Abstract
Recently developed inflatable nails avoid reaming and interlocking screws in tibial fractures and reflect a new principle for stabilization of long bone fractures. We asked if the bending stiffness, rotational rigidity, or play (looseness of rotation) differed between an inflatable versus large-diameter reamed interlocked nails, and whether the maximal torque to failure of the two bone-implant constructs differed. In a cadaveric model, we compared the biomechanical properties with those of an interlocked nail in eight pairs of fractured tibial bones. Bending stiffness, rotational rigidity, play (looseness in rotation), and torsional strength within 20° rotation were investigated using a biaxial servohydraulic testing system. For all biomechanical variables, we found a large interindividual variance between the pairs attributable to bone quality (osteoporosis) for both fixation methods. The inflatable nail had a higher bending stiffness, with a mean difference of 58 N/mm, and a lower torsional strength, with a mean difference of 13.5 Nm, compared with the locked nail. During torsional testing we noted slippage between the inflatable nail and bone. We observed no differences in play or rotational rigidity. Given the lower torsional strength we recommend caution with weightbearing until there are signs of fracture consolidation.
Introduction
Tibial fractures are the most common of the long bone fractures with an annual incidence of two tibial shaft fractures per 1000 individuals [1]. The choice of treatment depends on fracture location, displacement, comminution, soft tissue condition, and local tradition, but for displaced shaft fractures in the adult, some studies recommend reamed intramedullary nailing as the preferred method [1, 12, 15].
The reamed intramedullary nail provides biomechanical advantages through its central placement, large diameter, and locking screws that secure rotation and length. A small incision for nail entry away from the fracture reduces the risk of infection, and autotransplantation of bone through reaming promotes bone healing [8]. The procedure has a union rate greater than 95% for closed fractures in numerous clinical studies [7]. The technique, however, is not without disadvantages and complications. At many centers, the procedure requires 60 to 100 minutes of surgery [10, 20]. Fluoroscopy use during distal locking with a free-hand technique puts surgeons at risk of exposing their hands in the radiation field [20]. Complications are common, with complication rates as much as 58% [16] and reoperation rates as much as 35% [3, 11].
Inflatable nails are a relatively new device for intramedullary fixation of long bone fractures without reaming or locking screws [6]. The implant allows fast, minimal invasive and stable internal fixation for long bone fractures. The interface between bone and implant differs radically from traditional nails and is expected to have a different effect on fracture stability and biology. Good clinical results have been reported for this device for humeral and tibial fractures [3, 6, 9, 13, 25], with only one case report of a complication directly related to the implant [23]. One humerus cadaveric study compared an inflatable with a conventional intramedullary nail and the investigators observed higher bending stiffness but lower rotational stiffness related to the funnel-shaped intramedullary canal of the humerus [5]. For the proximal femur, the inflatable implant consists of an inflatable nail and an inflatable peg for the femoral neck. When tested mechanically in a cadaver model, the implant had similar results for pull-out and a superior torsional stability, compared with a standard hip lag screw [24].
We asked whether the bending stiffness, rotational rigidity, or play (looseness of rotation) differed between inflatable versus large-diameter reamed interlocked nails, and whether the maximal torque to failure of the two bone-implant constructs differed.
Materials and Methods
In a cadaveric fracture model, we tested the bone-implant construct for the inflatable nail compared with a traditional interlocked nail. Eight pairs of tibia were used, with one type of implant placed randomly at each side, and paired comparisons were made.
The inflatable implant is based on an expandable, stainless-steel tube with four reinforcement bars, a conical distal end, and a one-way valve in the proximal part (Fixion® IM Nail; Disc-O-Tech Medical Technologies Ltd, Herzliya, Israel). The nail is introduced in an unexpanded state into the medullary canal without reaming and without guide wire. By means of a hydraulic pump with a screw piston, saline is delivered into the nail to inflate it until a pressure of 50 to 70 bar is reached (Fig. 1A). This will increase its diameter until the reinforcement bars connect with the walls of the medullary cavity and lock to the bone. The 8.5-mm nail can expand to a maximum of 13.5 mm and the 10-mm nail to 16 mm.
Fig. 1A–B.
(A) The Grosse & Kempf® interlocked nail system and (B) the Fixion® inflatable nail system are shown.
