Abstract
Estrogen has pleiotropic actions, among which are its anti-apoptotic, anti-inflammatory, and vasodilatory effects. Recently, an interaction between 17β-estradiol (E2) and the transcription factor nuclear factor κB (NFκB) has been identified. NFκB has a central role in the control of genes involved in inflammation, proliferation, and apoptosis. Prolonged activation of NFκB is associated with numerous inflammatory pathological conditions. An important facet of E2 is its ability to modulate activity of NFκB via both genomic and nongenomic actions. E2 can activate NFκB rapidly via nongenomic pathways, increase cellular resistance to injury, and induce expression of the protective class of proteins, heat shock proteins (HSPs). HSPs can bind to many of the pro-apoptotic and pro-inflammatory targets of NFκB and, thus, indirectly inhibit many of its deleterious effects. In addition, HSPs can block NFκB activation and binding directly. Similarly, genomic E2 signaling can inhibit NFκB, but does so through alternative mechanisms. This review focuses on the molecular mechanisms of cross-talk between E2, NFκB, and HSPs, and the biological relevance of this cross-talk.
INTRODUCTION
Estrogen is known to induce a number of beneficial physiological effects, especially in the neurologic and cardiovascular systems. Many of the benefits can be attributed to the antioxidant and vasodilatory effects of 17β-estradiol (E2), the most biologically active metabolite of estrogen. Despite the body of literature addressing the effects of this hormone, many of the interactions between estrogen and cellular signaling remain unknown. E2 has been shown to interact with the transcription factor nuclear factor κB (NFκB) and to modulate its activity. There are two phases to this interaction, an acute NFκB activating response that mediates cellular protection, and a late, chronic response to estrogen that inhibits NFκB. These contrasting responses and their signaling pathways will be discussed below.
NFκB
NFκB is a pivotal and potent transcription factor that serves dual roles. Activation leads to the expression of products that are both pro-apoptotic and anti-apoptotic, as well as pro-inflammatory and anti-inflammatory. Thus, this transcription factor is unique in that it encompasses the spectrum from protection to injury. NFκB is a critical protein in tissue response to stress and injury. Activation leads to cellular proliferation and cell survival through the induction of multiple anti-apoptotic proteins, and suppression of other stress cascades (1). However, activation also leads to expression of pro-inflammatory cytokines. NFκB activation allows cells to be protected and proliferate, and at the same time can initiate an inflammatory response through the recruitment and activation of effector cells of the immune system (2). Thus, NFκB is a complex transcription factor regulating dual and opposing roles.
Prolonged activation of NFκB without resolution can lead to chronic inflammation and pathological conditions. Although acute inflammation alerts effector cells of potentially harmful stimuli, long-term cytokine expression can induce cell death through the extrinsic apoptotic pathway and lead to activation of pro-apoptotic signaling cascades, such as Jun N-terminal kinase (JNK), that normally is suppressed upon NFκB activation. Many pathological conditions, such as atherosclerosis, rheumatoid arthritis, inflammatory bowel disease, and cancer are linked to constitutive NFκB activation.
This review focuses on the ability of E2 to modulate cellular protection through its interaction with the inflammatory transcription factor NFκB and the stress-induced heat shock response. Recent evidence suggests that, in addition to the direct actions on NFκB, E2 may modulate inflammation and cell death through modulation of heat shock protein expression. The interaction between E2 and each of these factors will be reviewed, as will the ability of each component to modulate the activity of each other, as there is a complex interaction among heat shock factor (HSF)-1, NFκB, and the heat shock proteins (3).
Estrogen
Estrogen has a well-established role in reproductive function, but it also has widespread actions throughout the body, including in the skeletal, neurological, and cardiovascular systems. The effects of estrogen are mediated through the estrogen receptor (ER), which has two well-studied isomers, α and β, and one recently identified isomer, ER-X. ER subtype expression is tissue dependent. ER-α is most prevalent in the heart and liver, while ER-β is expressed more in the prostate and lung (4,5). ER has both genomic and nongenomic effects and is classically thought of as a nuclear receptor consisting of ligand-binding, DNA-binding, and transactivating domains (6). In the classical, genomic pathway, the ER exists as a monomer in the cytoplasm belonging to a multi-protein complex consisting of HSP 90, HSP 70, and immunophilins (Figure 1). HSP 90 is the dominant protein in this complex. HSP 90 binding to ER is essential to maintain ER’s conformation for binding of 17β-estradiol (7). Upon ligand binding, a conformational change is induced, the receptor translocates to the nucleus and dimerization occurs. Once in the nucleus, the complex is able to bind to estrogen response elements (ERE) directly or indirectly, through interaction with other DNA-bound transcription factors. After binding to DNA, ER both positively and negatively regulates target gene transcription.
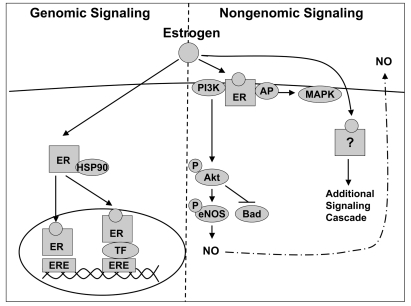
Figure 1.
Genomic and nongenomic E2 signaling. In the classical genomic pathway, E2 binds to cytosolic ER, and translocates to the nucleus where it binds directly to the ERE or binds to other transcription factors (TF) tethered to response elements and induces gene transcription. In addition, E2 is able to exert rapid cellular effects through several nongenomic mechanisms. E2 can bind to plasma membrane bound ER and directly activate signaling cascades, such as the PI3K/AKT pathway. Alternatively, upon binding E2, ER can recruit adaptor proteins, which activate signaling cascades. Lastly, E2 can bind non-membrane bound receptors and directly activate signaling pathways.
Nongenomic Effects of E2
Along with the genomic effects, E2 treatment can induce rapid cellular changes within minutes, and this response is termed non genomic as it does not entail transcription. The term “membrane initiated steroid signaling” (MISS) also has been used to describe the rapid effects of estrogen, as these signaling cascades largely originate from membrane bound receptors (8). The rapid effects of E2 occur via several mechanisms as outlined in Figure 1. ER localized to the plasma membrane may act coordinately with other membrane proteins, leading to initiation of signaling cascades. Nongenomic E2 signaling activates the phosphatidylinositol-3-OH kinase (PI3-K)/AKT pathway through direct interaction of ER with the p85α regulator subunit of PI3-K, leading to activation of endothelial nitric oxide synthase (eNOS) and inhibition of apoptosis through phosphorylation and degradation of the pro-apoptotic protein, Bad (9,10). A second mechanism involves recruitment of adaptor proteins to ER upon E2 binding, that can then go on to activate signaling cascades. Rapid mitogen-activated protein kinase (MAPK) activation by E2 has been found to be mediated through ER α recruitment of adaptor proteins, leading to activation of G protein-coupled receptor signaling (11). A recently proposed non-membrane-bound mechanism involves E2 binding to cytosolic receptors and inducing rapid cellular changes. E2 binding to the orphan G protein receptor 30 in the endoplasmic reticulum results in activation of G protein signaling (12,13).
Protective Effects of E2
Many of the effects of E2 are protective. In the cardiovascular system, E2 exerts powerful antioxidant effects, induces changes in lipid profiles by elevating high density lipoproteins, decreasing low density lipoproteins and activating eNOS leading to vasorelaxation. In addition to these effects, E2 alters the production of other vasoactive molecules, such as prostaglandins, all of which can influence the development of vascular disease (14). E2 inhibits the effects of inflammatory transcription factors, including AP-1 and NFκB, when activated, induces the expression of cytokines, inflammatory enzymes, adhesion molecules, and inflammatory receptors (15).
Estrogen and Sex Differences in Cardiovascular Disease
Further evidence for the beneficial effects of E2 are the male/female differences in cardioprotection in ischemia/reperfusion (I/R) and trauma-hemorrhage models. In I/R models, intact premenopausal female rodents compared with males have reduced injury as evidenced by smaller infarct size and greater recovery after I/R (16,17). Acute and/or chronic E2 supplementation provided protection both in isolated perfused hearts undergoing global ischemia and in in vivo ligation of the left anterior descending coronary artery (18,19). The exact mechanism is unknown, but it has been shown that females exhibit greater activation of AKT and protein kinase C (PKC) epsilon, and inhibition of either of these pathways led to the loss of protection in females, but had no effect on males (20). Both ER α and β have been shown to mediate the protective effects in I/R injury (21,22). Ovariectomy also negates cardioprotection in an I/R model of injury, and exogenous E2 treatment can restore protection (23). However, there are some studies that show no benefit of E2 in I/R injury (24,25). The discrepancies in protection could be due to species differences (rat versus dog and rabbit) or differences in estrogen treatment or cycle stage. Supporting this is Chaudry’s observation that proestrus female rats had improved cardiac function compared with males after resuscitation in a trauma-hemorrhage model. These effects were not seen during other phases of the estrus cycle, when estrogen levels are lower (26,27). E2 supplementation in ovariectomized females and male rats attenuated the depressed cardiovascular function associated with trauma-hemorrhage through activation of p38 MAPK and PI3-K/AKT (28,29).
