Abstract
Continual exposure of malarial parasite populations to different drugs may have selected not only for resistance to individual drugs but also for genetic traits that favor initiation of resistance to novel unrelated antimalarials. To test this hypothesis, different Plasmodium falciparum clones having varying numbers of preexisting resistance mechanisms were treated with two new antimalarial agents: 5-fluoroorotate and atovaquone. All parasite populations were equally susceptible in small numbers. However, when large populations of these clones were challenged with either of the two compounds, significant variations in frequencies of resistance became apparent. On one extreme, clone D6 from West Africa, which was sensitive to all traditional antimalarial agents, failed to develop resistance under simple nonmutagenic conditions in vitro. In sharp contrast, the Indochina clone W2, which was known to be resistant to all traditional antimalarial drugs, independently acquired resistance to both new compounds as much as a 1,000 times more frequently than D6. Additional clones that were resistant to some (but not all) traditional antimalarial agents acquired resistance to atovaquone at high frequency, but not to 5-fluoroorotate. These findings were unexpected and surprising based on current views of the evolution of drug resistance in P. falciparum populations. Such new phenotypes, named accelerated resistance to multiple drugs (ARMD), raise important questions about the genetic and biochemical mechanisms related to the initiation of drug resistance in malarial parasites. Some potential mechanisms underlying ARMD phenotypes have public health implications that are ominous.
Malaria is a major cause of morbidity and mortality around the world. The disease is present in 102 countries and is responsible for about 300 million clinical cases and 1–2 million deaths each year (1). Chloroquine, which for decades served as a cheap and reliable drug, is becoming ineffective against Plasmodium falciparum in most tropical areas (2). Other species of malarial parasites, such as Plasmodium vivax, also exhibit chloroquine resistance (3). As a consequence, there is an urgent need to develop novel antimalarial agents that are effective against drug-resistant malarial parasites (1, 4–6). Drug development efforts generally aim for compounds that work through new, independent mechanisms of action and that are structurally unrelated to existing antimalarial agents. While these efforts have led to reagents that are equally toxic to drug-sensitive and drug-resistant parasites in the laboratory, many new drugs fail to cure malaria in the field in a consistent and reliable manner. Failure of new antimalarial agents is usually due to the rapid appearance of resistance (7–11).
Mechanisms responsible for the initiation of drug resistance in malarial parasites are not understood. Suboptimal levels of drugs, possibly arising from failures to comply with recommended dosing regimens, or from long half-lives of certain hydrophobic drugs that remain in circulation from earlier treatments, probably contribute to a stepwise development of resistance (4, 10). However, it is possible that additional factors may also be involved. Drug resistance is observed most frequently and repeatedly in Southeast Asia (7–11). In Thailand, recrudescence and drug failures occur unexpectedly even in carefully controlled clinical settings (12). Anecdotal stories from the field suggest that resistance to new drugs occurs more easily in Southeast Asia than in other parts of the world. Some clones from Indochina are resistant to every common antimalarial agent and frequently display more than one mechanism by which they acquire resistance to a given antimalarial drug (see below). A conventional explanation for the last observation is that heavy use of antimalarial drugs in Southeast Asia may have presented parasite populations in this part of the world with more opportunities to acquire different types of resistance traits. In addition, meiotic recombination probably permitted concentration of independently acquired resistant traits into single clones (13).
In the present study, an alternative explanation was considered for the rapid failure of new drugs against malaria and for the prevalence of many different resistance traits in single parasite clones. It was hypothesized that resistance to new antimalarial agents may arise at different frequencies in different clones of P. falciparum and that some parasites that developed drug resistance in the past may be predisposed to acquire resistance to new unrelated antimalarial agents. To test this hypothesis, two hurdles needed to be surmounted. First, antimalarial agents that were equally effective against drug-sensitive and drug-resistant parasites had to be identified to follow independent selectable traits in parasites with different resistance backgrounds. Second, a method for estimating frequencies of resistance in parasite populations that grow only in suspension had to be developed. After solving these technical problems, it was discovered that the ability of parasite clones to acquire drug-resistance can vary by 2–3 orders of magnitude. Furthermore, the prior drug-resistance history of the parasites was related to the ability of individual clones to acquire resistance to new drugs.
