Abstract
Hip resurfacing is an attractive concept because it preserves rather than removes the femoral head and neck. Most early designs had high failure rates, but one unique design had a femoral stem. Because that particular device appeared to have better implant survival, this study assessed the clinical outcome and long-term survivorship of a hip resurfacing prosthesis. Four hundred forty-five patients (561 hips) were retrospectively reviewed after a minimum of 20 years’ followup or until death; 23 additional patients were lost to followup. Patients received a metal femoral prosthesis with a small curved stem. Three types of acetabular reconstructions were used: (1) cemented polyurethane; (2) metal-on-metal; and (3) polyethylene secured with cement or used as the liner of a two-piece porous-coated implant. Long-term results were favorable with the metal-on-metal combination only. The mean overall Harris hip score was 92 at 2 years of followup. None of the 121 patients (133 hips) who received metal-on-metal articulation experienced failure. The failure rate with polyurethane was 100%, and the failure rate with cemented polyethylene was 41%. Hip resurfacing with a curved-stem femoral component had a durable clinical outcome when a metal-on-metal articulation was used.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Hip resurfacing offers several functional benefits over THA: the size of the femoral head and neck remains close to normal, the resurfaced hip is stable [1, 2, 14, 40] and capable of an excellent range of motion [2, 3, 14, 30], and the joint retains a greater degree of normal biomechanical function [25, 30, 33, 42, 43]. It also offers several procedural benefits: it is more bone conserving than conventional hip arthroplasty because it does not involve decapitation of the femur, and it results in less blood loss and rehabilitates more easily [25, 42, 43]. The disadvantages of this procedure include the risk of femoral neck fracture (0%–7%) [2, 3, 14, 29, 40] and collapse of the femoral head resulting from osteonecrosis (0%–4%) [8, 26]. Additionally, it is a demanding procedure that requires anterior and posterior dislocation of the joint [2, 14, 40].
The first total hip resurfacing arthroplasty was developed by Charnley [10] using a polytetrafluorethylene-on-polytetrafluorethylene (Teflon® or Fluon®) bearing. The procedure failed because of osteonecrosis of the femoral head. Townley and Walker [39] introduced a device (total articular replacement arthroplasty, or TARA) with a small and short curved femoral stem; none of the other subsequent designs, including that of Charnley, used a femoral stem. In the 1970s, hip resurfacing was popular in several centers in Europe, Japan, England, and the United States. However, initial promising results [15, 16, 17, 44] gave way to unacceptable failure rates (22%–76%) [21, 22, 41], owing primarily to acetabular loosening from polyethylene wear (10%–46%) [4, 28, 36]. Less commonly, femoral neck fracture, osteonecrosis, or loosening of the femoral component occurred [4, 21, 22, 36, 41, 44].
Resurfacing was largely abandoned again until the 1990s when it was resurrected for the same reasons that made it attractive initially: many patients want an active lifestyle that would include participation in sports or recreation [33, 42, 43], they want to keep their bone, and some patients have the perception that revisions, if necessary, are easier than with a conventional stem-supported intramedullary hip prosthesis [2, 5, 6]. Modifications were made to the original design based on the presumed cause of failure, one of which was the requirement for a very thin and flexible polyethylene component when retaining a femoral implant the size of the normal femoral head. However, as noted earlier, none of the original devices that had high failure rates had a femoral stem. The one device that did have a femoral stem appeared to have better midterm outcomes than the nonstemmed devices [31, 38].
Therefore the following questions were raised: what are the functional results from curved-stem total hip resurfacing and what is the survivorship of the prosthesis over long-term followup?
Materials and Methods
Four hundred forty-five patients (561 hips) who underwent total hip resurfacing (TARA) procedures from 1960 to 1987 were retrospectively reviewed. Conventional THAs also were performed and it is estimated that approximately 20% of patients treated received a resurfacing prosthesis. Patients were generally selected for resurfacing procedures if they were younger than 60 years. Patients older than 60 years were offered the resurfacing procedure if they were active and if they had excellent bone quality on their radiographs. None of the patients had a prior implant arthroplasty, although 18 had previous surgery for a dislocated hip or fracture. The underlying diagnosis was osteoarthritis in 334 patients (75%), osteonecrosis in 44 (10%), posttraumatic arthritis in 31 (7%), inflammatory arthritis in 18 (4%), and developmental dysplasia in 18 (4%). The patient population consisted of 218 women and 227 men with a mean body weight of 71 and 82 kg, respectively (range, 50–107 kg). The mean age was 52 years (range, 30–74 years) with 97 patients aged 30 to 40 years, 118 aged 40 to 50 years, 109 aged 50 to 60 years, 100 aged 60 to 70 years, and 21 aged 70 to 74 years.