Population Studies, E2, and Cardiovascular Disease
Although estrogen replacement therapy had been thought to reduce cardiovascular risk, prospective double blind controlled studies, such as the World Health Initiative (WHI) study, showed that hormone replacement therapy in postmenopausal women led not only to an increased risk of breast cancer, but also to increased prevalence of cardiovascular disease (30). Subsequent studies have shown that the risk for breast cancer was significantly greater for estrogen-progestin combinations than for other HRT regimens (31,32). The WHI trials have been criticized for the type of estrogen replacement used as well as the late addition of estrogen post-menopause; an average of 10 years elapsed between menopause and the initiation of estrogen treatment in these trials (33). The unexpected finding of increased cardiovascular disease in these double-blind controlled prospective trials has emphasized the need for further basic investigation to understand the complex properties of these powerful hormones.
NFκB
NFκB is a complex transcription factor and has been extensively reviewed elsewhere (34–36). There are five mammalian Rel/NFκB proteins: RelA (p65), c-Rel, RelB, NFκB1(p50/p105), and NFκB2(p52/p100). P50 and p52 are the proteolytic products of p105 and p100, respectively. In unstimulated cells, NFκB is cytoplasmic bound to an inhibitor of κB (IκB). NFκB activation is mediated primarily by IκB kinase (IKK) phosphorylation of IκBα, which triggers the ubiquitination and subsequent proteasome-mediated degradation of IκBα. The IKK complex has two catalytic subunits, IKKα and IKKβ, and two regulatory subunits, IKKγ/NEMO and ELKS (37,38). IKKβ is essential for NFκB activation in the canonical pathway. Destruction of IκB results in the formation of NFκB dimers and their translocation to the nucleus (39). Alternate pathways include the non-canonical IκB kinase (IKK) dependent pathways and p38-mediated IKK-independent mechanisms (40). Heterodimer formation is necessary for nuclear activation, as p50 and p52 lack nuclear localization sequences (NLS), while p65 and RelB lack DNA binding domains. Transcriptional co-activators, such as the oncogene B-cell lymphoma 3 (Bcl-3), have been shown to disrupt the inactive homodimers, allowing for trans-activator binding and subsequent induction of NFκB responsive genes (40,41).
Non-Canonical and Alternate Pathways
The non-canonical pathway is activated via the TNF receptor-associated factors binding receptor and leads to RelB and p52 dimers (42). Ligands for this pathway include lymphotoxin b, B-cell activating factor, and CD40. In this pathway, the p100 subunit of the p100/RelB protein complex is phosphorylated by IKKα homodimers that are activated by NFκB-inducing kinase (35). The phosphorylation of p100 leads to its proteolytic cleavage to form a p52/Rel B heterodimer, that can then translocate to the nucleus. The third mechanism of NFκB activation is independent of the IKK complex. Both UV light and the pX factor from the Hepatitis B virus are shown to activate NFκB in this manner. Casein kinase 2 (CK2), not IKK, phosphorylates IκBα, targeting it for ubiquitination and degradation (40). CK2 also constitutively degrades cytosolic IκBα. Full activation of NFκB in an IKK-independent manner requires phosphorylation of the Rel proteins by the PI3-K/AKT and p38 MAPK pathways (43,44).
NFκB transcription factors exert their effects by binding to κB sites and modulating the expression of numerous target genes that can induce both protective and inflammatory responses, contributing to the dichotomous nature of the NFκB response. Genes involved in proliferation, cell survival, and cell adhesion are induced, as are cytokines and chemokines involved in inflammation. The increase in cytokine production results in feedback amplification of NFκB activation, as certain cytokines, particularly tumor necrosis factor-α (TNF-α), are potent transcription factor activators. Sustained NFκB activation can lead to the development of chronic inflammation and has been linked to the highly proliferative and anti-apoptotic properties of cancers (45).
ER and NFκB
Many studies have addressed the inhibitory actions of ER on NFκB activity and its suppression of the induction of inflammatory genes by NFκB. The interaction between the ER and NFκB was studied first in osteoclasts, as the loss of estrogen in menopause leads to increased bone reabsorption and osteoporosis. Overexpression of ER decreased interleukin-6 (IL-6) production in osteoblasts and stromal cells, leading to decreased osteoclast maturation. ER inhibited IL-6 expression by binding to c-Rel and Rel A in a ligand-independent fashion, preventing the formation of active NFκB dimers (46,47). In endometrial cancer cells, ER co-localized with the p65 subunit at ER and NFκB response elements. NFκB activation was attenuated in cells treated with E2 and IL-1 (48). In vivo hepatic NFκB activation by an atherogenic diet in ovariectomized mice was blocked by estrogen replacement, and this was ER dependent (49).
The interaction of E2 and ER with other transcription factors is complex. In a human osteosarcoma cell line, TNF recruited unliganded ERα to the TNFα promoter, which led to the association of ERα with cJun and NFκB at the promoter site and the induction of TNF. E2 treatment led to the dissociation of ERα from the TNFα promoter and the recruitment of a co-repressor protein, glutamate receptor interaction protein-1 (GRIP-1) (50). Conversely, Hirano et al. found that nanomolar concentrations of E2 for 6 h enhanced NFκB activation with TNF-stimulation in both Jurkat and primary human T cells. The enhanced activation was in part due to ERβ association with the p65 subunit, leading to the recruitment of GRIP-1, that in this case served as a co-activator. ER interacts with other transcription factors as well. In the presence of E2, ERα displaced CRE-binding protein (CBP) from the NFκB-binding elements in the promoters of MCP-1 and IL-8 in the breast cancer cell line MCF7, yet another level of regulation of NFκB by E2 (51).
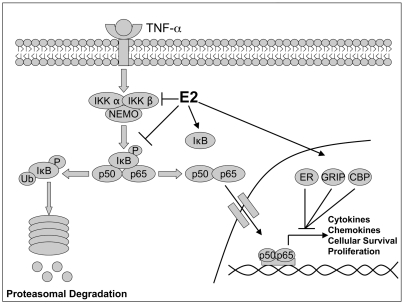
In addition to the direct inhibition of NFκB DNA binding, E2 alters NFκB activation through regulation of IKK activation and IκB expression. Pretreatment with E2 for 48 h in HUVECs inhibited LPS-induced IKK activation(52). Over-expression of ER led to increased IκBα expression upon E2 treatment in HeLa cells (53), and E2 treatment decreased phosphorylated IκBα levels in ischemic rats with constitutive NFκB activation (54). The inhibitory actions of E2 and the ER on NFκB are summarized in Figure 2.
Figure 2.
Interaction between E2 and NFκB. TNF-α induces NFκB activation via IKK phosphorylation of IκB, thereby allowing the p50/p65 heterodimer to translocate to the nucleus and induce gene transcription. E2 is able to modulate NFκB activation by suppressing IKK phosphorylation, suppressing IκB degradation, and increasing IκB expression. The recruitment of various co-repressors, such as ER, GRIP, and CBP, by E2 treatment also inhibits NFκB activity.
Timing is a critical factor. As discussed below, a very rapid activation of NFκB by E2 has been demonstrated in endothelial cells, cardiac myocytes, and splenocytes. The inhibition of NFκB by E2 that has been observed occurs much more slowly than this rapid response. Dai et al. reported that splenocytes from E2 supplemented rats had inhibition of nuclear translocation of p65, Rel-B, c-Rel, and p52; however, the p50 subunit displayed increased translocation and overall NFκB activity was increased as were downstream inducible genes in the E2 treated group. Upon further investigation, Bcl-3, a co-activator that can confer transactivation capability to the p50 or p52 subunit, was elevated with E2 treatment and displayed increased binding to NFκB regulated genes (24). In addition, we have found that human coronary artery endothelial cells (HCAEC) treated with nanomolar concentrations of E2 rapidly displayed increased p50 subunit activation (55). Similarly, a single dose of E2 in a trauma-hemorrhage model led to increased MAPK and NFκB activation mediated through ER α, and protected against resuscitation injury in male rats (56).