The interlocked tibia nail is made of stainless steel (Grosse & Kempf®; Stryker Osteosynthesis, Kiel, Germany). It is an unslotted nail with holes for two proximal and two distal static interlocking screws of 4.6-mm thread diameter and 3.8-mm core diameter (Fig. 1B). The most commonly used nail diameter in the tibia is 10 to 11 mm. This design of reamed interlocked nails is well documented in long-term clinical [7] and in biomechanical studies [21].
Eight pairs of human tibiae were obtained from fresh cadavers and frozen immediately after excision. The donors (five female, three male) ranged in age from 55 to 92 years (mean, 74.8 years). Patients with a history of bone disease or tibial fractures were excluded. Each pair was fixed by one inflatable and one interlocked nail, respectively, evenly distributed between the left and right sides. Before use, they were thawed at room temperature for approximately 12 hours and kept moist in saline until use. A 1-cm transverse saw cut from the front was placed at the anatomic longitudinal midpoint of the bone, and then bending was applied by manual force in flexion in the sagittal plane until fracture, causing a short oblique fracture line in all cases.
The bone was placed in a clamp in reduced position. When using the locked nails, the bone was opened at the midpoint between the tibial tuberosity and the tibial plateau, and a guide was introduced. Reaming was performed up to 11 mm. This provided at least 4 cm of bone contact on either side of the fracture. A 10-mm locked nail was used in all preparations. The locking screws (two in each end) were placed through both bone cortices with a jig. The inflatable nails were inserted through a similar opening; 8.5-mm nails were used. The unexpanded nail could be fully inserted without reaming in all instances. The pump then was connected to the valve, and the pump handle was rotated until the pressure reached 60 bar. By manual testing, the osteosynthesis appeared stable, which confirmed proper expansion of the nail. Radiographs were taken to confirm the nails were properly placed in the medullary cavity and the interlocking screws were within the holes of the nail (Fig. 2).
Fig. 2A–D.
(A, B) Anteroposterior and (C, D) lateral radiographs show the prepared specimens with the inserted nails (A, C: interlocked nail; B, D: inflatable nail) before mechanical testing.
Bending stiffness was first assessed by mounting the specimens in a mediolateral position in a four-point testing rig with 220 mm between the outer rollers and 35 mm between the inner rollers. The two inner rollers were connected with an axis centered over the fracture to ensure equal loading on both sides of the fracture (Fig. 3). An axial compression force was applied by a biaxial servohydraulic testing machine (859 Minibionix® II; MTS Corp, Indianapolis, IN) at a speed of 0.2 mm per second until 3 mm of deformation was reached and then returned to 0 mm. The stiffness was calculated from the slope of the curve. The deformation was small and within the elastic region, so that we observed no visual structural changes.
Fig. 3.
The setup for four-point testing of bending stiffness is shown.
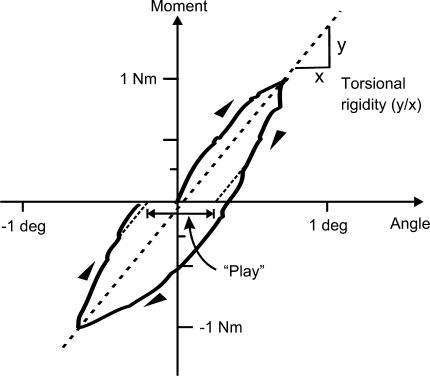
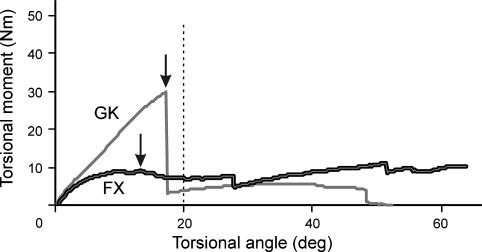
Thereafter, both ends of the bones were embedded in methylmethacrylate cement, but not including the locking screws. The entry hole in the proximal tibia for the nail was filled with a soft silicone material before embedding to prevent direct contact between the implant and the cement. The embedded ends of the specimens were mounted in the testing machine. Axial traction of 20 N was applied (Fig. 4). A moment then was imposed, starting at zero until reaching 1 Nm. This is less than 10% of the failure load and represents a load that does not cause gross structural changes. Then the rotational direction was changed until a moment of −1 Nm was reached. The rotational speed was 0.1 Nm per second. Moment and rotational angle were recorded continuously by the software. From the resulting curves, the torsional rigidity was calculated as the slope between 1 Nm and −1 Nm (Fig. 5). The play (the unconstrained rotation) was defined as the offset in angle between the curves obtained in the opposite directions. The offset angle was calculated from the points corresponding to 0.25 Nm and −0.25 Nm to avoid uncertainty in the region of zero moment (Fig. 5). In two specimens, the measurements of play and initial torsional rigidity were missed. Thereafter, a rotational force was applied at a speed of 0.5° per second for 60° or until the construct failed. The highest moment before reaching 20° rotation was defined as the overall torsional strength of the construct (Fig. 6). During the latter testing procedure, a compressive axial load of 150 N was applied, assumed to simulate the force from muscle tone and soft tissue resistance in a nonweightbearing situation.
