Abstract
Despite lack of convincing evidence that reduced aerobic fitness is associated with chronic back pain (CBP), exercise programs are regarded as being effective for persons with non-specific CBP. It is unsure whether gain in aerobic fitness following intervention is associated with functioning improvement in persons with CBP. The objective of this prospective cohort study was to study the impact of aerobic fitness on functioning in persons with CBP, at baseline and following 3-week intensive interdisciplinary intervention. This study included persons who had passed 8 weeks of sick-listing because of back pain (n = 94) and were referred to a 3-week intensive biopsychosocial rehabilitation program. Aerobic fitness was assessed with a sub-maximal bicycle test at baseline, at admission to and discharge from the rehabilitation program, and at 6 months follow-up. Contextual factors, body function, activity and participation were evaluated before and after intervention. In addition, working ability was recorded at 3-years follow-up. At baseline aerobic fitness was reduced in most subjects, but improved significantly following intervention. Baseline measurements and intervention effects did not differ among the diagnostic sub-groups. Neither contextual factors nor functioning at baseline were associated with aerobic fitness. Increase in aerobic fitness was not associated with improvements in functioning and contextual factors and work-return following intervention either. From this study we conclude that improvement of aerobic fitness seems of limited value as goal of treatment outcome for patients with CBP.
Keywords: Chronic low back pain, Aerobic fitness, Work-return, Multidisciplinary biopsychosocial rehabilitation, Exercise
Introduction
In order to explain persistent pain, activity limitation and participation restriction in chronic back pain (CBP), some decades ago the conceptions “disuse-” and “deconditioning syndrome” were introduced. These syndromes describe the consequences of longterm-inactivity as deficits in several physical and mental body functioning aspects, such as reduced lumbar mobility, aerobic and muscular fitness, and a higher prevalence of depression [25].
Despite the fact that there is little evidence to support the hypothesis that reduced paraspinal muscle strength and endurance is related to CBP [31], in the literature as well as in the treatment, the main focus has been on loss of muscular fitness The assumed association between aerobic fitness and CBP has been questioned as well [31]. Conflicting evidence is available that either supports or rejects an association between reduced aerobic fitness and CBP in general or within specific sub-diagnoses [4, 5, 36, 37, 42]. It is also doubtful whether persons with back pain develop aerobic deconditioning or whether reduced aerobic fitness is associated with other aspects related to CBP such as pain intensity, activity limitation, depression, fear of injury and kinesiophobia [7, 15, 26, 37, 38, 42, 43]. Furthermore, there is inconclusive evidence for the predictive value of aerobic fitness for work-return in CBP [20, 22, 24, 33]
Although in general aerobic fitness shows a dose−response relation to health outcomes [3], at present, there is modest evidence to suggest that exercise therapy and behavioural and multidisciplinary treatment programs that include exercise therapy are effective in reducing pain, improving physical functioning and activity and reducing the number of sick days in CBP [6, 19, 23, 27, 34]. Depending on intensity and duration, many of these programs for persons with CBP that include aerobic training do indeed affect aerobic fitness [28, 33, 36]. Yet, it is not inevitable that an increase in aerobic fitness has major impact on resolving the burden of CBP. Gain in aerobic fitness may be accompanied by improvements of other outcomes, but it is unclear whether these are relevant for the principal aim of intervention for CBP such as pain relief, disability reduction/functioning improvement and return to work. To our knowledge no studies have focussed on the specific value of gain in aerobic fitness for changes in other aspects of CBP before. The objective of this study was therefore to evaluate the impact of aerobic fitness on pain, functioning and some contextual variables in persons with CBP, at baseline and following an intensive interdisciplinary intervention.
Materials and methods
All inhabitants of an urban and a rural town (Sandefjord and Lardal municipality) in southern Norway who had passed 8 weeks of sick-listing1 with back pain as dominant symptom were referred to the outpatient department of the Kysthospital, Vestfold counties hospital for Physical Medicine and Rehabilitation2. All subjects were in writing and orally informed that their referral to the hospital and examination was part of the Vestfold Back Project. They went through a comprehensive diagnostic examination as an outpatient and referred to treatment if indicated [12]. All diagnostic procedures, history taking and data collection within this study were part of standard medical specialist practice and, therefore, not subjected to approval of an ethics committee.
Materials
The subjects included all persons admitted to the intervention programme during a period of 2 years. To be included in this study, the subjects had to be between 17 and 60 years of age and participators of the XXX Back Project. Two percent of the persons who were referred to the project did not show up for unknown reasons. Subjects who at the first examination (1) were not sick-listed anymore, (2) had a sickness grade less than 75%, (3) received a disability pension, (4) were pregnant, (5) were on sick leave because of back-surgery, (6) were taking medication influencing heart rate response, or (7) were employed as a civil servant3 were excluded from this study. In case of serious functional disability, either somatic or psychological, the patient was referred to a 3-week inpatient intervention program at the hospital. In addition, the patient had to be motivated for this intensive program. Of all 195 persons (98 females, 97 males) who met the primary inclusion criteria, 118 persons (61%) were referred to a 3-week inpatient intervention program at the hospital, because they were assumed to benefit from this program.
