Abstract
The treatment of unstable burst fractures of the atlas (Jefferson fractures) is controversial. Unstable Jefferson fractures have been managed successfully with either immobilization, typically halo traction or halo vest, or surgery. We report a patient with an unstable Jefferson fracture treated nonoperatively with a cervical collar, frequent clinical examinations, and flexion-extension radiographs. Twelve months after treatment, the patient achieved painless union of his fracture. The successful treatment confirms prior studies reporting unstable Jefferson fractures have been treated nonoperatively. The outcome challenges the clinical relevance of treatment algorithms that rely on the “rules of Spence” to guide treatment of unstable Jefferson fractures and illustrates instability may not necessarily be present in patients with considerable lateral mass widening. Additionally, it emphasizes a more reliable way of assessing C1–C2 stability in unstable Jefferson fractures is by measuring the presence and extent of anterior subluxation on lateral flexion and extension views.
Introduction
Burst fractures of the atlas (Jefferson fractures) occur when an axial force is transmitted across the occipital-cervical junction, causing the atlas to be compressed between the angulated articular surface of the axis and the occipital condyles. The impact forces cause an outward spread of the lateral masses of C1. The resulting four-part atlas fracture, with two in the posterior arch and two in the anterior arch, is classically referred to as the Jefferson fracture [20]. Most are relatively stable and not associated with neurologic deficits and can be treated by external immobilization with satisfactory outcomes. Unstable Jefferson fractures reflect a more severe injury of the atlas that occur when the transverse ligament is also ruptured secondary to the extent of spread of the C1 arch. These fractures are more difficult to treat because of the atlantoaxial instability. Many surgeons recommend operative stabilization of these unstable Jefferson fractures.
We present a patient with an unstable Jefferson fracture who was successfully treated nonoperatively with a cervical collar. At 12 months’ followup, he had achieved painless healing of C1 with ankylosis of C1–C2 with resumption of full premorbid activities.
Case Report
A 62-year-old man slipped and struck the back of his neck. He denied loss of consciousness and reported only neck pain. The day after the injury, he noted a change in his voice, transient chest tingling, and the inability to lift his head off his chest.
He delayed medical evaluation until 5 days later when he presented to his chiropractor. The patient’s chiropractor obtained radiographs of the patient’s neck (Fig. 1A) that were interpreted as normal. The chiropractor then performed a manipulation on his cervical spine. Postmanipulation, the patient reported nausea and his wife described his color as “ashen”.
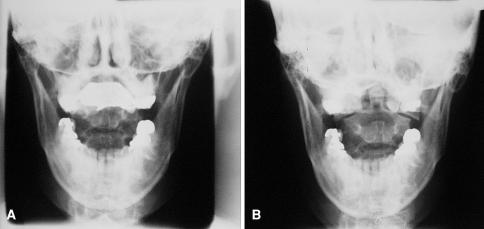
Fig. 1A–B.
(A) An inadequate open-mouth anteroposterior view was taken 5 days after the injury. (B) A repeat open-mouth anteroposterior view taken 6 days after the injury shows 14 mm of bilateral offset of the lateral masses, indicating an unstable Jefferson fracture.
He returned to his chiropractor the next day. Before performing another manipulation, the chiropractor obtained another open-mouth view of the patient’s cervical spine (Fig. 1B). The chiropractor identified the C1 fracture, and the patient ultimately was transferred to our hospital for evaluation.
On examination, he was hesitant to flex and extend his neck. His neck was nontender and he was neurologically intact. Plain films showed a 14-mm overlap of the C1-C2 lateral masses, confirming the diagnosis of an unstable Jefferson fracture (Fig. 1B). Coronal views confirmed separation of the lateral masses (Fig. 2A) and axial views showed a bony avulsion suggesting transverse ligament rupture (Fig. 2B). Because he had been walking without a cervical orthosis before his presentation, active flexion and extension films were attempted. The films showed no motion between C1 and C2 with an atlantodens interval of 3 mm. There was no movement identified between the occiput and the posterior arch of C1.
Fig. 2A–B.
(A) A computed tomographic scan in the coronal plane reveals 12-mm lateral mass separation, confirming the diagnosis of an unstable Jefferson fracture. (B) A computed tomographic scan in the plane of C1 shows the four fractures of the ring, two anterior and two posterior. Avulsion of the transverse ligament is evident on the right.
The radiographs and computed tomographic scans were reviewed with the patient. The unstable nature of his fracture was described and he was offered immobilization in a halo vest or surgical stabilization as treatment options. The patient was opposed to both options. Therefore, he was given a Miami J Cervical Collar™ (Jerome Medical, Moorestown, NJ) and observed with monthly clinical examinations, quarterly computed tomographic scans, and flexion-extension views at 6 months and 1 year postinjury.
At 3 months’ followup, the patient was encouraged to mobilize his neck as tolerated and was gradually weaned from wearing the collar. Examination revealed he was able to flex his neck within three fingerbreadths of his chest with extension to neutral only. He laterally rotated his neck 20° bilaterally. His neck was stiff. Motor testing remained normal. Computed tomographic scans showed evidence of healing of the posterior arch on the left with 11-mm overlap of the C1-C2 lateral masses. Flexion-extension films showed no motion across the occipitocervical junction and no increase in the atlantodens interval.
