Abstract
Background
Hodgkin's disease (HD) most commonly presents with progressive painless enlargement of peripheral lymph nodes, especially around the cervical region. A few children have systemic symptoms and weight loss. At the time of diagnosis, osseous involvement is uncommon
Case presentation
A case is described of Primary Multifocal Osseous Hodgkin's Lymphoma in a seven-year-old boy. He presented with a painful swelling in the sternum, and further investigations revealed deposits in his L1 vertebra, the left sacro-iliac joint and the right acetabulum.
Conclusion
The clinical, radiological and histological features of this disease can mimic other medical conditions, including Tuberculosis, making the diagnosis difficult and often leading to delays in treatment. This is a very rare condition and we believe this to be the youngest reported case in the literature.
Background
Hodgkin's disease (HD) most commonly presents with progressive painless enlargement of peripheral lymph nodes, especially around the cervical region. A few children have systemic symptoms and weight loss. At the time of diagnosis, osseous involvement is uncommon and even in the late stages only 9–35% of cases have any bony involvement [1]. It is therefore extremely rare for patients to present with primary Hodgkin's disease of the bone. If there is no associated extra-osseous involvement, the condition is referred to as primary osseous Hodgkin's lymphoma (POHL). It is termed primary multifocal osseous Hodgkin's lymphoma, if more than one osseous site is involved. The clinical, radiological and histological features of POHL can mimic other medical conditions, thereby making the diagnosis difficult, often leading to delays in treatment
We present a case of a seven-year-old boy diagnosed with primary multifocal osseous Hodgkin's lymphoma. We believe this to be the youngest such reported case and only the third ever reported paediatric case of primary multifocal osseous Hodgkin's lymphoma in the English literature.
Case presentation
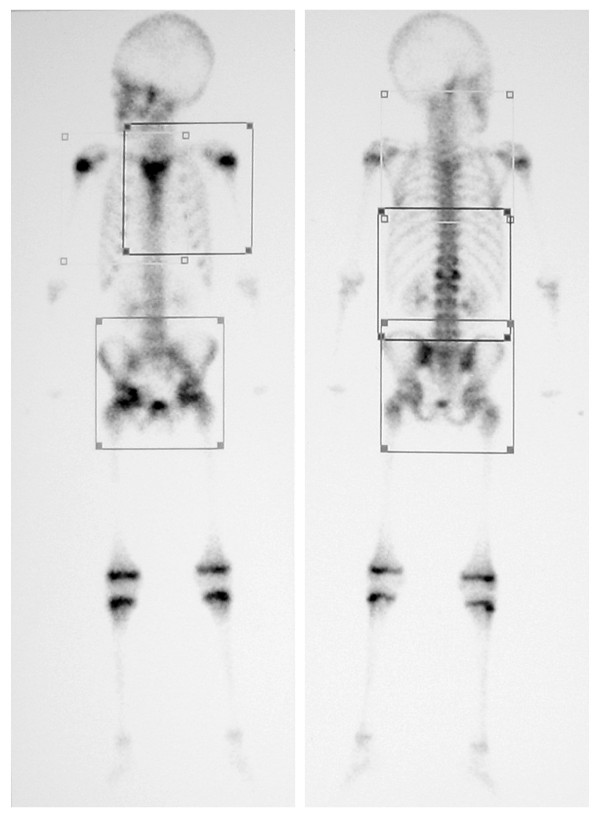
A seven year old male presented with a painless, firm 3 cm mass overlying his sternum. He was clinically well, apyrexial with no history of weight loss. Initial investigations revealed an elevated CRP (27.5), ESR (90), white cell count (22.3) with a neutrophilia (17.0) and a hypochromic microcytic anaemia (Hb: 9.3). Technecium99 bone scan (Figure 1) revealed increased uptake in the sternum, L1 vertebra, the left sacro-iliac joint and the right acetabulum.
Figure 1.
Bone scan at time of presentation. Demonstrating increased uptake in the sternum, L1 vertebra, left sacro-iliac joint and right acetabulum.