A total of 24 persons (20%) were not able to participate at the 6-months follow-up examination, mainly because of work obligations. These individuals are not included in the analysis, so, the final study group consisted of 94 subjects. There were no significant differences in baseline characteristics concerning age, gender, sub-diagnosis, and the other functioning and contextual variables between the 24 drop-outs and the included persons (data not shown). There was no difference in short-time intervention response regarding pain intensity and other body-functioning or work-return at 3-years follow-up either.
Following the initial clinical examination and medical history, the patients were divided in three categories of sub-diagnosis:
Chronic “Specific Back Pain” (SBP)—symptoms caused by a specific patho-physiological mechanism; displacement of thoracic or lumbar intervertebral disc without myelopathy (ICD 722.1), spinal stenosis (ICD 724.0), sciatica (ICD 724.3).
Chronic “Non-Specific Back Pain” (N-SBP)—symptoms without clear specific cause; spondylosis without myelopathy (ICD 721.2, 721.9), backache, unspecified (ICD 724.5).
Chronic “Widespread Pain” (WSP)—back pain as part of widespread musculoskeletal pain; myalgia (ICD 729.1). This last sub-group included persons with a fibromyalgia diagnosis according to the ACR-90 [44] criteria as well.
Baseline characteristics are presented in Table 1.
Table 1.
Subject characteristics of the three chronic back pain groups: specific (SBP), non-specific (N-SBP) and widespread (WSP)
| Characteristics | SBP | N-SBP | WSP | |||
|---|---|---|---|---|---|---|
| n | 19 | 55 | 20 | |||
| Gender (% male) | 55.6 | 52.7 | 35.0 | |||
| Age (years) (mean) | 43.3 (7.7) | 42.0 (9.7) | 40.1 (8.1) | |||
| Weight (kg) (mean) | 77.1 (11.5) | 79.0 (15.7) | 69.5 (21.3) | |||
| Current sick listing (days) (median) | 80.0 (22) | 79.0 (24) | 77.5 (20) | |||
| Time baseline—admission (days) (median) | 36.0 (89) | 28.0 (49) | 28.0 (60) | |||
| Time discharge—follow-up (days) (median) | 203.0 (17) | 196.0 (18) | 178.0 (76) | |||
| Pain duration (months) (median) | 24.0 (132) | 60.0 (185) | 41.0 (60) | |||
| Pain intensity (VAS) (mean) | 43.0 (28.3) | 41.6 (17.0) | 40.6 (15.8) | |||
| Oswestry disabilty index (mean) | 33.4 (12.9) | 25.3 (12.3) | 23.7 (12.9) | |||
| Highest education (%) | ||||||
| Primary school or less (≤8 years) | 27.8 | 56.3 | 50.0 | |||
| High school | 66.6 | 31.9 | 45.0 | |||
| College/university | 5.6 | 1.8 | 5.0 | |||
| Workload (%) | ||||||
| Sedentary | 15.8 | 11.1 | 10.0 | |||
| Light manual handling | 15.8 | 20.4 | 25.0 | |||
| Heavy manual handling | 68.5 | 68.6 | 65.0 | |||
Values are expressed as percentage, mean (with SD) or median values (with inter-quartile range)
Procedures
Data were collected at baseline, at admission (median 28 days following baseline assessment) to and discharge from the 3-week intervention program, and 6 months after discharge from the program. The medical insurance status of all subjects was registered for 3 years following initial sick-listing. Because of the short period of time between moments of data collection at baseline and at the start of the program, some variables that were not expected to change in such a short period were not repeated (Table 2).
Table 2.
