Abstract
In this paper, we evaluated the long-term results of uncemented total hip arthroplasties using tapered fully porous-coated cobalt-chrome stems (Autophor 900S). The average follow-up was 206 months in 127 hips (113 patients). The articulations of the joints were ceramic-on-polyethylene in 43 hips and ceramic-on-ceramic in 84. The survival rate of the stems at 17 years was 94.5%. A stable stem with bony ingrowth was identified in all 120 hips, excluding femoral revision cases (seven hips). The causes of the seven femoral revisions were aseptic loosening in four, infection in two, and stem fracture in one. No surgical intervention was performed for osteolysis or stress shielding. The Autophor 900S tapered fully porous-coated cobalt-chrome femoral stem revealed encouraging radiographic long-term stability.
Résumé
Nous avons évalué les résultats à long termes d’une prothèse totale de hanche non cimentée porous coated en chrome cobalt (Autophor 900S). Le suivi moyen a été de 206 mois pour 127 hanches (113 patients). Le couple de friction est un couple de friction céramique polyéthylène dans 43 hanches et céramique céramique dans 84 hanches. Le taux de survie à 17 ans de la pièce fémorale a été de 94.5%. Une stabilité de la pièce fémorale avec repousse osseuse a été mise en évidence dans 120 hanches en excluant les 7 cas de révision fémorale. L’origine de cette révision a été un descellement aseptique pour 4 d’entre elles, une infection pour deux d’entre elles, une fracture de la pièce fémorale pour l’une d’entre elle. Aucune intervention chirurgicale n’a été nécessaire du fait d’une ostéolyse ou d’un stress shielding. La prothèse Autophor 900S avec pièce fémorale chrome cobalt porous coated montre des résultats tout à fait encourageant avec une bonne stabilité à long terme.
Introduction
Although many authors have reported the results of various femoral implants, it is not clear which types of implants produce the best results. Some have advocated cemented stems after improving the cementing technique, while others prefer cementless stems.
Recently, encouraging long-term results have been reported for cementless tapered titanium stems and cementless cylindrical cobalt-chrome stems (Zweymüller [12], CLS [18], Mallory-Head [19], Tri-Lock [24], Anatomic Medullary Locking (AML) prosthesis [10], Taperloc stem [21], Anatomic hip stem [1], Ultralok [11], Spotorno stem [2], Omnifit [16], etc.). However, no long-term follow-up studies have been conducted on cementless total hip replacements with a tapered fully porous-coated cobalt-chrome stem.
This study was undertaken to determine the long-term results of uncemented total hip arthroplasty with a tapered fully porous-coated cobalt-chrome stem, which is extensively porous-coated (Autophor 900S).
Materials and methods
Patient demographics
Between March 1982 and September 1989, 142 consecutive unselected patients (157 hips) underwent uncemented total hip arthroplasty with a tapered fully porous-coated cobalt-chrome stem (Autophor 900S) at our institution. Of the 157 hips (142 patients), nine patients (ten hips) died and 20 patients (20 hips) were lost to follow-up. Of those lost to follow-up, 11 could not be located, despite considerable effort, including inquiries to the police; nine others refused to return for a clinical assessment or for a review of recent radiographs. Nine patients who were unable to return for a follow-up evaluation completed a telephone questionnaire and showed satisfactory results.
One hundred and twenty-seven hips (113 patients), including seven hips that required femoral stem revision surgery, were the subjects of this study. Mean patient age at the time of the operation was 41 years (range, 20–64 years). There were 88 men and 25 women. The majority of hips (98 hips; 77.2%) had a diagnosis of osteonecrosis, and ten hips (8.9%) had primary osteoarthrosis, four hips (3.1%) femoral neck fracture, one hip (0.8%) rheumatoid arthritis, and 14 hips (11.0%) secondary osteoarthrosis. Of the secondary osteoarthrosis cases, septic hip sequelae occurred in eight of 14 hips, dysplastic hips in four, and post-traumatic sequelae in two. Mean patient weight was 59.6 kg (range, 45–75 kg). Seven hips required femoral stem revision surgery, leaving 120 living hips (106 patients) who had not had revision surgery and who were available for follow-up at a median of 206 months (17 years; range, 15–22 years) after the index operation.