Heat Shock Proteins and the Stress Response
Heat Shock Proteins (HSP ) are a highly conserved family of proteins whose primary role is to protect cells by: i) refolding denatured proteins; ii) stabilizing macromolecules; and iii) targeting irreversibly denatured proteins for clearance. They also have a role in cell signaling. HSPs are divided into seven classes based on their molecular weight, amino acid sequence, and function: HSP 10, small HSPs, HSP 50, HSP 60, HSP 70, HSP 90, and HSP 100 (57). They are comprised of both constitutively expressed and inducible proteins, and their expression can be induced by a variety of stimuli including heat, ischemia, hypoxia, free radicals, and hypothermia (58,59). Heat shock proteins function not only as molecular chaperones, but also serve a protective role by inhibiting cellular damage, especially apoptosis.
Heat Shock Proteins and Apoptosis
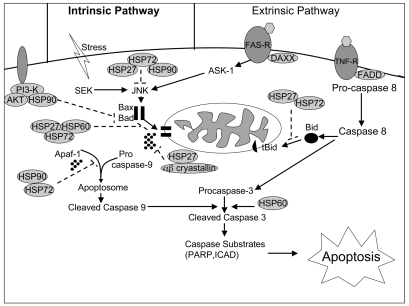
Apoptosis, or programmed cell death, is mediated through two pathways: the extrinsic and the intrinsic, as shown in Figure 3. In the extrinsic pathway, extra-cellular ligands, such as TNF-α, bind to the death receptor and induce the formation of a Death Inducing Signal Cascade (DISC). DISC formation leads to cleavage of procaspase 8 and initiates the cascade of effector caspases. The intrinsic pathway involves the loss of mitochondrial integrity through membrane permeabilization via the recruitment of Bax and Bad. This permeabilization leads to release of cytochrome c and formation of an apoptosome, cleavage of procaspase 9, and similar activation of effector caspases (60).
Figure 3.
Modulation of the extrinsic and intrinsic apoptotic signaling cascades by HSPs. HSP 27, 72, and 90 inhibit JNK activation through suppression of ASK-1 and SEK Kinase. HSP 27, 60, 72, and 90 can prevent Bid and Bax translocation to the mitochondria. Once mitochondrial permeability is compromised, αβ crystallin, HSP 27, 72, and 90 can prevent apoptosis by binding released cytochrome c and by preventing Apaf-1 oligomerization and recruitment of procaspase-9 for apoptosome formation. HSP 60 has both anti- and pro-apoptotic properties, binding Bax in the cytosol and accelerating maturation of caspase-3. Dashed lines indicate inhibitory effects.
A large body of work has addressed the inhibitory effect of HSPs on the intrinsic apoptotic pathway and is summarized in Figure 3. HSP 27, 72, and 90 prevent cell death by interfering with active apoptosome formation. HSP 27 and αβ-crystallin bind cytochrome c released from the mitochondria before it can associate with apoptotic protease activation factor-1 (Apaf-1) and recruit procaspase-9 (61,62). Both HSP 72 and HSP 90 complex with Apaf-1, and inhibit apoptosome formation (63,64). Overexpression of either HSP 27 or 72 inhibits the translocation of Bid and Bax to the mitochondrial membrane, inhibiting permeabilization and the release of cytochrome c (65,66). Similarly, HSP 60 binds Bax and Bak in the cytosol of cardiac myocytes, inhibiting apoptosis (67,68). Conversely, in a number of cancer cell lines, HSP 60 accelerates maturation of procaspase 3, and thus is pro-apoptotic (58,69,70). HSP 90 binds AKT and maintains its activity, and also phosphorylates and inactivates the pro-apoptotic protein, Bad (71,72). Further evidence of the anti-apoptotic role of the HSPs is that knockdown of HSF1 expression increased JNK-mediated cell death and decreased expression of the anti-apoptotic Bcl-2 family member, Bcl-XL (73). HSP 27, 72, and 90 all inhibit JNK-mediated cell death by suppressing phosphorylation directly or by inhibiting the upstream kinases (72,74). Thus, the HSPs are overall anti-apoptotic and protective of the cell.
Heat Shock Factors (HSF): The Regulation of HSP Expression
The heat shock response is primarily a protective response to stress and injury. Heat shock proteins originally were described in heat-shocked drosophila, but really are an ubiquitous set of protective proteins. Heat shock gene expression is predominately under the control of the transcription factor, heat shock factor (HSF), for which there are three mammalian isoforms, HSF-1, 2, and 4, and one avian isoform, HSF-3 (75). HSF-1 is the classical heat shock transcription factor, as it is responsible for the induction of heat shock genes in response to stress and for the development of thermotolerance. HSF-1 knockout results in defects in fertility, high levels of TNF-α, and failure to mount a heat shock response (76). However, HSF-1 knockout mice also are protected from tumor formation (77). HSF-2 has a role during development and differentiation, and its greatest activation is observed during embryogenesis and spermatogenesis. HSF-2 null mice are viable, but controversy exists as to whether they display brain abnormalities and defects in fertility (78,79). Recent evidence also suggests that HSF-2 may contribute to basal HSP 27 and 90 expression during cellular proliferation (80). The functions of HSF-4 remain to be elucidated, but it has been shown to act as a repressor of HSF-1 upon heat shock by binding to the heat shock element (HSE) and preventing nuclear body formation and subsequent HSP expression (81). It has been suggested that HSF-4 is a pseudo-transcription factor, as it lacks the carboxyl terminal repeat necessary for trimerization shared by HSF-1, 2, and 3 (82).
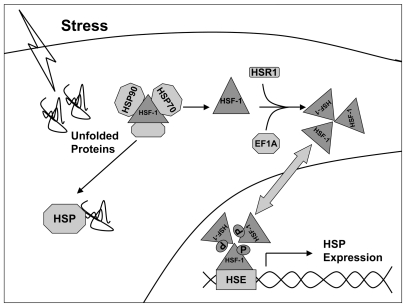
HSF normally resides in the cytoplasm as a monomer, and associates with a multi-protein chaperone complex. HSF-1 has been found to associate with multiple co-repressor proteins including immunophilin (FKBP52), p23, Ral1 Binding Protein, HSF Inhibitor, and, most importantly, HSP 70 and 90. Previous work in our lab and others has demonstrated that treatment with geldanamycin, an HSP 90 inhibitor, resulted in dissociation of the multi-protein HSP 90 complex, releasing HSF-1, followed by increased expression of HSP 72 (83,84). Following heat stress, HSF-1 dissociates from the complexes and forms a trimer by binding to other unbound monomeric HSF-1 proteins. Recent work by Shamovsky et al. suggests that HSF-1 trimerization requires the recruitment of the translational elongation factor, eEF1A, and a large noncoding RNA termed HSR1 (heat shock RNA 1). Loss of either reduced the ability of HSF-1 to trimerize, translocate to the nucleus, and upregulate HSP transcription after heat shock (85).
Overexpression of HSF-1 in mammalian cells leads to spontaneous binding to the HSE in the absence of heat shock, but, under normal conditions, HSF-1 is in a multi-protein complex, and heat and other stresses are necessary for its activation (75). It has been proposed that there is an equilibrium between HSP 90 and the proteins it binds, including HSF-1, other HSPs, the intracellular hormone receptors, and src (83). One theory for how heat shock leads to activation of HSF-1 and induction of HSPs, is that heat creates an accumulation of unfolded proteins within the cell, which, when sensed by cellular machinery, causes molecular chaperones to bind preferentially to the unfolded proteins and release HSF-1 (86). Free HSF-1 then trimerizes, is phosphorylated, and translocates to the nucleus where it forms nuclear bodies and binds to the heat shock element (HSE) as outlined in Figure 4. Translocation and activation are highly regulated through multiple serine sites on HSF-1. JNK and glycogen synthase kinase phosphorylate serine 303 and 307 and prevent nuclear translocation and/or HSF-1/HSE binding (75,87,88). However, it also has been observed that phosphorylation at serines 230 and 326 is necessary for HSP expression upon heat shock. Mutation of either residue to alanine led to decreased HSP expression upon heat shock, but did not result in impairment of HSF-1/HSE binding (89,90). Thus, the translocation of HSF-1 and the induction of HSP genes by stress is a multi-step process that is regulated tightly.
Figure 4.
Activation of HSF-1 and HSP expression. HSF-1 normally resides in the cytosol in a multi-protein complex with HSP 72 and 90. Upon heat shock, HSPs dissociate from the multi-protein complexes, freeing HSF-1. Heat shock RNA (HSR) and elongation factor 1 (eEF1α) are recruited by HSF-1 allowing the transcription factor to trimerize. Upon trimerization, HSF-1 translocates to the nucleus, binds to HSEs and is phosphorylated allowing for HSP gene transcription.
