Abstract
It is important for surgeons to understand patients’ expectations for surgery. We asked whether patient factors and preoperative functional outcome scores reflect the degree of expectations patients have for posterior spinal surgery. Second, we asked whether patients’ expectations for surgery predict improvements in functional outcome scores after surgery. We prospectively enrolled 155 consecutive surgical patients with greater than 90% followup. Patients’ expectations were evaluated preoperatively along with SF-36 and Oswestry disability questionnaires. Postoperatively (6 months for decompression; 1 year for fusions), we quantified patient-derived satisfaction regarding whether expectations were met and by patient-derived functional outcome scores. In patients undergoing decompression, gender, SF-36 general health domain, and SF-36 physical component score predicted patients with high expectations for surgery. Patients with high expectations also reported greater postoperative improvements in SF-36 role physical domain scores after surgery. Expectations for surgery were met in 81% of patients. In a subset of patients (21 of 143), expectations were not met. These patients reported lower mean preoperative SF-36 general health, vitality, and mean mental component scores.
Level of Evidence: Level I, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Surgery for degenerative conditions of the lumbar spine is a frequent indication for spinal surgery. The efficacy of spinal surgical procedures and its potential impact on the natural history of the degenerative process is under increasing scrutiny [5, 6]. The rates of spinal surgery for degenerative conditions have increased with time and our general population continues to age [3]. Various factors can influence patient outcome after lumbar spinal surgery that may be important in guiding patient selection for surgery [5, 6, 15].
Physical variables such as preoperative functional status and medical comorbidity have influenced surgical outcome [12, 15]. Psychologic variables reportedly correlate with patient satisfaction after spine surgery [13]. A patient’s preoperative rating of his or her health may be an important predictor of symptom severity, walking capacity, and satisfaction after lumbar decompression [13]. In one study of patients undergoing total joint arthroplasty, patients with high mental distress, such as anxiety and depression, before surgery were more likely to have worse reported physical outcomes than those with minimal or no mental distress [1].
What patients expect from spine surgery also appears to influence outcome [4, 10, 18]. Patients’ satisfaction after lumbar surgery may not always correlate with postoperative physical functioning [22]. Patient gender and type of surgery performed also may influence surgical outcome [19, 20]. The association between patients’ expectation for surgery and how that may relate to postoperative outcomes has not been clearly delineated. Patients with high expectations for surgery may have a greater result from surgery if their expectations reflect their motivation. Alternately, patients with high expectations for surgery may have unrealistic expectations in what surgery can accomplish and experience a poorer result from surgery.
The primary question was whether patient factors and baseline preoperative functional outcome scores reflected the degree of expectations that patients have for surgery. Second, we asked whether patients’ expectations for surgery predict patient-reported improvements in functional outcome after surgery.
Materials and Methods
We prospectively followed 155 consecutive patients undergoing posterior lumbar spinal surgery for degenerative conditions of the lumbar spine between 1998 and 2002. Indications for surgery included back, buttock, and/or lower extremity pain of spondylogenic origin. We included patients undergoing decompression and/or spondylodesis (spinal fusion) regardless whether they had prior lumbar surgery. Patients with spinal stenosis underwent decompression and patients with spondylolisthesis underwent decompression and fusion. We excluded 26 patients because they were not capable of completing the questionnaires (eg, cognitive or language limitations) (n = 17) or declined participation (n = 9). After the exclusions, 143 remaining patients were assessed with questionnaires (SF-36, Oswestry Disability Index) preoperatively and 6 months (decompressions) and 1 year (fusions) after surgery. The mean age of the 143 patients was 52 years (range, 18–84 years; male:female ratio, 1:1) (Fig. 1). We calculated preoperative patient comorbidity using the Charlson Comorbidity Index [2]. Institutional review board approval was obtained for the study.
Fig. 1.
This consort flow chart depicts patient recruitment and followup during the study period.
