Abstract
Objective
To investigate the course of alcoholism in males and females in a 14-year followup of persons with DSM-III alcoholism compared to very heavy drinkers and unaffected controls in a community sample.
Methods
Case-control study based on data from the 1997 Health Services Use and Cost study, a 14-year followup survey of 442 individuals who participated in 2 waves of the 1981–1983 St. Louis Epidemiologic Catchment Area study. Cases met criteria for DSM-III alcohol abuse (AA) or dependence (AD) at both waves of the ECA: “Two-times Alcohol Use Disorder Positives (ECA 2t-AUDPs).” Two comparison groups were frequency matched to 2t-AUDPs: 1) ECA Very Heavy Drinkers/One-time Alcohol Use Disorder Positives (ECA VHD/1t-AUDPs) and 2) ECA Alcohol-unaffecteds. Lifetime and past year alcohol use disorders, patterns of drinking and recovery among males and females are reported.
Results
84.6% of 2t-AUDPs again met lifetime DSM-III criteria at 14-year followup. At followup, only 9.3% male 2t-AUDPs and 20.7% female 2t-AUDPs met past year DSM-IV AUD criteria. Past year drinking patterns, however, revealed higher rates of DSM-IV AA or AD, problem- or risk drinking among 2t-AUDPs (61.7%) compared to both ECA VHD/1t-AUDPs (41.2%) and ECA Alcohol-unaffecteds (22.1%).
Conclusions
In a community sample, the rate of past year DSM-IV alcohol dependence was lower among male 2t-AUDPs than females, though both groups showed past year rates substantially lower than lifetime rates. However, less than half of ECA 2t-AUDPs exhibited low-risk or abstinent alcohol use behaviors, indicating that while remission from diagnosis is common, clinical relevance persists.
Keywords: Alcohol dependence, Risk drinking; Gender differences; Remission; Recovery; Disease course
1. Introduction
Numerous studies examining the course of alcoholism in treatment or high-risk samples indicate alcohol dependence (AD) is a chronic and serious disease with poor outcomes, medical comorbidities and mortality (Finney and Moos, 1991; Powell, et al., 1998; Noda, et al., 2001; Schuckit, et al., 2001). However, epidemiologic studies, which include high percentages of untreated cases, have shown elevated levels of remission from AD in individuals with lifetime history of alcoholism. Data from a recent large cross-sectional U.S. population study (National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), (NIAAA, 2001–2002)) found that 75.0% of individuals with onset of dependence prior to the past year no longer met criteria for AD within the past year. Additionally, 47.7% were without evidence of alcohol abuse (AA) or subclinical dependence problems. Moreover, rates of recovery increased with number of years since onset of dependence (Dawson, et al., 2005a). These findings mirrored a previous national study (National Longitudinal Alcohol Epidemiologic Survey (NLAES), (NIAAA, 1991–1992)) in which 72.2% of subjects with onset of AD prior to the past year no longer met past year AD or AA (Dawson, 1996a). Subclinical dependence symptoms were not elicited, likely accounting for the higher percentage of individuals in recovery than seen in NESARC. Keeping these important findings in mind, a potential shortcoming of these large population studies is their cross-sectional design which increases recall bias and attrition due to death in severely affected individuals.
Several prospective population studies have been completed which also demonstrate the finding that the course of alcoholism in community samples (i.e. untreated and treated individuals) tends to be less chronic compared to treatment only samples. De Bruijn et al. studied the three year course of alcohol use disorder in the Netherlands and found that 74% of subjects with DSM-IV AD (Diagnostic and Statistical Manual of Mental Disorders, version IV) (American Psychiatric Association, 1994) and 85% with DSM-IV alcohol abuse (AA) no longer met criteria at 3-year followup (de Bruijn, et al., 2006). The 5 year course of DSM-IV AA and AD in high-functioning males was studied by Schuckit, et al. revealing only 17.5% of males with AD at baseline retained that diagnosis 5 years later. Of men with baseline AA, only 19% again met criteria for AA at followup; 11.4% had gone on to develop AD (Schuckit, et al., 2000). Prospective community studies with very long followup periods portray a similar picture. For example, Vaillant followed two cohorts of males with a history of alcoholism over 60 years and found that alcohol dependence was rare by age 70 due both to death or stable abstinence. Of the core city (cohort 1, n=72) and college (cohort 2, n=19) survivors, 73% and 75%, respectively, had remitted by age 70 (Vaillant, 2003). Ojesjo’s 40 year followup of 41 males with a history of alcohol dependence, as identified in the Lundby general population study, showed 40% (50% of survivors) had stably remitted (Ojesjo, 2000). These longitudinal studies have added a great deal to our knowledge of the course of alcoholism in community populations. Yet, samples in these studies were predominantly male. As such, there remains a dearth of studies examining the natural history of alcoholism among women.
There exists consistent evidence of a unique course of disease in women. For example, a retrospective study of 419 treatment-seeking women enrolled in a multisite alcohol treatment matching study found that while women on average began getting drunk and experiencing problems later than men, they progressed more quickly than men from first getting drunk to first problems (Randall, et al., 1999). This “telescoping effect” has been documented by several other studies as well (Schuckit, et al., 1995; Johnson, et al., 2005). Additionally, females become addicted to alcohol at lower levels of use, and the durations to develop alcohol dependence and alcohol-related comorbidities are shorter in women than men. This suggests that, once heavy drinking starts, the female course to alcoholism is both faster and more severe when compared to males (NIAAA, 1999). Latest data from NESARC suggest the gap between male and female rates of AA are narrowing and, while the overall prevalence of AD has declined in the past decade, rates of AD are converging between men and women (Grant et al., 2004; Holdcraft and Iacono, 2002). Given these findings, further explication of the course and outcome of alcoholism in women over varied follow up periods is essential in order to improve gender-sensitive prevention and treatment.
Building on previous findings, our study seeks to expand current knowledge on the course of alcoholism. Large-scale government-initiated surveys that include DSM diagnostic measures have become more common. However, the Epidemiologic Catchment Area (ECA) survey, conducted in five sites throughout the U.S. in the early 1980s, was the first such study (NIMH, 1980–1985). Thus, this 14-year followup of the St. Louis site’s ECA provides important results on the long-term course of alcoholism at a diagnostic level, affording the unique opportunity to present both DSM-III and DSM-IV classifications. Additionally, the present study uses a prospective design with a long followup period and large sample size, allowing gender-specific comparisons. The goals of the present study are: a) to further elucidate the clinical course of alcoholism in a community sample prospectively followed up at 14 years; and b) to investigate whether there is evidence of gender differences. More specifically, we report the 14-year outcomes of drinking behaviors in individuals with DSM-III (Diagnostic and Statistical Manual of Mental Disorders, version III) (American Psychiatric Association, 1980) alcoholism compared with two comparison groups. Because focus on disorder alone might miss individuals who, though not meeting full diagnostic criteria, are still having problems with alcohol use, we also report rates of problem drinking, risk drinking, low risk drinking and abstinence. Finally, we describe the differential courses of drinking patterns between females and males.
2. Methods
2.1. Sample
The sample is a 14-year followup of a subsample of individuals who participated in both waves of the St. Louis Epidemiologic Catchment Area (ECA) Study between 1981 and 1983. The ECA Study had 5 sites throughout the United States, St. Louis being one of them. All participants in the St. Louis ECA were older than 18 years of age at the time of interview. 53% of participants in the St. Louis ECA were female, 80% were white, 19% were black and less than 1% were Hispanic. As Figure 1 illustrates, the St. Louis ECA had two waves of data collection between 1981 and 1983. Individuals participating in both waves constituted the sampling universe for the 14-year followup, occurring in 1997 (N=2527); ECA Waves 1 and 2 are considered collectively as baseline data for the 14-year followup. The 14-year followup study was originally designed to analyze health services use in individuals with a reliable past history of alcoholism (cases) compared to those without such history at the St. Louis ECA interviews (comparison groups).
