Abstract
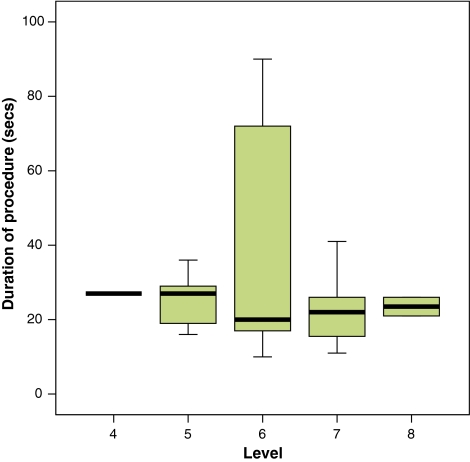
Several techniques have been described for selective nerve root blocks. We describe a novel ‘two-needle technique’, performed through the postero-lateral route with the patient in lateral position under C-arm guidance. The aim of the current study is to highlight the effectiveness and safety of cervical selective nerve root block for radiculopathy using this technique. We present results of a retrospective 2-year follow-up study of 33 injections carried out on 33 patients with radiculopathy due to cervical disc disease and or foraminal stenosis using this procedure. Patients with myelopathy, gross motor weakness and any other pathology were excluded. The outcome was measured comparing ‘Visual Analogue Score’ (VAS) and ‘Neck Disability Index’ (NDI) before the procedure with those at 6 weeks and 12 months after the procedure. Thirty patients were included in the final analysis. Average pre-operative VAS score was 7.4 (range 5–10), which improved to 2.2 (range 0–7) at 6 weeks and 2.0 (range 0–4) at 1 year and the mean NDI score prior to intervention was 66.9 (range 44–84), which improved to 31.7 (range 18–66) at 6 weeks and 31.1 (range 16–48) at 1 year. The improvements were statistically significant. Patients with involvement of C6 or C7 nerve roots responded slightly better at 6 weeks with regards to VAS improvement. Mean duration of radiation exposure during the procedure was 27.8 s (range 10–90 s). Only minor complications were noted—transient dizziness in two and transient nystagmus in one patient. Our ‘two-needle technique’ is a new, safe and effective non-surgical treatment for cervical radiculopathy.
Keywords: Cervical radiculopathy, Selective nerve root block, Two-needle technique, Steroid, Cervical spondylosis
Introduction
Cervical radiculopathy is a disabling condition frequently encountered in spinal practice. Average annual age-adjusted incidence is estimated to be about 83.2 per 100,000 population [1]. Cervical radiculopathy can be due to degenerative conditions such as cervical disc prolapse alone (20–25% of cases). It is more commonly due to a combination of factors, which include disc herniation, osteoarthritis of uncovertebral and facet joints, decreased disc height and spondylolisthesis of cervical vertebrae - collectively known as cervical spondylosis [1]. Rarer causes include nerve root compression by tumour or due to cervical trauma.
The natural course of radiculopathy due to degenerative aetiologies is generally favourable, with a majority of patients reporting spontaneous resolution of symptoms over a period of time [1, 2]. In a study involving a cohort of 51 patients with cervical radiculopathy managed non-operatively, review at 10 years revealed that 42% were asymptomatic, 30% had mild symptoms and 28% moderate symptoms [3]. Similar favourable natural resolution of symptoms was also reported in a large population based study from Rochester, Minnesota [1]. A minority of patients, in whom natural resolution of symptoms is not seen, do have persistent disabling pain requiring some form of intervention. Surgical treatment is generally reserved for unremitting and severe pain in patients in whom nonoperative treatment has failed [4, 5]. One effective modality of treatment for patients with unremitting pain is injection of steroid and local anaesthetic in the nerve root foramen into the peri-radicular space - cervical foraminal ‘selective nerve root block’ (SNRB) [6–10]. Here we describe a method of SNRB using a ‘two-needle technique’ with a 2-year follow-up of 30 patients in our centre.
