Abstract
Functionally active complement system and complement regulatory proteins are present in the normal human and rodent eye. Complement activation and its regulation by ocular complement regulatory proteins contribute to the pathology of various ocular diseases including keratitis, uveitis and age-related macular degeneration. Furthermore, a strong relationship between age-related macular degeneration and polymorphism in the genes of certain complement components/complement regulatory proteins is now well established. Recombinant forms of the naturally occurring complement regulatory proteins have been exploited in the animal models for treatment of these ocular diseases. It is hoped that in the future recombinant complement regulatory proteins will be used as novel therapeutic agents in the clinic for the treatment of keratitis, uveitis, and age-related macular degeneration.
Keywords: Complement system, Complement regulatory proteins, Eye, Corneal inflammation, Uveitis, Age-related macular degeneration
Complement system
Complement has long been recognized as a critical component of the innate immune system [1–6]. It comprises of soluble and surface proteins that play a central role in host defense against infection and in the modulation of antigen-specific immune and inflammatory responses [4, 5]. Thus, complement also serves as a bridge between innate and adaptive immunity. The complement system can be activated by three proteolytic cascades namely, the classical, the alternative, and the lectin pathways (Fig. 1). Although the initial signal for the activation of each cascade differs, complement activation via these pathways triggers a sequence of biologic reactions in which each component is activated by the upstream component [3, 5]. This sequential activation of complement components by all three pathways leads to the formation of membrane attack complex (MAC). Under normal conditions, the activation of the complement system is kept under tight control by the coordinated action of soluble and membrane-associated complement regulatory proteins (CRegs). However, interference with the function and/or expression of CRegs leads to unwanted host tissue damage and tissue pathology due to unregulated complement activation [7, 8].
Fig. 1.
Complement system and complement regulatory proteins (CRegs). The complement system can be activated through three pathways and complement activation triggers a sequence of biological reactions which result in the generation of effector molecules (e.g., C3a, C3b, C5a, MAC) with potent immunological activities. The classical pathway can be activated by antigen-antibody complexes or by substances such a C-reactive protein. C1, C2, C4, and C3 are the components of the classical pathway. Activation of the alternative pathway does not require the presence of an antibody; C3, factor B, factor D, and properdin are the components of the alternative pathway. Like the alternative pathway, the activation of the lectin pathway is also antibody independent and can be achieved by interaction of serum lectins (e.g., mannose-binding protein, MBL), with sugar residues present on the bacterial cell wall. All three pathways converge on a common reaction that results in the formation of an enzyme—C3 convertase. This enzyme cleaves C3 into C3a and C3b. C3b forms C5 convertase that ultimately leads to the formation of membrane attack complex (MAC). The complement cascade is regulated at different check points (shown with black blocks) by CRegs. The soluble CRegs are shown in white boxes and the membrane-bound CRegs are shown in gray boxes
CRegs can be broadly categorized into two classes—membrane-bound CRegs and soluble CRegs (Fig. 1). Membrane-bound CRegs (Fig. 1) include decay-accelerating factor (DAF, CD55), membrane co-factor protein (MCP, CD46), complement receptor 1 (CR1, CD35), and membrane inhibitor of reactive lysis (MIRL, CD59). DAF, a glycosylphosphatidylinositol (GPI)-anchored protein prevents the activation of the complement system by inhibiting the formation of C3 and C5 convertases of both the classical and alternative pathways and accelerating the decay of these convertases [9, 10]. However, DAF does not irreversibly inactivate C3b and C4b and, after interaction with DAF, these molecules still possess cytolytic activity. MCP a transmembrane glycoprotein regulates the complement cascade by serving as a co-factor for serine protease factor I, which irreversibly inactivates the hemolytic potential of C3b and C4b [11, 12]. CR1 has been reported to possess both decay-accelerating and co-factor activities [13]. Like DAF, CD59 is also attached to the cell surface by GPI anchors. CD59 acts at the terminal step of complement activation and prevents the formation of membrane attack complex (MAC, C5b-9 complex), the final activation product of all three complement cascades by blocking the incorporation of C9 [14, 15]. Crry (5I2 antigen) is a C3 convertase inhibitor that possesses both decay-accelerating and membrane co-factor activities and present only in rodents [16, 17]. However, DAF, MCP, and CD59 have also been identified and characterized in rodents [18–23].
C1 inhibitor (C1INH), C4 binding protein (C4bp), complement factor H (CFH), complement factor I (CFI), S-protein and clustrin, are the examples of important soluble CRegs (Fig. 1). C1INH regulates activation of the classical complement pathway by inactivating the protease function of activated C1 complex. It also prevents spontaneous activation of C1 and binding to the zymogen forms of C1r and C1s [24]. C4bp acts as a co-factor for CFI, catalyzing the cleavage and inactivation of C4b [25]. CFH inhibits C3 activation by binding to C3b and acting as a co-factor for factor I-mediated cleavage of C3b and also has decay-accelerating activity for the alternative pathway C3 convertase, C3bBb. It also competes with factor B for surface-bound C3b [26]. Both clustrin and S-protein prevent the formation of MAC [6]. Soluble forms of MCP, DAF, CR1, CD59, and Crry have been reported to be present in various biological fluids in both humans and rodents [27–30]. Thus, a wide variety of CRegs (both membrane bound and soluble) have evolved to create efficient checkpoints at critical steps of complement cascades so that the host could be protected from the inadvertent activation of complement on its own tissue (Fig. 1).
Since complement is a powerful cytotoxic defense system, regulation of complement activation is crucial for host tissue damage control during inflammation especially in a sensitive organ like the eye. The eye is an immunologically privileged site and ocular immune privilege does not refer to the absence of immune system but, rather its fine regulation [31]. The studies discussed in this article highlight the role of complement activation and regulation in the protection of the normal eye. In addition, the studies discussed below demonstrate the importance of interplay between complement activation and complement regulation in the development of vision-threatening complications such as keratitis, uveitis, and macular degeneration.
