Abstract
Low socioeconomic status (SES) has been linked to HIV and sexually transmitted disease (STD) at a macro level because the majority of new cases of HIV infection in the world have been reported in underdeveloped or developing countries. However, empirical data on the relationship between individual SES and HIV/STD related risk have been mixed. Employing quantitative data from 454 female sex workers, this study was designed to examine the profile of the study sample in terms of their individual SES, HIV/STD-related sexual risk across work locations with different social, cultural and economic conditions; and examine the relationship between work location and HIV-related risk behaviors, controlling for individual SES. We have shown in the current study that both SES and HIV/STD-related risk behaviors significantly differed by work location. However, the difference in individual SES was not sufficient to explain the difference of HIV/STD-related risk across the work locations. The findings underscore the need for effective prevention intervention efforts targeting female sex workers in rural area. Based on the findings, we also suggest that HIV/STD intervention efforts among female sex workers should take the social and cultural contextual factors of their working environment (and sexual risks) into consideration.
Keywords: HIV/STD, socioeconomic status (SES), sexual risk, female sex workers, China
Poverty or low socioeconomic status (SES) has been linked to HIV and sexually transmitted disease (STD) at a macro level because 90% of all new cases of HIV infection in the world have been reported in underdeveloped or developing countries (UNAIDS, 2004). However, empirical data on the relationship between individual SES and HIV/STD related risk have been mixed (Mosley, 2004; Wojcicki, 2005). Furthermore, little is known about whether low SES is directly associated with HIV/STD-related sexual risk among female sex workers (FSWs), a population at risk for HIV infection and transmission, in nations or regions where both HIV infection and commercial sex are emerging, such as China.
The current study was designed to explore the relationship between individual SES and HIV/STD-related risk among Chinese FSWs who provided sex service through entertainment establishments (e.g., restaurants, hotels, and hair-salons). These entertainment establishments were distributed in three geographic locations with different levels of economic development and different socio-cultural characteristics in a multi-ethnic county in China. The three locations of FSWs’ work place were employed in the current study as a proxy for local economic condition. The rural township (which is the informal trade center of local villages) represents a less economically developed rural setting; the county seat is the political, economic, and cultural center of the county and represents an urban setting; and the newly established development zone (e.g., areas officially designed to receive special, favorable governmental economic incentives for the purposes of attracting private investment and promoting trade) is in the “urban-rural” conjunction. The main research question is whether variation of HIV/STD-related risk among FSWs can be explained by individual SES. Specifically, our aims are to (1) examine the profile of the study sample in terms of their individual SES, HIV/STD-related sexual risk across work locations; and (2) examine whether the variation of sexual risk behaviors by work location can be explained by FSWs’ individual SES and other key demographic characteristics (e.g., age, length of sex work, current income, ethnicity, migratory status).
Background Information
HIV and Sex Work in China
While the actual HIV sero-prevalence in China remains uncertain, the current official estimate of numbers of persons infected with HIV exceeds 650,000. (China Ministry of Health, 2006). Most of the reported cases (64.7%) were among individuals 20 to 39 years of age, with a male predominance. Although injection drug use and commercial blood/plasma collection have been the major sources of infection, sexual transmission increased from 5.5% in1997 to 43.6% in 2005 (China Ministry of Health, 2006). Among the new infections in 2005, 49.8% were attributed to sexual transmission, surpassing for the first time the infections through IV drug use (48.6%) (China Ministry of Health, 2006). The resurgence of wide-scale commercial sex since the 1980’s has now accelerated to a nationwide phenomenon. Commercial sex has long been considered to be reservoir for transmission of sexual diseases (Asthana & Oostvogels, 1995; Davis, 1993; Ford & Koetsawang, 1991; Karim, Karim, Soldan, & Zondi, 1995). Despite recognition of the important role of female sex workers (FSWs) in China’s HIV and STD epidemics, we know little about their individual characteristics or the social and environmental context of their work, which have been shown to be closely related to HIV/STD risk behaviors for women (Logan, Cole, & Leukefeld, 2002; Yang et al., 2005a).
In the early 1950s the Chinese government declared that prostitution in mainland China had been eradicated (Gil, Wang, Anderson, Lin, & Wu, 1996). However, over the last decades, prostitution has emerged as a “flourishing industry”, as a consequence of more individual and economic freedom, increased disposable income and liberalization of sexual attitudes (Gil et al., 1996; Hershatter, 1996; Liao, Schensul, & Wolffers, 2003). The number of women engaging in commercial sex in mainland China has been estimated to be from 4 to 10 million (Yang et al., 2005c). Existing data revealed some characteristics of this population: most FSWs are young, in their teens or 20s, with only a primary or junior high school education. Most of them were migrants from rural areas. They are highly mobile, have high rates of STD (China CDC, 2004), and are often engaged in health risk behaviors including drug use, demonstrate low use of condoms, possess poor knowledge of HIV/STD prevention and perceive low HIV risk (Lau, et al., 2002; Liao et al., 2003; Qu et al., 2002; Rogers et al., 2002; Yang et al., 2005a).
Since the 1980s, informal or clandestine sex trade in the service or entertainment industry has spread from municipalities to small towns in remote areas (Hershatter, 1996; Pan, 1999; Huang, Henderson, Pan, & Cohen, 2004). In past studies on FSWs in China (Huang et al., 2004) as well as studies in Southeast Asia (Ford, Wirawan, & Fajan, 1995; Wirawan, Fajans, & Ford, 1995), the authors indicate that FSWs’ individual characteristics, HIV risk behaviors, and health risk behaviors may vary by geographic location of their work sites. Furthermore, studies on commercial sex in China have been conducted mainly in large cities or tourist attractions such as Guangzhou (provincial capital and largest city in South China) (van den Hoek et al., 2001), Shenzhen (the first Special Economic Zone in China, bordering Hong Kong) (Lau, Tsui, Siah, & Zhang, 2002), Hainan (the largest Special Economic Zone in China, an island in the South of Guangdong and Guangxi Provinces) (Liao, Schensul, & Wolffers, 2003), Beijing (capital city of China) (Rogers, Ying, Xin, Fung, & Kaufman, 2002), and Baise (a major trade center in Guangxi and southwest China) (Qu et al., 2002). In the existing literature, authors suggest an insufficient understanding of FSWs in more remote Chinese counties and smaller metropolitan or rural areas (as opposed to large cities or tourist attractions), especially these women’s individual and family SES, sexual risk behaviors, and these individual characteristics in relation to their work environment (Yang et al., 2005b).