Patients and methods
The study was carried out on 33 consecutive patients who underwent SNRB for cervical radiculopathy between January 2002 and January 2004. Majority of the patients at the time of presentation to the senior author (NK) had been managed initially with rest, analgesia and physiotherapy for at least 2 months by their general practitioner. Patients presenting with acute and severe symptoms resistant to conservative management were considered for root block earlier. Initial clinical assessment included detailed neurological examination and plain radiographs of the cervical spine. Magnetic resonance imaging (MRI) was performed on all patients for confirmation of the clinical diagnosis. Patients whose MRI findings were consistent with the clinical diagnosis were offered SNRB. The nerve roots involved in these patients were from C4 to C8. Patients presenting with motor power less than Medical Research Council (MRC) grade 4 and those in whom the pain pattern did not correlate with the radiological findings were not offered SNRB. Pregnant women and patients with cervical myelopathy, malignancy, inflammatory disease, coagulation disorder or sensitivity to corticosteroids were also excluded. None of the patients who underwent the procedure had any pending litigation related to the condition.
The outcome was measured using ‘neck disability index’ (NDI) and an 11—block ‘visual analogue scale’ (VAS) ranging from 0 (no pain) to 10 (maximal pain). The neck disability index is a negatively incremental score consisting of ten questions related to patients’ activities of daily living as well as work and recreational activities. These quantify the pain and physical limitations due to cervical radiculopathy. This score has been used as an outcome measure following non-operative [11, 12] as well as operative treatments [13–16] for cervical radiculopathy and has been shown to be reliable and valid [17]. All the patients were initially scored on the day of procedure using NDI questionnaire and VAS chart. Follow-up scores were done at 6 weeks and 1 year after the procedure at the time of their clinical review. All the patients were asked if the pain relief started within 24–48 h following the procedure. The degree of pain relief was measured by reduction in VAS score and the functional improvement by reduction in NDI. The final follow up was 2 years after the procedure and the patients were discharged if there was no deterioration in symptoms.
Technique
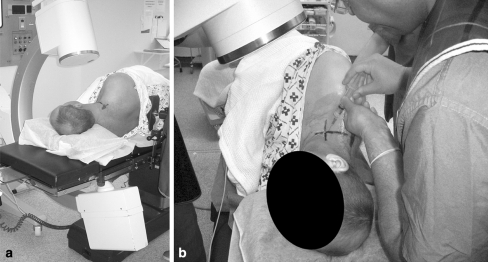
The selective nerve root block is done as a day case procedure by the senior author (NK). The procedure is explained to the patient and informed consent is obtained. This procedure is done in the operating theatre on an awake patient. The patient is placed in the lateral position on the operating table with the symptomatic side facing up. One or two pillows are placed under the head to prevent lateral flexion of the cervical spine. The neck is slightly extended and the patient is requested to depress both shoulders. This position helps to visualise the entire cervical spine in a majority of patients. The image intensifier C-arm (Phillips BV Libra) is centred on the relevant level and tilted by 20°–30° in order to obtain oblique projections of the cervical spine (Fig. 1a). This would show the neural foramen end-on (Fig. 2a). A metallic ruler is placed transversely on the patient’s neck, so that it projects at the upper border of the nerve root foramen of the level to be injected and parallel to the disc space. A horizontal line is drawn on the skin at this level. A vertical line is drawn joining the posterior borders of the lateral masses of the adjacent vertebrae. Intersection of these lines gives us the entry point for the needle (Fig. 1b), which overlies the bulk of the trapezius muscle and falls in the posterior triangle of the neck.
Fig. 1.
a Showing the position of patient and image intensifier. b Skin marking for the entry point
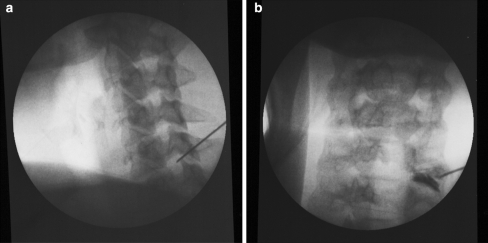
Fig. 2.