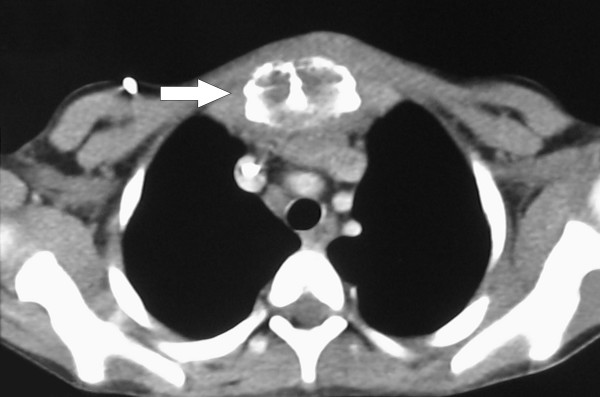
A CT scan of the chest (Figure 2) and sternum confirmed the presence of a sternal mass with no underlying soft tissue involvement. A fine needle biopsy of the sternal mass showed an inflammatory infiltrate. Bone marrow aspirates and trephine from the sternum showed a reactive marrow with no evidence of malignancy. Both ultrasound of the abdomen and echocardiogram were normal. On the basis of these results a provisional diagnosis of multi-focal osteomyelitis was made and the patient was started on antibiotic treatment (Benzylpenicillin, Flucloxacillin and Fusidic Acid). Despite this treatment his white cell count and inflammatory markers continued to rise.
Figure 2.
Axial CT of chest. Demonstrating the sternal mass (arrow) but no underlying soft tissue involvement.
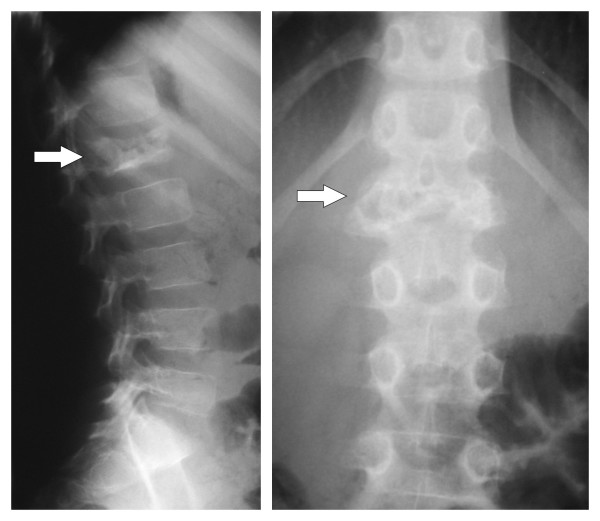
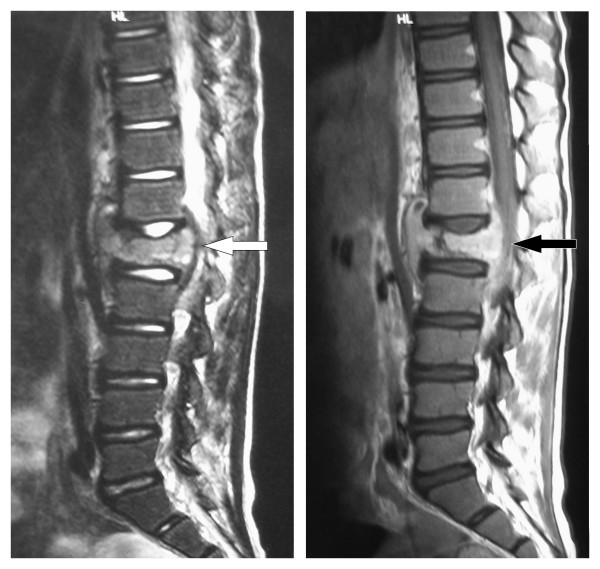
Five weeks after discharge he represented because of an enlarging sternal mass and the development of back pain with no associated neurology (Figure 3). He remained well with no weight loss or signs and symptoms of systemic disease. An open biopsy of the chest wall mass and a CT guided biopsy of the L1 spinal lesion were performed. These revealed macroscopically caseous material. Mantoux and Heaf tests were negative. An MRI scan of the lumbar spine (Figure 4) showed loss of height of L1 with disease extending bilaterally to the pedicles of T12 and L2. There was a soft tissue mass anterior and posterior to L1 causing spinal stenosis and impingement on the conus. Radiologically this was thought to resemble Potts disease and the macroscopic appearance of the lumbar specimen suggested a diagnosis of tuberculosis. Triple therapy was commenced (Rifampicin, Isoniazid and Pyrazinamide). The specimens were negative for acid fast bacilli, Ziehl-Neelson stain for TB was negative and no organisms were cultured. Subsequent histology from the sternal mass showed Hodgkin's lymphoma (Figure 5). Cells within the specimen were positive for CD30 and CD20 (Figure 6).
