Abstract
Background
For patients with peripheral arterial disease (PAD), depression is associated with worse patency and recurrent symptoms in the treated leg, but its association with death or cardiovascular events in other vascular beds is unknown.
Objective
To assess the association between depression and mortality or cardiovascular events outside the affected leg after PAD revascularization.
Design
Retrospective cohort study.
Subjects
Two hundred fifty-seven consecutive patients undergoing lower extremity revascularization for symptomatic PAD at a single institution between January 2000 and May 2005 were included in this study. By protocol, patients were previously screened for depression and diagnosed by the primary care provider.
Measurements
The outcomes evaluated included a composite of death or major adverse cardiovascular events (MACE; coronary heart disease, contralateral PAD, or cerebrovascular event) as well as major outcome categories of death, coronary heart disease, contralateral PAD, or cerebrovascular events.
Results
At revascularization, 35.0% patients had been diagnosed with depression. Those with depression were significantly younger and more likely to use tobacco. By life-table analysis, patients with depression had significantly increased risk for death/MACE, coronary heart disease, and contralateral PAD events, but not cerebrovascular events or death. By multivariate analysis, patients with depression were at significantly increased risk for death/MACE (hazard ratio [HR] = 2.05; p < .0001), contralateral PAD (HR = 2.20; p = .009), and coronary heart disease events (HR = 2.31; p = .005) but not cerebrovascular events or death.
Conclusions
Depression is common among patients undergoing revascularization for symptomatic PAD. After intervention, patients with depression are at significantly increased risk for coronary heart disease events and progression of contralateral PAD. Prospective analysis is required to confirm these results.
KEY WORDS: peripheral arterial disease, depression, follow-up study, disease progression, cardiovascular disease
INTRODUCTION
Depression is common among patients with coronary heart disease1–4 and peripheral arterial disease (PAD).5–7 For patients with acute coronary syndromes, depression is a risk factor for recurrent cardiovascular events and mortality.8–10 After coronary artery bypass surgery, it is associated with increased risk for recurrent cardiovascular events,4,11 rehospitalization for cardiac events,12 repeat coronary revascularization,4 and death.3,13,14 For patients with symptomatic PAD, we have previously described an association between depression and worse outcomes in the revascularized leg.5 By multivariate analysis, patients with depression at the time of PAD revascularization were at increased risk for recurrent symptomatic PAD in the treated leg and failure of revascularization. However, this study did not address the risk for cardiovascular events in vascular territories outside the treated leg. Previous reports have demonstrated an association between depression and adverse outcomes for patients undergoing coronary revascularization. Patients undergoing revascularization for PAD are at increased risk for secondary atherosclerotic events (including progression of PAD in the contralateral leg). However, we are not aware of any studies that have examined the relationship between depression and mortality or secondary cardiovascular events after lower extremity revascularization for symptomatic PAD.
The purpose of this study is to assess the relationship between depression and mortality or cardiovascular events outside the treated leg after PAD intervention. The study hypothesis is that patients with depression will have an increased risk of death or cardiovascular events after lower extremity revascularization for symptomatic PAD.
METHODS
Study Population
From January 2000 to May 2005, 263 patients had lower extremity revascularization for symptomatic PAD at the Western New York Veteran’s Administration Hospital. Two hundred fifty-seven patients met the inclusion criteria (symptomatic chronic atherosclerotic occlusive PAD, ability to complete a depression evaluation) and 6 were excluded from the study because they could not complete a depression evaluation (severe dementia, 5 patients; chronic schizophrenia and aphasia, 1 patient). Electronic medical records were retrospectively reviewed for all patients. Preoperative variables (based upon both clinical factors and test results), periprocedural results, and outcome data (death, coronary heart disease event, incident symptomatic contralateral PAD, or cerebrovascular event) were gathered using recommended reporting standards.15,16 Progression of PAD in the contralateral leg is a cardiovascular event that may be associated with depression and was therefore included as an outcome. Ipsilateral recurrent events or progression of PAD in the treated leg were not included as study end points because a previous report has established that depression is associated with recurrent symptoms and worse patency in this patient cohort.5
Depression was defined as new or persistent symptoms resulting in a recommendation for treatment (antidepressant medication or psychosocial therapy) within the previous year. Because depression is underdiagnosed, hospital guidelines recommend that all outpatients should be evaluated annually for depression using a 2-part protocol. To facilitate the diagnosis of depression, screening was performed using the General Health Questionnaire-12 with a score >3 resulting in further evaluation.17 For all patients, treatment for depression was recommended before the decision was made to intervene for PAD. Depression was not reevaluated at the time of PAD intervention. Care was taken to elucidate the indication for bupropion therapy (depression versus tobacco cessation).