a End-on view of the neural foramen seen on oblique X-ray. Tip of the needle is in the postero-superior quadrant of the foramen. b AP view of the same showing epidurogram
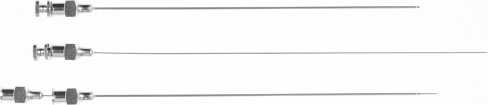
The injection site is aseptically prepared and local anaesthetic (2% lignocaine–Xylocaine® AstraZeneca, UK) is infiltrated into skin and subcutaneous tissues. For the ‘two-needle technique’ we use a 0.9 mm × 125 mm needle as the ‘outer needle’ and 0.45 mm × 150 mm needle as the ‘inner needle’ (Steriseal®–Unomedical, UK) (Fig. 3). The outer needle is well suited to negotiate the skin, deep fascia and muscle layers without bending. The 0.9 mm needle with stylet is introduced through the entry point on the skin and directed using image guidance through the bulk of the trapezius muscle, keeping it posterior to the neurovascular bundle of the neck. The needle is advanced under image guidance until the tip of the needle is just antero-lateral to the posterior border of neural foramen, without actually entering it (Fig. 4). An AP view is also obtained at this stage. The stylet is removed and the inner needle is inserted through the lumen of the outer needle. The inner needle is advanced with caution, to enter the nerve root canal under image guidance, observing the patient’s response. In a majority of patients, radicular pain is reproduced at this point, which usually matches their clinical symptoms. Aspiration is attempted with a 5 mL syringe to ensure that the needle tip is not in any blood vessel. 0.2–0.5 mL of radio-opaque dye (Iopamidol–Niopam 200® Bracco UK Ltd) is injected through the inner needle to obtain an epidurogram, showing spread of the contrast medium along the nerve root. A hard copy of the epidurogram (Fig. 2b) is printed for record. A mixture of 1 mL of long acting steroid (40 mg Triamcinolone acetonide–Kenalog®–Squibb UK) and 1.0–1.5 mL of long acting local anaesthetic (0.25% Bupivacaine–Marcaine®, AstraZeneca, UK) is injected through the needle into the peri-radicular space. The radiation exposure time for each procedure is recorded. The patient is observed for 4–6 h following the procedure and then discharged.
Fig. 3.
The two needles used in our technique. The top two pictures show the needles with stylets in situ. The bottom picture shows the long 0.45 mm diameter needle being passed through the lumen of shorter 0.9 mm needle
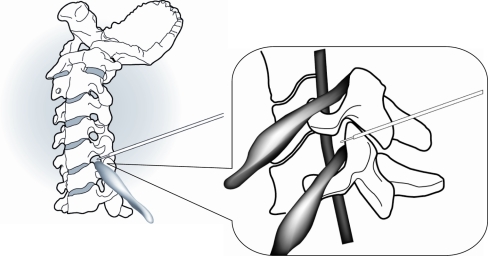
Fig. 4.
The safe zone—schematic diagram showing relationship between the tip of needle, the nerve root and the vertebral artery at the nerve root foramen. The safe zone refers to postero-superior quadrant of nerve root foramen as seen on oblique view. Note that only the 0.45 mm diameter needle is used to negotiate the nerve root foramen in the bony confines
Statistical methods
The demographic data, duration of symptoms at presentation, nerve root involved, radiation exposure time for procedure and the improvement in outcome measures (NDI and VAS) at 6 weeks and 1 year were analysed using SPSS software package (SPSS v14.0 for windows, SPSS inc., Chicago, IL, USA).
Paired sample t test was used to analyse the improvement in VAS and NDI scores. The influence of underlying diagnosis, side of involvement and gender was studied using independent sample t test and one way ANOVA was used to correlate the effect of level of nerve root involved to the improvement in outcome measures. Pearson’s correlation coefficient was used to study the influence of duration of symptoms at presentation, duration of radiation exposure and age of the patient on the improvement in outcome indicators.
Results
During the 24-month period, 33 patients underwent cervical foraminal selective nerve root block (SNRB) with the ‘two-needle technique’. Two patients were lost to follow-up and another patient had dual pathology of cervical disc prolapse and cervical rib on the same side, which left us with 30 patients for evaluation with a minimum 2-year follow-up. The patient with dual pathology underwent excision of cervical rib and hence was excluded from this study. Two patients underwent surgical intervention due to poor response after 6 weeks; hence outcome scores at 6 weeks are for 30 patients, whereas those at 1 year are for 28 patients.
There were 14 males and 16 females, with an average age of 44.7 years (range 25–67). Mean duration of symptoms before the procedure was 26 weeks (range 5–87). Seventeen patients had left sided symptoms and thirteen had symptoms on the right (Table 1). C6–C7 was the commonest level to be involved, with 11 patients (36%) showing narrowing of C7 neural foramen. C6 nerve root was affected in 10 patients (33%); C5 in 5 patients; C4 and C8 in two patients each (Table 2). Out of 30 patients, 12 were symptomatic from acute cervical disc disease, while the rest had symptoms due to acute exacerbation of cervical spondylosis.