HSF-1 and NFκB
Knockdown of HSF-1 in vascular smooth muscle cells resulted in the loss of HSP expression and greater NFκB activation upon angiotensin II treatment (91). In addition to the exacerbation of HSF-1 knockdown on NFκB activation, additional inflammatory transcription factors, such as AP-1, demonstrate higher activity following knockdown and challenge (91). Increased activation also is observed in the lungs from transgenic HSF-1 −/− mice treated with cadmium to induce NFκB (92). Xiao et al. (76) investigated the effects of sepsis on HSF-1 −/− mice using LPS administration. HSF-1 null mice had reduced survival (35% versus 60% in WT controls) and increased plasma TNF-α. Over-expression of HSF-1 in LPS-treated macrophages attenuated TNF-α transcription, while heat shock in itself shortens the duration of TNF-α expression (93). Thus, HSF-1 has broad anti-inflammatory properties.
E2 and Heat Shock Protein Expression
E2 treatment, both in vivo and in vitro, leads to increased expression of HSF-1, HSP 72, and HSP 90 in female cardiac myocytes and uterine tissue (83,94–97). In addition, E2 stimulates the phosphorylation of HSP 27 and αβ-crystallin via p38 MAP kinase, essential for the protective properties of these proteins (28). Further evidence of E2 increasing expression of HSPs are the observations that intact females have higher levels of HSP 72 than males, both basally and following ischemia/reperfusion, in cardiac and renal tissue (95,98). Reduction of female rat cardiac HSP 72 expression to that of males occurred 9 weeks after ovariectomy, suggesting the increase in HSP 72 is indirectly due to estrogen. Basal levels of HSP 27 and 90 were found to be decreased in female heart tissue compared with males, suggesting that not all HSPs are upregulated by E2 (99). Interestingly, the inbred Fischer rats did not show the same male/female difference in cardiac levels of HSP 72, while inbred Norway Brown rats did (AA Knowlton and J Stallone, unpublished data).
Although females express higher basal levels of HSP 72 in cardiac and liver tissue, evidence suggests that males may be able to express higher HSP levels after certain stressors. Studies by Paroo et al. (100,101) found that exercise induced greater increases in HSP 32 and 72 in males than in females, both in skeletal muscle and in cardiac tissue. Ovariectomy increased HSP expression above intact females, and could be reversed by in vivo E2 treatment; however, the rat age and the timing of ovariectomy and subsequent studies was not clear. Using a tail shock model, Nickerson et al. (102) found that males expressed higher post shock levels of HSP 72 in the liver, pituitary gland, and mesenteric lymph node compared with intact Fischer 344 female rats of unknown age; while no sex differences were observed in the adrenal gland, spleen, or heart. Further work needs to be done to discern why certain stresses may cause elevated HSP responses in males compared with females.
A problem in the field of estrogen and HSP expression is the variation seen in animal models. Many studies show decreased levels of HSP 72 upon ovariectomy, which can be restored by E2 replacement, or show females expressing higher endogenous levels of HSP 72 (94,95,103,104). However, other studies have reported that ovariectomy has no effect on HSP expression and that sex differences are not present (102,105). Discrepancies between studies on the effects of estrogen HSP expression could be due partly to differences in ages of animals used, or duration, preparation, and concentrations of E2 given (Table 1). It is important that appropriate-aged models be used, as sexually immature rats will not have the same response as adult animals. For example, studies using estrogen replacement in sexually immature rats between 8 to 10 weeks of age demonstrate less HSP 72 response than those using older SD rats (104,105). Increased duration of E2 replacement in ovariectomized animals also increased HSP 72 expression in ovariectomized rats (104,106).
Table 1.
Summary of the animal models used to assess the effects of estrogen on HSP expression. Species, strain, age, and length of time of E2 replacement following ovariectomy, as well as the reported change in HSP 72 expression are reported.
| Species | Strain | Age | Ovxa to Study | HSP 72 | |
|---|---|---|---|---|---|
| Bupha-Intr et al. 2004 (103) | Rat | SD | 8–9 weeks | 9 weeks | 20% decrease HSP 72 with ovx by Western |
| Fekete et al. 2006 (98) | Rat | N/A | N/A | Intact | F > M post Ischemia/Reperfusion |
| Nickerson et al. 2006 (102) | Rat | F344 | N/A | Intact | Female 0.46 versus male 0.4 pg/μg HSP 72 ELISA |
| Papacontantinou et al. 2003 (94) | Mouse | N/A | N/A | 4 days SC E2 0.02mg/mL | Ovx 66% decrease |
| Paroo et al. 2002 (101) | Rat | SD | N/A | Intact | Estrogen blocked exercise–associated increase HSP 72 |
| Shinohara et al. 2004 (105) | Rat | SD | 10 weeks | 1 week | Ovx no effect HSP 72 |
| Thawornkaiwong et al. 2007 (104) | Rat | SD | 8–9 weeks | 10 weeks SC E2 | Ovx 27% decrease in HSP 72 |
| Voss et al. 2003 (95) | Rat | SD | 12–16 weeks | 9 weeks | Female 29 pg/μg at peak estrus versus male 14 pg/μg; ovx 9 weeks to male |
Ovariectomized
Early E2 Treatment and Protection
Pretreatment with E2 in a trauma/hemorrhagic shock rat model prevented decreases in the cardiac expression of HSP 60 and 90, and also increased expression of HSP 32 (heme oxygenase-1) and 72 compared with shams upon resuscitation. Similar upregulation of HO-1 expression using the same model have been seen in the liver, intestine, and lung following E2 supplementation and is mediated by AKT activation (107). Activation of ER β, but not ER α, led to downstream activation of HSF-1 and increased HSP expression (108,109). Using a renal I/R model, Fekete et al. (98) found that males exhibited decreased renal function compared with intact females as assessed by higher levels of blood urea nitrogen and creatinine. Females were found to have greater renal HSP 72 expression both pre- and post-ischemia and decreased internalization of membrane bound Na-K-ATPase.
Acute Effects: E2, NFκB and HSPs
Previously, we have reported an interaction among E2, NFκB, and the HSP response. In male cardiac myocytes, 100 nM E2 increased HSP 72 expression (97). Treatment of female cardiac myocytes with E2 (10 uM) led to rapid activation of the p50 subunit of NFκB, activation of HSF-1 by 3 h, and increased HSP 72 and 90 expression. E2 treatment protected adult cardiac myocytes from hypoxia/reoxygenation. Inhibition of NFκB, but not HSF-1, led to attenuation of the cyto-protective effects after H/R, even though inhibition of either transcription factor negated the effects of E2 on HSP 72 expression (97). This suggests that other protective proteins are induced, and that the protective response to E2 is multi-faceted. Similar effects were seen in male HCAEC where 100 nM E2 induced activation of NFκB and HSF-1, followed by increased expression of HSP 72 and HPS90 (55). Activation of NFκB occurred within 5 to 15 min and lasted up to 1 h. NFκB was activated rapidly by as little as 1 nM E2 in endothelial cells, reflecting increased sensitivity to E2. Most work has focused on the long-term effects of E2. Thus, further work needs to be done to mechanistically understand how E2 activates NFκB and HSF-1 and which inducible genes are responsible for conferring protection against hypoxia/reoxygenation.
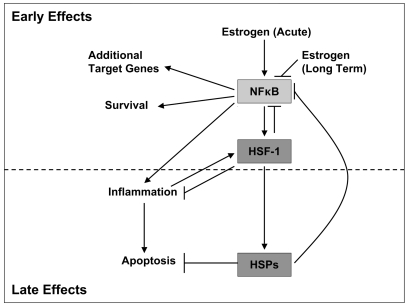
The Stress Response and NFκB—Late Effects
Many lines of evidence suggest that activation of HSF-1 and subsequent HSP expression suppresses NFκB activation. Heat shock has been shown to inhibit IKK activation, and to increase IκB-α levels both by inhibition of its phosphorylation and degradation and by increased expression (110–112). Furthermore, phosphorylation of HSP 27 by p38 leads to association with IKK in HeLa cells upon TNF-α treatment, and suppression of NFκB activity (113). Other heat shock proteins, such as HSP 72, have been shown to bind to both the IκB-α and the p65 subunit of the NFκB complex, inhibiting NFκB activation and downstream production of cytokines and inducible nitric oxide synthase (110,114). The acute and chronic actions of E2 on NFκB and the HSR are summarized in Figure 5.
Figure 5.
