Abstract
Progress in unravelling the cellular and molecular basis of mammalian circadian regulation over the past decade has provided us with new avenues through which we can explore central nervous system disease. Deteriorations in measurable circadian output parameters, such as sleep/wake deficits and dysregulation of circulating hormone levels, are common features of most central nervous system disorders. At the core of the mammalian circadian system is a complex of molecular oscillations within the hypothalamic suprachiasmatic nucleus. These oscillations are modifiable by afferent signals from the environment, and integrated signals are subsequently conveyed to remote central neural circuits where specific output rhythms are regulated. Mutations in circadian genes in mice can disturb both molecular oscillations and measurable output rhythms. Moreover, systematic analysis of these mutants indicates that they can express an array of abnormal behavioural phenotypes that are intermediate signatures of central nervous system disorders. Furthermore, the response of these mutants to psychoactive drugs suggests that clock genes can modify a number of the brain’s critical neurotransmitter systems. This evidence has led to promising investigations into clock gene polymorphisms in psychiatric disease. Preliminary indications favour the systematic investigation of the contribution of circadian genes to central nervous system disease.
Introduction
The correct functioning of the endogenous circadian clock enables organisms to anticipate daily environmental changes and temporally modify behavioural and physiological functions appropriately. All organisms maintain a large number of physiological variables (sleep-wake cycle, locomotor activity, temperature regulation, water/food intake, and levels of circulating hormones) under control of the circadian clock. There are well-known consequences of disrupted circadian function outside of the brain; metabolism, reproduction, and even longevity can be adversely affected when the means of determining time of day are altered at a molecular level (for review see [1]). Perhaps less has been said regarding the brain and the idea that altered clock function may contribute to neurological, behavioural, and psychiatric deterioration. Here, we explore the contribution of this complex circadian system to brain function in physiological and diseased states. Following a description of the molecular and neural basis of mammalian circadian oscillations and their relationship to brain function, we consider the wider behavioural effects of mutations and ablations of circadian system genes in mice. Furthermore, we explore the persistent observation of rhythm misregulation in psychiatric and neurological disorders and in their related mouse models. Finally, in considering the contribution of circadian regulation to disease symptomatology, we examine the association between clock gene polymorphisms and behavioural traits and disorders in humans. Although sparse, these reports suggest that clock gene misregulation can contribute to the severity of a broad spectrum of central nervous system (CNS) diseases.
Molecular and Neural Basis of Mammalian Circadian Oscillations
The suprachiasmatic nucleus (SCN) of the hypothalamus is the centre for the circadian system in the mammalian brain [2]. Through its neuronal and humoral outputs, the SCN can orchestrate a number of physiological and behavioural rhythms throughout the body. Perhaps surprisingly, these circadian rhythms are not derived from the multicellular network properties of the SCN but are in fact generated at a cell autonomous level. The endogenous clock is fundamentally encoded, at the molecular level, by interlocking autoregulatory transcriptional and translational feedback loops within every cell (see [1],[3] for reviews and Figure 1 for description). The same coordinated molecular circadian rhythms have been identified in a number of cell types, tissues, and organs throughout the body. This observation also applies to a wide range of CNS regions, including the olfactory bulb, pituitary, pineal gland, arcuate nucleus, and retina [4]–[11]. Importantly, it has been established that these rhythms are not externally driven by the output of the SCN, and the time or phase at which particular gene products peak is often region-specific [4],[5].
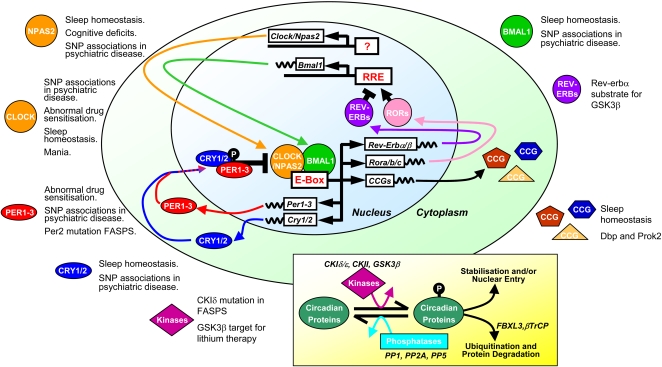
Figure 1. The Mammalian Molecular Circadian Oscillator.
The molecular circadian oscillator incorporates numerous transcriptional and posttranslational elements. Disruptions in many of the individual circadian elements in mice can lead to behavioural disturbances that mirror endophenotypes in human neurological and psychiatric disorders. Moreover, some studies have established circadian gene polymorphisms in psychiatric conditions and mutations in behavioural syndromes (see text for details). The central component of the figure depicts the core mammalian circadian feedback loop. CLOCK(or NPAS2):BMAL1 heterodimers drive the transcription of multiple genes (Cry1/2, Per1-3, Rev-Erba/b, Rora/b/c, multiple CCGs) through E-box elements. Nuclear accumulation of CRY and PER proteins can inhibit CLOCK:BMAL1-mediated transcription by directly interacting with the complex (black bar–ended arrow). As PER and CRY levels fall, the negative repression is lifted and CLOCK:BMAL1-driven transcription re-occurs. In an additional stabilising loop, REV-ERB and ROR proteins co-regulate the transcription of Bmal1 by competing for RREs in its promoter sequence. Rhythmic output of the clock is achieved through E-box elements in CCG which can impact a range of cell processes and physiology. The stability and subcellular localisation of circadian proteins is highly regulated by kinases and phosphatases (inset box). Although not entirely understood, the phosphorylation state of circadian proteins can affect their cellular localisation and/or stability. Mutations affecting the stability of Per proteins can accelerate the molecular clock in humans, leading to the inherited syndrome familial advanced sleep phase syndrome (FASPS).
Aside from generating robust rhythms, the circadian system must be sensitive to environmental cues and be able to adjust its phase to synchronise with the prevailing day/night rhythm, a process known as entrainment. In mammals, the signalling of environmental light exposure, carried by dedicated retinal afferents, is the most important entrainment cue of the SCN clock [12]. However, other cues such as food availability, novel environment, or social interaction may act as timekeeping cues (Figure 2). These signals reach the SCN clock through disparate neurotransmitter/neuromodulator and hormonal pathways and can reset the phase of expression within the autoregulatory feedback loops [13]–[16]. Non-SCN clocks can be directly sensitive to external timekeeping cues; the most obvious example is the retina [10],[11], although there is evidence that additional, extra-SCN oscillators receive relevant environmental phase-setting information directly [17]–[19]. However, as they also receive strong entrainment signals from the SCN [6],[8], it is a process of bidirectional communication and feedback that ultimately establishes the entrainment and phasing of molecular clocks throughout the brain and body. A final level of complexity and fine-tuning in molecular rhythms may also be derived from local crosstalk between clock tissues and nuclei (reviewed in [8]).
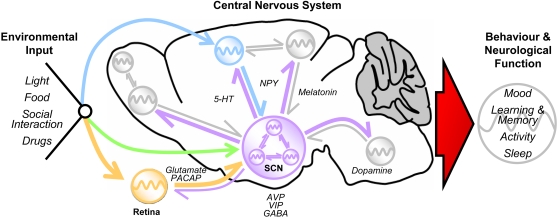
Figure 2. The Circadian System and the Mammalian Brain.