All patients were followed up until death or a minimum of 20 years; 374 (84%) of the 445 patients had died by the time of final followup. Twenty-three additional patients underwent hip resurfacing but were lost to followup and are not otherwise included in the results. The mean age at the time of death was 80 years (range, 58–99 years) and the mean survival time from surgery until the time of death was 22 years. The remaining 71 patients (16%) had been followed a minimum of 20 years (average, 27 years; range, 20–41 years) (Table 1). Prior Institutional Review Board approval was obtained for this study.
Table 1.
Survivorship among original 445 patients treated with hip resurfacing
| Years since surgery | Number (%) | Mean age at death or follow-up (years; range) |
|---|---|---|
| Patients who had died | 374 (84) | 80 (58–99) |
| Less than 5 years | 19 (5) | |
| 5–9 years | 24 (6) | |
| 10–19 years | 54 (14) | |
| 20–30 years | 166 (45) | |
| Longer than 30 years | 111 (30) | |
| Patients alive at followup | 71 (16) | 75 (53–94) |
| Survival periods | ||
| 20–30 years | 51 (72) | |
| 30–40 years | 18 (25) | |
| 40 years | 2 (3) | |
| Patients lost to followup | 23 | |
Surgery was performed by one of two surgeons (JWP, COT). Each surgical procedure was done through an anterolateral approach without trochanteric osteotomy. The hip was dislocated anteriorly and the femur prepared. The femoral head was downsized when possible, trying not to notch the femoral neck. The zenith of the femoral head was removed at an approximate 140° angle to the femur (measured by a goniometer), and all cystic or structurally damaged at-risk bone was removed. The guide stem then is placed into the femoral canal. Fitting this curved stem into the femur creates slight valgus relative to the medial trabecular system of the femur. Cylinder and chamfer cutters were made to complete the preparation of the femoral head [38]. Prostheses were placed using an interference fit, cemented, or porous-coated technique. The surgeon attempted to place the femoral component in valgus.
The type of prosthesis varied with the time at which the procedure was performed. In the earliest procedures from 1960 to 1962, the acetabular surface used was polyurethane (24 patients). This polymer was prepared by mixing the prepolymer with resin and the catalyst at the time of surgery and shaping it in situ or on the back table to the femoral prosthesis. Polyurethane therefore served as the anchoring cement for the femoral side and as the articular replacement and cement for the acetabulum. Although it is a plastic, it had a fairly rough finish. The length of the femoral stem varied from 127 to 165 mm, with longer stems used more commonly in the earlier cases. Metal-on-metal implants became available in 1962 and were used in 121 patients through the mid 1970s; these were made of cobalt chromium (DePuy Orthopaedics, Inc, Warsaw, IN; Howmedica, Rutherford, NJ; Zimmer, Inc, Warsaw, IN) (Fig. 1). They were implanted without cement on the acetabular side and with or without cement on the femoral side. Polyethylene components (DePuy), which became available in the 1970s (222 patients), had an initial thickness of 4.5 mm. These components were later increased to 6.0 mm and cemented in place using polymethylmethacrylate (Simplex®; Howmedica, NJ). The two-piece metal-polyethylene component (78 patients) was porous-coated with a coxcomb fin for adjunctive fixation (Fig. 2). Fifteen patients received a two-piece cementless acetabular prosthesis in one hip and a cemented polyethylene prosthesis in the other (Fig. 2).
Fig. 1.
A photograph shows the curved-stem metal-on-metal hip resurfacing prosthesis. The acetabular component has a small fin and screw holes for adjunctive fixation.
Fig. 2.
An anteroposterior radiograph shows a pelvis with a cemented polyethylene cup on the left side and a cementless two-piece acetabular prosthesis on the right side. The radiograph was taken 21 years after insertion of the prosthesis on the right and 29 years after insertion of the prosthesis on the left.