Role of complement in the protection of the normal eye
It is important that we discuss the role of complement and CRegs in ocular protection under normal conditions before discussing their importance in ocular pathology. As mentioned above, the eye is an immune-privileged organ [31] and is highly vulnerable to various immunological insults. Therefore, it is not surprising that the complement system, which represents the first line of defense, plays an important part not only in protecting the eye from immunological insults but also in maintaining the immune-privileged state of the eye. Our results and several other independent studies have demonstrated the presence of various components of the complement system in the normal eye [2, 32–37]. We have further shown that ocular complement components are not just silent bystanders but are chronically active at a low level in normal eye [32]. We reported that both iC3b (activation product of C3) and MAC (end product of complement activation) are present in normal rat eye indicating that the complement system is continuously activated at a low level in the normal eye [32]. In 2003, we documented that the interaction between complement activation product iC3b and its receptor is vital for the creation of immunosuppressive environment that leads to the induction and the maintenance of ocular immune privilege and protection of intraocular structures that are critical for vision [38]. The presence and expression pattern of CRegs in the normal human eye was first described by us [33]. We reported that membrane-bound CRegs—MCP, DAF, and CD59—are differentially expressed in normal human and eyes [33]. Our studies along with other independent studies that were performed later demonstrated that Crry and CD59 (membrane bound and soluble) are also present in the normal rodent eye [32, 34, 35]. We have further shown that ocular CRegs are functionally active and tightly regulate the activation of intraocular complement [27, 32]. Functional inhibition of ocular CRegs using specific antibodies resulted in unregulated complement activation leading to severe intraocular inflammation in normal animals [32]. Furthermore, complement inhibitory activity in normal human intraocular fluid was blocked by inhibiting the function of MCP, DAF, and CD59 [27].
Thus, our results clearly established that within the normal eye the complement system seems to perform two important functions. First, the chronic low level of complement activation serves as a primary defense mechanism of the eye against pathogenic infection and is finely regulated by the soluble and membrane-bound intraocular complement regulatory proteins. This enables destruction of the putative pathogen without inadvertent damage of ocular tissue, which is vital for the maintenance of vision. Second, complement activation products (such as iC3b) generated as a result of the low level of complement activation results in the selective suppression of harmful T cell responses. In this role complement protects the eye from innocent bystander destruction associated with the T cell response to the invading pathogens. Complement components and CRegs present in normal tears have also been reported to be functionally active and have been proposed to serve as first line of defense in protecting the eye [36]. However, additional studies are required to determine the role of the complement system in normal tears.
Role of complement in corneal disease
The cornea is constantly exposed to various physical as well as immunological insults. Indeed the normal cornea is well equipped to protect itself from these insults and has been shown to possess functional complement activity [39–46]. In addition, low levels of C3, C3 split products, and MAC were detected in the normal cornea [32, 39, 46]. This observation further proves that low level of complement activation is taking place in the normal cornea since complement activation is necessary for the generation of these products. Studies reported in the literature suggest that complement cascade can be aggressively activated in the cornea during an immune and inflammatory reaction [45, 46]. Two reports by Mondino and colleagues described interesting sets of experiments [45, 46]. In these experiments, the normal cornea from human donors was exposed to lipopolysaccharide (LPS), ribitol teichoic acid immune complex, acid (HCl), or alkali (NaOH) separately and the generation of anaphylatoxins—C3a, C4a, and C5a—as well as MAC in the corneas was monitored. It was reported that anaphylatoxins—C3a, C4a, and C5a—could be generated when the cornea was injured with LPS, immune complexes, acid, or alkali. Interestingly MAC could only be generated when the cornea was exposed to LPS or immune complexes. Cornea failed to generate MAC when insulted with acid or alkali. The immune response mounted to LPS or immune complex is similar to that generated against infectious agents like gram-negative bacteria. Indeed the complement system has been shown to play a critical role in protection against Pseudomonas aeruginosa infection that causes keratitis [47, 48]. Additionally, complement activation is believed to play an important role in ulceration of human cornea induced by gram-negative bacteria [49].
The aforementioned observations have important clinical implications. If in future anti-complement agents were to be considered for the treatment of corneal pathology, anaphylatoxins would be an ideal target for the patient presenting with chemical injury such as exposure to acid or alkali. On the other hand, in the case of bacterial infection both anti-anaphylatoxin and anti-MAC therapy should be considered. Although as discussed below the cornea possesses the ability to express different CRegs to protect itself from complement-mediated damage, it may not be able to upregulate various CRegs to an appropriate level during an acute episode of complement activation as observed during chemical insults or acute bacterial infection. In such cases, topical application of recombinant CRegs could be beneficial and serve as a better alternative for intervention.
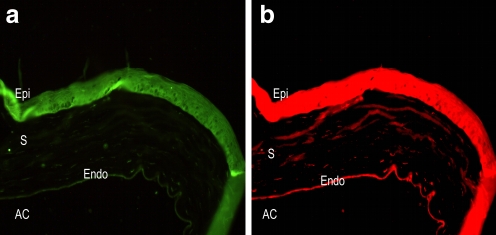
Enhanced complement activation can cause damage to the autologous corneal tissue during an infection or inflammation. Membrane-bound CRegs such as MCP, DAF, Crry (Fig. 2a), and CD59 (Fig. 2b) are expressed in the different layers of the cornea to protect this tissue from complement-mediated damage [27, 33, 50]. Interestingly, compared to corneal stroma and corneal endothelium, various CRegs are very strongly expressed on the corneal epithelium [33] (Fig. 2a and b). This high expression of CRegs on the corneal epithelium is crucial for the protection of the cornea because the cornea is continually exposed to various pathogens including bacteria. These bacteria produce phospholipase and other enzymes which can remove GPI-anchored DAF and CD59 from the corneal surface [51]. Thus, in the absence of a very high expression of CRegs on the corneal epithelium, bacterially induced loss of DAF and CD59 could be deleterious to the cornea and lead to vision loss after the putative pathogen has been destroyed by the complement system. To investigate if a deficiency or abnormality in the expression of CRegs may play a role in ocular surface disease, systemic examination of corneal tissue from patients with different diseases such as pseudophakic bullous keratopathy, HSV-1 keratitis, and herpes zoster scleritis is needed.
Fig. 2.
Complement regulatory proteins in normal cornea. The figure shows immunofluorescent staining for Crry (a) and CD59 (b) in the cornea of naive Lewis rat. Objective magnification ×20. Epi Epithelium, S stroma, Endo endothelium, AC anterior chamber
Role of complement in autoimmune uveitis
Uveitis, the inflammation of the uveal tract, can be classified anatomically as anterior, intermediate, posterior, or diffuse (panuveitis) depending on the segment of the eye that is affected. Each year, approximately 17% of active uveitis patients experience some degree of vision loss [52]. Uveitis may be idiopathic, associated with systemic diseases such as Behçet’s disease, and Vogt–Koyanagi–Harada disease or resulting from a variety of infectious agents. Inflammation resulting from uveitis may lead to conditions like cataract, glaucoma, and cystoid macular edema that may cause irreversible vision loss. Anterior uveitis is the most common form of uveitis, and the most common form of anterior uveitis is of unknown (i.e., idiopathic) etiology [52].
Although the exact cause of the disease is still unknown, a wide array of studies using different animal models have established that the inflammation in uveitis is due to an autoimmune response to various ocular antigens [53–56]. Unfortunately, almost all of the studies in the past three decades have focused on the role of T cells in the pathogenesis of uveitis [54, 57, 58]. Very few laboratories have investigated the role of the complement system in the development of autoimmune uveitis [32, 58–66].