At his 1-year followup, the patient had discontinued wearing the collar and continued to be pain-free. Examination revealed he had extension to neutral only, 30° lateral neck rotation bilaterally, and flexion to within two fingerbreadths of his chest. A lateral flexion-extension radiograph and computed tomographic scan showed complete healing of C1, ankylosis at C1-C2, and no evidence of C1-C2 subluxation (Figs. 3, 4).
Fig. 3A–B.
Computed tomographic scans in the (A) axial and (B) coronal planes show progression of healing of the C1 Jefferson fracture with partial bony fusion along the left anterior, right anterior, and left posterior rings. There is a mild shift of C1 to the left and mild deformation of the atlas ring. There is evidence of transverse ligament calcification.
Fig. 4A–B.
Lateral (A) flexion and (B) extension views of the cervical spine taken at the 1-year followup reveal a healed posterior arch of the C1 fracture. The atlantodens interval is preserved, confirming stability at C1-C2 on flexion and extension. A minimal degree of flexion-extension is evident by the interval between the skull and the posterior arch of C1.
Discussion
Stability at C1-C2 is maintained primarily by the transverse ligament. With considerable axial loading, separation of the lateral masses can occur, and the transverse ligament can be torn. Based on the clinical and radiographic assessments of Spence et al. [19] in cadavers, transverse ligament rupture occurs with lateral mass separation less than 6.9 mm. Jefferson fractures with torn transverse ligaments are inherently unstable and referred to as unstable Jefferson fractures. Instability at the atlantoaxial joint and subsequent subluxation can occur with unprotected flexion and extension movements. The degree of subluxation is observed on flexion-extension views by a change in the atlantodens interval; an interval greater than 2 to 3 mm in adults is deemed abnormal.
Although there is agreement regarding treatment of stable Jefferson fractures [6, 10, 11, 21], management of unstable Jefferson fractures remains controversial. Successful treatment of unstable Jefferson fractures should preserve rotation at the atlantoaxial joint and maintain alignment to allow healing of the atlas. Unstable Jefferson fractures have been treated successfully with immobilization with halo traction or vest and surgery. Treatment with a cervical collar is not the standard of treatment because it is presumed a collar would not sufficiently limit motion to prevent subluxation or allow healing.
Many authors argue most unstable Jefferson fractures heal satisfactorily with immobilization in halo traction or vest without surgery [5, 6, 9, 12, 13, 21]. Advocates of treatment with a halo vest argue it provides traction to align the splayed lateral masses through ligamentotaxis and reduces any impaction below C1-C2, thereby preventing subluxation and promoting healing. Critics of nonoperative immobilization cite high rates of nonunion and persistent posttraumatic pain as reasons to instead perform surgical stabilization [4, 20]. Several authors recommend initial immobilization for 8 weeks in a halo vest followed by C1-C2 fusion to stabilize the joint once the residual instability is documented through flexion-extension studies [16, 18]. Hein et al. [7] advocate immediate surgical stabilization, warning that repair of the dislocation after long-term immobilization can cause irreversible incongruence of the atlantoaxial joint followed by arthrosis and increasing neck pain. Kesterson et al. [8] recommend primary occipitocervical stabilization of Jefferson fractures; however, others recommend transfacet screw fixation at C1-C2 to maintain motion between the occiput and C1. Ruf et al. [17] preserved C1-C2 rotation, obtained anatomic reconstruction of the atlas, and achieved bony fusion using transoral reduction and osteosynthesis of C1. McGuire and Harkey [15] recommend primary stabilization using the Magerl transfacet screw technique [14].
Our case report underscores many important points regarding the treatment of unstable Jefferson fractures. First, the rules of Spence [19] may not correlate directly to C1-C2 stability. Historic treatment algorithms have relied on the radiographic distinction to establish stability at the atlantoaxial joint and to guide treatment. However, rupture of the transverse ligament does not definitively imply C1-C2 instability exists. As Dickman [1] discussed, the most reliable way of assessing C1-C2 stability in unstable Jefferson fractures is by measuring the extent of anterior subluxation on lateral flexion and extension views. The patient in our case report had considerable lateral mass widening (14 mm) with evidence of an avulsion of the transverse ligament. However, on serial flexion-extension radiographs, he showed only 3 mm of atlantoaxial separation (Figs. 1, 2). In this patient, it is likely the residual stability is provided by intact alar ligaments and/or portions of facet capsules, and scarring of the avulsed transverse ligament. Protective immobilization with a cervical collar produced adequate long-term stability to enable bony fusion of the atlas fracture.
