Abstract
Human γδ T cells are considered to play an important role in the early response to infection with intracellular pathogens. Evidence has been presented that the percentage of γδ T cells with Vc9Vd2 phenotype is dramatically increased in the peripheral blood of patients with acute brucellosis. This specific γδ T-cell subpopulation is known to be activated by small non-peptidic molecules that can either be produced by the pathogen itself or released from damaged cells after infection. In the present work we provide evidence that Vγ9Vδ2 T lymphocytes from peripheral blood mononuclear cells of healthy donors can be specifically activated by non-peptidic low-molecular-weight compound(s) from Brucella suis lysate. Moreover, we show that Vγ9Vδ2 T cells activated by this B. suis fraction produce tumour necrosis factor-α and interferon-γ, which reduce bacterial multiplication inside infected cells.
INTRODUCTION
Members of the genus Brucella are Gram-negative facultative intracellular bacteria that cause the most widespread zoonose worldwide, mostly in developing countries.1 Among Brucella species, B. melitensis, B. abortus, B. suis and B. canis are pathogenic for humans. After infection, most patients show an acute phase with undulant fever, which can progress either to recovery or to a chronic form of the disease. Recovery from Brucella infection is believed to be the result of a cell-mediated immune response.2, 3 Interestingly, Bertotto et al.4 have shown that the number of γδ T lymphocytes expressing the Vγ9 and Vδ2 gene products is dramatically increased in peripheral blood of patients infected with B. melitensis. Increase of Vγ9Vδ2 T cells is not restricted to Brucella infection as this phenomenon is also observed in many other pathogenic infections.5–14 Even though the exact function of Vγ9Vδ2 T cells has not yet been defined, these reports suggest that Vγ9Vδ2 T cells could play a central role in immunity against human pathogens.15, 16 This human T-cell subset displays a particular feature in that it is specifically stimulated by low-molecular-weight non-peptidic molecules displaying a phosphoester moiety.17–20 It has been postulated that γδ T cells could be activated by metabolites released by the pathogen or by ligands released by damaged cells after infection.15 These observations therefore prompted us to investigate whether Brucella molecules exist that can activate human Vγ9Vδ2 T cells and whether these activated cells have any effect on bacterial multiplication inside infected cells.
MATERIALS AND METHODS
Antibodies and reagents
Anti-CD3 (UCHT1), anti-pan αβ T-cell receptor (TCR), anti-pan γδ TCR, anti-Vγ9, anti-Vδ2, fluorescein isothiocyanate (FITC)-conjugated anti-Vδ2 and phycoerythrin (PE)-conjugated anti-CD3 antibodies were all from Immunotech (Marseille, France). Anti-human tumour necrosis factor-α (TNF-α) was from R & D Systems Inc. (Minneapolis, MN). Isopentenyl pyrophosphate (IPP), was from Sigma (St. Louis, MO).
Cells
Peripheral blood mononuclear cells (PBMC) from healthy donors were cultured at 2 × 106 cells/ml in RPMI-1640 supplemented with 10% heat-inactivated fetal calf serum (FCS) and gentamycin (20 µg/ml). In some experiments, αβ TCR-negative Jurkat T-cell mutants transfected with the Vγ9/Vδ2 TCR (DBS43), 21 kindly supplied by Dr Bukowski and Dr Brenner (Dept of Rheumatology and Immunology, Harvard Medical School, Harvard University, Boston, MA), were also used. Myelomonocytic THP-1 cells were cultured in the same medium.
Preparation of Brucella antigen
A 16-ml preculture of B. suis 1330 (American Type Culture Collection [ATCC], Rockville, MD) was added to 2·0 l of tryptic soy broth (TS) medium and grown to an optical density (OD) of 1·0 (540 nm). After two washes in phosphate-buffered saline (PBS), the bacteria were pelleted by centrifugation. The pellet was resuspended in 50 ml of H2O and autoclaved. The preparation was then centrifuged and clarified through a 0·2-µm filter. The supernatant was lyophilized and resuspended in 4 ml of PBS (B. suis extract). Some lysates were filtered through a 3000 molecular weight (MW) AMICON cut-off membrane (Millipore, Saint Quentin en Yvelines, France); after chloroform extraction, the fraction < 3000 MW was lyophilized and resuspended in 4 ml of PBS. This Brucella fraction was termed BSF. Heat-killed B. suis (HKBS) were B. suis bacteria killed by heating for 2 hr at 65° followed by treatment with an antibiotic (gentamycin 1·5 mg/ml) for 2 hr.