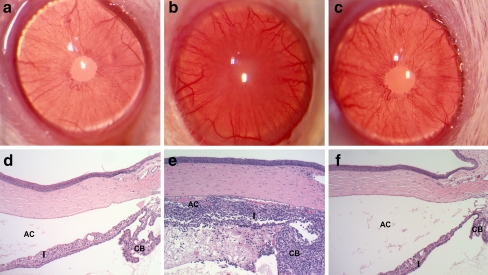
Through our recent studies, the critical role of complement and complement regulatory proteins (CRegs) in the pathogenesis of idiopathic anterior uveitis was addressed and recognized. Our laboratory has used experimental autoimmune anterior uveitis (EAAU)—an animal model of human autoimmune anterior uveitis—to investigate the role of the complement system, a significant and previously neglected facet of uveitis [53, 62, 63]. EAAU is induced by injecting bovine melanin-associated antigen emulsified in Freund’s complete adjuvant, in the foot pad of Lewis rats [53]. The onset of the disease (days 12–14 post immunization) is marked by inflammation of the iris/ciliary body followed by massive infiltration of the inflammatory cells in the anterior segment of the eye during the peak (days 16–19 post immunization) of EAAU (Fig. 3). The inflammation resolves after approximately 3 weeks, and the eye returns to the normal state with no apparent sign of any tissue damage (Fig. 3). Interestingly, studies from our laboratory have demonstrated that the activation of the complement system is critical for the development of EAAU [62]. During EAAU, the complement system is activated (detected by Western blot analysis for iC3b) in the eye, and the kinetics of complement activation follows a pattern that is similar to the clinical course of the disease. Furthermore, depletion of the complement system of the host resulted in complete inhibition of EAAU. In complement-depleted rats, the levels of IFN-γ, IP-10, ICAM-1, and LECAM-1 were extremely low compared to the complement-sufficient rats during EAAU. Our observations suggest that the activation of the local complement system plays a critical role in the development of inflammation during EAAU and suppression of intraocular complement system, thus may provide a successful strategy for uveitis therapy. At present, the exact mechanism and pathways involved in local complement activation during uveitis are not known. It is also not known if the increase in complement components in the anterior segment of the eye is due to the upregulation of their synthesis by resident ocular cells or is a result of spillover from the systemic complement system. Previous studies from our laboratory established that a functionally active complement system is present in the anterior segment of the eye because when a well-known activator of complement such as zymosan was injected in the anterior chamber, severe anterior uveitis was induced. This zymosan-induced uveitis was due to the activation of the complement system because anterior uveitis was completely inhibited when the complement system of the host was depleted [32]. Furthermore, we and others have reported the presence of various complement components in aqueous humor as well as other parts of the normal eye [32, 39, 41, 59, 61]. These observations taken together suggest that ocular complement is activated during the course of EAAU and the inhibition of the intraocular complement system may lead to more effective management and/or treatment of autoimmune uveitis.
Fig. 3.
Clinical and histologic pictures of rat eye during different stages of experimental autoimmune anterior uveitis (EAAU). No inflammation could be detected in the iris (I) and the ciliary body (CB) after clinical (a) and histologic (d) examination at day 8 post immunization (before the onset of EAAU). At the peak of disease (day 19 post immunization) the anterior chamber (AC) appeared cloudy and opaque due to the presence of proteinaceous material and inflammatory cells (b). Histopathologic picture of rat eye at the peak of EAAU (e) revealed severe inflammation of the iris (I) and ciliary body (CB). Heavy infiltration in the anterior chamber (AC) with spillover into the anterior vitreous was also observed at this time point. The eye appeared normal both clinically (c) and histologically (f) after the resolution of EAAU (day 30 post immunization). Objective magnification ×10
When considering anti-complement therapy, we cannot ignore the role of CRegs in the resolution of autoimmune uveitis. We have demonstrated that the functionally active CRegs downregulate intraocular complement activation and are critical to protect the ocular tissues from complement-mediated damage during EAAU [63]. We observed that various CRegs were upregulated during the course of EAAU on the resident ocular tissue and this upregulation was not due to the infiltrating inflammatory cells because the levels of CRegs remained upregulated after the resolution of the disease when all the infiltrating cells were cleared from the anterior segment of the eye [63]. Furthermore, when the function or expression of CRegs was inhibited in vivo, more severe EAAU with early onset and delayed resolution was observed. These observations demonstrate that ocular tissue can protect itself by upregulating various CRegs during uveitis and provide strong evidence for the use of recombinant CRegs as therapeutic agents in the treatment of autoimmune uveitis.
Activation of the complement system has also been reported in other animal models of anterior uveitis such as endotoxin-induced uveitis (EIU) [64, 65]. In EIU, it was demonstrated that the complement system is critical for the development of inflammation, and there is a local activation of the complement system as evident by accumulation of complement components (C1q, C3, and C4) in various parts of the eye during inflammation [66]. Activation of the complement system was also implicated in experimental allergic uveitis [67]. Using experimental autoimmune uveoretinitis (EAU) animal model, the complement system has been reported to play an important role in the pathogenesis posterior uveitis [68]. Recently, Read and co-workers demonstrated that the transgenic mice that express soluble Crry in the retina had decreased incidence and severity of EAU [68]. In these transgenic mice, EAU was not completely suppressed. This may be due to relatively low levels of Crry expressed compared with the levels that are required for the complete inhibition of the complement system. It is possible that a higher dose of exogenous Crry or similar CReg may result in complete inhibition of EAU.
Thus, these studies provide strong evidence that the complement system and CRegs play an important role in the pathogenesis of autoimmune uveitis and provide alternative approaches for the development of effective therapy. More research in the future will present us enough information to develop anti-complement therapy for uveitis. Hopefully, in the future, complement inhibitors might be used as novel anti-uveitic agents in the clinic for the treatment of this important form of human ocular disease.
Role of complement in age-related macular degeneration
Age-related macular degeneration (AMD) is the most common cause of legal blindness worldwide among the elderly over the age of 50. Approximately 1.8 million people in the United States alone have AMD and it is projected that by 2020, roughly 2.9 million people will develop this disease [69–71]. In AMD, there is a progressive destruction of the macula leading to the loss of central vision. AMD is classified into non-exudative (dry type) and exudative (wet type) [69–71]. In the dry type of AMD, drusen—small yellow deposits—are formed between the retinal-pigmented epithelium (RPE) and Bruch’s membrane [72]. In wet-type AMD, abnormal vessel growth takes place from choroid, termed choroidal neovascularization (CNV), under the retinal pigment epithelium [71, 72]. Although several risk factors are associated with AMD, the exact pathogenesis still remains unknown. The last few years have witnessed an amazing series of research establishing the central role of the complement system in the pathogenesis of AMD both in humans and in experimental animals. Various studies in the literature have indicated a potential role for complement in drusen formation in the non-exudative form of AMD in humans [73–75]. Complement components, complement activation products (C3a, C5a, MAC), and complement regulatory proteins (CD46, Vitronectin) have been localized in drusen in patients with AMD [73–75].
