Abstract
Five hundred orthopaedic surgeons and 336 anaesthetists were surveyed to assess current UK attitudes towards transfusion practice following arthroplasty surgery. Seventy-two percent of surgeons and 73% of anaesthetists responded to the survey. In an uncomplicated patient following total hip arthroplasty, 53.2% of surgeons and 63.1% of anaesthetists would transfuse at or below a haemoglobin (Hb) level of 8 g/dL. Surgeons tended to be more aggressive in their attitudes, with a mean transfusion threshold of 8.3 g/dL compared to 7.9 g/dL for anaesthetists (p < 0.01), and with 97% of surgeons transfusing two or more units compared to 78% of anaesthetists (p < 0.01). This threshold Hb increased if the patient was symptomatic (surgeons 9.3 g/dL, anaesthetists 8.8 g/dL, p < 0.05) or was known to have pre-existing ischaemic heart disease (surgeons 9.0 g/dL, anaesthetists 9.2 g/dL, p < 0.05). A wide variability in attitudes and practices is demonstrated, and the development and adoption of consensus guidelines needs to be encouraged if efforts to reduce the use of blood products are to succeed.
Résumé
Cinq cent chirurgiens orthopédiques et 336 médecins anesthésistes ont participé à une enquête permettant de déterminer quelles étaient les pratiques de transfusion au Royaume-Uni en chirurgie arthroplastique. Soixante douze pour cent des chirurgiens, 73% des anesthésistes ont répondu à cette enquête après avoir réalisé une arthroplastie sans complication chez un patient. 53,2% des chirurgiens et 63,1% des anesthésistes n’ordonnent une transfusion que si le taux d’hémoglobine est inférieur ou égal à 8 g/dL. Les chirurgiens ayant une tendance plus agressive quant à la transfusion à partir de 8,3 g/dL d’hémoglobine au lieu de 7,9 g/dL pour les anesthésistes (p < 0,01). La transfusion est alors de deux unités pour 97% des chirurgiens alors que seulement 78% des anesthésistes en éprouvent le besoin (p < 0,01). Le taux d’hémoglobine limite pour une transfusion augmente si le patient est symptomatique (9,3 g/dL d’hémoglobine pour les chirurgies, 8,8 g/dL pour les anesthésistes, p < 0,05) ou s’il a existé des problèmes de cœur ischémique au niveau cardiaque (chirurgiens 9,0 g/dL d’hémoglobine, anesthésistes 9,2 g/dL, p < 0,05). Il existe de ce fait une grande variété d’attitude dans les pratiques de la transfusion et ceci nous encourage à adopter un consensus avec des règles bien précises de façon à réduire la quantité de sang à transfuser.
Introduction
There is widespread controversy regarding what constitutes appropriate management of post operative anaemia in surgical patients. This issue has particular relevance in orthopaedic surgery [15], as not only is intraoperative blood loss often significant, but complications of anaemia such as fatigue can limit participation in rehabilitation programmes, potentially resulting in longer hospital stays and poorer long-term outcomes [10]. However, the traditional transfusion ‘trigger’ of haemoglobin (Hb)<10 g/dL first proposed in 1942 [1] is no longer tenable with increased awareness of transfusion risks and escalating costs [8]. This study was designed to assess current attitudes towards transfusion following arthroplasty surgery in the UK. Previous studies [11] have suggested surgeons may be more aggressive in their transfusion practices than anaesthetists, and we therefore aimed to compare attitudes in transfusion practice between orthopaedic surgeons and anaesthetists.
Methods
A random sample of 500 orthopaedic surgeons working at NHS hospitals in the United Kingdom was selected from the British Orthopaedic Association membership, and all 336 anaesthetist members of the British Society of Orthopaedic Anaesthetists were selected as participants. Questionnaires were distributed by post to addresses obtained from the association databases. Return envelopes were provided but no other incentive given. After the initial round non-respondents were identified from numbered return envelopes and repeat questionnaires sent. Questionnaires were removed and separated from the envelopes by an independent party prior to analysis to ensure anonymity of the study.