Patients were followed prospectively and asked to return at 1 year, 2 years, 5 years, and every 5 years thereafter. The Harris hip score was used (COT, JWP) to evaluate the surgical results [20]. The hip score at 2 years was used to grade the functional result. When this was not possible, patients were sent a written questionnaire (Appendix 1) or contacted by telephone and interviewed using the same questionnaire. Clinical examinations to final followup were available for 226 (51%) patients. Written questionnaires were available for 88 (20%) patients and telephone questionnaires were available for 131 (29%) patients. Patients were queried specifically about the need for additional surgery on their hip. If surgery had been performed, the patient was asked to provide information about that procedure. The date of death was obtained by direct communication with the family. Information regarding the patient’s hip function was obtained from the family for patients who had died. Twenty seven patients (6%) underwent a resurfacing procedure on one side and a conventional THA on the other. They were asked which was the better hip based on their perception of a more natural feel and superior strength or function.
Immediate postoperative radiographs were assessed and the abduction angle of the acetabular component and the stem shaft angle of the femoral prosthesis were measured [2, 7]. The femoral component was considered malpositioned if it was 5° more horizontal (varus) than the medial trabecular system of the proximal femur [12, 35]. The acetabular component was considered malpositioned if the abduction angle was greater than 65° or less than 30°. The observers (JWP, COT) were not blinded to the results.
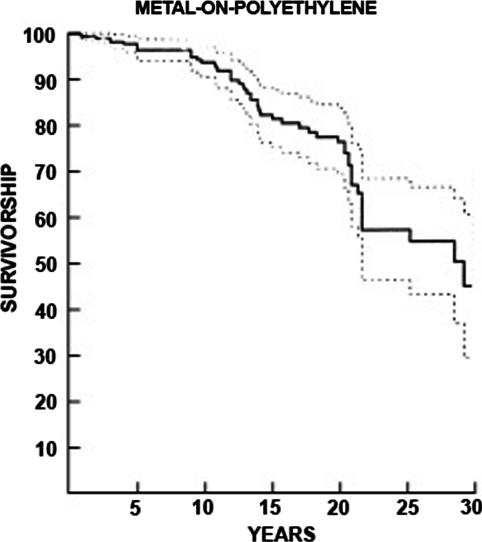
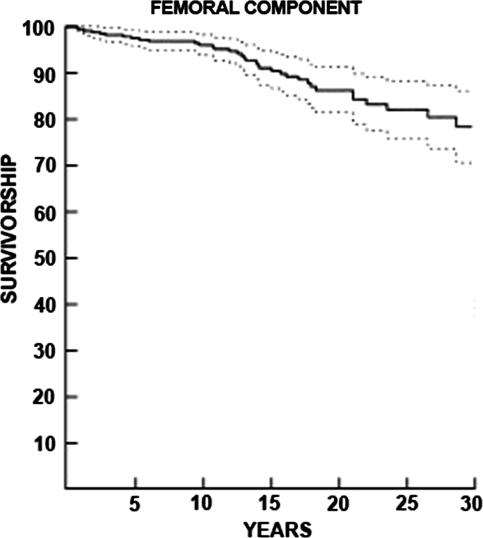
Survivorship was computed using Kaplan-Meier survivorship estimates [24]. and the end points consisted of revision or removal (or recommendation for revision or removal) of either component for any reason. Patients were censored at death or at revision. A 95% confidence interval was calculated. Survivorship analyses were calculated for each type of acetabular reconstruction used (Figs. 3, 4). Failure was defined by removal or revision of the prosthesis or consideration for revision based on reduction in function of the hip with radiographic evidence of loosening of the components, such as change in position of either the femoral or acetabular component or extensive radiolucent lines around the acetabular component and resorption of bone [1].
Fig. 3.
A Kaplan-Meier survivorship curve for the cemented polyethylene acetabular component is shown. The survivorship is 59% at 20 years after prosthesis insertion. Dashed lines indicate 95% confidence intervals.
Fig. 4.
A Kaplan-Meier survivorship curve for the curved-stem femoral component is shown. The survivorship rate is 84% at 20 years. Dashed lines indicate 95% confidence intervals.