The discovery of allelic variants of complement factor H (CFH) as a major risk factor for AMD has become a landmark study [76–79]. The polymorphism that gives rise to this allelic variant of CFH results from a tyrosine to histidine replacement at position 402. The “high risk” variant, i.e., homozygous for histidine residue at position 402 is associated with five- to sevenfold increased risk of AMD [76–79]. CFH consists of 20 short consensus repeats (SCRs) and the polymorphic site 402 resides in SCR7. SCR7 contains the binding site for C3b, glycosaminoglycans (GAG) and C-reactive protein (CRP). The polymorphism at position 402 in SCR7 reduces the binding affinity to CRP [80] and GAG [81]. Binding of CFH to CRP and GAG plays an important role in the regulation of the alternative pathway. Thus the polymorphic form of CFH with histidine at position 402 may have reduced ability to regulate the activation of the alternative pathway. This may lead to uncontrolled activation of alternative pathway which may result in the development of AMD. The loss of regulatory activity of CFH due to polymorphism can have a direct effect on the predisposition of the eye to AMD as it has been shown recently that CFH is expressed locally in the optic nerve, retina, and retinal pigment epithelium [82]. The importance of CFH in AMD was further demonstrated in a recent study. It was reported that the aged mice genetically deficient in CFH (cfh−/−) develop spontaneous changes in retina (e.g., photoreceptor dysfunction, increased deposition of C3 in retina, thinning of Bruch’s membrane) which is consistent with those seen in AMD [83].
Polymorphic variants of other complement components have also been shown to be associated with AMD. In a recent study, Gold et al. reported that complement components—factor B (CFB) and complement component 2 (C2)—are also associated with AMD [84]. In this report, the investigators identified high risk allele and two protective alleles for CFB and C2 that were associated with AMD. An independent study further established a similar association between CFB, C2, and AMD [85]. More recently, investigators compared 847 patients with AMD with 701 unaffected people and observed that a variant in the complement C3 gene affected the risk of developing AMD [86].
The aforementioned studies establish that the polymorphism in the genes of certain complement components and regulators genetically predisposes some individuals to AMD. However, we should also pay attention to the fact that other risk factors for AMD such as alcohol consumption and smoking nicotine can directly affect the level of complement activation and CRegs. For instance, chronic ethanol consumption upregulates CFB but downregulates CFH in mice [87]. Thus, association of alcohol consumption with AMD may be due to its direct effect on the complement system. Indeed we have reported that chronic alcohol consumption increases the size of CNV complex in rat model of laser-induced CNV [88]. Similarly, cigarette smoking has been shown to decrease the affinity of CFH for C3 and activate the complement system [89].
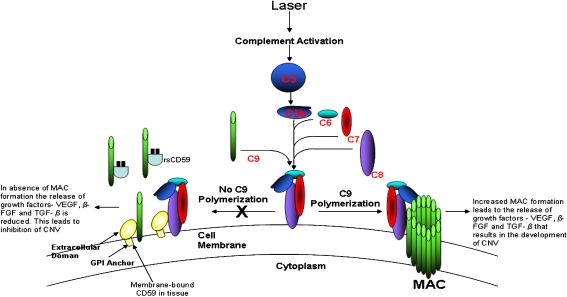
In our laboratory, we use a mouse model of laser-induced CNV to study the role of complement in the pathogenesis of wet-type AMD. A reliable way to produce CNV in animals is to rupture Bruch’s membrane with laser photocoagulation [90–92]. We and others have found that choroidal neovascularization induced in rodents by laser photocoagulation is useful to gain insights into the pathogenesis of new vessel growth from the choroid [90–96]. In 2005, we demonstrated for the first time using this animal model that complement activation and generation of MAC is critical for the development of laser-induced CNV. In this study, C3−/− mice and anti-C6-treated mice failed to develop CNV [93]. As mentioned above, the importance of C3 in the pathogenesis of AMD was recently confirmed by Yates et al., who established an association of C3 polymorphism with AMD [86]. We further observed that in the absence of MAC deposition, release of angiogenic factors such as vascular endothelial growth factor (VEGF), TGF-β2, and β-FGF was inhibited. This is a crucial observation as it suggests that the complement system is a potential therapeutic target for the treatment of CNV. Subsequently, we reported that the activation of complement by alternative pathway is responsible for MAC formation in laser-induced CNV. This alternative pathway activation was due to the decrease in CFH levels and increase in CFB levels in the RPE/choroid after laser treatment [94]. In a separate study, we used recombinant-soluble CD59-Fc chimeric protein to inhibit the formation of MAC after laser photocoagulation [95]. Treatment of mice with recombinant-soluble CD59-Fc inhibited the development of choroidal angiogenesis in the laser-induced mouse model by blocking MAC formation which in turn blocked the induction/release of angiogenic growth factors such as VEGF, β-FGF, and TGF-β2 (Fig. 4). Thus, our studies suggest that the recombinant forms of CD59 could be used as a potential drug in the future to treat CNV. Another potential target could be anaphylatoxins—C3a and C5a. It was reported that C3a and C5a are present not only in human drusen but are also localized in the choroid of mice with laser-induced CNV [97].
Fig. 4.
Role of CD59 in laser-induced choroidal neovascularization (CNV). Laser photocoagulation results in complement activation and MAC formation in the posterior segment of the eye. MAC is a complex assembly of C5b to C9 components with multimers of C9 forming a pore in the cell membrane. This causes increased release of growth factors—VEGF, TGFβ2, and β-FGF—which in turn leads to the development of CNV. The membrane-bound as well as recombinant-soluble (rs) CD59, bind to C9 and C8 and inhibit the polymerization of C9 which is prerequisite for MAC formation. In the absence of MAC, release of angiogenic factors is downregulated. This inhibits the growth of new vessel from the choroid (CNV)
Using the mouse model of laser-induced CNV, we observed that the CH50 levels in the serum of lasered mice varied when compared to non-lasered mice [93, 94]. Another study demonstrated that the plasma complement C3a des Arg levels increased in AMD patients compared to controls [98]. This increase in plasma C3a des Arg concentration reflects systemic complement activation. Thus systemic activation of the complement system may also contribute to the pathogenesis of AMD.