All patients were symptomatic at the time of PAD revascularization. The indications for intervention included disabling claudication (30.7%), ischemic rest pain (21.0%), and gangrene/nonhealing ulcer (48.2%). Interventions performed included open surgery (51.8%), percutaneous procedures (35.8%), and combined open/endovascular revascularizations (12.5%). All patients were discharged on life-long enteric-coated acetyl salicylic acid (81 mg daily); those receiving angioplasty/stenting were also prescribed at least 6 weeks of clopidogrel (75 mg daily). All patients were given preprocedural beta-blockade, which was titrated to a heart rate <60. After intervention, beta-blockade was continued for at least 30 days.
Outcome Measures
Outcomes recorded included a composite of death or major adverse cardiovascular events (MACE; coronary heart disease, contralateral PAD, or cerebrovascular event). Individual major outcome categories were also analyzed and included incident coronary heart disease events (hospitalization for acute myocardial infarction, unstable angina, or congestive heart failure), cerebrovascular events (hospitalization for transient ischemic attack or ischemic stroke), or revascularization or major amputation (transmetatarsal or leg amputation) for incident symptomatic contralateral PAD. Outcomes were recorded based upon review of the inpatient records, test results, and outpatient evaluations. Mortality data from the Veteran’s Administration database is sensitive with results similar to the National Death Index.18 The electronic medical record includes data from primary care and specialist physicians. Patients are routinely queried about care received at private-sector hospitals. Eleven patients presented with bilateral symptomatic PAD. For these patients, revascularization of the contralateral leg was not considered an outcome event. Follow-up was available for all patients (mean follow-up 28.3 ± 16.2 months).
Statistical Analysis
Statistical analysis was performed using the SAS 9.1 software (SAS Institute, Cary, NC, USA). Descriptive statistics were used to report baseline patient characteristics. Chi-square test and Student’s t test were used to compare demographics, comorbidities, and symptoms for patients with and without depression. The log-rank test was used to examine the association between depression and outcomes of interest.19 Univariate and multivariate analyses were utilized to assess the relationship between preoperative variables and outcomes. Factors in these analyses included: depression; age; diabetes; tobacco use (ever); tobacco use (current or within 1 year); hypertension; dyslipidemia; current statin use; carotid, renal, pulmonary, cerebrovascular, or cardiac disease; previous revascularization of the lower extremity, carotid artery (endarterectomy or angioplasty/stenting), or coronary artery (surgical or angioplasty/stenting); indication for intervention (disabling claudication, rest pain, or gangrene/ulcer), site of intervention (aortoiliac, femoropopliteal, femorotibial), and type of intervention (endovascular, open, or hybrid). The Cox proportional hazard model (with adjustment for other confounders that may affect the outcome) was used to estimate the relative risk for the variables on the selected outcomes.20 All p values are reported as 2-sided with a significant alpha level of 0.05. Approval for this project was obtained from the institutional review board for human subjects’ research at the Western New York Veteran’s Administration Hospital.
RESULTS
Two hundred fifty-seven patients had interventions for symptomatic PAD during the study period. Two hundred twenty-four patients were white (87.2%), 30 patients were black (11.7%), and 3 were Hispanic (1.2%). The mean age at the time of revascularization was 67.5 ± 10.4 years (range 37.7–89.9 years), and the patients were predominantly male (254 males, 98.8%; 3 females, 1.2%).
At the time of revascularization, 90 patients (35.0%) had been recently diagnosed with depression or were receiving antidepressant therapy. Among those recently diagnosed with depression, 16 had refused therapy (17.8%). Seventy-two patients (80.0%) were receiving antidepressant medications, and 2 were receiving psychosocial counseling (2.2%). Because of the small numbers of patients, subgroup analysis based upon the type of antidepressant medication or refusal of therapy was not possible. Data were not available to examine the age at onset of depression.