Results
The mean peak Harris hip score improved from 57 (range, 8–79) to 92 (range, 63–100) at 2 years. Flexion improved from a mean of 83° (range, 5°–118°) to a mean of 110° (range, 65°–140°) between preoperative and postoperative evaluations. Most patients experienced no pain and only four (less than 1%) experienced severe pain. Of the 445 patients assessed for postsurgical activity, 1/3 participated in strenuous athletics or work and only 22 (5%) did not work or participate in activities. Ninety percent were not limited in their activities (Table 2). Of the 27 patients who had a resurfacing procedure on one side and a conventional THA on the other, all indicated the hip that had resurfacing was the better hip.
Table 2.
Complications of hip resurfacing procedures
| Outcome | Number of patients (%) | Comments |
|---|---|---|
| Complications | ||
| Deep infection | 11 (2) | Over lifetime of prosthesis |
| Dislocation | 5 (< 1) | |
| Periprosthetic fracture (hips) | 6 (< 1) | Intertrochanteric and subtrochanteric |
| Femoral neck fractures | 10 (1.7) | |
| Intraoperative femoral neck fracture | 1 | Converted to THA |
| Femoral nerve palsy | 2 | Both patients recovered |
| Sciatic palsy | 5 (< 1) | Recovery: 2 full; 2 partial; 1 limited as a result of peroneal and tibial involvement |
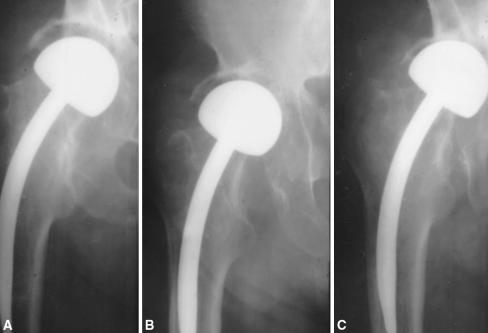
Among living patients and those who died with their implant in place, the survivorship for the femoral prosthesis (including patients with all three acetabular implants) was 84% (Fig. 4). However, the metal-on-metal prostheses had 100% survivorship. Failure rates for the remaining acetabular prostheses ranged from 34% to 100% (Table 3). The highest failure rate (100%) was seen with polyurethane. This bearing surface disappeared radiographically with time (Fig. 5); thereafter, this prosthesis seemed to function as a hemiarthroplasty. Of the two patients with polyurethane prostheses undergoing revision, one had metal-on-metal resurfacing with a good outcome, and the other underwent THA because of a femoral neck fracture. The cemented polyethylene acetabular prosthesis (Fig. 2) also resulted in high failure rates. The 15 patients who received a two-piece cementless acetabular prosthesis in one hip and a cemented polyethylene prosthesis in the other also experienced high failure rates (Table 3). All but two of the 141 revisions were in patients with metal-on-polyethylene articulation and two involved a metal-on-polyurethane prosthesis. None of the metal-on-metal prostheses underwent revision (Table 3). We removed both components and inserted an entirely new resurfacing prosthesis in two patients. The acetabular prosthesis alone was revised in 22 hips. The femoral component was secure in these cases. Revision surgery in the remaining patients (117 hips) was conventional THA. Thirty-two of 44 patients (73%) with osteonecrosis experienced prosthesis failure (mean time to failure, 7 years; range, 3–12 years).
Table 3.
Functional results of hip resurfacing
| Pain | Number (%) | Assessed 2 years after procedure |
|---|---|---|
| No pain | 459 (82) | |
| Slight pain | 86 (15) | |
| Moderate pain | 12 (2) | |
| Severe pain | 4 (< 1) | |
| Function: postsurgical activity | Assessed 2 years after procedure in 445 patients | |
| Highly active | 147 (33) | Strenuous sports or job |
| Active and no limitations necessary | 254 (57) | |
| Moderately active | 22 (5) | |
| Inactive | 22 (5) | |
| Patient satisfaction | ||
| Satisfied with outcome | 427 (96) | |
| Dissatisfied with outcome | 18 (4) | Nine patients were dissatisfied because of a limp or weakness Nine patients were dissatisfied because of pain |
Fig. 5A–C.
Anteroposterior radiographs show a metal-on-polyurethane curved-stem resurfacing prosthesis. (A) There is 9 mm of polyurethane immediately after insertion. (B) Two years later, approximately ½ of the polyurethane has worn away. (C) All the polyurethane has worn away 6 years after prosthesis insertion.