γδ T-cell expansion
PBMC were incubated either with IPP (40 µm), or with BSF (20 µl/ml), in the presence of recombinant interleukin (IL)-2 (rIL-2) (250 U/ml). Cells were harvested after 11 or 18 days of culture and the percentage of γδ T cells was determined by flow cytometry (FACS Vantage; Becton-Dickinson, San Jose, CA). In some experiments, γδ T-cell activation was performed on γδ-enriched T cells using anti-γ9 monoclonal antibody (mAb) and anti-immunoglobulin G (IgG)-coated Dynal magnetic beads (Dynal, Compiègne, France). After long-term culture (3–4 weeks) in the presence of rIL-2 (100 U/ml), the cells were restimulated after IL-2 deprivation. These cells were used for TNF-α and interferon-γ (IFN-γ) production.
Analysis of Cγ and IL-2 mRNA expression by using the reverse transcription–polymerase chain reaction (RT–PCR)
PBMC (107 cells) or DBS43 (106 cells) were stimulated with mAbs or Brucella extracts for 4 days or 6 hr, respectively. rIL-2 (250 U/ml) was added to the culture of PBMC. DBS43 cells were stimulated with phorbol 12-myristate 13-acetate (PMA). Cells were then lysed and total RNA was isolated using TRIzol™ (GibcoBRL, Cergy Pontoise, France), as described by the manufacturer. Reverse transcription was performed at 42° for 90 min on 5 µg of total RNA using Superscript reverse transcriptase II (Gibco BRL) and oligo(dT). Each synthesized cDNA (0·1 ng) was amplified as follows using Taq polymerase (Eurogentec, Seraing, Belgium) and 1 µm of specific primers: Cγ primers (for stimulated PBMC), 5′-AACATACCTTTGTCTTCTTG-3′ (sense) and 5′-GTACATGTAATATGCAGAGG-3′ (antisense) (29 cycles of 1 min at 95°, 1 min at 60° and 1 min at 72°); and IL-2 primers (for activated DBS43), 5′-GTCACAAACAGTGCACCTAC-3′ (sense) and 5′-ATGGTTGCTGTCTCATC-AGC-3′ (antisense) (28 cycles of 10 seconds at 95°, 30 seconds at 60° and 20 seconds at 72°). Amplification of β2 microglobulin was used as a control:5′-CCAGCAGAGAATGGAAAGTC-3′ (sense) and 5′-GATGCTGCTTACATGTC-TCG-3′ (antisense). All the oligonucleotide primer pairs were purchased from Eurobio (Les Ulis, France).
TNF-α and IFN-γ assays
γδ T cells were resuspended (at 2 × 106 cells/ml) in complete medium without IL-2. IPP (40 µm) or BSF (20 µl/ml) were or were not added to the culture; after 24 hr the supernatants were assayed for the presence of TNF-α. Serial twofold dilutions of each supernatant were tested in quadruplicate. The assay was performed as described previously22 using L929 fibroblasts. For measurement of IFN-γ concentration, 24-hr culture supernatants were analysed using a commercial enzyme-linked immunosorbent assay (ELISA) kit for IFN-γ (Genzyme, Cambridge, MA).23
Protease treatment of the stimulatory compounds
IPP and BSF or RPMI-1640 alone (as a control) were treated with 100 µg/ml of proteinase K (Sigma) for 30 hr at 37°. The enzymatic reaction was stopped by heating the samples at 65° for 5 min.20 As a control, untreated compounds were also heated for 5 min at 65°. The efficacy of this protease treatment was tested by performing an assay to check inhibition of the ability of an anti-CD3 mAb to stimulate T lymphocytes (results not shown).
THP-1 infection and co-culture with γδ T cells
Myelolomonocytic THP-1 cells (3 × 105/ml) were cultured with 107 m 1,25 dihydroxyvitamine D3 (VD) (Hoffmann La Roche, Basel, Switzerland).24 After 72 hr, the cells were differentiated and became adherent to plastic. After removing the culture medium, the adherent cells were infected with B. suis 1330 (at a multiplicity of infection [MOI] of 30) in 200 µl of complete medium. After 1 hr, the cells were washed with PBS, and 400 µl of complete medium containing 90 µg/ml of gentamycin was added to the adherent cells. Gentamycin-containing medium alone (600 µl) or a suspension of 2 × 106γδ T cells in this medium was placed in a separate chamber, which was then immersed in the culture well. Vγ9Vδ2 T cells were or were not stimulated with IPP (40 µm) or BSF (20 µl/ml). After 1·5, 7, 24 or 48 hr, adherent THP-1 cells were washed and lysed with 0·2% Triton-X-100. Serial 10-fold dilutions of the lysates were plated on TS-agar. The colony-forming units (CFU) were evaluated after 48 hr of incubation at 37°. In some experiments, supernatants from the 24-hr culture of activated Vγ9Vδ2 T cells were used instead of cells themselves put in separate chambers; when indicated, these supernatants were treated with anti-TNF-α mAb (3·2 µg/ml).