Fig. 1.
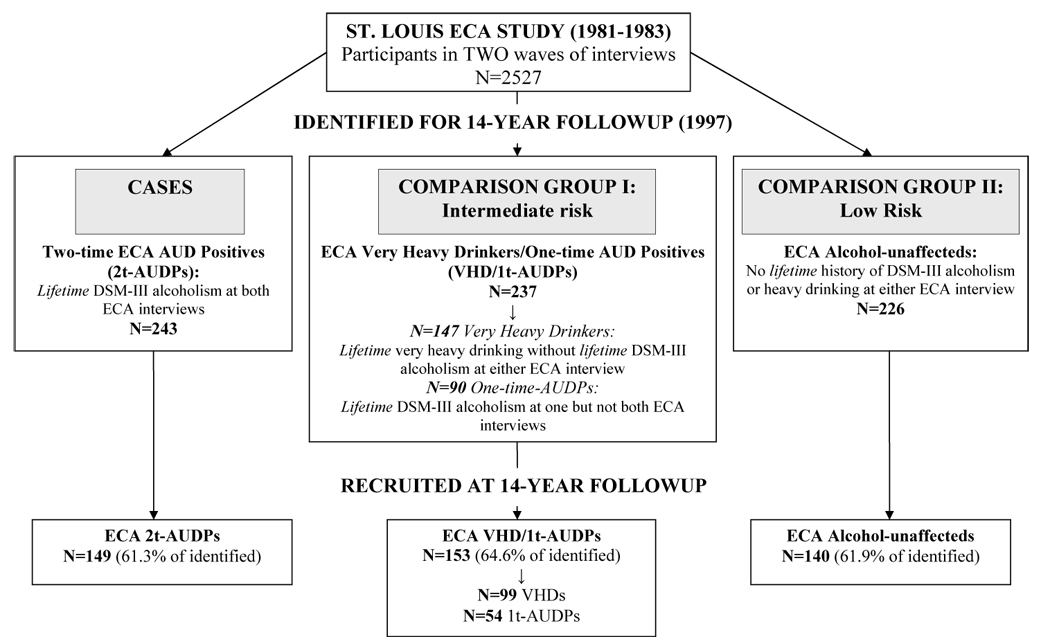
14-year followup study design
2.1.1. Cases
All individuals who met DSM-III lifetime criteria (i.e. reporting enough symptoms at any point in life to meet DSM-III criteria) for alcohol abuse (AA) and/or alcohol dependence (AD) at both 1981–1983 ECA waves (targeted N=243) were identified for followup interview 14-year later. This group is called “ECA Two-times Alcohol Use Disorder Positive (ECA 2t-AUDPs)” and constitutes cases in this case-control study. At the time the ECA was fielded, the official APA criteria were DSM-III and, thus, only these diagnoses were available. The DSM-III constructs of AA and AD differ from DSM-IV nomenclature. They are not hierarchical (i.e. one can have both abuse and dependence), tolerance or withdrawal are required for dependence, and the constructs do not require symptoms to cluster together in a specified period of time. Respondents were not required to meet an abuse criterion to get asked about dependence and questions about tolerance and withdrawal were not skipped if a respondent met criteria for AA. DSM-III AA requires A) a pattern of pathological alcohol use plus B) impairment in social or occupational functioning due to alcohol use, while DSM-III AD requires either A) or B) plus tolerance or withdrawal. 9.5% of participants who completed both interviews in the St. Louis ECA study (N=2572) qualified for the ECA 2t-AUDPs group (targeted N=243), all of whom were recruited for inclusion in the 14-year followup. 95% of the ECA 2t-AUDPs met criteria for DSM-III alcohol abuse with or without dependence at both ECA interviews. This highlights a difference between DSM-III alcoholism and DSM-IV AA or AD, namely, that it is very unusual for an individual to meet DSM-III AD without meeting criteria for alcohol abuse. Given this, we followed the ECA definition of DSM-III “alcoholism” to include DSM-III abuse and/or dependence (Helzer, et al., 1991).
2.1.2. Comparison groups
Two comparison groups—“ECA Very Heavy Drinkers/One-time Alcohol Use Disorder Positives” (ECA VHD/1t-AUDP) and “ECA Alcohol-unaffecteds”—were matched to the cases, “ECA Two-times AUD Positive” (ECA 2t-AUDPs), by age, gender and race. The comparison group, “ECA VHDs/1t-AUDPs” (targeted N=237), represented an intermediate-risk group and included two subsets of individuals: 1) primarily individuals with “very heavy drinking” without the presence of an AUD at either ECA interview, i.e. “ECA VHDs” (62%, N=147) and 2) additional individuals with an ECA AUD diagnosis at one ECA interview but not both, “One-time AUD Positive” (ECA 1t-AUDP) (48%, N=90). The inclusion of two different types of drinking patterns into one comparison group was part of the design of the original 14-year followup study and, therefore, is necessarily carried forward within this secondary data analysis.
Those with “very heavy drinking” (ECA VHDs) did not meet lifetime criteria for DSM-III alcoholism at either of the two 1981–83 ECA waves, but did endorse, at one or both interviews, 7 or more drinks in one day at least once a week for several months or 7 drinks daily for at least 2 weeks. No other quantity/frequency measures were obtained at ECA. Individuals with “one-time AUD diagnosis” (1t-AUDP) included those who met lifetime criteria for DSM-III alcoholism at only one 1981–83 ECA interview, but not both. Of these 90 individuals, 61% (N=55) were positive for a lifetime AUD at the first wave only. Conversely, 39% (N=35) were positive for a lifetime AUD at the second wave only. These 90 individuals are best thought of as unreliable reporters rather than as measures of both unreliability (for the 55 positive at Wave 1 only) or incident cases (for the 35 positive at Wave 2 only). This is because the measure for DSM-III alcoholism was “lifetime” only, i.e. symptoms were not required to begin within the preceding year for the 35 who met criteria for DSM-III alcoholism at the second but not the first wave. It is also important to note that this comparison group represents both individuals at increased risk for AUDs (“very heavy drinkers”) and individuals who have qualified for an AUD in the past, though not consistently across the two 1981–83 ECA interviews (“one-time AUDPs”). Thus, any comparison between the cases, ECA 2t-AUDPs, and the comparison group, ECA VHD/1t-AUDPs, is one of symptom severity and reliability (for the “1t-AUDP” individuals) as well as between those who did and did not experience symptomatology (for the “very heavy drinkers”) at the time of the St. Louis ECA.
The second comparison group, “ECA Alcohol-unaffecteds” (targeted N=226), was the control and included any individual without history of “very heavy drinking” or DSM-III alcoholism at either 1981–83 ECA interviews. Because information on lifetime abstention was unavailable from the ECA interviews, lifetime non-drinkers were included in the recruitment sample at 14-year followup. Four interviewed ECA Alcohol-unaffecteds (2 male, 2 female) reported no lifetime alcohol use at 14-year followup.