Implant
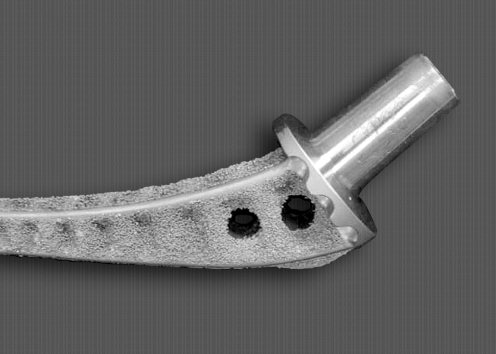
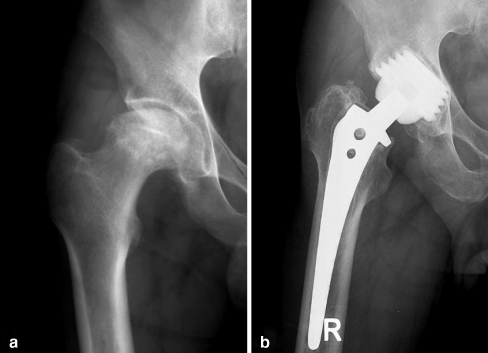
Fully porous-coated cobalt-chrome alloy femoral stems (Autophor, Osteo AG, Selzach, Switzerland) were inserted in all 127 hips (Fig. 1). The acetabular components inserted were truncated alumina ceramic acetabular components with a ceramic head (BIOLOX, Osteo AG, Selzach, Switzerland) in 84 hips (Fig. 2), and cementless self-cutting titanium acetabular components (CST, OsteoAG, Selzach, Switzerland) with a polyethylene liner and a ceramic head in 43 hips. All operations were performed by a single surgeon (SMR) using the Watson-Jones anterolateral approach.
Fig. 1.
A fully porous-coated cobalt-chrome alloy femoral stem (Autophor 900S)
Fig. 2.
a Preoperative anteroposterior radiograph of a 36-year-old male diagnosed as osteonecrosis of the femoral head. b Radiograph showing the stable acetabular cup and Autophor 900S stem 17 years after total hip arthroplasty using the Autophor 900S stem
Clinical evaluation
The 120 hips (106 patients) that did not undergo femoral stem revision were evaluated clinically. This consisted of a physical examination, a calculation of the Harris hip score [14], and administration of a patient questionnaire that requested data on thigh pain. Thigh pain was defined as a diffuse pain at the initiation of weight-bearing, even if it did not prevent walking.
Radiographic evaluation
Anteroposterior and lateral radiographs were available from the last follow-up visit, and these were compared with previous radiographs and analysed for radiolucent lines, changes in bone density, cortical hypertrophy, and heterotopic ossification. A complete radiographic follow-up series, including preoperative, postoperative, and last follow-up radiographs, was available for 120 hips (106 patients). Radiographs were examined by two observers (TRY, MSK).
Femoral component stability was graded using the classification of Engh et al. [8]. Fixation by bone ingrowth was defined as a stable implant with radiological evidence of bone ingrowth to the porous surface and no subsidence or shifting of the stem. Stable fixation by fibrous ingrowth was defined as an implant with radiopaque line formation around the stem, but with no progressive migration or shifting of the stem. An unstable implant was defined as one with definite evidence of either progressive subsidence or migration within the femoral canal.
Also, migration analysis was performed by measuring the vertical subsidence of the femoral component according to Callaghan et al. [4]. Vertical subsidence of the femoral component was measured as the change in the distance from the landmark of the femoral component to the most proximal point of the greater trochanter.
