Abstract
Objective
To examine the association between computerization of physician orders and prescribing medication errors.
Data Sources
Studies published in English language were identified through MEDLINE (1990 through December 2005), Cochrane Central Register of Controlled Trials, and bibliographies of retrieved articles. Of 252 identified in the search, 12 (4.8 percent) original investigations that compared rates of prescribing medication errors with handwritten and computerized physician orders were included.
Data Collection
Information on study design, participant characteristics, clinical settings, and outcomes rates were abstracted independently by two investigators using a standardized protocol.
Principal Findings
Compared with handwritten orders, 80 percent of studies (8/10 studies) reported a significant reduction in total prescribing errors, 43 percent in dosing errors (3/7 studies), and 37.5 percent in adverse drug events (3/8 studies). The use of computerized orders was associated with a 66 percent reduction in total prescribing errors in adults (odds ratio [OR]=0.34; 95 percent confidence interval [CI] 0.22–0.52) and a positive tendency in children (p for interaction=.028). The benefit of computerized orders was larger when the rate of errors was more than 12 percent with handwritten orders (p for interaction=.022). Significant heterogeneity in the results compromised pooled relative risks. One randomized controlled intervention demonstrated the greatest benefits of computerized orders on total prescribing errors (OR=0.02, 95 percent CI 0.01–0.02) and dosing errors (OR=0.28; 95 percent CI 0.15–0.52) with 775 avoided prescribing errors (95 percent CI 752–811) per 1,000 orders in a pediatric hospital.
Conclusions
Computerization of physicians' orders shows great promise. It will be more effective when linked to other computerized systems to detect and prevent prescribing errors.
Keywords: Medication errors, medical order entry systems, epidemiologic studies
BACKGROUND
Medication errors are associated with substantial death and injury (Kohn, Corrigan, and Donaldson 2000). More than half a million patients are injured or die each year in hospitals from adverse drug events (ADEs) (Classen et al. 1997) which may cost up to $5.6 million annually per hospital (Bates et al. 1997). In 1992, 5 percent of hospitalized patients experienced medication errors (Bond, Raehl, and Franke 2001). The rate increased substantially to 24 percent from 1995 to 2000 (LaPointe and Jollis 2003).
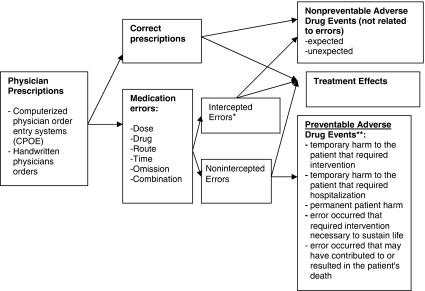
Physician ordering and transcription were responsible for 50–61 percent of all medication errors (Bates et al. 1995b; Leape et al. 1995). Figure 1 outlines the relationship between medication errors and ADEs. Computerized Physician Order Entry (CPOE) systems were expected to dramatically reduce error rates (Bates et al. 1995b). The Institute of Medicine has identified medication errors as a major threat to patient safety and has endorsed electronic prescribing as a promising approach to combating them (Board on Health Care Services [HCS] et al. 2006). One systematic review reported that CPOE substantially reduced medication errors but not clinical adverse events resulting from errors (Kaushal, Shojania, and Bates 2003).
Figure 1.
Conceptual Model of the Association between Physician Prescriptions, Medication Errors, and Adverse Drug Events
*Intercepted medication errors are medication errors with significant potential to harm a patient that did not actually reach a patient. They may result in adverse drug events not related to errors and therefore not preventable (severe cough after ACE inhibitors or vision loss after Sidenafil). Not intercepted errors may result in treatment effects (methicillin was prescribed for a patient allergic to penicillin, allergy did not occur, a patient recovered from bacterial infection) and preventable adverse events (allergic shock).
**Adverse drug events are injuries (clinical outcomes) resulting from drug use. Adverse drug events associated with a medication error are considered preventable
The implementation of CPOE has not always improved patient safety to expected levels (Han et al. 2005; Mirco et al. 2005; Nebeker et al. 2005; Del Beccaro et al. 2006). The clinical effects of CPOE on medication errors and clinical events have been studied previously without quantitative comparative effectiveness in different clinical settings (Kaushal, Barker, and Bates 2001a; Pape 2001; Wrobel 2003; Hughes and Edgerton 2005; Board on HCS et al. 2006; Jones and Moss 2006; Riskin, Shiff, and Shamir 2006; Joanna Briggs Institute 2006). The present review analyzes published evidence to test the hypothesis that medication errors and adverse clinical events decrease after computerization compared with handwritten physician orders in pediatric and adult patients independent of patient and provider characteristics.
METHODS
The protocol was created according to the recommendations for Meta-analysis of Observational Studies in Epidemiology (MOOSE) (Stroup et al. 2000). Electronic databases, including Medline, Cochrane Central Register of Controlled Trials, WorldCat, and Internet engines (http://www.Google.com), were searched using MeSH headings and keywords “Medical Records Systems, Computerized,”“Medication Errors,”“Medical Order Entry Systems,” and their combinations. Eligible studies were defined as original observational or interventional investigations published in English from 1990 to 2005.
The level of evidence was estimated using the U.S. Preventive Services Task Force criteria (Harris et al. 2001). Reviews, expert opinions, studies focused on long-term care, and studies comparing different degrees of decision support system in CPOE were excluded. The standardized abstraction protocol (The Cochrane Collaboration 2005) included the first author, year and journal of the publication, target population, clinical settings, randomization in intervention and random sampling in observational investigations, assessment of outcomes, adjustment for confounding factors, and outcomes rates using handwritten and computerized orders.
Statistical Analyses
Pooled odds ratios (ORs) and 95 percent confidence intervals (CIs) were calculated with fixed and random effects models (DerSimonian and Laird 1986). Independent variables were defined as physician order systems (computerized versus handwritten), target population, and clinical settings. Dependent variables were defined as medication errors and adverse events rates among total prescriptions and per 1,000 patient days. Meta-regression models analyzed possible interactions with the year of publication, presence of a control group versus pre- and post-CPOE comparisons, target population (pediatric versus adults), clinical settings (acute versus chronic care), and rate of outcomes in the group with handwritten orders. Publication bias was assessed with Egger's test (Egger et al. 1997), a modification of Macaskill's test (Peters et al. 2006), and the Trim and Fill method (Duval and Tweedie 2000). Heterogeneity between studies was quantified using the I2 statistic (Higgins et al. 2003). Statistical significance was analyzed at the 95 percent confidence level. All calculations were conducted using STATA software (Egger 2001).