Baseline patient and surgical demographics of patients in the study included an average age at surgery of 52 years (range, 18–84 years) and a male:female ratio of 1:1. Forty-three percent of surgeries were performed for disc herniation, 9% for isthmic spondylolisthesis, 10% for degenerative spondylolisthesis, 30% for stenosis, 6% for spondylosis, 1% for pseudarthrosis, and 1% for adjacent segment disease. Among the patients in whom decompression was performed (n = 94), single-level decompressions were performed in 70%, two-level decompressions in 21%, and multilevel in 9%. Thirty-four percent involved spinal fusion of which 75% were instrumented (Fig. 1). Among the patients in whom fusions were performed (n = 49), 49% had single-level fusions and 51% had multilevel fusions. Forty-two of 49 patients who had fusions also underwent spinal decompression. Revision cases and workers’ compensation or litigation cases accounted for 11% and 9%, respectively.
The mean Mental Component and Physical Component scores preoperatively were 42.1 ± 1.2 and 22.3 ± 1.1, respectively. These values are approximately one and three standard deviations below age- and gender-matched national norms. The mean preoperative Oswestry score was 48.7 ± 1.7%.
Surgery was performed by one of two spine fellowship-trained surgeons (AY, JF). Our standard approach for a disc herniation was a discectomy with partial medial facetectomy and lateral recess decompression either unilaterally or bilaterally according to patient symptoms. For fusion procedures, a posterior intertransverse process lumbar fusion was performed using autogenous iliac crest bone. Instrumented procedures used a pedicle screw/rod system (USS, Synthes, Inc, (Monument, CO) from 1998–2000 and Xia, Stryker®, (Kalamazoo, MI) from 2000–2002).
Patients were permitted activity ad lib after surgery. No lumbar orthoses were used postoperatively. A 6-week course of active and passive physiotherapy was recommended at the 6-week postoperative followup.
Patients were reviewed clinically and radiographically (fusion procedures) at 6 weeks, 3 months, 6 months, and 1 year (fusion procedures) after surgery. Study personnel not involved in care of the patients and blinded to outcome status sent the patients questionnaires before surgery and again 6 months and 1 year after surgery. In the cover letter, patients were instructed to contact the study coordinator for clarification needed for any of the survey questions. Patients were requested to complete the preoperative questionnaire during the week before surgery. Preoperatively, patients completed a generic health status measure (SF-36) and a disease-specific questionnaire (Oswestry Disability Index). In addition, patients completed an expectations questionnaire asking them to rate their expectations for surgery regarding relief of back and leg pain, their ability to sleep, recreational and daily activities, and return to work (Table 1). Postoperatively, we evaluated patients’ expectations and compared them with patient-derived functional outcome measures at 6 months for decompressions and 1 year for procedures involving spinal fusion. The postoperative expectation questionnaire investigated the patients’ attitudes toward the outcome of surgery as it related to meeting their initial expectations (Table 2). Surgeons were blinded to the patients’ expectations and functional outcome questionnaires until completion of the study.
Table 1.
Preoperative expectations questionnaire
| Parameter | Not at all likely | Slightly likely | Somewhat likely | Very likely | Extremely likely | Not applicable |
|---|---|---|---|---|---|---|
| Relief from back pain | 1 | 2 | 3 | 4 | 5 | 6 |
| Relief from leg pain | 1 | 2 | 3 | 4 | 5 | 6 |
| Relief from numbness, weakness, instability | 1 | 2 | 3 | 4 | 5 | 6 |
| To do more everyday household or yard activities | 1 | 2 | 3 | 4 | 5 | 6 |
| To sleep more comfortably | 1 | 2 | 3 | 4 | 5 | 6 |
| To go back to my usual job and normal activities | 1 | 2 | 3 | 4 | 5 | 6 |
| To exercise and do recreational activities | 1 | 2 | 3 | 4 | 5 | 6 |
Table 2.
Postoperative expectations questionnaire
| Parameter | Definitely yes | Probably yes | Not sure | Probably not | Definitely not | Not applicable |
|---|---|---|---|---|---|---|
| Relief from back pain | 1 | 2 | 3 | 4 | 5 | 6 |
| Relief from leg pain | 1 | 2 | 3 | 4 | 5 | 6 |
| Relief from numbness, weakness, instability | 1 | 2 | 3 | 4 | 5 | 6 |
| To do more everyday household or yard activities | 1 | 2 | 3 | 4 | 5 | 6 |
| To sleep more comfortably | 1 | 2 | 3 | 4 | 5 | 6 |
| To go back to my usual job and normal activities | 1 | 2 | 3 | 4 | 5 | 6 |
| To exercise and do recreational activities | 1 | 2 | 3 | 4 | 5 | 6 |
* Are you satisfied with your surgical result?; Are the results of your treatment what you expected? Yes No.