RESULTS
Stimulation of Vγ9Vδ2 T cells by B. suis extracts
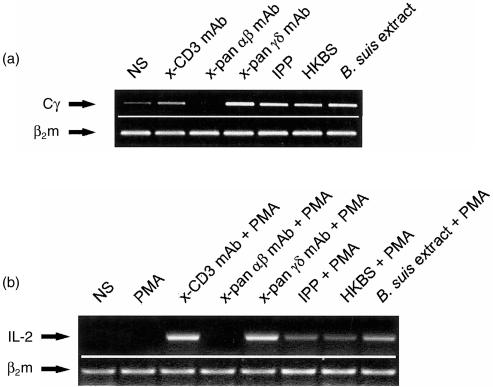
PBMC were cultured in the presence of either B. suis crude extract or HKBS (at a MOI of 100) and rIL-2. After a 4-day culture, the presence of mRNA encoding the TCR Cγ-chain was investigated using RT–PCR. IPP, which specifically activates Vγ9Vδ2 T cells, 18 was used as a positive control. Moreover, anti-CD3 mAb, a polyclonal activator of both αβ and γδ T cells, and anti-pan αβ mAb and anti-pan γδ mAb, were used as specific mitogens for αβ and γδ T lymphocytes, respectively. As shown in Fig. 1(a), a 343-bp cDNA fragment of the Cγ-chain was amplified in cells stimulated with anti-γδ mAb as well as with IPP, HKBS and B. suis crude extract. In anti-CD3-stimulated lymphocytes, the low intensity of the band can be explained by the fact that the majority of stimulated and dividing cells in these specific conditions are αβ T cells. No band was detected using anti-αβ mAb as a negative control. In order to confirm whether B. suis was able to activate Vγ9Vδ2-expressing cells, Vγ9Vδ2 TCR-transfected Jurkat cells were stimulated with B. suis crude extracts as well as with HKBS. A subclone of the DBS43 clone, obtained by transfecting Vγ9Vδ2 genes into a TCR-negative variant of the Jurkat cell line, was used. The resulting transfectant displayed the characteristics of Vγ9Vδ2 primary lymphocytes from human peripheral blood in terms of a specific response to non-peptidic phospholigands.21 These cells were therefore stimulated in the presence of PMA as a costimulatory signal, with IPP, B. suis crude extract or HKBS. Analysis of the expression of IL-2 mRNA using RT–PCR showed (Fig. 1b) an amplification fragment in positive controls, i.e. anti-CD3, anti-γδ mAb or IPP, but also in cells activated with B. suis crude extract or HKBS. In contrast, no stimulation was detected in cells stimulated with PMA alone or with anti-TCR αβ mAb. This result confirmed the presence, in B. suis crude extract, of (an) antigen(s) with the ability to directly activate Vγ9Vδ2 TCR-expressing lymphocytes.
Figure 1.
Expansion of Vγ9Vδ2-bearing cells in response to heat-killed Brucella suis (HKBS) or B. suis extract. (a) Proliferation of γδ T cells from culture of peripheral blood mononuclear cells PBMC was determined by amplification of the Cγ transcript fragment using reverse transcription–polyerase chain reaction (RT–PCR) after 4 days of stimulation with HKBS or with B. suis crude extract. Anti-CD3 monoclonal antibody (mAb) was used as a general polyclonal T-cell mitogen, isopentenyl pyrophosphate (IPP) or anti-pan γδ mAb as specific γδ T-cell activators, and anti-pan αβ mAb as a negative control. The intensity of the bands is clearly higher above basal level (non-stimulated [NS]) in HKBS and B. suis extract as well as in positive controls (anti-pan γδ mAb and IPP). (This is a representative experiment of at least five.) (b) Stimulation of DBS43 was performed in the presence of phorbol 12-myristate 13-acetate (PMA) as a costimulatory signalling molecule. Cell activation was estimated by amplification of the interleukin-2 (IL-2) mRNA fragment using RT–PCR after 6 hr of stimulation. PMA alone, inefficient for stimulating Jurkat cells, was used as a negative control. Other positive and negative controls were similar to those used in Figure 1a). HKBS and B. suis extract, as well as positive controls (anti-CD3, anti-pan γδ mAb and IPP), appear to induce IL-2 gene transcription in these Vγ9Vδ2-transfected Jurkat cells. (This is a representative experiment out of three.)