Table 1.
Demographics of patients included in the study
| Age (years) mean (range) | 44.7 (25–67) |
| Gender (%) | |
| Male | 14 (47) |
| Female | 16 (53) |
| Side of involvement (%) | |
| Right | 13 (43) |
| Left | 17 (57) |
| Duration of symptoms at presentation in weeks (range) | 26.77 (5–87) |
Table 2.
Improvement in outcome scores (VAS and NDI) at 6 weeks and 1 year after the procedure at different levels
| Level | N (%) | VAS–mean (range) | NDI–mean (range) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post (6 weeks) | Improvement | Post (1 year) | Improvement | Pre | Post (6 weeks) | Improvement | Post (1 year) | Improvement | ||
| C4 | 2 (7.7) | 6.5 (5–8) | 2.5 (2–3) | 4 | 2.5 (2–3) | 4 | 60 (44–76) | 20 (18–22) | 40 | 22 (16–28) | 38 |
| C5 | 5 (17.7) | 7.4 (6–9) | 2.6 (1–7) | 4.8 | 1.5 (0–3) | 5.9 | 71.2 (58–84) | 38.4 (26–66) | 32.8 | 31 (24–36) | 40.2 |
| C6 | 10 (33.3) | 7.2 (6–8) | 1.5 (0–3) | 5.7 | 1.8 (0–3) | 5.4 | 68.6 (60–82) | 31.4 (22–46) | 37.2 | 33 (26–46) | 35.6 |
| C7 | 11 (36.7) | 7.8 (6–10) | 2.3 (1–4) | 5.5 | 2.2 (1–4) | 5.6 | 65.3 (48–76) | 28.5 (20–64) | 36.8 | 31.4 (20−48) | 33.9 |
| C8 | 2 (7.7) | 6.5 | 4 (2−6) | 2.5 | 2 | 5 | 61 (54−68) | 35 (24−46) | 26 | 26 | 42 |
Average pre-operative VAS score was 7.4 (range 5–10), which improved to 2.2 (range 0–7) at 6 weeks and 2.0 (range 0–4) at 1 year. All patients reported that they experienced pain relief within 24–48 h following the procedure and that it sustained at 6 weeks. NDI scores also showed similar improvement. The average score prior to intervention was 66.9 (range 44–84), which improved to 31.7 (range 18–66) at 6 weeks and 31.1 (range 16–48) at 1 year. The reduction at 6 weeks in both VAS scores (95% CI 4.5–5.8) and the improvement in NDI (95% CI 30.4–40.0) were highly significant (Table 2). This improvement in symptoms was sustained at 1 year - reduction in VAS scores (95% CI 4.96–5.89) and the improvement in NDI (95% CI 32.04–39.67). Comparing the VAS and NDI scores at 6 weeks to those at 1 year, no significant differences were noted.
Patients with radiculopathy secondary to acute exacerbation of spondylosis showed better improvement in their NDI score at 6 weeks, when compared to those with disc prolapse (P = 0.021). However, the improvement in VAS scores at 6 weeks, NDI and VAS scores at 1 year did not show similar trend (Table 3).
Table 3.
Improvement in outcome scores (VAS and NDI) at 6 weeks and 1 year after the procedure according to the underlying diagnosis
| Improvement in outcome scores | Acute disc prolapse (12/30) | Cervical spondylosis (18/30) | P value | |
|---|---|---|---|---|
| At 6 weeks | VAS mean (SD) | 4.66 (2.18) | 5.4 (1.3) | 0.25 |
| NDI mean (SD) | 28.67 (15.14) | 39.5 (9.24) | 0.02 | |
| At 1 year | VAS mean (SD) | 5.7 (0.95) | 5.2 (1.35) | 0.3 |
| NDI mean (SD) | 32.6 (11.3) | 37.4 (8.3) | 0.2 | |
Neither the side of involvement nor the sex of patient had any effect (two sample t test) on the improvement in outcome scores after the procedure. The study of outcomes at different levels, using one-way ANOVA, suggested that the patients with involvement of C6 or C7 nerve roots responded slightly better at 6 weeks as the mean improvement of VAS was 5.7 for C6 (range 4–7) and 5.5 for C7 (range 4–7). For the other levels the means varied between 3.2 and 4.8 (P = 0.082).