EXPERIMENTAL PROCEDURES
Materials.
Human red blood cells and plasma for culturing P. falciparum were obtained from the American Red Cross (Baltimore). Parasites were maintained in culture according to published methods (14, 15). 5-Fluoroorotate was purchased from PCR Inc. (Gainesville, FL), and atovaquone was kindly provided by Dennis Kyle (Walter Reed Institute of Army Research, Washington, DC).
Parasite Clones.
P. falciparum clones W2 and D6 were originally obtained from W. Milhous (Walter Reed Institute of Army Research, Washington, DC). Subsequently, clones of W2, D6, HB3, FCR, and 3D7 were obtained from T. Wellems (National Institutes of Health). The relevant history and drug-susceptibility patterns of five clones used in the present study are described in Table 1. Most of these parasites were isolated from the field in the 1970s and early 1980s. During these years, resistance to traditional antimalarial drugs was firmly established in Southeast Asia but not in Africa. The Indochina clone W2 is representative of the most highly resistant strains of P. falciparum. Clone W2 is resistant to chloroquine, quinine, pyrimethamine, cycloguanil, and sulfadoxine (16–20). In addition, W2 exhibits multiple mechanisms by which it develops resistance to pyrimethamine and sulfadoxine (19–21). Many of these resistance traits are genetically separable (21, 22). Conversely, clone D6, originally isolated from Sierra Leone, is susceptible to all common antimalarial agents (16, 17). The other parasite clones show resistance to some, but not all, antimalarial agents (17–19). Clone FCR3 is chloroquine- and cycloguanil-resistant, but sensitive to pyrimethamine and sulfadoxine. Clone HB3 from Honduras is resistant to pyrimethamine but not chloroquine or sulfadoxine. Clone 3D7 is resistant to sulfadoxine due to its ability to use exogenous folate, but it is sensitive to chloroquine, cycloguanil, or pyrimethamine. The resistance traits of all the clones were acquired naturally in the field and not under culture conditions in the laboratory.
Table 1.
Susceptibility patterns of some P. falciparum clones
| Compound | Clones and origin
|
||||
|---|---|---|---|---|---|
| W2 (Indochina) | FCR3 (“The Gambia”) | HB3 (Honduras) | 3D7 (“Netherlands”) | D6 (Sierra Leonne) | |
| Chloroquine | R | R | S | S | S |
| Quinine | R | — | — | — | S |
| Pyrimethamine | R | S | R | S | S |
| Cycloguanil | R | R | S | S | S |
| Sulfadoxine | R | S | S | R | S |
| 5-Fluoroorotate | S | S | S | S | S |
| Atovaquone | S | S | S | S | S |
Parasites were considered sensitive (S) to each of the above compounds if there IC50 was lower than 15 nM for chloroquine, 15 nM for quinine, 1 nM for pyrimethamine, and 100 nM for sulfadoxine (16–21). Parasites were considered resistant (R) to each of the above compounds if there IC50 was higher than 100 nM for chloroquine, 50 nM for quinine, 25 nM for pyrimethamine, and 10,000 nM for sulfadoxine (16–21). All five parasite clones had an IC50 of 2–3 nM for 5-fluoroorotate and 2 nM for atovaquone.
Frequency of Drug Resistance in P. falciparum.
Frequency of resistance of malarial parasites to a given drug concentration cannot be measured accurately because it is not possible to visualize parasites in culture as colonies or as plaques. However, such frequencies can be estimated by starting with different numbers of parasites and determining the minimum number of parasites that are required to develop resistant progeny (23, 24).