RESULTS
From 252 articles included in the initial database (Appendix A), 12 studies reported rates of prescribing errors after CPOE and handwritten orders (Bates et al. 1998, 1999; Teich et al. 2000; Bizovi et al. 2002; Fontan et al. 2003; King et al. 2003; Cordero et al. 2004; Potts et al. 2004; Gandhi et al. 2005; Oliven et al. 2005; Shulman et al. 2005; Upperman et al. 2005), seven compared the effects of CPOE with different decision support systems (Chertow et al. 2001; Mekhjian et al. 2002; Overhage et al. 2002; Colombet et al. 2004; Galanter, Polikaitis, and DiDomenico 2004; Galanter, Didomenico, and Polikaitis 2005; Koppel et al. 2005; Mirco et al. 2005), and four analyzed the likelihood of preventing medication errors (Bates et al. 1995a; Kaushal et al. 2001b; Fortescue et al. 2003; Bobb et al. 2004). Among 12 studies eligible for meta-analysis (Bates et al. 1998, 1999; Teich et al. 2000; Bizovi et al. 2002; Fontan et al. 2003; King et al. 2003; Cordero et al. 2004; Potts et al. 2004; Gandhi et al. 2005; Oliven et al. 2005; Shulman et al. 2005; Upperman et al. 2005), three studies reported rates of medication errors per 1,000 patients days (Bates et al. 1998, 1999; King et al. 2003), and the others provided a number of errors among total prescriptions. Three out of 12 studies analyzed errors related to a wrong drug (Fontan et al. 2003; Potts et al. 2004; Shulman et al. 2005) and seven out of 12 reported errors related to a wrong dose (Teich et al. 2000; Bizovi et al. 2002; Fontan et al. 2003; Cordero et al. 2004; Potts et al. 2004; Oliven et al. 2005; Shulman et al. 2005) (Table 1). Total adverse events rates were obtained from a pooled estimation of eight studies (Bates et al. 1998, 1999; Bizovi et al. 2002; King et al. 2003; Potts et al. 2004; Gandhi et al. 2005; Shulman et al. 2005; Upperman et al. 2005) (Table 2).
Table 1.
Studies That Analyzed the Association between Computerized Physician Order Entry (CPOE) System and Medication Errors
| Author, Year, Sample Size | Design | Settings | Outcomes Assessment | Type of Errors | Absolute Change in Rate | p-Value |
|---|---|---|---|---|---|---|
| Bates et al. (1998) 6,711 admissions | Intervention, prospective before 9 months after CPOE comparisons | 6 randomly selected units in 726-bed tertiary care hospital | Staff reporting | Not intercepted serious ME | −55% | .01 |
| Staff interviewing | Not intercepted serious ME by stage of ordering | |||||
| Medical charts reviewing; κ*=0.81–0.98 | ||||||
| Ordering | −19% | .03 | ||||
| Transcription | −84% | <.001 | ||||
| Dispensing | −68% | .001 | ||||
| Administration | −59% | <.001 | ||||
| Bates et al. (1999) 1,817 admissions | Intervention, prospective before 4.5 years after CPOE comparisons | 3 units in 700-bed tertiary care academic hospital | Pharmacists reporting | Nonmissed dose errors | −82.8% | .0001 |
| Missed dose errors | 71% | .0001 | ||||
| Staff interviewing | Not intercepted serious medication errors | −85.5% | .0003 | |||
| Medical charts review | ||||||
| Type of errors | ||||||
| Dose | −55.16% | .03 | ||||
| Frequency | −91.67% | .0001 | ||||
| Route | −85.71% | .0001 | ||||
| Substitution | −100% | .0001 | ||||
| Documented allergy | −100% | .0001 | ||||
| Inappropriate drug | −100% | .002 | ||||
| Teich et al. (2000) 328,143 orders | Intervention, prospective before 2 years after CPOE comparisons | 720-bed urban tertiary-care academic hospital | Pharmacists review of medical charts and CPOE database | Wrong dose errors (prescribed dose exceed the highest recommended) | −1.9% | <.001 |
| Bizovi et al. (2002) 7,036 patients | Retrospective before–after CPOE analysis adjusted for prescriber type, patients age, and number of prescriptions | Emergency Department in tertiary care teaching hospital | Pharmacists reports | Relative risk | 95% CI | |
| Total medication errors | 0.31 | 0.2–0.6 | ||||
| Missing information | 0.28 | 0.1–1.1 | ||||
| Incorrect information | 0.29 | 0.1–0.6 | ||||
| Incorrect dose | 0.31 | 0.1–6.02 | ||||
| Fontan et al. (2003) 49 patients, 511 prescriptions | Randomized 8-week intervention | Nephrology ward in 510-bed pediatric and maternity hospital | Pharmacists review of medical charts | Total prescribing errors | −77% | <.0001 |
| Wrong drug | −0.3% | NS | ||||
| Wrong dose | −1.9% | NS | ||||
| Wrong route | −0.3% | NS | ||||
| King et al. (2003) 36,103 discharges, 179,183 patient days | Retrospective before–after CPOE analysis | 3 medical and 2 surgical wards in tertiary-care pediatric teaching hospital | Physicians review of medical charts; κ=0.64 (0.45–0.82) | Rate of total medication errors/1,000 patient-days | −2.06 | <.001 |
| Relative risk | 95% CI | |||||
| 0.6 | 0.48–0.74 | |||||
| Cordero et al. (2004) 194 admissions | Retrospective before 6 months after CPOE analysis | Newborn ICU in teaching hospital | Pharmacist reports; CPOE database | Total medication errors to prescribe gentamicin | −100% | |
| Wrong dose of gentamicin | −100% | |||||
| Upperman et al. (2005) 8,619 admissions | Intervention, prospective before 9 months after CPOE comparisons | Pediatric academic hospital | Investigators review of hospital discharge records | Total prescribing errors | −100% | |
| Potts et al. (2004) 514 patients | Intervention, prospective before 2 months after CPOE comparisons | 20-bed Pediatric ICU | Pharmacist and physicians review of medical charts κ*=0.96 | Overall errors | −95.9% | <.05 |
| Total prescribing errors | −99.4% | |||||
| Wrong dose | 7.6% | .69 | ||||
| Wrong drug | −88.8% | .07 | ||||
| Gandhi et al. (2005) 1,202 patients, 1,879 orders | Prospective comparison in practices with CPOE and handwritten orders | 4 adult primary care practices affiliated with academic medical center | Pharmacists reports | Total prescribing errors | −6.70% | .31 |
| Physicians interview | ||||||
| Patients interview κ=0.92 | ||||||
| Oliven et al. (2005) 1,350 patients | Prospective comparison in units with CPOE and handwritten orders | Acute care teaching hospital | Physician review of medical charts | Wrong dose or interval | −81.80% | <.001 |
| Error in drug interaction | −50% | <.01 | ||||
| Transcription errors | −81.80% | <.001 | ||||
| Drug–laboratory interaction | −64% | <.001 | ||||
| Wrong drug | −60% | <.01 | ||||
| OR | ||||||
| Total prescribing errors | 0.24 (0.17– 0.32) | |||||
| Shulman et al. (2005) 3,465 orders | Prospective before 37 weeks after CPOE analysis | Adult ICU in teaching hospital | Pharmacist and clinical review of medical charts | Total prescribing errors | −1.9% | <.04 |
| Wrong dose | 0.12% | |||||
| Wrong drug | −0.04% |
κ statistic to quantify the level of agreement in detection of ME and ADE.
CI, confidence interval; ICU, intensive care unit; ADE, adverse drug event.