Postoperative radiographs revealed technical errors in approximately 13% of patients, most commonly a malpositioned femoral component (28 hips or 5%), and smaller numbers of malpositioned acetabular components, malpositioned femoral and acetabular components in the same patient, with notched femoral necks, and incompletely seated femoral components in 36 instances (Table 4). Twenty-one of these 64 patients (33%) had a body mass index greater than 35. The most common complications seen at any time during the followup included deep infection, dislocation, and periprosthetic fracture. The periprosthetic fractures occurred sporadically any time after the surgical procedure from 6 months to 36 years later. Less frequently, intraoperative fracture and nerve palsy occurred (Table 5). Medical complications of various types occurred in approximately 5% of patients.
Table 4.
Radiographic findings after hip resurfacing
| Radiographic finding | Number of hips (%) | Comments |
|---|---|---|
| Femoral component malpositioned | 28 (5) | Greater than 5° more varus postoperatively measured versus medial trabecular system |
| Acetabular component malpositioned | 17 (4) | Includes 11 with hip resurfacing failure |
| Acetabular and femoral components malpositioned | 6 (1) | Includes three with hip resurfacing failure |
| Notched femoral neck | 11 (2) | Includes three with a femoral neck fracture |
| Femoral component incompletely seated | 2 (< 1) | Includes one with hip resurfacing failure |
Table 5.
Revisions of hip resurfacing prostheses
| Item | Type of prosthesis | |||
|---|---|---|---|---|
| Metal-on-polyurethane | Metal-on-metal | Metal-on-cemented polyethylene | Metal on two-piece cementless with polyethylene | |
| Revision needed | 2 | 0 | 105 | 34 |
| Patients/hips | 24/26 | 121/133 | 222/282 | 78/120 |
| Mean followup (years; range) | 24 (20–31) | 26 (20–41) | 25 (20–31) | 21 (20–22) |
| Alive at followup | 0 | 0 | 41 | 30 |
| Lost to followup | 0 | 2 | 15 | 6 |
| Prosthesis failure rate | 100% | 0 % | 41% | 34% |
| Reason for failure | ||||
| More than one reason in some patients | Polyurethane wear (26)Femoral neck fracture (1) | N/A | Loosening of acetabulum (76)Polyethylene wear (30)Loosening of femoral prosthesis (5)Femoral neck fracture (6) | Polyethylene wear (27)Component loosening with migration (11)Femoral neck fracture (3) |
N/A = not applicable.
Discussion
The curved-stem hip resurfacing prosthesis was the second attempt (1960) at total hip resurfacing [15]. John Charnley made the first attempt (1951) before his work on low-friction arthroplasty [11]. The innovator (COT) continued to use the curved-stem prosthesis for over 40 years and long-term followup of the patients is available.
There are some limitations of this study. The investigation is retrospective, but the primary outcome, prosthesis, and survival are known on all but a few patients who were lost to followup. Second, this study investigates a prosthesis that was in evolution as it was being used. Three different materials were used for the acetabular resurfacing, although most were metal-on-metal and metal-on-polyethylene a few were metal-on-polyurethane. Also the femoral component was secured without or with cement and varied in stem length adding variations for which statistical analysis could not be done. Pathologic specimens of failed cases or autopsy retrievals also are not available to show the reasons for success or failure. The two surgeons involved performed all of the clinical and radiographic analyses. Complete followup data (particularly radiographs) were not available on many patients so questionnaires were relied on for some of the information. There are no long-term functional outcomes reported in this study and validated instruments were not available at the time of surgery for the earlier patients. Finally, because this is a single patient series, there are no patients or groups available with other stemmed femoral devices for direct comparison.
The data suggest a survivorship of 59% at 20 years when using a polyethylene acetabular component. Mesko et al. [31] reported a 75% survivorship with the curved-stem TARA prosthesis at 10 years, but failure rates of 57% and 76% were reported in two other studies [21, 41]. The THARIES™ total resurfacing prosthesis had a failure rate of 50% at 10 years and 80% at 15 years [4, 28]. The Indiana conservative hip had a failure rate of 66% at 9 years and the Wagner had a failure rate of 60% at 8 years [22, 36].