The SCN acts as a “master” clock, sending neuronal and humoral output to a number of regions in the CNS. The SCN can passively drive rhythmicity in these regions, or nuclei may themselves have their own automomous clocks. Within the SCN, every cell is a potentially independent oscillator unit. Extensive intra-SCN signalling is used to synchronise the rhythms of multiple cells. Entrainment is a process whereby environmental stimuli can alter the timing or phase of central rhythms so that they are coincidental with the prevailing daily cycle (far left). Time cues reach the SCN via several pathways involving intermediate brain areas. Some of these relay nuclei may contain their own oscillators and/or have rhythms in their function (blue and orange arrows and oscillators). Others may not have rhythmic function (green arrow). Extra-SCN oscillators may directly utilise time cues (blue and orange oscillators) or may rely solely on the SCN to synchronise/entrain rhythms (lilac arrows to grey oscillators). These oscillators may also provide feedback which impacts on the operation of the SCN (grey return arrows). In addition, extra-SCN oscillators may drive/influence rhythmicity in other brain areas (smaller grey oscillator) and communicate with each other independently from the SCN (reciprocal grey arrows). Within the CNS, some neurotransmitters/neuromodulators involved in signalling are indicated. The overall output of this complex system (large red arrow) creates the daily rhythmicity seen in a range of neurological functions and behaviours (far right). There is a wider communication with clock/oscillator units throughout the entire body. However, these so-called “peripheral” oscillators and their actions are not shown here.
For molecular circadian rhythms to have an impact on physiology and behaviour, they must be converted into functionally relevant outputs. This is achieved by complex spatiotemporal regulation of gene expression that impacts on cell/tissue-specific function. The orchestrated expression of a number of so-called clock-controlled genes (CCGs) then dictates the temporal regulation of clock-output/functional rhythms in brain regions/systems and peripheral tissues. These may take the form of altered hormone release, changes in action potential firing rate, modified rates of cellular metabolism, etc. [3].
All of the above indicates that the generation of daily rhythms in behavioural and physiological functions, together with the ability to integrate a range of environmental inputs, relies on a complex circadian system. And evidently this system relies on the action of many genes. Moreover, novel genetic factors that influence circadian parameters continue to be identified in mutagenesis screens [20],[21], in QTL analyses [22],[23], and in protein interaction studies [24].
Neurological and Behavioural Phenotypes in Mouse Clock Mutants
Molecular-genetic modifications of the circadian system have a wide range of effects depending on the particular gene affected and also the nature of the mutation (Figure 1). Investigation of mouse clock mutants has focussed primarily on circadian behaviour by assessing overt activity rhythms and molecular rhythms in the SCN. The effects of circadian gene manipulation can range from the profound (complete loss of behavioural and molecular rhythmicity in constant conditions [25]–[27]) to subtle effects (e.g., altered phasing of behavioural/molecular rhythms [28]). However, a more systematic behavioural characterisation of mouse clock mutants could potentially uncover novel behavioural phenotypes associated with clock genes. Given the role of the SCN molecular oscillator in synchronising and entraining neural rhythms in discrete brain centres, clock mutants might affect CNS function through a primary deficit in SCN oscillator function, a deficit in discrete brain region oscillator function, or as a secondary consequence of specific neural rhythm dysfunction.
Disturbances in sleep parameters are associated with a spectrum of neurological and psychiatric disorders. Sleep patterns are affected not only by circadian timing mechanisms but also by independent homeostatic mechanisms that determine the amount of sleep required [29]. Analysis of sleep parameters predicts that mechanisms other than the regulation of sleep-wake timing are affected in clock mutants, as sleep anomalies in clock mutants do not always mirror the behavioural rhythm anomalies. Mutations in Clock (MGI:1861634), Bmal1 (MGI:2180361), and Cry1 (MGI:1270841)/Cry2 (MGI:2181206) [30]–[32] result in alterations in sleep time, sleep fragmentation, and atypical responses following sleep deprivation. Similarly, a number of other clock-related genes, including Npas2 (MGI:109232), Dbp (MGI:94866), and Prok2 (MGI:1354178) affect elements of sleep homeostasis [33]–[35]. However, further evidence exists for the functional segregation of circadian and homeostatic regulation of sleep, as Per1 (MGI:2182834)/Per2 (MGI:1934020) double mutants show no effects on sleep homeostatic mechanisms, although robust rhythms of sleep and wakefulness are lost in constant conditions [36],[37]. Thus, upon consideration of this data, effects of clock mutations on sleep homeostasis could be related to pleiotropy or brain region specificity of particular clock genes.
The process of memory formation in clock mutant mice has received limited attention. Npas2 can deputise for Clock in maintaining molecular rhythms in the SCN and is in fact the normal binding partner for Bmal1 in forebrain clocks [9],[38]. Mutants lacking Npas2 show deficits in the acquisition of cued and contextual fear-conditioning paradigms [39]. It is not feasible that the deficit in Npas2 null mice is secondary to major, centralised circadian disruption, as these mice show only a subtle activity phenotype. A pleiotropic, non-clock effect of Npas2 in memory formation is one possible explanation. Alternatively, the loss of Npas2 may abrogate particular extra-SCN brain clock(s) that regulate memory formation. Evidence for the participation of other clock genes in memory regulation is sparse. Although no specific memory deficits have been found in Per1/Per2 mutant mice [40], Drosophila Per mutants (FBgn0003068) are defective in long-term memory formation [41]. In the same study, no memory-associated deficits were found in timeless (FBgn0014396), clock (FBgn0023076), and cycle (FBgn0023094) mutants, indicating that an association between clock genes and memory regulation is not universal and a degree of functional segregation exists within the system.
There is increasing evidence that a dysfunctional circadian system could be a primary cause of altered emotional behaviour. The majority of this evidence in mice comes from studies on the ENU-induced mutation Clock. Homozygous mutants have a spectrum of behavioural abnormalities including low anxiety, mania, and hyperactivity [42],[43]. These behavioural abnormalities are perhaps explicable by the direct effects of the Clock mutation on core molecular circadian oscillations or are secondary to an alteration in the dynamics of communication between CNS clocks dysregulated by the altered function of the core oscillator. In support of the second possibility, behavioural disturbances in homozygotes are associated with increased dopaminergic activity [42],[43]. Further work strengthens the link between the circadian system and mood regulation. Dysregulation of either NPY or VIP, important neurotransmitters for signalling to and within the SCN, can lead to a number of behavioural disturbances, including alterations in anxiety-like behaviour and aggression [44],[45].
The observations that the mood-stabilising agent, lithium, can reverse behavioural disturbances in Clock mutant mice [43] adds to an increasing body of evidence that lithium’s therapeutic effects may be partially mediated through its effects on the circadian system. Lithium is a potent inhibitor of glycogen synthase kinase 3β (GSK3β, MGI:1861437). Mutations in the Drosophila homologue, shaggy (FBgn0003371), can lengthen the circadian period [46]. In mammalian systems, GSK3β can mediate its circadian effects through promoting the nuclear expression and stability of a number of clock proteins [47],[48]. Moreover, in cultured mammalian cells lithium treatment leads to the rapid proteasomal degradation of the clock protein Rev-erbα (MGI:2444210) and subsequent activation of the clock gene Bmal1 (MGI:1096381) [48].
Additional evidence for behavioural disturbances in clock gene mutants is supported by the fact that they appear to affect the sensitisation to, and preference for, drugs of abuse. This was first evidenced in a number of Drosophila mutants including period, clock, cycle, and doubletime (FBgn0002413) [49], where sensitisation to the effects of cocaine is eliminated. Similar effects were identified in some mouse mutants, although some had opposite effects. For example, mouse Per1 mutants show no behavioural sensitisation to cocaine, and, in a conditioned place preference task, show no preference to cocaine [50]. Per2 mutants have a hypersensitised response to cocaine, and the place preference response is strong [50]. Mice carrying the ENU-induced mutation Clock also show a hypersensitive response to cocaine and increased place preference [51]. These authors suggest that the increased expression and phosphorylation of tyrosine hydroxylase in mutants may affect dopaminergic function within the brain’s reward circuits. Effects of clock mutants on the brain’s neurochemical systems are not limited to the dopaminergic system. Expression of the glutamate transporter Eaat1 (MGI:99917) is reduced in mouse Per2 mutants, leading to decreased uptake of glutamate by astrocytes and increased extracellular glutamate levels [52]. Moreover, increases in alcohol consumption in Per2 mutant mice were reversed by agents believed to act through reducing abnormally high glutamatergic activity. Overall, the interactions between circadian clocks and addiction mechanisms seem to be complex. The possibility of pleiotropy in clock genes cannot be discounted, although these effects could be dissected using conditional mutants. Nevertheless, there is an increasing body of work detailing the interaction between the circadian system and brain neurotransmitter systems. As described above, clock gene expression can be modulated by a number of afferent neurotransmitter effects, and, conversely, the functions of efferent neurotransmitter systems/brain nuclei are modifiable by altered clock gene expression [42],[43],[52].