The clinical scenario and questionnaire was developed in consultation with experts in arthroplasty surgery, anaesthesia, haematology and statistics. The questionnaire’s clarity, content, and clinical relevance was assessed through piloting and empiric clinical sensibility testing. Analysis of formal testing-retesting procedures carried out on 10 orthopaedic registrars resulted in a kappa score of 0.78.
The scenario (Table 1) was constructed around a representative low risk patient undergoing a primary hip arthroplasty procedure. The scenario was then modified to determine the effect of a previous cardiac history and the presence of symptoms on the respondents’ transfusion threshold. Effort was made to keep the questionnaire clear and concise to maximise the response rate. Differences between transfusion levels for anaesthetists and surgeons were analysed using the two-sample Student t-test, as were differences in the transfusion levels within the subgroups of the anaesthetists and surgeons. Differences in the transfusion levels for the same patient with different symptoms were analysed using paired Student t-tests. Significance was defined as a p value <0.05, and results are expressed as mean ± standard deviation.
Table 1.
Clinical scenario used in survey
| A 65-year-old woman with no prior cardiac history is undergoing primary hip arthroplasty for osteoarthritis. During the operation there is moderate bleeding although the exact blood loss is not recorded. She has been given crystalloid as volume replacement, and when seen on the post operative ward round she appears pale but normovolaemic. |
|---|
| 1) At what haemoglobin level would you transfuse this patient? |
| 2) If the above patient was complaining of fatigue and dizziness on standing, at what haemoglobin level would you transfuse the patient? |
| 3) If the above patient was asymptomatic but known to have ischaemic heart disease, at what haemoglobin level would you transfuse the patient? |
Results
The response rate was 72% (362/500) amongst surgeons and 73% (246/336) amongst anaesthetists. Responses from 17 surgeons and 14 anaesthetists who were either not involved in arthroplasty surgery or retired were excluded, leaving 345 and 232 questionnaires for analysis, respectively. The mean number of years qualified was 10.4 (range 1–34) for surgeons and 11.9 (0–33) for anaesthetists.
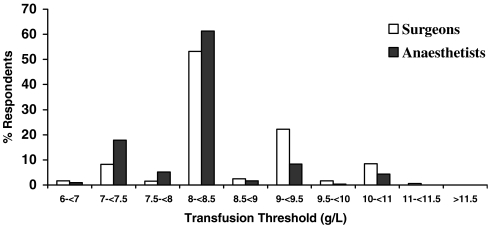
Transfusion thresholds ranged from Hb levels 6–11 g/dL amongst surgeons and 6–10 g/dL amongst anaesthetists and are summarised in Table 2. There was a significant (p < 0.01) difference in transfusion threshold between surgeons and anaesthetists, with a mean of 8.3 g/dL (±0.84) and 7.9 g/dL (±0.70), respectively; although the most common threshold was 8 g/dL in both surgeons (53.2%) and anaesthetists (63.1%) (Fig. 1).
Table 2.
Transfusion thresholds and target haemoglobin concentration at discharge
| Surgeons (n = 345) median Hb (mean±SD) g/dL | Anaesthetists (n = 232) median Hb (mean±SD) g/dL | |
|---|---|---|
| Unmodified scenario | 8 (8.3 ± .84) | 8 (7.9 ± .70) |
| Qualified <6 years | 8 (8.2 ± .72) n = 100* | 8 (7.7 ± .59) n = 56 |
| Qualified >6 years | 8 (8.4 ± .83) n = 218 | 8 (8.1 ± .72) n = 162 |
| Symptoms present | 9.5 (9.3 ± .86) | 8.5 (8.8 ± .93) |
| Ischaemic heart disease present | 9 (9.0 ± .93) | 9.5 (9.2 ± .94) |
| Target haemoglobin at discharge | 10 (9.8 ± 1.0) | 10 (9.4 ± 1.1) |
*Number of years qualified not stated in 27 surgeons and 14 anaesthetists
Fig. 1.