Currently, several different approaches are being used to treat wet AMD in humans [99]. Unfortunately, these treatment options have limitations due to their short-term and serious side effects. Although, photodynamic therapy (PDT) reduces the rate of vision loss in most patients, it does not lead to significant improvement in vision. Furthermore, repeated PDT can cause severe damage to the posterior segment of the eye and is not cost effective. Two drugs Lucentis and Macugen are approved by Federal Drug Administration for the treatment of AMD and both drugs inhibit vascular endothelial growth factor. One of the major drawbacks of Lucentis or Macugen is that repeated injections of these drugs are needed to treat AMD. Repeated injections can cause some serious side effects including hemorrhage of the eye membrane, eye pain, and vitreous floaters. Therefore, alternative therapeutic strategies with minimum side effects are required to better treat AMD patients. We believe that the results derived from the studies reviewed above would open up the window of opportunities for the development of anti-complement therapy in the treatment of AMD.
In view of important developments relative to the role of the complement system in AMD during the past several years, we believe that the next decade would be critical for such studies. We hope that the interest will continue to grow in the future so that an alternative therapy could be developed by inhibiting complement activation. Since untreated CNV leads to the irreversible loss of central vision, it is important for the pharmaceutical companies to utilize the knowledge available to them from different research laboratories and should make every effort to transfer this knowledge to develop new drugs and therapies for AMD patients.
Conclusions and clinical implications
During the last decade, a lot of progress has been made to understand the pathophysiology of corneal diseases, uveitis, and macular degeneration. Specifically, the studies defining the role of the complement system in ocular diseases have drawn a lot of attention. It is an exciting area for future investigations and the basic questions such as what triggers the complement activation and which specific pathway is involved in corneal diseases, uveitis and macular degeneration need to be addressed. This understanding will help us to develop better therapies for ocular diseases in the future so that blindness could be prevented.
The evidence derived from the studies reviewed here supports the concept that recombinant complement regulatory proteins may be therapeutically useful in the prevention of ocular tissue damage and in the treatment of various ocular diseases. Agents that specifically inhibit the complement system or complement activation products have been proven beneficial in the treatment of both human and experimental diseases over the past few years. Thus, the therapy based on complement inhibition has great potential in the future for the treatment of various ocular diseases such as keratitis, uveitis, and macular degeneration.
Acknowledgments
We thank our past and present collaborators. This work was supported in part by EY014623, EY016205, Research to Prevent Blindness NY, Pat & Willard Walker Eye Research Center, Jones Eye Institute and Arkansas Master Tobacco Settlement and Arkansas Biosciences Institute, University of Arkansas for Medical Sciences, Little Rock, AR, USA.
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Atkinson JP, Frank MM (1980) Complement. In: Parker CW (ed) Clinical immunology. Saunders, Philadelphia, pp 219–271
- 2.Jha P, Bora PS, Bora NS (2007) The role of complement system in ocular diseases including uveitis and macular degeneration. Mol Immunol 44(16):3901–3908 [DOI] [PMC free article] [PubMed]
- 3.Muller-Eberhard HJ (1988) Molecular organization and function of the complement system. Annu Rev Biochem 57:321–347 [DOI] [PubMed]
- 4.Frank MM, Fries LF (1991) The role of complement in inflammation and phagocytosis. Immunol Today 12:322–326 [DOI] [PubMed]
- 5.Reid KBM (1986) Activation and control of the complement system. Essays Biochem 22:27–68 [PubMed]
- 6.Morgan BP, Harris CL (1999) The complement system. In: Morgan BP, Harris CL (eds) Complement regulatory proteins. Academic, San Diego, pp 1–13
- 7.Liszewski MK, Farries TC, Lublin DM, Rooney IA, Atkinson JP (1996) Control of the complement system. Adv Immunol 61:201–283 [DOI] [PubMed]
- 8.Atkinson JP, Farries T (1987) Separation of self from non-self in the complement system. Immunol Today 8:212–215 [DOI] [PubMed]
- 9.Lublin DM, Atkinson JP (1987) Decay-accelerating factor and membrane cofactor protein. Curr Top Microbiol Immunol 153:123–145 [DOI] [PubMed]
- 10.Nicholson-Weller A (1992) Decay accelerating factor (CD55). Curr Top Microbiol Immunol 178:7–30 [DOI] [PubMed]
- 11.Liszewski MK, Post TW, Atkinson JP (1991) Membrane cofactor protein (MCP or CD46): Newest member of the regulators of complement activation gene cluster. Ann Rev Immunol 9:431–455 [DOI] [PubMed]
- 12.Liszewski MK, Atkinson JP (1992) Membrane cofactor protein. Curr Top Microbiol Immunol 178:45–60 [DOI] [PubMed]
- 13.Krych-Goldberg M, Atkinson JP (2001) Structure–function relationships of complement receptor type 1. Immunol Rev 180:112–122 [DOI] [PubMed]
- 14.Holguin MH, Parker CJ (1992) Membrane inhibitor of reactive lysis. Curr Top Microbiol Immunol 178:61–85 [DOI] [PubMed]
- 15.Watts MJ, Dankert JR, Morgan BP (1990) Isolation and characterization of a membrane-attack-complex inhibiting protein present in human serum and other biological fluids. Biochem J 265:471–477 [DOI] [PMC free article] [PubMed]
- 16.Kim YU, Kinoshita T, Molina H et al (1995) Mouse complement regulatory protein Crry/p65 uses the specific mechanisms of both human decay-accelerating factor and membrane cofactor protein. J Exp Med 181:151–159 [DOI] [PMC free article] [PubMed]