2.1.3. Responden ascertainment
In 1997, at the 14-year followup study, 706 individuals (243 ECA 2t-AUDPs, 237 ECA VHD/1t-AUDPs, 226 ECA Alcohol-unaffecteds) were identified for interview. Of these 706, 144 were deceased (20.4%), 442 were interviewed (62.6%) and 120 were not interviewed due to refusal (n=91, 12.9%), illness (n=15, 2.1%) or inability to locate (n=14, 2.0%). Among those located, alive and able to be interviewed, participation rate was 82.9%. A total of 149 ECA 2t-AUDPs, 153 ECA VHD/1t-AUDPs (64.7% “very heavy drinkers,” (N=99); 35.3% with “1t-AUD diagnosis” (N=54)), and 140 ECA Alcohol-unaffecteds comprised the analytical sample in the current study.
Ascertainment status was significantly associated with ECA alcohol use status. The male comparison groups, ECA VHD/1t-AUDPs (16.0%) and ECA Alcohol-unaffecteds (17.4%), were more likely to refuse interview compared with male cases, ECA 2t-AUDPs (9.2%) (p=.05, p=.02, respectively). Additionally, male ECA 2t-AUDPs were more likely to be dead at followup (26.7%), compared with male ECA VHD/1t-AUDPs (16.3%, p=.01) but not ECA Alcohol-unaffecteds (20.2%, p=.14). Female cases, ECA 2t-AUDPs, were more likely to be unlocated at followup (10.4%) compared to female ECA Alcohol-unaffecteds (0%, p=.02) but not female ECA VHD/1t-AUDPs (2.1%, p=.10). Despite differences in reasons for attrition, however, the proportion of interviewed among those able to be interviewed was not significantly different across the 3 ECA groups (80–87%, p=0.20) or by gender (81.5% males v. 88.8% females, p=.07), though there was a trend toward more participation by women.
2.2. Study assessments
The 1997 14-year followup study collected data by telephone. Questions operationalizing DSM-III and DSM-IV criteria for alcohol abuse and/or dependence were included using the Diagnostic Interview Schedule, version III (DIS-III) questions from the original 1981–83 ECA interviews and questions from a later version of the DIS, version IV (Robins, 1981a; Robins et al., 1999). The DIS is a highly structured interview with well-established reliability and validity (Robins, et al., 1981b; Robins, et al., 1982; Helzer et al., 1985; Compton and Cottler, 2004).
2.3. Measures of lifetime and past year DSM-III and IV alcohol use disorders
Our DSM-III definition of “alcoholism” included those who met criteria for either DSM-III alcohol abuse (AA) and/or dependence (AD) at any point in their life (i.e. “lifetime” DSM-III alcoholism). Since DSM-III alcoholism was asked about as “lifetime,” subjects affected at the 1981–83 ECA study should have met the same criteria at the 14-year followup, assuming retrospective stability of reporting over time.
To meet a lifetime DSM-IV AD diagnosis, respondents had to satisfy at least three of seven dependence criteria and these symptoms must have clustered together within any 12 month period. A lifetime DSM-IV AA diagnosis required at least one of four symptoms occurring repeatedly within any 12 month period.
We do not report rates of past year DSM-III alcoholism because a precise measure of this construct was not elicited at followup. In our analyses, however, we created a proxy measure which provided results similar to past year DSM-IV AA or AD. Given this, we report past year DSM-IV AA and AD only.
2.4. Measures of past year drinking behaviors, remission and recovery
In addition to focusing on disorder, we created a hierarchical variable incorporating problems and levels of alcohol consumption similar to one based on the 2001–02 NESARC study (Dawson, et al., 2005a). In clinical practice, remission from AD is defined on the basis of continued presence of one or more abuse or dependence symptoms. “Full remission” from AD implies no evidence of any abuse or dependence symptom, while “partial remission” implies having only one or two dependence criteria or one abuse criteria. These definitions of remission, however, do not capture individuals whose level of alcohol consumption, though not causing DSM-IV disorder, still puts them at high risk for relapse to dependence.
Therefore, in order to capture a finer categorization of the current alcohol use status of our sample, we created a variable with 5 mutually exclusive levels encompassing, 1) DSM-IV AUD, 2) problem drinking, 3) risk drinking, 4) low-risk drinking, and 5) abstention. “DSM-IV AUD” includes those who met full criteria for DSM-IV AA and/or AD in the past year. “Problem drinkers” did not meet past year DSM-IV AA or AD criteria but reported at least one alcohol-related problem in the past year. Clinically, ECA 2t-AUDPs with past year problem drinking are in “partial remission.” “Risk drinkers” did not have DSM-IV AUD or problem drinking behaviors but did meet criteria for past year risk drinking. “Risk drinking” was analyzed using the NIAAA definition of: a) more than 14 drinks per week for men (more than 7 for women), or b) more than 4 drinks (more than 3 for women) on any day in the past year (NIAAA, 2005; see also Dawson, 2000). Because our interview did not obtain average daily maximum consumption, however, we used self reported intoxication at least once in the past 12 months (same for men or women) to approximate the NIAAA guidelines of b) more than 4 drinks (more than 3 for women) on a single occasion in the past year. “Low risk drinkers” were current drinkers not meeting the conditions for DSM-IV AUD, problem-or risk drinking. Finally, those who reported alcohol abstention in the last year were classified as “Abstainers.”
Rates of recovery among the ECA 2t-AUDPs were determined by combining “Low risk drinkers” and “Abstainers.” This definition of recovery is more stringent than DSM-IV’s definition of “full remission.” In addition to the DSM-IV’s “full remission” requirement of being without evidence of any abuse or dependence symptom, “recovery” takes into account the level of alcohol consumption. Therefore, individuals in “recovery” from AD not only had no evidence of a past year AUD or any past year problems, but also were drinking in ways considered “low risk” for development of an AUD. According to this categorization, ECA 2t-AUDP individuals with problem- or risk drinking behaviors, while perhaps in “partial” or “full remission,” respectively, are not said to be in “recovery.”
2.5. Statistical analyses
Between group characteristics were analyzed using χ2 tests for all categorical predictors and one-way ANOVAs for continuous measures. Because the purpose of the study was to contrast cases with each comparison group, ECA 2t-AUDPs are the reference group. Thus, no comparisons of ECA VHD/1t-AUDPs and ECA Alcohol-unaffecteds are shown. While weights were used at the original ECA, the purpose of the 14-year followup was to describe the longitudinal course of individuals with DSM-III alcoholism 14 years later. Weighting was not applied in the followup study design and, as a consequence, weights were not used in this analysis. Chi-square tests were used to compare ECA 2t-AUDPs to each comparison group examining the relationship between ECA alcohol status and both lifetime and past year alcohol use disorders and past year drinking patterns. An α-level of 0.05 was considered significant. All statistical analyses were performed using SAS for Windows, Version 8.2.
3. Results
3.1. Sociodemographic characteristics
As displayed in Table 1, a majority of study participants were white (81.6% of males, 63.2% of females) and male (78.5%) with a mean age of 50.1 (±10.1) years at the 14-year followup. This reflects the fact that both comparison groups were frequency matched to cases on key demographic characteristics, including age, gender and ethnicity. Thus, because persons meeting criteria for DSM-III AA or AD at the time of ECA were overwhelmingly young, white and male, this is reflected in the demographics of the entire 14-year followup sample.
Table 1.