Diagram illustrating key interactions among E2, NFκB, HSF-1, and heat shock proteins (HSPs). Acute E2 treatment leads to NFκB activation and induction of genes responsible for cell survival and inflammation. NFκB activates HSF-1, which then induces HSPs. HSF-1 activation can suppress expression of inflammatory cytokines, such as TNF-α directly, or indirectly inhibit apoptosis and NFκB activation through HSP expression.
CONCLUSION
Although the actions of E2 have been studied extensively, there are still many properties that we do not understand. Recent research has shown that E2 modulates NFκB activity. There are early effects, with rapid nongenomic activation of NFκB that are protective. A later response to E2 results in the inhibition of NFκB. This may be mediated by activation of HSF-1 and HSP expression, but this has not been proven. The protective effects of estrogen on NFκB occur through both genomic and nongenomic signaling cascades, which have different effects on NFκB. Nongenomic E2 signaling activates NFκB, the heat shock response, and increases cellular resistance to injury. Heat shock protein expression leads to inhibition of apoptosis, inflammation, and suppresses NFκB activation. The negative feedback by the heat shock response attenuates the deleterious effects linked with chronic NFκB activation. Genomic E2 signaling acts as a further checkpoint to inhibit prolonged NFκB activity through the nuclear recruitment of ER and other cofactors to NFκB response elements. The complexity of the interaction among E2, NFκB, and the heat shock response underscores how much remains to be understood about E2. Further work is needed to determine the mechanism by which E2 activates NFκB and HSF-1, and whether other pathways are involved in this interaction.
ACKNOWLEDGMENTS
Supported by NIH HL077281 (AAK), HL079071(AAK), the Department of Veterans Affairs (AAK), and the American Heart Association Western States Affiliate (JPS).
Footnotes
Online address: http://www.molmed.org
REFERENCES
- 1.Bubici C, Papa S, Dean K, Franzoso G. Mutual cross-talk between reactive oxygen species and nuclear factor-kappa B: molecular basis and biological significance. Oncogene. 2006;25:6731–48. doi: 10.1038/sj.onc.1209936. [DOI] [PubMed] [Google Scholar]
- 2.Hayden MS, West AP, Ghosh S. NF-kappa B and the immune response. Oncogene. 2006;25:6758–80. doi: 10.1038/sj.onc.1209943. [DOI] [PubMed] [Google Scholar]
- 3.Knowlton AA. NF kappa B, heat shock proteins, HSF-1, and inflammation. Cardiovasc Res. 2006;69:7–8. doi: 10.1016/j.cardiores.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 4.Yu HP, et al. Tissue-specific expression of estrogen receptors and their role in the regulation of neutrophil infiltration in various organs following trauma-hemorrhage. J Leukoc Biol. 2006;79:963–70. doi: 10.1189/jlb.1005596. [DOI] [PubMed] [Google Scholar]
- 5.Couse JF, Lindzey J, Grandien K, Gustafsson JA, Korach KS. Tissue distribution and quantitative analysis of estrogen receptor-alpha (ER alpha) and estrogen receptor-beta (ER beta) messenger ribonucleic acid in the wild-type and ER alpha-knockout mouse. Endocrinology. 1997;138:4613–21. doi: 10.1210/endo.138.11.5496. [DOI] [PubMed] [Google Scholar]
- 6.Kalaitzidis D, Gilmore TD. Transcription factor cross-talk: the estrogen receptor and NF-kappa B. Trends Endocrinol Metab. 2005;16:46–52. doi: 10.1016/j.tem.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 7.Segnitz B, Gehring U. The function of steroid hormone receptors Is inhibited by the hsp90-specific compound geldanamycin. J Biol Chem. 1997;272:18694–18701. doi: 10.1074/jbc.272.30.18694. [DOI] [PubMed] [Google Scholar]
- 8.Hammes SR, Levin ER. Extranuclear steroid receptors: nature and actions. Endocr Rev. 2007;28:726–41. doi: 10.1210/er.2007-0022. [DOI] [PubMed] [Google Scholar]
- 9.Haynes MP, et al. Membrane estrogen receptor engagement activates endothelial nitric oxide synthase via the PI3-kinase-Akt pathway in human endothelial cells. Circ Res. 2000;87:677–82. doi: 10.1161/01.res.87.8.677. [DOI] [PubMed] [Google Scholar]
- 10.Patten RD, et al. 17beta-estradiol reduces cardiomyocyte apoptosis in vivo and in vitro via activation of phospho-Inositide-3 inase/Akt signaling. Circ Res. 2004;95:692–9. doi: 10.1161/01.RES.0000144126.57786.89. [DOI] [PubMed] [Google Scholar]
- 11.Song RX, Zhang Z, Sante RJ. Estrogen rapid action via protein complex formation involving ER alpha and Src. Trends Endocrinol Metab. 2005;16:347–53. doi: 10.1016/j.tem.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 12.Hewitt SC, Deroo BJ, Korach KS. Signal Transduction. A new mediator for an old hormone? Science. 2005;307:1572–3. doi: 10.1126/science.1110345. [DOI] [PubMed] [Google Scholar]
- 13.Revankar CM, Cimino DF, Sklar LA, Arterburn JB, Prossnitz ER. A transmembrane intracellular estrogen receptor mediates rapid cell signaling. Science. 2005;307:1625–1630. doi: 10.1126/science.1106943. [DOI] [PubMed] [Google Scholar]
- 14.Mendelsohn ME, Karas RH. The protective effects of estrogen on the cardiovascular system. N Engl J Med. 1999;340:1801–11. doi: 10.1056/NEJM199906103402306. [DOI] [PubMed] [Google Scholar]
- 15.Barnes PJ. Molecular mechanisms of corticosteroids in allergic diseases. Allergy. 2001;56:928–36. doi: 10.1034/j.1398-9995.2001.00001.x. [DOI] [PubMed] [Google Scholar]
- 16.Murphy E, Steenbergen C. Gender-based differences in mechanisms of protection in myocardial ischemia-reperfusion injury. Cardiovasc Res. 2007;75:478–86. doi: 10.1016/j.cardiores.2007.03.025. [DOI] [PubMed] [Google Scholar]
- 17.Bae S, Zhang L. Gender differences in cardioprotection against ischemia/reperfusion injury in adult rat hearts: focus on Akt and protein kinase C signaling. J Pharmacol Exp Ther. 2005;315:1125–35. doi: 10.1124/jpet.105.090803. [DOI] [PubMed] [Google Scholar]
- 18.Meldrum DR. Estrogen increases protective proteins following trauma and hemorrhage. Am J Physiol Regul Integr Comp Physiol. 2006;290:R809–11. doi: 10.1152/ajpregu.00802.2005. [DOI] [PubMed] [Google Scholar]
- 19.Kher A, et al. Sex differences in the myocardial inflammatory response to acute injury. Shock. 2005;23:1–10. doi: 10.1097/01.shk.0000148055.12387.15. [DOI] [PubMed] [Google Scholar]
- 20.Bae S, Zhang L. Gender differences in cardioprotection against ischemia/reperfusion injury in adult rat hearts: focus on Akt and protein Kinase C signaling. J Pharmacol Exp Ther. 2005;315:1125–35. doi: 10.1124/jpet.105.090803. [DOI] [PubMed] [Google Scholar]
- 21.Gabel SA, et al. Estrogen receptor beta mediates gender differences in ischemia/reperfusion injury. J Mol Cell Cardiol. 2005;38:289–97. doi: 10.1016/j.yjmcc.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 22.Wang M, Crisostomo P, Wairiuko GM, Meldrum DR. Estrogen receptor-alpha mediates acute myocardial protection in females. Am J Physiol Heart Circ Physiol. 2006;290:H2204–9. doi: 10.1152/ajpheart.01219.2005. [DOI] [PubMed] [Google Scholar]
- 23.Sbarouni E, Iliodromitis EK, Bofilis E, Kyriakides ZS, Kremastinos DT. Short-term estrogen reduces myocardial infarct size in oophorectomized female rabbits in a dose-dependent manner. Cardiovasc Drugs Ther. 1998;12:457–62. doi: 10.1023/a:1007750015372. [DOI] [PubMed] [Google Scholar]
- 24.Przyklenk K, Ovize M, Bauer B, Kloner RA. Gender does not influence acute myocardial infarction in adult dogs. Am Heart J. 1995;129:1108–13. doi: 10.1016/0002-8703(95)90390-9. [DOI] [PubMed] [Google Scholar]