Study of the stimulatory activity of the low-molecular-weight fraction from B. suis towards γδ T cells
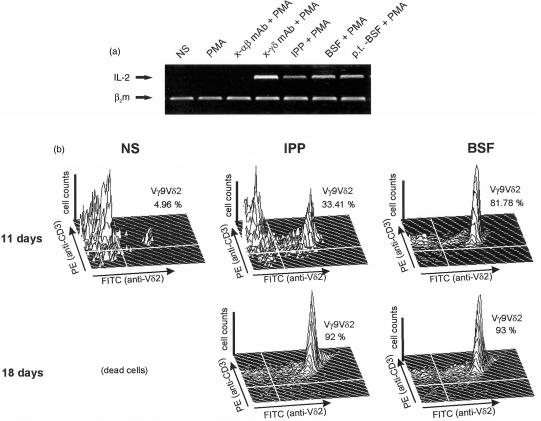
Because Vγ9Vδ2 T cells are normally stimulated with small non-peptidic molecules, a fraction (BSF) smaller than 3000 MW was prepared from a B. suis crude extract. This fraction exhibiting a UV spectrum with no evidence of the presence of peptides was treated with or without proteinase K and then tested for its ability to induce IL-2 mRNA expression in DBS43. As shown in Fig. 2(a), both untreated and protease-treated BSF were able to induce IL-2 mRNA expression. These results strongly suggest the presence in BSF of (a) non-peptidic γδ-activating molecule(s). It has to be noted that, although the IPP stimulatory activity was clearly blocked with phosphatase19, 20 and pyrophosphatase12 treatment, that of BSF was not inhibited under the same experimental conditions, suggesting that the active molecule could be a non-phosphorylated compound.
Figure 2.
Activation of Vγ9Vδ2 cells by Brucella suis low-molecular-weight fraction (BSF). (a) A B. suis fraction (of < 3000 MW), from crude extract (BSF), was treated or untreated with proteinase K and tested for its ability to stimulate Vγ9Vδ2-transfected Jurkat cells. Activation was estimated as described in Figure 1(b) by amplification of the interleukin-2 (IL-2) mRNA fragment using reverse transcription–polymerase chain reaction (RT–PCR) after 6 hr of stimulation. The positive and negative controls were anti-γδ monoclonal antibody (mAb), isopentenyl pyrophosphate (IPP) and anti-αβ mAb, respectively. BSF induced IL-2 gene transcription activation and was not impaired after protease treatment (p.t.-BSF). This experiment was repeated twice. (b) Human peripheral blood mononuclear cells (PBMC) were unstimulated or stimulated with IPP or BSF. Vγ9Vδ2 expansion was evaluated after 11 days or 18 days of culture by double staining (phycoerythrin [PE]-anti-CD3 mAb and fluorescein isothiocyanate [FITC]-anti-Vδ2 mAb) and flow cytometry analysis. After 18 days, the majority of the remaining viable cells were Vγ9Vδ2-expressing lymphocytes. (This is a representative experiment out of at least three.)
The preceding results show that BSF is able to stimulate Vγ9Vδ2 TCR-expressing cells. However, it was unknown whether it specifically induces proliferation of this T-cell subset. PBMC were therefore cultured for an extended period (11 or 18 days) in the presence of BSF or IPP and rIL-2. The viable cells were analysed by double staining (PE-anti-CD3 and FITC-anti-Vδ2 mAb) and flow cytometry. Figure 2(b) shows that the percentage of Vδ2-positive T cells (which strictly coexpress Vγ9) that at baseline represented ≈ 4%, increased to > 90% after an 18-day stimulation with BSF. Proteinase K treatment as well as phosphatase treatment of BSF did not alter the percentages of recovered Vγ9Vδ2 T cells after long-term culture (results not shown). This experiment clearly demonstrates that a low-molecular-weight, non-peptidic molecule of B. suis can specifically induce proliferation of Vγ9Vδ2 T cells.
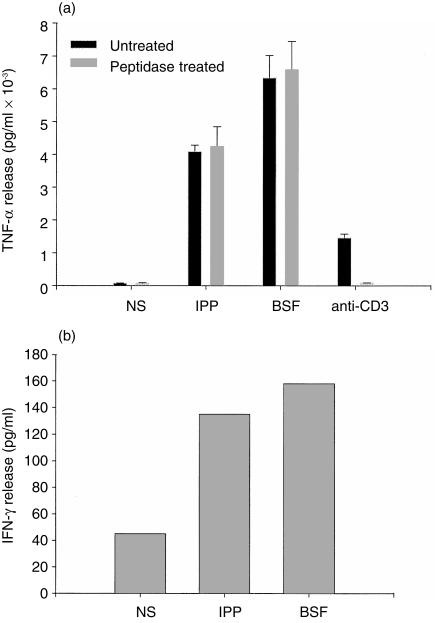
BSF activates Vγ9Vδ2 T cells to produce TNF-α and IFN-γ
γδ T-cell clones have been shown to produce several cytokines, including TNF-α12, 25 and IFN-γ, 23, 26 upon stimulation with non-peptidic antigens. It was therefore investigated whether these cytokines could be produced by Vγ9Vδ2 T cells upon stimulation with BSF. Vγ9Vδ2 T-cell lines that were established from IPP-stimulated PBMC or purified γδ T cells were stimulated either with IPP or with BSF. Figure 3(a) demonstrates that both antigens were able to trigger Vγ9Vδ2 T cells to produce TNF-α. Peptidase treatment of BSF did not modify its ability to induce TNF-α production. In a similar experiment, it was shown (Fig. 3b) that BSF, as well as IPP, was able to trigger IFN-γ production in purified Vγ9Vδ2 T cells.