Typically, atovaquone-sensitive and 5-fluoroorotate-sensitive parasites in about 10 infected erythrocytes were allowed to proliferate to ≈109 infected erythrocytes. The freshly grown cultures were used to innoculate a series of 10 ml culture flasks. Six control flasks were set up with 10 infected erythrocytes per flask (C1, C2, C3 and NT1, NT2, NT3). In addition, between 105 to 108 infected erythrocytes were set up, in triplicate, in a series of 10 ml cultures (T1, T2, etc.). Flasks C1, C2, C3 and flasks in the T-series (T1, T2, etc.) were challenged with 5-fluoroorotate or atovaquone with every medium change. Flasks NT1, NT2, NT3 were not treated with 5-fluoroorotate or atovaquone. Parasites were cultured by standard methods in the presence of 2% hematocrit with medium changes three times per week. In addition, cultures were split 1:2 with fresh erythrocytes once a week. Slides were prepared from every flask with each medium change and stained with Giemsa to test for emergence of parasites.
The small parasite populations in control flasks C1, C2, and C3 consistantly succumbed to drug pressure for all strains examined indicating that stock solutions of 5-fluoroorotate or atovaquone had not deteriorated or precipitated during the 2-month-long resistance-selection experiments. In contrast, the small parasite populations in control flasks NT1, NT2, and NT3 consistantly generated large numbers of parasites. This confirmed that the red cells, the culture medium with serum, and the gas mixtures were all functioning well enough to allow clonal cells to consistantly grow into large populations. Emergence of resistant parasites from flasks in the T-series depended on the initial size of the parasite population at the onset of selection, the concentration of drug during selection, and the clone used (see below).
RESULTS AND DISCUSSION
Choice of Selectable Traits.
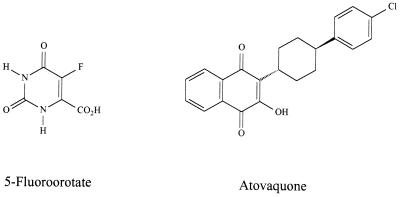
Resistance to 5-fluoroorotate and to atovaquone (Fig. 1) among different P. falciparum clones met the criteria for independent selectable traits. 5-Fluoroorotate is a potent antimalarial agent that is equally effective against all parasite isolates tested (refs. 16, 25, and 26; Table 1). It appears to act through mechanisms that are different from all antimalarial agents that are presently used in the field. Its toxicity arises through formation of 5-fluoropyrimidine nucleotides (15, 25, 27). Importantly, 5-fluoroorotate has never been used in the field, thus preselection for naturally occurring resistant mutants would not be anticipated. Nevertheless, because 5-fluoroorotate is transported through specific permeases and has to undergo at least five metabolic transformations to be converted to its toxic metabolite (15, 25, 27, 51), there are many potential sites to develop resistance. On this basis, it was expected that frequency of 5-fluoroorotate resistance might be measurable in small parasite populations in vitro (23). Atovaquone, a specific inhibitor of mitochondrial respiration in parasites, is a potent inhibitor of drug sensitive as well as drug resistant P. falciparum (refs. 28 and 29; Table 1). This antimalarial agent is structurally and mechanistically unrelated to 5-fluoroorotate (Fig. 1; refs. 15 and 25–29). Moreover, at the time the parasites employed in this study were isolated from the field, atovaquone had not been used for treatment. Because atovaquone has failed as a single antimalarial agent due to high rates of resistance (12), it was also expected that frequency of resistance might be high enough to be detected in small parasite populations in vitro (23).
Figure 1.
5-Fluoroorotate and atovaquone are structurally dissimilar. They have independent mechanisms of action, and do not experience cross-resistance in malarial parasites (23).
Clone-Specific Variation in Frequency of Drug Resistance.
When 108 infected erythrocytes from each of these five isolates were exposed continuously to 10−7 M 5-fluoroorotate over a period of 3 weeks, W2 populations generated mutant parasites resistant to 5-fluoroorotate (Table 2). In contrast, populations of FCR3, HB3, 3D7, and D6 failed to yield 5-fluoroorotate-resistant progeny even after 2 months of culture (Table 2). To quantitatively determine the difference in resistance acquisition among the clones, varying numbers of W2 were used at the start of the selection. As few as 106 erythrocytes infected with W2 were sufficient to give 5-fluoroorotate-resistant parasites (23). On this basis, it was estimated that W2 developed resistance to 10−7 M 5-fluoroorotate at least 100 times more frequently than FCR3, HB3, 3D7, or D6.