- 17.Takizawa H, Okada N, Okada H (1994) Complement inhibitor of rat cell membrane resembling mouse Crry/p65. J Immunol 152:3032–3038 [PubMed]
- 18.Spicer AP, Seldin MF, Gendler SJ (1995) Molecular cloning and chromosomal localization of the mouse decay-accelerating factor genes. Duplicated genes encode glycosylphosphatidylinositol-anchored and transmembrane forms. J Immunol 155:3079–3091 [PubMed]
- 19.Miwa T, Nonaka M, Okada N, Wakana S, Shiroishi T, Okada H (1998) Molecular cloning of rat and mouse membrane cofactor protein (MCP, CD46): preferential expression in testis and close linkage between the mouse Mcp and Cr2 genes on distal chromosome 1. Immunogenetics 48:363–371 [DOI] [PubMed]
- 20.Li B, Sallee C, Dehoff M, Foley S, Molina H, Holers VM (1993) Mouse Crry/p65: characterization of monoclonal antibodies and the tissue distribution of a functional homologue of human MCP and DAF. J Immunol 151:4295–4305 [PubMed]
- 21.Powell MB, Marchbank KJ, Rushmere NK, van den Berg CW, Morgan BP (1997) Molecular cloning, chromosomal localization, expression, and functional characterization of the mouse analogue of human CD59. J Immunol 158:1692–1702 [PubMed]
- 22.Qian YM, Qin X, Miwa T, Sun X, Halperin JA, Song WC (2000) Identification and functional characterization of a new gene encoding the mouse terminal complement inhibitor CD59. J Immunol 165:2528–2534 [DOI] [PubMed]
- 23.Morgan BP, Gasque P (1997) Extrahepatic complement biosynthesis: where, when and why? Clin Exp Immunol 107(1):1–7 [DOI] [PMC free article] [PubMed]
- 24.Davis AE 3rd (2004) Biological effects of C1 inhibitor. Drug News Perspect 17(7):439–446 [DOI] [PubMed]
- 25.Blom AM, Villoutreix BO, Dahlback B (2004) Functions of human complement inhibitor C4b-binding protein in relation to its structure. Arch Immunol Ther Exp (Warsz) 52(2):83–95 [PubMed]
- 26.Alexander JJ, Quigg RJ (2007) The simple design of complement factor H: looks can be deceiving. Mol Immunol 44(1–3):123–132 [DOI] [PubMed]
- 27.Sohn JH, Kaplan HJ, Suk HJ, Bora PS, Bora NS (2000) Complement regulatory activity of normal human intraocular fluid is mediated by MCP, DAF, and CD59. Invest Ophthalmol Vis Sci 41(13):4195–4202 [PMC free article] [PubMed]
- 28.Wheeler SF, Rudd PM, Davis SJ, Dwek RA, Harvey DJ (2002) Comparison of the N-linked glycans from soluble and GPI-anchored CD59 expressed in CHO cells. Glycobiology 12(4):261–271 [DOI] [PubMed]
- 29.Nonaka M, Miwa T, Okada N, Nonaka M, Okada H (1995) Multiple isoforms of guinea pig decay-accelerating factor (DAF) generated by alternative splicing. J Immunol 155(6):3037–3048 [PubMed]
- 30.Nickells MW, Alvarez JI, Lublin DM, Atkinson JP (1994) Characterization of DAF-2, a high molecular weight form of decay-accelerating factor (DAF; CD55), as a covalently cross-linked dimer of DAF-1. J Immunol 152(2):676–685 [PubMed]
- 31.Niederkorn JY (2002) Immune privilege in the anterior chamber of the eye. Crit Rev Immunol 22(1):13–46 [PubMed]
- 32.Sohn JH, Kaplan HJ, Suk HJ, Bora PS, Bora NS (2000) Chronic low level complement activation within the eye is controlled by intraocular complement regulatory proteins. Invest Ophthalmol Vis Sci 41(11):3492–3502 [PMC free article] [PubMed]
- 33.Bora NS, Gobleman CL, Atkinson JP, Pepose JS, Kaplan HJ (1993) Differential expression of the complement regulatory proteins in the human eye. Invest Ophthalmol Vis Sci 34(13):3579–3584 [PubMed]
- 34.Funabashi K, Okada N, Matsuo S, Yamamoto T, Morgan BP, Okada H (1994) Tissue distribution of complement regulatory membrane proteins in rats. Immunology 81:444–451 [PMC free article] [PubMed]
- 35.Bardenstein DS, Cheyer C, Okada N, Morgan BP, Medof ME (1999) Cell surface regulators of complement, 5I2 antigen, and CD59, in the rat eye and adnexal tissues. Invest Ophthalmol Vis Sci 40:519–524 [PubMed]
- 36.Willcox MD, Morris CA, Thakur A, Sack RA, Wickson J, Boey W (1997) Complement and complement regulatory proteins in human tears. Invest Ophthalmol Vis Sci 38(1):1–8 [PubMed]
- 37.Lass JH, Walter EI, Burris TE et al (1990) Expression of two molecular forms of the complement decay-accelerating factor in the eye and lacrimal gland. Invest Ophthalmol Vis Sci 31(6):1136–1148 [PubMed]
- 38.Sohn JH, Bora PS, Suk HJ, Molina H, Kaplan HJ, Bora NS (2003) Tolerance is dependent on complement C3 fragment iC3b binding to antigen-presenting cells. Nat Med 9(2):206–212 [DOI] [PMC free article] [PubMed]
- 39.Mondino BJ, Ratajczak HV, Goldberg DB, Schanzlin DJ, Brown SI (1980) Alternate and classical pathway components of complement in the normal cornea. Arch Ophthalmol 98(2):346–349 [DOI] [PubMed]
- 40.Mondino BJ, Hoffman DB (1980) Hemolytic complement activity in normal human donor corneas. Arch Ophthalmol 98(11):2041–2044 [DOI] [PubMed]
- 41.Mondino BJ, Brady KJ (1981) Distribution of hemolytic complement in the normal cornea. Arch Ophthalmol 99(8):1430–1433 [DOI] [PubMed]
- 42.Diehn JJ, Diehn M, Marmor MF, Brown PO (2005) Differential gene expression in anatomical compartments of the human eye. Genome Biol 6(9):R74 [DOI] [PMC free article] [PubMed]
- 43.Pleyer U, Mondino BJ, Sumner HL (1992) The effect of systemic decomplementation with cobra venom factor on corneal complement levels in guinea pigs. Invest Ophthalmol Vis Sci 33(7):2212–2215 [PubMed]
- 44.Verhagen C, Hoekzema R, Kijlstra A (1994) Human corneal extract enhances serum complement activity. Invest Ophthalmol Vis Sci 35(1):236–241 [PubMed]
- 45.Mondino BJ, Sumner HL (1990) Generation of complement-derived anaphylatoxins in normal human donor corneas. Invest Ophthalmol Vis Sci 31(10):1945–1949 [PubMed]
- 46.Mondino BJ, Chou HJ, Sumner HL (1996) Generation of complement membrane attack complex in normal human corneas. Invest Ophthalmol Vis Sci 37(8):1576–1581 [PubMed]