Outcome measurements and moments of data collection
| Variables | Analysis | Baseline | Follow-up | ||
|---|---|---|---|---|---|
| Medical status | Out-patient | In-patient (intervention) | Out-patient | ||
| Data collection | Baseline | Admission | Discharge | Follow-up | |
| Scoring (low-high functioning) | |||||
| Contextual factors | |||||
| Sociodemograhic data | C | ||||
| Pain history | Months | C | |||
| Sick-listing duration | Days | C | |||
| Disease comprehension | 0–10 max unclear–max clear | A | × | A | |
| Social well-being—job | 0–32 always satisfied–never satisfied | A | A | ||
| Social well-being—family/friends | 0–28 always satisfied–never satisfied | A | A | ||
| Body function and structure | |||||
| Aerobic capacity | Percentage from normal | ||||
| 100 = normal value | A | A | A | A | |
| Pain intensity | 0–100 No pain-worst imaginable pain | A | × | A | |
| Lumbar flexion | Percentage from normal | ||||
| 100 = normal value | A | × | × | A | |
| Mental distress ADI | 34–170 total score | A | × | × | A |
| Activity | |||||
| Functioning—ODI | 0–100 no disability–maximum disability | A | A | ||
| Lifting capability | Number of lifts | A | × | × | A |
| Jogging capability | 0 = < 500 m, 1 = ≥ 500 m |
A | × | A | |
| Participation | |||||
| Training frequency | 0 = < 2×/week, 1 = ≥ 2×/week |
A | A | ||
| Work ability—3 years after start sick-listing | 0 = workability < 25%, 1 = workability ≥ 25% |
A | A | ||
‘C’ indicates measurement only used for subject characteristics. ‘'A’ indicates measurement included for analysis, ‘×’ indicates measurement not used for analysis
Assessment of aerobic fitness
Aerobic fitness was assessed with “Åstrands sub-maximal 6-min protocol” [2] on a cycle ergometer (Siemens, Ergomed 840) with such a workload that after 6-min heart rate reached values between 120 and 170 beats/min. Heart rate was recorded at a 5 s interval with Sport Tester TM PM-3000 (Polar Electro). From mean heart rate and workload in the last minute, maximal oxygen uptake per kg body weight was estimated with the Åstrand nomogram [2]. Results were expressed as a percentage from normal values [10].
Assessment of contextual factors
Sociodemograhic data, and pain history were evaluated by a simple questionnaire. Comprehension concerning back pain origin and treatment were assessed at a ten-point Likert scale. Sick-listing duration was obtained from the Sickness register of the local offices of the National Insurance Scheme. Satisfaction with social aspects of life (family/friends and work) was evaluated by APGAR test (Adaptation, Partnership, Growth, Affection, and Resolve) [32].
Assessment of functioning
To quantify Body Structure and Function impairment, pain intensity was assessed by a 100 mm horizontal visual analogue scale (VAS). Lumbar spine flexion was assessed with an electronic digital inclinometer by measuring differences between range of motion in flexion in sacrum and T12-L1 [17]. To quantify mental distress, the anxiety, depression and irritability scheme (ADI) was used [13]. Only total scores were considered in this study. Back pain related activity limitation was assessed with the oswestry low back pain disability index (ODI) [9]. Ability to run was measured with a question from the Norwegian questionnaire “Sports, Leisure time and Living circumstances” [8]. Practical physical performance was evaluated with a standardised lifting test. Lifting technique was optional [41]. The number of lifts was recorded.
Participation restriction was assessed by checking out workability (workable vs. sick-listing or permanent disablement) from the records of the local offices of the National Insurance Scheme, 3 years following initial sick leave. In addition, training habits were evaluated with an item from the Norwegian questionnaire “Sports, Leisure time and Living circumstances” [8].
Intervention
The intervention, an intensive interdisciplinary biopsychosocial rehabilitation, was based on a functional restoration program and took its starting point from a cognitive–behavioural and functional approach in which treatment is guided by functioning instead of pain [25, 39]. An important message was that “hurt does not mean harm”.
The main aim of the treatment was to reduce disability and dysfunctional behaviour and to increase empowerment and participation in life situations by removing fear and uncertainty and increasing physical body functioning and activity.
The treatment consisted of a 3-week inpatient program with daily 6–8 h of activities, individually or in groups. The cognitive–behavioural approach was covered in the training, educational program and individual counselling with members of the multidisciplinary team. The physical training was based on the sports medicine approach, i.e. exercise with low intensity and many repetitions, with gradually increased intensity during the training period, aimed at an increase in aerobic fitness, strength and flexibility. They were encouraged to use their backs freely. Reinforcement of this message was incorporated in all activities with the aim of influencing their attitudes.
After the inpatient program, the patients were encouraged to continue exercising. Although our inpatient program consisted of indoor activities as well, outdoor activities were promoted in accordance with Norwegian traditions. Sophisticated fitness training equipment was not used out of the philosophy that the follow-up training would be easier if the patients were less dependent on extensive fitness equipment for their physical training.
Data analyses
Aerobic fitness and lumbar flexibility were related to adjusted normative data [10, 25] (raw data score/normal values × 100%), considering age and gender, and for aerobic fitness for bodyweight as well. A value of 100% indicates a result equal to the gender specific population average and values below 100% indicate effort below normal.
Change scores (difference between admission and discharge or between admission and follow-up) were calculated for all outcome measures. In case of missing data, data collected at admission to the intervention were replaced by baseline-data and data collected at discharge were replaced by follow-up data and vice versa. The analyses were performed with SPSS 15.0 software.