Sample characteristics at 14-year followup
| Group 1 | Group 2 | Group 3 | |||
|---|---|---|---|---|---|
| ECA Alcohol-unaffecteds | ECA VHD/1t-AUDPs | ECA 2t-AUDPs | Groups 1 v. 3a | Groups 2 v. 3a | |
| Total sample | (N=140) | (N=153) | (N=149) | ||
| Mean age (SD) | 50.2 (10.8) | 50.8 (10.5) | 49.3 (9.1) | 0.41 | 0.16 |
| % male | 75.0 | 79.7 | 80.5 | 0.26 | 0.86 |
| % white | 75.7 | 75.8 | 81.2 | 0.26 | 0.25 |
| % currently married | 67.4 | 63.6 | 57.0 | 0.07 | 0.25 |
| % educated beyond HSb | 53.8 | 50.4 | 50.7 | 0.61 | 0.95 |
| % past year fulltime employment | 70.3 | 62.9 | 65.8 | 0.41 | 0.60 |
| $ mean household income × 100 (SD) | 51.0 (32.4) | 46.6 (30.0) | 46.6 (30.6) | 0.24 | 1.00 |
| Males | (N=105) | (N=122) | (N=120) | ||
| Mean age (SD) | 50.2 (10.9) | 50.9 (10.4) | 49.2 (8.8) | 0.45 | 0.17 |
| % white | 81.0 | 79.5 | 84.2 | 0.53 | 0.35 |
| % currently married | 72.8 | 70.8 | 65.0 | 0.21 | 0.33 |
| % educated beyond HS | 63.2 | 49.1 | 55.4 | 0.26 | 0.35 |
| % past year fulltime employment | 78.6 | 65.8 | 70.8 | 0.18 | 0.40 |
| $ mean household income × 100 (SD) | 57.3 (32.2) | 49.0 (30.4) | 51.5 (30.2) | 0.16 | 0.53 |
| Females | (N=35) | (N=31) | (N=29) | ||
| Mean age (SD) | 50.3 (10.9) | 50.5 (11.2) | 49.5 (10.2) | 0.75 | 0.72 |
| % white | 60.0 | 61.3 | 69.0 | 0.46 | 0.53 |
| % currently married | 51.4 | 35.5 | 24.1 | 0.03c | 0.34 |
| % educated beyond HS | 28.6 | 54.8 | 32.1 | 0.76 | 0.08 |
| % past year fulltime employment | 45.7 | 51.6 | 44.8 | 0.94 | 0.60 |
| $ mean household income × 100 (SD) | 32.4 (25.5) | 36.7 (26.6) | 26.7 (23.5) | 0.36 | 0.13 |
P-values represent differences between ECA 2t-AUDPs and a) ECA Alcohol-unaffecteds (1 v. 3) and b) ECA VHD/1t-AUDPs (2 v. 3) using χ2 tests. Age and income used one-way ANOVAs
Any education after high school (HS) graduation
Statistically significant findings (p<.05) are in bold
There was no significant difference between the three groups (ECA 2t-AUDPs, ECA VHD/1t-AUDPs, and ECA Alcohol-unaffecteds) with respect to age, ethnicity, employment status, level of education or mean household income. However, there was a significant difference in marital status among females, with ECA Alcohol-unaffecteds having a two-fold higher rate of current marriage than female ECA 2t-AUDPs (51.4% v. 24.1%, respectively, (p=0.03)).
3.2. Lifetime and past year alcohol use disorders
At 14-year followup, 84.2% of male and 86.2% of female ECA 2t-AUDPs again met lifetime criteria for DSM-III alcoholism (data not shown). As might be expected, those ECA 2t-AUDPs who did not requalify for lifetime DSM-III alcoholism at the 14-year followup had reported a lower mean number of DSM-III AA and/or AD symptoms at the first 1981–83 ECA interview (mean=3.4, SD=1.9) compared to those who did requalify (mean=5.9, SD=3.4, p=0.001; results similar for the second ECA interview), indicating less severe illness at the time of the 1981–83 ECA study.
As shown in Table 2, results among ECA 2t-AUDPs were similar for lifetime DSM-IV diagnoses, where 79.2% of male and 82.8% of female ECA 2t-AUDPs met lifetime DSM-IV AA and/or AD criteria at followup. In contrast, 54.9% and 22.9% of male ECA VHD/1t-AUDPs and ECA Alcohol-unaffecteds, respectively, and 41.9% and 2.9% of female heavy drinkers and ECA Alcohol-unaffecteds, respectively, met DSM-IV criteria for lifetime AA and/or AD at 14-year followup.
Table 2.
Lifetime and past year DSM-IV alcohol use disorders (AUDs) at follow-up, by ECA drinking status and gender
| Lifetime diagnoses: | Past year diagnoses:d | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | Group 2 | Group3 | Group 1 | Group 2 | Group3 | |||||||
| ECA Alcohol-unaffecteds (%) | ECA VHD/1t-AUDPs(%) | ECA 2t-AUDPs(%) | Groups 1 v. 3a | Groups 2 v. 3a | ECA Alcohol-unaffecteds (%) | ECA VHD/1t-AUDPs (%) | ECA 2t-AUDPs (%) | Groups 1 v. 3a | Groups 2 v. 3a | |||
| Total Sample | (N=140) | (N=153) | (N=149) | Total Sample | (N=136)d | (N=153) | (N=149) | |||||
| DSM-IV | DSM-IV | |||||||||||
| AA and/or AD | 17.9 | 52.3 | 79.9 | <.0001b | <.0001 | AA and/or AD | 1.4 | 8.6 | 11.6 | <.001b | 0.39 | |
| AA only | 16.4 | 29.4 | 28.9 | 0.01 | 0.92 | AA only | 1.4 | 3.3 | 2.7 | 0.48 | 0.76 | |
| AD | 1.4 | 22.9 | 51.0 | <.0001 | <.0001 | AD | 0.0 | 5.3 | 8.9 | <.001 | 0.22 | |
| AD and abusec | 0.7 | 13.7 | 39.6 | <.0001 | <.0001 | AD and abusec | 0.0 | 4.6 | 1.4 | 0.17 | 0.10 | |
| Males | (N=105) | (N=122) | (N=120) | Males | (N=103)d | (N=122) | (N=120) | |||||
| DSM-IV | DSM-IV | |||||||||||
| AA and/or AD | 22.9 | 54.9 | 79.2 | <.0001 | <.0001 | AA and/or AD | 2.0 | 9.1 | 9.3 | 0.02 | 0.95 | |
| AA only | 21.0 | 30.3 | 30.8 | 0.09 | 0.93 | AA only | 1.9 | 3.3 | 3.3 | 0.52 | 0.98 | |
| AD | 1.9 | 24.6 | 48.3 | <.0001 | <.001 | AD | 0.0 | 5.8 | 6.0 | 0.01 | 0.95 | |
| AD and abusec | 1.0 | 15.6 | 37.5 | <.0001 | <.001 | AD and abusec | 0.0 | 5.8 | 1.7 | 0.18 | 0.10 | |
| Females | (N=35) | (N=31) | (N=29) | Females | (N=33)d | (N=31) | (N=29) | |||||
| DSM-IV | DSM-IV | |||||||||||
| AA and/or AD | 2.9 | 41.9 | 82.8 | <.0001 | <.01 | AA and/or AD | 0.0 | 6.4 | 20.7 | <.01 | 0.10 | |
| AA only | 2.9 | 25.8 | 20.7 | 0.02 | 0.64 | AA only | 0.0 | 3.2 | 0.0 | N/A | 0.33 | |
| AD | 0.0 | 16.1 | 62.1 | <.0001 | <.001 | AD | 0.0 | 3.2 | 20.7 | <.01 | 0.04 | |
| AD and abusec | 0.0 | 6.4 | 48.3 | <.0001 | <.001 | AD and abusec | 0.0 | 0.0 | 0.0 | N/A | N/A | |
P-values represent differences between ECA 2t-AUDPs and a) ECA Alcohol-unaffecteds (1 v. 3) and b) ECA VHD/1t-AUDPs (2 v. 3) using χ2 tests
Statistically significant findings (p<.05) are in bold
DSM-IV alcohol dependence (AD) does not distinguish between AD with abuse symptoms and AD without. “AD and abuse” indicates meeting criteria for both
4 respondents (2 males, 2 females) in the ECA alcohol-unaffected group were lifetime non-drinkers and were excluded in calculations for past year diagnoses
Because there were two ways to qualify for inclusion in the ECA Very Heavy Drinkers/One-time AUD Positive (VHD/1t-AUDPs) group, we compared lifetime DSM-III and DSM-IV outcomes on those reporting “very heavy drinking” only at either 1981–83 ECA interview (65% of ECA VHD/1t-AUDPs) with those who met criteria for DSM-III alcoholism at one ECA interview but not the other, “1t-AUDPs” (35%). Among the 65% who reported “very heavy drinking” without meeting criteria for an AUD at either ECA interview, 33.0% converted to lifetime DSM-III alcoholism (48.5% to lifetime DSM-IV AA and/or AD) by 14-year followup, highlighting the disease risk associated with these drinking patterns. Of the 35% who were “1t-AUDPs” at ECA, 53.7 % again met lifetime DSM-III alcoholism (59.3% met lifetime DSM-IV AA and/or AD) at followup (See online supplemental material for additional details).