- 47.Cleveland RP, Hazlett LD, Leon MA, Berk RS (1983) Role of complement in murine corneal infection caused by Pseudomonas aeruginosa. Invest Ophthalmol Vis Sci 24(2):237–242 [PubMed]
- 48.Hazlett LD, Berk R (1984) Effect of C3 depletion on experimental Pseudomonas aeruginosa ocular infection: histopathological analysis. Infect Immun 43(3):783–790 [DOI] [PMC free article] [PubMed]
- 49.Mondino BJ, Brown SI, Rabin BS, Bruno J (1978) Alternate pathway activation of complement in a Proteus mirabilis ulceration of the cornea. Arch Ophthalmol 96(9):1659–1661 [DOI] [PubMed]
- 50.Bardenstein DS, Dietz Y, Lass JH, Medof ME (1994) Localization of the complement membrane attack complex inhibitor (CD59) in human conjunctiva and lacrimal gland. Curr Eye Res 13(12):851–855 [DOI] [PubMed]
- 51.Cocuzzi E, Guidubaldi J, Bardenstein DS, Chen R, Jacobs MR, Medof EM (2000) Release of complement regulatory proteins from ocular surface cells in infections. Curr Eye Res 21(5):856–866 [DOI] [PubMed]
- 52.Bora NS, Kaplan HJ (2007) Intraocular diseases—anterior uveitis. Chem Immunol Allergy 92:213–220 [DOI] [PubMed]
- 53.Bora NS, Sohn JH, Kang SG, Cruz JM, Nishihori H, Suk HJ, Wang Y, Kaplan HJ, Bora PS (2004) Type I collagen is the autoantigen in experimental autoimmune anterior uveitis. J Immunol 172(11):7086–7094 [DOI] [PubMed]
- 54.Caspi RR (2006) Mechanisms underlying autoimmune uveitis. Drug Discov Today: Disease Mechanism 3:199–206 [DOI]
- 55.Gregerson DS, Merryman CF, Obritsch WF, Donoso LA (1990) Identification of a potent new pathogenic site in human retinal S-antigen which induces experimental autoimmune uveoretinitis in LEW rats. Cell Immunol 128(1):209–219 [DOI] [PubMed]
- 56.Nussenblatt RB (1991) Proctor lecture. Experimental autoimmune uveitis: mechanisms of disease and clinical therapeutic indications. Invest Ophthalmol Vis Sci 32(13):3131–3141 [PubMed]
- 57.Prendergast RA, Iliff CE, Coskuncan NM, Caspi RR, Sartani G, Tarrant TK, Lutty GA, McLeod DS (1998) T cell traffic and the inflammatory response in experimental autoimmune uveoretinitis. Invest Ophthalmol Vis Sci 39(5):754–762 [PubMed]
- 58.Foxman EF, Zhang M, Hurst SD, Muchamuel T, Shen D, Wawrousek EF, Chan CC, Gery I (2002) Inflammatory mediators in uveitis: differential induction of cytokines and chemokines in Th1- versus Th2-mediated ocular inflammation. J Immunol 168(5):2483–2492 [DOI] [PubMed]
- 59.Mondino BJ, Rao H (1983) Hemolytic complement activity in aqueous humor. Arch Ophthalmol 101(3):465–468 [DOI] [PubMed]
- 60.Mondino BJ, Glovsky MM, Chekiere L (1984) Activated complement in inflamed aqueous humor. Invest Ophthalmol Vis Sci 25:871–873 [PubMed]
- 61.Mondino BJ, Sumner H (1986) Anaphylatoxin levels in human aqueous humor. Invest Ophthalmol Vis Sci 27:1288–1292 [PubMed]
- 62.Jha P, Sohn JH, Xu Q, Nishihori H, Wang Y, Nishihori S, Manickam B, Kaplan HJ, Bora PS, Bora NS (2006) Complement system plays a critical role in the development of experimental autoimmune anterior uveitis (EAAU). Invest Ophthalmol Vis Sci 47:1030–1038 [DOI] [PMC free article] [PubMed]
- 63.Jha P, Sohn JH, Xu Q, Wang Y, Kaplan HJ, Bora PS, Bora NS (2006) Suppression of complement regulatory proteins (CRPs) exacerbates experimental autoimmune anterior uveitis (EAAU). J Immunol 176(12):7221–7231 [DOI] [PubMed]
- 64.Bando Y, Tanouchi Y, Fukuyado K, Matsuda S, Mimura Y (1989) The dynamics of leucocytes and complements in endotoxin induced uveitis. Nippon Ganka Gakkai Zasshi 93(3):369–374 [PubMed]
- 65.Rosenbaum JT, Wong K, Perez HD, Raymond W, Howes EL Jr (1984) Characterization of endotoxin-induced C5-derived chemotactic activity in aqueous humor. Invest Ophthalmol Vis Sci 25(10):1184–1191 [PubMed]
- 66.Montalvo V, Chan CC, Gery I, Campos MM, Wawrousek EF, Bush RA, Lambris JD (2007) Complement deposits on ocular tissues adjacent to sites of inflammation. Curr Eye Res 32(11):917–922 [DOI] [PubMed]
- 67.Marak GE, Wacker WB, Rao NA, Jack R, Ward PA (1979) Effects of complement depletion on experimental allergic uveitis. Ophthalmic Res 11:97–107
- 68.Read RW, Szalai AJ, Vogt SD, McGwin G, Barnum SR (2006) Genetic deficiency of C3 as well as CNS-targeted expression of the complement inhibitor sCrry ameliorates experimental autoimmune uveoretinitis. Exp Eye Res 82(3):389–394 [DOI] [PubMed]
- 69.Ferris FL, Fine SL, Hyman L (1984) Age-related macular degeneration and blindness due to neovascular maculopathy. Arch Ophthalmol 102:1640–1642 [DOI] [PubMed]
- 70.Yates JR, Moore AT (2000) Genetic susceptibility to age-related macular degeneration. J Med Genet 37:83–87 [DOI] [PMC free article] [PubMed]
- 71.Husain D, Ambati B, Adamis AP, Miller JW (2002) Mechanisms of age-related macular degeneration. Ophthalmol Clin North Am 15:87–91 [DOI] [PubMed]
- 72.Nowak JZ (2006) Age-related macular degeneration (AMD): pathogenesis and therapy. Pharmacol Rep 58(3):353–363 [PubMed]
- 73.Johnson LV, Leitner WP, Staples MK, Anderson DH (2001) Complement activation and inflammatory processes in drusen formation and age related macular degeneration. Exp Eye Res 73:887–896 [DOI] [PubMed]
- 74.Mullins RF, Russell SR, Anderson DH, Hageman GS (2000) Drusen associated with aging and age-related macular degeneration contain proteins common to extracellular deposits associated with atherosclerosis, elastosis, amyloidosis, and dense deposit disease. FASEB J 14:835–846 [PubMed]
- 75.Johnson LV, Ozaki S, Staples MK, Erickson PA, Anderson DH (2000) A potential role for immune complex pathogenesis in drusen formation. Exp Eye Res 70:441–449 [DOI] [PubMed]
- 76.Hageman GS, Anderson DH, Johnson LV, Hancox LS, Taiber AJ, Hardisty LI, Hageman JL, Stockman HA, Borchardt JD, Gehrs KM, Smith RJ, Silvestri G, Russell SR, Klaver CC, Barbazetto I, Chang S, Yannuzzi LA, Barile GR, Merriam JC, Smith RT, Olsh AK, Bergeron J, Zernant J, Merriam JE, Gold B, Dean M, Allikmets R (2005) A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration. Proc Natl Acad Sci USA 102(20):7227–7232 [DOI] [PMC free article] [PubMed]