Patients’ responses to the expectation questionnaires were used to define a priori the patients who had either high or low preoperative expectations for surgery and to determine if surgery met preoperative expectations. We assumed a high preoperative expectation for surgery if the average of applicable items (Table 1) was greater than 3.5 (ie, majority of replies to items in Table 1 indicating either a very likely or extremely likely response). Excluding items in which patients indicated the particular question stem was not applicable (ie, last column, Table 2), we summed and averaged patient-specific raw scores for the items that were applicable to the patient. We assumed a score of 2.5 or less would constitute overall expectations for surgery being met (ie, majority of items that were applicable to the patient would be recorded as either definitely yes or probably yes as depicted in Table 2). We considered 94 four patients to have lower preoperative expectations and 51 to have higher preoperative expectations. The distribution of patients with high versus low preoperative expectations for surgery was similar between the two surgical groups (decompression versus fusion).
We created two prediction models: (1) Patient age, gender, comorbidity, and preoperative functional outcome scores were evaluated to determine if these variables reflected patients who had either high or low expectations for surgery; and (2) Degree of improvement from baseline generic and disease-specific functional outcome scores after surgery was evaluated to determine if they could predict patients who possessed greater expectations for surgery. We performed a post hoc analysis by the operating surgeon to ensure surgery by one of the two surgeons did not influence patients’ outcomes and expectations in our study.
Improvement in patient-derived functional outcome measures after surgery was analyzed by paired analysis comparing patient-specific preoperative with postoperative SF-36 and Oswestry scores. After dichotomizing patients into those with high or low preoperative expectations, logistic regression analysis was performed. Because of the differences in length of followup according to surgery type (decompression versus fusion), subgroup analysis was performed separately for these two procedures. In the first prediction model on preoperative data, factors including patient age, gender, comorbidity, and preoperative functional scores (SF-36 domain scores, SF-36 Mental Component score, SF-36 Physical Component score, Oswestry Disability Index) were evaluated to determine if these variables reflected the likelihood of patients having high preoperative expectations for surgery. The second prediction model focused on postoperative analysis. We calculated the improvements each patient had after surgery for the eight domains of the SF-36, mental and physical components, and Oswestry Disability Index scores. We then determined if improvements to these variables predicted the likelihood of patients having had high expectations for surgery. Analysis was performed with and without inclusion of patients who are known to have poor prognostic factors for outcome (workers’ compensation/litigation, revision surgical cases).
Results
Several patient demographic and preoperative functional outcome variables reflected patients with high preoperative expectations for surgery. In the subgroup analysis of patients with decompressions (n = 94), gender, SF-36 general health domain, and SF-36 Physical Component scores reflected patients who had high preoperative expectations for surgery (Table 3). Specifically, male gender, better preoperative SF-36 general health domain, and poorer preoperative SF-36 Physical Component score reflected patients who possessed high expectations for surgery (Table 3). Remaining SF-36 domain and component scores were not statistically significant. In the subgroup analysis of patients undergoing fusion (n = 49), patient age, gender, and preoperative functional outcome scores did not reflect higher patient expectations. We observed no difference in patient age (p = 0.18), comorbidity (p = 0.5), distribution by revision (p = 0.6), or workers’ compensation/litigation cases (p = 0.4) comparing decompressive versus fusion groups. There were more (p = 0.02) males in the group having decompressions and patients undergoing decompression recorded higher SF-36 physical function (p = 0.04) and general health domain (p = 0.03) scores when compared with patients undergoing fusion preoperatively. In both groups, significant improvements in functional scores were observed after surgery (Table 4).
Table 3.