At the time of lower extremity revascularization, the patient demographics, comorbid conditions, and previous cardiovascular interventions were similar for most variables when patients with and without depression were evaluated (Table 1). When compared to patients without depression, depressed patients were younger at the time of intervention. Renal disease (baseline serum creatinine >1.5 mg/dL or renal replacement therapy) was less common among patients with depression, although there was no difference in the prevalence of severe renal disease (serum creatinine >5.9 or renal replacement therapy; 5.6% vs 4.8%; p = .79). At the time of intervention, depressed patients were more likely to be currently using tobacco or have used it within the previous year but there was no difference in lifetime history of tobacco abuse. Despite increased recent/current use of tobacco, depressed patients were less likely to have pulmonary disease or severe pulmonary disease (1.1% vs 8.4%; p = .02). Data were not available for cumulative tobacco exposure (such as pack per years). There was no difference in the proportion of patients receiving HMG-CoA reductase inhibitor therapy at the time of intervention (55.6% vs 58.1%; p = .70).
Table 1.
Preprocedural Demographics and Comorbidities for Patients with Symptomatic PAD Undergoing Intervention (n = 257 Patients)
| Variable | Depressed | Nondepressed | p value |
|---|---|---|---|
| Age (y) | 64.3 | 69.3 | .0002 |
| Race White (%) | 91.1 | 85.0 | .27 |
| Race African-American (%) | 8.9 | 13.2 | |
| Race Hispanic (%) | 0 | 1.8 | |
| Diabetes (%) | 44.4 | 49.7 | .42 |
| Hypertension (%) | 82.2 | 90.4 | .06 |
| Dyslipidemia (%) | 63.3 | 67.7 | .42 |
| Statin use (%) | 44.4 | 41.9 | .70 |
| Tobacco use (ever) (%) | 94.4 | 88.0 | .10 |
| Tobacco use (within 1 year) (%) | 72.2 | 50.1 | .001 |
| Coronary artery disease (%) | 64.4 | 66.5 | .74 |
| Renal disease (%) | 20.0 | 31.7 | .04 |
| Pulmonary disease (%) | 25.6 | 50.9 | <.0001 |
| Previous coronary revascularization (%) | 17.8 | 25.7 | .15 |
| Cerebrovascular disease (%) | 30.0 | 38.9 | .15 |
| Previous carotid endarterectomy (%) | 7.8 | 10.8 | .44 |
| Previous PAD revascularization (%) | 18.9 | 21.0 | .69 |
| Previous contralateral amputation (%) | 4.4 | 4.2 | .92 |
PAD: peripheral arterial disease
The perioperative course was similar for depressed and nondepressed patients. The site of lower extremity atherosclerotic disease, indication for intervention, and type of revascularization performed were not significantly different for the 2 groups (Table 2). The 30-day mortality was similar for the depressed and nondepressed patients (2.2% vs 4.2%; p = .41), as was the incidence of periprocedural complications (17.8% vs 22.2%; p = .41). At the time of discharge from the hospital, there was no difference in the proportion of depressed and nondepressed patients discharged to home, rehabilitation facility, or nursing home (75.0% vs 74.3%, 5.7% vs 11.4%, 19.3% vs 11.4%; p = .11).
Table 2.
Indications for Revascularization and Site of Intervention (n = 257 Patients)
| Variable | Depressed | Nondepressed | p value |
|---|---|---|---|
| Indication for intervention | |||
| Claudication (%) | 27.8 | 32.3 | .77 |
| Rest pain (%) | 22.2 | 20.4 | |
| Gangrene/tissue loss (%) | 50.0 | 47.3 | |
| Site of reconstructiona | |||
| Aortoiliac reconstruction (%) | 43.3 | 52.7 | .29 |
| Femoral–popliteal reconstruction (%) | 42.2 | 34.1 | |
| Femoral–distal reconstruction | 20.0 | 24.6 | |
| Type of reconstruction | |||
| Open surgery (%) | 50.0 | 52.7 | .91 |
| Percutaneous procedure (%) | 36.7 | 35.3 | |
| Hybrid procedure (%) | 13.3 | 12.0 |
aTwenty-four patients underwent combined aortoiliac and infrainguinal reconstruction. Therefore, the percentage of patients for each group is >100%.