Besides the geographic variation of their workplaces, the Chinese FSWs are also heterogeneous in several other aspects. First, these women enter the sex trade through different pathways or with different reasons. A small proportion of women (particularly young or underage girls) are deceived or forced into the trade against their will (Gil et al., 1996). A recent survey among a sample of 382 FSWs in Shenzhen reveled that about 15% of these young women (average age of 24 years) enter the profession against their free will (Shenzhen Academy of Social Science, 2004). A large proportion is driven into the business as a result of poverty and limited employment opportunities. Some women (in both rural and urban areas) choose the sex trade as a means to support their families. Some unskilled, low-educated female rural-to-urban migrants come to urban centers looking for better lives but find limited opportunity for legitimate employment or employment that would provide them with living conditions above subsistence. Attracted by a relatively high income, some women enter the sex trade as a route to rapid financial returns.
Second, there is a vast difference in their working conditions or working environment. Although some FSWs are street-based or freelance, the majority encounter their clients in entertainment establishments (e.g., karaoke, night club, dancing hall, disco, bar) or personal service sectors (e.g., hair washing rooms, hair salons, massage parlor, sauna, restaurant, hotel) (Huang et al., 2004). These establishment-based sex workers are called “Xiaojie” in Chinese (literally translating as “miss” in English) (Hong et al., 2006; Huang et al., 2004). Such establishments differ substantially in terms of the context of working and living (Huang et al., 2004; Yang et al., 2005b). However, little is known about whether the profiles of FSWs (e.g., SES, HIV-related risk behaviors) differ by working environment.
Methods
Study Site
In the current study, we utilized cross-sectional data drawn from the baseline assessment of a longitudinal HIV/STD intervention project in 2004–2005 (Li et al., 2006). The intervention project was conducted in H County, a suburban county of Nanning, the capital city of Guangxi Zhuang Autonomous Region (“Guangxi”). Guangxi, one of China’s five autonomous and multi-ethnic regions, is located in the southern part of the country. It is bordered by Guangdong Province on the east, the Gulf of Tonkin on the south and Vietnam on the southwest. Because of its central location in southwest China, Guangxi has historically been a transport hub for trade, commerce, and tourism in southwest China and South East Asia. Guangxi has a population of 46.8 million, among which 72% are rural residents. The average annual per capita was 6,666 RMB (approximately $800 US) for urban dwellers and 2,321 RMB (approximately $280 US) for rural residents in 2001 (Guangxi Bureau of Statistics, 2004).
Guangxi has witnessed an alarming rise in HIV prevalence in the past decade. A total of 11,979 HIV infected cases have been officially reported as of the end of 2004 (Guangxi CDC, 2005). Guangxi ranks third among Chinese provinces in terms of reported seropositive cases. Similar to the national epidemic, the majority of infected cases are from rural areas. The prosperous economy, international contact, and tourism in Guangxi have created a demand and market for commercial sex. According to the statistics from the public security agency, there were at least 50,000 FSWs in Guangxi, although the actual number was believed to be substantially higher (Liu et al., 2001). FSWs in Guangxi mostly provide sexual service through hotels, restaurants, nightclubs, karaoke bars, dancing halls, and other entertainment establishments (e.g., barbershop, hair-washing room, saunas, and massage parlors) (Liu et al., 2001).
Located in Nanning suburban area, H County has jurisdiction over 22 townships with a total population of 1.1 million (94.5% are rural residents). Similar to other areas of China, residents in H county are roughly divided in “urban” (county seat) and “rural” (villagers or rural centers). The population in H county consists of 23 ethnic groups with the majority of residents being Han (60%) and Zhuang (37%). Zhuang is one of the 55 ethnic minorities in China. Concentrated in the southwest China, the Zhuang ethnic group has its own dialect, but members can also speak the country’s official language, Mandarin Chinese. It was estimated that there are about 200 entertainment establishments with more then 2,000 women offering sexual service in the county. The majority of these women were working in restaurants, barbershops, hair-washing rooms, and massage parlors.
Sampling and Participants
Participants in the current study were recruited from restaurants, barbershops, hair-washing rooms, and massage parlors from three geographic locations in H County: the county seat, a recently established development zone in rural-urban conjunction, and one rural township. The county seat has an area of 15 square kilometers with a population of 100,000. The development zone, about 10 kilometers from the county seat, is an area of approximately 5 square kilometers in size. The zone was established in the late 1990s and has more than 100 small factories and businesses in the area. The development zone and surrounding areas have a population of 90,000. The rural township is 35 kilometers from the county seat and has a population of 35,000. The workplace (mainly restaurants, hair salons, hair-washing rooms, and massage parlors) was employed as the sampling units. We employed ethnographic targeted sampling to identify and recruit participants (Carlson, Wang, Siegel, Falck, & Guo, 1994). First, the research team and local health workers conducted an ethnographic-mapping of the establishments which provide sexual service. The ethnographic-mapping identified these establishments with information from local health care providers (e.g., STD clinicians, obstetricians or gynecologists), taxi drivers, public security agencies, and local business owners and residents. The mapping team collected data on the name and address of the establishment, estimated number of sex workers, operation history, and contact information of the owner/manager. A total of 85 establishments were identified in the three targeted areas (53 in county seat, 12 in the development zone, and 20 in the township) with an estimated more than 800 FSWs in these establishments.
Upon the completion of the ethnographic-mapping, the owners/managers of these establishments were contacted for their permission to conduct study on their premises. Among the 85 establishments identified, 57 (67%) agreed to participate in the study. Once we received the permission from the owner/manager, local outreach workers (mainly comprised of health workers from the county anti-epidemic station and local hospitals) approached the women in the establishments who were identified by the owner/manager as FSWs. Once the FSW status was confirmed by the women themselves, the outreach workers explained the purpose, procedure, potential benefits and potential risks of the study to these women and invited them to participate. Those women who expressed interest in the study were asked to provide written informed consent and were assured of confidentiality and privacy. Each woman who provided appropriate informed consent was assigned a unique personal code number. A total of 581 women were approached in the 57 workplaces and 454 (78%) agreed to participate. The final sample of 454 women was recruited from 34 restaurant-type establishments (n=380), 23 hair salons, hair-washing rooms or massage parlors (n=74) in three geographic locations (243 or 54% from the county seat, 131 or 29% from the development zone, and 80 or 18% from the rural township).