Figure 3.
Plain radiographs (AP and Lateral) of lumbar spine. Demonstrate destruction of the L1 vertebra (arrow).
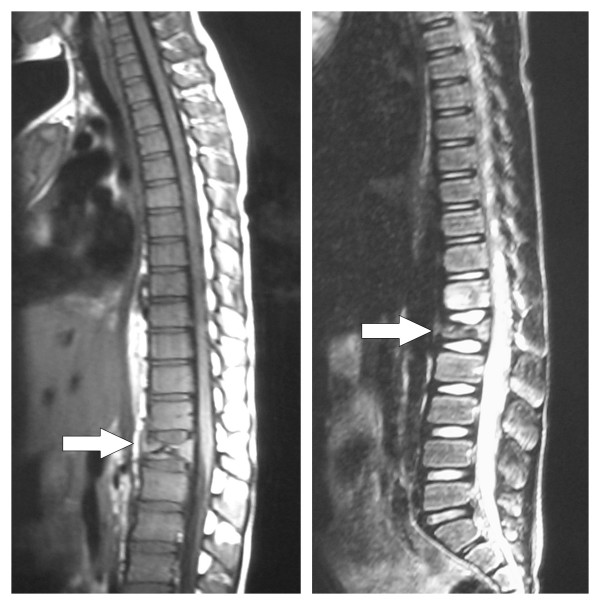
Figure 4.
MRI (T1 and T2 weighted images) of lumbar spine. Investigation undertaken 6 weeks after presentation showing loss of height of L1 with surrounding soft tissue mass and impingement on the conus.
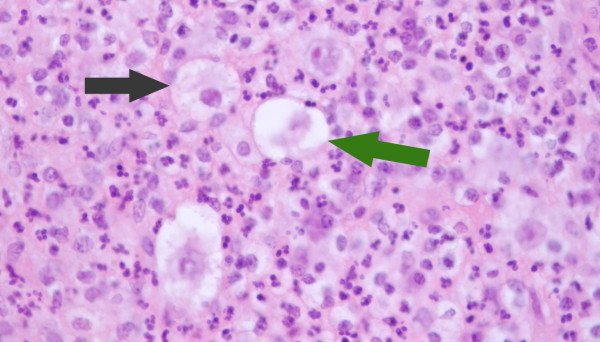
Figure 5.
Histology from sternal aspirate. Illustrates mixed inflammatory cells, lacunar cells (green arrow) and Hodgkin cells (black arrow).
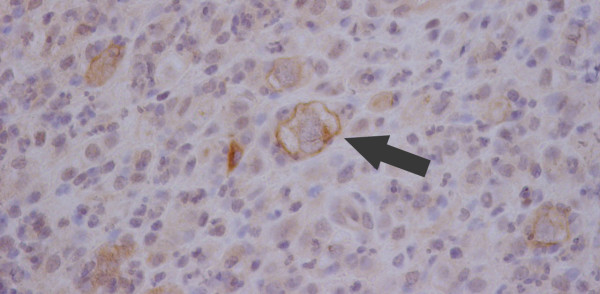
Figure 6.
Histology from sternal aspirate with stain for CD30. The large cells (arrow) are positive for CD30 found on the surface of Reed-Sternburg cells in Hodgkins Lymphoma.
Treatment with chemotherapy was started following the current UKCCSG (United Kingdom Childrens Cancer Survey Guidelines) for Hodgkin's disease, and antituberculous treatment was stopped. Staging showed no lymphadenopathy in the chest or abdomen. Two weeks after commencement of chemotherapy a dramatic decrease in soft tissue involvement around the spinal cord was seen on a repeat MRI. (Figure 7). The time from presentation to diagnosis was two months.
Figure 7.
MRI Thoraco-lumbar spine. Performed after commencement of chemotherapy regime. This illustrates the decrease in size of L1 lesion and reduction in impingement on the conus.