There was a statistically significant trend (Pearson’s r = 0.383, P = 0.037) that older patients showed better improvement in VAS scores at 6 weeks. No significant correlation was shown between duration of symptoms before procedure and improvement in either outcome measure following the procedure.
Mean duration of radiation exposure during the procedure was 27.8 s (range 10–90 s). The median exposure times for the nerve roots under consideration are highlighted in the box plot (Fig. 5).
Fig. 5.
Box plot showing the duration of procedure against different levels
Discussion
It is known that nerve roots and their nutrient vessels are vulnerable to mechanical and chemical injury due to lack of perineurium and a poorly developed epineurium [18]. In animal models of radiculopathy, inflammatory changes and increased levels of PLA2 have been demonstrated within nerve roots and dorsal root ganglion [19]. Studies also identify reduced PLA2 activity in the injured nerves with administration of epidural betamethasone [19], which forms the basis for using anti-inflammatory agents in the treatment of radiculopathy [20]. Additionally, corticosteroids may have a direct anaesthetic effect on small unmyelinated nociceptive C fibres within irritated neural tissue [21].
The role of selective nerve root blocks (SNRB) in treating cervical radiculopathy has been explored by various investigators [9, 10, 22, 23] as has been summarised in Table 4. Delivery of steroids around the nerve root near the site of its compression is achieved through percutaneous injection technique using fluoroscopy or CT guidance. The techniques previously described in the literature used single needles ranging in size from 21G to 25G [6, 7, 9, 10, 23]. Morvan et al. described an antero-lateral approach similar to a cervical discographic approach. Of the 71 injections performed in 51 patients, satisfactory results were obtained in 14% of cases. They performed the injection under radiographic control using a 21G needle but without contrast confirmation [24]. Bush et al. in their series of 68 patients have stated that 81% had complete relief from arm and neck pain. They have used a variety of techniques including a cervical plexus block done without radiographic control with 21G needle, a radiographic controlled foraminal injection with 22G needle and cervical epidural injection [6]. Slipman et al. have used a single 22G needle with contrast confirmation of needle position. In their series of 20 patients at a mean of 21.2 month follow-up, 60% had good to excellent results and a third required surgical intervention [8]. Vallee et al. reported significant reduction in pain in 62% of 32 patients with cervical radiculopathy treated with SNRBs. They injected the steroid with a 21G spinal needle under fluoroscopy control and did not use the contrast to confirm needle tip position [9]. Larkin et al. described a technique in which a catheter is entered into the posterior epidural space via a more caudal route and advanced up the spinal canal and turned into the target foramen essentially performing an “inside-out” injection [25].
Table 4.
Summary of the literature of the techniques for SNRB’s
| Author | Number patients/injections | Position of the patient | Approach | Radiographic modality | Needle size/contrast | Outcome |
|---|---|---|---|---|---|---|
| Morvan (1988) | 51/71 | Sitting | Anterolateral | X-ray | 21 G no contrast |
Satisfactory in 14% |
| Bush (1996) | 68/170 | Not mentioned | Lateral | X-ray in some patients | 21 G / 22 G mixed |
81% complete relief |
| Slipman (2000) | 20/44 | Supine | Lateral | X-ray | 22 G Contrast |
60% good to excellent |
| Vallee (2001) | 32/41 | Sitting | Anterolateral | X-ray | 21 G No contrast |
62% significant relief |
| Cyteval (2004) | 30/30 | Supine | Anterolateral | CT | 22 G Contrast |
60% good to excellent |
| Wagner (2005) | ∼200 | Supine | Anterolateral | CT | 25 G Contrast |
Not mentioned |
Cyteval et al. have described a technique in which the patient is supine on CT table, and a 22G spinal needle was used through anterolateral or lateral approach along with contrast confirmation of needle tip position [7]. Good to excellent results were noted in 60% of 30 patients in their series. In another technical note by Wagner, similar CT guided procedure was described, but using 25G needle and with contrast medium. He stated that more than 200 injections were performed with 100% success in blocking the nerve roots. No serious complications were reported [23].