Altered Circadian Parameters in CNS Disorders
Undoubtedly, circadian parameters are consistently disrupted in a spectrum of CNS disorders (Table 1). In many cases, these disruptions may be secondary to compromised neural circuitry where brain regions regulating output rhythms are disturbed. Nevertheless, it has been difficult to establish whether circadian system disturbances can contribute to CNS disorders or whether they are merely symptomatic of the disease process. In all likelihood, disruption of circadian oscillators can at least modify disease severity, whereas, in some instances, they may play a more primary role in the aetiology of the disease.
Table 1. Rhythm/Sleep Endophenotypes in Human CNS Disease and in Mouse Models.
| Human Disease or Condition | Disturbed Rhythm/Sleep Endophenotype | Relevant Phenotypes in Mouse Models |
| Familial advanced sleep phase syndrome (FASPS) | Early sleep and wake times, shortened circadian rhythms [112]. | Mice expressing human mis-sense mutations in Per2 or CKIδ have advanced phase of activity in a light-dark schedule and a shortened activity rhythm [92],[102]. |
| Delayed sleep phase syndrome (DSPS) | Extreme evening preference, delayed phase of activity, sleep, core body temperature, and melatonin [113]. | No model. |
| Seasonal affective disorder (SAD) | Depressive symptoms occur during shorter winter days [88]–[90]. | No model. |
| Mood disorders (unipolar depression) and psychoses (schizophrenia, bipolar) | Depression. Increased sleep latency, impaired sleep continuity, phase advance in endogenous circadian system relative to sleep schedule, phase advances in growth hormone, plasma melatonin, increased plasma cortisol at night. All major affective disorders include circadian phase disturbances in sleep, activity, temperature, and hormone levels (for reviews see [84]–[86]). | No accurate mouse model. Mutants in serotonergic and dopaminergic systems show disturbances in circadian phase and/or sleep parameters [94]–[97]. Clock mutant has low anxiety, mania, and hyperactivity [42],[43]. Cognitive disturbances in Npas2 mutant [39]. Abnormal sensitisation to drugs of abuse in Clock and Per mutants [50]–[52]. |
| Autism spectrum disorders (ASD) | Longer sleep latency and greater sleep fragmentation. Abnormalities in circadian rhythm and mean concentration of plasma melatonin [81]. | Mice expressing a conditional deletion of Pten have a significantly longer free-running period [83]. |
| Down syndrome | Reduced sleep maintenance, sleep fragmentation, reduction in percent REM sleep, sleep apnea [73]–[75]. | Ts65Dn mouse mutant shows increased activity in the light phase, a reduction in rhythm amplitude, and a 4-h advance in the phase of activity [76],[77]. |
| Smith-Magenis syndrome | Inverted rhythm of melatonin secretion [69],[71]. Advanced sleep/wake phase. Nighttime wakening, daytime sleepiness. Reduced total and NREM sleep [70]. | Heterozygous deletion mutant mice have a hypoactive phenotype and a significantly shorter circadian period [72]. |
| Prader-Willi syndrome | Sleep apnea, sleep-related and behavioural disturbances including daytime napping and excessive daytime sleepiness [75],[78],[79]. | Mice deficient for mage-like 2 gene (Magel2) have a reduced circadian activity amplitude with increased daytime activity [80]. |
| Parkinson disease (PD) | Sleep fragmentation, sleep apnea, REM sleep behaviour disorder, excessive daytime sleepiness [53]. | No recorded circadian or sleep disturbances in genetic mouse models [114]. |
| Huntington disease (HD) | Nocturnal awakening and progressive disintegration of daily activity rhythms [55]. | R6/2 mouse transgenic line has increased daytime and reduced nocturnal activity. Progresses to a complete disintegration of diurnal and circadian activity rhythms [55]. |
| Alzheimer disease (AD) | Fragmented sleep, increased nocturnal activity, and reduced daytime activity. Delayed phase in peak of daily activity [57]. | Alterations in sleep regulation and timing in Tg2576 [62] and PDAPP mice [61]. Tg2576 mice also have a significantly longer circadian period [62]. Both TgCRND8 and APP23 mice show changes in daily activity profiles potentially analogous to those seen in AD patients [63],[64]. |
| Aging | Sleep disturbances due to earlier wake time and reduced sleep consolidation. Partially attributed to age-related reduction in amplitude and advance in phase of circadian rhythms [56],[58]. | Aging lengthens the period and reduces the amplitude of circadian activity rhythms. The onset of daily activity is significantly delayed and the variability of onset is increased [67]. |
| Prion diseases | Severe sleep abnormalities, progressive loss of circadian rest-activity, and melatonin rhythms [54],[59],[60]. | Increased sleep fragmentation and significantly longer circadian period in activity in prion protein null mutants [65]. |
In neurodegenerative disease and aging (Table 1), disturbances in sleep mechanisms and circadian disturbances in phase and amplitude of activity and temperature regulation are common symptomatic features secondary to a deterioration in brain circuitry [53]–[60]. Circadian activity disturbances have been described in a number of transgenic mouse models of Alzheimer Disease (AD, OMIM; #104300), and in some cases these precede the onset of typical AD pathologies [61]–[64]. The neurodegenerative prion diseases also express a spectrum of sleep and circadian rhythm disturbances [54],[59],[60]. Interestingly, these disturbances are mirrored in mice that are null for the prion protein [65]. In the Huntington R6/2 mouse transgenic line, disintegration of activity rhythms mimic those seen in Huntington patients (OMIM; +143100), and these behavioural disturbances are accompanied by altered clock gene rhythms in the SCN, motor cortex, and striatum [55]. Similarly, aging alters activity onsets, lengthens circadian period, reduces circadian amplitude, and alters SCN electrophysiology in mice [66],[67]. Age-related circadian changes may also be symptomatic of brain circuitry deterioration as, for example, comparable effects of aging are seen in wild-type and Clock mutant mice [68].
Circadian disturbances are more likely to contribute to the aetiology of a number of syndromic disorders (Table 1). These disturbances are likely to be due to deficits in specific oscillating neural and molecular circuits that are regulated by the clock. Smith-Magenis syndrome (SMS, OMIM #182290), associated with heterozygous deletions on Chromosome 17, is characterised by significant sleep disturbances with a reversed secretion rhythm of melatonin [69]–[71]. Mice carrying an engineered heterozygous deletion of the SMS syntenic region (Del(11Cops3-Zfp179)1Jrl, MGI:3521985) have a hypoactive phenotype and an abnormal circadian period [72]. Sleep disturbances are also features of Down syndrome (OMIM #190685) patients [73]–[75], and the Ts65Dn mouse mutant expresses a number of abnormal circadian parameters including increased activity in the light phase, a reduction in rhythm amplitude, and a four-hour advance in the phase of activity [76],[77]. Patients with Prader-Willi syndrome (PWS, OMIM #176270) also exhibit a spectrum of sleep-related and behavioural disturbances [75],[78],[79]. Mice deficient for the mage-like 2 gene (Magel2), an SCN-enriched transcript within the PWS deletion region, have a reduced circadian activity amplitude with increased daytime activity relative to controls (MGI:3760092) [80].