Past year rates of DSM-IV alcohol use disorders (AUDs) are also displayed in Table 2. In contrast to lifetime prevalence, past year DSM-IV AA and/or AD were strikingly low among males in all three ECA groups, suggestive of a high rate of past year remission among the ECA 2t-AUDPs—either full or partial. Only 9.3% of male ECA 2t-AUDPs met criteria for past year DSM-IV AA and/or AD. This rate did not differ significantly from either male ECA VHDs or 1t-AUDPs, of whom 9.1% met criteria for a DSM-IV AUD (7.1% of VHDs and 11.8% of 1t-AUDPs, respectively. See online supplemental material for full details). Rates of past year diagnosis were significantly higher in male ECA 2t-AUDPs when compared with male ECA Alcohol-unaffecteds, however, of whom 2.0% met past year criteria for a DSM-IV AUD (p=0.02).
A somewhat different pattern of past year alcohol use disorders was observed for female ECA 2t-AUDPs. While, like males, past year rates of DSM-IV AA and/or AD were low among female ECA 2t-AUDPs (20.7% compared with a lifetime rate of 82.8%), the rate of past-year DSM-IV AD (20.7%) was, nonetheless, significantly higher than seen in male counterparts (20.7% v. 6.0%, p=.01). When combining past year rates of AA and/or AD, there was a trend for rates of past year DSM-IV AA and/or AD to be higher among female ECA 2t-AUDPs (20.7%) compared to male ECA 2t-AUDPs (9.3%, p<.09). Female ECA VHD/1t-AUDPs showed rates that paralleled those in men, with 6.4% meeting past year DSM-IV AUD criteria. Because so few females were “1t-AUD Positive (1t-AUDPs)” at ECA (n=3), separate analyses for this group were not done. No female ECA Alcohol-unaffecteds met criteria for any past year AUD.
3.3. Past year drinking behaviors and rates of recovery
Individuals who do not meet criteria for past year DSM-IV AA or AD may still be drinking at levels that put them at risk for relapse to dependence. Therefore, to examine this, we created a 5 level hierarchical variable, modeled after a similar construct in NESARC studies (Dawson, et al., 2005a), incorporating alcohol use disorder, problems with alcohol use, and consumption levels (measuring both the frequency and quantity of alcohol intake known to put individuals at risk of developing an AUD). As seen in Table 3, overall drinking patterns were significantly different between male ECA 2t-AUDPs and both ECA VHD/1t-AUDPs and ECA Alcohol-unaffecteds (p<.01 and <.0001, respectively). Overall drinking patterns among female ECA 2t-AUDPs also differed compared to ECA Alcohol-unaffecteds (p<.001) and there was a trend toward significant difference when compared to ECA VHD/1t-AUDPs (p=.05).
Table 3.
Past year drinking patterns at 14-year followupa
| Group 1 | Group 2 | Group 3 | |||
|---|---|---|---|---|---|
| ECA Alcohol-unaffecteds (%) | ECA VHD/1t-AUDPs (%) | ECA 2t-AUDPs (%) | Groups 1 v. 3b | Groups 2 v. 3b | |
| Males | (N=105) | (N=122) | (N=120) | ||
| 1. DSM-IV AA or AD | 1.9 | 9.0 | 9.3 | ||
| 2. Problem drinker | 8.6 | 17.2 | 33.3 | ||
| 3. Asymptomatic risk drinker | 10.5 | 14.8 | 20.8 | ||
| 4. Low-risk drinker | 52.4 | 36.9 | 19.2 | ||
| 5. Abstainer | 26.7 | 22.6 | 17.5 | <.0001c | <.01 |
| “Risk Plus”d | 21.0 | 41.0 | 63.3 | <.0001 | <.001 |
| Female | (N=35) | (N=31) | (N=29) | ||
| 1. DSM-IV AA or AD | 0 | 6.4 | 20.7 | ||
| 2. Problem drinker | 2.9 | 9.7 | 27.6 | ||
| 3. Asymptomatic risk drinker | 22.9 | 25.8 | 6.9 | ||
| 4. Low-risk drinker | 42.9 | 35.5 | 20.7 | ||
| 5. Abstainer | 31.4 | 22.6 | 24.1 | <.001 | 0.07 |
| “Risk Plus”d | 25.7 | 41.9 | 55.2 | 0.02 | 0.30 |
Patterns of drinking are presented using a 5 level severity scale and are mutually exclusive: 1) past year DSM-IV alcohol abuse or dependence; 2)≥1 past year drinking problem without DSM-IV AA or AD; 3) drinking, on average, >14 drinks/week (>7 for women) OR physical signs of intoxication at least once in past 12 months without AUD or problem drinking; 4) drinkers without any AUD, problem- or risk drinking; 5) past year alcohol abstention
P-values represent differences between ECA 2t-AUDPs and a) ECA Alcohol-unaffecteds (1 v. 3) and b) ECA VHD/1t-AUDPs (2 v. 3) using χ2 tests
Statistically significant findings (p<.05) are in bold
“Risk Plus” indicates % with any AUD, problem- or risk drinking patterns; it excludes low-risk drinkers and abstainers only
More specifically, past year DSM-IV AUD diagnoses, problem- or risk drinking, collectively termed “risk plus,” were more common among ECA 2t-AUDPs than both the ECA VHD/1t-AUDPs and the ECA Alcohol-unaffected comparison groups. Among males, 63.3% of ECA 2t-AUDPs compared to 41.0% of ECA VHD/1t-AUDPs (p<.001, also significant for VHD and 1t-AUDP groups separately) and 21.0% ECA Alcohol-unaffecteds (p<.0001) were drinking at or above a threshold considered risky (“risk plus”), modeled after the NIAAA clinical guidelines (NIAAA, 2005). Among females, 55.2% of ECA 2t-AUDPs were in the “risk plus” category, compared to 41.9% of ECA VHD/1t-AUDPs (p=NS) and 25.7% of ECA Alcohol-unaffecteds (p=0.02). Thus, while only 9.3% of male ECA 2t-AUDPs met criteria for a past year DSM-IV AUD, an additional one-third (33.3%) reported at least one past year drinking problem and 20.8% reported risk drinking. Similarly, 27.6% of female ECA 2t-AUDPs reported at least one problem with alcohol in the past year and 6.9% reported risk drinking, in addition to the 20.7% with past year DSM-IV AUD.