Distribution of transfusion thresholds (scenario Q1)
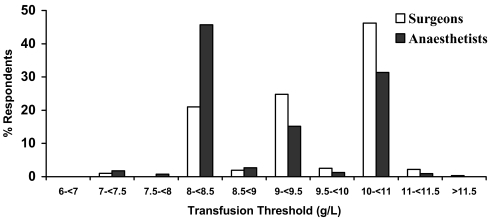
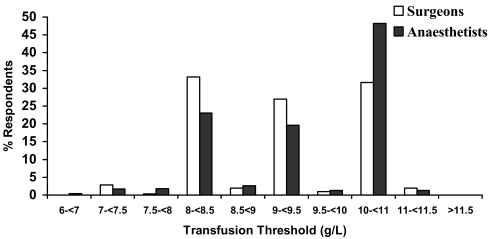
If the same patient in the scenario was complaining of symptoms, the threshold haemoglobin value increased significantly (p < 0.01) in both surgeons (mean 9.3 g/dL ± 0.86) and anaesthetists (mean 8.8 g/dL ±0.93) when compared to no symptoms. Again, the threshold haemoglobin among anaesthetists was lower when compared to surgeons (8.8 g/dL vs. 9.3 g/dL, respectively, p < 0.01) (Fig. 2). If the same patient also had ischaemic heart disease, the threshold haemoglobin again increased significantly (p < 0.01) in both surgeons (mean 9.0 g/dL ±.93) and anaesthetists (mean 9.2 g/dL ±.94) when compared to no ischaemic heart disease. However, the trend seen in the previous questions was reversed with anaesthetists choosing a significantly higher threshold haemoglobin than surgeons (9.2 g/dL vs. 9.0 g/dL, respectively, p < 0.01) (Fig. 3).
Fig. 2.
Distribution of transfusion thresholds when patient complaining of symptoms (scenario Q2)
Fig. 3.
Distribution of transfusion thresholds in patient with ischaemic heart disease (scenario Q3)
Following the decision to transfuse, 97% of surgeons would transfuse two or more units compared with 78% of anaesthetists (p < 0.01). The average estimated cost of a single unit of blood was $US267.90 (£GBP136.22, range £10–500) for surgeons and $US249.35 (£GBP126.77, range £10–500) for anaesthetists, close to the $US236.96 (£GBP120.48) the National Blood Service in the UK charges per unit to cover the cost of collection, processing, and issue (National Blood Service, 2005, personal communication). When asked about the risks of allogenic transfusion, over 80% of both surgeons and anaesthetists listed febrile reactions, communicable disease transmission, and haemolytic reactions as associations (data not shown). 35% of anaesthetists and 27% of surgeons also listed higher wound infection rates, presumably secondary to the immunosuppressive effects of allogenic blood [9].
Discussion
Orthopaedic surgery is a major consumer of allogenic blood, accounting for over 10% of all red blood cell transfusions in the UK, with 39% of this used in arthroplasty surgery [17]. The risks of blood transfusion are well documented, including viral disease transmission, haemolytic reactions, and more recent concerns such as prion diseases and immunosuppression [2]. In the decision to transfuse, these risks are balanced against clinical assessment of the degree of anaemia that is tolerable in an individual patient, and therefore below which ‘threshold’ blood should be given.
The results of our survey show a degree of consensus (51% of surgeons and 63% of anaesthetists) on a transfusion threshold of 8 g/dL in an uncomplicated patient post hip arthroplasty surgery. However, a large amount of variability in opinion existed both within and between specialties. While recent literature has supported more restrictive thresholds, the data on orthopaedic patients is limited. In the largest randomised trial to date comparing such thresholds, Hebert et al. [7] showed no difference in 30 day mortality between a liberal (Hb<10 g/dL) or restrictive (Hb<7 g/dL) transfusion strategy in 838 critically ill patients. In a retrospective review of 8,787 high-risk elderly patients following hip fracture, Carson et al. [3] demonstrated no increased mortality between those who were transfused and those who were not down to a haemoglobin value of 8.0 g/dL.