We have used a ‘two-needle technique’ to achieve the same. The use of a larger diameter (0.9 mm) needle equivalent to 20 gauge allows easier penetration through the skin and soft tissues, until it reaches the nerve root foramen, enabling us to pass the thinner diameter (0.45 mm) needle equivalent to 26 gauge in the desired direction in the peri-radicular space, avoiding the possibility of thinner needle being bent. This reduces the risk of needle breakage when compared to techniques, which use only single thin needle. Moreover, we believe that entering the foramen with smallest possible diameter needle minimises the risk of vascular injury or dural injury leading to leakage of CSF.
SNRB is an effective modality of treatment in a selected group of patients i.e. those with symptomatic radicular arm and neck pain without significant motor weakness in upper limbs. In our series of 30 patients, 28 showed good to excellent clinical response to SNRBs. Patients with acute exacerbation of spondylosis have shown better improvement in early stages, which favours trial of SNRB over surgery in this subset of patients. Two patients who did not respond to injections and underwent surgical interventions for symptom relief had prolapsed cervical discs. In patients with true radiculopathy secondary to prolapsed disc, response to SNRB is less favourable and hence need for further surgical intervention is more likely.
There was no significant difference noted between improvement at 6 weeks and 1 year. This suggests that, if the benefit of injection was not seen at 6 weeks, it is advisable to carry out another trial of injection soon or consider operative intervention depending on patients’ preference, rather than waiting for a delayed improvement. The observed superior improvement in patients with C6 and C7 involvement, compared to other levels could be partly explained by the difficulty in performing injection at more proximal or distal levels. Although the numbers were not large to produce a statistically significant difference, the results suggest that higher levels of involvement are more likely to get a poor response and consequently may be considered for surgical intervention sooner, if there is no adequate response after first injection.
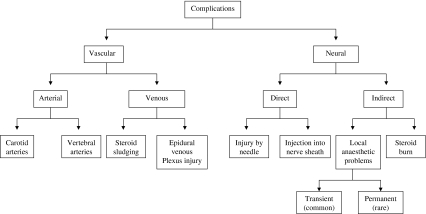
Furman et al. in a prospective study of 504 cervical SNRBs reported that fluoroscopically confirmed intravascular uptake of contrast medium was noted in 19% of procedures. However, none of the patients in their series developed any serious complications of procedure [26]. Serious complications such as arterial [27] and spinal cord [28] injuries have also been reported. SNRB in the cervical spine is believed to have a relatively low risk of complications, but we feel that a complication rate of 1% [29] is difficult to reproduce. Although this procedure is deemed to be safe, there are potential and some times serious complications that can occur with SNRB (Fig. 6); hence meticulous care should be taken while performing it. The importance of using a safer and reproducible technique can not be overemphasised. We encountered no major complications in our series. One patient developed transient nystagmus that lasted for 2 min and resolved spontaneously. Detailed neurological examination in that patient did not reveal any other deficit. Two patients had transient dizziness following the procedure.
Fig. 6.
Flow chart showing possible complications associated with percutaneous needle techniques in the cervical spine. The described ‘two needle technique’ minimises the risk of most of the complications associated with vascular or dural sheath injury
We would like to introduce the concept of ‘safe zone’ for needle placement in SNRB. Immediately lateral to the external opening of the nerve root foramen, the vertebral artery passes closely in front of the zygoapophyseal joint. The spinal nerve, in its dural sleeve, lies in the lower half of the foramen. The upper half is occupied by epiradicular veins. We define the ‘safe zone’ as the space in the postero-superior aspect of root canal, limited on the medial aspect by an imaginary line joining the midpoints of articular processes. Hence, on the AP view, the needle tip should not pass beyond the line connecting sagittal midpoints of articular processes to avoid puncturing dura [30] On the oblique projection, the needle tip should be placed in the postero-superior quadrant of nerve root foramen (Figs. 2a, 4). The placement of needle in this ‘safe zone’ minimises the risk of injury to dura or blood vessels. In combination with other safeguards such as using contrast media, withdrawing the syringe plunger before administering the injectate to make sure that there is no intravascular placement of needle tip and by using smallest possible diameter needle beyond the bony confines of nerve root foramen; our technique demonstrates a safer and reproducible way of performing the procedure.