Other behavioural disorders with circadian and sleep-related disturbances include autism spectrum disorders (ASD) (OMIM %209850) [81]). Behavioural disturbances in ASD may arise in part from an inability of an individual’s circadian oscillator to entrain to environmental and social cues. One specific correlate of ASD is a low level of melatonin, and one of the enzymes critical in the synthesis of melatonin, acetylserotonin-O-methyltransferase (ASMT, OMIM *300015), is implicated as a susceptibility gene for ASD [82]. Mutations in the phosphatase and tensin homologue on Chromosome ten (PTEN) have been reported in autistic individuals with macrocephaly. In mice carrying a conditional deletion of Pten (MGI:2182005), abnormal phenotypes include macrocephaly, increased susceptibility to seizures, social interaction deficits, anxiety, and a significantly longer free-running period [83].
The contribution of the circadian regulatory system, arising from conflicts between internal biological clocks and environmental (solar) and social clocks, is evident in affective disorders. All major affective disorders (such as unipolar depression, OMIM #608516; bipolar disorder, and schizophrenia, OMIM #181500) include circadian phase disturbances in sleep, activity, temperature, and hormone levels (for reviews see [84]–[86]). Moreover, there is evidence that if rhythms can be altered/stabilised using relevant therapies, improvements in the primary symptoms can occur. For example, in some instances sleep deprivation has an antidepressant effect in patients [87]. Conversely, many disorders with a primary anomaly in the circadian system are associated with depressed mood. Seasonal affective disorder (SAD; OMIM #608516) is a common condition where depressive symptoms occur during shorter winter days [88]–[90]. Two inherited sleep phase disorders, familial advanced sleep phase syndrome (FASPS; OMIM #604348) and delayed sleep phase syndrome (DSPS), are both associated with abnormal affective states [91],[92]. Furthermore, individuals with a behavioural preference for “eveningness” have a greater tendency to develop depression [93]. Because of the difficulties in classifying these diseases/conditions in humans and because of their multigenic nature, it is difficult to study their aetiology in mouse models. However, although no mouse mutants have been developed to model complete affective disorders, a number of mutants in serotonergic and dopaminergic systems displaying features of these disorders also show disturbances in circadian phase and/or sleep parameters [94]–[97].
Polymorphisms in Human Clock Genes Alter More Than Rhythms
The contribution of circadian gene dysregulation to CNS disorders has only recently been explored through the analysis of clock gene polymorphisms. Circadian gene polymorphisms may simply underlie a morning or evening preference in human populations, but extremes in these behaviours may also underlie the more complex phenotypes associated with psychiatric disorders. A quantitative scoring system for diurnal preference, the Horne-Ostberg questionnaire [98], has been used as the basis for association studies, and these have been carried out either in random populations or in families inheriting FASPS or DSPS. Many studies implicate altered dynamics in clock protein phosphorylation as a critical factor (see Figure 1). For example, the shorter 4-repeat allele of a 54-bp coding-region polymorphism in the PER3 (OMIM *603427) gene is associated with extreme evening preference and DSPS [99]. Moreover, in comparisons between short- and long-repeat patients, slow wave sleep was greater in 5-repeat individuals, and deficits in cognitive performance following sleep loss were greater [100]. This 54-bp sequence is in a region of PER3 encoding a putative phosphorylation domain. The significance of these observations has been highlighted by the identification of two distinct mutations in familial ASPS pedigrees. The first [101], a mis-sense mutation in PER2 (OMIM *603426), is within the binding domain for casein kinase I epsilon (CKIε; OMIM *600863) and results in hypophosphorylated PER2 in vitro. Transgenic mice expressing this mutation had an advanced phase of activity in a light–dark schedule and a short free-running period of activity [102]. A second mis-sense mutation was found in CKIδ (OMIM *600864) itself [92], the mutation resulting in reduced enzymatic activity in vitro. Again, the phenotype in a mouse transgenic line mimicked that of the human individuals.
Conflicts between internal biological clocks and environmental (solar) and social clocks should be evident in individuals with extreme diurnal preferences, and this could have the potential to disrupt homeostatic processes and behaviours affected by them. In fact, Xu et al. [92] observed that four out of five patients with FASPS showed either evidence of the clinical features of, or a history of, depression. Observations such as this and the hypothesis that certain genetic susceptibility factors are shared across the psychosis spectrum [103] have led several groups to investigate clock gene associations in a number of mood disorders and psychoses. The most evident example is in SAD. Partonen et al. [104] found that SAD was associated with SNP variants in PER2, BMAL1 (OMIM *602550), and NPAS2 (OMIM *603347) with additive effects from combined risk genotypes. An earlier study had also identified significant associations between diurnal preference and SAD with a significant effect of NPAS2 471 Leu on disease susceptibility [105].
Investigations into clock gene associations with other affective disorders are in their infancy. Although limited, there are a number of indications warranting further investigation into associations with bipolar disorder, schizoaffective disorder, schizophrenia, and autism [106]–[111]. Variants of PER1 (OMIM *602260), PER3, NPAS2, BMAL1, CLOCK (OMIM *601851), and TIM (OMIM *603887) all showed specific associations with a number of disorders. The promise of these pilot studies should encourage more systematic studies in investigating the contribution of clock gene variants to the onset and severity of CNS disorders.
Conclusions
Biological rhythms are undoubtedly disrupted in a spectrum of CNS disorders. Establishing the contribution of clock genes to cause and effect in these disorders has proven difficult. Nevertheless, these investigations continue to be helped through the systematic characterisation of behavioural phenotypes in mouse circadian mutants, the identification of new genetic factors that contribute to circadian and behavioural function, and the investigations of clock gene polymorphisms in all CNS disease areas. Continued investigation into these three areas should lead to new insights into the causes and progression of neurological and psychiatric disorders.
Acknowledgments
We thank V. Tucci, A. Acevedo, and G. Blanco for helpful comments.
Footnotes
The authors have declared that no competing interests exist.