We questioned whether representing problem drinking to be a more severe category than risk drinking was a valid assumption. Therefore, we looked at problem drinkers to determine if they also exhibited risk drinking patterns in addition to reported problems. Indeed, of male problem drinkers, 77.1% reported levels of consumption meeting risk-drinking threshold (100% female problem drinkers), implying that problem drinkers are also high quantity and/or frequency drinkers.
Combining low-risk drinkers and abstainers, 36.7% male and 44.8% female ECA 2t-AUDPs met our criteria for recovery (i.e. no DSM-IV AUD, problem- or risk drinking). The two comparison groups showed higher rates of low-risk drinking or abstinence. Among men, 59.0% of ECA VHD/1t-AUDPs and 79.0% of ECA Alcohol-unaffecteds were either past year low-risk drinkers or abstainers. Among women, 58.1% and 74.3% of ECA VHD/1t-AUDPs and ECA Alcohol-unaffecteds, respectively, either abstained or were low-risk drinkers. Notably, among the ECA 2t-AUDPs who met criteria for recovery, about half (52.3% male, 46.0% female) had returned to low-risk patterns of drinking in the past year, i.e. non-abstinent recovery.
4. Discussion
4.1. Gender differences
Some interesting results emerged from the gender-specific analysis. Female ECA 2t-AUDPs were more than three times likely to meet past year DSM-IV AD diagnosis (and more than two times likely to meet any DSM-IV AUD) than their male counterparts (See Table 2). Prior research has shown that severity of illness is the greatest predictor for the stability of alcoholism (Culverhouse, et al., 2005). Diagnosed in the early 1980s when prevalence of female drinking was lower and alcohol use disorders among females more stigmatizing than today, the female ECA 2t-AUDPs in our study may represent more severe cases with a lower likelihood of full or partial remission over time. At 14-year followup, we had good participation rates and were able to locate all but 14 of the 706 (98%) respondents targeted for the study. However, of those fourteen, five (36%) were female ECA 2t-AUDPs. This may evidence severe illness and/or poor social support.
Another possible explanation for the higher degree of persistence is that female ECA 2t-AUDPs had fewer economic and social resources than their male counterparts as implied by their low household incomes and percent currently married. Additionally, though the majority of female ECA 2t-AUDPs were not currently married, many had a history of living with a heavy- or problem drinking partner. Thus, the chronic course in females with alcoholism may have been influenced by a history of living in an environment that promoted development of and continued disease. Fourthly, ECA alcoholic females may have more comorbid medical conditions (Grazier et al., 1999) that make recovery more difficult compared to men. Finally, the persistence of alcoholism seen in our sample females may be indicative of a different clinical course of alcoholism in women. All of these possible explanations point to the need for further research and analyses to determine differential risks and protective effects among women compared to men.
Another interesting finding was the very low rate of lifetime DSM-IV AA and/or AD in female ECA Alcohol-unaffecteds. At 14-year followup, only 2.9% met lifetime criteria for DSM-IV AA and none met criteria for lifetime DSM-IV AD. Such results are expected in light of strong and consistent evidence that the age of risk for an AUD is late adolescence/early adulthood, a period which most individuals in this sample had passed through by the time of the St. Louis ECA (Heltzer, et al., 1991; Grant, 1997; Grant et al., 2004). Beyond this age, there appears only modest incidence of alcohol use disorders.
4.2 Stability of lifetime AUD diagnoses
These data from a 14-year followup of a well defined community sample with a large sample size reveal high recall accuracy among those with a lifetime alcohol use disorder. The vast majority (84.6%) of ECA 2t-AUDPs requalified for lifetime DSM-III diagnosis at followup and a comparable percentage (79.9%) of ECA 2t-AUDPs met lifetime criteria for DSM-IV AA and/or AD. Of the 15.4% who did not requalify for diagnosis at 14-year followup, we found a lower mean number of symptoms at the baseline ECA interviews, indicating less severe illness. Other studies have shown similar stability of lifetime AD diagnosis over varying lengths of time (Demallie, et al., 1995; Schuckit, et al., 2001; Culverhouse, et al., 2005). There appeared to be a dose-response relationship between reported alcohol use behaviors at the 1981–83 interviews and prevalence of lifetime AUD 14 years later. Among ECA VHD/1t-AUDPs, 40.5% met lifetime DSM-III alcoholism diagnosis at 14-year followup (33.0% of VHDs, 53.7% of 1t-AUDPs). This suggests that requiring DSM-III AUD diagnosis be met at two time points in order to be included in the ECA 2t-AUDPs group identified those with severer illness and more accurately captured true cases. Additionally as mentioned, 33.0% of ECA “very heavy drinkers” (ECA VHDs) failing to qualify for DSM-III alcoholism at either ECA interview, “converted” to lifetime DSM-III alcoholism by the 14-year followup compared to 9.3% of ECA Alcohol-unaffecteds, thus, highlighting the at-risk nature of these behaviors.
4.3 Rates of remission from alcohol use disorders
When past year diagnoses were considered, rates of remission from alcohol use disorders (AUDs) were high among those with a history of alcoholism. At followup, only 9.3% of male and 20.7% of female ECA 2t-AUDPs met past year criteria DSM-IV AA and/or AD. Yet, problem- and risk drinking persisted among ECA 2t-AUDPs, even when not meeting criteria for an AUD. Studies have shown that risk drinking is associated with greater possibility of developing alcohol use disorders and several major chronic diseases (Rehm, et al., 2003; Dawson, et al., 2005b). Predicting from this that risk drinking also increases the likelihood of relapse among individuals in full or partial remission from AUDs, this finding has important clinical implications. In particular, it underscores the need to repeatedly screen drinking behaviors using the NIAAA risk drinking guidelines in individuals with a prior history of alcoholism or heavy drinking. Many clinicians rely on the CAGE questionnaire (Ewing, 1984), which has high specificity but will likely miss at-risk behaviors. Reliance on DSM-IV criteria alone, though catching diagnosis once relapse has occurred, will likely miss those at risk for relapse.
Our results are consistent with a recent report from NESARC of individuals with onset of alcohol dependence prior to the past year. In that sample, of subjects with onset of alcohol dependence 10–19 years prior to interview (time course comparable to our sample), three quarters no longer met criteria for DSM-IV AA or AD, yet 20% continued to have subclinical dependence symptoms and 16% more reported risk drinking (Dawson, et al., 2005a). While our ECA 2t-AUDP sample reported lower rates of past year DSM-IV AA and/or AD (11%), we found more subclinical problems and risk drinking (50%), reaching a conclusion similar to that of the NESARC investigators, namely, that remission from AUDs alone do not capture the full extent of alcohol use pathology.
4.4 Rates of recovery
A significant minority (38%) of ECA 2t-AUDPs (37% male, 45% female) reported past-year recovery from an AUD, i.e. without evidence of any AUD, problem- or risk drinking. This rate is highly consistent with NESARC findings where 39% of individuals with onset of dependence 10–19 years prior were in recovery (Dawson, et al., 2005a). Also consistent with NESARC findings, non-abstinent recovery (i.e. drinking at low-risk levels) in ECA 2t-AUDPs accounted for 51% (52% male, 46% female) of those in recovery (53% in NESARC), thus, providing further evidence that past year recovery is possible without abstinence in a community sample. While past year recovery is a less valid predictor for stable recovery than longer periods of low-risk behaviors (Vaillant, 2003), these rates nonetheless underscore the remitting nature of alcohol use disorders, at least in this community sample where milder cases of dependence are more common than would be observed in treated-only samples.
4.5 Limitations
Several limitations of this analysis exist. First, the two comparison groups were frequency matched to cases on age, race and gender and, thus, the sample as a whole reflects individuals who lived in St. Louis in the early 1980s and survived to the time of followup. This limits the generalizability of our results to other populations.