Survey Procedure
Study participants were given a self-administered questionnaire entitled “Health Survey for Women in the Service Sectors”. The questionnaire contains four main components: Demographic information, living and working conditions, health behaviors including sexual experience and history of sex work, and HIV/AIDS-related knowledge and attitudes. The questionnaire takes about 45–60 minutes to complete. The questionnaire was pilot-tested in two waves among 22 women (7 in wave one and 15 in wave two) to make sure that the content and language were appropriate for the study population. The participants completed the questionnaire in a separate room or a private space and recorded their unique personal code number on the questionnaire. No one (e.g., coworker, employer, or client) was allowed to stay with the participant during the survey except a trained interviewer who was available to provide the participant with assistance if needed. For participants (about 10%) with limited literacy, the interviewer read each question and response options to the participants from the interviewer’s copy of the questionnaire, while the participants marked the response in their own copy (so that the interviewer would not see their answers).
Most of the outreach workers and interviewers were health care workers from the county anti-epidemic station and local hospitals. They were carefully chosen and rigorously trained (and re-trained) on survey procedures and confidential issues and were asked to sign a pledge to protect the respondent’s privacy and confidentiality. The study protocol was approved by the Institutional Review Board at Wayne State University in the United States and Beijing Normal University and Guangxi Zhuang Autonomous Region Center for Disease Control and Prevention in China.
Measures
Individual and family characteristics and SES
Participants were asked to provide information regarding their demographic characteristics which included age, years of formal schooling; ethnicity (Han, Zhuang, and other); home residence (non-Guangxi versus Guangxi), type of hometown (rural village, small town/county seat, small/medium city, major city); marital status (single without a boyfriend or fiancé, single with a boyfriend or fiancé, married, divorced); whether the participant had a child; reasons for being a sex worker; experience with law enforcement (e.g., was arrested, was fined, was sent to a women reeducation center); and average monthly income in H county (in Chinese currency Yuan). For the purpose of data analysis in the current study, an SES composite score was created by indexing FSWs with no more than 6 years of formal schooling, being ethnic minority, growing up in rural villages, getting into sex trade by either family financial hardship or inability to find other legitimate work. One point was assigned to each of these five criteria. The composite score was appropriately reversed so that a higher score indicates a higher level of SES. The final SES score ranged from 0 to 5 with a mean of 2.15 and standard deviation (SD) of 1.24.
HIV/STD-related sexual risk
The data regarding FSWs’ sexual risk behaviors included age of sexual onset, length of time being a sex worker, partner of first sexual intercourse (e.g., client, boyfriend, husband, friends or other acquaintance). The participants were asked about the average number of clients per week; maximum number of clients per day; number of stable sexual partners (including long-term clients), and whether they had been raped or forced to have sex in last 6 months, had had a “sugar-daddy” (i.e., a rich man) in last 6 months; or had exchanged sex for drugs, sex with clients under the influence of alcohol, or sex with clients during menstruation. Participants were also asked about their sex acts with clients including group sex, oral sex, and anal sex; how often they used a condom with their clients and stable partners, and personal history of STDs. In addition, information was collected on substance use in the previous 6 months including alcohol intoxication, and illegal drug and injection drug use.
A sexual risk composite score was created by indexing those migrants who had their sexual debut before age 18, had their first sex with a client, had sex with their clients under the influence of alcohol, had sex with their clients during menstruation, had group sex or anal sex with their clients, had never used a condom with either their clients or their stable partners, had both commercial partners and non-commercial partners concurrently, had a history of STD infection, had been intoxicated at least once with alcohol during previous 6 months, had been raped during the previous 6 months, had used illicit drugs including injection drugs, had exchanged sex for drugs, had illicit drug-using clients or clients with STD infection. For the purpose of data analysis in the current study, one point was assigned to each of the 16 risk behaviors. The actual sexual risk composite score ranged from 0 to 9 with a mean of 3.68 and an SD of 1.94. A higher score indicates a higher level of HIV/STD related risk.
Statistical Analysis
First, Chi-square (for categorical variables) and ANOVA (for continuous variables) were employed to assess the group differences in individual SES and HIV/STD-related risk by work location. Second, two general linear model (GLM) analyses were conducted to assess whether the SES and sexual risk behaviors differ by the work location. In the first GLM model, the SES composite score was employed as the dependent variable and the work location as the main between-subjects factor. Home residence (non-Guangxi versus Guangxi) was employed as an additional between-subjects factor. Age, length of sex work, and current monthly income were employed as covariates in the GLM model. The second GLM model with the sexual risk composite score as the dependent variable followed the same design except that ethnicity (Han, Zhuang, and other) was employed as an additional between-subjects factor and SES was employed as an additional covariate in the second model. The ethnicity was not included in the first GLM model because the ethnicity was already included in the formation of the dependent variable (i.e., SES composite score). All statistical analyses were performed using SPSS V11.5 for Windows.
Results
Demographic Characteristics
As shown in Table 1, the participants were significantly different by working location in a number of demographic characteristics. The sample had a mean age of 23.50 years (SD=5.09) with about 70% younger than 25 years of age and an average of 5.69 years of formal schooling (SD=3.30). Compared to women working in county seat or development zone, women in the township were younger and less educated. Overall, the average monthly income was 576 Yuan (70 US dollars), with 696 Yuan (85 US dollars) for women in the county seat, 419 (50 US dollars) in the development zone, and 468 (55 US dollars) in the township (p<.0001). Although the history of pregnancy was similar across the work locations, more women in the county seat (55%) than those in development zone (48%) or township (36%) had had abortions (p<.05).
Table 1.
Demographic Characteristics of 454 Female Sex Workers in a Chinese County
| Overall | County Seat | Development Zone | Township | |
|---|---|---|---|---|
| N (%) | 454 (100%) | 243 (54%) | 131 (29%) | 80 (18%) |
| Mean age±SD | 23.50±5.09 | 23.36±4.69 | 24.08±5.62 | 22.99±5.34 |
| Mean yrs of schooling±SD | 5.69±3.30 | 6.12±3.33 | 5.81±2.97 | 4.19±3.34**** |
| Mean income±SD (100 Yuan) | 5.76±5.23 | 6.96±6.45 | 4.19±2.39 | 4.68±3.23**** |
| Ethnicity (p=.006) | ||||
| Han | 55 | 54 | 66 | 39 |
| Zhuang | 32 | 34 | 26 | 37 |
| Other | 14 | 13 | 9 | 24 |
| Guangxi Residence | 66 | 74 | 50 | 68**** |
| Type of hometown (p=.007) | ||||
| Rural | 80 | 74 | 80 | 95 |
| County Seat | 13 | 16 | 13 | 5 |
| Small/Medium City | 4 | 5 | 5 | 0 |
| Major City | 3 | 4 | 2 | 0 |
| Marital status (p=.001) | ||||
| Single with boyfriend | 36 | 35 | 32 | 43 |
| Single, no boyfriend | 24 | 31 | 18 | 14 |
| Married | 35 | 26 | 47 | 43 |
| Divorce | 5 | 7 | 3 | 1 |
| Reasons for being sex worker | ||||
| Quick/easy money | 5 | 5 | 5 | 5 |
| Easy/pleasant job | 6 | 3 | 11 | 9** |
| No better job | 41 | 32 | 52 | 50**** |
| Influenced by others | 15 | 9 | 19 | 26**** |
| Marriage failure | 8 | 9 | 10 | 3 |
| Revenge on men | 2 | 2 | 4 | 1 |
| Deceived/forced | 5 | 7 | 5 | 0 |
| Family financial difficulty | 65 | 67 | 57 | 74* |
| Other | 3 | 3 | 2 | 4 |
| At least one pregnancy | 63 | 60 | 64 | 54 |
| At least one abortion | 50 | 55 | 48 | 36* |
Note: Numbers presented in the tables are percentages unless noticed otherwise.