The presence of osteolysis was noted and recorded using Gruen zones on the femoral side [13]. Expansile, erosive, or ballooning type osteolysis was designated as scalloping osteolysis. Scalloping osteolysis was distinguished from a linear pattern of bone resorption, which was designated as linear osteolysis.
To evaluate the extent of stress shielding, the femur was divided into four levels on anteroposterior radiographs [7]. The first line was drawn transversely along the inferior end of the lesser trochanter, the second line was drawn transversely at the tip of the femoral stem, and the third line was drawn midway between the first and second lines. The three lines divided the femur area into four levels. First-degree stress shielding was defined as demineralisation of the medial cortex at the first level; second-degree stress shielding as demineralisation of the medial cortex into the second level; third-degree stress shielding as demineralisation extending into the third level; and fourth-degree stress shielding if a whole level had thin cortex and was osteoporotic.
Heterotopic bone formation was graded according to the criteria of Brooker et al. [3].
Statistical analysis
The survival rate was estimated using the Kaplan-Meier method. Failure was defined as revision surgery for any reason. The time to revision was calculated as the time between the date of implantation and the date of revision. Patients without revision were recorded at the date of the last follow-up or death.
Results
Clinical findings
Of the 120 hips (106 patients) that had not undergone femoral stem revision, no patient reported isolated thigh pain or any association with another disorder. Patients who had not undergone revision had a mean Harris hip score of 87.3 points (range, 62 to 100 points) at the time of their last follow-up.
Revisions
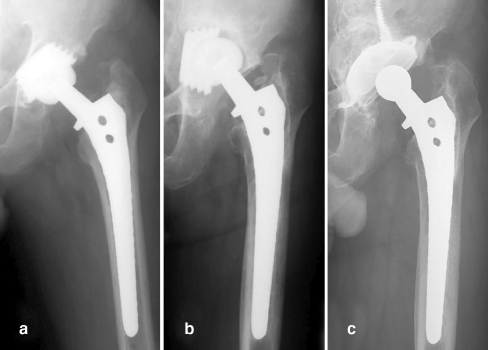
Twenty-seven hips (26 patients) had been revised, leaving 100 hips without revision. Twenty-five cups needed revision surgery because of aseptic loosening in 23 and infection in two (Table 1) (Fig. 3). Seven femoral stems were revised because of aseptic loosening in four, infection in two, and stem fracture in one. Four total revisions were performed due to aseptic loosening of both acetabular and femoral components.
Table 1.
Relationship between revisions and joint articulations
| Revision | Cause | Ceramic-on-polyethylene (43 hips) | Ceramic-on-ceramic (84 hips) | Total (127 hips) |
|---|---|---|---|---|
| Cup | Aseptic loosening | 10 (2*) | 13 (2*) | 23 (4*) |
| Infection | 1 | 1 | 2 | |
| Stem | Aseptic loosening | 2* | 2* | 4* |
| Infection | 1 | 1 | 2 | |
| Stem fracture | 0 | 1 | 1 |
*Represents the number of patients who had total revisions
Fig. 3.
a Anteroposterior radiograph of a 52-year-old male who received total hip arthroplasty using a Autophor 900S stem and truncated alumina ceramic acetabular components due to osteonecrosis of the femoral head. b A migration of the acetabular component occurred 8 years postoperatively. c A socket revision was performed, and the Autophor 900S stem remained stable after 9 years postoperatively
Radiographic findings
The radiographic follow-up of stems was possible in 120 hips (average 17 years), excluding the femoral revision cases (seven hips).