To assess whether the estimated values for aerobic fitness deviated from normative data a one-sample t test was used (test value = 100). For sociodemographic data and aerobic fitness, differences between the three diagnostic categories were evaluated. For factors measured at an interval and ratio scale, oneway-Anova was applied and for nominal data Pearson Chi-square. To assess the effect of the intervention program on aerobic fitness and the other factors a paired-samples t test or Wilcoxon test for paired data was used.
The association between aerobic fitness and the other measures were calculated with the estimation of Pearsons correlation coefficients (r). Difference in aerobic fitness in persons with unlike future work status (workable vs. not workable) was analysed with Independent-Samples t tests.
P < 0.05 were considered as being statistically significant. For the correlation analyses (Table 4), a Bonferroni correction was used because of multiple testing (k = 33). In these analyses the level of significance was set to 0.002
Table 4.
Pearson correlation coefficients evaluating association between aerobic fitness and functioning and contextual factors at baseline, at follow-up and the correlation coefficient between changes in aerobic fitness and changes in Functioning and contextual factors following intervention
| Baseline | Follow-up | Intervention changes (discharge-admission) | |
|---|---|---|---|
| Contextual factors | |||
| Disease comprehension (0–10) | 0.118 | 0.081 | −0.050 |
| APGAR family/friends (0–16) | −0.237 | −0.234 | −0.228 |
| APGAR job (0–28) | 0.121 | 0.001 | −0.097 |
| Body function | |||
| Pain intensity (0–100) | 0.110 | −0.059 | −0.108 |
| Lumbar flexion (normal = 100) | 0.276* | 0.149 | 0.093 |
| Mental distress (total score 34–170) | −0.043 | −0.078 | 0.064 |
| Activity | |||
| Oswestry (0–100) | −0.108 | −0.042 | 0.139 |
| Lifting | 0.060 | 0.064 | −0.120 |
| Jogging > 500 m (0/1) (%) | 0.047 | −0.023 | 0.143 |
| Participation | |||
| Training ≥ 2× week (0/1) (%) | 0.101 | −0.041 | 0.106 |
| Workability 3 years later (0/1) (%) | 0.037 | 0.032 | 0.034 |
* P = 0.008, but, because of multiple testing, the level of significance was set to 0.002
Results
Baseline
The persons with CBP, showed significantly reduced values for aerobic fitness compared to normative data (Table 3). Reduction was significantly greater in men (25%) than in women (13%), (P = 0.004). Aerobic fitness seemed not associated with pain duration or sub-group diagnosis.
Table 3.
Aerobic fitness at baseline and discharge (VO2max estimated from Åstrand nomogram and % from normal) in all patients and in patients with specific back pain (SBP), non-specific back pain (N-SBP) and widespread pain (WSP)
| All subjects | SBP | N-SBP | WSP | |||||
|---|---|---|---|---|---|---|---|---|
| Female n = 48 | Male n = 46 | Female n = 9 | Male n = 10 | Female n = 26 | Male n = 29 | Female n = 13 | Male n = 7 | |
| Aerobic fitness—baseline | ||||||||
| VO2max estimated (ml/kg) | 27.8 | 29.7 | 26.0 | 28.4 | 26.5 | 30.7 | 31.2 | 27.4 |
| Percentage of normative data | 86.7 | 74.6 | 80.1 | 72.0 | 84.7 | 76.4 | 95.2 | 71.2 |
| Aerobic fitness—discharge | ||||||||
| VO2max estimated (ml/kg) | 30.2 | 33.6 | 27.5 | 31.2 | 29.2 | 35.1 | 33.9 | 30.8 |
| Percentage of normative data | 95.0 | 80.4 | 87.2 | 80.5 | 94.2 | 81.2 | 102.0 | 77.2 |
| P-value—gender difference | 0.004 | 0.346 | 0.228 | 0.029 | ||||
| P-value—sub-diagnosis difference | 0.259 | 0.498 | ||||||
| P-value—compared to normal (=100) | 0.000 | 0.000 | 0.057 | 0.000 | 0.000 | 0.000 | 0.397 | 0.000 |
| Pearson correlation coefficient | ||||||||
| Aerobic fitness—pain duration | −0.081 | −0.005 | −0.156 | 0.102 | ||||
| P-value—correlation—pain duration | 0.445 | 0.985 | 0.261 | 0.669 | ||||
P-values for group differences in aerobic fitness at baseline concerning gender, diagnostic sub-group and compared to normal. Pearson correlations between aerobic fitness and pain duration at baseline
Aerobic fitness was not correlated with other functioning measures and contextual factors (Table 4) at baseline either. Only lumbar flexion showed a tendency to be moderately correlated (r = 0.276, P = 0.008, not significant) with aerobic fitness at baseline.
