of the study; to gathering, analysis, and interpretation of data; and to preparing the manuscript for submission.
Competing interests
None declared
This article has been peer reviewed.
References
- 1.American College of Obstetricians and Gynecologists Committee on Practice Bulletins—Gynecology. Clinical management guidelines for obstetrician-gynecologists. Number 59, January 2005. Intrauterine device. Obstet Gynecol. 2005;105(1):223–32. doi: 10.1097/00006250-200501000-00060. [DOI] [PubMed] [Google Scholar]
- 2.Black A, Francoeur D, Rowe T, Collins J, Miller D, Brown T, et al. SOGC clinical practice guidelines: Canadian contraception consensus. J Obstet Gynaecol Can. 2004;26(3):219–96. [PubMed] [Google Scholar]
- 3.Andersson K, Odlind V, Rybo G. Levonorgestrel-releasing and copper-releasing (Nova-T) IUDs during five years of use: a randomized comparative trial. Contraception. 1994;49(1):56–72. doi: 10.1016/0010-7824(94)90109-0. [DOI] [PubMed] [Google Scholar]
- 4.Milsom I, Andersson K, Jonasson K, Lindstedt G, Rybo G. The influence of the Gyne-T 380S IUD on menstrual blood loss and iron status. Contraception. 1995;52(3):175–9. doi: 10.1016/0010-7824(95)00163-5. [DOI] [PubMed] [Google Scholar]
- 5.Larsson G, Milsom I, Jonasson K, Lindstedt G, Rybo G. The long-term effects of copper surface area on menstrual blood loss and iron status in women fitted with an IUD. Contraception. 1993;48(5):471–80. doi: 10.1016/0010-7824(93)90136-u. [DOI] [PubMed] [Google Scholar]
- 6.Andersson JK, Rybo G. Levonorgestrel-releasing intrauterine device in the treatment of menorrhagia. Br J Obstet Gynaecol. 1997;97(8):690–4. doi: 10.1111/j.1471-0528.1990.tb16240.x. [DOI] [PubMed] [Google Scholar]
- 7.Barrington JW, Bowens-Simpkins P. The levonorgestrel intrauterine system in the management of menorrhagia. Br J Obstet Gynaecol. 1997;104(5):614–6. doi: 10.1111/j.1471-0528.1997.tb11542.x. [DOI] [PubMed] [Google Scholar]
- 8.Irvine GA, Campbell-Brown MB, Lumsden MA, Heikkila A, Walker JJ, Cameron IT. Randomised comparative trial of the levonorgestrel intrauterine system and norethisterone for treatment of idiopathic menorrhagia. Br J Obstet Gynaecol. 1998;105(6):592–8. doi: 10.1111/j.1471-0528.1998.tb10172.x. [DOI] [PubMed] [Google Scholar]
- 9.Istre O, Trolle B. Treatment of menorrhagia with the levonorgestrel intrauterine system versus endometrial resection. Fertil Steril. 2001;76(2):304–9. doi: 10.1016/s0015-0282(01)01909-4. [DOI] [PubMed] [Google Scholar]
- 10.Lethaby A, Cooke I, Rees M. Progesterone or progestogen-releasing intrauterine systems for heavy menstrual bleeding. Cochrane Database Syt Rev. 2005;(4):CD002126. doi: 10.1002/14651858.CD002126.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Hurskainen R, Teperi J, Rissanen P, Aalto A, Grenman S, Kivelä A, et al. Quality of life and cost-effectiveness of levonorgestrel-releasing intrauterine system versus hysterectomy for treatment of menorrhagia: a randomised trial. Lancet. 2001;357(9252):273–7. doi: 10.1016/S0140-6736(00)03615-1. [DOI] [PubMed] [Google Scholar]
- 12.Lähteenmäki P, Haukkamaa M, Puolakka J, Riikonen U, Sainio S, Suvisaari J, et al. Open randomized study of use of levonorgestrel releasing intrauterine system as alternative to hysterectomy. BMJ. 1998;316(7138):1122–6. doi: 10.1136/bmj.316.7138.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sivin I. Another look at the Dalkon Shield: meta-analysis underscores its problems. Contraception. 1993;48(1):1–12. doi: 10.1016/0010-7824(93)90060-k. [DOI] [PubMed] [Google Scholar]
- 14.Espey E, Ogburn T. Perpetuating negative attitudes about the intrauterine device: textbooks lag behind the evidence. Contraception. 2002;65(6):389–95. doi: 10.1016/s0010-7824(02)00307-4. [DOI] [PubMed] [Google Scholar]
- 15.Van Lunsen RH, Arnolds HT, van Maris MG. Choices and changes in contraceptive behaviour; the role of information sources. Patient Educ Couns. 1994;23(3):197–202. doi: 10.1016/0738-3991(94)90035-3. [DOI] [PubMed] [Google Scholar]
- 16.Kooiker CH, Scutchfield FD. Barriers to prescribing the Copper T 380A intrauterine device by physicians. West J Med. 1990;153(3):279–82. [PMC free article] [PubMed] [Google Scholar]
- 17.Weisberg E, Fraser IS, Goss S. The decline in popularity of the intrauterine device. A survey of general practitioner attitudes and practices in New South Wales. Med J Aust. 1994;160(1):19–21. [PubMed] [Google Scholar]
- 18.Vos AG, Veldhuis HM, Lagro-Janssen TL. Intrauterine contraception: the role of general practitioners in four Dutch general practices. Contraception. 2004;69(4):283–7. doi: 10.1016/j.contraception.2003.12.002. [DOI] [PubMed] [Google Scholar]