Medical Research Council
References
- 1.Ko CH, Takahashi JS. Molecular components of the mammalian circadian clock. Hum Mol Genet. 2006;15(Spec No 2):R271–R277. doi: 10.1093/hmg/ddl207. [DOI] [PubMed] [Google Scholar]
- 2.Moore RY. Organization and function of a central nervous system circadian oscillator: the suprachiasmatic hypothalamic nucleus. Fed Proc. 1983;42:2783–2789. [PubMed] [Google Scholar]
- 3.Reppert SM, Weaver DR. Coordination of circadian timing in mammals. Nature. 2002;418:935–941. doi: 10.1038/nature00965. [DOI] [PubMed] [Google Scholar]
- 4.Abe M, Herzog ED, Yamazaki S, Straume M, Tei H, et al. Circadian rhythms in isolated brain regions. J Neurosci. 2002;22:350–356. doi: 10.1523/JNEUROSCI.22-01-00350.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abraham U, Prior JL, Granados-Fuentes D, Piwnica-Worms DR, Herzog ED. Independent circadian oscillations of Period1 in specific brain areas in vivo and in vitro. J Neurosci. 2005;25:8620–8626. doi: 10.1523/JNEUROSCI.2225-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Granados-Fuentes D, Prolo LM, Abraham U, Herzog ED. The suprachiasmatic nucleus entrains, but does not sustain, circadian rhythmicity in the olfactory bulb. J Neurosci. 2004;24:615–619. doi: 10.1523/JNEUROSCI.4002-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Granados-Fuentes D, Saxena MT, Prolo LM, Aton SJ, Herzog ED. Olfactory bulb neurons express functional, entrainable circadian rhythms. Eur J Neurosci. 2004;19:898–906. doi: 10.1111/j.0953-816x.2004.03117.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guilding C, Piggins HD. Challenging the omnipotence of the suprachiasmatic timekeeper: Are circadian oscillators present throughout the mammalian brain? Eur J Neurosci. 2007;25:3195–3216. doi: 10.1111/j.1460-9568.2007.05581.x. [DOI] [PubMed] [Google Scholar]
- 9.Reick M, Garcia JA, Dudley C, McKnight SL. NPAS2: An analog of clock operative in the mammalian forebrain. Science. 2001;293:506–509. doi: 10.1126/science.1060699. [DOI] [PubMed] [Google Scholar]
- 10.Ruan GX, Zhang DQ, Zhou T, Yamazaki S, McMahon DG. Circadian organization of the mammalian retina. Proc Natl Acad Sci U S A. 2006;103:9703–9708. doi: 10.1073/pnas.0601940103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tosini G, Menaker M. Circadian rhythms in cultured mammalian retina. Science. 1996;272:419–421. doi: 10.1126/science.272.5260.419. [DOI] [PubMed] [Google Scholar]
- 12.Abrahamson EE, Moore RY. Suprachiasmatic nucleus in the mouse: Retinal innervation, intrinsic organization, and efferent projections. Brain Res. 2001;916:172–91. doi: 10.1016/s0006-8993(01)02890-6. [DOI] [PubMed] [Google Scholar]
- 13.Lamont EW, Diaz LR, Barry-Shaw J, Stewart J, Amir S. Daily restricted feeding rescues a rhythm of period2 expression in the arrhythmic suprachiasmatic nucleus. Neuroscience. 2005;132:245–248. doi: 10.1016/j.neuroscience.2005.01.029. [DOI] [PubMed] [Google Scholar]
- 14.Stephan FK. The other circadian system: Food as a Zeitgeber. J Biol Rhythms. 2002;17:284–292. doi: 10.1177/074873040201700402. [DOI] [PubMed] [Google Scholar]
- 15.Tataroglu O, Davidson AJ, Benvenuto LJ, Menaker M. The methamphetamine-sensitive circadian oscillator (MASCO) in mice. J Biol Rhythms. 2006;21:185–194. doi: 10.1177/0748730406287529. [DOI] [PubMed] [Google Scholar]
- 16.Hannibal J, Fahrenkrug J. Neuronal input pathways to the brain’s biological clock and their functional significance. Adv Anat Embryol Cell Biol. 2006;182:1–71. [PubMed] [Google Scholar]
- 17.Granados-Fuentes D, Tseng A, Herzog ED. A circadian clock in the olfactory bulb controls olfactory responsivity. J Neurosci. 2006;26:12219–12225. doi: 10.1523/JNEUROSCI.3445-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hara R, Wan K, Wakamatsu H, Aida R, Moriya T, et al. Restricted feeding entrains liver clock without participation of the suprachiasmatic nucleus. Genes Cells. 2001;6:269–278. doi: 10.1046/j.1365-2443.2001.00419.x. [DOI] [PubMed] [Google Scholar]
- 19.Wakamatsu H, Yoshinobu Y, Aida R, Moriya T, Akiyama M, et al. Restricted-feeding-induced anticipatory activity rhythm is associated with a phase-shift of the expression of mPer1 and mPer2 mRNA in the cerebral cortex and hippocampus but not in the suprachiasmatic nucleus of mice. Eur J Neurosci. 2001;13:1190–1196. doi: 10.1046/j.0953-816x.2001.01483.x. [DOI] [PubMed] [Google Scholar]
- 20.Bacon Y, Ooi A, Kerr S, Shaw-Andrews L, Winchester L, et al. Screening for novel ENU-induced rhythm, entrainment, and activity mutants. Genes Brain Behav. 2004;3:196–205. doi: 10.1111/j.1601-183X.2004.00070.x. [DOI] [PubMed] [Google Scholar]
- 21.Godinho SI, Maywood ES, Shaw L, Tucci V, Barnard AR, et al. The after-hours mutant reveals a role for Fbxl3 in determining mammalian circadian period. Science. 2007;316:897–900. doi: 10.1126/science.1141138. [DOI] [PubMed] [Google Scholar]
- 22.Hofstetter JR, Svihla-Jones DA, Mayeda AR. A QTL on mouse chromosome 12 for the genetic variance in free-running circadian period between inbred strains of mice. J Circadian Rhythms. 2007;5:7. doi: 10.1186/1740-3391-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hofstetter JR, Trofatter JA, Kernek KL, Nurnberger JI, Mayeda AR. New quantitative trait loci for the genetic variance in circadian period of locomotor activity between inbred strains of mice. J Biol Rhythms. 2003;18:450–462. doi: 10.1177/0748730403259468. [DOI] [PubMed] [Google Scholar]
- 24.Brown SA, Ripperger J, Kadener S, Fleury-Olela F, Vilbois F, et al. PERIOD1-associated proteins modulate the negative limb of the mammalian circadian oscillator. Science. 2005;308:693–696. doi: 10.1126/science.1107373. [DOI] [PubMed] [Google Scholar]
- 25.Bunger MK, Wilsbacher LD, Moran SM, Clendenin C, Radcliffe LA, et al. Mop3 is an essential component of the master circadian pacemaker in mammals. Cell. 2000;103:1009–1017. doi: 10.1016/s0092-8674(00)00205-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.King DP, Vitaterna MH, Chang AM, Dove WF, Pinto LH, et al. The mouse Clock mutation behaves as an antimorph and maps within the W19H deletion, distal of Kit. Genetics. 1997;146:1049–1060. doi: 10.1093/genetics/146.3.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kume K, Zylka MJ, Sriram S, Shearman LP, Weaver DR, et al. mCRY1 and mCRY2 are essential components of the negative limb of the circadian clock feedback loop. Cell. 1999;98:193–205. doi: 10.1016/s0092-8674(00)81014-4. [DOI] [PubMed] [Google Scholar]
- 28.Debruyne JP, Noton E, Lambert CM, Maywood ES, Weaver DR, et al. A clock shock: Mouse CLOCK is not required for circadian oscillator function. Neuron. 2006;50:465–477. doi: 10.1016/j.neuron.2006.03.041. [DOI] [PubMed] [Google Scholar]
- 29.Borbely AA, Achermann P. Sleep homeostasis and models of sleep regulation. J Biol Rhythms. 1999;14:557–568. doi: 10.1177/074873099129000894. [DOI] [PubMed] [Google Scholar]