Conclusions
This study reports the results of cervical SNRBs done in one institution by single surgeon using ‘two needle technique’. The technique used has not been described for cervical root blocks in the past. Majority of patients experienced significant early relief from their symptoms, which was sustained until 2 years after the procedure. Only two of the 30 patients available for follow-up at 2 years required surgery for their condition. We did not encounter any serious complications with our technique. We believe that, using a 20G needle to reach the nerve root foramen and entering the foramen with a 26G needle under fluoroscopic control makes this procedure safe. Observing the recommendations highlighted in our discussion may further improve the safety of the procedure. The patient number is not large to make universal recommendations, however the noted clinical improvement and absence of serious complications in our group prompt us to conclude that in well selected group of patients, SNRB with ‘two needle technique’ gives consistent, reproducible results and is safe to perform.
Acknowledgments
Mr. David Goda, Senior lecturer statistics, University of Wolverhampton for statistical support and help.
References
- 1.Radhakrishnan K, Litchy WJ, O’Fallon WM, Kurland LT. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994;117(Pt 2):325–335. doi: 10.1093/brain/117.2.325. [DOI] [PubMed] [Google Scholar]
- 2.Lestini WF, Wiesel SW (1989) The pathogenesis of cervical spondylosis. Clin Orthop Relat Res 69–93 [PubMed]
- 3.Lees F, Turner JW. Natural history and prognosis of cervical spondylosis. Br Med J. 1963;5373:1607–1610. doi: 10.1136/bmj.2.5373.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saal JS, Saal JA, Yurth EF. Nonoperative management of herniated cervical intervertebral disc with radiculopathy. Spine. 1996;21:1877–1883. doi: 10.1097/00007632-199608150-00008. [DOI] [PubMed] [Google Scholar]
- 5.Dillin W, Booth R, Cuckler J, Balderston R, Simeone F, Rothman R. Cervical radiculopathy. A review. Spine. 1986;11:988–991. doi: 10.1097/00007632-198612000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Bush K, Hillier S. Outcome of cervical radiculopathy treated with periradicular/epidural corticosteroid injections: a prospective study with independent clinical review. Eur Spine J. 1996;5:319–325. doi: 10.1007/BF00304347. [DOI] [PubMed] [Google Scholar]
- 7.Cyteval C, Thomas E, Decoux E, Sarrabere MP, Cottin A, Blotman F, Taourel P. Cervical radiculopathy: open study on percutaneous periradicular foraminal steroid infiltration performed under CT control in 30 patients. AJNR Am J Neuroradiol. 2004;25:441–445. [PMC free article] [PubMed] [Google Scholar]
- 8.Slipman CW, Lipetz JS, Jackson HB, Rogers DP, Vresilovic EJ. Therapeutic selective nerve root block in the nonsurgical treatment of atraumatic cervical spondylotic radicular pain: a retrospective analysis with independent clinical review. Arch Phys Med Rehabil. 2000;81:741–746. doi: 10.1016/s0003-9993(00)90104-7. [DOI] [PubMed] [Google Scholar]
- 9.Vallee JN, Feydy A, Carlier RY, Mutschler C, Mompoint D, Vallee CA. Chronic cervical radiculopathy: lateral-approach periradicular corticosteroid injection. Radiology. 2001;218:886–892. doi: 10.1148/radiology.218.3.r01mr17886. [DOI] [PubMed] [Google Scholar]
- 10.Windsor RE, Storm S, Sugar R, Nagula D. Cervical Transforaminal injection: review of the literature, complications, and a suggested technique. Pain Physician. 2003;6:457–465. [PubMed] [Google Scholar]
- 11.Chiu TT, Hui-Chan CW, Chein G. A randomized clinical trial of TENS and exercise for patients with chronic neck pain. Clin Rehabil. 2005;19:850–860. doi: 10.1191/0269215505cr920oa. [DOI] [PubMed] [Google Scholar]
- 12.Giles Muller LG R. Chronic spinal pain: a randomized clinical trial comparing medication, acupuncture, and spinal manipulation. Spine. 2003;28:1490–1502. doi: 10.1097/00007632-200307150-00003. [DOI] [PubMed] [Google Scholar]