Fig. 4.

A specimen loaded in the servohydraulic biaxial testing machine for measurement of play, torsional rigidity, and maximal rotational strength is shown.
Fig. 5.
A typical curve for calculation of play and rotational rigidity is shown.
Fig. 6.
A typical curve for calculation of maximal rotational strength, defined as maximal moment before 20° deformation, is shown. GK = interlocked nail; FX = inflatable nail.
Mean differences for each pair were calculated for all mechanical variables and paired comparisons for the two nails were analyzed by the one-sample t test of differences, using SPSS statistical software (SPSS Inc, Chicago, IL). We calculated statistical power post hoc for the different variables.
Results
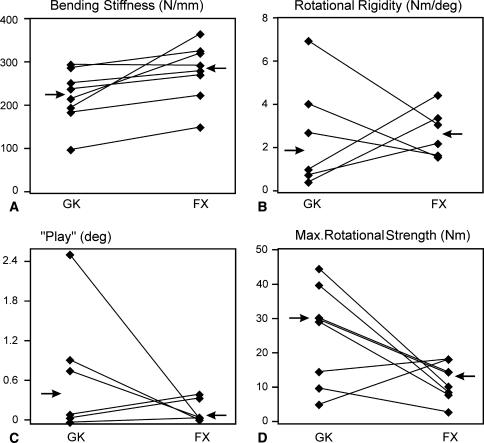
We observed a large interindividual variation for the mechanical results. The inflatable nail had a higher (p = 0.02) bending stiffness than the locked nail, with a mean of 280.8 N/mm and 222.7 N/mm, respectively. We found no differences in initial torsional rigidity and play between the two types of nails. We observed a large scatter for those two parameters in the group of interlocked nails (Fig. 7). For torsional rigidity, power analysis revealed an effect size of 4.51 Nm per degree would be needed to obtain a difference at 80% power, whereas the observed difference was only 0.08 Nm per degree. The corresponding values for play were a needed effect size of 2.22° at 80% power and an observed difference of 0.77 (Table 1).
Fig. 7A–D.
Results of biomechanical testing show interindividual variance in terms of (A) bending stiffness, (B) rotational rigidity, (C) play, and (D) maximal rotational strength. GK = interlocked nail; FX = inflatable nail. Arrows indicate mean in all figures.
Table 1.
Biomechanical testing results of an interlocking intramedullary nail and an inflatable nail
| Biomechanical test | Interlocking nail (GK) | Expandable nail (FX) | Paired difference (GK − FX) (p value) | Median paired ratio (GK/FX) |
|---|---|---|---|---|
| Bending stiffness (N/mm)(n = 8) | 222.7 (169.5–275.9) | 280.8 (224.7–336.8) | −58.1 (−103.5–12.6) (p = 0.02) | 1.2 |
| Rotational rigidity (Nm/degree)(n = 6) | 2.72 (0.07–5.37) | 2.80 (1.62–3.97) | −0.08 (−3.22–3.07) (p = 0.95) | 1.7 |
| Play (degrees)(n = 6) | 1.15 (−0.24–2.54) | 0.38 (0.12–0.64) | 0.77 (−0.77–2.32) (p = 0.26) | 1.8 |
| Maximum rotational strength (Nm)(n = 8) | 26.1 (14.3–37.9) | 12.6 (8.1–17.1) | 13.49 (−0.08–27.05) (p = 0.05) | 0.4 |
Values are expressed as means, with confidence intervals in parentheses.