Metal-on-metal hip resurfacing had a survival rate of 100% in this study and as a generic type is the most commonly used resurfacing today. Success rates of 94% or better are reported with as much as 9 (range, 2–9 years) years of followup [2, 3, 14, 40].
Femoral neck fracture is a rare complication after hip resurfacing, occurring at reported rates of 0% to 7% [2, 3, 29, 37]. The rate of femoral fracture and femoral component failure was low in this series. This was despite the effort made to downsize the femoral head that resulted in femoral neck notching in some cases. Placing the femoral component in valgus reduces the stresses in the superior aspect of the femoral head and neck [23, 27, 45]. Femoral components placed in 5° valgus have a factor of 6.1 reduction in the relative risk of an adverse outcome [7]. Obese patients have a higher incidence of varus positioning and femoral neck fracture.
Most early resurfacing implants involved hemispheric preparation of the femoral head followed by placement of a hemispheric femoral implant; unfortunately, shear often resulted in loosening of these implants. These implants also did not have a femoral stem [4, 16, 22, 36]. The presence of a stem reduces the shear force on the prosthetic femoral head-native femoral neck junction by 34% [13, 19]. A curved femoral stem reduces the shear force on the femoral neck by 17% compared with a straight stem [13, 19]. This may be an additional explanation for the lower rate of femoral neck fracture and femoral component loosening observed in the current study with other implants [4, 22, 28, 36]. The preparation required to implant a curved stem promotes valgus positioning of the femoral component [18, 38]. Although I report what appears to be the first attempt to use a metal-on-metal resurfacing prosthesis, there were other early innovators. Gerard [17] used a metal-on-metal prosthesis but did not fix the acetabular component to the pelvis; Mueller [32] also performed metal-on-metal resurfacing procedures. In this series, a prosthesis originally known as cup-stem arthroplasty was used [39], in which the hemisphere was replaced by a flat-topped cylinder. The technique used to place this implant excised at-risk bone in the femoral head and this may have contributed to the low failure rate. The head design provides compressive resistance stability; and a short, curved stem on the prosthesis adds stability without stress relieving the proximal femur [13, 38]. Current designs use a straight femoral stem [3, 14, 40]. The results in this report and biomechanical considerations suggest a curved femoral stem may be the superior design for a resurfacing prosthesis.
The difficulties with hip resurfacing in this series were primarily on the acetabular side. Well-performed femoral resurfacing rarely fails with time; this was true when an interference press-fit technique was used when neither cement nor porous coating was yet available. Early procedures involved the use of materials that did not provide an appropriate acetabular surface. Charnley [10, 11] used polytetrafluorethylene in the first hip resurfacing procedure and it failed. In this series, polyurethane failed every time. However, polyurethane does not cause an osteolytic reaction; as a result, patients functioned generally well as it wore away. They had some pain and radiographs of the hip looked as though hemiarthroplasty had been performed (Fig. 5). The crude polyurethane used in the early days has now been reformulated. Thus far, the wear characteristics of the new formulation seem favorable [9]. Another contributor to resurfacing arthroplasty failure in this series (and in others) was the use of cemented polyethylene acetabular components that loosened and wore through, often resulting in osteolysis [1, 4, 16, 21, 22, 36]. Metal-backed cemented polyethylene sockets were not used in this series, but others have reported prosthesis failure when they were used in such procedures [34, 41].
Exposing and positioning the acetabular component with the femoral head in the way is technically difficult [2, 3, 37]. Exacting preparation of the femoral head is necessary. Hip resurfacing using the curved femoral stem performed well on the femoral side for more than 20 years. Although polyethylene acetabular components failed regularly, metal acetabular components performed well. Hip resurfacing may be an attractive option for a young patient fearing a potentially difficult future total hip replacement revision.
Acknowledgments
I thank Charles O. Townley, MD, for contributing his cases and knowledge. He died on December 22, 2006.
Footnotes
The author certifies that he has no commercial associations (eg. consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
The author certifies that his institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Amstutz H. Surface replacement arthroplasty. In: Amstutz HC, ed. Hip Arthroplasty. Edinburgh, UK: Churchill Livingstone; 1991:295–332.