- 30.Laposky A, Easton A, Dugovic C, Walisser J, Bradfield C, et al. Deletion of the mammalian circadian clock gene BMAL1/Mop3 alters baseline sleep architecture and the response to sleep deprivation. Sleep. 2005;28:395–409. doi: 10.1093/sleep/28.4.395. [DOI] [PubMed] [Google Scholar]
- 31.Naylor E, Bergmann BM, Krauski K, Zee PC, Takahashi JS, et al. The circadian clock mutation alters sleep homeostasis in the mouse. J Neurosci. 2000;20:8138–8143. doi: 10.1523/JNEUROSCI.20-21-08138.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wisor JP, O’Hara BF, Terao A, Selby CP, Kilduff TS, et al. A role for cryptochromes in sleep regulation. BMC Neurosci. 2002;3:20. doi: 10.1186/1471-2202-3-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dudley CA, Erbel-Sieler C, Estill SJ, Reick M, Franken P, et al. Altered patterns of sleep and behavioral adaptability in NPAS2-deficient mice. Science. 2003;301:379–383. doi: 10.1126/science.1082795. [DOI] [PubMed] [Google Scholar]
- 34.Franken P, Lopez-Molina L, Marcacci L, Schibler U, Tafti M. The transcription factor DBP affects circadian sleep consolidation and rhythmic EEG activity. J Neurosci. 2000;20:617–625. doi: 10.1523/JNEUROSCI.20-02-00617.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hu WP, Li JD, Zhang C, Boehmer L, Siegel JM, et al. Altered circadian and homeostatic sleep regulation in prokineticin 2-deficient mice. Sleep. 2007;30:247–256. [PMC free article] [PubMed] [Google Scholar]
- 36.Kopp C, Albrecht U, Zheng B, Tobler I. Homeostatic sleep regulation is preserved in mPer1 and mPer2 mutant mice. Eur J Neurosci. 2002;16:1099–1106. doi: 10.1046/j.1460-9568.2002.02156.x. [DOI] [PubMed] [Google Scholar]
- 37.Shiromani PJ, Xu M, Winston EM, Shiromani SN, Gerashchenko D, et al. Sleep rhythmicity and homeostasis in mice with targeted disruption of mPeriod genes. Am J Physiol Regul Integr Comp Physiol. 2004;287:R47–R57. doi: 10.1152/ajpregu.00138.2004. [DOI] [PubMed] [Google Scholar]
- 38.DeBruyne JP, Weaver DR, Reppert SM. CLOCK and NPAS2 have overlapping roles in the suprachiasmatic circadian clock. Nat Neurosci. 2007;10:543–545. doi: 10.1038/nn1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Garcia JA, Zhang D, Estill SJ, Michnoff C, Rutter J, et al. Impaired cued and contextual memory in NPAS2-deficient mice. Science. 2000;288:2226–2230. doi: 10.1126/science.288.5474.2226. [DOI] [PubMed] [Google Scholar]
- 40.Zueger M, Urani A, Chourbaji S, Zacher C, Lipp HP, et al. mPer1 and mPer2 mutant mice show regular spatial and contextual learning in standardized tests for hippocampus-dependent learning. J Neural Transm. 2006;113:347–356. doi: 10.1007/s00702-005-0322-4. [DOI] [PubMed] [Google Scholar]
- 41.Sakai T, Tamura T, Kitamoto T, Kidokoro Y. A clock gene, period, plays a key role in long-term memory formation in Drosophila. Proc Natl Acad Sci U S A. 2004;101:16058–16063. doi: 10.1073/pnas.0401472101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Easton A, Arbuzova J, Turek FW. The circadian Clock mutation increases exploratory activity and escape-seeking behavior. Genes Brain Behav. 2003;2:11–19. doi: 10.1034/j.1601-183x.2003.00002.x. [DOI] [PubMed] [Google Scholar]
- 43.Roybal K, Theobold D, Graham A, DiNieri JA, Russo SJ, et al. Mania-like behavior induced by disruption of CLOCK. Proc Natl Acad Sci U S A. 2007;104:6406–6411. doi: 10.1073/pnas.0609625104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Karl T, Burne TH, Herzog H. Effect of Y1 receptor deficiency on motor activity, exploration, and anxiety. Behav Brain Res. 2006;167:87–93. doi: 10.1016/j.bbr.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 45.Wersinger SR, Caldwell HK, Christiansen M, Young WS., III Disruption of the vasopressin 1b receptor gene impairs the attack component of aggressive behavior in mice. Genes Brain Behav. 2007;6:653–660. doi: 10.1111/j.1601-183X.2006.00294.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Martinek S, Inonog S, Manoukian AS, Young MW. A role for the segment polarity gene shaggy/GSK-3 in the Drosophila circadian clock. Cell. 2001;105:769–779. doi: 10.1016/s0092-8674(01)00383-x. [DOI] [PubMed] [Google Scholar]
- 47.Iitaka C, Miyazaki K, Akaike T, Ishida N. A role for glycogen synthase kinase-3beta in the mammalian circadian clock. J Biol Chem. 2005;280:29397–29402. doi: 10.1074/jbc.M503526200. [DOI] [PubMed] [Google Scholar]
- 48.Yin L, Wang J, Klein PS, Lazar MA. Nuclear receptor Rev-erbalpha is a critical lithium-sensitive component of the circadian clock. Science. 2006;311:1002–1005. doi: 10.1126/science.1121613. [DOI] [PubMed] [Google Scholar]
- 49.Andretic R, Chaney S, Hirsh J. Requirement of circadian genes for cocaine sensitization in Drosophila. Science. 1999;285:1066–1068. doi: 10.1126/science.285.5430.1066. [DOI] [PubMed] [Google Scholar]
- 50.Abarca C, Albrecht U, Spanagel R. Cocaine sensitization and reward are under the influence of circadian genes and rhythm. Proc Natl Acad Sci U S A. 2002;99:9026–9030. doi: 10.1073/pnas.142039099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McClung CA, Sidiropoulou K, Vitaterna M, Takahashi JS, White FJ, et al. Regulation of dopaminergic transmission and cocaine reward by the Clock gene. Proc Natl Acad Sci U S A. 2005;102:9377–9381. doi: 10.1073/pnas.0503584102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Spanagel R, Pendyala G, Abarca C, Zghoul T, Sanchis-Segura C, et al. The clock gene Per2 influences the glutamatergic system and modulates alcohol consumption. Nat Med. 2005;11:35–42. doi: 10.1038/nm1163. [DOI] [PubMed] [Google Scholar]
- 53.Ferreira JJ, Desboeuf K, Galitzky M, Thalamas C, Brefel-Courbon C, et al. Sleep disruption, daytime somnolence, and sleep attacks in Parkinson disease: A clinical survey in PD patients and age-matched healthy volunteers. Eur J Neurol. 2006;13:209–214. doi: 10.1111/j.1468-1331.2006.01262.x. [DOI] [PubMed] [Google Scholar]
- 54.Landolt HP, Glatzel M, Blattler T, Achermann P, Roth C, et al. Sleep-wake disturbances in sporadic Creutzfeldt-Jakob disease. Neurology. 2006;66:1418–1424. doi: 10.1212/01.wnl.0000210445.16135.56. [DOI] [PubMed] [Google Scholar]
- 55.Morton AJ, Wood NI, Hastings MH, Hurelbrink C, Barker RA, et al. Disintegration of the sleep-wake cycle and circadian timing in Huntington disease. J Neurosci. 2005;25:157–163. doi: 10.1523/JNEUROSCI.3842-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Van Someren EJ. Circadian rhythms and sleep in human aging. Chronobiol Int. 2000;17:233–243. doi: 10.1081/cbi-100101046. [DOI] [PubMed] [Google Scholar]
- 57.Volicer L, Harper DG, Manning BC, Goldstein R, Satlin A. Sundowning and circadian rhythms in Alzheimer disease. Am J Psychiatry. 2001;158:704–711. doi: 10.1176/appi.ajp.158.5.704. [DOI] [PubMed] [Google Scholar]