This case report also supports prior studies that emphasized the importance of examining the type of transverse ligament fracture when making the decision to pursue surgical intervention. Dickman et al. [2, 3] classified transverse ligament injuries into two main types, which have two distinctly different treatment outcomes. Type I injuries are intrasubstance ruptures of the transverse ligament that are incapable of healing and because of instability are believed by most to require surgery. Type II injuries are avulsions of the transverse ligament on the C1 lateral mass that can heal if the fracture is immobilized nonoperatively. Although the study was limited to isolated injuries of the transverse ligament, its principles can be applied to treatment of Jefferson fractures with transverse ligament disruption. Our case report suggests avulsion fractures of the transverse ligament can be sufficiently stabilized by a cervical collar to allow union of the atlas fracture and healing of the avulsion (Figs. 3, 4).
Although our single case obviously cannot justify treatment of all unstable Jefferson fractures with a cervical collar, it does show instability may not necessarily be present in patients with considerable lateral mass widening. In our patient, either the cervical collar limited his motion sufficiently in flexion-extension to allow scarring of the ligament or the spread of the lateral masses of C1 did not alter the integrity of the transverse ligament. In patients with unstable Jefferson fractures who are opposed to surgery, we believe it is important to observe clinical instability before recommending surgical stabilization.
Footnotes
Each author certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his institution has approved the reporting of this case report, that all investigations were conducted in conformity with ethical principles of research, and that a waiver of informed consent was obtained.
References
- 1.Dickman CA. Letters. Spine. 2004;29:2196. 15454718 [DOI]
- 2.Dickman CA, Greene KA, Sonntag VK. Injuries involving the transverse atlantal ligament: classification and treatment guidelines based upon experience with 39 injuries. Neurosurgery. 1996;38:44–50. [DOI] [PubMed]
- 3.Dickman CA, Hadley MN, Browner C, Sonntag VK. Neurosurgical management of acute atlas-axis fractures: a review of 25 cases. J Neurosurg. 1989;70:45–49. [DOI] [PubMed]
- 4.Guiot B, Fessler RG. Complex atlantoaxial fractures. J Neurosurg. 1999;91:139–143. [DOI] [PubMed]
- 5.Hadley MN, Dickman CA, Browner CM, Sonntag VK. Acute traumatic atlas fractures: management and long-term outcome. Neurosurgery. 1988;23:31–35. [DOI] [PubMed]
- 6.Han SY, Witten DM, Mussleman JP. Jefferson fractures of the atlas: report of six cases. J Neurosurg. 1976;44:368–371. [DOI] [PubMed]
- 7.Hein C, Richter HP, Rath SA. Atlantoaxial screw fixation for the treatment of isolated and combined unstable Jefferson fractures: experiences with 8 patients. Acta Neurochir (Wein). 2002;144:1187–1192. [DOI] [PubMed]
- 8.Kesterson L, Benzel E, Orrison W, Coleman J. Evaluation and treatment of atlas burst fractures (Jefferson fractures). J Neurosurg. 1991;75:213–220. [DOI] [PubMed]
- 9.Koch RA, Nickel VL. The halo vest: an evaluation of motion and forces across the neck. Spine. 1978;3:103–107. [DOI] [PubMed]
- 10.Landellis CD, Van Peteghem PK. Fractures of the atlas: classification, treatment and morbidity. Spine. 1988;13:450–452. [DOI] [PubMed]
- 11.Lee TT, Green BA, Petrin DR. Treatment of stable burst fracture of the atlas (Jefferson fracture) with rigid cervical collar. Spine. 1998;23:1963–1967. [DOI] [PubMed]
- 12.Levine AM, Edwards CC. Treatment of injuries in the C1-C2 complex. Orthop Clin North Am. 1986;17:31–44. [PubMed]
- 13.Levine AM, Edwards CC. Fractures of the atlas. J Bone Joint Surg Am. 1991;73:680–691. [PubMed]
- 14.Magerl F, Seemann PS. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Weidner PA, ed. Cervical Spine. New York, NY: Springer-Verlag; 1987:322–327.
- 15.McGuire RA Jr, Harkey HL. Primary treatment of unstable Jefferson’s fractures. J Spinal Disord. 1995;8:233–236. [DOI] [PubMed]
- 16.O’Brien JJ, Butterfield WL, Gossling HR. Jefferson fracture with disruption of the transverse ligament: a case report. Clin Orthop Relat Res. 1977;126:135–138. [PubMed]
- 17.Ruf M, Melcher R, Harms J. Transoral reduction and osteosynthesis C1 as a function-preserving option in the treatment of unstable Jefferson fractures. Spine. 2004;29:823–827. [DOI] [PubMed]
- 18.Schlicke LH, Callahan RA. A rational approach to burst fractures of the atlas. Clin Orthop Relat Res. 1981;154:18–21. [PubMed]
- 19.Spence KF Jr, Decker S, Sell KW. Bursting atlantal fracture associated with rupture of the transverse ligament. J Bone Joint Surg Am. 1970;52:543–549. [PubMed]
- 20.Vieweg U, Meyer B, Schramm J. Differential treatment in acute upper cervical spine injuries: a critical review of a single-institution series. Surg Neurol. 2000;54:203–210; discussion 201–211. [DOI] [PubMed]
- 21.Zimmerman E, Grant J, Vise WM, Yashon D, Hunt WE. Treatment of Jefferson fracture with a halo apparatus: report of two cases. J Neurosurg. 1976;44:372–375. [DOI] [PubMed]