Table 2.
Frequency of resistance to 5-fluoroorotate
| Initial size of parasite population per flask | Outcome of selection*
|
||||
|---|---|---|---|---|---|
| W2 (Indochina) | FCR3 (“The Gambia”) | HB3 (Honduras) | 3D7 (“Netherlands”) | D6 (Sierra Leonne) | |
| 108 | 3 /3 | 0 /3 | 0 /3 | 0 /3 | 0 /3 |
| 107 | 3 /3 | 0 /3 | 0 /3 | 0 /3 | 0 /3 |
| 106 | 3 /3 | 0 /3 | 0 /3 | 0 /3 | 0 /3 |
| 105 | 0 /3 | 0 /3 | 0 /3 | 0 /3 | 0 /3 |
The ratios represent the number of flasks that yielded resistant parasites within 2 months of culture, divided by the initial number of flasks setup.
To establish that clone-specific differences in resistance frequencies were independent of the selectable marker, frequency of resistance to atovaquone was estimated for each of the clones. As shown in Table 3, only the W2 clones developed resistance to 10−8 M atovaquone when starting with 105 infected erythrocytes. In sharp contrast, populations derived from clones D6 and HB3 failed to develop resistance to 10−8 M atovaquone even when the experiments were initiated with 108 parasites per flask. Clones FCR3 and 3D7 developed resistance to atovaquone when the selection was initiated with a minimum of 106 infected erythrocytes, suggesting that these clones had an intermediate propensity to develop resistance to 10−8 M atovaquone.
Table 3.
Frequency of resistance to atovaquone
| Initial population per flask | Outcome of selection*
|
||||
|---|---|---|---|---|---|
| W2 (Indochina) | FCR3 (“The Gambia”) | HB3 (Honduras) | 3D7 (“Netherlands”) | D6 (Sierra Leonne) | |
| 108 | 3 /3 | 3 /3 | 0 /3 | 3 /3 | 0 /3 |
| 107 | 3 /3 | 3 /3 | 0 /3 | 3 /3 | 0 /3 |
| 106 | 3 /3 | 3 /3 | 0 /3 | 3 /3 | 0 /3 |
| 105 | 3 /3 | 0 /3 | 0 /3 | 0 /3 | 0 /3 |
| 104 | 0 /3 | 0 /3 | 0 /3 | 0 /3 | 0 /3 |
The ratios represent the number of flasks that yielded resistant parasites within 2 months of culture, divided by the initial number of flasks setup.
Overall, only clone W2 consistently displayed high frequency of resistance to the two different and unrelated inhibitors of parasite proliferation. The difference in frequency of resistance between W2 and D6 or HB3 was two to three orders of magnitude. These observations suggest that clone W2, which is resistant to all common antimalarial agents, carries genetic traits that greatly facilitate independent acquisition of resistance to two new and unrelated compounds, whereas D6, which has always been vulnerable to every antimalarial agent, lacks these traits. The present findings cannot be dismissed by simple conventional explanations. (i) Prior cross-resistance with traditional antimalarial drugs cannot be responsible for the development of W2 populations resistant to 5-fluoroorotate or to atovaquone. Based on traditional antiproliferation tests, all five isolates used in this study were equally susceptible to 5-fluoroorotate and to atovaquone (Table 1). Furthermore, small inocula of every clone failed to proliferate in the presence of either 10−7 M 5-fluoroorotate or 10−8 M atovaquone, but large populations of W2 freshly derived from 10 to 100 parasites permitted selection of mutants. (ii) Clone-specific differences in growth rates did not contribute to the variation in frequency of appearance of drug-resistant parasites, as it took approximately the same time for each clone to grow to a density of about 106 parasites per 10 ml culture in the absence of drug pressure, starting with 10 infected erythrocytes (Table 4). Furthermore, the newly emerged mutants proliferated under drug pressure as well as the parent clones in the absence of drug pressure (data not shown). (iii) The protocols used in the present experiments selected for resistant mutants did not reflect some type of dormancy (30). During the selection steps, drug pressure was maintained continuously over 2 months by introducing the antimalarial every 2 days with each medium change. Additionally, W2 parasites that emerged under 10−7 M 5-fluoroorotate or 10−8 M atovaquone exhibited IC50 values that were 100 times and 30 times higher, respectively, than the parent populations (23, 24). (iv) Mutants against the two new antimalarial agents arose through independent mechanisms. 5-Fluoroorotate-resistant mutants did not show cross-resistance to atovaquone and vice versa, and the frequency of resistance to a combination of 5-fluoroorotate and atovaquone approximated a multiple of the frequency of resistance to each compound alone (23).