Table 2.
Studies Included in Meta-Analysis to Analyze the Association between Computerized Physician Order Entry System and Adverse Drug Events
| Author, Year, Sample Size | Adverse Event Type | Absolute Change in Rate | p-Values |
|---|---|---|---|
| Bates et al. (1998) 6,711admissions | Preventable ADE | −17% | .37 |
| Not intercepted potential ADE | −84% | .002 | |
| All ADE | −5% | .77 | |
| Not preventable ADE | 0% | .99 | |
| All potential ADE | −71% | .02 | |
| Intercepted potential ADE | −58% | .15 | |
| Bates et al. (1999) 1,817 admissions | Not intercepted potential ADE | −100% | .0006 |
| Intercepted potential ADE | −96.80% | .15 | |
| Preventable ADE | −62.10% | .05 | |
| Total ADE | −34.70% | .09 | |
| Bizovi et al. (2002) 7,036 patients | Total potential ADE | Relative risk | 95% CI |
| 0.87 | 0.14–5.39 | ||
| Upperman et al. (2005) 8,619 admissions | Total ADE | 23.30% | .3 |
| Harmful ADE | −40% | .05 | |
| Potts et al. (2004) 514 patients | Potential ADE | −40.9% | <.001 |
| Gandhi et al. (2005) 1,202 patients | Potential ADE | −1.40% | .16 |
| Shulman et al. (2005) 3,465 orders | Intercepted ADE | −67% | |
| Total not-intercepted and intercepted ADE | −1.8% | .01 | |
| King et al. (2003) 36,103 discharges, 179,183 patient days | ADE | Rate ratio | |
| Potential ADE | 1.3 (0.47–3.52) | .6 | |
| 0.24(0.09–0.68) | <.001 |
Clinical settings and outcome assessment provided in the Table 1.
ADE, adverse drug events.
Definitions of Exposure
Most studies defined CPOE as “direct entry of medical orders into the computer” (Ash et al. 2004). However, within this definition, authors reported different CPOE software packages with and without a decision-making support system (Appendix B). Several studies conducted at the Brigham and Women's Hospital used the Brigham Integrated Computing System (BICS) (Bates et al. 1998, 1999; Teich et al. 2000; Chertow et al. 2001). Potts et al. (2004) analyzed the effects of software (WizOrder) created and implemented by the faculty at Vanderbilt University. Other investigators used a vendor-based system modified for adult and pediatric patients (Mekhjian et al. 2002; Cordero et al. 2004). We could not quantify the functionality of the CPOE software used and assumed that any differences would not modify the impact on outcomes.
Definitions of Outcomes
The majority of the studies used the definition of medication errors developed by the American Society of Health-System Pharmacists (No authors listed 1998). Medication errors were defined as “any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the health care professional, patient, or consumer.” Prescribing errors are the most common errors and include wrong drug, form, dosage or frequency; wrong route; and contraindicated drug use and interaction (Fontan et al. 2003). Errors in administering drugs, a subcategory of medication errors, include omission of a dose; and wrong dose, route, or time. Bates et al. (1998) further categorized medication errors and adverse events by severity and harm for patients. Potts et al. (2004) defined rules violations as errors not compliant with standard hospital practices (e.g., abbreviations). An ADE was defined as “an injury from a medicine (or lack of an intended medicine).” The U.S. Pharmacopeia Convention classified ADEs by length and severity (Santell et al. 2003). We included in the meta-analyses rates of total prescribing medication errors, of wrong dose and wrong drug errors, and of ADEs.
Study Designs
Only one intervention study randomly allocated patients to CPOE or handwritten orders (Fontan et al. 2003). Few authors used random sampling of patients (Bates et al. 1998) or physician practices (Weingart et al. 2003) to minimize selection bias and increase the external validity of studies. Two prospective studies had formal control groups (Gandhi et al. 2005; Oliven et al. 2005) (Table 1). Adjustment for confounding by patient and provider characteristics was reported in one study (Bizovi et al. 2002).
Tests for Publication Bias
Macaskill's and Egger's tests for publication bias were not statistically significant for any of the outcomes. The Trim and Fill method indicated a modest amount of publication or small study bias in dosing errors, but without any practical impact on the pooled estimate. There was no apparent bias for medication errors. For adverse events, funnel plot asymmetry was absent if the large study (King et al. 2003) was omitted. The Trim and Fill method is recommended as a tool for sensitivity analysis, and in this case should be interpreted with some caution due to both the small number of studies and the large amount of heterogeneity between studies (Terrin et al. 2003).
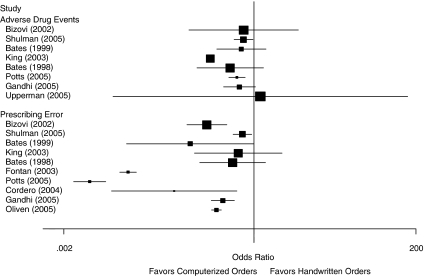
Medication Errors
We calculated the ORs of medication errors for each study to enable inclusion of all studies with differential reporting of outcomes (Figure 2). All studies reported a reduction in medication errors after CPOE. The strength of the association differed among studies with 98.6 percent of variance between studies attributable to heterogeneity (p<.0001). The presence of a control group versus before–after comparisons, clinical setting, and inclusion of not intercepted errors did not influence the association between CPOE and medication errors. However, two factors significantly modified the effects of CPOE: the rate of medication errors in the group with handwritten physician orders (p for interaction=.022) and target population (p for interaction=.028). The use of CPOE was associated with a 66 percent reduction in medication errors in adults (OR=0.34; 95 percent CI 0.22–0.52) and a similar effect in children, although not statistically significant in a pooled analysis (OR=0.31; 95 percent CI 0.09–1.02) (Table 3). The effect of CPOE was larger when the rate of medication errors was more than 12 percent (highest 20 percent of the distribution) with handwritten physician orders.
Figure 2.
Odds Ratios of Medication Prescribing Errors and Adverse Drug Events with Computerized Physician Order Entry (CPOE) System Compared with Handwritten Orders. Box Size Is Proportional to Individual Study Precision
Table 3.