After lower extremity revascularization, death or cardiovascular morbidity was common with only 110 patients (42.8%) alive and free of secondary atherosclerotic events. During follow-up, 81 patients died (excluding 9 periprocedural deaths). Forty-six patients developed symptomatic contralateral PAD that required revascularization (41 patients) or major amputation (5 patients). The proportion of depressed patients receiving primary amputation was similar to nondepressed patients (p = .71). For patients with symptomatic progression of contralateral PAD, the indication for intervention was disabling claudication in 12 patients, ischemic rest pain in 10 patients, and gangrene/ulcer in 24 patients (p = .75 depressed versus nondepressed patients). Thirteen patients had cerebrovascular events (stroke, 9 patients; transient ischemic attack, 4 patients; p = .51 depressed versus nondepressed patients). Fifty-seven patients had coronary heart disease events (congestive heart failure, 6 patients; unstable angina, 25 patients; myocardial infarction, 26 patients; p = .64 depressed versus nondepressed patients).
During follow-up, patients with depression were at increased risk for the composite outcome of death or MACE. With life-table evaluation, depressed patients were significantly more likely to die or suffer a recurrent atherosclerotic event (Fig. 1). By multivariate analysis, depression was a significant and independent predictor of death/MACE (Table 3). When individual major outcome categories were examined, life-table analysis showed that depressed patients had a significantly increased risk of coronary heart disease events and contralateral PAD events but not death or cerebrovascular events (Fig. 2). Multivariate analysis results also showed that depression was significantly associated with coronary heart disease events and contralateral PAD (Table 3).
Figure 1.
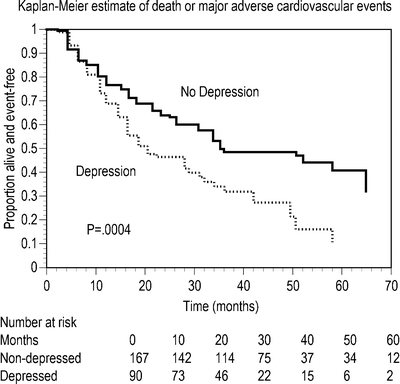
Product–limit estimates of time to death or MACE for 90 patients with depression and 167 patients without depression at the time of intervention
Table 3.
Results of Multivariate Analysis for Outcome Categories According to Baseline Characteristics
| Hazard ratio (95%CI) | p value | |
|---|---|---|
| Death or MACE | ||
| Depression | 2.05 (1.16–2.86) | <.0001 |
| Age (per year) | 1.03 (1.01–1.05) | .0004 |
| Cardiac disease | 1.78 (1.21–2.63) | .003 |
| Death | ||
| Age (per year) | 1.05 (1.03–1.08) | <.0001 |
| Previous contralateral amputation | 2.92 (1.36–6.27) | .006 |
| Cardiac disease | 1.77 (1.05–2.98) | .03 |
| Renal disease | 2.13 (1.39–3.27) | .0006 |
| Gangrene/ulcer as indication for intervention | 2.88 (1.51–5.50) | .001 |
| Coronary heart disease events | ||
| Depression | 1.75 (1.03–2.98) | .04 |
| Cardiac disease | 2.42 (1.28–4.60) | .007 |
| Contralateral PAD | ||
| Depression | 2.20 (1.22–3.96) | .009 |
| Cardiac disease | 2.21 (1.09–4.49) | .03 |
| Infrainguinal PAD | 1.70 (1.19–2.45) | .006 |
| Cerebrovascular events | ||
| Carotid revascularization | 5.51 (1.60–18.92) | .007 |
| Coronary revascularization | 9.87 (2.02–48.38) | .005 |
Figure 2.