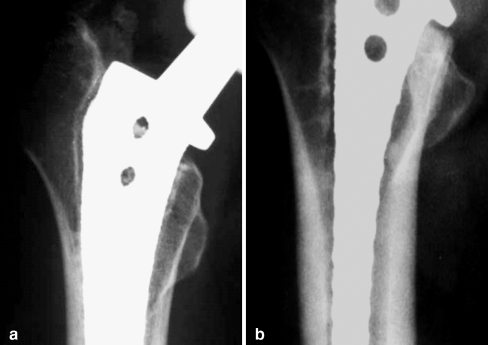
Overall, femoral components were graded as stabilised by bone ingrowth in 120 hips (100%). There was no case of stem subsidence over 4 mm. An average subsidence of 2.44 mm occurred with a range of 0 mm to 4 mm. Femoral osteolysis was noted in 32 hips (26.7%). In 32 hips, the pattern of osteolysis was linear and was confined to Gruen zones 1 and 7 in 21 of 32 hips. The maximum width of the linear osteolysis ranged from 2 mm to 8 mm with, an average of 3.2 mm, and its length ranged from 20 mm to 120 mm, with an average of 52 mm. Scalloping osteolysis was noted in 11 of 32 hips. In all hips with scalloping osteolysis, the osteolytic lesions were identified in Gruen zones 1 or 7 (Fig. 4).
Fig. 4a, b.
Anteroposterior radiographs showing linear osteolysis (a) and scalloping osteolysis (b)
Stress shielding was graded into four categories. Grade I stress shielding was identified in 82 hips (68.3%), Grade II in 22 hips (18.3%), Grade III in 11 hips (9.2%), and Grade IV in five hips (4.2%).
Heterotopic ossification was presented in 54 (45%) of 120 hips. Thirty-eight hips (31.7%) were Grade I, nine hips (7.5%) Grade II, and seven hips (5.8%) Grade III.
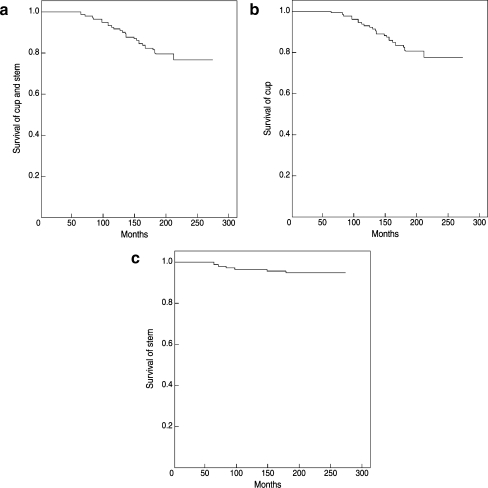
Survival analysis
The survival rate of the stem only at 17 years was 94.5% (95% confidence interval, 91.9% to 97.1%; standard error, 3.74). The cumulative survival rate of both hip components was 78.7% (95% confidence interval, 75.1% to 82.3%; standard error, 5.68); ceramic-on-polyethylene was 74.4% (95% confidence interval, 71.5% to 77.3%; standard error, 4.58), and ceramic-on-ceramic was 81.0% (95% confidence interval, 77.9% to 84.1%; standard error, 4.90). The survival rate of the cup only was 80.3% (95% confidence interval, 76.9% to 83.7%; standard error, 5.37) at 17 years. Survivorship curves derived with the Kaplan-Meier method are presented in Fig. 5.
Fig. 5a–c.
Survivorship curves derived with the Kaplan-Meier method [16] with a 95% confidence interval. a Survivorship curve with revision of both the stem or the cup for any reason as the end point. b Survivorship curve with revision of the cup only for any reason as the end point. c Survivorship curve with revision of the stem only for any reason as the end point
Discussion
The use of cementless femoral components for primary hip replacement increased significantly in the mid-1980s after numerous reported failures of first-generation cemented primary hip replacements, particularly in young patients [6, 23]. This resulted in the development of various cementless porous-coated stems [20]. Several long-term follow-up studies of different cementless designs have been reported recently and are compared in Table 2.
Table 2.