Meta-Analyses of the Association between Computerized Physician Order Entry System and Medication Errors with Random Effects Models
| Outcomes/Authors | Odds Ratio (95% CI) | Number Needed to Treat to Prevent One Event | Number of Avoided Events per 1,000 Prescriptions (95% CI) |
|---|---|---|---|
| Medication errors | 0.14 (0.05–0.43) | Not valid due to heterogeneity in odds ratios | Not valid due to heterogeneity in odds ratios |
| Fontan et al. (2003) | 0.02 (0.01–0.02) | 3 | 775 (752–811) |
| Potts et al. (2004 | 0.001 (0.00–0.01) | 8 | 299 (296–301) |
| Cordero et al. (2004) | 0.07 (0.01–0.57) | 55 | 127 (53–132) |
| Bizovi et al. (2002) | 0.21 (0.11–0.41) | 15 | 18 (14–21) |
| Gandhi et al. (2005) | 0.36 (0.25–0.53) | 10 | 67 (48–80) |
| Oliven et al. (2005) | 0.29 (0.25–0.34) | 50 | 96 (89–102) |
| Shulman et al. (2005) | 0.69 (0.51–0.93) | 142 | 20 (5–32) |
| *Bates et al. (1998) | 0.12 (0.02–0.99) | 143 | 7 (1–8) |
| King et al. (2003) | 0.60 (0.14–2.51) | ||
| Bates et al. (1999) | 0.50 (0.17–1.46) | ||
| Subgroup analyses of association of CPOE and prescribing errors | |||
| Adults (Bates et al. 1998, 1999; Teich et al. 2000; Bizovi et al. 2002; Gandhi et al. 2005; Oliven et al. 2005; Shulman et al. 2005) | 0.34 (0.22–0.52) | Not valid due to heterogeneity in odds ratios | Not valid due to heterogeneity in odds ratios |
| Children (Fontan et al. 2003; King et al. 2003; Cordero et al. 2004; Potts et al. 2004; Upperman et al. 2005) | 0.31 (0.09–1.02) | ||
| Rate of medication errors in the group with handwritten physician orders <12% (Bates et al. 1998, 1999; Bizovi et al. 2002; King et al. 2003; Gandhi et al. 2005; Shulman et al. 2005) | 0.39 (0.24–0.62) | Not valid due to heterogeneity in odds ratios | Not valid due to heterogeneity in odds ratios |
| Rate of medication errors in the group with handwritten physician orders >12% (Fontan et al. 2003; Cordero et al. 2004; Potts et al. 2004; Oliven et al. 2005) | 0.07 (0.05–0.08) | ||
| Wrong drug | 0.80 (0.27–2.36) | Not valid due to heterogeneity in odds ratios | Not valid due to heterogeneity in odds ratios |
| Shulman et al. (2005) | 0.85 (0.21–3.42) | ||
| Fontan et al. (2003) | 1.50 (0.53–4.21) | ||
| Potts et al. (2004) | 0.16 (0.02–1.34) | ||
| Wrong dose | 0.44 (0.23–0.85) | Not valid due to heterogeneity in odds ratios | Not valid due to heterogeneity in odds ratios |
| Teich et al. (2000) | 0.26 (0.24–0.29) | 65 | 15 (15–16) |
| Bizovi et al. (2002) | 0.36 (0.04–3.44) | ||
| Oliven et al. (2005) | 0.19 (0.11–0.34) | 76 | 13 (11–15) |
| Shulman et al. (2005) | 1.10 (0.56–2.16) | ||
| Fontan et al. (2003) | 0.28 (0.15–0.52) | 52 | 19 (13–23) |
| Potts et al. (2004) | 1.08 (0.74–1.57) | ||
| Cordero et al. (2004) | 0.54 (0.05–6.27) | ||
| Adverse drug events | 0.52 (0.30–0.91) | Not valid due to heterogeneity in odds ratios | Not valid due to heterogeneity in odds ratios |
| Upperman et al. (2005) | 1.23 (0.01–152.3) | ||
| Potts et al. (2004) | 0.57 (0.44–0.75) | 109 | 9 (5–12) |
| Bizovi et al. (2002) | 0.71 (0.12–4.28) | ||
| Gandhi et al. (2005) | 0.62 (0.37–1.05) | ||
| Shulman et al. (2005) | 0.71 (0.52–0.96) | 86 | 12 (2–20) |
| Bates et al. (1998) | 0.66 (0.30–1.48) | ||
| *King et al. (2003) | 0.24 (0.23–0.25) | 7 | 141 (139–144) |
| Bates et al. (1999) | 0.46 (0.16–1.36) | ||
Studies that reported rates of medication errors and adverse drug events per 1,000 patient days.
CI, confidence interval; CPOE, Computerized Physician Order Entry.
The calculated “number needed to treat” and “number of orders needed to prescribe with CPOE to prevent one event” for each study with significant ORs are shown in Table 3. Heterogeneity remained significant in subgroups of adult and children populations and in studies with different baseline rates of medication errors with more than 70 percent of the variation attributable to differences between individual studies. Therefore, pooled ORs are not reliable and valid estimates of effects of CPOE and clinical decisions should be made based on results from individual studies. The greatest benefit of CPOE was demonstrated in one randomized controlled trial with 775 avoided medication errors (95 percent CI 752–811) per 1,000 orders (Fontan et al. 2003).
The rate of prescribing a wrong drug did not decrease after CPOE. Medication errors related to a wrong dose were significantly reduced in three studies with nonsignificant changes in four other studies (Table 3). The results of individual studies varied significantly (p for heterogeneity <.001). A greater decrease in dose errors was observed in studies with a control group compared with pre- and post-CPOE analyses (p for interaction <.001). Randomized intervention demonstrated a 72 percent reduction in risk of wrong dose medication errors using CPOE (OR=0.28; 95 percent CI 0.15–0.52) with 19 avoided medication errors per 1,000 orders.
ADEs
Total adverse events were lessened after CPOE in three studies (Table 3) with a positive but not statistically significant tendency to reduce ADE in four studies. The test for heterogeneity was significant (p<.001) and could not be explained with meta-regression: neither year of publication (p=.9), the presence of control group (p=.8), the target population (p=.6), nor clinical setting (p=.9) affected the association between CPOE and ADE. The use of CPOE would prevent 9 ADEs per 1,000 prescriptions in pediatric (Potts et al. 2004) and 12 ADEs per 1,000 prescriptions in adult population (Shulman et al. 2005).
DISCUSSION
The present review of a randomized trial (Fontan et al. 2003) (level of evidence I) and several uncontrolled interventions (Bates et al. 1998; Teich et al. 2000; Cordero et al. 2004; Potts et al. 2004; Upperman et al. 2005) and observational studies (Bizovi et al. 2002; Gandhi et al. 2005; Oliven et al. 2005; Shulman et al. 2005) (levels of evidence II2–II3) confirmed previous contentions (Kaushal, Shojania, and Bates 2003; Koppel 2005) that implementation of CPOE was associated with a significant reduction in medication errors in adult and pediatric populations. The observed heterogeneity in results, not explained by known population and design characteristics, did not provide a valid quantitative estimation of relative risk. The statistical tests did not detect publication bias but the results can be misleading when the number of the studies are small and between-study heterogeneity is significant. (Terrin et al. 2003; Lau et al. 2006) These tests cannot eliminate the possibility of publication bias, but given the interest in this topic it seems likely that negative findings would be reported. Despite a significant reduction in medication errors in most studies, the results should be interpreted with caution. Nonrandomized uncontrolled interventions may provide biased overestimated effects of CPOE (Ioannidis et al. 2001) that are difficult to use for evidence-based decision making (Schulz et al. 1995).