Patient parameters and baseline functional outcome scores as predictors
| Parameter | Odds ratio | 95% Confidence interval | p Value* |
|---|---|---|---|
| Age | 1.08 | 0.98–1.19 | 0.11 |
| Gender | 0.18 | 0.03–1.00 | 0.05* |
| Comorbidity | 1.01 | 0.97–1.05 | 0.75 |
| SF-36 Physical functioning domain | 1.03 | 0.98–1.09 | 0.20 |
| SF-36 Role physical domain | 1.01 | 0.99–1.04 | 0.34 |
| SF-36 Bodily pain | 1.04 | 0.99–1.10 | 0.12 |
| SF-36 General health | 1.04 | 1.01–1.08 | 0.02* |
| SF-36 Vitality | 1.04 | 1.00–1.09 | 0.06 |
| SF-36 Social functioning | 1.01 | 0.97–1.06 | 0.58 |
| SF-36 Role emotional | 1.01 | 0.97–1.04 | 0.74 |
| SF-36 Mental health | 1.05 | 0.97–1.13 | 0.24 |
| SF-36 Mental Component score | 0.81 | 0.63–1.04 | 0.10 |
| SF-36 Physical Component score | 0.75 | 0.59–0.96 | 0.02* |
| Oswestry Disability Index | 1.00 | 0.96–1.04 | 0.98 |
* p < 0.05.
Table 4.
Results of SF-36 and Oswestry Disability Index scores
| Parameter | Preoperative ± SD | Postoperative ± SD |
|---|---|---|
| SF-36 Physical functioning domain | 30.0 ± 2.1 | 61.6 ± 2.4 |
| SF-36 Role physical domain | 10.8 ± 2.0 | 50.7 ± 3.5 |
| SF-36 Bodily pain domain | 23.8 ± 1.5 | 57.9 ± 2.2 |
| SF-36 General health domain | 58.4 ± 2.3 | 67.9 ± 2.1 |
| SF-36 Vitality domain | 38.3 ± 1.8 | 56.3 ± 1.8 |
| SF-36 Social functioning domain | 40.7 ± 2.3 | 73.3 ± 2.4 |
| SF-36 Role emotional domain | 45.2 ± 3.8 | 69.6 ± 3.4 |
| SF-36 Mental health domain | 61.9 ± 1.9 | 72.8 ± 1.5 |
| SF-36 Mental Component score | 42.1 ± 1.2 | 48.1 ± 1.1 |
| SF-36 Physical Component score | 22.3 ± 1.1 | 38.6 ± 1.2 |
| Oswestry Disability Index (percent disability) | 48.7 ± 1.7 | 23.1 ± 1.9 |
SD = standard deviation.
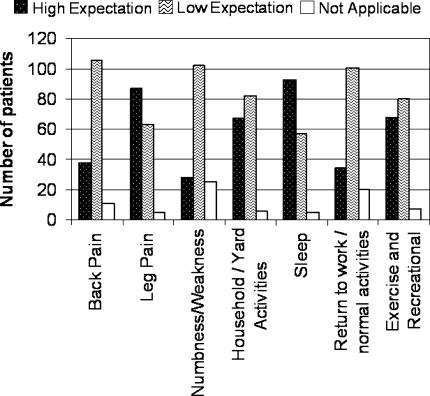
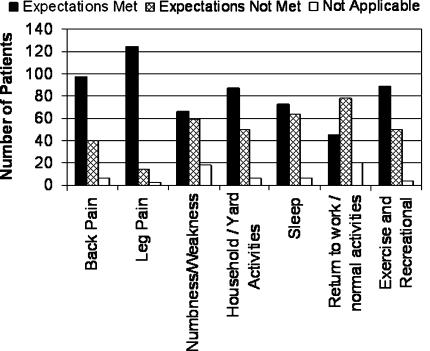
In our second prediction model, higher preoperative expectations predicted greater improvement in some but not all functional outcome measures after surgery. Patients with higher preoperative expectations had greater improvement in mean SF-36 role physical domain scores (OR, 3.7; 95% CI, 1.59–8.58; p = 0.002). In the majority of patients expectations for surgery were met (Figs. 2, 3). Overall patient satisfaction with surgery as quantified in our postoperative questionnaire was 81% (116 of 143). In general, patients had a higher expectation for the relief of leg versus back pain and a higher expectation for improvements in sleep and return to household and recreational activities (Fig. 2). Expectations for return to work-related activities were lower than expectations for relief of leg pain (Fig. 2). In 19% (27 of 143 patients) of patients, surgery did not meet overall expectations. Of these 27 patients, there were two cases of pseudarthroses, one case of pedicle screw misplacement, and three additional cases in which medical comorbidities were believed to be contributing factors.
Fig. 2.