p<.05,
p<.01,
p<.001,
p<.0001
Family financial hardship was endorsed by two-thirds of the women as a major reason for their involvement in commercial sex. It was selected by more women in the township (74%) than in the county seat (67%) and development zone (57%) (p<.05). The other leading reasons women selected included inability to find a better job (41%) and influence from their friends or fellow villagers (15%). More women in the development zone and township than in the county seat selected the inability to find a better job (p<.001). Likewise, more women in the township than women in the development zone or county seat said that they were influenced by their friends or fellow villagers (p<.001). Five percent (n=24) of the study participants (17 in the county seat and 7 in the development zone) reported being deceived or forced into commercial sex.
Not shown in the table, a small proportion of women had experienced an encounter with police or other law enforcement agencies because of their involvement in commercial sex. Four percent (n=19) had been arrested, 3% (n=12) had been fined, and less than 1% (n=3) had been sent to a women’s reeducation center. While the numbers are not sufficient to examine the difference across work locations, all three women who had been sent to the women’s reeducation centers were working at the county seat.
HIV/STD-related Sexual Risk
The age of sexual onset ranged from 13 to 27 years (with mean of 18.62 years) with the majority (85%) having had sex on or before 20 years of age. Overall, the sample had a history of being a sex worker for just over one year (Table 2). Women in the township reported a shorter history of sex work than their counterparts in other locations (p<.001).
Table 2.
HIV/STD-related Risk Behaviors among 454 Chinese Female Sex Workers
| Overall | County Seat | Development Zone | Township | |
|---|---|---|---|---|
| N (%) | 454 (100%) | 243 (54%) | 131 (29%) | 80 (18%) |
| Age of sexual onset | 18.62±2.11 | 18.73±2.20 | 18.47±2.09 | 18.54±1.87 |
| Time being a sex worker (months) | 12.18±12.16 | 12.39±11.78 | 14.35±14.30 | 8.06±7.94*** |
| Partner of first sex (p=.005) | ||||
| Clients | 16 | 15 | 17 | 16 |
| Boyfriend | 45 | 54 | 35 | 35 |
| Husband | 32 | 24 | 40 | 41 |
| Friend | 5 | 5 | 5 | 6 |
| Other | 2 | 1 | 3 | 3 |
| Average # of clients per week | 2.00±1.75 | 2.40±2.18 | 1.41±.78 | 1.65±.73**** |
| Maximum clients per day | 1.25±.60 | 1.34±.72 | 1.08±.27 | 1.20±.54**** |
| # of stable partners | 1.29±.58 | 1.31±.59 | 1.30±.64 | 1.16±.42 |
| Had a sugar-daddy in last 6 months | 8 | 11 | 3 | 5* |
| Being raped in last 6 months | 15 | 20 | 13 | 5** |
| Illegal drug use last 6 months | 2 | 1 | 5 | 1 |
| Injection drug use last 6 months | 1 | 1 | 2 | 0 |
| Exchanged sex for drug | <.5 | 1 | 0 | 0 |
| Sex with alcohol | 29 | 29 | 32 | 26 |
| Sex with clients during menstruation | 7 | 8 | 6 | 5 |
| Sex acts | ||||
| Group sex | 4 | 7 | 2 | 0 |
| Oral Sex | 2 | 3 | 2 | 1 |
| Anal sex | 2 | 3 | 2 | 0 |
| Never used a condom with clients | 19 | 8 | 32 | 31**** |
| Never used a condom with stable partners | 42 | 37 | 53 | 40 |
| Ever had a STD | 19 | 23 | 20 | 9* |
Note: Numbers presented in the tables are percentages unless noticed otherwise.
p<.05,
p<.01,
p<.001,
p<.0001
Sixteen percent of the sample reported that they had their first sexual intercourse with their clients and an additional 7% with friends or other acquaintance. Although the overall pattern of their first sexual partner differed by locations, the proportion of women having their first sex with a client was similar across work locations.
The women reported an average of two clients per week (range .25 to 14 clients), with 2.40 clients among women in county seat, 1.41 in the development zone, and 1.65 in the township. About one half of the women had one client per week and about one-fifth had three or more clients per week. Women in the county seat reported a higher number of clients per day (1.34) than those in the development zone (1.08) or township (1.20).
Two-thirds of the participants reported having stable partners (husband, fiancé, boyfriend, lover or long-term client). The average number of stable partners was similar across work locations. About 8% of the participants reported that they had a sexual relationship with a “sugar-daddy” (a rich man) in the previous six months, with more women in the county seat than women in the development zone or the township (p<.05). About 15% of the sample reported being raped or forced to have sex during the previous 6 months, with more women in county seat than those in development zone or township reporting such an experience (p<.01). Two percent of the women used illicit drugs and 1% injected drugs during the previous 6 months. Two women in the county seat reported exchanging sex for drugs. About 29% of the women had had sex with clients under the influence of alcohol and the percentage was similar across the work locations.
The overall condom use was low among this group, with only 15% and 8% of them always using a condom with their clients and stable partners, respectively. Nineteen percent and 42% of the participants never used a condom with their clients and partners. The rate of never using a condom with clients was significantly different among work location (p<.001) with the rates being substantially higher among FSWs in the development zone (32%) and rural township (31%) than those in the county seat (8%). About one-fifth of the sample reported a history of STDs, which was higher among women in the county seat and the development zone than in rural township.
Multivariate Analysis
As shown in Table 3, GLM analysis for SES revealed that SES differed significantly by work location (p<.001), after controlling for key demographic characteristics. As depicted in Figure 1, SES level declined significantly in the order of county seat (2.30), development zone (2.28), and rural township (1.86). Likewise, SES differed by home residence (p<.001) with Guangxi FSWs having a lower SES than non-Guangxi FSWs (1.86 versus 2.71). SES was also significantly associated with the current monthly income (r=.22, p<.001) with FSWs from higher SES background making more money in H County.