Figure 3.
Analysis of tumour necrosis factor-α (TNF-α) and interferon-γ (IFN-γ) production by isopentenyl pyrophosphate (IPP) or Brucella suis low-molecular-weight fraction (BSF)-activated γδ T cells. (a) Human γδ T cells, previously treated or untreated with proteinase K, were stimulated or unstimulated with IPP, BSF or anti-CD3 monoclonal antibody (mAb). After 24 hr, the supernatant was tested for its cytotoxic activity against L929 fibroblasts, and TNF-α level was estimated by comparison to a reference curve established using serial dilutions of human recombinant TNF-α (rTNF-α). Anti-CD3 mAb was used as a proteic mitogenic control to test the efficacy of proteinase K treatment. (This is a representative experiment out of three.) (b) Human γδ T cells were stimulated for 24 hr with IPP or BSF, and the concentration of IFN-γ (in pg/ml) was determined in the resulting culture supernatants by using a commercial IFN-γ enzyme-linked immunosorbent assay (ELISA) kit. (This experiment was repeated twice.)
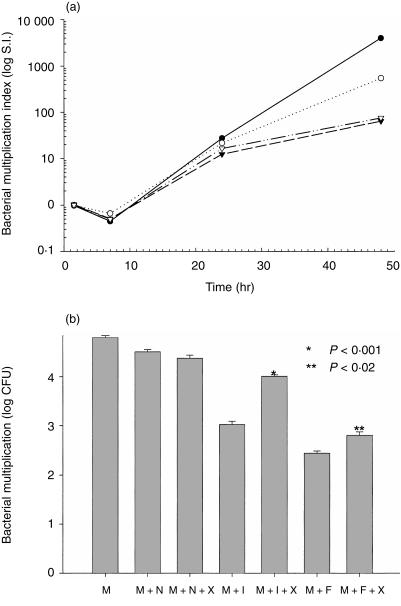
BSF-activated Vγ9Vδ2 T cells impair B. suis multiplication inside the macrophage-like THP-1 cell line
Cytokines have a direct effect on the survival and multiplication of intracellular bacteria.27 Therefore, the effect of activated Vγ9Vδ2 T cells was tested on the multiplication of phagocytized Brucella. A THP-1 myelomonocytic cell model was used that was infected with B. suis, as described previously.24 After treatment with gentamycin to kill residual extracellular bacteria, the infected cells were cultured alone or in the presence of non-activated or of IPP- or BSF-activated Vγ9Vδ2 T cells, the two cell populations being cultured in two separate chambers. After 24–48 hr, a marked decrease in bacterial multiplication was observed in infected THP-1 cells cultured in the presence of IPP- or BSF-activated γδ T cells (Fig. 4a). As expected, maximal TNF-α release was detected in parallel after 24–48 hr in the culture medium (results not shown). Similar results were obtained when supernatants of activated Vγ9Vδ2 T-cell cultures were used with infected THP-1 cells during 24 hr of culture (Fig. 4b). Moreover, Fig. 4(b) shows that the inhibitory effect of bacterial multiplication by supernatants from activated Vγ9Vδ2 T cells could be at least partially reversed by using a blocking anti-TNF-α mAb. Of note, a small decrease was also observed when infected THP-1 cells were incubated in the presence of non-activated γδ T cells.
Figure 4.
Effect of Brucella suis low-molecular-weight fraction (BSF)-activated Vγ9Vδ2 on B. suis multiplication in infected THP-1 cells. (a) THP-1 cells were infected with B. suis and cultured in the absence (•) or in the presence of non-activated (○), isopentenyl pyrophosphate (IPP)-activated (▾) or BSF-activated (▿) Vγ9Vδ2 T cells placed in separate chambers. At several time-points during incubation, infected THP-1 cells were lysed and each lysate was plated on semisolid tryptic soy broth (TS) agar medium. After 48 hr of culture, the intracellular bacteria from each lysate were estimated by evaluating the number of colony-forming units (CFU) (This is a representative experiment out of at least three.) (b) THP-1 were infected with B. suis and cultured in the absence (M) or in the presence of untreated supernatants from a 24-hr non-activated (N) or IPP-(I)- or BSF-(F)-activated Vγ9Vδ2 culture. In parallel, cells were cultured with supernatants that had been pretreated with anti-tumour necrosis factor-α (TNF-α) monoclonal antibody (mAb) (X). After 24 hr of incubation, THP-1 cells were lysed, plated and the number of CFU evaluated as described above. Each experiment was performed in triplicate. Statistical analyses were performed using the Student’s t-test. (This experiment was repeated twice.)