- 25.McCully JD, et al. Age- and gender-related differences in ischemia/reperfusion injury and cardioprotection: effects of diazoxide. Ann Thorac Surg. 2006;82:117–23. doi: 10.1016/j.athoracsur.2006.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jarrar D, Wang P, Cioffi WG, Bland KI, Chaudry IH. The female reproductive cycle is an important variable in the response to trauma-hemorrhage. Am J Physiol Heart Circ Physiol. 2000;279:H1015–21. doi: 10.1152/ajpheart.2000.279.3.H1015. [DOI] [PubMed] [Google Scholar]
- 27.Yang S, et al. Estrus cycle: influence on cardiac function following trauma-hemorrhage. Am J Physiol Heart Circ Physiol. 2006;291:H2807–15. doi: 10.1152/ajpheart.00195.2006. [DOI] [PubMed] [Google Scholar]
- 28.Hsu JT, et al. Role of p38 mitogen-activated protein kinase pathway in estrogen-mediated cardioprotection following trauma-hemorrhage. Am J Physiol Heart Circ Physiol. 2007;292:H2982–7. doi: 10.1152/ajpheart.01303.2006. [DOI] [PubMed] [Google Scholar]
- 29.Yu HP, et al. The PI3K/Akt pathway mediates the nongenomic cardioprotective effects of estrogen following trauma-hemorrhage. Ann Surg. 2007;245:971–7. doi: 10.1097/01.sla.0000254417.15591.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nelson HD, Humphrey LL, Nygren P, Teutsch SM, Allan JD. Postmenopausal hormone replacement therapy: scientific review. JAMA. 2002;288:872–81. doi: 10.1001/jama.288.7.872. [DOI] [PubMed] [Google Scholar]
- 31.Beral V. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003;362:419–27. doi: 10.1016/s0140-6736(03)14065-2. [DOI] [PubMed] [Google Scholar]
- 32.Hulley SB, Grady D. The WHI estrogen-alone trial—do things look any better? JAMA. 2004;291:1769–1771. doi: 10.1001/jama.291.14.1769. [DOI] [PubMed] [Google Scholar]
- 33.Turgeon JL, McDonnell DP, Martin KA, Wise PM. Hormone therapy: physiological complexity belies therapeutic simplicity. Science. 2004;304:1269–73. doi: 10.1126/science.1096725. [DOI] [PubMed] [Google Scholar]
- 34.Hoffmann A, Baltimore D. Circuitry of nuclear factor kappa B signaling. Immunol Rev. 2006;210:171–86. doi: 10.1111/j.0105-2896.2006.00375.x. [DOI] [PubMed] [Google Scholar]
- 35.Karin M, Lin A. NF-kappa B at the crossroads of life and death. Nat Immunol. 2002;3:221–7. doi: 10.1038/ni0302-221. [DOI] [PubMed] [Google Scholar]
- 36.Jones WK, Brown M, Ren X, He S, McGuinness M. NF-kappa B as an integrator of diverse signaling pathways: the heart of myocardial signaling? Cardiovasc Toxicol. 2003;3:229–54. doi: 10.1385/ct:3:3:229. [DOI] [PubMed] [Google Scholar]
- 37.Sigala JLD, et al. Activation of transcription factor NF-kappa B requires ELKS, an I kappa B kinase regulatory subunit. Science. 2004;304:1963–7. doi: 10.1126/science.1098387. [DOI] [PubMed] [Google Scholar]
- 38.Ghosh S, Karin M. Missing pieces in the NF-kappa B puzzle. Cell. 2002;109:S81–96. doi: 10.1016/s0092-8674(02)00703-1. [DOI] [PubMed] [Google Scholar]
- 39.Baldwin AS., Jr The NF-kappa B and I kappa B proteins: new discoveries and insights. Annu Rev Immunol. 1996;14:649–83. doi: 10.1146/annurev.immunol.14.1.649. [DOI] [PubMed] [Google Scholar]
- 40.Kato T, Jr, Delhase M, Hoffmann A, Karin M. CK2 Is a C-terminal I kappa B kinase responsible for NF-kappa B activation during the UV response. Mol Cell. 2003;12:829–39. doi: 10.1016/s1097-2765(03)00358-7. [DOI] [PubMed] [Google Scholar]
- 41.Dai R, Phillips RA, Ahmed SA. Despite inhibition of nuclear localization of NF-kappa B p65, c-Rel, and RelB, 17-beta estradiol up-regulates NF-kappa B signaling in mouse splenocytes: the potential role of Bcl-3. J Immunol. 2007;179:1776–83. doi: 10.4049/jimmunol.179.3.1776. [DOI] [PubMed] [Google Scholar]
- 42.Scheidereit C. I kappa B kinase complexes: gateways to NF-kappa B activation and transcription. Oncogene. 2006;25:6685–705. doi: 10.1038/sj.onc.1209934. [DOI] [PubMed] [Google Scholar]
- 43.Madrid LV, Mayo MW, Reuther JY, Baldwin AS., Jr Akt stimulates the transactivation potential of the RelA/p65 subunit of NF-kappa B through utilization of the I kappa B kinase and activation of the mitogen-activated protein kinase p38. J Biol Chem. 2001;276:18934–40. doi: 10.1074/jbc.M101103200. [DOI] [PubMed] [Google Scholar]
- 44.Pando MP, Verma IM. Signal-dependent and -independent degradation of free and NF-kappa B-bound I kappa B alpha. J Biol Chem. 2000;275:21278–86. doi: 10.1074/jbc.M002532200. [DOI] [PubMed] [Google Scholar]
- 45.Karin M. Nuclear factor-kappa B in cancer development and progression. Nature. 2006;441:431–6. doi: 10.1038/nature04870. [DOI] [PubMed] [Google Scholar]
- 46.Stein B, Yang MX. Repression of the interleukin-6 promoter by estrogen receptor is mediated by NF-kappa B and C/EBP beta. Mol Cell Biol. 1995;15:4971–9. doi: 10.1128/mcb.15.9.4971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Galien R, Garcia T. Estrogen receptor impairs interleukin-6 expression by preventing protein binding on the NF-kappa B site. Nucl Acids Res. 1997;25:2424–9. doi: 10.1093/nar/25.12.2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Feldman I, Feldman GM, Mobarak C, Dunkelberg JC, Leslie KK. Identification of proteins within the nuclear factor-kappa B transcriptional complex including estrogen receptor-alpha. Am J Obstet Gynecol. 2007;196:394.e1–394.e13. doi: 10.1016/j.ajog.2006.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Evans MJ, Eckert A, Lai K, Adelman SJ, Harnish DC. Reciprocal antagonism between estrogen receptor and NF-kappa B activity in vivo. Circ Res. 2001;89:823–30. doi: 10.1161/hh2101.098543. [DOI] [PubMed] [Google Scholar]
- 50.Cvoro A, et al. Distinct roles of unliganded and liganded estrogen receptors in transcriptional repression. Mol Cell. 2006;21:555–64. doi: 10.1016/j.molcel.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 51.Nettles KW, et al. CBP is a dosage dependent regulator of NF{kappa}B suppression by the estrogen receptor. Mol Endocrinol. 2007 doi: 10.1210/me.2007-0324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Simoncini T, et al. Estrogens and glucocorticoids inhibit endothelial vascular cell adhesion molecule-1 expression by different transcriptional mechanisms. Circ Res. 2000;87:19–25. doi: 10.1161/01.res.87.1.19. [DOI] [PubMed] [Google Scholar]
- 53.Dodel RC, Du Y, Bales KR, Gao F, Paul SM. Sodium salicylate and 17beta-estradiol attenuate nuclear transcription factor NF-kappa B translocation in cultured rat astroglial cultures following exposure to amyloid A beta(1-40) and lipopolysaccharides. J Neurochem. 1999;73:1453–60. doi: 10.1046/j.1471-4159.1999.0731453.x. [DOI] [PubMed] [Google Scholar]
- 54.Wen Y, et al. Estrogen attenuates nuclear factor-kappa B activation induced by transient cerebral ischemia. Brain Res. 2004;1008:147–54. doi: 10.1016/j.brainres.2004.02.019. [DOI] [PubMed] [Google Scholar]
- 55.Hamilton KL, Mbai FN, Gupta S, Knowlton AA. Estrogen, heat shock proteins, and NF kappa B in human vascular endothelium. Arterioscler Thromb Vasc Biol. 2004;24:1628–33. doi: 10.1161/01.ATV.0000137188.76195.fb. [DOI] [PubMed] [Google Scholar]
- 56.Suzuki T, et al. Salutary effects of 17beta-estradiol on T-cell signaling and cytokine production after trauma-hemorrhage are mediated primarily via estrogen receptor-alpha. Am J Physiol Cell Physiol. 2007;292:C2103–11. doi: 10.1152/ajpcell.00488.2006. [DOI] [PubMed] [Google Scholar]