Table 3.
GLM Tests of Between-Subjects Effects for SES
| Source | Type III Sum of Squares | Df | Mean Square | F | Sig. |
|---|---|---|---|---|---|
| Corrected Model | 163.409(a) | 8 | 20.426 | 16.894 | .000 |
| Intercept | 174.983 | 1 | 174.983 | 144.728 | .000 |
| Age | 4.487 | 1 | 4.487 | 3.712 | .055 |
| Current income | 34.958 | 1 | 34.958 | 28.914 | .000 |
| Length of sex work | 3.793 | 1 | 3.793 | 3.138 | .077 |
| Location | 25.284 | 2 | 12.642 | 10.456 | .000 |
| Residence | 51.035 | 1 | 51.035 | 42.211 | .000 |
| Location * Residence | 3.122 | 2 | 1.561 | 1.291 | .276 |
| Error | 525.933 | 435 | 1.209 | ||
| Total | 4322.000 | 444 | |||
| Corrected Total | 689.342 | 443 |
R Squared = .237 (Adjusted R Squared = .223)
Figure 1. Mean score of SES and HIV/STD-related risk by workplace, home residence, and ethnicity.
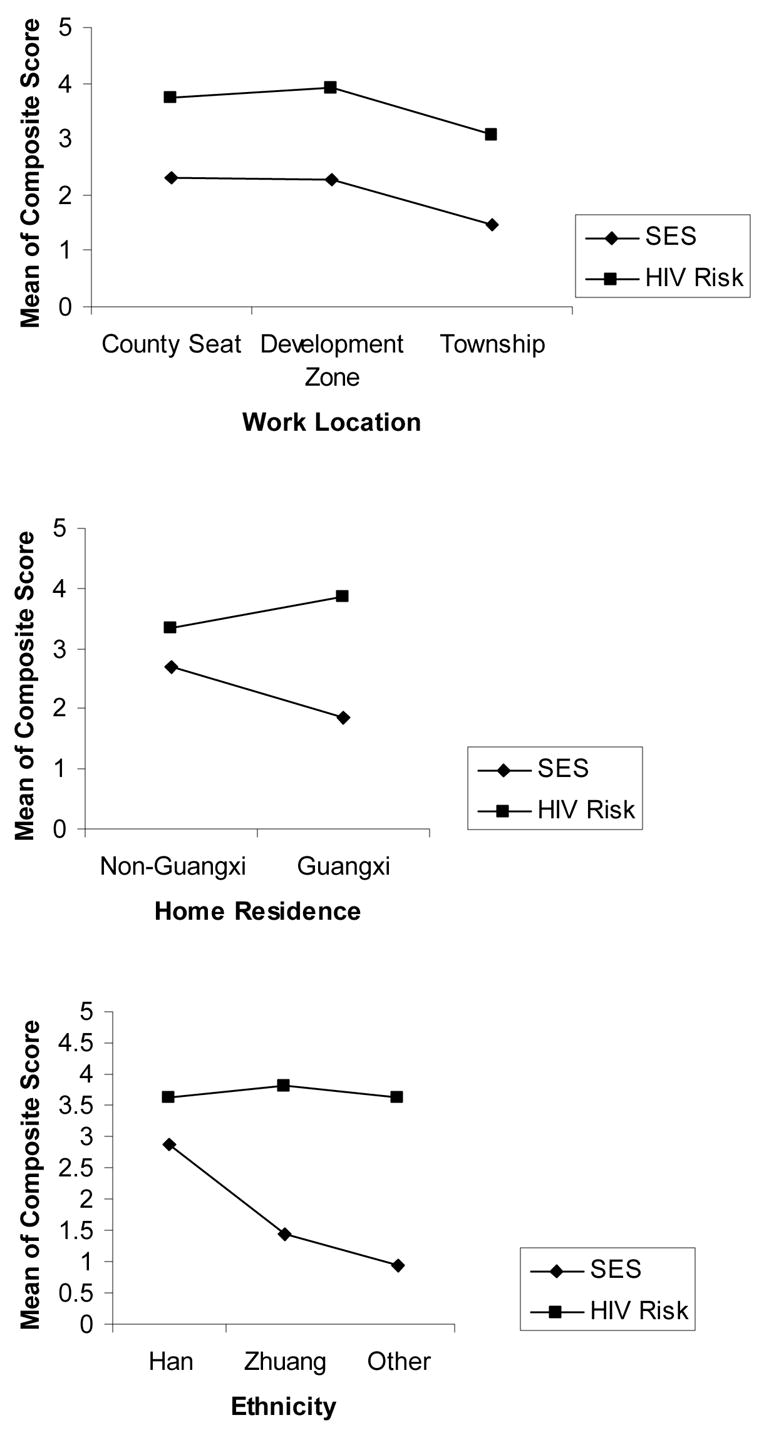
Note: SES was statistically different by work location (p=.000), home residence (p=.000), and ethnicity (p=.000); HIV/STD-related risk was statistically different by work location (p=.007) and home residence (p=.011).
Similarly, GLM analysis with HIV/STD related risk controlling for key demographic characteristics including SES (Table 4) shown that work location is significantly associated with sexual risk, with FSWs in the county seat and development engaging in a higher level of risk than those in the rural township (Figure 1). The GLM analysis revealed a significant main effect of ethnicity (p=.05) and significant two-way interaction between location, home residence, and ethnicity. In addition, the sexual risk was significantly associated with younger age (r=−.23, p<.001), longer duration of sex work (r=.21, p<.001), and higher income (r=.13, p<.05). However, SES was not a significant covariate in the model.
Table 4.