DISCUSSION
The work presented herein demonstrates that BSF, a low-molecular-weight fraction (< 3000 MW) from B. suis, is able to trigger activation of Vγ9Vδ2 T cells. The activity of BSF is resistant to protease treatment indicating that the active molecule is a non-peptidic compound. Numerous molecules stimulating Vγ9Vδ2 T cells were characterized as molecules displaying a phosphate moiety and the activity of these ligands was abolished upon treatment with phosphatase. The activity of the < 3000 MW B. suis fraction we prepared was not abolished upon phosphatase treatment, suggesting that the active compound is not a phospholigand. This result is not totally surprising as a recent publication has shown that Vγ9Vδ2 T cells can also be stimulated with non-phosphorylated alkylamines.28
A study by Bertotto et al.4 has shown that γδ T cells from children with brucellosis were not responsive to heat-killed B. melitensis in vitro. Several hypotheses can be presented to explain the apparent discrepancy between these results and ours. It cannot be excluded that B. melitensis, in contrast to B. suis, produces no Vγ9Vδ2-stimulating non-peptidic antigens. This seems unlikely because, during the acute phase of the infection, these children had a high level of circulating γδ T cells. More likely is another hypothesis based on the results of Bürk et al., 29 showing that γδ T cells stimulated for an extended time-period (which is the case in infected patients) progressively lose their capacity to proliferate in response to non-peptidic antigens. It has also been found that several surface antigens are transiently expressed on these cells upon stimulation with non-peptidic antigens, and their capacity to respond to stimulatory agents appears to be closely related to expression of these antigens (F. Ottones et al., manuscript in preparation).
We established that stimulation of Vγ9Vδ2 T cells with the low-molecular-weight Brucella fraction leads to TNF-α and IFN-γ production. We used Vγ9Vδ2 T cells in coculture with infected THP-1 cells in two separate chambers. The use of two separate chambers, which prevents any physical contact between the two cell populations, allows the effect of a single, diffusible factor to be evaluated. One possibility is that activated Vγ9Vδ2 T cells impair bacterial multiplication through TNF-α production, which overcomes bacterial protection. Indeed, a study from our laboratory22, 24 provided evidence that Brucella prevents TNF-α release from macrophages during infection, thereby assisting the bacterial evasion of antimicrobial defences. Using a blocking anti-TNF-α mAb, we were able to reverse, at least partially, the impairment of bacterial multiplication induced by an activated Vγ9Vδ2 T-cell supernatant. Several cytokines, including TNF-α and IFN-γ, are released by stimulated γδ cells but also by infected monocytic cells. The observed impairment of bacterial multiplication is unlikely to be caused by a single cytokine and is probably caused by several different cytokines acting in synergy, as previously described.30–32 This can explain why an anti-TNF-α mAb can only partially reverse the survival impairment triggered by supernatants from activated γδ T cells. This result suggests that cytokine release triggered upon bacterial non-peptidic antigen stimulation appears to be one of the key events in the protective role played by Vγ9Vδ2 T cells against infection with an intracellular pathogen. We observed a small decrease in bacterial multiplication when infected THP-1 cells were incubated in the presence of non-activated γδ T cells. In fact, when non-activated γδ T cells were cultured in the presence of infected monocytic cells, an increasing amount of cytokine (TNF-α) was detected in the culture medium while no cytokine production was observed when the monocytic cells were uninfected. The possibility exists that small amounts of bacterial non-peptidic antigens are released from infected cells, which stimulate γδ T cells to produce cytokines that might have an effect on bacterial multiplication. No decrease in bacterial survival was observed when untreated or IPP- or BSF-treated αβ T cells were used instead of γδ T lymphocytes (results not shown). Taken together, these results suggest that the cytokines released by γδ T cells stimulated by Brucella antigen could be of crucial importance for the blockade of Brucella replication in the macrophage host cell and thus be of major importance in the progression to remission.
In summary, the results presented herein provide evidence that (a) non-peptidic low-molecular-weight molecule(s) from Brucella is/are able to activate human Vγ9Vδ2 T lymphocytes. Such (a) compound(s) could be responsible for the dramatic increase of Vγ9Vδ2 T cells observed in patients with brucellosis and, through the high-level cytokine production they induce in these cells, appear(s) to be important for the overall immune response triggered during Brucella infection.