Table 4.
Relative proliferation rates of P. falciparum clones
| Clone | Source | Growth rate,* days |
|---|---|---|
| W2 | Indochina | 19 |
| FCR3 | “The Gambia” | 24 |
| HB3 | Honduras | 25 |
| 3D7 | “Netherlands” | 22 |
| D6 | Sierra Leonne | 28 |
Proliferation rates are expressed as the number of days required for 10 infected erythrocytes to proliferate to about 106 cells in a flask under the culture conditions described in the text.
Implications on the Evolution of Malarial Drug Resistance.
The present findings change our view of the evolution of drug resistance in malarial parasites. The ability of certain P. falciparum clones to readily develop resistance to structurally and mechanistically unrelated compounds may represent a new and powerful strategy by infectious organisms to combat different chemotherapeutic agents. We call these phenotypes accelerated resistance to multiple drugs (ARMD). The well-studied multiple drug resistance phenotype in infectious organisms and in malignant cells is characterized by simultaneous inheritance of resistance to some amphipathic drugs and is attributable to overexpression or amplification of a single gene (31–35). In contrast, ARMD organisms may develop resistance to unrelated compounds through independent genetic alterations and, as a result, provide parasites with a selective advantage against a broader range of chemotherapeutic agents. At present, it is uncertain whether W2, the only clone that developed resistance to atovaquone and to 5-fluoroorotate, shows enhanced expression of a single mechanism shared by all ARMD parasites or whether W2 harbors more than one ARMD mechanism.
Potential Mechanisms Underlying ARMD Phenotypes.
One possibility is that clones such as W2 may have acquired a general mutator phenotype that provides a population of 108 cells in a culture flask with a 1,000-fold higher genetic diversity than equal number of non-ARMD parasites such as clone D6. Mutator phenotypes have been well studied in a variety of cell types, including bacteria, yeast, and mammalian cells (36–40). Any one of over a dozen molecular mechanisms can give rise to mutator phenotypes, including altered polymerases, altered DNA repair enzymes, and altered metabolic pools (36, 41, 42). Alternatively, instead of a general mutator mechanism, ARMD P. falciparum clones may use recombination-based strategies to cause more frequent loss of function mutations or to change gene expression (43). The possibility that ARMD parasites under drug pressure experience bursts of mutagenic activity that involve genetic rearrangements cannot be eliminated (44, 45). Finally, it is possible that neither an increase in mutation rate nor an increase in recombination rate are involved. The variations in frequency of resistance may simply be related to preexisting silent polymorphisms at the resistance loci. For instance, a population of ARMD parasites such as W2, which starts with a large arsenal of drug-resistance mechanisms, may modify an existing mechanism of resistance to generate phenotypically observable resistance to a new drug. The lower resistance frequencies in clones such as D6 and HB3 could be explained if these parasites must first acquire the basic mechanism of resistance and then adapt it to the drug being used in the selection process. It should be noted, however, that resistance to chloroquine or to pyrimethamine in itself is not sufficient to facilitate resistance to 5-fluoroorotate, because clones FCR3 and HB3 fail to develop resistance as easily as W2.