- 2.Amstutz HC, Ball ST, Le Duff MJ, Dorey FJ. Resurfacing THA for patients younger than 50 years. Clin Orthop Relat Res. 2007;460:159–164. [DOI] [PubMed]
- 3.Amstutz HC, Beaule PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg Am. 2004;86:28–39. [PubMed]
- 4.Amstutz HC, Dorey F, O’Carroll PF. THARIES resurfacing arthroplasty: evolution and long-term results. Clin Orthop Relat Res. 1986:213:92–114. [PubMed]
- 5.Alberton GM, High WA, Morrey BF. Dislocation after total hip arthroplasty: an analysis of risk factors and treatment options. J Bone Joint Surg Am. 2002:84:1788–1797. [PubMed]
- 6.Ball ST, Le Duff MJ, Amstutz HC. Early results of conversion of failed femoral component in hip resurfacing arthroplasty. J Bone Joint Surg Am. 2007:89:735–741. [DOI] [PubMed]
- 7.Beaule PE, Lee JL, Le Duff MJ, Amstutz HC, Ebramzadeh E. Orientation of the femoral component in surface arthroplasty of the hip. J Bone Joint Surg Am. 2004:86:2015–2021. [DOI] [PubMed]
- 8.Campbell P, Beaule PE, Ebramzadeh E, Le Duff M, DeSmet K, Lu Z, Amstutz HC. The John Charnley Award: a study of implant failure in metal-on-metal surface arthroplasties. Clin Orthop Relat Res. 2006;453:35–46. [DOI] [PubMed]
- 9.Carbone A, Howie DW, McGee M, Field J, Pearcy M, Smith N, Jones E. Aging performance of a compliant bearing acetabular prosthesis in an ovine hip arthroplasty model. J Arthroplasty. 2006;21:899–906. [DOI] [PubMed]
- 10.Charnley J. Arthroplasty of the hip: a new operation. Lancet. 1961;1:1129–1132. [DOI] [PubMed]
- 11.Charnley J. Low Friction Arthroplasty of the Hip: Theory, Practice. New York, NY: Springer; 1979.
- 12.Clark JM, Freeman MA, Witham D. The relationship of neck orientation to the shape of the proximal femur. J Arthroplasty. 1987;2:99–109. [DOI] [PubMed]
- 13.Collier J, Kennedy F, Mayor M, Townley CO. The importance of stem geometry, porous coating and collar angle of femoral hip prosthesis on the strain distribution in the normal femur. Trans Soc Biomater. 1983;9:96.
- 14.Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing arthroplasty of the hip in patients under 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–184. [DOI] [PubMed]
- 15.Freeman MA. Total surface replacement hip arthroplasty. Clin Orthop Relat Res. 1978;134:2–4. [PubMed]
- 16.Freeman MA, Cameron HU, Brown GC. Cemented double cup arthroplasty of the hip: a 5-year experience with the ICLH prosthesis. Clin Orthop Relat Res. 1978;134:45–52. [PubMed]
- 17.Gerard Y. Hip arthroplasty by matching cups. Clin Orthop Relat Res. 1978;134:25–35. [PubMed]
- 18.Grecula MJ, Thomas JA, Kreuzer SW. Impact of implant design on femoral head hemiarthroplasty. Clin Orthop Relat Res. 2004;418:41–47. [DOI] [PubMed]
- 19.Haboush EJ. A new operation for arthroplasty of the hip based on biomechanics, photoeleasticity, fast setting dental acrylic, and other considerations. Bull Hosp Joint Dis. 1953;14:242–276. [PubMed]
- 20.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty: an end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed]
- 21.Head WC. Total articular resurfacing arthroplasty: analysis of failure in 67 hips. J Bone Joint Surg Am. 1984;66:28–34. [PubMed]
- 22.Howie DW, Campbell D, McGee M, Cornish BL. Wagner resurfacing hip arthroplasty: the results of one hundred consecutive arthroplasties after eight to ten years. J Bone Joint Surg Am. 1990;72:708–714. [PubMed]
- 23.Huiskes R, Strens PH, van Heck J, Slooff TJ. Interface stresses in the resurfaced hip: finite element analysis of load transmission in the femoral head. Acta Orthop Scand. 1985;56:474–478. [DOI] [PubMed]