However, mortality is uncommon following elective arthroplasty, and outcome measures such as functional status, time to discharge, and post operative infection rate are more relevant. In particular, concern regarding the ability of the patient to participate in often demanding rehabilitation programmes may explain the higher transfusion thresholds seen amongst orthopaedic surgeons in this survey. A retrospective review of 5,793 patients undergoing hip fracture repair [10] showed a direct correlation between improved functional status and higher haemoglobin values. However, clinical data on arthroplasty patients is limited and other studies in hip fracture patients have shown no benefit to functional status with higher transfusion thresholds [5].
Previous surveys performed among anaesthetists have suggested a recent change in attitudes, with a Canadian survey [6] of critical care physicians performed in 1994 and repeated in 2002 showing a significant decrease in reported transfusion thresholds, and a 1981/2002 survey of American anaesthetists had similar findings [14]. This trend is perhaps reflected in the slightly lower thresholds chosen by younger (qualified<6 yrs) consultants in our survey.
The increased impact of anaemia on patients with cardiovascular disease has previously been documented. In a study of 1,958 surgical patients who refused blood transfusion for religious reasons [4], patients with pre-existing cardiovascular disease had higher rates of both morbidity and mortality when the haemoglobin level was 10 g/dL or less. Awareness of this was reflected in the results of our study, although a history of ischaemic heart disease appeared to be of more significance to anaesthetists, with their mean transfusion threshold rising to higher than that of surgeons (9.2 vs. 9.0 g/dL, respectively), in contrast to the previous scenarios.
There are a number of limitations to our study. Any survey such as this has the disadvantage of identifying attitudes and perceptions only, which may differ from actual clinical practice. Our study also surveyed consultants, when often the decision to transfuse in a hospital setting may be made by more junior staff. However, our findings are consistent with current data from observational studies [3, 15], which show haemoglobin levels 8–8.9 g/dL to be the most common ‘trigger’ for blood transfusion. Additionally, while our overall response rate of 73% compares favourably to previous surveys of orthopaedic surgeons [18], a degree of non-response bias remains. Our study also did not address alternative ‘blood sparing’ techniques such as autologous pre-donation of blood and cell salvage.
Current guidelines published by the British Committee for Standards in Haematology [13] state that transfusion is indicated in patients with a haemoglobin of <7 g/dL, and ‘should be avoided’ when the haemoglobin is >10 g/dL. This leaves a considerable grey area in patients with values between 7–10 g/dL, and further clinical trials are needed to determine what constitutes best practice in such patients. This study documents the uncertainty that exists by showing the considerable variation in transfusion practices among surgeons and anaesthetists, and to our knowledge is the first such survey of orthopaedic surgeons. The effectiveness of a written, planned and specific protocol in dramatically reducing the use of allogenic transfusion within an orthopaedic unit has been recently demonstrated [12, 16], and such an approach may be needed in order to rationalise transfusion practices post arthroplasty surgery.
Acknowledgement
This paper was funded by a grant from the Royal National Orthopaedic Hospital Research Trust.