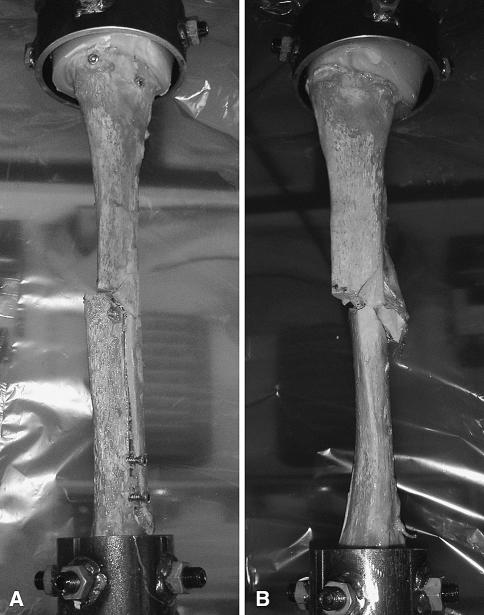
During testing of torsional strength, all interlocked nail-bone constructs failed by fracture of the bone through the distal locking screw holes. The hydraulic nail-bone constructs failed initially by slippage between the nail and bone. At higher deformations, the initial fracture site developed new fracture lines in most of the specimens (Fig. 8). The rotational strength for the inflatable nail was lower (p = 0.05) than that for the interlocked nail, with 12.6 Nm and 26.1 Nm peak moments, respectively, before reaching 20° rotation.
Fig. 8A–B.
Specimens after rotational testing to failure for (A) the interlocked nail and (B) the inflatable nail are shown.
Discussion
Recently developed inflatable nails avoid reaming and interlocking screws in tibial fractures and reflect a new principle for stabilization of long bone fractures. These nails have been used clinically in the humerus and tibia with some success [3, 6, 9, 13, 25]. We asked if the bending stiffness, rotational rigidity, or play (looseness of rotation) differed between an inflatable versus large-diameter reamed interlocked nails, and whether the maximal torque to failure of the two bone-implant constructs differed.
It is difficult to fully mimic the mechanical forces in the clinical situation with the combined effects of canal pressure from the osteosynthesis, muscular axial compression forces, friction in the fracture, and soft tissue resistance. We opposed the tendency of elongation/separation of fragments by the obliquity of the fracture during rotation in the unlocked hydraulic nail construct by application of axial load. The amount of resistance in vivo is not known, but we have estimated the value in a nonweightbearing situation to 150 N. In vivo, the axial forces will increase and tend to separate fragments axially, with increased rotational force. We used an oblique fracture, which gives increased resistance to rotation by the obliqueness of the fracture line, and the more subtle irregularities of a fracture, which results in a great increase of friction compared with osteotomies [22]. This model is considered more similar to the most frequent types of low-energy clinical tibial shaft fractures. A more comminuted fracture with low intrinsic axial and rotational stability would be, in our opinion, less suitable for stabilization by a nail without interlocking screws. The data may also be influenced by bone quality, which we did not determine. However, these influences would be limited by the paired study design.
Bending stiffness, rotational rigidity, and play influence the healing environment for a diaphyseal fracture. We found a 25% higher mean bending stiffness in the inflatable nail. We presume this relates to better contact between the implant and the walls of the medullary canal and a stiffer implant. We have not performed tests of the implant alone and therefore cannot differentiate between these factors.
We assume the rotational play indicates an instability that can occur during normal clinical loading, even without weightbearing. Play will induce shearing movements in the initial healing phase that can prevent or delay fracture consolidation as reported in animal models [2, 18]. We found no differences in play, but the scatter of the results was higher with the interlocked nail (Fig. 6). We observed the same pattern for rotational rigidity and maximal rotational strength. Owing to what we considered a high effect size, we found a difference between the implants for maximal rotational strength. The scatter suggests the interlocked nail system may be more technique and operator sensitive, and more influenced by bone quality. The high scatter is to some degree compensated for by the use of paired comparison. However, a higher number or a more homogenous selection of specimens could have revealed differences not detected in this study.
The maximum torque before fracture for intact tibia cadaver bones is in the order of 100 Nm [17]. Our findings of torsional strength of 13 Nm for the inflatable nail and 26 Nm for the interlocked nail are, in relation to intact tibiae, quite low. In this study, we used the 8.5-mm inflatable nail with expanding capacity up to 13.5 mm. The larger-diameter nail (10 mm with expansion to 16 mm) might have resulted in improved mechanical properties. However, the manufacturer recommends using the large diameter only for an isthmus diameter greater than 12 mm, and reaming of the opposite side resulted in good cortical contact at lower diameters in all specimens.