Earlier Observations That May Be Related to the Present Findings.
Some previous unexplained results on genetic variations among malarial parasites may be related to ARMD phenotypes. In mouse models of malaria, chloroquine resistance could be developed in some pyrimethamine-resistant Plasmodium chabaudi and in Plasmodium vinckei, but not from pyrimethamine-sensitive parasites (refs. 46 and 47; and V. E. Rosario and D. Walliker, personal communication). Similarly, Peters and Porter (48) noted that resistance to WR 122455 appeared more readily in chloroquine-resistant Plasmodium bergei than in chloroquine-sensitive lines.
The increased plasticity of some P. falciparum genomes may offer selective advantages that extend beyond drug-resistance. Some clones of malarial parasites, such as Dd2 (derived from W2-mef), “switch and adapt” to erythrocytes stripped of sialic acid, but other clones such as FCR-3/A2 do not (49, 50). If the observed variations in frequencies of resistance to antimalarial compounds are due to increased mutations or increased genetic rearrangements in some clones, it will be of interest to determine whether parasite populations will differ in their sensitivities to immunological treatments.
Conclusions.
P. falciparum clones can display very large differences in frequency of resistance to two unrelated antimalarial agents. There is an intriguing correlation between the drug-resistance history of the clones examined and the propensity of the clones to acquire resistance to 5-fluoroorotate or to atovaquone. To fully understand the role of ARMD phenotypes in the global spread of drug-resistant malarial parasites, it will be necessary to determine the mechanisms underlying ARMD phenotypes and to determine whether ARMD phenotypes themselves have spread to other parts of the world along with the individual traits conferring resistance to antimalarial agents such as chloroquine, mefloquine, and Fansidar.
Acknowledgments
We thank W. Milhous and D. Kyle (Walter Reed Army Institute of Research) and T. Wellems (National Institutes of Health) for parasite clones and for helpful discussions. We are also grateful to J. Boothroyd, B. T. DeCicco, J. Golin, V. Rao, D. P. Rathod, S. D. Tuljapurkar, B. Ullman, and A. Vaidya for encouragement and helpful comments. This work was supported by Public Health Service Grants from the National Institutes of Health (AI 26912 and AI 01112). PKR is a recipient of a Burroughs Wellcome Fund New Initiatives in Malaria Research Award.
ABBREVIATION
- ARMD
accelerated resistance to multiple drugs
References
- 1.Oaks S C Jr, Mitchell V S, Pearson G W, Pearson C C J, editors. Malaria: Obstacles and Opportunities. Washington, DC: National Academy Press; 1991. [PubMed] [Google Scholar]
- 2.White N J. N Engl J Med. 1996;335:800–806. doi: 10.1056/NEJM199609123351107. [DOI] [PubMed] [Google Scholar]
- 3.Rieckmann K H, Davis D R, Hutton D C. Lancet. 1989;ii:1183–1184. doi: 10.1016/s0140-6736(89)91792-3. [DOI] [PubMed] [Google Scholar]