- 57.Jolly C, Morimoto RI. Role of the heat shock response and molecular chaperones in oncogenesis and cell death. J Natl Cancer Inst. 2000;92:1564–72. doi: 10.1093/jnci/92.19.1564. [DOI] [PubMed] [Google Scholar]
- 58.Kregel KC. Molecular biology of thermoregulation: invited review: Heat shock proteins: modifying factors in physiological stress responses and acquired thermotolerance. J Appl Physiol. 2002;92:2177–86. doi: 10.1152/japplphysiol.01267.2001. [DOI] [PubMed] [Google Scholar]
- 59.Gupta S, Knowlton AA. HSP 60, Bax, apoptosis and the heart. J Cell Mol Med. 2005;9:51–8. doi: 10.1111/j.1582-4934.2005.tb00336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Riedl SJ, Salvesen GS. The apoptosome: signaling platform of cell death. Nat Rev Mol Cell Biol. 2007;8:405–13. doi: 10.1038/nrm2153. [DOI] [PubMed] [Google Scholar]
- 61.Bruey JM, et al. Hsp27 negatively regulates cell death by interacting with cytochrome c. Nat Cell Biol. 2000;2:645–52. doi: 10.1038/35023595. [DOI] [PubMed] [Google Scholar]
- 62.Concannon CG, Orrenius S, Samali A. Hsp27 inhibits cytochrome c-mediated caspase activation by sequestering both procaspase-3 and cytochrome c. Gene Expr. 2001;9:195–201. doi: 10.3727/000000001783992605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Beere HM, et al. Heat-shock protein 70 inhibits apoptosis by preventing recruitment of procaspase-9 to the Apaf-1 apoptosome. Nat Cell Biol. 2000;2:469–475. doi: 10.1038/35019501. [DOI] [PubMed] [Google Scholar]
- 64.Pandey P, et al. Negative regulation of cytochrome c-mediated oligomerization of Apaf-1 and activation of procaspase-9 by heat shock protein 90. EMBO J. 2000;19:4310–22. doi: 10.1093/emboj/19.16.4310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bivik C, Rosdahl I, Ollinger K. Hsp70 protects against UVB induced apoptosis by preventing release of cathepsins and cytochrome c in human melanocytes. Carcinogenesis. 2007;28:537–44. doi: 10.1093/carcin/bgl152. [DOI] [PubMed] [Google Scholar]
- 66.Stankiewicz AR, Lachapelle G, Foo CPZ, Radicioni SM, Mosser DD. Hsp70 inhibits heat-induced apoptosis upstream of mitochondria by preventing Bax translocation. J Biol Chem. 2005;280:38729–39. doi: 10.1074/jbc.M509497200. [DOI] [PubMed] [Google Scholar]
- 67.Kirchhoff SR, Gupta S, Knowlton AA. Cytosolic heat shock protein 60, apoptosis, and myocardial injury. Circulation. 2002;105:2899–904. doi: 10.1161/01.cir.0000019403.35847.23. [DOI] [PubMed] [Google Scholar]
- 68.Shan YX, et al. Hsp10 and Hsp60 modulate Bcl-2 family and mitochondria apoptosis signaling induced by doxorubicin in cardiac muscle cells. J Mol Cell Cardiol. 2003;35:1135–43. doi: 10.1016/s0022-2828(03)00229-3. [DOI] [PubMed] [Google Scholar]
- 69.Xanthoudakis S, et al. Hsp60 accelerates the maturation of pro-caspase-3 by upstream activator proteases during apoptosis. EMBO J. 1999;18:2049–56. doi: 10.1093/emboj/18.8.2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chandra D, Choy G, Tang DG. Cytosolic accumulation of HSP60 during apoptosis with or without apparent mitochondrial release: evidence that its pro-apoptotic or pro-survival functions involve differential interactions with caspase-3. J Biol Chem. 2007;282:31289–301. doi: 10.1074/jbc.M702777200. [DOI] [PubMed] [Google Scholar]
- 71.Sato S, Fujita N, Tsuruo T. Modulation of Akt kinase activity by binding to Hsp90. Proc Natl Acad Sci U S A. 2000;97:10832–7. doi: 10.1073/pnas.170276797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhang R, et al. Hsp90-Akt phosphorylates ASK1 and inhibits ASK1-mediated apoptosis. Oncogene. 2005;24:3954–63. doi: 10.1038/sj.onc.1208548. [DOI] [PubMed] [Google Scholar]
- 73.Jacobs AT, Marnett LJ. Heat shock factor 1 attenuates 4-hydroxynonenal-mediated apoptosis: critical role for heat shock protein 70 induction and stabilization of Bcl-XL. J Biol Chem. 2007;282:33412–20. doi: 10.1074/jbc.M706799200. [DOI] [PubMed] [Google Scholar]
- 74.Meriin AB, et al. Protein-damaging stresses activate c-Jun N-terminal kinase via inhibition of its dephosphorylation: a novel pathway controlled by HSP72. Mol Cell Biol. 1999;19:2547–55. doi: 10.1128/mcb.19.4.2547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pirkkala L, Nykanen P, Sistonen L. Roles of the heat shock transcription factors in regulation of the heat shock response and beyond. FASEB J. 2001;15:1118–31. doi: 10.1096/fj00-0294rev. [DOI] [PubMed] [Google Scholar]
- 76.Xiao X, et al. HSF1 is required for extra-embryonic development, postnatal growth and protection during inflammatory responses in mice. EMBO J. 1999;18:5943–52. doi: 10.1093/emboj/18.21.5943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dai C, Whitesell L, Rogers AB, Lindquist S. Heat shock factor 1 is a powerful multifaceted modifier of carcinogenesis. Cell. 2007;130:1005–18. doi: 10.1016/j.cell.2007.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.McMillan DR, et al. Heat shock transcription factor 2 is not essential for embryonic development, fertility, or adult cognitive and psychomotor function in mice. Mol Cell Biol. 2002;22:8005–14. doi: 10.1128/MCB.22.22.8005-8014.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kallio M, et al. Brain abnormalities, defective meiotic chromosome synapsis and female subfertility in HSF2 null mice. EMBO J. 2002;21:2591–601. doi: 10.1093/emboj/21.11.2591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wilkerson DC, Skaggs HS, Sarge KD. HSF2 binds to the Hsp90, Hsp27, and c-Fos promoters constitutively and modulates their expression. Cell Stress Chaperones. 2007;12:283–90. doi: 10.1379/CSC-250.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhang Y, Frejtag W, Dai R, Mivechi NF. Heat shock factor-4 (HSF-4a) is a repressor of HSF-1 mediated transcription. J Cell Biochem. 2001;82:692–703. doi: 10.1002/jcb.1191. [DOI] [PubMed] [Google Scholar]
- 82.Nakai A, et al. HSF4, a new member of the human heat shock factor family which lacks properties of a transcriptional activator. Mol Cell Biol. 1997;17:469–81. doi: 10.1128/mcb.17.1.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Knowlton AA, Sun L. Heat-shock factor-1, steroid hormones, and regulation of heat-shock protein expression in the heart. Am J Physiol Heart Circ Physiol. 2001;280:H455–64. doi: 10.1152/ajpheart.2001.280.1.H455. [DOI] [PubMed] [Google Scholar]
- 84.Zou J, Guo Y, Guettouche T, Smith DF, Voellmy R. Repression of heat shock transcription factor HSF1 activation by HSP 90 (HSP 90 complex) that forms a stress-sensitive complex with HSF1. Cell. 1998;94:471–80. doi: 10.1016/s0092-8674(00)81588-3. [DOI] [PubMed] [Google Scholar]
- 85.Shamovsky I, Ivannikov M, Kandel ES, Gershon D, Nudler E. RNA-mediated response to heat shock in mammalian cells. Nature. 2006;440:556–60. doi: 10.1038/nature04518. [DOI] [PubMed] [Google Scholar]
- 86.Christians ES, Yan LJ, Benjamin IJ. Heat shock factor 1 and heat shock proteins: critical partners in protection against acute cell injury. Crit Care Med. 2002;30:S43–50. [PubMed] [Google Scholar]
- 87.Chu B, Zhong R, Soncin F, Stevenson MA, Calderwood SK. Transcriptional activity of heat shock Factor 1 at 37 degrees C Is repressed through phosphorylation on two distinct serine residues by glycogen synthase kinase 3 and protein kinases Calpha and Czeta. J Biol Chem. 1998;273:18640–6. doi: 10.1074/jbc.273.29.18640. [DOI] [PubMed] [Google Scholar]