Comparison of the long-term results of different cementless stems in the literature
| Authors (year, journal name) | Stem | Follow-up duration (years) | Survival rate of stem (%) |
|---|---|---|---|
| Archibeck et al. [1] (2001, JBJSa) | Anatomic hip | 10 | 100 |
| Hsieh et al. [16] (2002, Chang Gung Med J) | Omnifit | 10.2 | 93 |
| Engh et al. [10] (1997, JBJS) | AML | 11 | 97 |
| Parvizi et al. [21] (2004, JOAb) | Taperloc | 11 | 99.1 |
| Grübl et al. [12] (2002, JBJS) | Zweymüller | 10 | 99 |
| Aldinger et al. [2] (2003, JBJS-Bc) | Spotorno | 12 | 92 |
| Mallory et al. [19] (2001, JOA) | Mallory-Head | 12.2 | 97.5 |
| Grant et al. [11] (2004, JOA) | Ultralok | 12.2 | 96.6 |
| Lee and Nah [18] (2003, JKOAd) | CLS | 12.3 | 100 |
| Teloken et al. [24] (2002, JBJS) | Tri-Lock | 15 | 100 |
aJournal of Bone and Joint Surgery—American Volume
bJournal of Arthroplasty
cJournal of Bone and Joint Surgery—British Volume
dJournal of the Korean Orthopaedic Association
Grübl et al. [12] reported on 127 hips in 123 patients using Zweymüller, a tapered rectangular titanium stem. At an average follow-up of 120.7 months after the index operation, the probability of survival of both the femoral and the acetabular components at ten years, with any revision as an end point, was 0.92. The probability of survival of the cup was 0.93 and that of the stem was 0.99. Lee and Nah [18] followed up 33 hips (29 patients) with CLS stems placed in patients with osteonecrosis of the femoral head for 12.3 years and reported no stem revision.
Extensively porous-coated cementless implants have achieved good results using biological fixation. The most commonly used was AML. Engh et al. [10] followed up 196 of these stems implanted in patients with an average age of 55 years for 11 years and found a mechanical failure rate of only 2.6%. Kronick et al. [17] reported on 174 hips in 154 patients younger than 50 years of age using the AML and Prodigy extensively porous-coated stems. At an average follow-up of 8.3 years, 99.4% of the stems showed stable fixation, 96% had bone ingrowth, 3.4% were fibrous stable, and 1.1% were revised. The rate of osteolysis in the femur was 14% and was limited to proximal Gruen zones 1 and 7.
Engh et al. [9] retrospectively reviewed the outcome of 3,314 total hip arthroplasties performed with AML, Prodigy, and Solution stems (all DePuy, Warsaw, IN). These hips included 460 proximally coated stems and 2,854 extensively coated stems. The survival rates for proximally and extensively coated stems were >95% at 15 years, using revision for any reason as an endpoint. Slight differences in thigh pain, stress shielding, and patient satisfaction were not significant. The 2.8% rate of component loosening among proximally coated stems was significantly higher than the 1.1% rate observed with extensively coated stems. Because of the relatively straightforward, reproducible surgical technique associated with extensively porous-coated stems and the perception of a marginally better outcome, they preferred to use extensively porous-coated stems for all primary total hip arthroplasties.
Autophor 900S and AML stems are similar in that they are extensively porous-coated cobalt-chromium-alloy components. To the authors’ knowledge, no long-term study has been conducted on the Autophor 900S stem, which is tapered and rectangular-shaped. Our study reveals that using the Autophor 900S stem provides excellent results; 114 hips (95%) were stable with bone ingrowth at a mean of 17 years, which is comparable with other results [1, 2, 10–12, 16, 18, 19, 21, 24].
The greater total surface area of the porous coatings on extensively porous-coated stems provides a greater surface area for bone ingrowth. However, with extensively coated stems, there were some concerns regarding cortical atrophy and thigh pain, which led to changes in the design of the cementless stem that reduced the porous surface to a small area on the proximal aspect of the stem. Others thought that a more flexible titanium alloy stem might preserve bone and decrease the incidence of thigh pain compared with a cobalt-chrome stem.