In addition to previous reviews, we statistically examined the impact of study design and clinical settings on comparative effectiveness of CPOE. The beneficial effect of CPOE was larger in studies with greater baseline rates of medication errors in both the present analysis and in previous publications (Choi et al. 1992). The risk of harmful events related to medication errors was three time higher in children compared with adults with the same rate of medication errors (Fortescue et al. 2003), although the effects of CPOE was less potent in pediatric settings. The use of CPOE eliminated medication errors in specialized units (Mekhjian et al. 2002; Cordero et al. 2004) that prescribed fewer groups of drugs, and therefore had a higher probability of positive effects from the interventions. Time of exposure, geographical locations, academic affiliation of the clinics, and changes in drug coverage have been identified as possible effect modifiers and should be included into future analysis (Choi et al. 1992).
The use of CPOE was not associated with a substantial improvement in patient safety (Kaushal, Shojania, and Bates 2003; Oren, Shaffer, and Guglielmo 2003). Nonrandomized controlled interventions examined the effects of CPOE on preventable adverse events associated with medication errors. Two studies showed a significant reduction in potential ADEs in pediatric populations, by 43 percent in an intensive care unit (Potts et al. 2004) (OR=0.57, 95 percent CI 0.44–0.75) and by 76 percent in medical and surgical wards (King et al. 2003) (OR=0.24; 95 percent CI 0.24–0.25). Some authors reported reduction by 84–100 percent in intercepted (prevented) adverse events in adults (Bates et al. 1998, 1999). Differences in definition of outcomes and in interception strategies to prevent patient adverse events (Figure 1) may bias the results of individual studies and pooled analysis.
The variability in CPOE systems complicated comparing the results (Appendix B). Although more than two-thirds (7/10) of the products included in the meta-analysis have incorporated a clinical decision support system into CPOE (Bates et al. 1998, 1999; Teich et al. 2000; Bizovi et al. 2002; Fontan et al. 2003; Cordero et al. 2004; Potts et al. 2004; Gandhi et al. 2005; Oliven et al. 2005), they vary in the degree of decision support capacities. The majority (Bates et al. 1998, 1999; Teich et al. 2000; Bizovi et al. 2002; Fontan et al. 2003; Gandhi et al. 2005; Oliven et al. 2005) provide defaults, acceptable values, and required fields such as dose, duration, and frequency, to facilitate complete and accurate order entry. Several can also perform drug–allergy, drug–drug, drug–disease, and drug–lab interaction checking (Bates et al. 1998, 1999; Teich et al. 2000; Bizovi et al. 2002; Fontan et al. 2003; Cordero et al. 2004; Potts et al. 2004; Gandhi et al. 2005; Oliven et al. 2005). This order-checking function has the potential to reduce drug interactions and contraindications. Only two products have the advanced feature of patient-specific dose calculation (Cordero et al. 2004; Potts et al. 2004) which helps physicians detect prescription errors in a timely manner. Retrospective studies did not analyze differences in availability, inducement, physician's participation, and saturation of CPOE in participating hospitals. According to a survey of 964 randomly selected American hospitals, 83.7 percent of hospitals did not have CPOE available for the physicians, 6.5 percent reported partial availability, and only 9.6 percent reported complete implementation (all orders could be entered in all stations) (Ash et al. 2004).
Authors have used different strategies to detect errors and patient injuries including review of patient charts, incident reports, attending medical rounds to detect undocumented medication errors, interview of medical personnel and patients, comparisons of pharmacists and physicians orders, and follow-up pharmacokinetic examinations of patients (Flynn et al. 2002; Pronovost, Miller, and Wachter 2006). The most common method to measure medication errors—self-report—may underestimate the true rate of outcomes (Kohn and Donaldson 2000; Pronovost, Miller, and Wachter 2006). Direct observations uncovered a 17.9 percent error rate, while chart review found only 0.9 percent (Flynn et al. 2002). Clinically significant medication errors were detected in 71 percent by direct observations, only 9 percent by records review, and none by incident report review. The agreement between evaluators using a κ statistic to measure medication errors differed across studies but was generally around 0.7, with the lowest agreement around the severity of adverse events (0.35). We could not include agreement coefficients in the meta-analysis because not all authors provided this information.
The studies do not allow broad generalizability. As is often the case with innovations, they were primarily conducted in teaching hospitals. CPOE's effects in more typical practice settings where the level of care may be different remains to be determined.
Clinics use other strategies in addition to CPOE to improve patient safety. Some evidence suggests that a combination of CPOE with a decision support system (Chertow et al. 2001; Tamblyn et al. 2003), computerized drug dosing (Hunt et al. 1998) and drug administration systems (Rothschild et al. 2005), automated safety alerts for particular drugs (Galanter, Polikaitis, and DiDomenico 2004; Galanter, Didomenico, and Polikaitis 2005), and clinical pharmacy services (Bond, Raehl, and Franke 2002) may decrease medication errors and preventable adverse events. Future research should assess the effects of combined strategies that include CPOE to improve patient safety.
CONCLUSIONS
Existing evidence (levels I–II3) suggests a significant reduction in prescribing medical errors is associated with implementing CPOE systems, but the effects are not consistent among patient populations and clinical settings and are compromised by the design of studies. Sites that use CPOE still experience high rates of medication errors and ADEs. Most of the studies reviewed were conducted in academic centers. The effect of CPOE in more typical practice settings remains to be determined. Future research is needed to investigate the true impact of CPOE on patient safety. Although a randomized trial would be more definitive (Wahrendorf, Blettner, and Edler 1985; Lachin, Matts, and Wei 1988; Signorini et al. 1993), a retrospective multicenter cohort study of randomly selected nationally representative samples of patients and physicians is more feasible and less expensive to estimate the effects of CPOE. In all studies, clear common definitions of intervention and outcomes and valid methods to measure them are essential to detect the effectiveness of CPOE on patient safety.
Acknowledgments
Author contributions:
Study concept and design: Kane R. L., Shamliyan T. A.
Acquisition of data: Shamliyan T. A., Jing Du.
Analysis and interpretation of data: Shamliyan T. A., Duval S., Kane R. L.
Drafting of the manuscript: Shamliyan T. A., Duval S., Jing Du., Kane R. L.
Statistical expertise: Duval S.
Study supervision: Kane R. L.
Supplementary material
The following supplementary material for this article is available:
Literature Search Strategies and Eligibility Status of the Reviewed Studies.
A Summary of CPOE Functionality by Product/Vendors.
This material is available as part of the online article from: http://www.blackwell-synergy.com/doi/abs/10.1111/j.1475-6773.2007.00751.x (this link will take you to the article abstract).