- 88.Park J, Liu AY. JNK phosphorylates the HSF1 transcriptional activation domain: role of JNK in the regulation of the heat shock response. J Cell Biochem. 2001;82:326–38. doi: 10.1002/jcb.1163. [DOI] [PubMed] [Google Scholar]
- 89.Guettouche T, Boellmann F, Lane W, Voellmy R. Analysis of phosphorylation of human heat shock factor 1 in cells experiencing a stress. BMC Biochemistry. 2005;6:4. doi: 10.1186/1471-2091-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Holmberg CI, et al. Phosphorylation of serine 230 promotes inducible transcriptional activity of heat shock factor 1. EMBO J. 2001;20:3800–10. doi: 10.1093/emboj/20.14.3800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chen Y, Currie RW. Small interfering RNA knocks down heat shock factor-1 (HSF-1) and exacerbates pro-inflammatory activation of NF-[kappa]B and AP-1 in vascular smooth muscle cells. Cardiovascular Research. 2006;69:66–75. doi: 10.1016/j.cardiores.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 92.Wirth D, Bureau F, Melotte D, Christians E, Gustin P. Evidence for a role of heat shock factor 1 in inhibition of NF-kappa B pathway during heat shock response-mediated lung protection. Am J Physiol Lung Cell Mol Physiol. 2004;287:L953–61. doi: 10.1152/ajplung.00184.2003. [DOI] [PubMed] [Google Scholar]
- 93.Singh IS, Viscardi RM, Kalvakolanu I, Calderwood S, Hasday JD. Inhibition of tumor necrosis factor-alpha transcription in macrophages exposed to febrile range temperature. A possible role for heat shock factor-1 as a negative transcriptional regulator. J Biol Chem. 2000;275:9841–8. doi: 10.1074/jbc.275.13.9841. [DOI] [PubMed] [Google Scholar]
- 94.Papaconstantinou AD, Goering PL, Umbreit TH, Brown KM. Regulation of uterine hsp90alpha, hsp72 and HSF-1 transcription in B6C3F1 mice by beta-estradiol and bisphenol A: involvement of the estrogen receptor and protein kinase C. Toxicol Lett. 2003;144:257–70. doi: 10.1016/s0378-4274(03)00215-7. [DOI] [PubMed] [Google Scholar]
- 95.Voss MR, et al. Gender differences in the expression of heat shock proteins: the effect of estrogen. Am J Physiol Heart Circ Physiol. 2003;285:H687–92. doi: 10.1152/ajpheart.01000.2002. [DOI] [PubMed] [Google Scholar]
- 96.Yang X, Dale EC, Diaz J, Shyamala G. Estrogen dependent expression of heat shock transcription factor: implications for uterine synthesis of heat shock proteins. J Steroid Biochem Mol Biol. 1995;52:415–9. doi: 10.1016/0960-0760(94)00191-n. [DOI] [PubMed] [Google Scholar]
- 97.Hamilton KL, Gupta S, Knowlton AA. Estrogen and regulation of heat shock protein expression in female cardiomyocytes: cross-talk with NF kappa B signaling. J Mol Cell Cardiol. 2004;36:577–84. doi: 10.1016/j.yjmcc.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 98.Fekete A, et al. Sex differences in heat shock protein 72 expression and localization in rats following renal ischemia-reperfusion injury. Am J Physiol Renal Physiol. 2006;291:F806–11. doi: 10.1152/ajprenal.00080.2006. [DOI] [PubMed] [Google Scholar]
- 99.Voss MR, et al. Gender differences in the expression of heat shock proteins: the effect of estrogen. Am J Physiol Heart Circ Physiol. 2003;285:H687–92. doi: 10.1152/ajpheart.01000.2002. [DOI] [PubMed] [Google Scholar]
- 100.Paroo Z, Haist JV, Karmazyn M, Noble EG. Exercise improves postischemic cardiac function in males but not females: consequences of a novel sex-specific heat shock protein 70 response. Circ Res. 2002;90:911–7. doi: 10.1161/01.res.0000016963.43856.b1. [DOI] [PubMed] [Google Scholar]
- 101.Paroo Z, Dipchand ES, Noble EG. Estrogen attenuates postexercise HSP70 expression in skeletal muscle. Am J Physiol Cell Physiol. 2002;282:C245–51. doi: 10.1152/ajpcell.00336.2001. [DOI] [PubMed] [Google Scholar]
- 102.Nickerson M, Kennedy SL, Johnson JD, Fleshner M. Sexual dimorphism of the intracellular heat shock protein 72 response. J Appl Physiol. 2006;101:566–75. doi: 10.1152/japplphysiol.00259.2006. [DOI] [PubMed] [Google Scholar]
- 103.Bupha-Intr T, Wattanapermpool J. Cardioprotective effects of exercise training on myofilament calcium activation in ovariectomized rats. J Appl Physiol. 2004;96:1755–60. doi: 10.1152/japplphysiol.01227.2003. [DOI] [PubMed] [Google Scholar]
- 104.Thawornkaiwong A, Pantharanontaga J, Wattanapermpool J. Hypersensitivity of myofilament response to Ca2+ in association with maladaptation of estrogen-deficient heart under diabetes complication. Am J Physiol Regul Integr Comp Physiol. 2007;292:R844–51. doi: 10.1152/ajpregu.00365.2006. [DOI] [PubMed] [Google Scholar]
- 105.Shinohara T, et al. Estrogen inhibits hyperthermia-induced expression of heat-shock protein 72 and cardioprotection against ischemia/reperfusion injury in female rat heart. J Mol Cell Cardiol. 2004;37:1053–61. doi: 10.1016/j.yjmcc.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 106.Kohno H, et al. Receptor-mediated suppression of cardiac heat-shock protein 72 expression by testosterone in male rat heart. Endocrinology. 2007;148:3148–55. doi: 10.1210/en.2006-1581. [DOI] [PubMed] [Google Scholar]
- 107.Yu HP, et al. Mechanism of the salutary effects of flutamide on intestinal myeloperoxidase activity following trauma-hemorrhage: up-regulation of estrogen receptor-{beta}-dependent HO-1. J Leukoc Biol. 2006;79:277–84. doi: 10.1189/jlb.0705363. [DOI] [PubMed] [Google Scholar]
- 108.Yu HP, et al. Maintenance of lung myeloperoxidase activity in proestrus females after trauma-hemorrhage: upregulation of heme oxygenase-1. Am J Physiol Lung Cell Mol Physiol. 2006;291:L400–6. doi: 10.1152/ajplung.00537.2005. [DOI] [PubMed] [Google Scholar]
- 109.Yu HP, et al. Mechanism of cardioprotection following trauma-hemorrhagic shock by a selective estrogen receptor-beta agonist: upregulation of cardiac heat shock factor-1 and heat shock proteins. J Mol Cell Cardiol. 2006;40:185–94. doi: 10.1016/j.yjmcc.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 110.Chen HW, Kuo HT, Wang SJ, Lu TS, Yang RC. In vivo heat shock protein assembles with septic liver NF-kappa B/I-kappa B complex regulating NF-kappa B activity. Shock. 2005;24:232–8. doi: 10.1097/01.shk.0000174020.87439.f2. [DOI] [PubMed] [Google Scholar]
- 111.Yoo CG, et al. Anti-inflammatory effect of heat shock protein induction Is related to stabilization of I kappa B alpha through preventing I kappa B kinase activation in respiratory epithelial cells. J Immunol. 2000;164:5416–23. doi: 10.4049/jimmunol.164.10.5416. [DOI] [PubMed] [Google Scholar]
- 112.Dunsmore KE, Denenberg AG, Page K, Wong HR. Mechanism and function of heat shock-dependent I kappa B alpha expression. Inflamm Res. 2006;55:254–9. doi: 10.1007/s00011-006-0080-2. [DOI] [PubMed] [Google Scholar]
- 113.Park KJ, Gaynor RB, Kwak YT. Heat shock protein 27 association with the I kappa B kinase complex regulates tumor necrosis factor alpha-induced NF-kappa B Activation. J Biol Chem. 2003;278:35272–8. doi: 10.1074/jbc.M305095200. [DOI] [PubMed] [Google Scholar]
- 114.Chan JYH, Ou CC, Wang LL, Chan SHH. Heat shock protein 70 confers cardiovascular protection during endotoxemia via inhibition of nuclear factor-kappa B activation and inducible nitric oxide synthase expression in the rostral ventrolateral medulla. Circulation. 2004;110:3560–6. doi: 10.1161/01.CIR.0000143082.63063.33. [DOI] [PubMed] [Google Scholar]