Patients generally had higher expectations for relief of leg versus back pain and for improvements in sleep and return to household and recreational activities. There appeared to be a lower expectation for return to work-related activities.
Fig. 3.
The majority of patients believed their expectations for surgery were met in the seven categories relating to symptoms and physical function.
For the 21 of 27 patients whose expectations for surgery were not met and no other poor prognostic factor could be identified, we observed lower reported preoperative SF-36 general health, vitality domain scores, and mean Mental Component scores (p = 0.02, 0.01, and 0.04, respectively). Patients in whom expectations were not met also reported less (p < 0.05) improvement in SF-36 and Oswestry scores when compared with patients in whom expectations were met. Patients were likely to be less satisfied if they had prior lumbar surgery (p = 0.02) and were involved with workers’ compensation or litigation (p < 0.001). They also were more likely (p = 0.004) to undergo additional spinal surgery.
Discussion
What patients expect from spine surgery is important as it relates to patient satisfaction. Patients’ satisfaction after lumbar surgery may not always correlate with postoperative physical functioning [22]. We therefore asked whether patient factors and baseline preoperative functional outcome scores reflected the degree of expectations that patients have for surgery. We then asked whether patient expectations for surgery predict patient-reported improvements in functional outcome after surgery. By determining if patients’ expectations for surgery are met and whether this translates into satisfaction after surgery is important to our role as clinicians.
We note several limitations. Varying diagnostic degenerative conditions of the lumbar spine were evaluated. We did perform a subgroup analysis in the current study evaluating decompressive and fusion procedures separately. Although the SF-36 includes a mental component to the assessment, a formal psychometric evaluation was not performed on the study cohort. This study evaluated the short-term satisfaction and outcomes of patients undergoing posterior lumbar spinal surgery for degenerative conditions. At the last followup, despite improvement after surgery, the mean SF-36 Physical Component score of our patients was still on average one standard deviation below age- and gender-matched national norms [8]. Longer-term followup may be needed to determine any potential additional improvement after surgery and how this may influence patients’ expectations [12, 14].
We observed several patient demographic and preoperative functional outcome variables reflecting patients who reported higher preoperative expectations for surgery. Male gender, greater perceived SF-36 general health, and lower reported SF-36 Physical Component scores were predictors of patients possessing greater expectations for surgery in the decompressive group. In a study of older patients than those in our study cohort, Shabat et al. evaluated patients older than 65 years undergoing decompression for lumbar spinal stenosis [19]. They observed the satisfaction rate after surgery at a minimum of 1-year followup as determined by telephone interview was worse in women, although both genders reported improvements in activities of daily living and reduction in pain perception. Hakkinen et al. also reported gender differences existed in baseline Oswestry Disability Index scores in patients undergoing surgery for lumbar disc herniation [7]. They observed greater baseline disability in walking, sex life, social life, and traveling items of the Oswestry Disability Index in women. In our study, a lower baseline SF-36 Physical Component score was predictive of greater expectations for surgery. When considering an outcome measure that gauges a patient’s perception of their overall function from a physical perspective, the issue of chronicity of clinical course may be an important variable in addition to the absolute magnitude of that function that a patient reports before surgery. Because current indications for surgery are primarily for pain and function, patients reporting lower function physically may have more to gain by surgical intervention and therefore have greater expectations for their surgical results.
Patients with high expectations also reported greater improvements in SF-36 role physical domain after surgery, but not greater improvements in other SF-36 domains, component scores, and Oswestry Disability Index. Longer patient followup and/or a larger sample size may be necessary to more accurately define parameters in which expectations impact the magnitude of improvements in functional outcomes. We did observe that patients’ expectations for surgery were met in the majority of patients (81%). We also observed that when expectations for surgery were met, greater patient satisfaction and improvements in functional outcome were reported. Spinal surgery for degenerative conditions of the lumbar spine are more likely to be successful in meeting patients’ expectations for relief of radicular leg symptoms when compared with low back pain [13]. Revision lumbar surgery, workers’ compensation, and litigation predicted a poorer functional outcome; however, these cases accounted for a small proportion of our study cohort. Katz et al. studied the prognostic importance of patients’ assessment of their health and comorbidity in outcome after surgery in degenerative lumbar spinal stenosis [15]. They observed that patients who perceived their general health to be poor were less likely to show substantial improvement after surgery when compared with patients who perceived their general health to be good. In our subgroup analysis of patients undergoing decompression, we also observed that patients who reported a higher SF-36 general health domain score also tended to have greater expectations for surgery. Gepstein et al. [4] reported the expectations related to satisfaction and preoperative expectations could aid in predicting postoperative satisfaction in elderly patients with lumbar spinal stenosis. However, in their study, preoperative expectation was assessed by one question regarding either low or high expectations for successful surgical treatment when compared with our study evaluating several parameters of pain, physical, and daily function relating to expectations [4]. A patient’s motivation appears important in that patients with high expectations for surgery may more likely report improved function and satisfaction after surgery [10, 17].