- 24.Kaplan E, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [DOI]
- 25.Lilikakis AK, Arora A, Villar RN. Early rehabilitation comparing hip resurfacing and total hip replacement. Hip Int. 2005;15:189–194. [DOI] [PubMed]
- 26.Little CP, Ruiz AL, Harding IJ, McLardy-Smith P, Gundle R, Murray DW, Athanasou NA. Osteonecrosis in retrieved femoral heads after failed resurfacing arthroplasty of the hip. J Bone Joint Surg Br. 2005;87:320–323. [DOI] [PubMed]
- 27.Long JP, Bartel DL. Surgical variables affect mechanics of a hip resurfacing system. Clin Orthop Relat Res. 2006;453:115–122. [DOI] [PubMed]
- 28.Mai MT, Schmalzried TP, Dorey FJ, Campbell PA, Amstutz HC. The contribution of frictional torque to loosening at the cement bone interface in THARIES hip replacements. J Bone Joint Surg Am. 1996;78:505–511. [DOI] [PubMed]
- 29.Marker DR, Seyler TM, Jinnah RH, Delanois RE, Ulrich SD, Mont MA. Femoral neck fractures after metal-on-metal total hip resurfacing. J Arthroplasty. 2007;22(7 suppl 3):66–71. [DOI] [PubMed]
- 30.Mont MA, Seyler TM, Ragland PS, Starr R, Erhart J, Bhave A. Gait Analysis of patients with resurfacing hip arthroplasty compared with hip osteoarthritis and standard total hip arthroplasty. J Arthroplasty. 2007;22:100–108. [DOI] [PubMed]
- 31.Mesko JW, Goodman FG, Stanescu S. Total articular replacement arthroplasty: a three-to ten-year case-controlled study. Clin Orthop Relat Res. 1994;300:168–177. [PubMed]
- 32.Mueller M. The benefits of metal-on-metal total hip replacement. Clin Orthop Relat Res. 1995;311:54–59. [PubMed]
- 33.Naal FD, Maffiuletti NA, Munzinger U, Hersche O. Sports after hip resurfacing. Am J Sports Med. 2007;35:705–711. [DOI] [PubMed]
- 34.Pritchett JW. Success rates of the TARA hip. Am J Orthop. 1998;27:658. [PubMed]
- 35.Pritchett JW, Perdue KD, Dona GA. The neck shaft-plate shaft angle in slipped capital femoral epiphysis. Orthop Rev. 1989;28:1187–1192. [PubMed]
- 36.Ritter MA, Lutgring JD, Berend ME, Pierson JL. Failure mechanisms of total hip resurfacing. Clin Orthop Relat Res. 2006;453:110–114. [DOI] [PubMed]
- 37.Shimmin AJ, Back D. Femoral neck fractures following Birmingham hip resurfacing: a national review of 50 cases. J Bone Joint Surg Br. 2005;87:463–464. [DOI] [PubMed]
- 38.Townley CO. Hemi and total articular replacement arthroplasty of the hip with a fixed femoral cup. Orthop Clin North Am. 1982;13:869–894. [PubMed]
- 39.Townley CO, Walker S. Intramedullary cup-stem arthroplasty of the hip. J Bone Joint Surg Am. 1961;43:602.
- 40.Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing: a minimum follow-up of five years. J Bone Joint Surg Br. 2005;87:167–170. [DOI] [PubMed]
- 41.Treuting RJ, Waldman D, Hooten J, Schmalzried TP, Barrack RL. Prohibitive failure rate of the total articular replacement arthroplasty at five to ten years. Am J Orthop. 1997;26:114–118. [PubMed]
- 42.Vail TP, Mina CA, Yergler JD, Pietrobon R. Metal-on-metal hip resurfacing compares favorably with THA at 2 years followup. Clin Orthop Relat Res. 2006;453:123–131. [DOI] [PubMed]
- 43.Vendittoli PA, Lavigne M, Roy AG, Lusignan D. A prospective randomized clinical trial comparing metal-on-metal total hip replacement and metal-on-metal total hip resurfacing in patients less than 65 years old. Hip Int. 2006;16:73–81. [DOI] [PubMed]
- 44.Wagner H. Surface replacement arthroplasty of the hip. Clin Orthop Relat Res. 1978;134:102–130. [PubMed]
- 45.Watanabe Y, Shiba N, Matsuo S, Higuchi F, Tagawa Y, Inoue A. Biomechanical study of resurfacing arthroplasty: finite element analysis of the femoral component. J Arthroplasty. 2000;15:505–511. [DOI] [PubMed]