References
- 1.Adams RC, Lundy JS (1942) Anesthesia in cases of poor surgical risk: some suggestions for decreasing the risk. Surg Gynecol Obstet 74:1011–1019
- 2.Busch MP, Kleinman SH, Nemo GJ (2003) Current and emerging infectious risks of blood transfusions. JAMA 289(8):959–962 [DOI] [PubMed]
- 3.Carson JL, Duff A, Berlin JA, Lawrence VA, Poses RM, Huber EC, O’Hara DA, Noveck H, Strom BL (1998) Perioperative blood transfusion and postoperative mortality. JAMA 279(3):199–205 [DOI] [PubMed]
- 4.Carson JL, Duff A, Poses RM, Berlin JA, Spence RK, Trout R, Noveck H, Strom BL (1996) Effect of anaemia and cardiovascular disease on surgical mortality and morbidity. Lancet 348(9034):1055–1060 [DOI] [PubMed]
- 5.Carson JL, Terrin ML, Barton FB, Aaron R, Greenburg AG, Heck DA, Magaziner J, Merlino FE, Bunce G, McClelland B, Duff A, Noveck H (1998) A pilot randomized trial comparing symptomatic vs. hemoglobin-level-driven red blood cell transfusions following hip fracture. Transfusion 38(6):522–529 [DOI] [PubMed]
- 6.Hebert PC, Fergusson DA, Stather D, McIntyre L, Martin C, Doucette S, Blajchman M, Graham ID; Canadian Critical Care Trials Group (2005) Revisiting transfusion practices in critically ill patients. Crit Care Med 33(1):7–12 [DOI] [PubMed]
- 7.Hebert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, Tweeddale M, Schweitzer I, Yetisir E; Canadian Critical Care Trials Group (1999) A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med 340(6):409–417 [DOI] [PubMed]
- 8.Helm AT, Karski MT, Parsons SJ, Sampath JS, Bale RS (2003) A strategy for reducing blood-transfusion requirements in elective orthopaedic surgery. Audit of an algorithm for arthroplasty of the lower limb. J Bone Joint Surg 85(4):484–489 [DOI] [PubMed]
- 9.Kendall SJ, Weir J, Aspinall R, Henderson D, Rosson J (2000) Erythrocyte transfusion causes immunosuppression after total hip replacement. Clin Orthop Relat Res 381:145–155 [DOI] [PubMed]
- 10.Lawrence VA, Silverstein JH, Cornell JE, Pederson T, Noveck H, Carson JL (2003) Higher Hb level is associated with better early functional recovery after hip fracture repair. Transfusion 43(12):1717–1722 [DOI] [PubMed]
- 11.Matot I, Einav S, Goodman S, Zeldin A, Weissman C, Elchalal U (2004) A survey of physicians’ attitudes toward blood transfusion in patients undergoing cesarean section. Am J Obstet Gynecol 190(2):462–467 [DOI] [PubMed]
- 12.Muller U, Exadaktylos A, Roeder C, Pisan M, Eggli S, Juni P (2004) Effect of a flow chart on use of blood transfusions in primary total hip and knee replacement: prospective before and after study. BMJ 328(7445):934–938 [DOI] [PMC free article] [PubMed]
- 13.Murphy MF, Wallington TB, Kelsey P, Boulton F, Bruce M, Cohen H, Duguid J, Knowles SM, Poole G, Williamson LM (2001) British committee for standards in haematology, blood transfusion task force. Guidelines for the clinical use of red cell transfusions. Br J Haematol 113(1):24–31 [DOI] [PubMed]
- 14.Nuttall GA, Stehling LC, Beighley CM, Faust RJ (2003) American society of anesthesiologists committee on transfusion medicine. Current transfusion practices of members of the American Society of Anesthesiologists: a survey. Anesthesiology 99(6):1433–1443 [DOI] [PubMed]
- 15.Rosencher N, Kerkkamp HE, Macheras G, Munuera LM, Menichella G, Barton DM, Cremers S, Abraham IL (2003) OSTHEO investigation. Orthopedic surgery transfusion hemoglobin European overview (OSTHEO) study: blood management in elective knee and hip arthroplasty in Europe. Transfusion 43(4):459–469 [DOI] [PubMed]
- 16.Spencer J, Thomas SR, Yardy G, Mukundan C, Barrington R (2005) Are we overusing blood transfusing after elective joint replacement? A simple method to reduce the use of a scarce resource. Ann R Coll Surg Engl 87(1):28–30 [DOI] [PMC free article] [PubMed]
- 17.Stanworth SJ, Cockburn HAC, Boralessa H, Contreras M (2002) Which groups of patients are transfused? A study of red cell usage in London and southeast England. Vox Sanguinis 83(4):352 [DOI] [PubMed]
- 18.Torella F, Haynes SL, Lardi A, O’Dwyer ST, McCollum CN (2001) Unchanging attitudes to autologous transfusion in the UK. Transfus Med 11(1):15–19 [DOI] [PubMed]