Discussion
The incidence of skeletal Hodgkin's disease varies from 9–14% during the course of the disease with up to 30–50% at post mortem [1]. Skeletal involvement may present in four different ways: POHL (either solitary or multifocal); simultaneously in osseous and non-osseous sites; or recurrence of disease at osseous sites. We consider that in order to make a diagnosis of POHL there should not be any signs or symptoms of systemic disease at the time of presentation or at the time of staging. Historically it was felt that primary Hodgkin's of the bone did not occur and that bony involvement was a feature of haematological dissemination of the disease, thereby implying a less favourable prognosis [2]. Granger et al., [3] reported a 5 year survival of just 4.2% with 80% of deaths occurring within first 3 years. POHL must therefore be distinguished from systemic HD with diffuse bone marrow involvement (Ann Arbor IV, see table 1), as it appears that POHL may have a better prognosis than systemic Hodgkin's with bony involvement [4]. The most recent case reported in the literature regards a 51 year old female who presented with left hip pain and was subsequently lymphadenopathy in the cervical and inguninal nodes. She was staged as VIB. The question remains as to whether POHL has a better prognosis than HD with bony involvement [5].
Table 1.
Staging of Lymphoma: Ann Arbor classification
| Stage I Disease in a single lymph node region |
| Stage II Disease in two or more regions on the same side of the diaphragm |
| Stage III Disease in lymph node regions on both sides of the diaphragm |
| Stage IV Diffuse or disseminated involvement of one or more extralymphatic organs or tissues with or without associated lymph node enlargement. |
There are thirty three clearly reported cases of primary osseous lymphoma at either single or multiple sites, in all ages, in the scientific literature since 1927. Table 2 details these 32 cases as well as this current case. It does not include patients who presented with disease at non osseous and osseous sites, or those patients in whom hodgkins disease disseminated to the bone. At least 7 of these cases were reported prior to 1954 when CT, MRI and PET scanning was not available, so it cannot be stated for certain, whether these cases had any evidence of lymphadenopathy within the chest or abdomen. We are uncertain therefore, whether these are true cases of POHL.
Table 2.
A table of cases in the literature who presented with Hodgkin's lymphoma disease at single or multiple bony sites.
| Year | Author and [reference] | Age (years) | Gender (M/F) | Site(s) | Therapy | Outcome |
| 1927 | Gerbert et al. [10] | 42 | M | T4-T8 | XRT | Alive at 10mo LTFU |
| 1936 | Gerbert et al. [10] | 39 | F | L humerus | Surgery | DOD 12mo |
| 1943 | Gerbert et al. [10] | 5 | F | L scapula | XRT | NED |
| 1958 | Gerbert et al. [10] | 53 | M | L Humerus, L Ilium | XRT | DOD at 4mo |
| 1960 | Ostrowski et al. [6] | 73 | F | R Femur | XRT | DOD at 4 yrs |
| 1968 | Ostrowski et al. [6] | 34 | M | L Humerus | XRT | AWD at 10 yrs |
| 1979 | Gerbert et al. [10] | 25 | F | L humerus | XRT | NED 4.5 yrs |
| 1982 | Chan et al. [1] | 12 | M | R tibia | XRT & CT | Alive at 66mo |
| 1982 | Chan et al. [1] | 18 | M | R ulna, L tibia and fibula | XRT & CT | Alive at 18mo |
| 1982 | Chan et al. [1] | 20 | M | T11 | XRT & CT | Alive at 15mo |
| 1982 | Chan et al. [1] | 11 | F | T8-10, L femur, Pelvis | XRT & CT | Alive at 7mo |
| 1982 | Chan et al. [1] | 68 | F | R SI joint | None | Died 2mo |
| 1982 | Chan et al. [1] | 29 | M | T10-T12 | Surgery | ? |
| 1982 | Chan et al. [1] | 45 | M | Sternum | Surgery, XRT & CT | Alive at 10mo |