Second, the St. Louis ECA (1981–83) did not elicit past year DSM-III alcohol abuse or dependence; rather, it obtained lifetime diagnoses only at both waves. Therefore, precise rates of remission from DSM-III alcoholism at 14-year followup are unavailable. However, analysis using a proxy measure of past year DSM-III alcoholism mimicked rates of past year DSM-IV AA and/or AD, allowing reasonable inferences. Similarly, because we lacked full criteria for a past year DSM-III alcoholism diagnosis, we were unable to assess the duration of remission for the ECA 2t-AUDPs. Nonetheless, the general 14-year followup results of a) high past year remission from an AUD but b) low past year rates of recovery from any drinking problem or risk drinking behaviors are not altered by the absence of this information.
Third, our definition of “risk drinking” was modified from NIAAA guidelines. Those guidelines outline thresholds on both frequency and quantity of drinking. By using self reported signs of intoxication at least once in the past 12 months (same for men or women) to approximate the quantity threshold of the NIAAA guidelines (more than 4 drinks (3 for women) on a single occasion in the past year), we possibly introduced estimation error (most likely overestimating the amount of past year risk drinking). To correct for this, we reanalyzed our results using a higher threshold, i.e. reported signs of intoxication at least three times in the past year. While rates of risk drinking went down in all groups, conclusions remained the same, i.e. while past year remission from diagnosis is common among those with a prior history of DSM-III alcoholism, problem-or risk drinking behaviors remain significant.
Fourth, this analysis includes self-report data only, obtained from a telephone survey. Because no corroborating information is available, recall bias and minimization by participants may have been significant. Unfortunately, this self-report limitation is most often unavoidable in large community surveys, such as the one conducted here. However, the high lifetime stability of DSM-III alcoholism diagnosis at 14-year followup points to good recall of prior drinking habits.
Our results also contain a possible bias toward more severe illness because cases had to meet criteria for DSM-III alcoholism twice in order to be included. Additionally, it is important to recognize that the 1981–83 ECA was not designed to look solely at alcohol abuse or dependence. Rather, its purpose was to obtain prevalence rates on and characterizations of numerous psychiatric disorders in the general population. Finally, our gender-specific analyses are limited by the small sample of women. Even so, many of the analyses among women remained statistically significant.
5. Conclusions
While these results confirm previous studies showing moderate rates of remission among those with a history of alcoholism, they also point to the importance of screening such individuals for subdiagnostic levels of drinking even decades after the onset of dependence. Screening measures like the CAGE (Ewing, 1984) tap into more severe illness and may miss problem- and other at-risk drinking in a community population. On the other hand, our results indicate that non-abstinent recovery certainly occurs. This is particularly significant for primary care physicians who encounter patients with milder forms of alcohol use disorders than addiction specialists and, therefore, may target non-abstinent recovery as a likely goal. Even as this observation is noted, caution is warranted given the short (i.e. 1 year) period of observed recovery. Vaillant has advocated individuals in recovery be followed for at least 5 years to determine whether recovery is stable (Vaillant, 2003).
Finally, our findings among female ECA 2t-AUDPs warrant close attention. Over the last 25 years since ECA, the gender gap in alcohol use disorders has narrowed and prevalence rates among females are increasing (Holdcraft and Iacono, 2002; Grant, et al., 2004). Recognizing the higher degree of persistence of AUDs among females in our sample compared to men, important questions arise as to whether this is merely a cohort effect, a result of limited social and economic resources, affected-partner status or higher comorbidity, or rather reflects a different clinical course of alcoholism in females. These questions highlight the need for a nationally representative longitudinal study with a long followup period, such as is being planned with NESARC, in order to confirm generalizability of our results. If the clinical course of alcoholism among females is indeed more persistent, this will have serious public health consequences in a nation where rates of alcohol use and alcohol use disorders among women are climbing and where comorbidity and poor outcomes develop more rapidly than in men.
Supplementary Material
Acknowledgements
A preliminary version of these results was presented at the 2006 Guze Symposium at Washington University in St. Louis, MO, March 2006 and at the National Institute of Drug Abuse Research Training Institute in Bethesda, MD, April 2006. Additionally, this paper was used as a thesis defense for a master degree in psychiatric epidemiology at Washington University, February 2007 and we kindly thank Drs. Cottler, Lynskey, and Price for their review and contribution.
Role of Funding Source Funding for this study was provided by National Institutes of Health Grants AA10333, AA11998 and AA12640 (National Institute of Alcohol Abuse and Alcoholism) and KO8MH64134 and T32MH17104-23 (National Institute of Mental Health). The NIH had no further role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplementary results of this study can be viewed by accessing the online version of this paper at http://dx.doi.org by entering doi:xxxxxxxx.
Contributors Authors Bucholz and Grazier designed the study, wrote the protocol and received the funding. Authors Edens, Bucholz and Glowinski undertook the statistical analysis. Authors Bucholz and Glowinski provided mentoring for the first author, and author Edens wrote the first draft of the manuscript. All authors contributed to and have approved of the final manuscript.
Conflict of Interest All authors declare that they have no conflicts of interest.
References
- American Psychiatric Association Task Force on Nomenclature and Statistics. Diagnostic and Statistical Manual of Mental Disorders, third ed. (DSM-III) Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, fourth ed. (DSM-IV) Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Booth BM, Fortney SM, Fortney JC, Curran GM, Kirchner JE. Short-term course of drinking in an untreated sample of at-risk drinkers. J. Stud. Alcohol. 2001;62:580–588. doi: 10.15288/jsa.2001.62.580. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Zipp JF, Robins LN, Spitznagel EL. Difficult-to-recruit respondents and their effect on prevalence estimates in an epidemiologic survey. Am. J. Epidemiol. 1987;125:329–339. doi: 10.1093/oxfordjournals.aje.a114534. [DOI] [PubMed] [Google Scholar]
- Compton WM, Cottler LB. The Diagnostic Interview Schedule. In: Hersen M, Segal DL, Hilsenroth MJ, editors. The Comprehensive Handbook of Psychological Assessment, Volume 2: Personality Assessment. Hoboken, NJ: 2004. pp. 153–162. [Google Scholar]
- Culverhouse R, Bucholz KK, Crowe RR, Hesselbrock V, Nurnberger JI, Porjesz B, Schuckit MA, Reich T, Bierut LJ. Long-term stability of alcohol and other substance dependence diagnoses and habitual smoking: An evaluation after 5 years. Arch. Gen. Psychiatry. 2005;62:753–760. doi: 10.1001/archpsyc.62.7.753. [DOI] [PubMed] [Google Scholar]