On the femoral side, osteolytic lesions were confined to the periarticular area adjacent to the collar or behind the shoulder of the prosthesis. None of the lesions progressed distal to Gruen Zones 1 or 7, and there was no late loosening secondary to femoral osteolysis. The results on the acetabular side proved to be less satisfactory than those on the femoral side, and the survival rate for acetabular cups was 80.3%. Loosening of the acetabular component occurred late in our series, at a mean of 11.4 years (range, 5.3 to 17.8) after the index operation. There are several obvious differences between truncated ceramic sockets and hemispherical porous-coated sockets [22].
Stress shielding is likely to be a continuous problem in a cementless stem, and poses several problems, such as the breakage of bone in the osteoporotic region and stem removal difficulties due to strong distal fixation during revision surgery. However, in our study, stress-shielding did not adversely affect the outcome at the last follow-up.
Campbell et al. [5] reviewed the cases of 148 patients managed by porous-coated hip arthroplasty and found a prevalence of thigh pain of 13% and 22% one and two years after surgery, respectively. They concluded that thigh pain was secondary to stem instability. Hartley et al. [15] reported that all of their four patients (14% of the series) with activity-limiting thigh pain had a proximally coated AML stem and that no patient with an extensively coated stem had such pain. They suggested that micromotion between the stem and the femoral cortex is related to thigh pain. In our study, no patient reported isolated thigh pain at the last follow-up. We speculate that stable bony ingrowth into a fully porous-coated stem decreased micromotion at the bone–implant interface and that this eventually resolved thigh pain. Moreover, patient long-term adaptation after operation reduces the rate of thigh pain and this may also be a reason why this femoral component worked so well.
In our series, cumulative survival with any femoral revision as the end point was 94.5% at 17 years and the results on the acetabular side proved to be less satisfactory than those on the femoral side as the survival rate for the cup was 80.3%. Thus, the Autophor 900S tapered fully porous-coated cobalt-chrome femoral implant revealed encouraging radiographic stability over a long-term period and highly reliable results.
Contributor Information
Taek Rim Yoon, Email: tryoon@chonnam.ac.kr.
Sung-Man Rowe, Email: smrowe@chonnam.ac.kr.
References
- 1.Archibeck MJ, Berger RA, Jacobs JJ, Quigley LR, Gitelis S, Rosenberg AG, Galante JO (2001) Second-generation cementless total hip arthroplasty. Eight to eleven-year results. J Bone Jt Surg Am 83(11):1666–1673 [DOI] [PubMed]
- 2.Aldinger PR, Breusch SJ, Lukoschek M, Mau H, Ewerbeck V, Thomsen M (2003) A ten- to 15-year follow-up of the cementless spotorno stem. J Bone Jt Surg Br 85(2):209–214 [DOI] [PubMed]
- 3.Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Jt Surg Am 55(8):1629–1632 [PubMed]
- 4.Callaghan JJ, Salvati EA, Pellicci PM, Wilson PD Jr, Ranawat CS (1985) Results of revision for mechanical failure after cemented total hip replacement, 1979 to 1982. A two to five-year follow-up. J Bone Jt Surg Am 67(7):1074–1085 [PubMed]
- 5.Campbell AC, Rorabeck CH, Bourne RB, Chess D, Nott L (1992) Thigh pain after cementless hip arthroplasty. Annoyance or ill omen. J Bone Jt Surg Br 74(1):63–66 [DOI] [PubMed]