- 13.Lafuente J, Casey AT, Petzold A, Brew S. The Bryan cervical disc prosthesis s an alternative to arthrodesis in the treatment of cervical spondylosis: 46 consecutive cases. J Bone Joint Surg Br. 2005;87:508–512. doi: 10.1302/0301-620X.87B4.15436. [DOI] [PubMed] [Google Scholar]
- 14.Peolsson A, Vavruch L, Oberg B. Predictive factors for arm pain, neck pain, neck specific disability and health after anterior cervical decompression and fusion. Acta Neurochir (Wien) 2006;148:167–173. doi: 10.1007/s00701-005-0660-x. [DOI] [PubMed] [Google Scholar]
- 15.Boehm H, Greiner-Perth R, El-Saghir H, Allam Y. A new minimally invasive posterior approach for the treatment of cervical radiculopathy and myelopathy: surgical technique and preliminary results. Eur Spine J. 2003;12:268–273. doi: 10.1007/s00586-002-0522-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Center for Devices and radiological Health, Food and Drug Administration (2000) Guidance document for the preparation of IDEs for spinal systems
- 17.Vernon H, Mior S. The neck disability index: a study of reliability and validity. J Manipulative Physiol Ther. 1991;14:409–415. [PubMed] [Google Scholar]
- 18.Rydevik B, Brown MD, Lundborg G. Pathoanatomy and pathophysiology of nerve root compression. Spine. 1984;9:7–15. doi: 10.1097/00007632-198401000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Lee HM, Weinstein JN, Meller ST, Hayashi N, Spratt KF, Gebhart GF. The role of steroids and their effects on phospholipase A2. An animal model of radiculopathy. Spine. 1998;23:1191–1196. doi: 10.1097/00007632-199806010-00001. [DOI] [PubMed] [Google Scholar]
- 20.Olmarker K, Byrod G, Cornefjord M, Nordborg C, Rydevik B. Effects of methylprednisolone on nucleus pulposus-induced nerve root injury. Spine. 1994;19:1803–1808. doi: 10.1097/00007632-199408150-00003. [DOI] [PubMed] [Google Scholar]
- 21.Johansson A, Hao J, Sjolund B. Local corticosteroid application blocks transmission in normal nociceptive C-fibres. Acta Anaesthesiol Scand. 1990;34:335–338. doi: 10.1111/j.1399-6576.1990.tb03097.x. [DOI] [PubMed] [Google Scholar]
- 22.Bush K, Chaudhuri R, Hillier S, Penny J. The pathomorphologic changes that accompany the resolution of cervical radiculopathy. A prospective study with repeat magnetic resonance imaging. Spine. 1997;22:183–186. doi: 10.1097/00007632-199701150-00009. [DOI] [PubMed] [Google Scholar]
- 23.Wagner AL. CT fluoroscopic-guided cervical nerve root blocks. AJNR Am J Neuroradiol. 2005;26:43–44. [PMC free article] [PubMed] [Google Scholar]
- 24.Morvan G, Mompoint D, Bard M (1998) Direct intra-foraminal injection of corticosteroids in the treatment of cervico-brachial pain. In: Bard M, Laredo J (eds) Interventional radiology in bone and joint. Springer, Heidelberg, pp 253–257
- 25.Larkin TM, Carragee E, Cohen S. A novel technique for delivery of epidural steroids and diagnosing the level of nerve root pathology. J Spinal Disord Tech. 2003;16:186–192. doi: 10.1097/00024720-200304000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Furman MB, Giovanniello MT, O’Brien EM. Incidence of intravascular penetration in transforaminal cervical epidural steroid injections. Spine. 2003;28:21–25. doi: 10.1097/00007632-200301010-00007. [DOI] [PubMed] [Google Scholar]
- 27.Brouwers PJ, Kottink EJ, Simon MA, Prevo RL. A cervical anterior spinal artery syndrome after diagnostic blockade of the right C6-nerve root. Pain. 2001;91:397–399. doi: 10.1016/S0304-3959(00)00437-1. [DOI] [PubMed] [Google Scholar]
- 28.Ludwig MA, Burns SP. Spinal cord infarction following cervical transforaminal epidural injection: a case report. Spine. 2005;30:E266–E268. doi: 10.1097/01.brs.0000162401.47054.00. [DOI] [PubMed] [Google Scholar]
- 29.Ma DJ, Gilula LA, Riew KD. Complications of fluoroscopically guided extraforaminal cervical nerve blocks. An analysis of 1036 injections. J Bone Joint Surg Am. 2005;87:1025–1030. doi: 10.2106/JBJS.D.02139. [DOI] [PubMed] [Google Scholar]
- 30.Rathmell JP, Aprill C, Bogduk N. Cervical transforaminal injection of steroids. Anesthesiology. 2004;100:1595–1600. doi: 10.1097/00000542-200406000-00035. [DOI] [PubMed] [Google Scholar]