| 1982 | Chan et al. [1] | 21 | F | Sternum | Surgery & XRT | Alive at 24mo |
| 1982 | Chan et al. [1] | 41 | M | Skull, ischium, L spine | XRT | Died 3mo |
| 1982 | Chan et al. [1] | 17 | F | T7 – T8 | XRT | Died 24mo |
| 1982 | Chan et al. [1] | 9 | M | R tibia | Surgery & XRT | Died 26mo |
| 1982 | Chan et al. [1] | 27 | F | R tibia | XRT | Died 3mo |
| 1982 | Chan et al. [1] | 62 | M | L humerus | Surgery | Died 1 mo |
| 1982 | Chan et al. [1] | 40 | M | T2 | Surgery | Died 8mo |
| 1982 | Chan et al. [1] | 24 | F | L femur | Surgery & XRT | Died 12mo |
| 1989 | Mac Cormick et al. [11] | 61 | M | T spine, R 12th rib, R clavicle | CT | remission |
| 1991 | Gross et al [7] | 17 | F | T10, L4, 11th rib, L ilium | CT, XRT, BMT | DOD |
| 1991 | Gross et al [7] | 12 | F | T11-12, L3-4, L scapula, L10th rib, L ilium, L acetabulum, L femur | CT | AWD at 2.5 yrs |
| 1993 | Borg et al [12] | 31 | M | Sacrum | CT & XRT | NED 5 yrs |
| 1995 | Ostrowski et al. [6] | 61 | F | T11 | resection & XRT | AWD at 22 mo |
| 1995 | Fried et al. [13] | 21 | F | L clavicle | CT | NED 36mo |
| 1995 | Gerbert et al. [10] | 63 | M | L femur, R ilium | CT & XRT | NED 6mo |
| 1996 | Citow et al [8] | 54 | F | T4, T5 | Surgery, CT & XRT | AWD at 36 mo |
| 1999 | Gerbert et al. [10] | 21 | M | R femur, R tibia | CT & XRT | NED 48mo |
| 2006 | Chandra et al [5] | 51 | F | L ileum | CT & XRT | Alive |
| 2006 | Present case | 7 | M | L1, sternum, Lt SI joint, Rt acetabulum | CT | AWD |
CT – chemotherapy
AWD – alive with disease
XRT – Radiotherapy
DOD – died of disease
LTFU – lost to follow up
NED – no evidence of disease
The two cases presented by Ostrowski et al., [6] were among 25 patients diagnosed with osseous Hodgkin's disease from a group of over 500 patients known to have had Hodgkin's lymphoma, at the Mayo clinic between 1927 and 1996. Five of the twenty five had POHL; three had disease at a single bony site and two had multifocal bony disease.
Gross et al., [7] presented two cases in adolescents (12 years and 17 years) who presented in a very similar pattern to ours. Both presented with back pain and raised inflammatory markers. Investigation revealed widespread osseous involvement. In the case of the 17 year old, treatment was delayed by a misdiagnosis of eosinophilic granuloma. The 12 year old is one of two other paediatric cases of primary multifocal osseous Hodgkin's lymphoma that we have identified. The other case was an 11 year old girl with disease in the thoracic spine, pelvis and left femur [1].
There have been two paediatric cases identified by our literature review of patients with POHL at a single site. A case report by Citow JS et al., [8] of a 54 year old female, with back pain and spinal cord compression, thought to be secondary to tuberculosis. Only when antituberculous treatment failed, did re-examination and investigations reveal POHL as the cause.
Radiologically, bony lesions of Hodgkin's disease may be lytic, sclerotic or mixed. One study showed that 75% were lytic, 13.6% mixed and 11.4% mixed [3]. When they involve the vertebral column, the disease can spread from one vertebral body to another across the intra-vertebral disc space and cause destruction of the disc [9].
In all reported cases, the correct diagnosis was only reached after extensive and repeated investigations and review of the histology. The average time to diagnosis from initial presentation was 6–8 months. The most frequent misdiagnosis was osteomyelitis. Our case highlights the difficulties in diagnosing this rare form of Hodgkin's disease.
TB in England has increased by 25 per cent over the last 10 years. Most TB in England occurs among people in inner cities – two in every five cases are in London (see table 3).
Table 3.
