Abstract
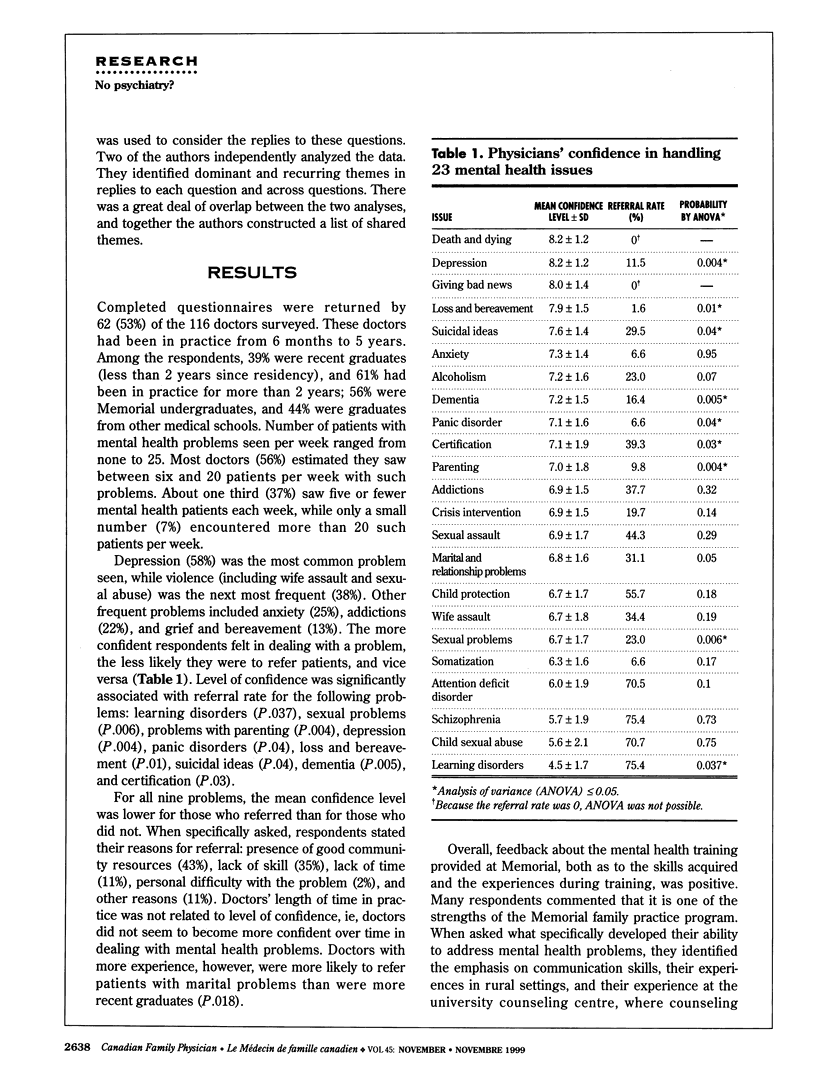
OBJECTIVE: To assess whether the mental health component of the family medicine residency program at Memorial University of Newfoundland, which contains no formal mental health training with psychiatrists, adequately prepares residents for practice, and to assess which aspects of their training enhanced their mental health skills most. DESIGN: Cross-sectional mailed survey. SETTING: A 2-year family practice residency program with a focus on training for rural practice offering integrated and eclectic multidisciplinary mental health training rather than formal psychiatry experience. PARTICIPANTS: Graduates of the family practice residency program, 1990 to 1995. Completed questionnaires were returned by 62 of 116 physicians. MAIN OUTCOME MEASURE: Confidence of respondents in dealing with 23 mental health problems. RESULTS: Respondents felt prepared to address most of the mental health needs of their patients. Higher levels of confidence were associated with lower referral rates. There was no significant relationship between time spent in practice and confidence in dealing with mental health problems. Graduates' confidence correlated with areas in the program identified as strong. CONCLUSIONS: The program appears to train family doctors effectively to meet the mental health needs of their patients.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bonisteel P. Short course in psychiatric emergencies and crisis intervention. Can Fam Physician. 1990 Jun;36:1109–1111. [PMC free article] [PubMed] [Google Scholar]
- Brown J. B., Weston W. W. Training in Psychosocial Issues: Survey of family medicine graduates. Can Fam Physician. 1992 Apr;38:806–812. [PMC free article] [PubMed] [Google Scholar]
- Feightner J. W., Worrall G. Early detection of depression by primary care physicians. CMAJ. 1990 Jun 1;142(11):1215–1220. [PMC free article] [PubMed] [Google Scholar]
- Jones L. R., Badger L. W., Ficken R. P., Leeper J. D., Anderson R. L. Mental health training of primary care physicians: an outcome study. Int J Psychiatry Med. 1988;18(2):107–121. doi: 10.2190/jgyr-82l9-4tv0-qkwd. [DOI] [PubMed] [Google Scholar]
- Kates N. Training psychiatric residents to work with primary care physicians: results of a national survey. Can J Psychiatry. 1993 Mar;38(2):79–82. doi: 10.1177/070674379303800202. [DOI] [PubMed] [Google Scholar]
- Kessler L. G., Cleary P. D., Burke J. D., Jr Psychiatric disorders in primary care. Results of a follow-up study. Arch Gen Psychiatry. 1985 Jun;42(6):583–587. doi: 10.1001/archpsyc.1985.01790290065007. [DOI] [PubMed] [Google Scholar]
- Schurman R. A., Kramer P. D., Mitchell J. B. The hidden mental health network. Treatment of mental illness by nonpsychiatrist physicians. Arch Gen Psychiatry. 1985 Jan;42(1):89–94. doi: 10.1001/archpsyc.1985.01790240091010. [DOI] [PubMed] [Google Scholar]
- Smith R. C., Marshall A. A., Cohen-Cole S. A. The efficacy of intensive biopsychosocial teaching programs for residents: a review of the literature and guidelines for teaching. J Gen Intern Med. 1994 Jul;9(7):390–396. doi: 10.1007/BF02629520. [DOI] [PubMed] [Google Scholar]
- Smith R. C., Mettler J. A., Stöffelmayr B. E., Lyles J. S., Marshall A. A., Van Egeren L. F., Osborn G. G., Shebroe V. Improving residents' confidence in using psychosocial skills. J Gen Intern Med. 1995 Jun;10(6):315–320. doi: 10.1007/BF02599950. [DOI] [PubMed] [Google Scholar]
- Stewart M. A. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995 May 1;152(9):1423–1433. [PMC free article] [PubMed] [Google Scholar]
- Swanson J. G. Family physicians' approach to psychotherapy and counseling. Perceptions and practices. Can Fam Physician. 1994 Jan;40:53–58. [PMC free article] [PubMed] [Google Scholar]