Acknowledgments
The authors would like to thank Dr Bukowski and Dr Brenner (Dept of Rheumatology and Immunology, Harvard School of Medicine, Harvard Medical School, Boston, MA) for providing the Vγ9Vδ2-transfected Jurkat cell line (DBS43).
Glossary
Abbreviations
- BSF
Brucella suis fraction
- HKBS
heat-killed Brucella suis
- IFN-γ
interferon-γ
- IPP
isopentenyl pyrophosphate
- mAb
monoclonal antibody
- PBMC
peripheral blood mononuclear cells
- rIL-2
recombinant interleukin-2
- RT–PCR
reverse transcription–polymerase chain reaction
- TNF-α
tumour necrosis factor-α
REFERENCES
- 1.Brinley WJ, Corbel MJ. Brucella infections in man and animals. In: Smith G R, editor. Principles of Bacteriology, Virology and Immunity. Vol. 3. London: Edward Arnold; 1990. p. 548. Bacterial Diseases. [Google Scholar]
- 2.Serre A, Bascoul S, Vendrell JP, Cannat A. Human immune response to Brucella infection. Ann Inst Pasteur Microbiol. 1987;138:113. doi: 10.1016/0769-2609(87)90088-3. [DOI] [PubMed] [Google Scholar]
- 3.Araya LN, Elzer PH, Rowe GE, Enright FM, Winter AJ. Temporal development of protective cell-mediated and humoral immunity in BALB/c mice infected with Brucella abortus. J Immunol. 1989;143:3330. [PubMed] [Google Scholar]
- 4.Bertotto A, Gerli R, Spinozzi F, et al. Lymphocytes bearing the γδ T cell receptor in acute Brucella melitensis infection. Eur J Immunol. 1993;23:1177. doi: 10.1002/eji.1830230531. [DOI] [PubMed] [Google Scholar]
- 5.Barnes PF, Grisso CL, Abrams JS, Band H, Rea TH, Modlin RL. γδ T lymphocytes in human tuberculosis. J Infect Dis. 1992;5:506. doi: 10.1093/infdis/165.3.506. [DOI] [PubMed] [Google Scholar]
- 6.De Paoli P, Gennari D, Martelli P, Cavarzenari V, Comoretto R, Santini G. Gamma delta T cell receptor-bearing lymphocytes during Epstein–Barr virus infection. J Infect Dis. 1990;161:1013. doi: 10.1093/infdis/161.5.1013. [DOI] [PubMed] [Google Scholar]
- 7.De Paoli P, Gennari D, Martelli P, et al. A subset of gamma delta lymphocytes is increased during HIV-1 infection. Clin Exp Immunol. 1991;83:187. doi: 10.1111/j.1365-2249.1991.tb05612.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hara T, Mizuno Y, Takaki K, et al. Predominant activation and expansion of Vγ9-bearing γδ T cells in vivo as well as in vitro in Salmonella infection. J Clin Invest. 1992;90:204. doi: 10.1172/JCI115837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ho M, Webster HK, Tongtawe P, Tattanapanyasat K, Weidanz WP. Increased gamma delta T cells in acute Plasmodium falciparum malaria. Immunol Lett. 1990;25:139. doi: 10.1016/0165-2478(90)90105-y. [DOI] [PubMed] [Google Scholar]
- 10.Jouen-Beades F, Paris E, Dieulois C, et al. In vivo and in vitro activation and expansion of γδ T cells during Listeria monocytogenes infection in humans. Infect Immun. 1997;65:4267. doi: 10.1128/iai.65.10.4267-4272.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Perrera MK, Carter R, Goonewardene R, Mendis KN. Transient increase in circulating gamma/delta T cells during Plasmodium vivax malarial paroxysms. J Exp Med. 1994;179:311. doi: 10.1084/jem.179.1.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Poquet Y, Kroca M, Halary F, et al. Expansion of Vγ9Vδ2 T cells is triggered by Francisella tularensis-derived phosphoantigens in tularemia vaccination. Infect Immun. 1998;66:2107. doi: 10.1128/iai.66.5.2107-2114.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Raziuddin S, Telmasani AW, El-Hag El-Awad M, Al-Amari O, Al-Janadi M. Gamma delta T cells and the immune response in visceral leishmaniasis. Eur J Immunol. 1992;22:1143. doi: 10.1002/eji.1830220506. [DOI] [PubMed] [Google Scholar]
- 14.Scalize F, Gerli R, Castellucci F, et al. Lymphocytes bearing the γδ T cell receptor in acute toxoplasmosis. Immunology. 1992;76:668. [PMC free article] [PubMed] [Google Scholar]
- 15.De Libero G. Sentinel function of broadly reactive human γδ T cells. Immunol Today. 1997;18:22. doi: 10.1016/s0167-5699(97)80010-2. [DOI] [PubMed] [Google Scholar]