- 6.Chandler HP, Reineck FT, Wixson RL, McCarthy JC (1981) Total hip replacement in patients younger than thirty years old. A five-year follow-up study. J Bone Jt Surg Am 63(9):1426–1434 [PubMed]
- 7.Engh CA, Bobyn JD (1988) The influence of stem size and extent of porous coating on femoral bone resorption after primary cementless hip arthroplasty. Clin Orthop Relat Res 231:7–28 [PubMed]
- 8.Engh CA, Glassman AH, Griffin WL, Mayer JG (1988) Results of cementless revision for failed cemented total hip arthroplasty. Clin Orthop Relat Res 235:91–110 [PubMed]
- 9.Engh CA, Hopper RH Jr (2002) The odyssey of porous-coated fixation. J Arthroplasty 17(4 Suppl 1):102–107 [DOI] [PubMed]
- 10.Engh CA Jr, Culpepper WJ 2nd, Engh CA (1997) Long-term results of use of the anatomic medullary locking prosthesis in total hip arthroplasty. J Bone Jt Surg Am 79(2):177–184 [DOI] [PubMed]
- 11.Grant P, Grogaard B, Nordsletten L (2004) Ultralok uncemented femoral prostheses: 12 to 15 year follow-up evaluation. J Arthroplasty 19(3):274–280 [DOI] [PubMed]
- 12.Grübl A, Chiari C, Gruber M, Kaider A, Gottsauner-Wolf F (2002) Cementless total hip arthroplasty with a tapered, rectangular titanium stem and a threaded cup: a minimum ten-year follow-up. J Bone Jt Surg Am 84(3):425–431 [DOI] [PubMed]
- 13.Gruen TA, McNeice GM, Amstutz HC (1997) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 141:17–27 [PubMed]
- 14.Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Jt Surg Am 51(4):737–755 [PubMed]
- 15.Hartley WT, McAuley JP, Culpepper WJ, Engh CA Jr, Engh CA Sr (2000) Osteonecrosis of the femoral head treated with cementless total hip arthroplasty. J Bone Jt Surg Am 82(10):1408–1413 [DOI] [PubMed]
- 16.Hsieh PH, Shih CH, Lee PC, Chen CH, Yang WE (2002) Primary total hip arthroplasty without the use of bone cement: a 10-year follow-up of 157 hips. Chang Gung Medical J 25(5):298–305 [PubMed]
- 17.Kronick JL, Barba ML, Paprosky WG (1997) Extensively coated femoral components in young patients. Clin Orthop Relat Res 344:263–274 [DOI] [PubMed]
- 18.Lee JM, Nah SJ (2003) 10–15 year follow-up results of total hip arthroplasty using a CLS (cementless spotorno) stem for osteonecrosis of the femoral head. J Korean Orthop Assoc 38(4):349–354
- 19.Mallory TH, Lombardi AV Jr, Leith JR, Fujita H, Hartman JF, Capps SG, Kefauver CA, Adams JB, Vorys GC (2001) Minimal 10-year results of a tapered cementless femoral component in total hip arthroplasty. J Arthroplasty 16(8 Suppl 1):49–54 [DOI] [PubMed]
- 20.Nourbash PS, Paprosky WG (1998) Cementless femoral design concerns. Rationale for extensive porous coating. Clin Orthop Relat Res 355:189–199 [DOI] [PubMed]
- 21.Parvizi J, Keisu KS, Hozack WJ, Sharkey PF, Rothman RH (2004) Primary total hip arthroplasty with an uncemented femoral component: a long-term study of the Taperloc stem. J Arthroplasty 19(2):151–156 [DOI] [PubMed]
- 22.Piston RW, Engh CA, De Carvalho PI, Suthers K (1994) Osteonecrosis of the femoral head treated with total hip arthroplasty without cement. J Bone Jt Surg Am 76(2):202–214 [DOI] [PubMed]
- 23.Sutherland CJ, Wilde AH, Borden LS, Marks KE (1982) A ten-year follow-up of one hundred consecutive Muller curved-stem total hip-replacement arthroplasties. J Bone Jt Surg Am 64(7):970–982 [PubMed]
- 24.Teloken MA, Bissett G, Hozack WJ, Sharkey PF, Rothman RH (2002) Ten to fifteen-year follow-up after total hip arthroplasty with a tapered cobalt-chromium femoral component (tri-lock) inserted without cement. J Bone Jt Surg Am 84(12):2140–2144 [DOI] [PubMed]