Please note: Blackwell Publishing is not responsible for the content or functionality of any supplementary materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Ash JS, Gorman PN, Seshadri V, Hersh WR. Computerized Physician Order Entry in U.S. Hospitals: Results of a 2002 Survey. Journal of the American Medical Informatics Association. 2004;11(2):95–9. doi: 10.1197/jamia.M1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aspden P Institute of Medicine (U.S.) Committee on Identifying and Preventing Medication Errors. Preventing Medication Errors. Washington, DC: National Academies Press; 2007. [Google Scholar]
- Bates DW, Cullen DJ, Laird N, Petersen LA, Small SD, Servi D, Laffel G, Sweitzer BJ, Shea BF, Hallisey R, Vander Vliet M, Nemeskal R, Leape LL. Incidence of Adverse Drug Events and Potential Adverse Drug Events. Implications for Prevention. ADE Prevention Study Group. Journal of the American Medical Association. 1995b;274(1):29–34. [PubMed] [Google Scholar]
- Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, Teich JM, Burdick E, Hickey M, Kleefield S, Shea B, Vander Vliet M, Seger DL. Effect of Computerized Physician Order Entry and a Team Intervention on Prevention of Serious Medication Errors. Journal of the American Medical Association. 1998;280(15):1311–6. doi: 10.1001/jama.280.15.1311. [DOI] [PubMed] [Google Scholar]
- Bates DW, Spell N, Cullen DJ, Burdick E, Laird N, Petersen LA, Small SD, Sweitzer BJ, Leape LL. The Costs of Adverse Drug Events in Hospitalized Patients. Adverse Drug Events Prevention Study Group. Journal of the American Medical Association. 1997;277(4):307–11. [PubMed] [Google Scholar]
- Bates DW, Teich JM, Lee J, Seger D, Kuperman GJ, Ma'Luf N, Boyle D, Leape L. The Impact of Computerized Physician Order Entry on Medication Error Prevention. Journal of the American Medical Informatics Association. 1999;6(4):313–21. doi: 10.1136/jamia.1999.00660313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bizovi KE, Beckley BE, McDade MC, Adams AL, Lowe RA, Zechnich AD, Hedges JR. The Effect of Computer-Assisted Prescription Writing on Emergency Department Prescription Errors. Academic Emergency Medicine. 2002;9(11):1168–75. doi: 10.1111/j.1553-2712.2002.tb01572.x. [DOI] [PubMed] [Google Scholar]
- Bobb A, Gleason K, Husch M, Feinglass J, Yarnold PR, Noskin GA. The Epidemiology of Prescribing Errors: The Potential Impact of Computerized Prescriber Order Entry. Archives of Internal Medicine. 2004;164(7):785–92. doi: 10.1001/archinte.164.7.785. [DOI] [PubMed] [Google Scholar]
- Bond CA, Raehl CL, Franke T. Medication Errors in United States Hospitals. Pharmacotherapy. 2001;21(9):1023–36. doi: 10.1592/phco.21.13.1023.34617. [DOI] [PubMed] [Google Scholar]
- Bond CA, Raehl CL, Franke T. Clinical Pharmacy Services, Hospital Pharmacy Staffing, and Medication Errors in United States Hospitals. Pharmacotherapy. 2002;22(2):134–47. doi: 10.1592/phco.22.3.134.33551. [DOI] [PubMed] [Google Scholar]
- Chertow GM, Lee J, Kuperman GJ, Burdick E, Horsky J, Seger DL, Lee R, Mekala A, Song J, Komaroff AL, Bates DW. Guided Medication Dosing for Inpatients with Renal Insufficiency. Journal of the American Medical Association. 2001;286(22):2839–44. doi: 10.1001/jama.286.22.2839. [DOI] [PubMed] [Google Scholar]
- Choi T, Thomas NA, Nyugen M, Sandler V, Kassel W, Edlavitch SA, Kane RL. Effects of Drug Audit Information to Providers of High-Risk Elderly Patients in a Prepaid Group Practice. In: Ahronheim JC, Rowe JW, Cristofalo VJ, editors. Annual Review of Gerontology and Geriatrics: Focus on Medications and the Elderly. Vol. 12. New York: Springer Publishing Company; 1992. pp. 76–94. [Google Scholar]
- Classen DC, Pestotnik SL, Evans RS, Lloyd JF, Burke JP. Adverse Drug Events in Hospitalized Patients. Excess Length of Stay, Extra Costs, and Attributable Mortality. Journal of the American Medical Association. 1997;277(4):301–6. [PubMed] [Google Scholar]
- Colombet I, Bura-Riviere A, Chatila R, Chatellier G, Durieux P. Personalized versus Non-Personalized Computerized Decision Support System to Increase Therapeutic Quality Control of Oral Anticoagulant Therapy: An Alternating Time Series Analysis. BMC Health Service Research. 2004;4(1):27. doi: 10.1186/1472-6963-4-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordero L, Kuehn L, Kumar RR, Mekhjian HS. Impact of Computerized Physician Order Entry on Clinical Practice in a Newborn Intensive Care Unit. Journal of Perinatology: Official Journal of the California Perinatal Association. 2004;24(2):88–93. doi: 10.1038/sj.jp.7211000. [DOI] [PubMed] [Google Scholar]
- Del Beccaro MA, Jeffries HE, Eisenberg MA, Harry ED. Computerized Provider Order Entry Implementation: No Association with Increased Mortality Rates in an Intensive Care Unit. Pediatrics. 2006;118(1):290–5. doi: 10.1542/peds.2006-0367. [DOI] [PubMed] [Google Scholar]
- DerSimonian R, Laird N. Meta-Analysis in Clinical Trials. Controlled Clinical Trials. 1986;7(3):177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Duval S, Tweedie R. Trim and Fill: A Simple Funnel-Plot-Based Method of Testing and Adjusting for Publication Bias in Meta-Analysis. Biometrics. 2000;56(2):455–63. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Egger M. Systematic Reviews in Health Care. London: BMJ; 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in Meta-Analysis Detected by a Simple, Graphical Test. British Medical Journal (Clinical Research Edition) 1997;315(7109):629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn EA, Barker KN, Pepper GA, Bates DW, Mikeal RL. Comparison of Methods for Detecting Medication Errors in 36 Hospitals and Skilled-Nursing Facilities. American Journal of Health-System Pharmacy: Official Journal of the American Society of Health-System Pharmacists. 2002;59(5):436–46. doi: 10.1093/ajhp/59.5.436. [DOI] [PubMed] [Google Scholar]
- Fontan JE, Maneglier V, Nguyen VX, Loirat C, Brion F. Medication Errors in Hospitals: Computerized Unit Dose Drug Dispensing System versus Ward Stock Distribution System. Pharmacy World and Science. 2003;25(3):112–7. doi: 10.1023/a:1024053514359. [DOI] [PubMed] [Google Scholar]
- Fortescue EB, Kaushal R, Landrigan CP, McKenna KJ, Clapp MD, Federico F, Goldmann DA, Bates DW. Prioritizing Strategies for Preventing Medication Errors and Adverse Drug Events in Pediatric Inpatients. Pediatrics. 2003;111(4, part 1):722–9. doi: 10.1542/peds.111.4.722. [DOI] [PubMed] [Google Scholar]