- 16.Boismenu R, Havran WL. An innate view of gamma delta T cells. Curr Opin Immunol. 1997;9:57. doi: 10.1016/s0952-7915(97)80159-8. [DOI] [PubMed] [Google Scholar]
- 17.Constant P, Davodeau F, Peyrat MA, et al. Stimulation of human γδ T cells by nonpeptidic mycobacterial ligands. Science. 1994;264:267. doi: 10.1126/science.8146660. [DOI] [PubMed] [Google Scholar]
- 18.Tanaka Y, Morita CT, Tanaka Y, Nieves E, Brenner MB, Bloom BR. Natural and synthetic non peptide antigens recognized by human γδ T cells. Nature. 1995;375:155. doi: 10.1038/375155a0. [DOI] [PubMed] [Google Scholar]
- 19.Schoel B, Sprenger S, Kaufmann SHE. Phosphate is essential for stimulation of Vgamma 9 Vdelta 2 T lymphocytes by mycobacterial low molecular weight ligand. Eur J Immunol. 1994;24:1886. doi: 10.1002/eji.1830240826. [DOI] [PubMed] [Google Scholar]
- 20.Tanaka Y, Sano S, De Nieves E, et al. Non peptide ligands for human γδ T cells. Proc Natl Acad Sci USA. 1994;91:8175. doi: 10.1073/pnas.91.17.8175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bukowski JF, Morita CT, Tanaka Y, Bloom BR, Brenner MB, Band H. Vγ2Vδ2 TCR-dependent recognition of non-peptide antigens and Daudi cells analyzed by TCR gene transfer. J Immunol. 1995;154:998. [PubMed] [Google Scholar]
- 22.Caron E, Peyrat T, Köhler S, Cabane S, Liautard J-P, Dornand J. Live Brucella spp. fail to induce tumor necrosis factor alpha excretion upon infection of U937-derived phagocytes. Infect Immun. 1994;62:5267. doi: 10.1128/iai.62.12.5267-5274.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pichyangkul S, Saengkrai P, Yongvanitchit K, Stewart A, Heppner DG. Activation of γδ T cells in malaria: interaction of cytokines and a schizont-associated Plasmodium falciparum antigen. J Infect Dis. 1997;176:233. doi: 10.1086/514029. [DOI] [PubMed] [Google Scholar]
- 24.Caron E, Gross A, Liautard J-P, Dornand J. Brucella species release a specific, protease-sensitive inhibitor of TNF-α expression active on human macrophage-like cells. J Immunol. 1996;257:2885. [PubMed] [Google Scholar]
- 25.Lang F, Peyrat M-A, Constant P, et al. Early activation of human Vγ9Vδ2 T cell broad cytotoxicity and TNF production by nonpeptidic mycobacterial ligands. J Immunol. 1995;154:5986. [PubMed] [Google Scholar]
- 26.Garcia VE, Sieling PA, Gong JH, et al. Single-cell cytokine analysis of γδ T cell responses to nonpeptide mycobacterial antigens. J Immunol. 1997;159:1328. [PubMed] [Google Scholar]
- 27.Jiang X, Baldwin CL. Effects of cytokines on intracellular growth of Brucella abortus. Infect Immun. 1993;61:124. doi: 10.1128/iai.61.1.124-134.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bukowski JF, Morita CT, Brenner MB. Human γδ T cells recognize alkylamines derived from microbes, edible plants, and tea: implication of innate immunity. Immunity. 1999;11:57. doi: 10.1016/s1074-7613(00)80081-3. [DOI] [PubMed] [Google Scholar]
- 29.Bürk MR, Carena I, Donda A, Mariani F, De Mori L, Libero G. Functional inactivation in the whole population of human Vγ9Vδ2 T lymphocytes induced by a nonpeptidic antagonist. J Exp Med. 1997;185:91. doi: 10.1084/jem.185.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Flesch IE, Kaufmann SH. Activation of tuberculostatic macrophage functions by gamma interferon, interleukin-4, and tumor necrosis factor. Infect Immun. 1990;58:2675. doi: 10.1128/iai.58.8.2675-2677.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leenen PJ, Canono BP, Drevets DA, Voerman JS, Campbell PA. TNF α and interferon γ stimulate a macrophage precursor cell line to kill Listeria monocytogenes in a nitric oxide-independent manner. J Immunol. 1994;153:5141. [PubMed] [Google Scholar]
- 32.Ten Hagen TL, Van Vianen W, Heremans H, Bakker-Woudenberg IA. Differential nitric oxide and TNFα production of murine Kupffer cell subfractions upon priming with IFNγ and TNFα. Liver. 1998;18:299. doi: 10.1111/j.1600-0676.1998.tb00809.x. [DOI] [PubMed] [Google Scholar]