- Dawson DA. Correlates of past-year status among treated and untreated people with former alcohol dependence. Alcohol. Clin. Exp. Res. 1996a;20:771–779. doi: 10.1111/j.1530-0277.1996.tb01685.x. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Archer L, Grant BF. Reducing alcohol-use disorders via decreased consumption: A comparison of population and high-risk strategies. Drug Alcohol Depend. 1996b;42:39–47. doi: 10.1016/0376-8716(96)01260-4. [DOI] [PubMed] [Google Scholar]
- Dawson DA. U.S. Low-risk drinking guidelines: An examination of four alternatives. Alcohol. Clin. Exp. Res. 2000;24:1820–1829. [PubMed] [Google Scholar]
- Dawson DA. Toward the attainment of low-risk drinking goals: a 10 year progress report. Alcohol. Clin. Exp. Res. 2004;28:1371–1378. doi: 10.1097/01.alc.0000139811.24455.3e. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005a;100:281–292. doi: 10.1111/j.1360-0443.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Li T. Quantifying the risks associated with exceeding recommended drinking limits. Alcohol. Clin. Exp. Res. 2005b;29:902–908. doi: 10.1097/01.alc.0000164544.45746.a7. [DOI] [PubMed] [Google Scholar]
- De Bruijn C, van den Brink W, de Graaf R, Vollebergh WAM. The three year course of alcohol use disorders in the general population: DSM-IV, ICD-10 and the Craving Withdrawal Model. Addiction. 2006;101:385–392. doi: 10.1111/j.1360-0443.2006.01327.x. [DOI] [PubMed] [Google Scholar]
- Demallie DA, Cottler LB, Compton WM. Alcohol abuse and dependence: consistency in reporting of symptoms over ten years. Addiction. 1995;90:615–625. doi: 10.1046/j.1360-0443.1995.9056153.x. [DOI] [PubMed] [Google Scholar]
- Ewing JA. Detecting Alcoholism: The CAGE Questionnaire. JAMA. 1984;252:1905–1907. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- Finney JW, Moos RH. The long-term course of treated alcoholism: I. Mortality, relapse and remission rates and comparisons with community controls. J. Stud. Alcohol. 1991;52:44–54. doi: 10.15288/jsa.1991.52.44. [DOI] [PubMed] [Google Scholar]
- Grant BF. Prevalence and correlates of alcohol use and DSM-IV alcohol dependence in the United States: Results of the National Longitudinal Alcohol Epidemiologic Survey. J. Studies Alcohol. 1997;58:464–473. doi: 10.15288/jsa.1997.58.464. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grazier KL, Bucholz KK, Compton WM. Health services use of community alcoholics compared to controls. Alcohol Clin. Exp. Res. 1999;23:133A. [Google Scholar]
- Helzer JE, Burnam A, McEvoy LT. Alcohol abuse and dependence. In: Robins LN, Regier DA, editors. Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. New York, NY: 1991. pp. 81–115. [Google Scholar]
- Helzer JE, Robins LN, McEvoy LT, Spitznagel EL, Stoltzman RK, Farmer A, Brockington IF. A comparison of clinical and diagnostic interview schedule diagnoses: Physician reexamination of lay-interviewed cases in the general population. Arch. Gen. Psychiatry. 1985;42:657–666. doi: 10.1001/archpsyc.1985.01790300019003. [DOI] [PubMed] [Google Scholar]
- Holdcraft LC, Iacono WG. Cohort effects on gender differences in alcohol dependence. Addiction. 2002;97:1025–1036. doi: 10.1046/j.1360-0443.2002.00142.x. [DOI] [PubMed] [Google Scholar]
- Johnson PB, Richter L, Kleber HD, McLellan AT, Caris D. Telescoping of drinking-related behaviors: gender, racial/ethnic, and age comparisons. Subst. Use Misuse. 2005;40:1139–1151. doi: 10.1081/JA-200042281. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA) National Longitudinal Alcohol Epidemiologic Survey. Rockville, MD: NIAAA; 1991–1992. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA) Are women more vulnerable to alcohol’s effects? Alcohol Alert. 1999;46 [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA) National Epidemiologic Survey on Alcohol and Related Conditions. Rockville, MD: NIAAA; 2001–2002. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA) Helping Patients Who Drink Too Much: A Clinician’s Guide. Rockville, MD: NIAAA; 2005. [Google Scholar]
- National Institute of Mental Health (NIMH) Epidemiologic Catchment Area Study. Rockville, MD: U.S. Dept. of Health and Human Services, NIMH; 1980–1985. [Google Scholar]
- Noda T, Imamichi H, Kawati A, Hirano K, Ando T, Iwata Y, Yoneda H. Long-term outcome in 306 males with alcoholism. Psychiatry Clin Neurosci. 2001;55:579–586. doi: 10.1046/j.1440-1819.2001.00909.x. [DOI] [PubMed] [Google Scholar]
- Ojesjo L, Hagnell O, Otterbeck L. The course of alcoholism among men in the Lundby Longitudinal Study, Sweden. J. Stud. Alcohol. 2000;61:320–322. doi: 10.15288/jsa.2000.61.320. [DOI] [PubMed] [Google Scholar]
- O’Rourke N, Hatcher L, Stepanski EJ. A Step-by-Step Approach to Using SAS® for Univariate and Multivariate Statistics. Second Edition. Cary, NC: SAS Institute Inc.; 2005. [Google Scholar]
- Powell BJ, Landon JF, Cantrell PJ, Penick EC, Nickel EJ, Liskow BI, Coddington TM, Campbell JL, Dale TM, Vance MD, Rice AS. Prediction of drinking outcomes for male alcoholics after 10 to 14 years. Alcohol Clin. Exp. Res. 1998;22:559–566. doi: 10.1111/j.1530-0277.1998.tb04293.x. [DOI] [PubMed] [Google Scholar]
- Randall CL, Roberts JS, Del Boca FK, Carroll KM, Connors GJ, Mattson ME. Telescoping of landmark events associated with drinking: A gender comparison. J. Stud. Alcohol. 1999 doi: 10.15288/jsa.1999.60.252. [DOI] [PubMed] [Google Scholar]
- Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: An overview. Addiction. 2003;98:1209–1228. doi: 10.1046/j.1360-0443.2003.00467.x. [DOI] [PubMed] [Google Scholar]
- Robins LN, Cottler LB, Bucholz KK, Compton WM, North CS, Rourke KM. Diagnostic Interview Schedule for DSM-IV. St. Louis, MO: 1999. [Google Scholar]
- Robins LN, Helzer JE, Cottler LB, Goldring E. NIMH Diagnostic Interview Schedule. Version III revised. St. Louis, MO: 1988. [Google Scholar]
- Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule: It’s history, characteristics and validity. Arch. Gen. Psychiatry. 1981b;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Croughan J, Williams JBW, Spitzer RL. NIMH Diagnostic Interview Schedule. Version III. Rockville, MD: National Institute of Mental Health; 1981a. [DOI] [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Orvaschel H, Anthony JC, Blazer DG, Burnam A, Burke JD. The Diagnostic Interview Schedule. In: Eaton WW, Kessler LG, editors. Epidemiologic Field Methods in Psychiatry: The NIMH Epidemiologic Catchment Area Program. Orlando, FL: 1985. pp. 143–170. [Google Scholar]
- Robins LN, Helzer JE, Ratcliff KS, Seyfried W. Validity of the Diagnostic Interview Schedule, Version II: DSM-III diagnoses. Psychological Medicine. 1982;12:855–879. doi: 10.1017/s0033291700049151. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Smith TL, Danko GP, Bucholz KK, Reich T, Bierut L. Five-Year Clinical Course Associated With DSM-IV Alcohol Abuse or Dependence in a Large Group of Men and Women. Am. J. Psychiatry. 2001;158:1084–1090. doi: 10.1176/appi.ajp.158.7.1084. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Smith TL, Landi NA. The 5-year clinical course of high-functioning men with DSM-IV alcohol abuse or dependence. Am. J. Psychiatry. 2000;157:2028–2035. doi: 10.1176/appi.ajp.157.12.2028. [DOI] [PubMed] [Google Scholar]
- Vaillant GE. A 60-year followup of alcoholic men. Addiction. 2003;88:1043–1051. doi: 10.1046/j.1360-0443.2003.00422.x. [DOI] [PubMed] [Google Scholar]
- Wilsnack RW, Kristjanson AF, Wilsnack SC, Crosby RD. Are U.S. women drinking less (or more)? Historical and aging trends, 1981–2001. J. Stud. Alcohol. 2006;67:341–348. doi: 10.15288/jsa.2006.67.341. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