TB in England has increased by 25 per cent over the last 10 years. Most TB in England occurs among people in inner cities – two in every five cases are in London. Tuberculosis in the UK (2004 statistics) from global health facts.
| New cases | 7101 |
| New case rate (per 100,000) | 12 |
| People with TB | 5497 |
| TB prevalence (per 100, 000) | 9 |
| TB deaths | 710 |
| Death rate (per 100, 000) | 1 |
Conclusion
This case indicates that Primary Multifocal OHL may present in childhood. It demonstrates the difficulties in reaching a definitive diagnosis, and the need to continually evaluate patients and diagnoses, especially when patients fail to respond to initial therapies.
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
CL, SG, JU and JK all contributed to the literature review. CL,SG and NC have written and revised the manuscripts. All authors read and approved final manuscript for publication.
Acknowledgments
Acknowledgements
Written consent was obtained from the patient for publication of this case report.
Contributor Information
Clare R Langley, Email: clarelangley@hotmail.com.
Simon JW Garrett, Email: garrettsimon@hotmail.com.
Jill Urand, Email: jill.urand@btinternet.com.
Janice Kohler, Email: Janice.Kohler@suht.swest.nhs.uk.
Nick MP Clarke, Email: ortho@soton.ac.uk.
References
- Chan KW, Rosen G, Miller DR, Tan CT. Hodgkin's disease in adolescents presenting as a primary bone lesion. Am J Ped Hematol Oncol. 1982;4:7–11. [PubMed] [Google Scholar]
- Horan FT. Bone involvement in Hodgkin's disease. Br J Surg. 1969;56:277–281. doi: 10.1002/bjs.1800560410. [DOI] [PubMed] [Google Scholar]
- Granger W, Whitaker P. Hodgkin's disease in both with special reference to periosteal reaction. Br J Radiol. 1967;40:939–948. doi: 10.1259/0007-1285-40-480-939. [DOI] [PubMed] [Google Scholar]
- Stuhlbarg J, Ellis FW. Hodgkin's disease of the bone: favourable prognostic significance? Am J Roentgenol Radium Ther Nucl Med. 1965;93:568–572. [PubMed] [Google Scholar]
- Chandra D, Ewton A, Baker K. Hodgkin's disease presenting with osseous involvement. Am J Hematol. 2006;81:550–551. doi: 10.1002/ajh.20650. [DOI] [PubMed] [Google Scholar]
- Ostrowski ML, Inwards CY, Strickler JG, Witzig TE, Wenger DE, Unni KK. Osseous Hodgkin's disease. Cancer. 1999;85:1166–1178. doi: 10.1002/(SICI)1097-0142(19990301)85:5<1166::AID-CNCR22>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- Gross SB, Robertson WW, Jr, Lange BJ, Bunin NJ, Drummond DS. Primary Hodgkin's disease of bone. A report of two cases in adolescents and review of the literature. Clin Orthopaed Rel Res. 1992;283:276–280. [PubMed] [Google Scholar]
- Citow JS, Rini B, Wollmann R, Macdonald R. Isolated, primary extranodal Hodgkin's disease of the spine: Case report. Neurosurgery. 2001;49:453–456. doi: 10.1097/00006123-200108000-00037. [DOI] [PubMed] [Google Scholar]
- McElwain TJ, Selby P. Hodgkin's disease. 1. Oxford: Blackwell S.C. Publications; 1987. pp. 105–106. 141–146. [Google Scholar]
- Gebert C, Hardes J, Ahrens H, Buerger H, Winkelmann W, Gosheger G. Primary multifocal osseous Hodgkin disease: a case report and review of the literature. J cancer Res Clin Oncol. 2005;131:163–168. doi: 10.1007/s00432-004-0641-0. [DOI] [PubMed] [Google Scholar]
- MacCormick R, Covert A, Gross M. Primary bone involvement in Hodgkin's disease. CMAJ. 1989;140:1059–1060. [PMC free article] [PubMed] [Google Scholar]
- Borg MF, Chowdhury AD, Bhoopal S, Benjamin CS. Bone involvement in Hodgkin's disease. Australasian Radiology. 1993;37:63–66. doi: 10.1111/j.1440-1673.1993.tb00011.x. [DOI] [PubMed] [Google Scholar]
- Fried G, Ben Arieh Y, Haim N, Dale J, Stein M. Primary Hodgkin's disease of the bone. Med Paediatr Oncol. 1995;24:204–207. doi: 10.1002/mpo.2950240312. [DOI] [PubMed] [Google Scholar]