The notion of meeting patients’ expectations for treatment is important in their perception of satisfaction [10, 11, 16]. We observed concordance in that patients who believed their expectations for surgery were not met also reported less improvement as quantified by functional outcome measures. Although surgery type (fusion versus decompression) was not associated with the probability of meeting expectations after surgery in our study, the study by Toyone et al. of 98 patients with decompression suggested patients who were undergoing surgery for stenosis were more likely to have unrealistic expectations when compared with patients undergoing surgery for disc herniation [20]. Overall satisfaction with spinal surgery was 71% to 86% in their series, which is consistent with the results of our study.
An important consideration in patient satisfaction and expectations for surgery is the surgeon-patient discussion regarding the role of surgery for the patient’s condition. Although there is the potential for surgeon bias in educating what patients may expect from surgery, we used a standard discussion between the operating surgeon and the patient regarding the role and expected benefits of surgery. Preoperative information was provided by our two surgeons, including a standardized patient-oriented information package for either decompressive or fusion surgery. The provision of information whereby leg pain is managed more satisfactorily than back pain may prebias patients’ expectations for outcome [13]. What patients retain from preoperative instructions and surgical counseling in informed consent is generally poor [9, 21]. Patients’ expectations for surgery is a multifaceted issue, and patient characteristics and surgical counseling regarding what patients expect from surgery influence outcome. Although we have dichotomized patients into those with high versus low expectations for surgery based on their responses to aspects of physical function and symptoms, what constitutes unrealistic expectations patients may have for surgery and conversely surgical counseling that is appropriate to guide realistic expectations for surgery requires additional study.
Posterior lumbar spinal surgery for degenerative conditions can assist in improving patients’ symptoms and functioning. The expectations for surgery are met in the majority of patients. Patients’ preoperative perception of general health, vitality, and mental health was worse in patients in whom surgery did not meet expectations. In patients undergoing decompressive surgery, gender and some baseline functional measures including the SF-36 physical component score could reflect patients who were more likely to possess a higher degree of expectation for their surgical result. A higher degree of expectation for surgery modestly predicted greater improvement in some but not all functional outcome measures after surgery. Functional outcome measures may be of value in guiding patient selection and education regarding potential surgical outcomes.
Acknowledgments
We appreciate the contributions of Christine Le, Emi Do, Dawn Barbieri, Dr. Mubarak Al-gahtany, and Lynn Antwi-Boasiako to this study, and we thank Dr. Marjan Vidmar for assistance with the statistical analysis.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Ayers DC, Franklin PD, Trief PM, Ploutz-Snyder R, Freund D. Psychological attributes of preoperative total joint replacement patients: implications for optimal physical outcome. J Arthroplasty. 2004;19(7 suppl 2):125–130. [DOI] [PubMed]
- 2.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–1251. [DOI] [PubMed]
- 3.Ciol MA, Deyo RA, Howell E, Kreif S. An assessment of surgery for spinal stenosis: time trends, geographic variations, complications, and reoperations. J Am Geriatr Soc. 1996;44:285–290. [DOI] [PubMed]