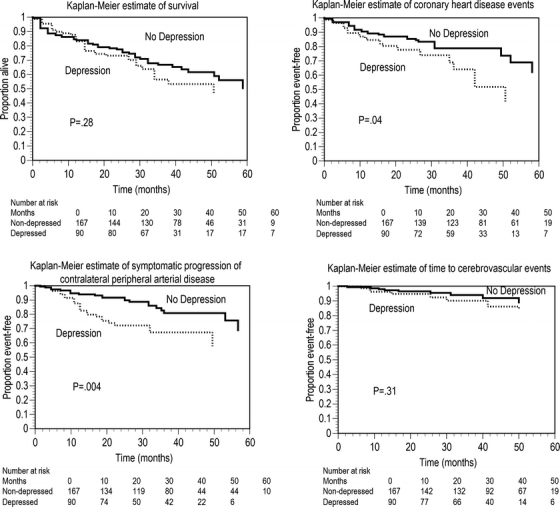
Product–limit estimates of time to death, coronary heart disease event, symptomatic contralateral PAD, or cerebrovascular event for 90 patients with depression and 167 patients without depression at the time of intervention
DISCUSSION
The aim of the present study was to evaluate the association between depression and outcome after revascularization for symptomatic PAD. We found that patients with depression were at significantly increased risk for the combined end point of death or cardiovascular events during follow-up. In particular, multivariate analysis revealed that depression was associated with coronary heart disease events and symptomatic contralateral PAD, but not death or cerebrovascular events. Subjects with and without depression had similar comorbidities and cardiovascular risk factors, except that patients with depression were younger, and more frequently tobacco users, but less likely to have pulmonary or renal disease. We did not find differences in complications, medical care, discharge status, or other factors that may have contributed to the association between depression and adverse outcomes. Despite the overall similarity between the groups, patients with depression were at significantly increased risk for follow-up coronary heart disease or contralateral PAD events. In a separate manuscript, we reported that patients with depression at the time of PAD intervention were at increased risk for failure of the revascularization and recurrent symptoms in the treated leg.5 To our knowledge, the present study is the first to examine the association between depression at the time of PAD intervention and mortality or subsequent cardiovascular events in other vascular beds.
The findings in the present study that patients with depression were at significantly increased risk for progression of contralateral leg PAD or coronary heart disease events deserve further comment. With multivariate analysis, patients with depression had a twofold increased risk of death or MACE during follow-up. This composite end point was chosen in an attempt to obtain a broad understanding of the association between depression and clinically significant events after PAD revascularization. Analysis of each major outcome category revealed that depression was associated with an increased risk for progression of PAD in the contralateral leg (hazard ratio [HR] = 2.20) and coronary heart disease events (HR = 1.75) but not all-cause mortality or cerebrovascular events. However, there were only 13 cerebrovascular events during follow-up, so the study may not have had an adequate sample size to detect this association. Cause of death could not be determined for approximately one third of patients. Although depression was not associated with death from all causes, perhaps an association exists with cardiovascular mortality. Alternatively, depression may have a particular association with PAD and coronary heart disease events after lower extremity revascularization. These questions merit further analysis in future research projects.
The present report adds to a growing body of knowledge regarding depression and PAD, although little previous research examines the associations between depression and severely symptomatic PAD. In our study, 35.0% of patients undergoing revascularization for symptomatic PAD had previously been diagnosed with depression. Previous reports have also described a high prevalence of depression for patients with PAD. A report from the Women’s Health Initiative Study found that women with a history of PAD had a significantly increased risk of current depression.21 Penninx, in a large community-based cohort, noted that significantly more elderly subjects with self-reported PAD had depression than those without PAD (10.6% vs 7.7%).22 However, another population-based study found no association between depression and subclinical PAD.23 In a smaller sample of patients from a single center, Arseven noted depression in 24% of PAD patients not severe enough to require intervention. The authors also found that increasing severity of PAD was associated with significantly more depressive symptoms.6 McDermott found that 21.7% of patients with PAD had a significant number of depressive symptoms (Geriatric Depression Scale score >5). Similar to the present study, depressive symptoms were significantly associated with younger age and current tobacco use.7 The prevalence of depression in the current study was similar to that noted for patients with acute myocardial infarction (15–27%),1 unstable angina (41%),2 and before coronary artery surgery (15.2–32.0%).3,4
The association between depression and coronary heart disease has been more thoroughly described and is addressed by 2 recent metaanalyses. Van Melle concluded that depression at the time of myocardial infarction was associated with all-cause mortality, cardiac mortality, and recurrent cardiac events.10 The metaanalysis by Barth included patients with myocardial infarction, angiographically documented coronary artery disease or coronary revascularization (surgery or angioplasty/stenting). These authors also found an association between depression and mortality after coronary heart disease event.9 Depression is associated with worse outcomes after coronary revascularization. Frasure-Smith linked depression with mortality after coronary artery bypass surgery.8 Borowicz found perioperative depression to be associated with increased risk of recurrent chest pain and repeat coronary revascularization up to 5 years after surgery.4 Another report found that depression was associated with recurrent cardiac events 12 months after cardiac surgery.11