- 4.White N J. J Antimicrob Chemother. 1992;30:571–585. doi: 10.1093/jac/30.5.571. [DOI] [PubMed] [Google Scholar]
- 5.Shuster B G, Milhous W K. Parasitol Today. 1993;9:167–168. doi: 10.1016/0169-4758(93)90139-7. [DOI] [PubMed] [Google Scholar]
- 6.White N J, Olliaro P L. Parasitol Today. 1996;12:399–401. doi: 10.1016/0169-4758(96)10055-7. [DOI] [PubMed] [Google Scholar]
- 7.Looareesuwan S, Harinasuta T, Chongsuphasiddhi T. Southeast Asian J Trop Med Public Health. 1992;23:621–634. [PubMed] [Google Scholar]
- 8.Palmer K J, Holliday S M, Brogden R N. Drugs. 1993;45:430–475. doi: 10.2165/00003495-199345030-00009. [DOI] [PubMed] [Google Scholar]
- 9.Bryson H M, Goa K L. Drugs. 1992;45:236–258. doi: 10.2165/00003495-199243020-00009. [DOI] [PubMed] [Google Scholar]
- 10.Peters W. Phamacol Ther. 1990;47:499–508. doi: 10.1016/0163-7258(90)90067-c. [DOI] [PubMed] [Google Scholar]
- 11.Peters W. Handb Exp Pharmacol. 1984;68:423–445. [Google Scholar]
- 12.Looareesuwan S, Viravan C, Webster H K, Kyle D E, Hutchinson D B, Canfield C J. Am J Trop Med Hyg. 1996;54:62–66. doi: 10.4269/ajtmh.1996.54.62. [DOI] [PubMed] [Google Scholar]
- 13.Walliker D, Quakyi I A, Wellems T E, McCutchan T F, Szanfman A, London W T, Corcoran L M, Burkot T R, Carter R. Science. 1987;236:1661–1666. doi: 10.1126/science.3299700. [DOI] [PubMed] [Google Scholar]
- 14.Trager W, Jensen J B. Science. 1976;193:673–675. doi: 10.1126/science.781840. [DOI] [PubMed] [Google Scholar]
- 15.Rathod P K, Leffers N P, Young R D. Antimicrob Agents Chemother. 1992;36:704–711. doi: 10.1128/aac.36.4.704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rathod P K, Khatri A, Hubbert T, Milhous W K. Antimicrob Agents Chemother. 1989;33:1090–1094. doi: 10.1128/aac.33.7.1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oduola A M J, Milhous W K, Weatherly N F, Bowdre J H, Desjardins R E. Exp Parasitol. 1988;67:354–360. doi: 10.1016/0014-4894(88)90082-3. [DOI] [PubMed] [Google Scholar]
- 18.Foote S J, Galatis D, Cowman A F. Proc Natl Acad Sci USA. 1990;87:3014–3017. doi: 10.1073/pnas.87.8.3014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peterson D S, Milhous W K, Wellems T E. Proc Natl Acad Sci USA. 1990;87:3018–3022. doi: 10.1073/pnas.87.8.3018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Milhous W K, Weatherly N F, Bowdre J H, Desjardins R E. Antimicrob Agents Chemother. 1985;27:525–530. doi: 10.1128/aac.27.4.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang P, Read M, Sims P F G, Hyde J E. Mol Microbiol. 1997;23:979–986. doi: 10.1046/j.1365-2958.1997.2821646.x. [DOI] [PubMed] [Google Scholar]
- 22.Wellems T E. Parasitol Today. 1991;7:110–112. doi: 10.1016/0169-4758(91)90168-n. [DOI] [PubMed] [Google Scholar]
- 23.Gassis S, Rathod P K. Antimicrob Agents Chemother. 1996;40:914–919. doi: 10.1128/aac.40.4.914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rathod P K, Khosla M, Gassis S, Young R D, Lutz C. Antimicrob Agents Chemother. 1994;38:2871–2876. doi: 10.1128/aac.38.12.2871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rathod, P. K. (1997) J. Pharm. Pharmacol. 49 (Suppl. 2), 65–69.