- 4.Gepstein R, Arinzon Z, Adunsky A, Folman Y. Decompression surgery for lumbar spinal stenosis in the elderly: preoperative expectations and postoperative satisfaction. Spinal Cord. 2006;44:427–431. [DOI] [PubMed]
- 5.Gibson JN, Grant IC, Waddell G. Surgery for lumbar disc prolapse. Cochrane Database Syst Rev. 2000(3):CD001350. [DOI] [PubMed]
- 6.Gibson JN, Waddell G, Grant IC. Surgery for degenerative lumbar spondylosis. Cochrane Database Syst Rev. 2000(3):CD001352. [DOI] [PubMed]
- 7.Häkkinen A, Kautiainen H, Järvenpää S, Arkela-Kautiainen M, Ylinen J. Changes in the total Oswestry Index and its ten items in females and males pre- and post-surgery for lumbar disc herniation: a 1-year follow-up. Eur Spine J. 2007;16:347–352. [DOI] [PMC free article] [PubMed]
- 8.Hopman WM, Towheed T, Anastassiades T, Tenenhouse A, Poliquin S, Berger C, Joseph L, Brown JP, Murray TM, Adachi JD, Hanley DA, Papadimitroupolos E. Canadian normative data for the SF-36 health survey. Canadian Multicentre Osteoporosis Study Research Group. CMAJ. 2000;163:265–271. [PMC free article] [PubMed]
- 9.Hutson MM, Blaha JD. Patients’ recall of preoperative instruction for informed consent for an operation. J Bone Joint Surg Am. 1991;73:160–162. [PubMed]
- 10.Iversen MD, Daltroy LH, Fossel AH, Katz JN. The prognostic importance of patient pre-operative expectations of surgery for lumbar spinal stenosis. Patient Educ Couns. 1998;34:169–178. [DOI] [PubMed]
- 11.Jackson JL, Kroenke K. The effect of unmet expectations among adults presenting with physical symptoms. Ann Intern Med. 2001;134(9 pt 2):889–897. [DOI] [PubMed]
- 12.Jönsson B, Annertz M, Sjöberg C, Strömqvist B. A prospective, consecutive study of surgically treated lumbar spinal stenosis. Part II: Five-year follow-up by an independent observer. Spine. 1997;22:2938–2944. [DOI] [PubMed]
- 13.Katz JN, Lipson SJ, Brick GW, Grobler LJ, Weinstein JN, Fossel AH, Lew RA, Liang MH. Clinical correlates of patient satisfaction after laminectomy for degenerative lumbar spinal stenosis. Spine. 1995;20:1155–1160. [DOI] [PubMed]
- 14.Katz JN, Lipson SJ, Chang LC, Levine SA, Fossel AH, Liang MH. Seven- to 10-year outcome of decompressive surgery for degenerative lumbar spinal stenosis. Spine. 1996;21:92–98. [DOI] [PubMed]
- 15.Katz JN, Stucki G, Lipson SJ, Fossel AH, Grobler LJ, Weinstein JN. Predictors of surgical outcome in degenerative lumbar spinal stenosis. Spine. 1999;24:2229–2233. [DOI] [PubMed]
- 16.Lin CT, Albertson GA, Schilling LM, Cyran EM, Anderson SN, Ware L, Anderson RJ. Is patients’ perception of time spent with the physician a determinant of ambulatory patient satisfaction? Arch Intern Med. 2001;161:1437–1442. [DOI] [PubMed]
- 17.Mahomed NN, Liang MH, Cook EF, Daltroy LH, Fortin PR, Fossel AH, Katz JN. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol. 2002;29:1273–1279. [PubMed]
- 18.Rönnberg K, Lind B, Zoëga B, Halldin K, Gellerstedt M, Brisby H. Patients’ satisfaction with provided care/information and expectations on clinical outcome after lumbar disc herniation surgery. Spine. 2007;32:256–261. [DOI] [PubMed]
- 19.Shabat S, Folman Y, Arinzon Z, Adunsky A, Catz A, Gepstein R. Gender differences as an influence on patients’ satisfaction rates in spinal surgery of elderly patients. Eur Spine J. 2005;14:1027–1032. [DOI] [PubMed]
- 20.Toyone T, Tanaka T, Kato D, Kaneyama R, Otsuka M. Patients’ expectations and satisfaction in lumbar spine surgery. Spine. 2005;30:2689–2694. [DOI] [PubMed]
- 21.Turner P, Williams C. Informed consent: patients listen and read, but what information do they retain? N Z Med J. 2002;115:U218. [PubMed]
- 22.Yamashita K, Hayashi J, Ohzono K, Hiroshima K. Correlation of patient satisfaction with symptom severity and walking ability after surgical treatment for degenerative lumbar spinal stenosis. Spine. 2003;28:2477–2481. [DOI] [PubMed]