GLM Tests of Between-Subjects Effects for HIV/STD-related risk
| Source | Type III Sum of Squares | DF | Mean Square | F | Sig. |
|---|---|---|---|---|---|
| Corrected Model | 300.705(a) | 19 | 15.827 | 5.163 | .000 |
| Intercept | 254.504 | 1 | 254.504 | 83.031 | .000 |
| SES | .001 | 1 | .001 | .000 | .983 |
| Age | 85.564 | 1 | 85.564 | 27.915 | .000 |
| Current income | 12.582 | 1 | 12.582 | 4.105 | .043 |
| Length of sex work | 82.298 | 1 | 82.298 | 26.849 | .000 |
| Location | 34.348 | 2 | 17.174 | 5.603 | .004 |
| Residence | 1.472 | 1 | 1.472 | .480 | .489 |
| Ethnicity | 18.455 | 2 | 9.227 | 3.010 | .050 |
| Location*Residence | 32.372 | 2 | 16.186 | 5.281 | .005 |
| Location*Ethnicity | 29.483 | 4 | 7.371 | 2.405 | .049 |
| Residence*Ethnicity | 26.816 | 2 | 13.408 | 4.374 | .013 |
| Location*Residence*Ethnicity | 8.223 | 2 | 4.111 | 1.341 | .263 |
| Error | 1278.169 | 417 | 3.065 | ||
| Total | 7364.000 | 437 | |||
| Corrected Total | 1578.874 | 436 |
R2 = .190 (Adjusted R2 = .154)
Through further inspection of cell means, we found that the significant two-way interactions are results of the uneven level of sexual risk by either home residence or ethnicity across various work locations (Figure 2).
Figure 2. Mean score of HIV/STD related risk by interactions between workplace, home residence, and ethnicity.
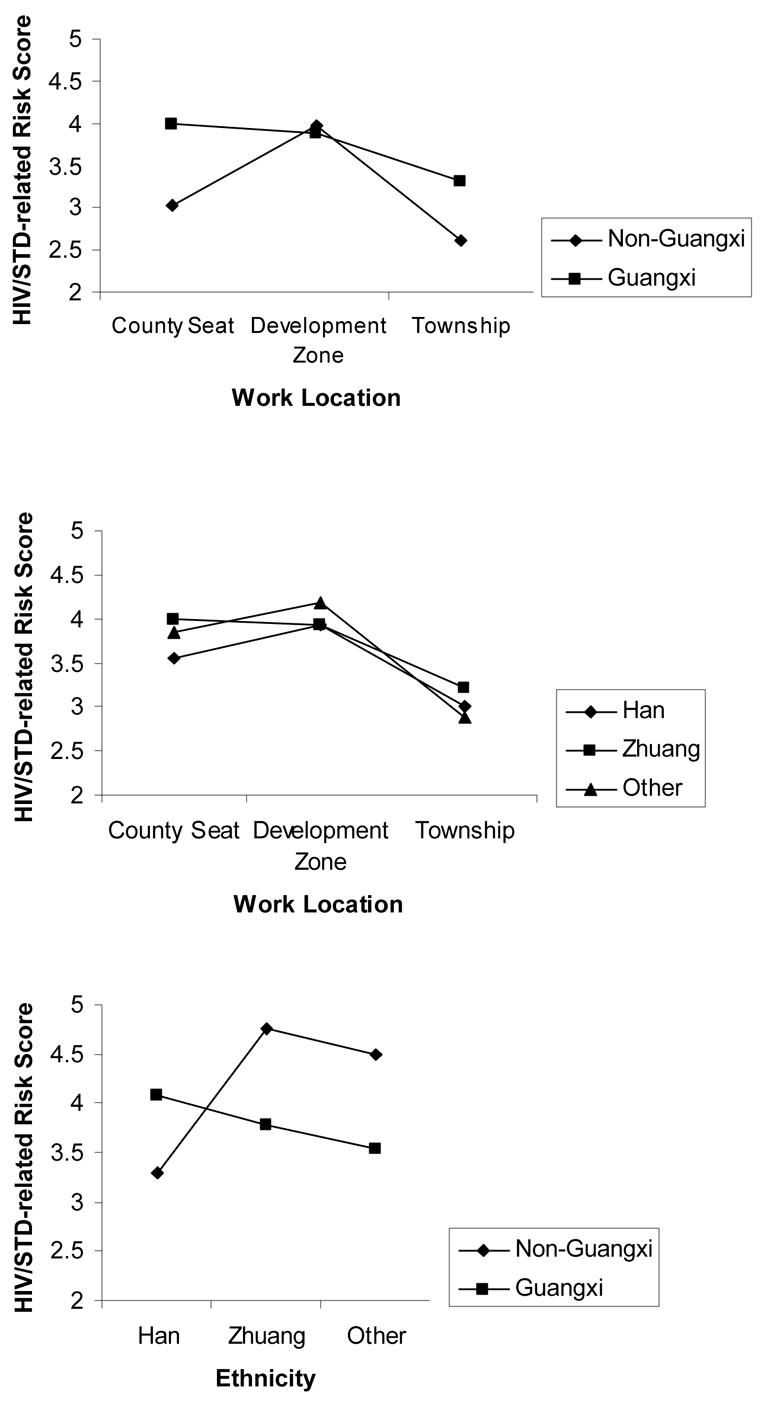
Note: All three interactions (i.e., work location by home residence; work location by ethnicity; and home residence by ethnicity) were statistically significant (p=.005, .049, and .013, respectively).
Discussion
In the current study, we provided data on individual SES and HIV/STD-related sexual risks among women providing sexual services in a multi-ethnic area in China. The SES and HIV/STD risks were examined for differences by work location, a proxy of local economic condition. In the current study, we found that both SES and HIV/STD-related risk behaviors were significantly different by work location. However, the difference in SES was not sufficient to explain the difference of HIV/STD-related risk across the work locations, which highlights the importance of other social and cultural factors in contributing to the HIV/STD related risk.
The sample in the current study is different in a number of key demographic characteristics from FSWs in studies conducted in other parts of China. First, the women in the current study were less educated, with more than 50% of women finishing no more than 6 years of formal schooling (or elementary school), compared to 13% in Beijing (Rogers et al., 2002) and 32% in Shenzhen (Lau et al., 2002). However, there were a number of similarities between findings in the current study and previous studies. First, most of the women were driven into the business of commercial sex by poverty or limited employment opportunities. The majority of the women perceived that they had no or little choice in their lives to do something else. Second, they were subject to sexual harassment and related violence as 15% reported having been raped or forced to have sex during the last 6 months.
Third, despite their young age, short personal history of sex work, and relatively low number of clients, the sample in the current study faces a significant risk of HIV/STD infection and transmission. The self-reported history of STD infection was similar to those in more economically advantaged regions such as Shenzhen (15%, Lau et al., 2002). The proportion of women who never used a condom with their clients during previous month was similar to those reported in other studies (Yang et al., 2005c). Similarly, condom use with stable partners was also low among this population. In addition, most of FSWs in the current study had concurrent multiple sexual partners in a mixture of commercial and non-commercial partners.
A very small proportion of FSWs in the current study had experience with law enforcement (e.g., being arrested, fined, or incarcerated). One of the reasons for such a low incidence might be the relative short personal history of sex work among the study population. Another possibility is that the actual number of arrests and incarceration are indeed small, despite the governmental intention to eliminate commercial sex. Nevertheless, this low number confirms the importance of community-based research among this population.