- 58.Dijk DJ, Duffy JF, Czeisler CA. Contribution of circadian physiology and sleep homeostasis to age-related changes in human sleep. Chronobiol Int. 2000;17:285–311. doi: 10.1081/cbi-100101049. [DOI] [PubMed] [Google Scholar]
- 59.Plazzi G, Schutz Y, Cortelli P, Provini F, Avoni P, et al. Motor overactivity and loss of motor circadian rhythm in fatal familial insomnia: An actigraphic study. Sleep. 1997;20:739–742. doi: 10.1093/sleep/20.9.739. [DOI] [PubMed] [Google Scholar]
- 60.Portaluppi F, Cortelli P, Avoni P, Vergnani L, Maltoni P, et al. Progressive disruption of the circadian rhythm of melatonin in fatal familial insomnia. J Clin Endocrinol Metab. 1994;78:1075–1078. doi: 10.1210/jcem.78.5.8175963. [DOI] [PubMed] [Google Scholar]
- 61.Huitron-Resendiz S, Sanchez-Alavez M, Gallegos R, Berg G, Crawford E, et al. Age-independent and age-related deficits in visuospatial learning, sleep-wake states, thermoregulation, and motor activity in PDAPP mice. Brain Res. 2002;928:126–137. doi: 10.1016/s0006-8993(01)03373-x. [DOI] [PubMed] [Google Scholar]
- 62.Wisor JP, Edgar DM, Yesavage J, Ryan HS, McCormick CM, et al. Sleep and circadian abnormalities in a transgenic mouse model of Alzheimer disease: A role for cholinergic transmission. Neuroscience. 2005;131:375–385. doi: 10.1016/j.neuroscience.2004.11.018. [DOI] [PubMed] [Google Scholar]
- 63.Ambree O, Touma C, Gortz N, Keyvani K, Paulus W, et al. Activity changes and marked stereotypic behavior precede Abeta pathology in TgCRND8 Alzheimer mice. Neurobiol Aging. 2006;27:955–964. doi: 10.1016/j.neurobiolaging.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 64.Van Dam D, D’Hooge R, Staufenbiel M, Van Ginneken C, Van Meir F, et al. Age-dependent cognitive decline in the APP23 model precedes amyloid deposition. Eur J Neurosci. 2003;17:388–396. doi: 10.1046/j.1460-9568.2003.02444.x. [DOI] [PubMed] [Google Scholar]
- 65.Tobler I, Gaus SE, Deboer T, Achermann P, Fischer M, et al. Altered circadian activity rhythms and sleep in mice devoid of prion protein. Nature. 1996;380:639–642. doi: 10.1038/380639a0. [DOI] [PubMed] [Google Scholar]
- 66.Nygard M, Hill RH, Wikstrom MA, Kristensson K. Age-related changes in electrophysiological properties of the mouse suprachiasmatic nucleus in vitro. Brain Res Bull. 2005;65:149–154. doi: 10.1016/j.brainresbull.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 67.Valentinuzzi VS, Scarbrough K, Takahashi JS, Turek FW. Effects of aging on the circadian rhythm of wheel-running activity in C57BL/6 mice. Am J Physiol. 1997;273:R1957–R1964. doi: 10.1152/ajpregu.1997.273.6.R1957. [DOI] [PubMed] [Google Scholar]
- 68.Kolker DE, Vitaterna MH, Fruechte EM, Takahashi JS, Turek FW. Effects of age on circadian rhythms are similar in wild-type and heterozygous Clock mutant mice. Neurobiol Aging. 2004;25:517–523. doi: 10.1016/j.neurobiolaging.2003.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.De Leersnyder H, Bresson JL, de Blois MC, Souberbielle JC, Mogenet A, et al. Beta 1-adrenergic antagonists and melatonin reset the clock and restore sleep in a circadian disorder, Smith-Magenis syndrome. J Med Genet. 2003;40:74–78. doi: 10.1136/jmg.40.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.De Leersnyder H, Claustrat B, Munnich A, Verloes A. Circadian rhythm disorder in a rare disease: Smith-Magenis syndrome. Mol Cell Endocrinol. 2006;252:88–91. doi: 10.1016/j.mce.2006.03.043. [DOI] [PubMed] [Google Scholar]
- 71.Potocki L, Glaze D, Tan DX, Park SS, Kashork CD, et al. Circadian rhythm abnormalities of melatonin in Smith-Magenis syndrome. J Med Genet. 2000;37:428–433. doi: 10.1136/jmg.37.6.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Walz K, Spencer C, Kaasik K, Lee CC, Lupski JR, et al. Behavioral characterization of mouse models for Smith-Magenis syndrome and dup(17)(p11.2p11.2). Hum Mol Genet. 2004;13:367–378. doi: 10.1093/hmg/ddh044. [DOI] [PubMed] [Google Scholar]
- 73.Harvey MT, Kennedy CH. Polysomnographic phenotypes in developmental disabilities. Int J Dev Neurosci. 2002;20:443–448. doi: 10.1016/s0736-5748(02)00008-4. [DOI] [PubMed] [Google Scholar]
- 74.McKay SM, Angulo-Barroso RM. Longitudinal assessment of leg motor activity and sleep patterns in infants with and without Down syndrome. Infant Behav Dev. 2006;29:153–168. doi: 10.1016/j.infbeh.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 75.Cotton S, Richdale A. Brief report: Parental descriptions of sleep problems in children with autism, Down syndrome, and Prader-Willi syndrome. Res Dev Disabil. 2006;27:151–161. doi: 10.1016/j.ridd.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 76.Colas D, London J, Gharib A, Cespuglio R, Sarda N. Sleep-wake architecture in mouse models for Down syndrome. Neurobiol Dis. 2004;16:291–299. doi: 10.1016/j.nbd.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 77.Stewart LS, Persinger MA, Cortez MA, Snead OC., III Chronobiometry of behavioral activity in the Ts65Dn model of Down syndrome. Behav Genet. 2007;37:388–398. doi: 10.1007/s10519-006-9119-y. [DOI] [PubMed] [Google Scholar]
- 78.Nixon GM, Brouillette RT. Sleep and breathing in Prader-Willi syndrome. Pediatr Pulmonol. 2002;34:209–217. doi: 10.1002/ppul.10152. [DOI] [PubMed] [Google Scholar]
- 79.Vgontzas AN, Kales A, Seip J, Mascari MJ, Bixler EO, et al. Relationship of sleep abnormalities to patient genotypes in Prader-Willi syndrome. Am J Med Genet. 1996;67:478–482. doi: 10.1002/(SICI)1096-8628(19960920)67:5<478::AID-AJMG7>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 80.Kozlov SV, Bogenpohl JW, Howell MP, Wevrick R, Panda S, et al. The imprinted gene Magel2 regulates normal circadian output. Nat Genet. 2007;39:1266–1272. doi: 10.1038/ng2114. [DOI] [PubMed] [Google Scholar]
- 81.Malow BA. Sleep disorders, epilepsy, and autism. Ment Retard Dev Disabil Res Rev. 2004;10:122–125. doi: 10.1002/mrdd.20023. [DOI] [PubMed] [Google Scholar]
- 82.Melke J, Goubran Botros H, Chaste P, Betancur C, Nygren G, et al. Abnormal melatonin synthesis in autism spectrum disorders. Mol. 2007;Psychiatry1:90–98. doi: 10.1038/sj.mp.4002016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ogawa S, Kwon CH, Zhou J, Koovakkattu D, Parada LF, et al. A seizure-prone phenotype is associated with altered free-running rhythm in Pten mutant mice. Brain Res. 2007;1168:112–123. doi: 10.1016/j.brainres.2007.06.074. [DOI] [PubMed] [Google Scholar]
- 84.Boivin DB. Influence of sleep-wake and circadian rhythm disturbances in psychiatric disorders. J Psychiatry Neurosci. 2000;25:446–458. [PMC free article] [PubMed] [Google Scholar]
- 85.McClung CA. Circadian genes, rhythms, and the biology of mood disorders. Pharmacol Ther. 2007;114:222–232. doi: 10.1016/j.pharmthera.2007.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wirz-Justice A. Biological rhythm disturbances in mood disorders. Int Clin Psychopharmacol. 2006;21(Supplement 1):S11–S15. doi: 10.1097/01.yic.0000195660.37267.cf. [DOI] [PubMed] [Google Scholar]