Intervention response
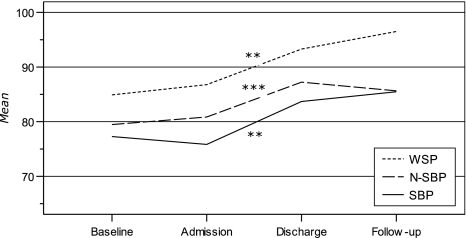
Irrespective of diagnostic sub-group, aerobic fitness improved significantly after intervention with 12.6% in the group of persons with specific back pain, 9.7% in non-specific back pain and 7.8% in persons with widespread pain (Fig. 1). However, aerobic fitness was still significantly below (20%) normal values in male patients. No additional improvements or relapse was seen during the follow-up period.
Fig. 1.
Aerobic fitness (% from normal)—intervention response, in patients with specific back pain (SBP), non-specific back pain (N-SBP) and widespread pain (WSP). P-values evaluate significant changes. ** P ≤ 0.05, *** P ≤ 0.01
In addition, pain intensity (42.6–36.4, P = 0.044) and ODI (26.4–20.2), P < 0.0005) decreased and the other body function and activity performance measures, social-well-being at work and disease comprehension increased significantly following intervention.
After intervention, aerobic fitness was not correlated with any of the other functioning and contextual factors, nor did the improvements in aerobic fitness correlate with improvement in any of the other factors (see Table 4).
Predictive value for future work status
At 3 years following initial sick-listing, 31.6% of persons with SBP, 30.9% of persons with N-SBP and 20.0% of the persons with WSP were, again or still, sick-listed or were permanently disabled (not-workable).
Aerobic fitness at baseline, after intervention and gain in aerobic fitness following intervention did not differ between the persons who were not on sick leave anymore (workable) and those who were not workable 3 years later (Table 5).
Table 5.
Differences in aerobic fitness at baseline, discharge and change in aerobic fitness between patients who are not-workable/workable, 3 years following baseline measurement, in patients with specific back pain (SBP), non-specific back pain (N-SBP) and widespread pain (WSP)
| Aerobic fitness—baseline | Aerobic fitness—discharge | Aerobic fitness—% change | |||||||
|---|---|---|---|---|---|---|---|---|---|
| SBP | N-SBP | WSP | SBP | N-SBP | WSP | SBP | N-SBP | WSP | |
| Sick-listed or permanent disability | 80.4 | 78.4 | 83.5 | 86.3 | 86.6 | 87.5 | 5.9 | 6.4 | 4.3 |
| Workable | 73.8 | 81.1 | 87.6 | 82.5 | 87.5 | 94.7 | 8.7 | 6.4 | 7.1 |
| P-value | 0.440 | 0.647 | 0.766 | 0.640 | 0.888 | 0.653 | 0.681 | 0.993 | 0.657 |
Discussion
Exercises are a central component in almost all multidisciplinary treatment programs for CBP patients [11, 30]. In recent reviews on exercise therapy the specific value of aerobic exercises could not be evaluated since only a minority of the studies had specifically used aerobic exercises [1, 14].
In this study, sub-maximal cycle-ergometry was chosen to estimate aerobic fitness. Maximal work tests in these persons may rather represent a measure of activity limitation rather than a real impairment of aerobic capacity. Because of a high degree of psychological distress, pain and disability CBP patients often tend to overrate their actual individual effort and do not achieve maximal effort [16, 29, 35, 40]. A sub-maximal test or comparison of anaerobic threshold seems therefore preferable. Although indirect measurement introduces limitation in inter-subject accuracy the reliability for the Åstrand protocol and nomogram is found to be acceptable in persons with CBP [18]. This was confirmed in our study, since aerobic fitness did not change in the pre-intervention period.
Aerobic fitness is strongly related to gender, age and bodyweight. To compare groups fairly, we related estimated maximal oxygen uptake per kg body weight for each individual to normative data. Because of the absence of updated Norwegian normative data for oxygen uptake, an American database was used to relate our results to [10]. Despite the fact that American normative data of aerobic fitness tends to underestimate Scandinavian values, aerobic fitness in our population seemed below normative values at baseline and comparable with a similar Norwegian back pain population [5]. These results seem to support the assumption of an association between reduced aerobic fitness and CBP. After intervention aerobic fitness was only reduced in male patients.
In case poor aerobic fitness in sick-listed persons with CBP is acknowledged, still it is unsure whether this is specifically related to biological or behavioural aspects of CBP or to other characteristics of this population. It has been shown before that low education, unemployment, retirement, as well as blue-collar work is associated with reduced values of maximal oxygen uptake [21]. It deserves notice that these characteristics correspond very well to the sociodemographics of the subjects evaluated in this paper [45]. The association of specific sociodemographic characteristics with aerobic fitness, CBP and long-lasting sickness in general need to be evaluated further.
As expected, aerobic fitness improved significantly following intervention. Though, since neither this gain in aerobic fitness nor its baseline values were related to other functioning improvements, aerobic fitness may not be considered as essential for intervention success. Increase in aerobic fitness as aim of treatment in CBP seems therefore of limited value since gain in aerobic fitness is not one of the primary outcomes for CBP management.