Researchers in both China and international communities have been concerned with “bridging effect” of FSWs in a rapid spread of HIV from a high risk population (e.g., IDU) to general population in China (Yang et al., 2005c). One aspect of the “bridging” is the mixture of commercial sex and illicit drug use among FSWs. However, rates of illicit drug use, particularly rate of IDU was low among this population. Although drug use was locally prevalent in Guangxi (Hammett et al., 2003), very few women reported exchanging sex for drugs. One of the reasons for this low rate of drug use among FSWs may be because they were relatively new to sex work. In addition, a small number of women in the current study reported having anal sex. This finding is consistent with previous studies in which the rate of anal sex among Chinese FSWs was about 1% (van den Hoek et al., 2001; Qu et al., 2002). The low rates of illicit drug use (including IDU) and other risk sexual behavior (e.g., anal sex) among FSWs present a window of opportunity for early prevention efforts among this population.
Whereas in one qualitative study in China, Huang and colleagues (2004) suggested that protected sex might be more prevalent among FSWs working in more economically developed areas, in the current study there was no relationship between low SES and HIV/STD related risk, after controlling for other key demographic characteristics, among the study sample. The finding indicates that factors other than individual SES may be associated with HIV/STD related risk. For example, researchers have suggested a significant role of gatekeepers (e.g., owners and managers of entertainment establishments) in condom use among FSWs (Yang et al., 2005d). The data in the current study support the notion that disadvantaged family and individual SES background might have been a strong force to drive these women into sex trade and that women from poorer families might have to work in (or start from) a less economically-developed area (e.g., rural township).
There are limitations in the current study. First, the sample was recruited through convenience sampling rather than random sampling. Because commercial sex is technically illegal in China, a random sampling is not feasible. Therefore, caution is needed in generalizing the findings from this study to other FSW populations. However, the fact that our sample is comparable to other Guangxi-based studies (Qu et al., 2002) in a number of key demographic characteristics (e.g., age, ethnicity, education, residence) provided evidence of the representativeness of our sample. Second, the current sample is multi-ethnic. Although the proportion of ethnic minorities in the current sample mirrored the ethnical composition of the Guangxi population, the sample limited the generalizability of the finding to other regions where other ethnic groups (e.g., Han) predominate the population. Third, some important information (e.g., family income, parental education) was not collected due to space/time limitation of the survey instrument.
Despite these methodological limitations, the findings in the current study have some important public health implications. First, there is an urgent need for effective prevention intervention programs targeting this new, but rapid growing FSW population, particularly in remote, rural areas. Given the low level of education, low income, and young age of this population, empowerment and alternative employment/education opportunities should be part of the intervention efforts. Second, the associations between the local socioeconomic conditions and HIV risk behaviors among FSWs imply that HIV/STD intervention efforts among FSWs must take the social and cultural contextual factors of their working environment (and sexual risks) into consideration. Recent researchers addressing women, sex and HIV suggest that most existing HIV/STD behavioral prevention intervention efforts do not sufficiently consider the range of important contextual and social factors that influence women’s sexual behaviors (Logan et al., 2002). Intervention efforts may be more effective if efforts at multiple levels (e.g., individual, family, community, environmental, and structural) can be implemented synergistically across multiple contexts of risk factors (Pequegnat & Stover, 2000).
Acknowledgments
This study is supported by a grant from the NIH Office of AIDS Research (R01MH064878-3S1). The authors want to thank other research team members from the China CDC Center for AIDS/STD Control (Hui Liu), China CDC Resources Center for STD Prevention and Treatment (Guojun Liang, Ping Yang, Xiaohong Su), Guangxi Zhouang Automous Region CDC (Wei Lu, Dongmei Huang, Weijian Lu, Qinghua Chen, Linzhen Guo), Heng County Anti-Epidemic Station (Canjian Lu, Feng Chen, Qinghua Lei, Zutiab Lu, Zilong Meng, Jiancheng Zhou, Yan Nong, Biwei Wei, Li Ma, Huang Ling), Beijing Normal University (Danhua Lin and Linyuan Zeng), Wayne State University Pediatric Prevention Research Center (Jiantong Guo, Hongjie Liu, Xinguang Chen). The authors also want to thank Joanne Zwemer for assistance in preparing the manuscript.
References
- Asthana S, Oostvogels R. Community Participation in HIV Prevention: Problems and Prospects for Community-Based Strategies among FSWs in Madras. Social Science and Medicine. 1995;43 (2):133–148. doi: 10.1016/0277-9536(95)00348-7. [DOI] [PubMed] [Google Scholar]
- Carlson RB, Wang J, Siegal HA, Falck RS, Guo J. An Ethnographic Approach to Targeted Sampling: Problems and Solutions in AIDS Prevention Research among Injection Drug and Crack-Cocaine Users 1994. Human Organization. 1994;53(3):279–286. [Google Scholar]
- China CDC National Center for AIDS/STD Control and Prevention. 2003 HIV/STD Epidemic in China. Beijing, China: China CDC; 2004. [Google Scholar]
- China Ministry of Health, UNAIDS, WHO. 2005 Update on the HIV/AIDS Epidemic and Response in China. Beijing: UNAIDS China Office; 2006. [Google Scholar]
- Davis N. Prostitution: An International Handbook on Trends, Problems, and Policies. London: Greenwood Press; 1993. [Google Scholar]
- Ford N, Koetsawang S. The Socioculturel Context of the Transmission of HIV in Thailand. Social Sciences and Medicine. 1991;33:405–414. doi: 10.1016/0277-9536(91)90321-3. [DOI] [PubMed] [Google Scholar]
- Ford K, Wirawan DN, Fajan P. AIDS knowledge, risk behaviors, and condom use among four groups of FSWs in Bali, Indonesia. Journal of AIDS and Human Retrovirology. 1995;10:569–576. [PubMed] [Google Scholar]
- Gil VE, Wang MS, Anderson AF, Lin CM, Wu ZO. Prostitutes, prostitution and STD/HIV transmission in mainland China. Social Science Medicine. 1996;42:141–152. doi: 10.1016/0277-9536(95)00064-x. [DOI] [PubMed] [Google Scholar]
- Guangxi Bureau of Statistics. Guangxi Social and Economic Development Statistics. 2004 Available at www.gxi.gov.cn/gxzw/dzjg.