- 77.Klein RJ, Zeiss C, Chew EY, Tsai JY, Sackler RS, Haynes C, Henning AK, SanGiovanni JP, Mane SM, Mayne ST, Bracken MB, Ferris FL, Ott J, Barnstable C, Hoh J (2005) Complement factor H polymorphism in age-related macular degeneration. Science 308(5720):385–389 [DOI] [PMC free article] [PubMed]
- 78.Haines JL, Hauser MA, Schmidt S, Scott WK, Olson LM, Gallins P, Spencer KL, Kwan SY, Noureddine M, Gilbert JR et al (2005) Complement factor H variant increases the risk of age-related macular degeneration. Science 308:419–421 [DOI] [PubMed]
- 79.Edwards AO, Ritter R 3rd, Abel KJ, Manning A, Panhuysen C, Farrer LA (2005) Complement factor H polymorphism and age-related macular degeneration. Science 308:421–424 [DOI] [PubMed]
- 80.Laine M, Jarva H, Seitsonen S, Haapasalo K, Lehtinen MJ, Lindeman N, Anderson DH, Johnson PT, Järvelä I, Jokiranta TS, Hageman GS, Immonen I, Meri S (2007) Y402H polymorphism of complement factor H affects binding affinity to C-reactive protein. J Immunol 178(6):3831–3836 [DOI] [PMC free article] [PubMed]
- 81.Prosser BE, Johnson S, Roversi P, Herbert AP, Blaum BS, Tyrrell J, Jowitt TA, Clark SJ, Tarelli E, Uhrín D, Barlow PN, Sim RB, Day AJ, Lea SM (2007) Structural basis for complement factor H linked age-related macular degeneration. J Exp Med 204(10):2277–2283 [DOI] [PMC free article] [PubMed]
- 82.Mandal MN, Ayyagari R (2006) Complement factor H: spatial and temporal expression and localization in the eye. Invest Ophthalmol Vis Sci 47(9):4091–4097 [DOI] [PubMed]
- 83.Coffey PJ, Gias C, McDermott CJ, Lundh P, Pickering MC, Sethi C, Bird A, Fitzke FW, Maass A, Chen LL, Holder GE, Luthert PJ, Salt TE, Moss SE, Greenwood J (2007) Complement factor H deficiency in aged mice causes retinal abnormalities and visual dysfunction. Proc Natl Acad Sci USA 104(42):16651–16656 [DOI] [PMC free article] [PubMed]
- 84.Gold B, Merriam JE, Zernant J, Hancox LS, Taiber AJ, Gehrs K, Cramer K, Neel J, Bergeron J, Barile GR, Smith RT, Hageman GS, Dean M, Allikmets R (2006) Variation in factor B (BF) and complement component 2 (C2) genes is associated with age-related macular degeneration. Nat Genet 38:458–462 [DOI] [PMC free article] [PubMed]
- 85.Maller J, George S, Purcell S, Fagerness J, Altshuler D, Daly MJ, Seddon JM (2006) Common variation in three genes, including a noncoding variant in CFH, strongly influences risk of age-related macular degeneration. Nat Genet 38(9):1055–1059 [DOI] [PubMed]
- 86.Yates JR, Sepp T, Matharu BK, Khan JC, Thurlby DA, Shahid H, Clayton DG, Hayward C, Morgan J, Wright AF, Armbrecht AM, Dhillon B, Deary IJ, Redmond E, Bird AC, Moore AT, Genetic Factors in AMD Study Group (2007) Complement C3 variant and the risk of age-related macular degeneration. New Eng J Med 357:553–561 [DOI] [PubMed]
- 87.Bykov I, Junnikkala S, Pekna M, Lindros KO, Meri S (2007) Effect of chronic ethanol consumption on the expression of complement components and acute-phase proteins in liver. Clin Immunol 124(2):213–220 [DOI] [PubMed]
- 88.Bora PS, Kaliappan S, Xu Q, Kumar S, Wang Y, Kaplan HJ, Bora NS (2006) Alcohol linked to enhanced angiogenesis in rat model of choroidal neovascularization. FEBS J 273(7):1403–1404 [DOI] [PubMed]
- 89.Kew RR, Ghebrehiwet B, Janoff A (1985) Cigarette smoke can activate the alternative pathway of complement in vitro by modifying the third component of complement. J Clin Invest 75(3):1000–1007 [DOI] [PMC free article] [PubMed]
- 90.Ryan SJ (1982) Subretinal neovascularization. Natural history of an experimental model. Arch Ophthalmol 100:1804–1809 [DOI] [PubMed]
- 91.Miller H, Miller B, Ishibashi T, Ryan SJ (1990) Pathogenesis of laser-induced choroidal subretinal neovascularization. Invest Ophthalmol Vis Sci 31(5):899–908 [PubMed]
- 92.Kimura H, Sakamoto T, Hinton DR et al (1995) A new model of subretinal neovascularization in the rabbit. Invest Ophthalmol Vis Sci 36:2110–2119 [PubMed]
- 93.Bora PS, Sohn JH, Cruz JM, Jha P, Nishihori H, Wang Y, Kaliappan S, Kaplan HJ, Bora NS (2005) Role of complement and complement membrane attack complex in laser-induced choroidal neovascularization. J Immunol 174(1):491–497 [DOI] [PubMed]
- 94.Bora NS, Kaliappan S, Jha P, Xu Q, Sohn JH, Dhaulakhandi DB, Kaplan HJ, Bora PS (2006) Complement activation via alternative pathway is critical in the development of laser-induced choroidal neovascularization: role of factor B and factor H. J Immunol 177(3):1872–1878 [DOI] [PubMed]
- 95.Bora NS, Kaliappan S, Jha P, Xu Q, Sivasankar B, Harris CL, Morgan BP, Bora PS (2007) CD59, a complement regulatory protein, controls choroidal neovascularization in a mouse model of wet-type age-related macular degeneration. J Immunol 178(3):1783–1790 [DOI] [PubMed]
- 96.Bora PS, Kaliappan S, Lyzogubov VV, Tytarenko RG, Thotakura S, Viswanathan T, Bora NS (2007) Expression of adiponectin in choroidal tissue and inhibition of laser induced choroidal neovascularization by adiponectin. FEBS Lett 581(10):1977–1982 [DOI] [PubMed]
- 97.Nozaki M, Raisler BJ, Sakurai E, Sarma JV, Barnum SR, Lambris JD, Chen Y, Zhang K, Ambati BK, Baffi JZ, Ambati J (2006) Drusen complement components C3a and C5a promote choroidal neovascularization. Proc Natl Acad Sci USA 103(7):2328–2333 [DOI] [PMC free article] [PubMed]
- 98.Sivaprasad S, Adewoyin T, Bailey TA, Dandekar SS, Jenkins S, Webster AR, Chong NV (2007) Estimation of systemic complement C3 activity in age-related macular degeneration. Arch Ophthalmol 125:515–519 [DOI] [PubMed]
- 99.Liu M, Regillo CD (2004) A review of treatments for macular degeneration: a synopsis of currently approved treatments and ongoing clinical trials. Curr Opin Ophthalmol 15(3):221–226 [DOI] [PubMed]