However, this conclusion does not tell us anything about the value of aerobic exercise training for general health benefit and for essentially cognitive behavioural effects. Apart from physical benefits, exercise may rather be effective as an approach for affecting behavioural, cognitive, affective and disability components of CBP [27]. As we know, such factors play crucial roles in the development and maintenance of CBP. Verbunt et al. [38] found that aerobic fitness neither was correlated to disability nor to fear of injury, they did find a significant correlation between fear of injury and disability. Exercise may therefore be useful for reducing back-pain related disability as a tool to lessen excessive fear and concerns about back pain and alter maladaptive pain attitudes, beliefs and behaviour. Probably these are the factors which mediate functioning and participation improvement, including return to work. It is therefore of importance to consider the impact of treatment on these factors. Unfortunately, back pain beliefs and consequential avoidance behaviour were not evaluated in this study.
Conclusion
We conclude that intensive interdisciplinary biopsychosocial rehabilitation increased the reduced aerobic fitness of persons with different sub-diagnoses of CBP. However, this improvement was not associated with improvement in any other physical and mental functioning, social well-being or return to work. The results of this study suggest that focus on the cognitive–behavioural approach in the intervention is more important to improve results than adding a functional approach and increasing physical fitness. Improvement of aerobic fitness seems of limited value as goal of treatment outcome for persons with CBP.
Footnotes
All residents in Norway are required to be members of the National Social Insurance Scheme. Individuals with a sickness leave exceeding 3 days need a sickness certificate from their primary physician. Individuals with more than 8 weeks of sickness leave must be issued the Sickness Certificate II to be eligible for more sickness benefits.
Now: Hospital for Rehabilitation—Stavern, Rikshospitalet Medical Centre
For civil servants there are no detailed data registered at the local National Social Insurance offices.
References
- 1.Abenhaim L, Rossignol M, Valat JP, Nordin M, Avouac B, Blotman F, Charlot J, Dreiser RL, Legrand E, Rozenberg S, Vautravers P. The role of activity in the therapeutic management of back pain. Report of the International Paris Task Force on Back Pain. Spine. 2000;25:1S–33S. doi: 10.1097/00007632-200002151-00001. [DOI] [PubMed] [Google Scholar]
- 2.Åstrand P-O, Rodahl K. Textbook of work physiology. Physiological bases of exercise. Singapore: McGraw-Hill; 1987. [Google Scholar]
- 3.Blair SN, Cheng Y, Holder JS. Is physical activity or physical fitness more important in defining health benefits? Med Sci Sports Exerc. 2001;33:S379–S399. doi: 10.1097/00005768-200105001-01549. [DOI] [PubMed] [Google Scholar]
- 4.Brennan GP, Ruhling RO, Hood RS, Shultz BB, Johnson SC, Andrews BC. Physical characteristics of patients with herniated intervertebral lumbar discs. Spine. 1987;12:699–702. doi: 10.1097/00007632-198709000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Brox JI, Storheim K, Holm I, Friis A, Reikeras O. Disability, pain, psychological factors and physical performance in healthy controls, patients with sub-acute and chronic low back pain: a case-control study. J Rehabil Med. 2005;37:95–99. doi: 10.1080/16501970410017738. [DOI] [PubMed] [Google Scholar]
- 6.COST B13 Working Group on Guidelines for Chronic Low Back Pain. European guidelines for the management of chronic non-specific low back pain (2004) European Commission Research Directorate General
- 7.Cunha IT, Simmonds MJ, Protas EJ, Jones S. Back pain, physical function, and estimates of aerobic capacity: what are the relationships among methods and measures? Am J Phys Med Rehabil. 2002;81:913–920. doi: 10.1097/00002060-200211000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Danielsen Ø (1989) Den nye bredde idretten. Ønsker og behov for fysisk aktivitet. 3. Delrapport for prosjektet ‘Idrett, fritid og levekår’. 088. Oslo, Fafo
- 9.Fairbank JC, Davies JB, Couper J, O’Brian JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–272. [PubMed] [Google Scholar]