Many associations have been noted that may explain the relationship between depression and coronary artery disease.24 A higher prevalence of atherosclerotic risk factors in depressed patients has been described, including tobacco abuse, obesity, diabetes, and sedentary lifestyle.24 Increased platelet reactivity, a risk factor for both atherosclerosis and acute myocardial infarction, has been described in depressed patients.24 Serotonin, important in both depression and platelet function, has been proposed as the link between depression and platelet reactivity. Dysregulation of both the hypothalamic–pituitary axis and the autonomic nervous system are risk factors for coronary artery disease and are also present in depressed patients.24 It is important to note that patients with depression are more likely to be noncompliant with medical therapy.24 Finally, depression in older adults may be caused by atherosclerotic cerebrovascular disease (vascular depression) with a common pathogenesis as coronary artery disease and PAD.23
Another possible explanation for the observed association between depression and atherosclerosis events is that depression may be a result of the cardiovascular symptoms (such as chronic pain or functional disability).25 Symptomatic PAD is associated with chronic pain, reduced functional status, and a poor health-related quality of life,26 all of which may lead to depression.27 Depression in the elderly has a significant detrimental effect on health-related quality of life,28 and patients with major depression have significant impairments in psychological, physical, and social functioning.29 Intervention for PAD and coronary artery disease is often undertaken to improve health-related quality of life and improve physical functioning. If some of the depressed patients in the present study had persistent depression, perhaps the described association with follow-up PAD revascularization and coronary heart disease events may be explained by depression-related declines in quality of life or physical functioning. Further research is needed to better understand the complex (and possibly bidirectional) relationship between depression and PAD.
There are a number of weaknesses in the current study that should be addressed. Because it is retrospective, the results may reflect the inaccuracies of the medical record or biases of the clinicians or researchers. The study design also prevents any conclusions regarding the directionality of the associations. Because the study population is overwhelmingly male and predominantly white, the results may not be generalizable to women and nonwhite patients. We were unable to assess the adequacy of depression therapy or the severity of depressive symptoms at the time of intervention. Patients with refractory depression or more severe symptoms may represent a subset with increased risk of cardiovascular events. The medical record did not contain complete information regarding age at onset of first depression. Examination of the impact of early onset versus late onset depression may provide a better understanding of the associations described in this report. Patients may have received care outside the Veteran’s Administration system. However, during routine biannual follow-up (in clinic or by phone), all patients were routinely queried regarding cardiovascular events and treatment in other facilities. It is also unlikely that depression status would affect a patient’s decision to seek care in another hospital. Therefore, care received at private-sector hospitals likely did not significantly alter the findings of the study. Finally, depression was not reevaluated at the time of intervention. Therefore, the prevalence of depression may have been underestimated (which would increase the risk for a false-negative study result). However, this study weakness should not affect the conclusions of the report—patients with a recent diagnosis of depression or receiving antidepressant therapy are at increased risk for cardiovascular events after lower extremity revascularization.
In conclusion, depression was common among patients undergoing intervention for symptomatic PAD. After revascularization, depression was associated with death or cardiovascular events, predominantly from coronary heart disease or contralateral PAD. Prospective analysis is required to confirm these results.
Acknowledgements
This work was conducted at, and supported by, the VA Western New York Healthcare System, Buffalo, NY, USA. Doctor Cherr is supported by a grant from the Dennis W. Jahnigen Career Development Scholars Awards Program, which is administered by the American Geriatrics Society through a program funded by The John A. Hartford Foundation of New York City and The Atlantic Philanthropies.
Conflicts of Interest None disclosed.