- Galanter WL, Didomenico RJ, Polikaitis A. A Trial of Automated Decision Support Alerts for Contraindicated Medications Using Computerized Physician Order Entry. Journal of the American Medical Informatics Association. 2005;12(3):269–74. doi: 10.1197/jamia.M1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galanter WL, Polikaitis A, DiDomenico RJ. A Trial of Automated Safety Alerts for Inpatient Digoxin Use with Computerized Physician Order Entry. Journal of the American Medical Informatics Association. 2004;11(4):270–7. doi: 10.1197/jamia.M1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandhi TK, Weingart SN, Seger AC, Borus J, Burdick E, Poon EG, Leape LL, Bates DW. Outpatient Prescribing Errors and the Impact of Computerized Prescribing. Journal of General Internal Medicine. 2005;20(9):837–41. doi: 10.1111/j.1525-1497.2005.0194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han YY, Carcillo JA, Venkataraman ST, Clark RS, Watson RS, Nguyen TC, Bayir H, Orr RA. Unexpected Increased Mortality after Implementation of a Commercially Sold Computerized Physician Order Entry System. Pediatrics. 2005;116(6):1506–12. doi: 10.1542/peds.2005-1287. [DOI] [PubMed] [Google Scholar]
- Harris R P H M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, Atkins D for the Methods Word Group, Third U.S. Preventive Services Task Force. Current Methods of the U.S. Preventive Services Task Force: A Review of the Process. American Journal of Preventive Medicine. 2001;20(3S):21–35. doi: 10.1016/s0749-3797(01)00261-6. Available at http://www.elsevier.com/locate/ajpmonline. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring Inconsistency in Meta-Analyses. British Medical Journal (Clinical Research Edition) 2003;327(7414):557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes RG, Edgerton EA. Reducing Pediatric Medication Errors: Children Are Especially at Risk for Medication Errors. American Journal of Nursing. 2005;105(5):79–80. doi: 10.1097/00000446-200505000-00035. 82, 85 passim. [DOI] [PubMed] [Google Scholar]
- Hunt DL, Haynes RB, Hanna SE, Smith K. Effects of Computer-Based Clinical Decision Support Systems on Physician Performance and Patient Outcomes: A Systematic Review. Journal of the American Medical Association. 1998;280(15):1339–46. doi: 10.1001/jama.280.15.1339. [DOI] [PubMed] [Google Scholar]
- Ioannidis JP, Haidich AB, Pappa M, Pantazis N, Kokori SI, Tektonidou MG, Contopoulos-Ioannidis DG, Lau J. Comparison of Evidence of Treatment Effects in Randomized and Nonrandomized Studies. Journal of the American Medical Association. 2001;286(7):821–30. doi: 10.1001/jama.286.7.821. [DOI] [PubMed] [Google Scholar]
- Joanna Briggs Institute. Strategies to Reduce Medication Errors with Reference to Older Adults. Nursing Stand. 2006;20(41):53–7. doi: 10.7748/ns.20.41.53.s60. [DOI] [PubMed] [Google Scholar]
- Jones S, Moss J. Computerized Provider Order Entry: Strategies for Successful Implementation. Journal of Nursing Administration. 2006;36(3):136–9. doi: 10.1097/00005110-200603000-00007. [DOI] [PubMed] [Google Scholar]
- Kaushal R, Barker KN, Bates DW. How Can Information Technology Improve Patient Safety and Reduce Medication Errors in Children's Health Care? Archives of Pediatrics and Adolescent Medicine. 2001a;155(9):1002–7. doi: 10.1001/archpedi.155.9.1002. [DOI] [PubMed] [Google Scholar]
- Kaushal R, Bates DW, Landrigan C, McKenna KJ, Clapp MD, Federico F, Goldmann DA. Medication Errors and Adverse Drug Events in Pediatric Inpatients. Journal of the American Medical Association. 2001b;285(16):2114–20. doi: 10.1001/jama.285.16.2114. [DOI] [PubMed] [Google Scholar]
- Kaushal R, Shojania KG, Bates DW. Effects of Computerized Physician Order Entry and Clinical Decision Support Systems on Medication Safety: A Systematic Review. Archives of Internal Medicine. 2003;163(12):1409–16. doi: 10.1001/archinte.163.12.1409. [DOI] [PubMed] [Google Scholar]
- King WJ, Paice N, Rangrej J, Forestell GJ, Swartz R. The Effect of Computerized Physician Order Entry on Medication Errors and Adverse Drug Events in Pediatric Inpatients. Pediatrics. 2003;112(3, part 1):506–9. doi: 10.1542/peds.112.3.506. [DOI] [PubMed] [Google Scholar]
- Kohn L T C J, Donaldson MS. To Err Is Human: Building a Safer Health System. Washington, DC: National Academic Press; 2000. [PubMed] [Google Scholar]
- Kohn LT, Corrigan J, Donaldson MS. To Err Is Human: Building a Safer Health System. Washington, DC: National Academic Press; 2000. [PubMed] [Google Scholar]
- Koppel R, Metlay JP, Cohen A, Abaluck B, Localio AR, Kimmel SE, Strom BL. Role of Computerized Physician Order Entry Systems in Facilitating Medication Errors. Journal of the American Medical Association. 2005;293(10):1197–203. doi: 10.1001/jama.293.10.1197. [DOI] [PubMed] [Google Scholar]
- Lachin JM, Matts JP, Wei LJ. Randomization in Clinical Trials: Conclusions and Recommendations. Controlled Clinical Trials. 1988;9(4):365–74. doi: 10.1016/0197-2456(88)90049-9. [DOI] [PubMed] [Google Scholar]
- LaPointe NM, Jollis JG. Medication Errors in Hospitalized Cardiovascular Patients. Archives of Internal Medicine. 2003;163(12):1461–6. doi: 10.1001/archinte.163.12.1461. [DOI] [PubMed] [Google Scholar]
- Lau J, Ioannidis JP, Terrin N, Schmid CH, Olkin I. The Case of the Misleading Funnel Plot. British Medical Journal (Clinical Research Edition) 2006;333(7568):597–600. doi: 10.1136/bmj.333.7568.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leape LL, Bates DW, Cullen DJ, Cooper J, Demonaco HJ, Gallivan T, Hallisey R, Ives J, Laird N, Laffel G, et al. Systems Analysis of Adverse Drug events. ADE Prevention Study Group. Journal of the American Medical Association. 1995;274(1):35–43. [PubMed] [Google Scholar]
- Mekhjian HS, Kumar RR, Kuehn L, Bentley TD, Teater P, Thomas A, Payne B, Ahmad A. Immediate Benefits Realized following Implementation of Physician Order Entry at an Academic Medical Center. Journal of the American Medical Informatics Association. 2002;9(5):529–39. doi: 10.1197/jamia.M1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirco A, Campos L, Falcao F, Nunes JS, Aleixo A. Medication Errors in an Internal Medicine Department. Evaluation of a Computerized Prescription System. Pharmacy World and Science. 2005;27(4):351–2. doi: 10.1007/s11096-005-2452-z. [DOI] [PubMed] [Google Scholar]
- Nebeker JR, Hoffman JM, Weir CR, Bennett CL, Hurdle JF. High Rates of Adverse Drug Events in a Highly Computerized Hospital. Archives of Internal Medicine. 2005;165(10):1111–6. doi: 10.1001/archinte.165.10.1111. [DOI] [PubMed] [Google Scholar]