The theoretical basis for the inflatable implant is that expansion of the nail results in high pressure against the inner wall of the medullary cavity and an extended area of contact, both contributing to high frictional forces between bone and nail. At the same time, the larger diameter of the nail increases the area and polar moment of inertia, increasing the torsional and bending resistance of the nail by a factor of 4. The absence of locking screws may imply immediate full dynamization of the fracture postoperatively.
Mechanical testing by Blum et al. [5] of the inflatable nail in the humerus revealed a lower torsional stiffness for humeral bones with a funnel-shaped medullary cavity than for bones with a well-defined isthmus. A transverse osteotomy fracture model was used, with a gap of 3 mm. Thus, there is no friction at the fracture site, and with a funnel-shaped medullary cavity and without soft tissue, there is virtually no resistance to rotation with the inflatable nail. We found the same relatively low rotational strength for the inflatable nail in our tibial model, with a well defined isthmus and a fracture type with a high inherent rotational stability and good contact between the fragments.
This new concept of nail construction using a hydraulic inflatable nail, inserted in an unexpanded condition, has provided good results in certain diaphyseal fractures of long bones [3, 9, 13, 25]. The clinical data, however, are somewhat limited, with only one controlled study published [3]. The inflatable nail had a shorter duration of surgery and fewer reoperations and rehospitalizations compared with an interlocking intramedullary nail (Mathys, Bettlach, Switzerland). The control nail in that study was an unreamed nail, which would affect the outcome negatively compared with a large-diameter reamed nail, according to several studies [4, 7, 8]. Intuitively, and as suggested by our data and that of Blum et al. [5], the weak link of an inflatable nail without locking screws would be control of rotation, whereas the ability to fill out the intramedullary canal diameter would give good control of shear and bending forces. None of the clinical studies report malrotation with inflatable nails used in the tibia [3, 9, 13, 25]. This is in accordance with most studies of tibia fractures treated with conventional intramedullary nailing. However, in two studies where malrotation was specifically examined, malrotation greater than 10° was reported in more than 20% of the patients treated with a conventional intramedullary nail, which suggests malrotation often is underreported and difficult to assess clinically [14, 19].
The values for torsional strength of approximately 15 Nm for the hydraulic nailing still means withstanding up to 60 N at the forefoot, which we consider sufficient for controlled weightbearing. The tested nail-bone consisted of isolated tibiae, whereas in clinical situations soft tissue and the presence of the fibula will influence, and probably increase, the stability, especially in rotation. Our experimental design using axial compression force will add stability but we suspect does not fully compensate for the lack of the surrounding tissue.
The hydraulic nail, in contrast to the locked nail, depends on intrinsic stability in the fracture. Based on the current results, we recommend restricting its use to diaphyseal fractures with greater than 50% contact between the main fragments, and weightbearing should be recommended with caution until there are signs of fracture consolidation. However, as the procedure is fast and provides good results in clinical studies, clinical use in selected cases may be warranted.
Acknowledgments
We thank Stein Atle Lie, PhD, Department of Health, University Research Bergen, for assistance in the statistical analysis.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Alho A, Benterud JG, Høgevold HE, Ekeland A, Stromsøe K. Comparison of functional bracing and locked intramedullary nailing in the treatment of displaced tibial shaft fractures. Clin Orthop Relat Res. 1992;277:243–250. [PubMed]
- 2.Augat P, Burger J, Schorlemmer S, Henke T, Peraus M, Claes L. Shear movement at the fracture site delays healing in a diaphyseal fracture model. J Orthop Res. 2003;21:1011–1017. [DOI] [PubMed]