- 87.Wirz-Justice A, Van den Hoofdakker RH. Sleep deprivation in depression: What do we know, where do we go? Biol Psychiatry. 1999;46:445–453. doi: 10.1016/s0006-3223(99)00125-0. [DOI] [PubMed] [Google Scholar]
- 88.Lam RW, Levitan RD. Pathophysiology of seasonal affective disorder: A review. J Psychiatry Neurosci. 2000;25:469–480. [PMC free article] [PubMed] [Google Scholar]
- 89.Levitan RD. The chronobiology and neurobiology of winter seasonal affective disorder. Dialogues Clin Neurosci. 2007;9:315–324. doi: 10.31887/DCNS.2007.9.3/rlevitan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Magnusson A, Boivin D. Seasonal affective disorder: An overview. Chronobiol Int. 2003;20:189–207. doi: 10.1081/cbi-120019310. [DOI] [PubMed] [Google Scholar]
- 91.Shirayama M, Shirayama Y, Iida H, Kato M, Kajimura N, et al. The psychological aspects of patients with delayed sleep phase syndrome (DSPS). Sleep Med. 2003;4:427–433. doi: 10.1016/s1389-9457(03)00101-1. [DOI] [PubMed] [Google Scholar]
- 92.Xu Y, Padiath QS, Shapiro RE, Jones CR, Wu SC, et al. Functional consequences of a CKIdelta mutation causing familial advanced sleep phase syndrome. Nature. 2005;434:640–644. doi: 10.1038/nature03453. [DOI] [PubMed] [Google Scholar]
- 93.Drennan MD, Klauber MR, Kripke DF, Goyette LM. The effects of depression and age on the Horne-Ostberg morningness-eveningness score. J Affect Disord. 1991;23:93–98. doi: 10.1016/0165-0327(91)90096-b. [DOI] [PubMed] [Google Scholar]
- 94.Andrieux A, Salin PA, Vernet M, Kujala P, Baratier J, et al. The suppression of brain cold-stable microtubules in mice induces synaptic defects associated with neuroleptic-sensitive behavioral disorders. Genes Dev. 2002;16:2350–2364. doi: 10.1101/gad.223302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Brun P, Begou M, Andrieux A, Mouly-Badina L, Clerget M, et al. Dopaminergic transmission in STOP null mice. J Neurochem. 2005;94:63–73. doi: 10.1111/j.1471-4159.2005.03166.x. [DOI] [PubMed] [Google Scholar]
- 96.Sollars PJ, Ogilvie MD, Rea MA, Pickard GE. 5-HT1B receptor knockout mice exhibit an enhanced response to constant light. J Biol Rhythms. 2002;17:428–437. doi: 10.1177/074873002237137. [DOI] [PubMed] [Google Scholar]
- 97.Sollars PJ, Ogilvie MD, Simpson AM, Pickard GE. Photic entrainment is altered in the 5-HT1B receptor knockout mouse. J Biol Rhythms. 2006;21:21–32. doi: 10.1177/0748730405283765. [DOI] [PubMed] [Google Scholar]
- 98.Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110. [PubMed] [Google Scholar]
- 99.Archer SN, Robilliard DL, Skene DJ, Smits M, Williams A, et al. A length polymorphism in the circadian clock gene Per3 is linked to delayed sleep phase syndrome and extreme diurnal preference. Sleep. 2003;26:413–415. doi: 10.1093/sleep/26.4.413. [DOI] [PubMed] [Google Scholar]
- 100.Viola AU, Archer SN, James LM, Groeger JA, Lo JC, et al. PER3 polymorphism predicts sleep structure and waking performance. Curr Biol. 2007;17:613–618. doi: 10.1016/j.cub.2007.01.073. [DOI] [PubMed] [Google Scholar]
- 101.Toh KL, Jones CR, He Y, Eide EJ, Hinz WA, et al. An hPer2 phosphorylation site mutation in familial advanced sleep phase syndrome. Science. 2001;291:1040–1043. doi: 10.1126/science.1057499. [DOI] [PubMed] [Google Scholar]
- 102.Xu Y, Toh KL, Jones CR, Shin JY, Fu YH, et al. Modeling of a human circadian mutation yields insights into clock regulation by PER2. Cell. 2007;128:59–70. doi: 10.1016/j.cell.2006.11.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Berrettini WH. Are schizophrenic and bipolar disorders related? A review of family and molecular studies. Biol Psychiatry. 2000;48:531–538. doi: 10.1016/s0006-3223(00)00883-0. [DOI] [PubMed] [Google Scholar]
- 104.Partonen T, Treutlein J, Alpman A, Frank J, Johansson C, et al. Three circadian clock genes Per2, Arntl, and Npas2 contribute to winter depression. Ann Med. 2007;39:229–238. doi: 10.1080/07853890701278795. [DOI] [PubMed] [Google Scholar]
- 105.Johansson C, Willeit M, Smedh C, Ekholm J, Paunio T, et al. Circadian clock-related polymorphisms in seasonal affective disorder and their relevance to diurnal preference. Neuropsychopharmacology. 2003;28:734–739. doi: 10.1038/sj.npp.1300121. [DOI] [PubMed] [Google Scholar]
- 106.Benedetti F, Serretti A, Colombo C, Barbini B, Lorenzi C, et al. Influence of CLOCK gene polymorphism on circadian mood fluctuation and illness recurrence in bipolar depression. Am J Med Genet B Neuropsychiatr Genet. 2003;123:23–26. doi: 10.1002/ajmg.b.20038. [DOI] [PubMed] [Google Scholar]
- 107.Mansour HA, Wood J, Logue T, Chowdari KV, Dayal M, et al. Association study of eight circadian genes with bipolar I disorder, schizoaffective disorder, and schizophrenia. Genes Brain Behav. 2006;5:150–157. doi: 10.1111/j.1601-183X.2005.00147.x. [DOI] [PubMed] [Google Scholar]
- 108.Nicholas B, Rudrasingham V, Nash S, Kirov G, Owen MJ, et al. Association of Per1 and Npas2 with autistic disorder: Support for the clock genes/social timing hypothesis. Mol Psychiatry. 2007;12:581–592. doi: 10.1038/sj.mp.4001953. [DOI] [PubMed] [Google Scholar]
- 109.Nievergelt CM, Kripke DF, Barrett TB, Burg E, Remick RA, et al. Suggestive evidence for association of the circadian genes PERIOD3 and ARNTL with bipolar disorder. Am J Med Genet B Neuropsychiatr Genet. 2006;141:234–241. doi: 10.1002/ajmg.b.30252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nievergelt CM, Kripke DF, Remick RA, Sadovnick AD, McElroy SL, et al. Examination of the clock gene Cryptochrome 1 in bipolar disorder: Mutational analysis and absence of evidence for linkage or association. Psychiatr Genet. 2005;15:45–52. doi: 10.1097/00041444-200503000-00008. [DOI] [PubMed] [Google Scholar]
- 111.Takao T, Tachikawa H, Kawanishi Y, Mizukami K, Asada T. CLOCK gene T3111C polymorphism is associated with Japanese schizophrenics: A preliminary study. Eur Neuropsychopharmacol. 2007;17:273–276. doi: 10.1016/j.euroneuro.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 112.Jones CR, Campbell SS, Zone SE, Cooper F, DeSano A, et al. Familial advanced sleep-phase syndrome: A short-period circadian rhythm variant in humans. Nat Med. 1999;5:1062–1065. doi: 10.1038/12502. [DOI] [PubMed] [Google Scholar]
- 113.Okawa M, Uchiyama M. Circadian rhythm sleep disorders: Characteristics and entrainment pathology in delayed sleep phase and non-24-h sleep-wake syndrome. Sleep Med Rev. 2007;11:485–496. doi: 10.1016/j.smrv.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 114.Fleming SM, Chesselet MF. Behavioral phenotypes and pharmacology in genetic mouse models of Parkinsonism. Behav Pharmacol. 2006;17:383–391. doi: 10.1097/00008877-200609000-00004. [DOI] [PubMed] [Google Scholar]