References
- 1.Rudisch B, Nemeroff CB. Epidemiology of comorbid coronary artery disease and depression. Biol Psychiatry. 2003;54:227–40. [DOI] [PubMed]
- 2.Lespérance F, Frasure-Smith N, Juneau M, Théroux P. Depression and 1-year prognosis in unstable angina. Arch Intern Med. 2000;160:1354–60. [DOI] [PubMed]
- 3.Baker RA, Andrew MJ, Schrader G, Knight JL. Preoperative depression and mortality in coronary artery bypass surgery: preliminary findings. ANZ J Surg. 2001;71:139–42. [DOI] [PubMed]
- 4.Borowicz L Jr, Royall R, Grega M, et al. Depression and cardiac morbidity 5 years after coronary artery bypass surgery. Psychosomatics. 2002;43:464–71. [DOI] [PubMed]
- 5.Cherr GS, Wang J, Zimmerman PM, Dosluoglu HH. Depression is associated with worse patency and recurrent leg symptoms after lower extremity revascularization. J Vasc Surg. 2007;457:44–50. [DOI] [PubMed]
- 6.Arseven A, Guralnik JM, O’Brien E, et al. Peripheral arterial disease and depressed mood in older men and women. Vasc Med. 2001;6:229–34. [DOI] [PubMed]
- 7.McDermott MM, Greenland P, Guralnik JM, et al. Depressive symptoms and lower extremity functioning in men and women with peripheral arterial disease. J Gen Intern Med. 2003;18:461–7. [DOI] [PMC free article] [PubMed]
- 8.Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation. 1995;91:999–1005. [DOI] [PubMed]
- 9.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66:802–13. [DOI] [PubMed]
- 10.van Melle JP, de Jonge P, Spijkerman TA, et al. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosom Med. 2004;66:814–22. [DOI] [PubMed]
- 11.Connerney I, Shapiro PA, McLaughlin JS, et al. Relation between depression after coronary artery bypass surgery and 12-month outcome: a prospective study. Lancet. 2001;358:1766–71. [DOI] [PubMed]
- 12.Burg MM, Benedetto MC, Rosenberg R, Soufer R. Presurgical depression predicts medical morbidity 6 months after coronary artery bypass graft surgery. Psychosom Med. 2003;65:111–8. [DOI] [PubMed]
- 13.Burg MM, Benedetto MC, Soufer R. Depressive symptoms and mortality two years after coronary artery bypass graft surgery (CABG) in men. Psychosom Med. 2003;65:508–10. [DOI] [PubMed]
- 14.Blumenthal JA, Lett HS, Babyak MA, et al. Depression as a risk factor for mortality after coronary artery bypass surgery. Lancet. 2003;362:604–9. [DOI] [PubMed]
- 15.Rutherford RB, Baker JD, Ernst C, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997;26:517–38. [DOI] [PubMed]
- 16.Ahn SS, Rutherford RB, Becker GJ, et al. Reporting standards for lower extremity arterial endovascular procedures. J Vasc Surg. 1993;17:1103–7. [DOI] [PubMed]
- 17.Goldberg DP, Gater R, Sartorius N, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. 1997;27:191–7. [DOI] [PubMed]
- 18.Cowper DC, Kubal JD, Maynard C, Hynes DM. A primer and comparative review of major US mortality databases. Ann Epidemiol. 2002;12:462–8. [DOI] [PubMed]
- 19.Peto R, Peto J. Asymptotically efficient rank invariant procedures. J R Stat Soc A. 1972;135:185–207.
- 20.Cox DR. Regression models and life tables. J R Stat Soc B. 1972;34:187–220.
- 21.Wassertheil-Smoller S, Shumaker S, Ockene J, et al. Depression and cardiovascular sequelae in postmenopausal women: the Women’s Health Initiative. Arch Intern Med. 2004;164:289–98. [DOI] [PubMed]
- 22.Penninx BWH, Aartjan TF, Beekman JO, et al. Psychological status among elderly people with chronic diseases: does type of disease play a part? J Psychosom Res. 1996;40:521–34. [DOI] [PubMed]
- 23.Tiemeier H, van Dijck W, Hofman A, et al. Relationship between atherosclerosis and late-life depression: the Rotterdam Study. Arch Gen Psychiatry. 2004;61:369–76. [DOI] [PubMed]
- 24.Lett HS, Blumenthal JA, Babyak MA, et al. Depression as a risk factor for coronary artery disease: evidence, mechanisms, and treatment. Psychom Med. 2004;66:305–15. [DOI] [PubMed]
- 25.Whooley MA. Mind your heart. Ann Intern Med. 2006;144:858–60. [DOI] [PubMed]
- 26.Breek JC, Hamming JF, De Vries J, et al. The impact of walking impairment, cardiovascular risk factors, and comorbidity on quality of life in patients with intermittent claudication. J Vasc Surg. 2002;36:94–9. [DOI] [PubMed]
- 27.Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163:2433–45. [DOI] [PubMed]
- 28.Ruo B, Rumsfeld JS, Hlatky MA, et al. Depressive symptoms and health-related quality of life: the Heart and Soul Study. JAMA. 2003;290:215–21. [DOI] [PMC free article] [PubMed]
- 29.Coulehan JL, Schulberg HC, Block M, et al. Treating depressed primary care patients improves their physical, mental, and social functioning. Arch Intern Med. 1997;157:1113–20. [DOI] [PubMed]