- 3.Ben-Galim P, Rosenblatt Y, Parnes N, Dekel S, Steinberg EL. Intramedullary fixation of tibial shaft fractures using an expandable nail. Clin Orthop Relat Res. 2007;455:234–240. [DOI] [PubMed]
- 4.Blachut PA, O’Brien PJ, Meek RN, Broekhuyse HM. Interlocking intramedullary nailing with and without reaming for the treatment of closed fractures of the tibial shaft: a prospective, randomized study. J Bone Joint Surg Am. 1997;79:640–646. [DOI] [PubMed]
- 5.Blum J, Karagul G, Sternstein W, Rommens PM. Bending and torsional stiffness in cadaver humeri fixed with a self-locking expandable or interlocking nail system: a mechanical study. J Orthop Trauma. 2005;19:535–542. [DOI] [PubMed]
- 6.Capelli RM, Galmarini V, Molinari GP, De Amicis A. The Fixion expansion nail in the surgical treatment of diaphyseal fractures of the humerus and tibia: our experience. Chir Organi Mov. 2003;88:57–64. [PubMed]
- 7.Court-Brown CM. Reamed intramedullary tibial nailing: an overview and analysis of 1106 cases. J Orthop Trauma. 2004;18:96–101. [DOI] [PubMed]
- 8.Finkemeier CG, Schmidt AH, Kyle RF, Templeman DC, Varecka TF. A prospective, randomized study of intramedullary nails inserted with and without reaming for the treatment of open and closed fractures of the tibial shaft. J Orthop Trauma. 2000;14:187–193. [DOI] [PubMed]
- 9.Franck WM, Olivieri M, Jannasch O, Hennig FF. An expandable nailing system for the management of pathological humerus fractures. Arch Orthop Trauma Surg. 2002;122:400–405. [DOI] [PubMed]
- 10.Gugala Z, Nana A, Lindsey RW. Tibial intramedullary nail distal interlocking screw placement: comparison of the free-hand versus distally-based targeting device techniques. Injury. 2001;32(suppl 4):SD21–SD25. [DOI] [PubMed]
- 11.Harris I, Lyons M. Reoperation rate in diaphyseal tibia fractures. ANZ J Surg. 2005;75:1041–1044. [DOI] [PubMed]
- 12.Hooper GJ, Keddell RG, Penny ID. Conservative management or closed nailing for tibial shaft fractures: a randomised prospective trial. J Bone Joint Surg Br. 1991;73:83–85. [DOI] [PubMed]
- 13.Jovanovic A, Pirpiris M, Semirli H, Doig SG. Fixion nails for humeral fractures. Injury. 2004;35:1140–1142. [DOI] [PubMed]
- 14.Kahn KM, Beals RK. Malrotation after locked intramedullary tibial nailing: three case reports and review of the literature. J Trauma. 2002;53:549–552. [DOI] [PubMed]
- 15.Karladani AH, Granhed H, Edshage B, Jerre R, Styf J. Displaced tibial shaft fractures: a prospective randomized study of closed intramedullary nailing versus cast treatment in 53 patients. Acta Orthop Scand. 2000;71:160–167. [DOI] [PubMed]
- 16.Koval KJ, Clapper MF, Brumback RJ, Ellison PS Jr, Poka A, Bathon GH, Burgess AR. Complications of reamed intramedullary nailing of the tibia. J Orthop Trauma. 1991;5:184–189. [DOI] [PubMed]
- 17.Martens M, van Audekercke R, de Meester P, Mulier JC. The mechanical characteristics of the long bones of the lower extremity in torsional loading. J Biomech. 1980;13:667–676. [DOI] [PubMed]
- 18.Mølster AO. Effects of rotational instability on healing of femoral osteotomies in the rat. Acta Orthop Scand. 1984;55:632–636. [DOI] [PubMed]
- 19.Puloski S, Romano C, Buckley R, Powell J. Rotational malalignment of the tibia following reamed intramedullary nail fixation. J Orthop Trauma. 2004;18:397–402. [DOI] [PubMed]
- 20.Sanders R, Koval KJ, DiPasquale T, Schmelling G, Stenzler S, Ross E. Exposure of the orthopaedic surgeon to radiation. J Bone Joint Surg Am. 1993;75:326–330. [DOI] [PubMed]
- 21.Schandelmaier P, Krettek C, Tscherne H. Biomechanical study of nine different tibia locking nails. J Orthop Trauma. 1996;10:37–44. [DOI] [PubMed]
- 22.Seligson D, Byrt W, Hogan M, Pope M. The mechanical basis for the combined use of internal and external fixation by direct measurement of fracture gap motion (abstract). 2nd International Symposium on Internal Fixation of Fractures. Lyon, France: Faculte Medecine Alexis Carrel; 1982:166–167.
- 23.Smith MG, Canty SJ, Khan SA. Fixion: an inflatable or deflatable nail? Injury. 2004;35:329–331. [DOI] [PubMed]
- 24.Steinberg EL, Blumberg N, Dekel S. The Fixion proximal femur nailing system: biomechanical properties of the nail and a cadaveric study. J Biomech. 2005;38:63–68. [DOI] [PubMed]
- 25.Steinberg EL, Geller DS, Yacoubian SV, Shasha N, Dekel S, Lorich DG. Intramedullary fixation of tibial shaft fractures using an expandable nail: early results of 54 acute tibial shaft fractures. J Orthop Trauma. 2006;20:303–309. [DOI] [PubMed]