- 10.Fletcher GF, Balady GJ, Amsterdam EA, Chaitman B, Eckel R, Fleg J, Froelicher VF, Leon AS, Pina IL, Rodney R, Simons-Morton DA, Williams MA, Bazzarre T. Exercise standards for testing and training: a statement for healthcare professionals from the American Heart Association. Circulation. 2001;104:1694–1740. doi: 10.1161/hc3901.095960. [DOI] [PubMed] [Google Scholar]
- 11.Guzman J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C (2002) Multidisciplinary bio-psycho-social rehabilitation for chronic low back pain. Cochrane Database Syst Rev. CD000963 [DOI] [PubMed]
- 12.Haldorsen EMH, Wormgoor MEA, Bjørholt PG, Ursin H. Predictors for outcome of a functional restoration program for low back patients- A 12 month follow-up study. Eur J Phys Med Rehabil. 1998;8:103–109. [Google Scholar]
- 13.Havik OE, Mæland JG. ADI-skjemaet. Reliabilitet og validitet for et kort spørreskjema rettet mot angst, depresjon og irritabilitet. Tidsskrift for Norsk Psykologforening. 1983;20:70–78. [Google Scholar]
- 14.Hayden J, Tulder M, Malmivaara A, Koes B (2005) Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev. CD000335 [DOI] [PMC free article] [PubMed]
- 15.Hurri H, Mellin G, Korhonen O, Harjula R, Harkapaa K, Luoma J. Aerobic capacity among chronic low-back-pain patients. J Spinal Disord. 1991;4:34–38. [PubMed] [Google Scholar]
- 16.Hutten MM, Hermens HJ, Ijzerman MJ, Lousberg R, Zilvold G. Distribution of psychological aspects in subgroups of chronic low back pain patients divided on the score of physical performance. Int J Rehabil Res. 1999;22:261–268. doi: 10.1097/00004356-199912000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Keeley J, Mayer TG, Cox R, Gatchel RJ, Smith J, Mooney V. Quantification of lumbar function. Part 5: Reliability of range-of-motion measures in the sagittal plane and an in vivo torso rotation measurement technique. Spine. 1986;11:31–35. doi: 10.1097/00007632-198601000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Keller A, Hellesnes J, Brox JI. Reliabilty of the isokinetic trunk extensor test, Biering-Sørensen test, and Åstrand bicycle test. Assessment of intraclass correlation coefficient and critical difference in patients with chronic low back pain and healthy individuals. Spine. 2001;26:771–777. doi: 10.1097/00007632-200104010-00017. [DOI] [PubMed] [Google Scholar]
- 19.Kool J, Bie R, Oesch P, Knusel O, Brandt P, Bachmann S. Exercise reduces sick leave in patients with non-acute non-specific low back pain: a meta-analysis. J Rehabil Med. 2004;36:49–62. doi: 10.1080/16501970310020104. [DOI] [PubMed] [Google Scholar]
- 20.Koopman FS, Edelaar M, Slikker R, Reynders K, Woude LH, Hoozemans MJ. Effectiveness of a multidisciplinary occupational training program for chronic low back pain: a prospective cohort study. Am J Phys Med Rehabil. 2004;83:94–103. doi: 10.1097/01.PHM.0000107482.35803.11. [DOI] [PubMed] [Google Scholar]
- 21.Lakka TA, Kauhanen J, Salonen JT. Conditioning leisure time physical activity and cardiorespiratory fitness in sociodemographic groups of middle-ages men in eastern Finland. Int J Epidemiol. 1996;25:86–93. doi: 10.1093/ije/25.1.86. [DOI] [PubMed] [Google Scholar]
- 22.LeFort SM, Hannah TE. Return to work following an aquafitness and muscle strengthening program for the low back injured. Arch Phys Med Rehabil. 1994;75:1247–1255. doi: 10.1016/0003-9993(94)90014-0. [DOI] [PubMed] [Google Scholar]
- 23.Liddle SD, Baxter GD, Gracey JH. Exercise and chronic low back pain: what works? Pain. 2004;107:176–190. doi: 10.1016/j.pain.2003.10.017. [DOI] [PubMed] [Google Scholar]
- 24.Ljungkvist I. Short- and long-term effects of a 12-week intensive functional restoration programme in individuals work-disabled by chronic spinal pain. Scand J Rehab Med. 2000;40:1–14. [PubMed] [Google Scholar]
- 25.Mayer TG, Gatchel RJ. Functional restoration for spinal disorders: the sports medicine approach. Philadelphia: Lea Febiger; 1988. [Google Scholar]
- 26.McQuade KJ, Turner JA, Buchner DM (1988) Physical fitness and chronic low back pain. An analysis of the relationships among fitness, functional limitations, and depression. Clin Orthop Relat Res 233:198–204 [PubMed]
- 27.Rainville J, Hartigan C, Martinez E, Limke J, Jouve C, Finno M. Exercise as a treatment for chronic low back pain. Spine J. 2004;4:106–115. doi: 10.1016/S1529-9430(03)00174-8. [DOI] [PubMed] [Google Scholar]