- Guangxi CDC China National Center for HIV/STDS Control and Prevention. 2004 National HIV/AIDS Sentinel Surveillance Statistics. Beijing, China: National Center for HIV/STDS Control and Prevention; 2005. Guangxi HIV/AIDS Sentinel Surveillance Report in 2004; pp. 236–239. [Google Scholar]
- Hammett TM, Des Jarlais DC, Liu W, Ngu D, Tung ND, Hoang TV, et al. Development and implementation of a cross-border HIV prevention intervention for injection drug users in Ning Ming County (Guangxi Province), China and Lang Son Province, Vietnam. International Journal of Drug Policy. 2003;14:389–398. [Google Scholar]
- Hershatter G. Sex in modern China. In: Hershatter G, Honig E, Lipman J, editors. Remapping China-Fissures in Historical Terrain. 77: 96; California: Stanford University Press; 1996. [Google Scholar]
- Hong Y, Stanton B, Li X, Yang H, Lin D, Fang X, et al. Rural-to-urban migrants and the HIV epidemic in China: A qualitative study. AIDS and Behavior. 2006;19:1–10. doi: 10.1007/s10461-005-9039-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y, Henderson GE, Pan S, Cohen MS. HIV/AISD risk among brothel-based female sex workers in China: Assessing the terms, content, and knowledge of sex work. Sexually Transmitted Diseases. 2004;31(11):695–700. doi: 10.1097/01.olq.0000143107.06988.ea. [DOI] [PubMed] [Google Scholar]
- Karim QA, Karim SS, Soldan K, Zondi M. Reducing the Risk of HIV Infection among South African Sex Workers: Socio-Economic and Gender Barriers. American Journal of Public Health. 1995;85(11):1521–1525. doi: 10.2105/ajph.85.11.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau JT, Tsui HY, Siah PC, Zhang KL. A study on female sex workers in southern China (Shenzhen): HIV-related knowledge, condom use and STD history. AIDS Care. 2002;14:219–33. doi: 10.1080/09540120220104721. [DOI] [PubMed] [Google Scholar]
- Li X, Wang B, Fang X, Zhou R, Stanton B, Hong Y, et al. Short term effect of a cultural adaptation of voluntary counseling and testing among female sex workers in China: A quasi-experimental trial. AIDS Education and Prevention. 2006;18(5):406–419. doi: 10.1521/aeap.2006.18.5.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao S, Schensul J, Wolffers I. Sex-related health risks and implications for interventions with hospitality women in Hainan, China. AIDS Education & Prevention. 2003;15:109–21. doi: 10.1521/aeap.15.3.109.23834. [DOI] [PubMed] [Google Scholar]
- Liu W, Chen J, Dai Q, Qin Z, Liang S, Li Y, et al. Assessing population mobility and HIV vulnerability, Guangxi, People’s Republic of China. Bangkok, Thailand: The United Nations Development Programme South Easy Asia HIV and Development Project; 2001. [Google Scholar]
- Logan TK, Cole J, Leukefeld C. Women, sex and HIV: Social and contextual factors, meta-analysis of published intervention, and implications for practice and research. Psychology Bulletin. 2002;128(6):851–885. doi: 10.1037/0033-2909.128.6.851. [DOI] [PubMed] [Google Scholar]
- Mosley A. Does HIV or poverty cause AIDS? Biomedical and epidemiological perspectives. Theoretical Medicine and Bioethics. 2004;25(5–6):399–421. doi: 10.1007/s11017-004-2076-7. [DOI] [PubMed] [Google Scholar]
- Pan SM. Reality and absurdity-underground sex industry in China. Beijing: Qun Yan Publishing House; 1999. [Google Scholar]
- Pequegnat W, Stover E. Behavioral prevention is today’s AIDS vaccine! AIDS. 2000;14(Suppl 2):S1–7. [PubMed] [Google Scholar]
- Qu S, Liu W, Choi KH, Li R, Jiang D, Zhou Y, et al. The Potential for Rapid Sexual Transmission of HIV in China: Sexually Transmitted Diseases and Condom Failure Highly Prevalent Among Female Sex Workers. AIDS & Behavior. 2002;6(3):267–275. [Google Scholar]
- Rogers SJ, Ying L, Xin YT, Fung K, Kaufman J. Reaching and identifying the STD/HIV risk of sex workers in Beijing. AIDS Education & Prevention. 2002;14:217–27. doi: 10.1521/aeap.14.3.217.23892. [DOI] [PubMed] [Google Scholar]
- Shenzhen Academy of Social Science. Shenzhen 2004 Blue Book: Shenzhen 2004 Development Report. Shenzhen, China: Shenzhen Academy of Social Science; 2004. [Google Scholar]
- UNAIDS. 2004 Report On The Global HIV/AIDS Epidemic: 4th Global Report. Geneva, Switzerland: UNAIDS; 2004. [Google Scholar]
- van den Hoek A, Yuliang F, Dukers NH, Zhiheng C, Jiangting F, Lina Z, et al. High prevalence of syphilis and other sexually transmitted diseases among sex workers in China: potential for fast spread of HIV. AIDS. 2001;15:753–9. doi: 10.1097/00002030-200104130-00011. [DOI] [PubMed] [Google Scholar]
- Wirawan DN, Fajans P, Ford K. AIDS and STDs: risk behavior patterns among sex workers in Bali, Indonesia. AIDS Care. 1995;5(3):291–305. doi: 10.1080/09540129308258612. [DOI] [PubMed] [Google Scholar]
- Wojcicki JM. Socioeconomic status as a risk factor for HIV infection in women in east, central and southern Africa: A systematic review. Journal of Biosocial Science. 2005;37:1–36. doi: 10.1017/s0021932004006534. [DOI] [PubMed] [Google Scholar]
- Yang H, Li X, Stanton B, Fang X, Lin D, Mao R, et al. HIV-related risk factors associated with commercial sex among female migrants in China. Health Care for Women International. 2005a;26:134–148. doi: 10.1080/07399330590905585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H, Li X, Stanton B, Fang X, Lin D, Mao R, et al. Workplace and HIV/STD risk behavior and perceptions among female migrant workers in China. AIDS Care. 2005b;17(7):819–833. doi: 10.1080/09540120500099902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H, Li X, Stanton B, Liu H, Fang X, Lin D, et al. Heterosexual transmission of HIV in China: A systematic review of behavioral studies in last two decades. Sexually Transmitted Diseases. 2005c;32(5):270–280. doi: 10.1097/01.olq.0000162360.11910.5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H, Li X, Stanton B, Fang X, Zhao R, Dong B, et al. Condom-use among female sex workers in China: role of gatekeepers. Sexually Transmitted Diseases. 2005d;32(9):572–580. doi: 10.1097/01.olq.0000175418.48665.95. [DOI] [PMC free article] [PubMed] [Google Scholar]