- No authors listed. Suggested Definitions and Relationships among Medication Misadventures, Medication Errors, Adverse Drug Events, and Adverse Drug Reactions. American Journal of Health-System Pharmacy. 1998;55(2):165–6. doi: 10.1093/ajhp/55.2.165. [DOI] [PubMed] [Google Scholar]
- Oliven A, Michalake I, Zalman D, Dorman E, Yeshurun D, Odeh M. Prevention of Prescription Errors by Computerized, On-Line Surveillance of Drug Order Entry. International Journal of Medical Informatics. 2005;74(5):377–86. doi: 10.1016/j.ijmedinf.2005.03.010. [DOI] [PubMed] [Google Scholar]
- Oren E, Shaffer ER, Guglielmo BJ. Impact of Emerging Technologies on Medication Errors and Adverse Drug Events. American Journal of Health-System Pharmacy. 2003;60(14):1447–58. doi: 10.1093/ajhp/60.14.1447. [DOI] [PubMed] [Google Scholar]
- Overhage JM, Dexter PR, Perkins SM, Cordell WH, McGoff J, McGrath R, McDonald CJ. A Randomized, Controlled Trial of Clinical Information Shared from Another Institution. Annals of Emergency Medicine. 2002;39(1):14–23. doi: 10.1067/mem.2002.120794. [DOI] [PubMed] [Google Scholar]
- Pape TM. Searching for the Final Answer: Factors Contributing to Medication Administration Errors. Journal of Continuing Education in Nursing. 2001;32(4):152–60. doi: 10.3928/0022-0124-20010701-05. quiz 90–1. [DOI] [PubMed] [Google Scholar]
- Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of Two Methods to Detect Publication Bias in Meta-Analysis. Journal of the American Medical Association. 2006;295(6):676–80. doi: 10.1001/jama.295.6.676. [DOI] [PubMed] [Google Scholar]
- Potts AL, Barr FE, Gregory DF, Wright L, Patel NR. Computerized Physician Order Entry and Medication Errors in a Pediatric Critical Care Unit. Pediatrics. 2004;113(1, part 1):59–63. doi: 10.1542/peds.113.1.59. [DOI] [PubMed] [Google Scholar]
- Pronovost PJ, Miller MR, Wachter RM. Tracking Progress in Patient Safety: An Elusive Target. Journal of the American Medical Association. 2006;296(6):696–9. doi: 10.1001/jama.296.6.696. [DOI] [PubMed] [Google Scholar]
- Riskin A, Shiff Y, Shamir R. Parenteral Nutrition in Neonatology—To Standardize or Individualize? Israel Medical Association Journal. 2006;8(9):641–5. [PubMed] [Google Scholar]
- Rothschild JM, Keohane CA, Cook EF, Orav EJ, Burdick E, Thompson S, Hayes J, Bates DW. A Controlled Trial of Smart Infusion Pumps to Improve Medication Safety in Critically Ill Patients. Critical Care Medicine. 2005;33(3):533–40. doi: 10.1097/01.ccm.0000155912.73313.cd. [DOI] [PubMed] [Google Scholar]
- Santell JP, Hicks RW, McMeekin J, Cousins DD. Medication Errors: Experience of the United States Pharmacopeia (USP) MEDMARX Reporting System. Journal of Clinical Pharmacology. 2003;43(7):760–7. [PubMed] [Google Scholar]
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical Evidence of Bias. Dimensions of Methodological Quality Associated with Estimates of Treatment Effects in Controlled Trials. Journal of the American Medical Association. 1995;273(5):408–12. doi: 10.1001/jama.273.5.408. [DOI] [PubMed] [Google Scholar]
- Shulman R, Singer M, Goldstone J, Bellingan G. Medication Errors: A Prospective Cohort Study of Hand-Written and Computerised Physician Order Entry in the Intensive Care Unit. Critical Care (London, U.K.) 2005;9(5):R516–21. doi: 10.1186/cc3793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Signorini DF, Leung O, Simes RJ, Beller E, Gebski VJ, Callaghan T. Dynamic Balanced Randomization for Clinical Trials. Statistics in Medicine. 1993;12(24):2343–50. doi: 10.1002/sim.4780122410. [DOI] [PubMed] [Google Scholar]
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-Analysis of Observational Studies in Epidemiology: A Proposal for Reporting. Meta-Analysis of Observational Studies in Epidemiology (MOOSE) Group. Journal of the American Medical Association. 2000;283(15):2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- Tamblyn R, Huang A, Perreault R, Jacques A, Roy D, Hanley J, McLeod P, Laprise R. The Medical Office of the 21st Century (MOXXI): Effectiveness of Computerized Decision-Making Support in Reducing Inappropriate Prescribing in Primary Care. Canadian Medical Association Journal—Journal de l'Association Medicale Canadienne. 2003;169(6):549–56. [PMC free article] [PubMed] [Google Scholar]
- Teich JM, Merchia PR, Schmiz JL, Kuperman GJ, Spurr CD, Bates DW. Effects of Computerized Physician Order Entry on Prescribing Practices. Archives of Internal Medicine. 2000;160(18):2741–7. doi: 10.1001/archinte.160.18.2741. [DOI] [PubMed] [Google Scholar]
- Terrin N, Schmid CH, Lau J, Olkin I. Adjusting for Publication Bias in the Presence of Heterogeneity. Statistics in Medicine. 2003;22(13):2113–26. doi: 10.1002/sim.1461. [DOI] [PubMed] [Google Scholar]
- The Cochrane Collaboration. “The Cochrane Handbook for Systematic Reviews of Interventions”. 2005. [2007 May]. Available at http://www.cochrane.org/resources/handbook/handbook.pdf.
- Upperman JS, Staley P, Friend K, Neches W, Kazimer D, Benes J, Wiener ES. The Impact of Hospitalwide Computerized Physician Order Entry on Medical Errors in a Pediatric Hospital. Journal of Pediatric Surgery. 2005;40(1):57–9. doi: 10.1016/j.jpedsurg.2004.09.024. [DOI] [PubMed] [Google Scholar]
- Wahrendorf J, Blettner M, Edler L. An Investigation of the Adequacy of a Randomization. Controlled Clinical Trials. 1985;6(4):249–58. doi: 10.1016/0197-2456(85)90101-1. [DOI] [PubMed] [Google Scholar]
- Weingart SN, Toth M, Sands DZ, Aronson MD, Davis RB, Phillips RS. Physicians' Decisions to Override Computerized Drug Alerts in Primary Care. Archives of Internal Medicine. 2003;163(21):2625–31. doi: 10.1001/archinte.163.21.2625. [DOI] [PubMed] [Google Scholar]
- Wrobel JP. Are We Ready for the Better Medication Management System? Medical Journal of Australia. 2003;178(9):448–50. doi: 10.5694/j.1326-5377.2003.tb05288.x. [DOI] [PubMed] [Google Scholar]
- Bates DW, Boyle DL, Vander Vliet MB, Schneider J, Leape L. Relationship between Medication Errors and Adverse Drug Events. Journal of General Internal Medicine: Official Journal of the Society for Research and Education in Primary Care Internal Medicine. 1995a;10(4):199–205. doi: 10.1007/BF02600255. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Literature Search Strategies and Eligibility Status of the Reviewed Studies.
A Summary of CPOE Functionality by Product/Vendors.