- 26.Gomez Z, Rathod P K. Antimicrob Agents Chemother. 1990;34:1371–1375. doi: 10.1128/aac.34.7.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hekmat-Nejad M, Rathod P K. Antimicrob Agents Chemother. 1996;40:1628–1632. doi: 10.1128/aac.40.7.1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hudson A T. Parasitol Today. 1993;9:66–68. doi: 10.1016/0169-4758(93)90040-m. [DOI] [PubMed] [Google Scholar]
- 29.Shrivastava I, Rottenberg H, Vaidya A B. J Biol Chem. 1997;272:3961–3966. doi: 10.1074/jbc.272.7.3961. [DOI] [PubMed] [Google Scholar]
- 30.Nakazawa S, Kanbara H, Aikawa M. Exp Parasitol. 1995;81:556–563. doi: 10.1006/expr.1995.1149. [DOI] [PubMed] [Google Scholar]
- 31.Gottesman M M, Pastan I. Annu Rev Biochem. 1993;62:385–427. doi: 10.1146/annurev.bi.62.070193.002125. [DOI] [PubMed] [Google Scholar]
- 32.Cowman A F. Aust N Z J Med. 1995;25:837–844. doi: 10.1111/j.1445-5994.1995.tb02889.x. [DOI] [PubMed] [Google Scholar]
- 33.Ullman B. J Bioenerg Biomembr. 1995;27:77–84. doi: 10.1007/BF02110334. [DOI] [PubMed] [Google Scholar]
- 34.Wilson C M, Serrano A E, Walsey A, Bogenschutz M P, Shankar A H, Wirth D F. Science. 1989;244:1184–1186. doi: 10.1126/science.2658061. [DOI] [PubMed] [Google Scholar]
- 35.Wellems T E, Panton L J, Gluzman I Y, do Rozario V E, Gwandz R W, Walker-Jonah A, Krogstad D J. Nature (London) 1990;345:253–255. doi: 10.1038/345253a0. [DOI] [PubMed] [Google Scholar]
- 36.Miller J H. Annu Rev Biochem. 1996;50:625–643. doi: 10.1146/annurev.micro.50.1.625. [DOI] [PubMed] [Google Scholar]
- 37.Kunz B A, Henson E S, Roche H, Ramotar D, Nunoshiba T, Demple B. Curr Genet. 1995;27:102–109. [Google Scholar]
- 38.Prakash S, Sung P, Prakash L. Annu Rev Genet. 1993;27:33–70. doi: 10.1146/annurev.ge.27.120193.000341. [DOI] [PubMed] [Google Scholar]
- 39.Modrich P. Science. 1994;266:1959–1960. doi: 10.1126/science.7801122. [DOI] [PubMed] [Google Scholar]
- 40.Umar A, Kunkel T A. Eur J Biochem. 1996;238:297–307. doi: 10.1111/j.1432-1033.1996.0297z.x. [DOI] [PubMed] [Google Scholar]
- 41.Kornberg A, Baker T. DNA Replication. New York: Freeman; 1991. [Google Scholar]
- 42.Weinberg G, Ullman B, Martin D W., Jr Proc Natl Acad Sci USA. 1981;78:2447–2451. doi: 10.1073/pnas.78.4.2447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hernandez-Rivas R, Hinterberg K, Scherf A. Mol Biochem Parasitol. 1996;78:137–148. doi: 10.1016/s0166-6851(96)02618-7. [DOI] [PubMed] [Google Scholar]
- 44.McClintock B. Science. 1984;226:792–801. doi: 10.1126/science.15739260. [DOI] [PubMed] [Google Scholar]
- 45.Federoff N, Botstein D, editors. The Dynamic Genome: Barbara McClintock’s Ideas in the Century of Genetics. Plainview, NY: Cold Spring Harbor Lab. Press; 1992. [Google Scholar]
- 46.Rosario V E. Nature (London) 1976;261:585–586. doi: 10.1038/261585a0. [DOI] [PubMed] [Google Scholar]
- 47.Powers K G, Jacobs R L, Good W C, Koontz L C. Exp Parasitol. 1969;26:193–202. doi: 10.1016/0014-4894(69)90112-x. [DOI] [PubMed] [Google Scholar]
- 48.Peters W, Porter M. Ann Trop Med Parasitol. 1976;70:271–281. doi: 10.1080/00034983.1976.11687123. [DOI] [PubMed] [Google Scholar]
- 49.Dolan S A, Miller L H, Wellems T E. J Clin Invest. 1990;86:618–624. doi: 10.1172/JCI114753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Soubes S C, Wellems T E, Miller L H. Exp Parasitol. 1997;86:79–83. doi: 10.1006/expr.1997.4153. [DOI] [PubMed] [Google Scholar]
- 51.Lauer S A, Rathod P K, Ghori N, Haldar K. Science. 1997;276:1122–1125. doi: 10.1126/science.276.5315.1122. [DOI] [PubMed] [Google Scholar]