- 28.Robert JJ, Blide RW, McWhorter K, Coursey C. The effects of a work hardening program on cardiovascular fitness and muscular strength. Spine. 1995;20:1187–1193. doi: 10.1097/00007632-199505150-00014. [DOI] [PubMed] [Google Scholar]
- 29.Schmidt AJ. Cognitive factors in the performance level of chronic low back pain patients. J Psychosom Res. 1985;29:183–189. doi: 10.1016/0022-3999(85)90040-6. [DOI] [PubMed] [Google Scholar]
- 30.Schonstein E, Kenny D, Keating J, Koes B, Herbert RD. Physical conditioning programs for workers with back and neck pain: a cochrane systematic review. Spine. 2003;28:E391–E395. doi: 10.1097/01.BRS.0000092482.76386.97. [DOI] [PubMed] [Google Scholar]
- 31.Smeets RJ, Wade D, Hidding A, Leeuwen PJ, Vlaeyen JW, Knottnerus JA. The association of physical deconditioning and chronic low back pain: a hypothesis-oriented systematic review. Disabil Rehabil. 2006;28:673–693. doi: 10.1080/09638280500264782. [DOI] [PubMed] [Google Scholar]
- 32.Smilkstein G, Ashworth C, Montano D. Validity and reliability of the family APGAR as a test of family function. J Fam Pract. 1982;10:311. [PubMed] [Google Scholar]
- 33.Storheim K, Brox JI, Holm I, Bo K. Predictors of return to work in patients sick listed for sub-acute low back pain: a 12-month follow-up study. J Rehabil Med. 2005;37:365–371. doi: 10.1080/16501970510040344. [DOI] [PubMed] [Google Scholar]
- 34.Hayden JA, van Tulder MW, Malmivaara A, Koes BW (2005) Exercise therapy for treatment of non-specific low back pain. Cochrane Database of Systematic Reviews, Issue 3. Art. No.: CD000335. doi:10.1002/14651858. Pub 2. [DOI] [PMC free article] [PubMed]
- 35.Valim V, Oliveira LM, Suda AL, Silva LE, Faro M, Neto TL, Feldman D, Natour J. Peak oxygen uptake and ventilatory anaerobic threshold in fibromyalgia. J Rheumatol. 2002;29:353–357. [PubMed] [Google Scholar]
- 36.Velde G, Mierau D. The effects of exercise on percentile rank aerobic capacity, pain, and sef-rated disability in patients with chronic low-back pain: A retrospective chart review. Arch Phys Med Rehabil. 2000;81:1457–1463. doi: 10.1053/apmr.2000.9629. [DOI] [PubMed] [Google Scholar]
- 37.Verbunt JA, Seelen HA, Vlaeyen JW, Heijden GJ, Heuts PH, Pons K, Knottnerus JA. Disuse and deconditioning in chronic low back pain: concepts and hypotheses on contributing mechanisms. Eur J Pain. 2003;7:9–21. doi: 10.1016/S1090-3801(02)00071-X. [DOI] [PubMed] [Google Scholar]
- 38.Verbunt JA, Seelen HA, Vlaeyen JW, Heijden GJ, Knottnerus JA. Fear of injury and physical deconditioning in patients with chronic low back pain. Arch Phys Med Rehabil. 2003;84:1227–1232. doi: 10.1016/S0003-9993(03)00132-1. [DOI] [PubMed] [Google Scholar]
- 39.Waddell G. A new clinical model for the treatment of low back pain. Spine. 1987;12:632–644. doi: 10.1097/00007632-198709000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Wallbom AS, Geisser ME, Haig AJ, Yamakawa K, Montgomery D. Concordance between rating of perceived exertion and function in persons with chronic, disabling back pain. J Occup Rehabil. 2002;12:93–98. doi: 10.1023/A:1015060530414. [DOI] [PubMed] [Google Scholar]
- 41.Wie SL (1996) An evaluation of lifting function in persons with low-back pain. An assessment and evaluation of the reliability and validity of the dynamic lift test “Kystatesten Lifting-low.” Master’s thesis. Bergen: University of Bergen. (GENERIC)Ref Type: Thesis/Dissertation
- 42.Wittink H, Hoskins MT, Wagner A, Sukiennik A, Rogers W. Deconditioning in patients with chronic low back pain: fact or fiction? Spine. 2000;25:2221–2228. doi: 10.1097/00007632-200009010-00013. [DOI] [PubMed] [Google Scholar]
- 43.Wittink H, Michel TH, Sukiennik A, Gascon C, Rogers W. The association of pain with aerobic fitness in patients with chronic low back pain. Arch Phys Med Rehabil. 2002;83:1467–1471. doi: 10.1053/apmr.2002.34597. [DOI] [PubMed] [Google Scholar]
- 44.Wolfe F, Multicenter Criteria Committee The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis Rheum. 1990;33:160–172. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 45.Wormgoor ME, Indahl A, Tulder MW, Kemper HC. Functioning description according to the icf model in chronic back pain: disablement appears even more complex with decreasing symptom-specificity. J Rehabil Med. 2006;38:93–99. doi: 10.1080/16501970510044052. [DOI] [PubMed] [Google Scholar]